Abstract
Introduction:
Medical postgraduate student experience considerable stress during their training, which may cause agony to the individual or affect care rendered to the patient. Significant burnout and psychopathology has not been uncommon.
Materials and Methods:
A study was done to assess the relation between perceived stress, coping pattern, burnout, and general psychopathology among the postgraduate medical students.
Results:
Perceived stress was associated with higher scores on general psychopathology and burnout. Postgraduate students who displayed positive coping strategies had lesser perceived stress. Females had higher scores on perceived stress and psychopathology.
Conclusion:
Stress is one of the major growing mental problems among highly educated health professional, and it should not be ignored as it can cause many other health issues.
Keywords: Burnout, coping, medical, perceived stress, postgraduate students
Stress, an internal state, may be due to physical demands put on the body (illnesses, exercise, extremes in temperature, etc.) or the environmental and social conditions which are taken as potentially harmful, beyond control, or exceeding resources of coping in the individual. Stressed condition can lead to many psychological responses such as anxiety, hopelessness, irritability, depression, or a general feeling of being unable to cope with life. Virtually all changes in the environment – be it a pleasant one, for example, a vacation, demands person's ability to cope; and the little stress is productive in helping us to adapt to change. But beyond some point, “stress” becomes “distress.” The act which may lead to distress varies significantly from person to person, but some events seem to be definite stressors for most of us, majority being injuries, infections in the body, harmful, or annoying events in the environment, major transitions in life or changes which drives us to cope in a novel way and the anticipated/actual threats to self-esteem.[1]
Stress is a common problem among undergraduate and the postgraduate medical students since they are expected to imbibe and master a large amount of knowledge, attitudes, and skills for which they do have to strive hard which in turn subject them to a lot of stress.[2] Gender and absence of family support, are also important risk factor.[3]
In India, doctors often find it hard to decide whether they should work or study full-time for the PG entrance examination soon after the graduation.[4] Due to significant disproportion between number of medical graduates passing out and the availability of postgraduate medical seats, doctors do struggle to get their postgraduate seat of interest.[5] Additionally parent and family influences them to take a specialty of their choice, thus adding further to the burden.[6]
After entering a postgraduate medical course, the residents should learn to balance multiple demands in life such as taking responsibility of patients care, financial hardships, on-call schedules, death of patients, need for never-ending learning, updating one-self, the tasks of teaching, requirements of collaborating with physicians and senior residents, along with other necessities of family/personal life.[7] It has been observed that excessive levels of stress may lead to dissatisfactions, decreased morale, and reduced work performance.[8] Factors which have significant negative effects are: heavy patient load, dearth of sleep, absence of regular breaks, non-compromising duty, and too many drab work.[7] However, unfortunately, so many myths around medical profession exist-that doctors are not at the risk of stress, they don’t fall ill or even if they do, help is readily available.[9]
Satisfaction with residency period is the result of a ratio between positive learning and the negative work experience: reward-punishment ratio. If learning is good enough; residents are then willing to tolerate some amount of discomfort, whether it is emanating from the educational environment in general or it is from within a specific individual. However, if the level of discomfort is too much; the quantum of learning declines, frustration rises, and the satisfaction wanes.[9]
It has been seen that at all the level, medical professionals fail to discuss their stress with their colleagues, while the peers choose to ignore the vivid symptoms of stress in the fellow residents. But as a carrier of the patient's anxieties, medical professional's more so postgraduate medical students spend a significant amount of emotional energy handling the wishes of the patients, very often neglecting their own requirements. The prevalence of psychiatric morbidity varies significantly from 6% to 36% depending on the definition of case, nature of sample selection, tools of measurement used, and definition of endpoints.[10] The prevalence found in women doctors is 36% and that in men doctors is 24%.[11] It is also found that medical students as well as the medical professionals don’t seek out for medical help for these problems; which they will otherwise advice for their patients.[12]
Burn-out comprises constellation of symptoms which arises in professionals in relation to their work. Erstwhile hardworking, diligent and committed persons may become increasingly disillusioned, dissatisfied, and cynical in relation to their work and other aspects of the life. Doctors who earlier cared about their patients experience themselves dreading the clinical work and getting more and more detached and uncaring toward their patients.[11] It can be said that doctors are particularly prone to burn-out because of above specified daily challenges faced. Burnout though is a measure of induced distress, has also been seen associated with neuroticism and Type A behavior.[13] Researchers have observed the burnout to be as high as 45% in multicentric studies on medical students.[14] While a burnout or the reaction to stress can be taken as a result of the pressing situation; general psychopathology of anxiety, or depression does point toward a bigger gamut of stress vulnerability interaction or a multifactorial causation. A high level of burnout and depression are not found uncommon in postgraduate medical students.
The coping concept emanates from the psychological studies which were conducted on stress. As per the conceptual analysis of stress by Lazarus and Folkman, principle of coping works on two cognitive appraisals – (a) perception of a threatening scenario and (b) person's available resources to deal with it. Coping as per definition is “cognitive and behavioral efforts to master, reduce or tolerate the internal and/or external demands that are created by the stressful transaction.”[15] While internal disposition is known to affect the distress and burnout, it was observed that the coping strategies of an individual too influence the manifestations significantly. Coping strategies, which are behavioral or psychological efforts employed to master or minimize stressful events, affect the medical residents variably. Studies have revealed that the active coping strategies such as positive reframing, acceptance, and planning affect the mental health outcome favorably whereas avoidant strategies such as denial, drug, or alcohol use worsen the situation.[16]
Although there is adequate study on effects of stress during undergraduate medical training; there are limited data on the effect of stress on postgraduate medical students. Evaluation of perceived stress and its relation to general psychopathology, pattern of coping and burnout in postgraduate medical residents will not only reveal a clear nature, pattern and extent of the problem but as well throw light on stress vulnerability interaction. An insight into prevalence, nature, and extent of burnout and general psychopathology in these doctors will draw us empathetic and primed toward early intervention if required for an improved future. The aim of the present study is to assess the relation between perceived stress, patterns of coping, level of burnout, and general psychopathology among the postgraduate medical students. The objectives are to determine the pattern of perceived stress among postgraduate medical students; to assess the pattern of coping among postgraduate medical students; to determine the presence of significant burnout and general psychopathology among postgraduate medical students, and to ascertain the relation between perceived stress, coping pattern, burnout, and general psychopathology.
MATERIALS AND METHODS
The study was undertaken in a reputed Government Hospital with an established Medical Council of India curriculum. The study was approved by the Institutional Ethics Committee. Around 68 postgraduate medical residents from various departments were taken up for the study after informed consent. A good rapport was established between the investigator and respondent. The instructions of each part of the questionnaires were adequately explained, and care was taken to ensure that they understood the questionnaire. Each participant was requested to respond to each item in the questionnaire freely and frankly without any hesitation. Each participant was asked to clarify for understanding before they attempted to respond.
Structured pro forma was used for recording demographic profile and relevant medical history. Perceived Stress Scale (PSS),[17] a widely used 10-item psychological instrument, was used to measure the degree to which situations in an individual's life are appraised as stressful, over the last 1-month duration. The Brief COPE,[18] a self-report questionnaire, was used to assess a number of different coping behaviors and thoughts the person may have in response to a specific situation. Aspect of coping seen are self-distraction, active coping, denial, substance use, use of emotional support, use of instrumental support, behavioral disengagement, venting, positive reframing, planning, humor, acceptance, religion, and self-blame. General Health Questionnaire (GHQ 12), a self-administered standardized 12-item screening test,[19] was used to find out the presence of psychiatric disorders in individuals. Score of more than 2 was taken as abnormal. Maslach burnout Inventory (MBI)[20] was used which is a valuable tool for assessing professional burnout. Burnout was assessed on following paradigms: depressive-anxiety syndrome, depersonalization, and reduction of person achievement. Scoring on each component yield mild, moderate, and high level of burnout. Residents suffering from any major psychiatric disorder or with past history of one were excluded from this study. The data was analyzed using appropriate statistical tests.
RESULTS
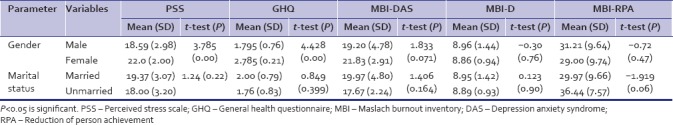
The subjects were postgraduate medical students pursuing their Masters in various specialties in a tertiary care hospital. There were total of 68 residents among which 16 residents were from final year, 25 from 2nd year and 27 from 1st year. Sociodemographic profile is as brought out in Table 1. Self-administered questionnaire of PSS, Maslach burnout inventory, Brief COPE inventory, and General Health Questionnaire-12 were given to the subjects in the middle of the academic year from November to December to avoid the examination-related academic pressures. Association of various psychological variables with sociodemographic profile is as brought out in Table 2. Females were found to have statistically significant high PSS scores and GHQ-12 scores compared to their male counterpart. There was no significant difference between married and unmarried residents. Mean and SDs of important psychological variables revealed that 55.9% of residents were above cutoff on scores of general psychopathology. On MBI-Depressive-Anxiety score, 30.9% of residents had low-level burnout, 64.7% had moderate level burnout, and others (4.4%) had high burnout. On MBI-Depersonalization component 1.5% of residents had mild level burnout, a significant portion 95.6% had moderate level burnout, and 2.9% had high-level burnout. On Reduction of personal achievement component, 50% had mild level burnout, and 20.6% had moderate level burnout whereas 29.4% students had high level of reduction of personal achievement.
Table 1.
Sociodemographic profile of the study population
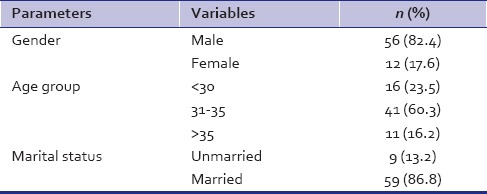
Table 2.
Association of various psychological variables with sociodemographic profile
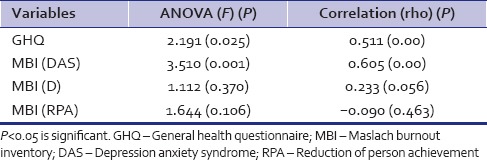
The mean of various components of coping and its correlation with perceived stress is as brought out in Table 3. Use of emotional response, use of instrumental support, religion, denial, self-blame, planning, and acceptance were found to be more commonly practiced coping. A significant correlation was found with coping skill like use of emotional response (positive), religion (positive), denial (negative), self-blame (negative), planning (positive), venting (negative), and disengagement (negative). The use of instrumental support (positive), acceptance (positive), positive reframing (positive), humor (positive), planning (positive), substance use (positive), and active coping (positive) did not correlate with scores on perceived stress. Analysis of association and correlation of various psychological variables with the PSS scores is shown in Table 4. Perceived stress had statistically significant association with general psychopathology and depressive-anxiety component of burnout. Perceived stress was found to have a significant positive correlation with general psychopathology and burnout depressive-anxiety syndrome.
Table 3.
Mean of various components of coping and its correlation with perceived stress
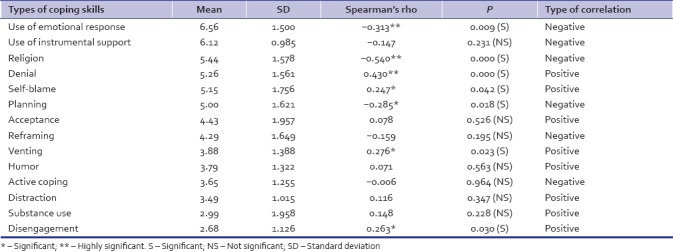
Table 4.
Association and correlation of various psychological variables with the perceived stress scale
DISCUSSION
Studies of medical students from various medical colleges in India and other countries worldwide identified a high frequency of stress.[2,21,22,23] The present study also showed a high-stress level in postgraduate medical students. More than 75% residents in our study were more than 30 yrs of age. However, there was no significant association of perceived stress with age. Earlier studies showed a higher stress level in younger age group compared to elder group, but the results were not statistically significant.[2,24] Stress levels were more in married residents than as compared to unmarried in a study by Gobblur et al.[21] However our study did not show any significant association between marital status and stress level. A study conducted by Das et al.[25] had concluded that gender as a factor does not influence the level of stress rather it influence the level of depression among male and female students. In an another study by Amr et al.,[23] male and female medical students were similar on level of perceived stress, number of stressors, clinical anxiety, physical well-being factors, and the extraversion scale. Our study observed that the difference between the mean scores of PSS for females and males was statistically highly significant akin to Gobblur et al.[21] and Abdulghani et al.[22] In addition, in our study, there was significant scores on GHQ-12 among females indicating high risk for general psychopathology. Nearly 55.9% of students were above cut-off on scores of general psychopathology. This score was higher than few researchers,[16,26,27,28] it was lesser than that of Inam et al.[29] who found it to the tune of 60% and above. High-level burnout was 4.4% on depressive-anxiety; 2.9% on depersonalization; and 29.4% on reduction of personal achievement. Dyrbye et al. found the burnout to be around 45% in their study.[14] Perceived stress had statistically significant association with general psychopathology and depressive-anxiety component of burnout akin to Singh et al.[30] It was also seen that higher the perceived stress, higher was the scores on burnout. Findings are akin to those of similar researches in the past.[11,31] There is no much research on postgraduate medical students existing in this direction. GHQ showed significant association and correlation with perceived stress akin to Singh et al.[30] Not much research exists in this direction.
In a study conducted on among 376 medical and medical sciences undergraduates,[28] it was found that subjects were using used positive coping strategies (active coping, religious coping, positive reframing, planning, and acceptance) more than avoidant strategies (denial, self-blame, and alcohol or substance use). Further, it also showed that perceived stress had statistically significant association with general psychopathology and depressive-anxiety component of burnout. In our study residents who had higher score on perceived stress were found to have statistically significant positive correlation with negative coping strategies like denial, self blame, venting and those with high score on positive coping skills like use of emotional support, religious practices, planning had negative correlation with perceived stress indicating developing positive coping skills would decrease the stress and hence general psychopathology. The scores of perceived stress had a significant association with score of general psychopathology and depressive anxiety component of burnout in our evaluation.
Our study has provided significant findings regarding correlation of Perceived stress with general health and burnout. The findings are further supported by earlier studies done both in Indian and foreign medical colleges as highlighted above. It provides a sound groundwork for planning interventions to reduce postgraduate medical student's mental morbidity and avoid burnout. The interventions so planned will help the postgraduate medical students in improving their quality of work output both in professional and personal front.
CONCLUSION
To conclude, higher scores on perceived stress were associated with higher scores on general psychopathology and burnout (Depression anxiety syndrome). Residents who displayed positive coping strategies such as use of emotional response, religion, and planning had lesser perceived stress. Residents who displayed negative coping strategies such as denial, self-blame, venting, and disengagement had increased perceived stress. Females had higher scores on perceived stress and GHQ-12 compared to males. Stress is one of the major growing mental problems among highly educated health professional and it should not be ignored as it can cause many other health issues. It should be evaluated and its remedy must be done to get better future health consultants.
Limitations of the study
The family history of psychiatric diagnosis was not given importance. The family construct was not given much importance which is one of the main factors influencing stress level. The study did not take into consideration of the individual departmental and personal activities during which questionnaire was given. The medical college in which the study was conducted consisted of residents belonging mostly to clinical subjects. Among the paraclinical and preclinical postgraduates, only pathology residents could participate as it is the only nonclinical postgraduation available in the college. Evaluation of pre- and para-clinical postgraduates would have added to our findings regarding stress level. Since the information was collected on a self-administered questionnaire because of respondent's interpretation of the questions or simply because of inaccuracies of responses or desire to report their emotions in a certain way, we cannot fully rule out information bias, even though we made adequate efforts at clarification, replication, and simplification. The cross-sectional design of our study is yet another limitation since associations presented lack of temporality. Prospective studies are necessary to study the associations between the occurrence of stressors and incidence of stress.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Morgan CT, King RA, Weisz JR, Schopler J. Introduction to Psychology. 7th ed. New Delhi: McGraw Hill Education(India) Private Limited; 1993. [Google Scholar]
- 2.Shete A, Garkal K. Study of stress, anxiety, and depression among postgraduate medical students. CHRISMED J Health Res. 2015;2:119–23. [Google Scholar]
- 3.Baldassin S, Alves TC, de Andrade AG, Nogueira Martins LA. The characteristics of depressive symptoms in medical students during medical education and training: A cross-sectional study. BMC Med Educ. 2008;8:60. doi: 10.1186/1472-6920-8-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Medical PG. Preparation: How to Deal with Inevitable Stress? – Gate To Medicine. [Last accessed on 2017 Oct 23]. Available from: http://www.gatetomedicine.com/blog/work-study-is-it-stressful/
- 5.Medical Students Want the Government to Increase PG seats India Medical Times. [Last accessed on 2017 Oct 23]. Available from: http://www.indiamedicaltimes.com/2017/01/11/medical-studentswant-the-government-to-increase-pg-seats/
- 6.Eze BI, Okoye OI, Maduka-Okafor FC, Aguwa EN. Factors influencing choice of medical specialty of preresidency medical graduates in Southeastern Nigeria. J Grad Med Educ. 2011;3:367–71. doi: 10.4300/JGME-D-10-00101.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daugherty SR, Baldwin DC, Jr, Rowley BD. Learning, satisfaction, and mistreatment during medical internship: A national survey of working conditions. JAMA. 1998;279:1194–9. doi: 10.1001/jama.279.15.1194. [DOI] [PubMed] [Google Scholar]
- 8.Stress: Effect on Employee Performance. [Last accessed on 2017 Oct 23]. Available from: https://www.ukessays.com/essays/management/factors-causing-stress-which-effect-employees-performanceptcl-management-essay.php .
- 9.Garg G. Postgraduate lifestyle: Stress and satisfaction. Indian J Pediatr. 2005;72:991. doi: 10.1007/BF02731679. [DOI] [PubMed] [Google Scholar]
- 10.Aktekin M, Karaman T, Senol YY, Erdem S, Erengin H, Akaydin M, et al. Anxiety, depression and stressful life events among medical students: A prospective study in Antalya, Turkey. Med Educ. 2001;35:12–7. doi: 10.1046/j.1365-2923.2001.00726.x. [DOI] [PubMed] [Google Scholar]
- 11.Guthrie E, Black D. Psychiatric disorder, stress and burnout. Adv Psychiatr Treat. 1997;3:275–81. [Google Scholar]
- 12.Wallin U, Runeson B. Attitudes towards suicide and suicidal patients among medical students. Eur Psychiatry. 2003;18:329–33. doi: 10.1016/j.eurpsy.2003.03.006. [DOI] [PubMed] [Google Scholar]
- 13.Shaufeli W, Enzmann D, Francis T. The Burnout Companion to Studyand Practice – A Critical Analysis. London: CRC Press; 1998. [Google Scholar]
- 14.Dyrbye LN, Thomas MR, Huntington JL, Lawson KL, Novotny PJ, Sloan JA, et al. Personal life events and medical student burnout: A multicenter study. Acad Med. 2006;81:374–84. doi: 10.1097/00001888-200604000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Muller L, Spitz E. Multidimensional assessment of coping: Validation of the brief COPE among french population. Encephale. 2003;29:507–18. [PubMed] [Google Scholar]
- 16.Sreeramareddy CT, Shankar PR, Binu VS, Mukhopadhyay C, Ray B, Menezes RG, et al. Psychological morbidity, sources of stress and coping strategies among undergraduate medical students of Nepal. BMC Med Educ. 2007;7:26. doi: 10.1186/1472-6920-7-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 18.Carver CS. You want to measure coping but your protocol's too long: Consider the Brief COPE. International J Behavioral Medicine. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 19.General Health Questionnaire (GHQ) [Last accessed on 2017 Sep 14]. Available from: https://www.gl-assessment.co.uk/products/general-health-questionnaire-ghq/
- 20.Maslach C, Jackson SE. The measurement of experienced burnout. J Occupational Behavior. 1981;2:99–113. [Google Scholar]
- 21.Gobbur SB, Nigudgi SR, Reddy S. Prevalence of stress among post graduate doctors at Mahadevappa Rampure Medical College Kalaburagi, Karnataka. Int J Community Med Public Health. 2016;3:576–80. [Google Scholar]
- 22.Abdulghani HM, AlKanhal AA, Mahmoud ES, Ponnamperuma GG, Alfaris EA. Stress and its effects on medical students: A cross-sectional study at a college of medicine in Saudi Arabia. J Health Popul Nutr. 2011;29:516–22. doi: 10.3329/jhpn.v29i5.8906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Amr M, Hady El Gilany A, El-Hawary A. Does gender predict medical students' stress in Mansoura, Egypt? Med Educ Online. 2008;13:12. doi: 10.3885/meo.2008.Res00273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johari AB, Hassim N. Stress and coping strategies among medical students in National University of Malaysia, Malaysia University of Sabah and Universiti Kuala Lumpur Royal College of Medicine Perak. J Kesihatan Masyarakat. 2009;15:106–15. [Google Scholar]
- 25.Das P, Sahoo R. Stress and depression among post graduate students. Int J Sci Res Public. 2012;2:1–5. [Google Scholar]
- 26.Guthrie E, Black D, Bagalkote H, Shaw C, Campbell M, Creed F. Psychological stress and burnout in medical students: A five-year prospective longitudinal study. J R Soc Med. 1998;91:237–43. doi: 10.1177/014107689809100502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Supe AN. A study of stress in medical students at seth G.S. Medical College. J Postgrad Med. 1998;44:1–6. [PubMed] [Google Scholar]
- 28.Al-Dubai SA, Al-Naggar RA, Alshagga MA, Rampal KG. Stress and coping strategies of students in a medical faculty in Malaysia. Malays J Med Sci. 2011;18:57–64. [PMC free article] [PubMed] [Google Scholar]
- 29.Inam SB. Anxiety and depression among students of a medical college in Saudi Arabia. Int J Health Sci (Qassim) 2007;1:295–300. [PMC free article] [PubMed] [Google Scholar]
- 30.Singh S, Prakash J, Das RC, Srivastava K. A cross-sectional assessment of stress, coping, and burnout in the final-year medical undergraduate students. Ind Psychiatry J. 2016;25:179–83. doi: 10.4103/ipj.ipj_68_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maslach C, Leiter MP. 1st ed. San Francisco: Jossey-Bass; 1997. The Truth About Burnout: How Organizations Cause Personal Stress and What to Do About it. [Google Scholar]


