This editorial refers to ‘Drebrin regulates angiotensin II-induced aortic remodeling’ by L. Zhang et al., pp. 1806–1815.
Despite major advances in hypertension therapy, even optimally treated hypertensive patients have high mortality compared with normotensive subjects. One manifestation of hypertension is aortic remodelling that predisposes to several cardiovascular diseases. There are still many unknowns on the mechanisms of the cellular and structural changes of hypertension-induced aortic remodelling. A publication by Zhang et al.1 reports effects of drebrin on angiotensin II (AngII)-induced aortic remodelling, which provides new insights into understanding mechanisms of vascular diseases.
Drebrin is an actin-binding protein that was identified originally in neuronal cells.2 It has two isoforms that are splice variants, with drebrin A being expressed in neural cells, and drebrin E is present in several other cell types, including vascular smooth muscle cells (SMCs).3 Stiber et al.3 found that drebrin was abundant in atherosclerotic lesion of humans and mice. They also demonstrated increased drebrin expression in SMCs following wire injury of the carotid artery in mice. This initial observation provided a rationale for Zhang et al.1 to develop and study mice with SMC-specific deletion of drebrin.
SMC-specific deletion of drebrin was achieved by breeding drebrin-floxed mice with mice expressing Cre under the control of the endogenous SM22 promoter. The authors confirmed that there was profound reduction of drebrin in SMCs. Consistent with previous reports, the SM22 promoter also led to deletion of drebrin in non SMCs including fibroblasts.4 Deletion of drebrin in SMCs had no effect on AngII-induced increases in systolic and diastolic blood pressures, as measured by both a tail-cuff based technique and radiotelemetry. Drebrin deficiency in SMCs also had no effects on AngII-induced ex vivo aortic contractility, which occurs only in the infrarenal region of the aorta.5 Despite the lack of effect of drebrin deficiency on physiological parameters, there were profound effects on aortic pathology. This included increased AngII-induced aortic wall thickness, lumen area, and elastin breaks of the excised ascending aorta, and increased diameter of the aortic sinus in vivo (Figure 1). These changes did not occur in saline-infused mice. This augmentation of AngII-induced aortic pathology was only observed in the ascending aorta, not the descending aorta or bronchial arteries. Previous studies have demonstrated AngII-induced aortic thickening is due to hyperplasia in the ascending aorta, and hypertrophy in the rest of the aorta.6,7 Therefore, the response in SMC-specific drebrin deleted mice is consistent with a region-specific effect on hyperplasia.
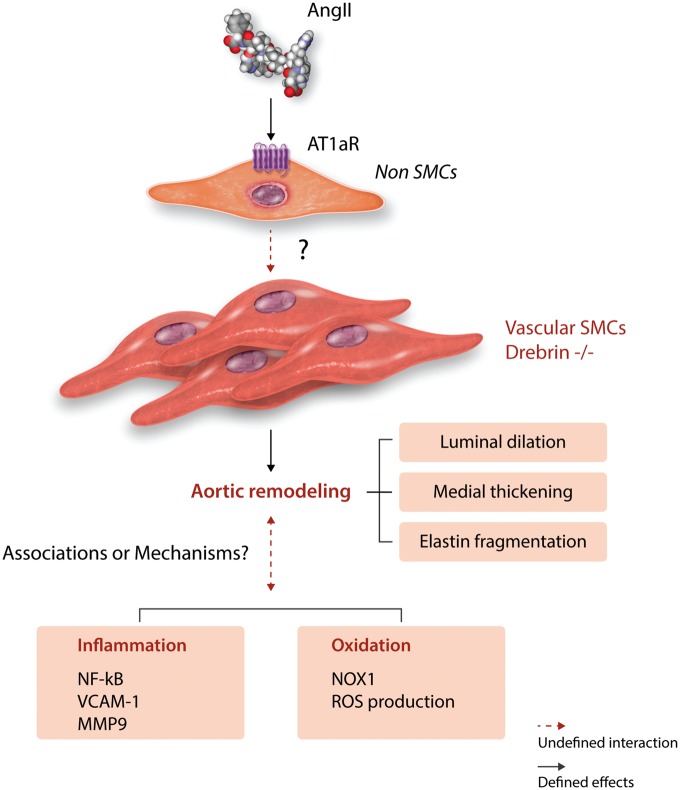
Figure 1.
Schematic summary of the findings reported by Zhang et al.1 and discussions in this Editorial. AngII and its receptor (AT1aR) interact in non SMCs, which lead to aortic remodelling. Depletion of drebrin in SMCs augments this AngII-mediated effect through undefined mechanisms.
Having demonstrated the compelling phenotype of drebrin deficiency, subsequent studies delved into defining mechanisms of this effect. This included measurements of SMC proliferation, increased collagen I mRNA abundance, phosphorylation of ERK1/2, enhanced NFκB signalling, increased VCAM-1 expression, increased MMP-9 abundance and enzymatic activity, increased adventitial macrophage accumulation, increased superoxide, and increased Nox1 mRNA and protein (Figure 1). All these measurements were performed on tissues extracted from mice infused with AngII for 28 days. At this interval, there is profound pathology in the ascending aorta. This leads to a ‘chicken and egg’ situation in terms of mechanistic interpretation: Did the measured changes promote the pathology? Or were they a consequence of the pathology? Indeed at this interval of AngII infusion, in addition to processes promoting pathology, they may be reparative responses in an attempt to ‘heal’ the aorta. There is no clear mode to resolve this conundrum. One potential approach is to acquire tissues at selected intervals during the disease evolution to determine whether changes can be observed prior to the appearance of overt pathology. While this potentially enables greater mechanistic insight, it also greatly ratchets up the difficulty of performing the studies.
One mechanism explored for promoting pathology was the potential for AngII responsiveness to be enhanced in the affected region. This was examined through measurement of mRNA abundance of AngII type 1a (AT1a) receptors, which was not measurably increased by drebrin deletion. Although there has been a pervasive assumption that AngII-induced aortic pathology is due to direct stimulation of SMCs, this has not been sustained by experimental approaches. Indeed, several groups have deleted AT1a receptor from SMCs but failed to detect effects on AngII-induced aortic pathologies.5,8,9 Consistent with AngII-induced aortic pathology not being attributed to direct stimulation of AT1a receptor on SMCs, the authors failed to co-precipitate drebrin and AT1a receptors in HEK-293 cells. These findings implicate that effects of SMC-specific drebrin on preventing aortic remodelling are not through direct interaction with AngII activation of AT1a receptors (Figure 1).
This study also begs the question of why drebrin deficiency only influenced AngII-induced pathology in the ascending aorta. One potential explanation is the difference of embryonic origins of SMCs in the ascending and descending aortic regions. The aortic sinus and ascending aorta are populated with SMCs derived from second heart field and cardiac neural crest, whereas the descending aorta is populated with SMCs derived from somites.10–14 Although it is a spatial concordance of these different embryonic origins with the effect of drebrin deletion on AngII-induced aortic remodelling, there has no direct evidence that SMCs from these different locations display functional differences.
Defining sex differences is important, since this has a major effect on many cardiovascular responses.15 In this study, both male and female mice were studied. Given the recent clinical data illustrating sex differences in thoracic aortic aneurysm phenotype in male and female patients, it would be interesting to explore whether drebrin deletion in aortic remodelling is afforded similarly to male and female mice. Representing the data in a sex-specific manner may provide further insight into understanding mechanisms of the regional specific pathology.
In conclusion, drebrin deficiency in SMCs leads to region-specific aortic remodelling in AngII-infused mice. We look forward to future studies to provide further mechanistic insight into AngII-induced aortic pathology.
Conflict of interest: none declared.
Funding
The authors’ research work was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under award numbers R01HL133723 and R01HL139748 and the American Heart Association SFRN in Vascular Disease (18SFRN33960001). H.S. is supported by an AHA postdoctoral fellowship (18POST33990468). The content in this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
The opinions expressed in this article are not necessarily those of the Editors of Cardiovascular Research or of the European Society of Cardiology.
References
- 1. Zhang L, Wu JH, Huang TQ, Nepliouev I, Brian L, Zhang Z, Wertman V, Rudemiller NP, McMahon TJ, Shenoy SK, Miller FJ, Crowley SD, Freedman NJ, Stiber JA.. Drebrin regulates angiotensin II-induced aortic remodeling. Cardiovasc Res 2018;114:1806–1815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shirao T. The roles of microfilament-associated proteins, drebrins, in brain morphogenesis: a review. J Biochem 1995;117:231–236. [DOI] [PubMed] [Google Scholar]
- 3. Stiber JA, Wu JH, Zhang L, Nepliouev I, Zhang ZS, Bryson VG, Brian L, Bentley RC, Gordon-Weeks PR, Rosenberg PB, Freedman NJ.. The actin-binding protein drebrin inhibits neointimal hyperplasia. Arterioscler Thromb Vasc Biol 2016;36:984–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zhang JC, Kim S, Helmke BP, Yu WW, Du KL, Lu MM, Strobeck M, Yu Q, Parmacek MS.. Analysis of SM22alpha-deficient mice reveals unanticipated insights into smooth muscle cell differentiation and function. Mol Cell Biol 2001;21:1336–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rateri DL, Moorleghen JJ, Balakrishnan A, Owens AP 3rd, Howatt DA, Subramanian V, Poduri A, Charnigo R, Cassis LA, Daugherty A.. Endothelial cell-specific deficiency of Ang II type 1a receptors attenuates Ang II-induced ascending aortic aneurysms in LDL receptor−/− mice. Circ Res 2011;108:574–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Owens AP 3rd, Subramanian V, Moorleghen JJ, Guo Z, McNamara CA, Cassis LA, Daugherty A.. Angiotensin II induces a region-specific hyperplasia of the ascending aorta through regulation of inhibitor of differentiation 3. Circ Res 2010;106:611–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Poduri A, Rateri DL, Howatt DA, Balakrishnan A, Moorleghen JJ, Cassis LA, Daugherty A.. Fibroblast angiotensin II type 1a receptors contribute to angiotensin II-induced medial hyperplasia in the ascending aorta. Arterioscler Thromb Vasc Biol 2015;35:1995–2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sparks MA, Parsons KK, Stegbauer J, Gurley SB, Vivekanandan-Giri A, Fortner CN, Snouwaert J, Raasch EW, Griffiths RC, Haystead TA, Le TH, Pennathur S, Koller B, Coffman TM.. Angiotensin II type 1A receptors in vascular smooth muscle cells do not influence aortic remodeling in hypertension. Hypertension 2011;57:577–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Galatioto J, Caescu CI, Hansen J, Cook JR, Miramontes I, Iyengar R, Ramirez F.. Cell type-specific contributions of the angiotensin II type 1a receptor to aorta homeostasis and aneurysmal disease—Brief Report. Arterioscler Thromb Vasc Biol 2018;38:588–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Majesky MW. Developmental basis of vascular smooth muscle diversity. Arterioscler Thromb Vasc Biol 2007;27:1248–1258. [DOI] [PubMed] [Google Scholar]
- 11. Sawada H, Rateri DL, Moorleghen JJ, Majesky MW, Daugherty A.. Smooth muscle cells derived from second heart field and cardiac neural crest reside in spatially distinct domains in the media of the ascending aorta—Brief Report. Arterioscler Thromb Vasc Biol 2017;37:1722–1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jiang X, Rowitch DH, Soriano P, McMahon AP, Sucov HM.. Fate of the mammalian cardiac neural crest. Development 2000;127:1607–1616. [DOI] [PubMed] [Google Scholar]
- 13. Wasteson P, Johansson BR, Jukkola T, Breuer S, Akyurek LM, Partanen J, Lindahl P.. Developmental origin of smooth muscle cells in the descending aorta in mice. Development 2008;135:1823–1832. [DOI] [PubMed] [Google Scholar]
- 14. Leroux-Berger M, Queguiner I, Maciel TT, Ho A, Relaix F, Kempf H.. Pathologic calcification of adult vascular smooth muscle cells differs on their crest or mesodermal embryonic origin. J Bone Miner Res 2011;26:1543–1553. [DOI] [PubMed] [Google Scholar]
- 15. Arnold AP, Cassis LA, Eghbali M, Reue K, Sandberg K.. Sex hormones and sex chromosomes cause sex differences in the development of cardiovascular diseases. Arterioscler Thromb Vasc Biol 2017;37:746–756. [DOI] [PMC free article] [PubMed] [Google Scholar]