Abstract
HIV-related symptoms have a deleterious effect on quality of life. One determinant of HIV symptom burden among individuals of color may be discrimination. The aim of this study was to explore whether multiple lifetime discrimination events are associated with a greater number of HIV-related symptoms among heterosexual HIV-positive men of color and to examine the influence of anxiety and social support on this relationship. Data for this study were drawn from a cross-sectional survey of 307 heterosexual HIV-positive men recruited from health and social service agencies in New York City (NYC). This study indicated that the number of discrimination events experienced in one’s lifetime was positively associated with the number of HIV-related symptoms experienced in the past month. Moreover, the direct effect of discrimination on HIV symptoms remained significant after anxiety was included as a mediator in the model, and there was a significant indirect effect of discrimination on HIV symptoms through anxiety. Evidence supported a potential moderated mediation effect involving social support: As social support increased, the indirect effect of discrimination on HIV symptoms through anxiety decreased. The results of this study suggest an association between discrimination and HIV-related symptom burden. Furthermore, the relationship between number of major discrimination experiences and HIV symptom burden was partially mediated by anxiety. Future research should consider how lifetime discrimination might be associated with negative health outcomes among HIV-positive individuals of color.
Keywords: HIV/AIDS, physiological and endocrine disorders, social determinants of health, psychosocial and cultural issues, social support, psychosocial and cultural issues, mental health, men of color, special populations
With the advent of highly active antiretroviral therapy (HAART), HIV transformed from a progressive fatal illness to a manageable chronic condition (Deeks, Lewin, & Havlir, 2013). Life expectancy among treated HIV-positive individuals has increased during this time and is approaching that of HIV-negative individuals (Antiretroviral Therapy Cohort Collaboration, 2008; Samji et al., 2013). HIV symptoms, however, which may be physical (e.g., pain, diarrhea), psychological (e.g., depression, anxiety), and cognitive (e.g., memory loss) continue to be a major concern (Portillo, Holzemer, & Chou, 2007). These symptoms may result from the disease process itself as well as secondary complications (e.g., medication side effects, common comorbidities). Such symptoms, which may occur regardless of CD4+ count (Lee et al., 2009; Willard et al., 2009), may affect quality of life (Ellis et al., 2010; Lorenz, Cunningham, Spritzer, & Hays, 2006; Vyavaharkar, Moneyham, Murdaugh, & Tavakoli, 2012) as well as ART adherence (Gay et al., 2011; Harding et al., 2010).
Men of color continue to be disproportionately represented among HIV-positive heterosexual men living in the United States (Centers for Disease Control and Prevention, 2017). Almost no studies have examined the determinants of HIV symptom burden among heterosexual men of color; however, the socioecological model suggests that HIV outcomes must be understood in the context of social and structural factors (Baral, Logie, Grosso, Wirtz, & Beyrer, 2013). One such factor that may influence HIV symptom burden is discrimination. For example, in a study of men who have sex with men, Bogart and colleagues (2013) reported that a combination of discrimination types (racial, homophobic, and serostatus related) predicted the number of HIV symptoms (e.g., fever, diarrhea) among both Blacks and Latinos (Bogart, Landrine, Galvan, Wagner, & Klein, 2013).
Mediators and moderators of the relationship between discrimination and negative physical health outcomes among HIV-positive individuals of color are also unknown. Scholars have suggested that associations between perceived discrimination and self-reported physical health, as well as a number of chronic health conditions (e.g., diabetes), may be at least partially mediated by poor mental health (Brondolo et al., 2011; Carter, Walker, Cutrona, Simons, & Beach, 2016; Earnshaw et al., 2012; Molina, Alegría, & Mahalingam, 2013). Anxiety, in particular, may mediate the relationship between discrimination and HIV symptom burden through its effects on stress. Social support may act as a moderator of the relationship between discrimination and physical health as well as of the mediating role of anxiety. Studies have demonstrated mixed evidence regarding the buffering effects of social support on the relationship between discrimination and mental (e.g., depression, anxiety) and physical health (e.g., self-rated health, cardiovascular reactivity to stress) among men and women of color (Ajrouch, Reisine, Lim, Sohn, & Ismail, 2010; Brondolo, Ver Halen, Pencille, Beatty, & Contrada, 2009; Gerrard, Gibbons, Fleischli, Cutrona, & Stock, 2018; McNeil, Fincham, & Beach, 2014; Nadimpalli, James, Yu, Cothran, & Barnes, 2015); however, no studies have explored these associations in regard to HIV symptom burden.
The aim of this study was to explore whether experiences of multiple lifetime discrimination events affect HIV somatic symptom burden (i.e., the number of HIV symptoms experienced) among heterosexual HIV-positive Black and Latino men. This study also explored the degree to which anxiety explained the relationship between discrimination and HIV symptom burden and assessed whether social support modified the relationship between discrimination and anxiety. Study hypotheses were as follows: (a) discrimination will be positively associated with HIV somatic symptom burden; (b) anxiety will partially mediate the relationship between self-reported discrimination and HIV-related somatic symptom burden; and (c) this mediation relationship will be stronger among those who reported low social support.
Methods
Sample and Procedures
Data for this study were drawn from the “Men’s Talk on HIV Risk” (MENTOR) Project, a cross-sectional survey of heterosexual HIV-positive primarily Black and Latino men. Participants (N = 317) were recruited from health and social service agencies located in the South Bronx and Harlem, New York, in 2011 and 2012. Participants had to fulfill the following eligibility criteria: (a) male; (b) HIV-positive; (c) 18–60 years old; (d) English or Spanish fluency; (e) heterosexually identified; and (f) had vaginal or anal sex with a woman in the past 3 months. Prior to completing the survey, participants signed a consent form detailing study procedures. Surveys were administered in English or in Spanish by interviewers using Computer-Assisted Personal Interview (CAPI) software (QDS version 6.2.1, Nova Research). Participants were compensated $50 for their time. The Institutional Review Board of the University of Rochester approved all study procedures.
Measures
HIV-related symptoms were assessed using 15 items pertaining to somatic HIV symptoms drawn from an HIV symptom index developed by Justice and colleagues (2001), which asked about symptoms men experienced during the past month. Dichotomous response affirmative answers were summed to obtain a total symptom score.
Six items reflecting lifetime experience of major discrimination events were drawn from the Major Experiences of Discrimination scale (Williams, Yan, Jackson, & Anderson, 1997). Men were asked if they were ever unfairly fired from a job; had not been hired for a job for unfair reasons; were unfairly stopped, searched, questioned, physically threatened, or abused by the police; were unfairly discouraged by a teacher or advisor from continuing education; were unfairly prevented from moving into a neighborhood because the landlord or a realtor refused to sell or rent a house or apartment; or had moved into a neighborhood where neighbors made life difficult for the participant or his family. Dichotomous response affirmative answers were summed to obtain a total discrimination score.
Anxiety was assessed using seven items from the Client Diagnostic Questionnaire (Aidala et al., 2004). Men were asked if they had experienced any of the following symptoms over the past 4 weeks: feeling nervous, anxious, on edge, or worrying a lot about different things; feeling restless so that it is hard to sit still; getting tired very easily; muscle tension, aches, or soreness; trouble falling or staying asleep; trouble concentrating on things; and becoming easily annoyed or irritable. Participants responded to these items on a 4-point Likert scale, where 1 = not at all and 4 = nearly every day. Response scores were then averaged to create a total anxiety score.
Social support was assessed using 12 items taken from the Lubben Social Network Scale—Revised (Lubben, Gironda, & Lee, 2002). Participants were asked about the number of friends/relatives seen during the past month; how often they saw the friend/relative that they had the most contact with; how many friends/relatives they felt comfortable talking about personal matters with; how many friends/relatives that they felt they could call on for help; how often a friend/relative would reach out to the participant when he had an important decision to make; and how often at least one of their friends/relatives was available to talk when the participant had an important decision to make. Questions regarding number of supportive others were answered on a 6-point Likert scale, with anchors of 0 = none and 5 = 9 or more. Questions regarding frequency of contact were answered on a 6-point Likert scale, with 0 = less than monthly and 5 = daily. Finally, questions regarding communication with supportive others were answered on a 6-point Likert scale, ranging from 0 = never to 5 = always. Items were averaged to create a total social support score.
Sociodemographic variables were included in the models as covariates due to their hypothesized association with health. These variables included self-reported race/ethnicity (Black vs. Latino vs. Other), age, monthly household income, and education (completed high school or obtained general equivalency diploma [GED] vs. not). CD4+ count and diagnosis of AIDS were also included in the model.
Analysis
Standard data cleaning methods were conducted; outliers were Winsorized by setting all outlying values to the value of the highest or lowest non-outlying value. Descriptive analyses (central tendency, dispersion) were performed to characterize the sample. A correlation matrix was generated to examine the correlational structure of the data. Path analysis (moderated mediation) was performed to test the hypothesis that anxiety mediates the relationship between perceived discrimination and HIV-related symptom burden and that this mediation effect will tend to be weaker among those who reported greater social support. The direct and indirect effects (via anxiety) of discrimination on HIV symptom burden were calculated, and an interaction term was included to test the moderating effects of social support on the relationship between discrimination and anxiety. The effects of selected covariates on HIV-related symptoms were adjusted for in the model. Analyses were performed using PROCESS macro (Model 7) for SPSS (v. 2.16; Hayes, 2013). Individuals with missing data (n = 10) were removed from the dataset via list-wise deletion, resulting in a final sample size of 307.
Results
Table 1 presents descriptive data for the sample of 307 HIV-positive self-identified heterosexual men. On average, men reported experiencing about two lifetime discrimination events (mode = 1), and nearly four HIV symptoms in the past month. Discrimination was positively associated with anxiety (r = .204; p ⩽ .001) and number of HIV symptoms (r = .279; p ⩽ .001). Social support was negatively associated with anxiety (r = −.129; p = .022) and HIV symptoms (r = −.168; p = .003).
Table 1.
Participant Characteristics (n = 307).
| Total (n = 307) |
Black (n = 199) |
Latino (n = 92) |
Othera (n = 16) | |||||
|---|---|---|---|---|---|---|---|---|
| Variable | Frequency | % | Frequency | % | Frequency | % | Frequency | % |
| Age | ||||||||
| Mean (±SD) | 47.9 (5.9) | – | 48.51 (5.95) | – | 46.53 (5.75) | – | 47.69 (6.24) | – |
| Range | 33–59 | – | 33–59 | – | 33–56 | – | 33–57 | – |
| High school diploma/GED | 177 | 57.7 | 116 | 58.29 | 52 | 56.52 | 9 | 56.25 |
| Monthly income | ||||||||
| Mean (±SD) $ | 815.13 (399.82) | – | 828.26 (401.66) | – | 775.64 (376.0) | – | 878.81 (508.46) | – |
| Range | 0–1,670 | – | 0–1,670 | – | 100–1,670 | – | 0–1,670 | – |
| Number of lifetime discrimination events | ||||||||
| 0 | 42 | 13.7 | 26 | 13.07 | 15 | 16.3 | 1 | 6.25 |
| 1 | 111 | 36.2 | 70 | 35.18 | 33 | 35.87 | 8 | 50 |
| 2 | 63 | 20.5 | 42 | 21.11 | 18 | 19.57 | 3 | 18.75 |
| 3+ | 91 | 29.6 | 59 | 29.65 | 24 | 26.09 | 4 | 25 |
| Number of HIV symptoms in past month | ||||||||
| Mean (±SD) | 3.83 (2.68) | – | 3.72 (2.73) | – | 3.95 (2.63) | – | 4.5 (2.34) | |
| Range | 0–11 | – | 0–11 | – | 0–11 | – | 0–9 | |
| Social support score (scored 1–5) | ||||||||
| Mean (±SD) | 2.58 (0.85) | – | 2.59 (0.81) | – | 2.52 (0.91) | – | 2.79 (1.01) | |
| Range | 0.5–4.75 | – | 0.5–4.75 | – | 0.64–4.58 | – | 0.58–4.42 | |
| Anxiety score (scored 1–4) | ||||||||
| Mean (±SD) | 1.95 (0.67) | – | 1.9 (0.65) | – | 2.07 (0.67) | – | 1.89 (0.63) | |
| Range | 1.0–3.5 | – | 1.0–3.5 | – | 1.0–3.5 | – | 1.14–3.43 | |
| CD4+ | ||||||||
| Mean (±SD) | 446.77 (259.0) | – | 454.4 (262.3) | – | 437.02 (256.12) | – | 407.94 (242.6) | |
| Range | 4–995 | – | 4–995 | – | 20–995 | – | 50–792 | |
| Ever diagnosed with AIDS | 162 | 52.8 | 102 | 51.26 | 50 | 54.35 | 10 | 62.5 |
Note. a “Other” racial/ethnic category consisted of nine self-identified mixed racial/ethnic participants (all included Black/African American or Latino); one Native American; and six Caucasian participants. GED = general equivalency diploma.
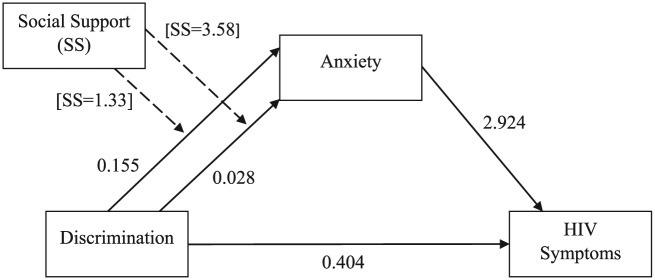
The path model (Figure 1; Table 2) identified that after adjusting for anxiety and other covariates, the number of discrimination events experienced in one’s lifetime was positively associated with the number of HIV-related somatic symptoms experienced in the past month (B = 0.404, 95% CI [0.190, 0.619]). Results further indicate that anxiety partially mediated the relationship between discrimination and HIV somatic symptoms and that the strength of this indirect effect is conditional on the level of social support. As social support increased, the magnitude of the mediation effect of discrimination on HIV symptoms via anxiety decreased. For every one-unit increase in social support, the effect of discrimination on HIV somatic symptoms through anxiety decreased by 0.164 (95% CI [–.0351, –0.012]). The model R2 was .41, indicating that the model explained a substantial portion of the variance in number of HIV-related somatic symptoms.
Figure 1.
Path diagram showing model unstandardized coefficients. Effects of discrimination on anxiety are conditional on level of social support (shown as 10th and 90th percentile in square brackets).
Table 2.
Path Analysis Results Showing Unstandardized Coefficients (95% CI) and p Values for Moderated Mediation of Discrimination on HIV Symptoms Through Anxiety, Moderated by Social Supporta.
| Predictor variable | Anxiety (mediator) | HIV symptoms (outcome variable) | |
|---|---|---|---|
| Direct effect | Total effect | ||
| Discrimination | 0.230 [0.082, 0.377] .002 | 0.404 [0.190, 0.619] <.001 | 0.664 [0.409, 0.919] <.001 |
| Social Support (SS) | 0.018 [−0.119, 0.154] .801 | – | – |
| Discrimination × SS | −0.056 [−0.112, 0.00] .049 | – | – |
| Anxiety | – | 2.924 [2.462, 3.386] <.001 | 3.119 [2.668, 3.570] <.001 |
| Conditional indirect effects of discrimination on HIV symptoms through anxiety | |||
| Level of social support (moderator)b | Indirect effect | ||
| 1.333 | 0.452 [0.239, 0.706] | ||
| 2.000 | 0.342 [0.201, 0.514] | ||
| 2.583 | 0.246 [0.113, 0.393] | ||
| 3.167 | 0.150 [−0.044, 0.335] | ||
| 3.583 | 0.082 [−0.176, 0.313] | ||
Note. aModel adjusted for age, race/ethnicity, education, income, CD4 count, and AIDS diagnosis.
Values for moderator are 10th, 25th, 50th, 75th, and 90th percentiles.
Discussion
Consistent with study hypotheses, the results of this study suggest a positive association between number of lifetime discrimination events and HIV symptom burden among HIV-positive heterosexual Black and Hispanic men. Furthermore, the relationship between number of discrimination events and HIV symptom burden was partially mediated by anxiety. Although not measured in this study, one hypothesis to explain these results involves the effects of discrimination on anxiety-induced stress. Although the minority stress theory has been most often applied to sexual minority populations, it may be a useful tool to understand the effects of discrimination on heterosexual, HIV-positive men of color. Meyer (2003) defines minority stress as “excess stress to which individuals from stigmatized social categories are exposed as a result of their social, often a minority, position” and suggests that expectations of future discriminatory events, as well as the internalization of society’s negative valuations, play a role in the development of such stress (Meyer, 2003). Studies have indicated that exposure to discrimination is associated with higher allostatic load (i.e., adverse physiological effects incurred by chronic stress; Brody et al., 2014). Furthermore, research indicates that anxiety mediates the relationship between discrimination and markers of physiological stress (e.g., cortisol; Lee et al., 2018). Anticipating discrimination due to past experiences may lead to heightened vigilance against future discrimination, which in turn leads to increased anxiety and threat-related cognitions, as well as a heightened physiological stress response (Sawyer, Major, Casad, Townsend, & Mendes, 2012).
Results also provide evidence consistent with the study hypothesis that social support may moderate the relationship between lifetime discrimination and anxiety, such that the effect of discrimination on anxiety decreases at higher levels of social support, indicating that social support may help to buffer the adverse effects of discrimination on anxiety and, by extension, HIV symptoms. Studies have suggested that social support is associated with increased viral load suppression (Friedman et al., 2017) and ART adherence (Power et al., 2003; Simoni, Frick, & Huang, 2006), suggesting one pathway by which social support may affect HIV symptom burden. Additionally, Thoits (2011) suggests several plausible mechanisms by which social support may influence health outcomes, including (a) the provision of advice or assistance in implementing emotion-focused or problem-solving coping strategies; and (b) the demonstration of caring, acceptance, and (particularly among those with similar experiences) understanding, which can lead to a sense of belonging and increased self-worth (Thoits, 2011). In addition, social support has been linked to the development of in-group identity (Shehadeh, Rubens, Attonito, & Jennings, 2018), which in turn has been linked to increased physical and mental health (Matheson, McQuaid, & Anisman, 2016). Physiologically, social support has been linked to the release of oxytocin, which in turn has been associated with lower anxiety and decreased stress markers (Heinrichs, Baumgartner, Kirschbaum, & Ehlert, 2003). In addition, social support has been associated with better immune functioning and immune-mediated inflammatory processes (Uchino, 2006). Interventions to reduce HIV symptom burden, therefore, might focus on anxiety reduction by building support networks and encouraging active communication within such networks.
Structural interventions focusing on the reduction of mutually reinforcing forms of institutional and social discrimination are also necessary to reduce not only HIV somatic symptom burden but a wide array of negative physical and mental health outcomes affecting individuals of color. For example, policies that eliminate racial profiling, disproportionate arrests and incarceration of Black and Latino men, and violence experienced at the hands of the police may greatly reduce anxiety and thus contribute to better health among individuals of color. Similarly, enforcement of fair housing laws and social initiatives aimed at reducing “white flight” may reduce residential segregation, which has also been tied to adverse health outcomes among Blacks and Latinos. Enforcement of fair labor laws and programs to improve job opportunities may help to reduce economic disparities among Whites and individuals of color, making such individuals less anxious and better able to address HIV somatic symptoms as they arise. Finally, intervening in all of these areas may ultimately reduce chronic stress and maladaptive coping above and beyond the protection offered by social support. Without intervening on the structural level, efforts to address discrimination through individual-level interventions may only be a superficial and ultimately unsustainable solution to health problems experienced by HIV-positive men of color.
In interpreting these results, it is important to distinguish between major discrimination events (as explored in this study) and day-to-day discrimination, as everyday unfair treatment and microaggressions (i.e., subtle or casual degradation or dismissal of marginalized individuals; Wong, Derthick, David, Saw, & Okazaki, 2014) may also play a role in increasing HIV-related symptoms among HIV-positive Black and Latino men. For example, Ong and colleagues (2017) have reported that chronic exposure to day-to-day racial mistreatment is associated with increased allostatic load (Ong, Williams, Nwizu, & Gruenewald, 2017). Studies have indicated that everyday discrimination is associated with poor self-rated health (Earnshaw et al., 2016; Mouzon, Taylor, Woodward, & Chatters, 2017), chronic illness (Earnshaw et al., 2016; Mouzon et al., 2017), pain (Sue et al., 2007), and the degree to which chronic illnesses interfere with daily life (Mouzon et al., 2017) or create role limitations (Sue et al., 2007). Given that higher allostatic load has been associated with exposure to repeated or chronic stressors, the experience of day-to-day discrimination may in fact play a greater role in perpetuating negative health outcomes than major discrimination events (Colen, Ramey, Cooksey, & Williams, 2008).
Future research should examine whether associations between discrimination and HIV symptomology hold for other groups, such as women of color. Intersectionality theory suggests that social identities are multiple and interdependent and that these intersections of identity are mirrored by interlocking systems of oppression and privilege on the macro level (Bowleg, 2012). Although men are privileged due to their gender, this privilege increases and decreases in accordance with membership in other social groups (e.g., racial/ethnic minorities, those with low socioeconomic status; those who are HIV positive; men who have sex with men; Bogart et al., 2013). Grollman (2014) has demonstrated that members of multiple stigmatized groups had poorer health outcomes than singly disadvantaged or privileged individuals and that this relationship was partially mediated by multiple forms of discrimination (Grollman, 2014). The findings of Lewis and colleagues (2017), for example, suggest that gendered racial microaggressions are associated with negative mental and physical health outcomes among Black women (Lewis, Williams, Peppers, & Gadson, 2017). Thus, women might face additional or different types of discrimination that play a unique role in perpetuating health disparities in this group.
Finally, following the work of Bogart and colleagues (2013), future research should further examine associations between discrimination and objective measures of health among HIV-positive Black and Latino men (e.g., CD4+, viral load; Bogart et al., 2013) as well as explore mediators and moderators of these relationships. Other potential mediators of the relationship between discrimination and physical health might include anger (Brondolo et al., 2011; Gerrard et al., 2018; Gibbons et al., 2014), depression (Gerrard et al., 2018; Gibbons et al., 2014), or negative health behaviors (e.g., substance use)/failure to engage in healthy behaviors (Terra & Jules, 2002). Alternative moderators of this relationship might include other coping mechanisms than seeking social support (e.g., spirituality; Gerrard et al., 2018; Pascoe & Smart-Richman, 2009; Terra & Jules, 2002).
This study has several limitations. The cross-sectional design of the study precludes making causal inferences, and these results should be viewed as hypothesis generating rather than hypothesis testing. The measure of discrimination used assessed the number of different types of discrimination events experienced, not the frequency of each type of discrimination event or the context of discrimination experienced (e.g., due to race or HIV status); thus, it was not possible to determine if one source of discrimination might have had greater consequences than another. Mouzon and colleagues (2017) have reported that both racial discrimination and non-attributed discrimination predicted poorer health outcomes among Blacks, while nonracial discrimination demonstrated no effect (Mouzon et al., 2017). Thus, future research should compare the specific effects of racial discrimination on HIV-related symptoms with other forms of discrimination, as Bogart and colleagues did when exploring the effects of discrimination on health outcomes among men who have sex with men (Bogart et al., 2013). Furthermore, items relating to symptom severity were not included; thus, it was not possible to determine the degree to which symptoms interfered with individuals’ quality of life or which symptoms were most problematic to participants. Finally, this study did not succeed in recruiting younger men (i.e., those below age 33 years). Given high rates of HIV infection among men aged 18–24 years—particularly young men of color (Centers for Disease Control and Prevention, 2018)—future research should focus on how discrimination affects HIV somatic symptom burden among young adults.
Conclusion
HIV-positive heterosexual men of color are vulnerable to the effects of discrimination on physical health outcomes. Self-reported lifetime discrimination is positively associated with HIV symptomology, both directly and indirectly via increased anxiety. Social support, however, may have a buffering effect on this relationship. Future research should explore how discrimination produces negative health outcomes among individuals of color and how social support and other forms of coping can mitigate adverse effects.
Appendix. List of HIV-Related Somatic Symptoms (Justice et al., 2001)
Muscle aches or joint pain
Fevers, chills, or sweats
Feeling dizzy or lightheaded
Pain, numbness or tingling in the hands or feet
Problems with sex
Nausea or vomiting
Diarrhea
Skin problems, such as rash, dryness or itching
Cough or trouble catching breath
Problems with weight loss or wasting
Headache
Hair loss or changes in the way hair look
Fatigue
Difficulty sleeping
Loss of appetite
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institutes of Health, National Institute of Child Health and Human Development [grant number R01HD057793] and by the University of Rochester Center for AIDS Research [grant number NIH P30AI078498].
ORCID iD: Amy Braksmajer  https://orcid.org/0000-0002-4307-3141
https://orcid.org/0000-0002-4307-3141
References
- Aidala A., Havens J., Mellins C. A., Dodds S., Whetten K., Martin D., … Ko P. (2004). Development and validation of the Client Diagnostic Questionnaire (CDQ): A mental health screening tool for use in HIV/AIDS service settings. Psychology of Health and Medicine, 9(3), 362–380. [Google Scholar]
- Ajrouch K. J., Reisine S., Lim S., Sohn W., Ismail A. (2010). Perceived everyday discrimination and psychological distress: Does social support matter? Ethnicity and Health, 15(4), 417–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antiretroviral Therapy Cohort Collaboration. (2008). Life expectancy of individuals on combination antiretroviral therapy in high-income countries: A collaborative analysis of 14 cohort studies. The Lancet, 372(9635), 293–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baral S., Logie C. H., Grosso A., Wirtz A. L., Beyrer C. (2013). Modified social ecological model: A tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health, 13(1), 482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogart L. M., Landrine H., Galvan F. H., Wagner G. J., Klein D. J. (2013). Perceived discrimination and physical health among HIV-positive Black and Latino men who have sex with men. AIDS and Behavior, 17(4), 1431–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L. (2012). The problem with the phrase women and minorities: Intersectionality—an important theoretical framework for public health. American Journal of Public Health, 102(7), 1267–1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody G. H., Lei M. K., Chae D. H., Yu T., Kogan S. M., Beach S. R. (2014). Perceived discrimination among African American adolescents and allostatic load: A longitudinal analysis with buffering effects. Child Development, 85(3), 989–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brondolo E., Hausmann L. R., Jhalani J., Pencille M., Atencio-Bacayon J., Kumar A., … Crupi R. (2011). Dimensions of perceived racism and self-reported health: Examination of racial/ethnic differences and potential mediators. Annals of Behavioral Medicine, 42(1), 14–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brondolo E., Ver Halen N. B., Pencille M., Beatty D., Contrada R. J. (2009). Coping with racism: A selective review of the literature and a theoretical and methodological critique. Journal of Behavioral Medicine, 32(1), 64–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter S. E., Walker R. L., Cutrona C. E., Simons R. L., Beach S. R. (2016). Anxiety mediates perceived discrimination and health in African-American women. American Journal of Health Behaviors, 40(6), 697–704. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2017). Diagnoses of HIV infection in the United States and dependent areas, 2016 Atlanta, GA: Centers for Disease Control and Prevention. [Google Scholar]
- Centers for Disease Control and Prevention. (2018). Fact sheet: HIV and youth. Retrieved from https://www.cdc.gov/hiv/pdf/group/age/youth/cdc-hiv-youth.pdf
- Colen C. G., Ramey D. M., Cooksey E. C., Williams D. R. (2018). Racial disparities in health among nonpoor African Americans and Hispanics: The role of acute and chronic discrimination. Social Science & Medicine, 199, 167–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deeks S. G., Lewin S. R., Havlir D. V. (2013). The end of AIDS: HIV infection as a chronic disease. The Lancet, 382(9903), 1525–1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw V. A., Rosenthal L., Carroll-Scott A., Santilli A., Gilstad-Hayden K., Ickovics J. R. (2016). Everyday discrimination and physical health: Exploring mental health processes. Journal of Health Psychology, 21(10), 2218–2228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw V. A., Rosenthal L., Lewis J. B., Stasko E. C., Tobin J. N., Lewis T. T., … Ickovics J. R. (2012). Maternal experiences with everyday discrimination and infant birth weight: A test of mediators and moderators among young, urban women of color. Annals of Behavioral Medicine, 45(1), 13–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis R. J., Rosario D., Clifford D. B., McArthur J. C., Simpson D., Alexander T., … Ances B. (2010). Continued high prevalence and adverse clinical impact of human immunodeficiency virus–associated sensory neuropathy in the era of combination antiretroviral therapy: The CHARTER Study. Archives of Neurology, 67(5), 552–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman M. R., Coulter R. W., Silvestre A. J., Stall R., Teplin L., Shoptaw S., … Plankey M. W. (2017). Someone to count on: Social support as an effect modifier of viral load suppression in a prospective cohort study. AIDS Care, 29(4), 469–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gay C., Portillo C. J., Kelly R., Coggins T., Davis H., Aouizerat B. E., … Lee K. A. (2011). Self-reported medication adherence and symptom experience in adults with HIV. Journal of the Association of Nurses in AIDS Care, 22(4), 257–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerrard M., Gibbons F. X., Fleischli M. E., Cutrona C. E., Stock M. L. (2018). Moderation of the effects of discrimination-induced affective responses on health outcomes. Psychology & Health, 33(2), 193–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons F. X., Kingsbury J. H., Weng C. Y., Gerrard M., Cutrona C., Wills T. A., Stock M. (2014). Effects of perceived racial discrimination on health status and health behavior: A differential mediation hypothesis. Health Psychology, 33(1), 11–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grollman E. A. (2014). Multiple disadvantaged statuses and health: The role of multiple forms of discrimination. Journal of Health and Social Behavior, 55(1), 3–19. [DOI] [PubMed] [Google Scholar]
- Harding R., Lampe F. C., Norwood S., Date H. L., Clucas C., Fisher M., … Sherr L. (2010). Symptoms are highly prevalent among HIV outpatients and associated with poor adherence and unprotected sexual intercourse. Sexually Transmitted Infections, 86(7), 520–524. [DOI] [PubMed] [Google Scholar]
- Hayes A. (2013). PROCESS SPSS Macro [Computer software and manual]. [Google Scholar]
- Heinrichs M., Baumgartner T., Kirschbaum C., Ehlert U. (2003). Social support and oxytocin interact to suppress cortisol and subjective responses to psychosocial stress. Biological Psychiatry, 54, 1389–1398. [DOI] [PubMed] [Google Scholar]
- Justice A. C., Holmes W., Gifford A. L., Rabeneck L., Zackin R., Sinclair G., … Cohn S. E. (2001). Development and validation of a self-completed HIV symptom index. Journal of Clinical Epidemiology, 54(12), S77–S90. [DOI] [PubMed] [Google Scholar]
- Lee D. B., Peckins M. K., Heinze J. E., Miller A. L., Assari S., Zimmerman M. A. (2018). Psychological pathways from racial discrimination to cortisol in African American males and females. Journal of Behavioral Medicine, 41(2), 208–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee K. A., Gay C., Portillo C. J., Coggins T., Davis H., Pullinger C. R., Aouizerat B. E. (2009). Symptom experience in HIV-infected adults: A function of demographic and clinical characteristics. Journal of Pain and Symptom Management, 38(6), 882–893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis J. A., Williams M. G., Peppers E. J., Gadson C. A. (2017). Applying intersectionality to explore the relations between gendered racism and health among Black women. Journal of Counseling Psychology, 64(5), 475. [DOI] [PubMed] [Google Scholar]
- Lorenz K. A., Cunningham W. E., Spritzer K. L., Hays R. D. (2006). Changes in symptoms and health-related quality of life in a nationally representative sample of adults in treatment for HIV. Quality of Life Research, 15(6), 951–958. [DOI] [PubMed] [Google Scholar]
- Lubben J., Gironda M., Lee A. (2002). Refinements to the Lubben social network scale: The LSNS-R. The Behavioral Measurement Letter, 7(2), 2–11. [Google Scholar]
- Matheson K., McQuaid R. J., Anisman H. (2016). Group identity, discrimination, and well-being: Confluence of psychosocial and neurobiological factors. Current Opinion in Psychology, 11, 35–39. [Google Scholar]
- McNeil S. N., Fincham F. D., Beach S. R. H. (2014). Does spousal support moderate the association between perceived racial discrimination and depressive symptoms among African American couples? Family Processes, 53(1), 109–119. [DOI] [PubMed] [Google Scholar]
- Meyer I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina K. M., Alegría M., Mahalingam R. (2013). A multiple-group path analysis of the role of everyday discrimination on self-rated physical health among Latina/os in the U.S. Annals of Behavioral Medicine, 45(1), 33–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouzon D. M., Taylor R. J., Woodward A., Chatters L. M. (2017). Everyday racial discrimination, everyday non-racial discrimination, and physical health among African Americans. Journal of Ethnic & Cultural Diversity in Social Work, 26(1–2), 68–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadimpalli S. B., James B. D., Yu L., Cothran F., Barnes L. L. (2015). The association between discrimination and depressive symptoms among older African Americans: The role of psychological and social factors. Experimental Aging Research, 41(1), 1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong A. D., Williams D. R., Nwizu U., Gruenewald T. L. (2017). Everyday unfair treatment and multisystem biological dysregulation in African American adults. Cultural Diversity and Ethnic Minority Psychology, 23(1), 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe E. A., Smart-Richman L. (2009). Perceived discrimination and health: A meta-analytic review. Psychological Bulletin, 135(4), 531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Portillo C. J., Holzemer W. L., Chou F. (2007). HIV symptoms. Annual Review of Nursing Research, 25, 259. [PubMed] [Google Scholar]
- Power R., Koopman C., Volk J., Israelski D. M., Stone L., Chesney M. A., Spiegel D. (2003). Social support, substance use, and denial in relationship to antiretroviral treatment adherence among HIV-infected persons. AIDS Patient Care and STDs, 17(5), 245–252. [DOI] [PubMed] [Google Scholar]
- Samji H., Cescon A., Hogg R. S., Modur S. P., Althoff K. N., Buchacz K., … Justice A. (2013). Closing the gap: Increases in life expectancy among treated HIV-positive individuals in the United States and Canada. PloS One, 8(12), e81355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawyer P. J., Major B., Casad B. J., Townsend S. S., Mendes W. B. (2012). Discrimination and the stress response: Psychological and physiological consequences of anticipating prejudice in interethnic interactions. American Journal of Public Health, 102(5), 1020–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shehadeh N., Rubens M., Attonito J., Jennings T. (2018). Social support and its impact on ethnic identity and HIV risk among migrant workers. Journal of Racial and Ethnic Health Disparities, 5(1), 96–103. [DOI] [PubMed] [Google Scholar]
- Simoni J. M., Frick P. A., Huang B. (2006). A longitudinal evaluation of a social support model of medication adherence among HIV-positive men and women on antiretroviral therapy. Health Psychology, 25(1), 74–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sue D. W., Capodilupo C. M., Torino G. C., Bucceri J. M., Holder A., Nadal K. L., Esquilin M. (2007). Racial microaggressions in everyday life: Implications for clinical practice. American Psychologist, 62(4), 271. [DOI] [PubMed] [Google Scholar]
- Terra L. B.-R., Jules P. H. (2002). Racist experiences and health outcomes: An examination of spirituality as a buffer. Journal of Black Psychology, 28(1), 18–36. [Google Scholar]
- Thoits P. A. (2011). Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior, 52(2), 145–161. [DOI] [PubMed] [Google Scholar]
- Uchino B. N. (2006). Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine, 29(4), 377–387. [DOI] [PubMed] [Google Scholar]
- Vyavaharkar M., Moneyham L., Murdaugh C., Tavakoli A. (2012). Factors associated with quality of life among rural women with HIV disease. AIDS and Behavior, 16(2), 295–303. [DOI] [PubMed] [Google Scholar]
- Willard S., Holzemer W. L., Wantland D. J., Cuca Y. P., Kirksey K. M., Portillo C. J., … Jane Hamilton M. (2009). Does “asymptomatic” mean without symptoms for those living with HIV infection? AIDS Care, 21(3), 322–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D. R., Yan Y., Jackson J. S., Anderson N. B. (1997). Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology, 2(3), 335–351. [DOI] [PubMed] [Google Scholar]
- Wong G., Derthick A. O., David E. J. R., Saw A., Okazaki S. (2014). The what, the why, and the how: A review of racial microaggressions research in psychology. Race and Social Problems, 6(2), 181–200. [DOI] [PMC free article] [PubMed] [Google Scholar]