Abstract
Ongoing trends have revealed an inverse relationship between population growth and the number of practicing urologists in the U.S. per capita, which threatens urologic care accessibility. Furthermore, different regions in the United States may be more negatively impacted due to higher population growth rates. The state of Florida witnessed over a 10% higher growth rate compared with national figures between 2000 and 2015. Coupled with data suggesting that since the 1980s, the number of U.S. urologists per capita has been decreasing, the foreseeable future presents many challenges regarding health equity and accessibility. This secondary analysis aimed to investigate the implications of forecasted urologic care decline within a growing population and how it can contribute to adverse male health outcomes. National- and state-level data were collected to calculate a series of urologic care ratios as defined by the number of urologists compared with population sizes. Analyses revealed that national-level urologic care ratios and prostate cancer incidence rates have a significant positive relationship, lending to the conclusion that with fewer urologists, the number of cases identified will decrease. State-level forecasted models indicated that the urologic care ratio will decrease approximately 30% in Florida from 6.23 per 100,000 in 2010 to 4.39 per 100,000 by the year 2030. As growth in demand for urologic care will increase in the next decade, a dire public health scenario is potentially unfolding. Future implications of undiagnosed prostate cancer due to the lack of access will drive an increase in mortality rates as well as health equity concerns for men.
Keywords: access to care, prostate cancer, health care utilization, health related quality of life, general health and wellness
Overview of the Issue
Increasing Population Size and Decreasing Urologic Health Care Accessibility
Between 2000 and 2015, the population of the United States grew 14.12%, while the state of Florida grew 26.83%, nearly double the national rate (U.S. Census Bureau, 2011, 2015). This, however, is not necessarily a new phenomenon as Florida has historically outpaced the national population growth rate since the early 1980s. For example, Figure 1 illustrates how population growth in Florida is consistently growing faster than that of the United States. Despite these rate differences, the United States and Florida are demographically similar in median age, sex, race, and ethnicity.
Figure 1.
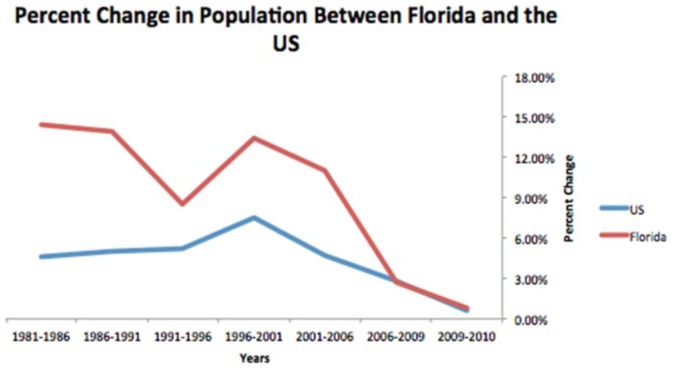
Percentage change in population between Florida and the United States (1986-2010).
As average male life expectancy in the United States has risen by nearly 10%, from 70 to nearly 77 since 1980 (National Center for Health Statistics, 2015), certain regions of the country are simultaneously experiencing a rapid in-migration of older populations. Flynn, Longino, Wiseman, and Biggar (1985), for example, discussed net migration patterns of older Americans relocating to Florida in increasing amounts over three decades ago. Conway and Rork (2016) confirm the same phenomenon occurring in present day. Considering the expeditious overall growth rates, longer life expectancies, and migration patterns of U.S. retirees, certain regions of the country (in this particular case, Florida) will arguably witness exponential demand for urologic care within the next 10 to 20 years.
There is a problem, however, as it pertains to projected availability of urologic care. Williams, Satiani, Thomas, and Ellison (2009) approximate that 12,000 urologists will be needed in the United States by 2030 to be able to meet the demand for urologic services. The population of urologists in the United States, however, has been declining since the early 1980s. Williams et al. (2009) forecasts that only 8,184 urologists are expected to practice in 2030, which is 32% below the recommended amount needed.
This available service issue, unfortunately, is not unique to urology. Williams et al. (2009) states that the United States is projected to have 21.7% less practicing surgeons than it will need in 2030. Juraschek, Zhang, Ranganathan, and Lin (2012) examined the supply and demand of registered nurses and forecasted a severe shortage by 2030 in nearly every state in the United States. Passiment (2006) discussed the shortage of health care workers within the system of laboratory and other technical positions. These various shortages, while being impactful on their own, compounds when combined with all of the other shortages the health care industry may possibly face in the next 10 to 20 years. Marschall and Karimuddin (2003), for example, discussed the negative impact on surgical care at large due to practitioner shortages. If trends continue, quality and quantity of life may be significantly affected.
In terms of the unique situation with urologic care, particularly in regions of the United States like Florida, which is home to the some of the largest and fastest growing retirement communities in the nation (i.e., The Villages; Beach, n.d.), a possible windfall of a rising demand and lessening supply looms. It is, therefore, imperative to discuss current and projected urologic patient panel sizes in order to assess health outcome implications stemming from a rising demand and lessening supply.
Increasing Demand and Quality of Care: Ideal Urologic Patient Panel Sizes
It is important to understand why the aforementioned urologic care demand–supply issue is currently occurring in order to assist in preventing future adverse health outcomes. A major factor, as Kerfoot, Masser, and DeWolf (2006) presented, is that urological education has been slowly removed from medical school curricula with less than one in five medical schools currently requiring a urology rotation. In a historical sense, nearly all medical schools mandated a urology rotation in the 1950s, roughly only 50% in the 1970s, with a steady decline up into the 21st century (Kerfoot et al., 2006). Benson (1994), for example, indicated at the time that up to 15% of medical students have had no exposure to urologic care education. Although the cause of such a phenomenon is unclear, the effect is evident in the present-day decline in the availability of urologic services.
According to Altschuler, Margolius, Bodenheimer, and Grumbach (2012), the ideal patient panel size for a primary care physician is approximately 2,500 due to an increased demand for hours worked per patient treated. In regard to urology, these numbers can vary, according to these authors’ projections. As opposed to primary care, not everyone in the population requires urological care within a given year. The ideal urologic patient panel size, therefore, can be larger than that of a primary care physician. With a conservative estimate of a urologic patient panel size ranging between 5,000 and 7,500 patients, a urologic care ratio of approximately 13 to 20 urologists per 100,000 people is needed to adequately service the population.
Through the life span men require urologic care for differing reasons. For men younger than the age of 50 years, one of the more common reasons for visiting a urologist is prostatitis, which accounts for approximately 10% of all urologist visits within this age group (Collins, Stafford, O’Leary, & Barry, 1998). In terms of prostate cancer (PCa), furthermore, this group accounts for only 1% of all diagnoses (C. Smith et al., 2000). In men 65 years of age and older, approximately 20+% of men are diagnosed with PCa and nearly 28% having enlarged prostates (Issa, Fenter, Black, Grogg, & Kruep, 2006). Clearly, younger men require urologic care for, typically, less life-threatening conditions than older men. This difference, combined with the forecasted population changes in the United States and Florida in coming years, will have a significant impact on the amount and acuity of urologic care.
Yao, Foltz, Odisho, and Wheeler (2015) indicated that for each one additional urologist in a given population, PCa mortality decreases by 0.499 per 100,000 people. Conversely, this also translates into the notion that a depressed urologist ratio can lead to higher mortality rates and years of potential life lost, not to mention possible economic effects therein (see Brott et al., 2011). Evidence additionally suggests that the urologic care ratio is possibly related to diseases not typically associated with urological care, such as colorectal cancer (Albarrak, Ho, & Cheung, 2011), implying that insufficient urologic care accessibility reaches beyond urological diseases, and thus contribute to a decrease in overall quality and quantity of life.
Considering the recent decrease in the present amount of urologists, and an even lesser amount in forecasted models, a lingering concern is a larger workload for future urologic care practitioners, and with that, potential burnout. Shanafelt et al. (2016) indicated that physicians consistently report higher rates of burnout (~50%) and dissatisfaction compared with the general population (~25%). Shanafelt et al. (2012) discussed burnout manifesting symptoms of depression, suicidal thoughts, and a dissatisfaction with work–life balance. The authors further suggested that with burnout comes the risk of physicians decreasing their availability to a more part-time schedule in order to compensate for the growing demand (and subsequent mental strain and pressure) placed on them. The supply of urologists working full-time, therefore, could possibly drop even further, leading to an even worsening situation in the next decade.
The inverse relationship between population growth and the number of practicing urologists in the United States per capita poses a significant threat to future urologic care accessibility, and therefore overall health and wellness of aging male populations. Considering different regions in the United States, particularly Florida, may be more negatively affected due to higher population growth rates and increasing migration levels of retiree populations, the foreseeable future within these areas presents many challenges regarding health equity and accessibility.
Furthermore, underserved communities, particularly African American males, may be affected even more negatively due to current access to quality care issues and disparate PCa outcomes as compared with their Caucasian counterparts. For example, Siegel, Miller, and Jemal (2015) highlight that African American males have the highest overall cancer incidence and mortality rates among all racial/ethnic groups, with an increased risk of PCa death calculated to be about 150% higher than Caucasians. Much of this health outcome disparity, according to Siegel et al. (2015), is attributed to higher rates of poverty among African Americans, as well as a lack of access to high-quality health care resources, including detection and treatment services. It would be a fair assumption to suggest that this population would experience the lion’s share of access issues into the next 10 to 20 years, which would lead to even more disparate health outcomes.
The overarching goal of the following analysis was to forecast the status of urologic health care within the next 10 to 20 years nationally and within the state of Florida. Specifically, urologic care ratios were calculated to serve as potential indicators for PCa incidence and mortality rates within a certain population.
Method
Search Strategy
Demographic information, specific health outcomes between the years 1981 and 2015, and urologic care facility counts were gathered from several national- and state-level (i.e., Florida) public source databases. The majority of the information was extracted from the Florida Department of Health’s Florida Charts, the U.S. Census, ReferenceUSA, U.S. Healthcare databases, and from the American Urologic Association. Due the nature of the demographic data and the time range, some data were unavailable within the aforementioned databases. Further searching was required and the missing data were obtained from published research and government reports.
The data extracted from Florida Charts were matched with the corresponding year of data for population, race, ethnicity, and other demographic information from the 2010 to 2015 U.S. Census. ReferenceUSA provided the count of urologists for Florida through a search filtering process, while U.S. Healthcare data allowed for narrowing the search to primary specialists in urological surgery. Pruthi, Neuwahl, Nielsen, and Fraher (2013) provided for verification on the number of urologists serving in the United States between the years 1981 and 2010. The most current urologist count for Florida was also pulled from ReferenceUSA, while the 2015 national count was sourced from the American Urologic Association.
Primary Measures
Primary outcome variables included national- and state-level PCa-specific incidence and mortality rates, as well as a count of actively practicing urologists per region and overall population per region. To gauge the effect of population growth and decreasing urologic care facilities, present-day and projected “urologic care ratios” were calculated by dividing the number of urologists by the population for both the state of Florida and the United States as a whole.
Results
Descriptive Analyses
Demographic information on race/ethnicity, sex, and median age were extracted to verify population comparability between national- and state-level data. This process assisted in (a) isolating causal factors of observed health outcome differences to the effects of decreasing urologist density and not demographic differences and (b) promoting external validity of findings.
Population growth rates between the years 2000 and 2015 increased for both the United States (14.21%) and Florida (26.83%; see Table 1). Significant differences in growth rate, median age, sex, and race/ethnicity categories exist between Florida and the United States due to the extremely large sample sizes, however, practical significance of the differences should be considered in tandem with statistical probabilities of difference. All-cause, all-cancer-specific, and PCa-specific mortality rates were consistently lower in the state of Florida as compared with the United States (Table 2). PCa-specific incidence rates in Florida were also less than national figures.
Table 1.
U.S. Census Data.
| Population and demographics | ||||||||
|---|---|---|---|---|---|---|---|---|
| Population, 2000-2015 | Sex/age, 2010 | |||||||
| Region | 2000 | 2010 | 2015 | 2000-2015 | Region | Male | Female | Median age |
| USA | 281,421,906 | 308,745,538 | 321,418,820 | +14.21% | USA | 49% | 51% | 37.6 |
| Florida | 15,982,378 | 18,801,310 | 20,271,272 | +26.83% | Florida | 48.9% | 51.1% | 40.7 |
| Race and ethnicity, 2010 | ||||||||
| Region | White | Black | Native Indian or Alaska Native | Asian | Other | Latino/Hispanic | ||
| USA | 72.4% | 12.6% | 0.95% | 4.8% | 6.2% | 16.4% | ||
| Florida | 75% | 16% | 0.4% | 2.4% | 3.6% | 22.5% | ||
Table 2.
General Health Statistics by Region (2010).
| Mortality rates (per 100,000) | |||
|---|---|---|---|
| Region | All-cause | All-cancer-specific | Prostate cancer–specific |
| USA | 863.6 | 207.9 | 21.81 |
| Florida | 810 | 195.6 | 18.63 |
| Prostate cancer–specific incidence rate (per 100,000) | |||
| USA | 122.2 | ||
| Florida | 113.2 | ||
Note. Adapted from http://www.floridacharts.com/FLQUERY/Death/DeathRate.aspx.
Current and Projected Urologic Care Ratios
Although Florida’s current urologic care ratio (6.23 per 100,000) is more than double the national rate (3.10 per 100,000; Table 3), they are both well below these authors’ defined standard of 13 to 20 per 100,000. Given the population and urologist supply projections for 2030, national- and state-level projected urologic care ratios are forecasted to be even lower than present-day figures at 2.18 and 4.39 per 100,000, respectively (Figure 2).
Table 3.
Urologist Rate by Region (2015).
| Region | Population size | Number of urologists | Urologic care ratio (per 100,000) |
|---|---|---|---|
| Current (2015) | |||
| USA | 321,442,019 | 9,979 | 3.10 |
| Florida | 20,271,272 | 1,263 | 6.23 |
| Projected (2030) | |||
| USA | 373,504,00 | 8,164 | 2.18 |
| Florida | 23,601,000 | 1,035 | 4.39 |
Note. Adapted from http://0-www.referenceusa.com.iii.ocls.info/UsHealthcare/Search/Custom/2a4a67c5cf384f669f5897c6f8ad366d; https://www.auanet.org/common/pdf/research/census/State-Urology-Workforce-Practice-US.pdf; and Urologic Care Ratio Projections for 2030 (S. Smith & Rayer, 2013).
Figure 2.
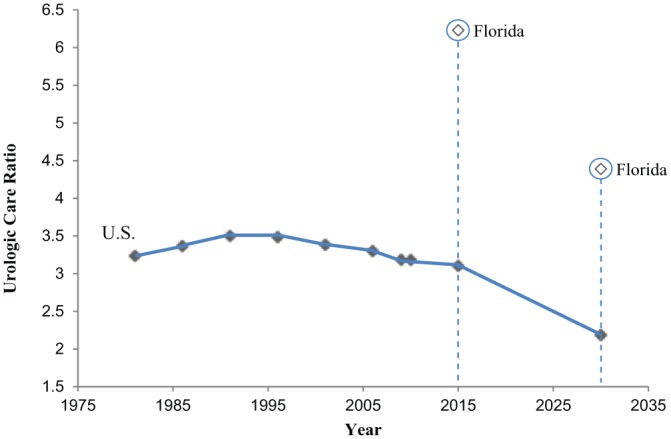
Urologic care ratio trend by year in the United States.
Urologic Care Ratio as a Predictive Measure
A series of Spearman’s correlations were performed on the data up to 2010 to determine the relationship of national PCa-specific incidence and mortality rates with urologic care ratios (Table 4). Statistically significant correlations at the 0.05 critical value level demonstrated strong positive relationships between PCa incidence and mortality rates with urologic care ratios.
Table 4.
Significant Correlations Between PCa Mortality and Incidence Rates and Urologic Care Ratios.
| Variable 1 | Variable 2 | Spearman’s correlation | p |
|---|---|---|---|
| PCa incidence rate (USA) | Urologic care ratio | 0.73 | .038 |
| PCa mortality rate (USA) | Urologic care ratio | 0.88 | .004 |
Urologic care ratio and PCa-specific incidence and mortality rates required a transformation before being included in subsequent inferential analyses to standardize the data and avoid violating linearity assumptions. Table 5 presents the results of a Box–Cox test used to determine which transformations of nonlinear data were appropriate. Furthermore, a set of nonparametric regressions (Table 6) were run to identify predictors of PCa-specific mortality and incidence rates. Independent variables for the regression included median age, urologic care ratio, and population size.
Table 5.
Transformation Values for Primary Measures.
| Variable | Lambda value | Transformation |
|---|---|---|
| PCa incidence rate (USA) | −0.5 | Reciprocal square root |
| PCa mortality rate (USA) | 1 | No transformation |
| Urologic care ratio (USA) | −1 | Reciprocal |
| PCa incidence rate (Florida) | −1 | Reciprocal |
| PCa mortality rate (Florida) | 0 | Log |
Note. PCa = prostate cancer.
Table 6.
Nonparametric Regression Results for Prostate Cancer (PCa) Incidence and Mortality Rates Between Florida and the United States.
| Dependent variable | Independent variable | Beta coefficient | t | p |
|---|---|---|---|---|
| PCa incidence rate (USA) | Urologic care ratio | 1.19 | 4.35 | .012 |
| Median age | 0.009 | 1.69 | .17 | |
| Population | ~0 | na | na | |
| PCa mortality rate (USA) | Urologic care ratio | −284.15 | −3.46 | .026 |
| Median age | 1.04 | 0.67 | .54 | |
| Population | ~0 | −1.58 | .19 | |
| PCa incidence rate (Florida) | Median age | −0.001 | −4.83 | .005 |
| Population | ~0 | na | na | |
| PCa mortality rate (Florida) | Median age | 0.06 | 3.33 | .02 |
| Population | ~0 | −8.53 | .0004 |
Figure 3 shows the relationship derived from the Spearman’s correlation and nonparametric regression between PCa incidence rate and urologic care ratio. The relationship illustrates that as urologic care ratios increase, PCa incidence also increases.
Figure 3.
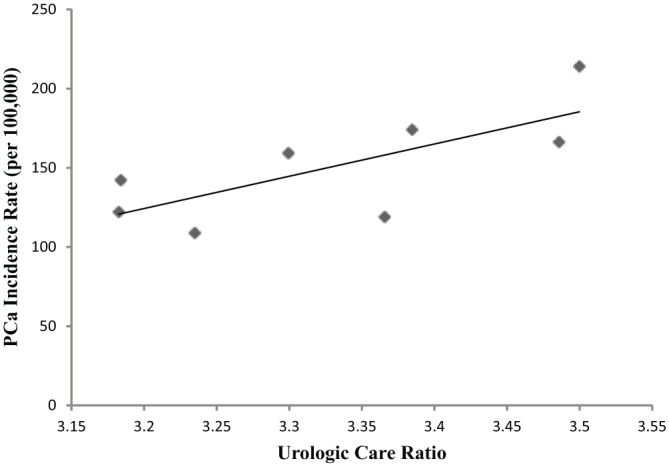
Prostate cancer (PCa) incidence rate by urologic care ratio (USA).
Discussion
Population growth rates are increasing across the United States, however, some regions are experiencing disproportionate growth (i.e., Florida) as compared with the rest of the country (Passel & Cohn, 2008). Taking into further consideration that the number of urologists is projected to decline over the course of the next decade and beyond, a potential health care crisis may begin to unfold in the very near future. Potentially exacerbating this issue further is the fact that regions with the highest growth rates in the United States (again, Florida and the rest of the Sun Belt) have the highest number of immigrant retirees, which would increase demand for urologic services. As indicated in Table 6, median age serves as a significant predictor of PCa incidence rates in Florida. Arguably, as a population grows older, the more powerful of a predictor age becomes on urologic care services.
Urologic Care Accessibility and Implications on Men’s Health Outcomes
The approximate 6.23 urologists per 100,000 Floridians is well below the recommended rate of 13 to 20 per 100,000. Projecting to the year 2030, a 18% decrease in the number of practicing urologists nationwide (Pruthi et al., 2013) lowers Florida’s urologic care ratio to an alarming 5.11 per 100,000, assuming the decrease in total clinicians affects each state proportionately. This projected figure, however, is a conservative estimate due to the assumption of 0% growth in the state of Florida between the years 2015 and 2030. More realistic forecasts using a 15% growth rate for Florida from the present 20.2 million residents to 23.6 million (S. Smith & Rayer, 2013) estimates the urologic care ratio at 4.39 per 100,000. Combine this with the fact that the population in greatest need of urological care are those older than the age of 40 years (see Klein, 2013), Florida’s proportional growth in elderly populations coupled with a decrease in the amount of urologists starts to paint a clearer picture of an impending health care crisis.
These data generally support Odisho, Cooperberg, Fradet, Ahmad, and Carroll’s (2010) discussion of lowered PCa mortality from the expansion of urologic care, Frye et al.’s (2015) work that associated urologic care ratios with PCa mortality rates, and Holmes et al.’s (2012) determination that PCa mortality is related to increasing distances from a urologist. Essentially, these findings support the idea that increasing urologists in a region can detect more cases of PCa (arguably earlier), which will assist in decreasing mortality related to the disease. For example, as shown in Figure 3, PCa incidence is directly related to the urologic care ratio, whereas the ratio increases, PCa incidence also increases. An increase in incidence is attributable to more cases being detected as more men are able to receive adequate and regular urologic care.
These authors must also suggest, however, that a decrease in PCa mortality would not necessarily only result from an increase in the urologic care ratio. There is a high probability that PCa mortality might also decrease when the urologic care ratio is lower due simply because less cases will be diagnosed by the ever-dwindling access to screenings. This relates to Jemal et al.’s (2015) piece suggesting that the lowered use of prostate-specific antigen tests associates with lowering PCa incidence, which is primarily due to lesser amounts of cases being detected, not a lowering amount of cases existing.
While mortality rates are an important aspect of any discussion in health care, many urological diseases are not life threatening, but nevertheless have an immense impact on quality of life when left untreated and unresolved. Untreated urologic conditions, for example, have been linked to nonurological illnesses such as depression and anxiety (Milsom, Kaplan, Coyne, Sexton, & Kopp, 2012). Not only will a urologist deficit lead to increased mortality for diseases such as prostate and renal cancer but it will lead to a deterioration in quality of life as diseases like benign prostatic hyperplasia or idiopathic urinary incontinence go untreated. This may then lead to increased rates of depression and other mental illnesses which have a wide host of comorbidities and impacts on the health of a community.
Future Implications of Men’s Health in the State of Florida
Florida is a diverse region with significant numbers of both urban and rural populations. While large urban areas such as Orlando, Tampa, Jacksonville, and Miami may be somewhat insulated from the growing gap due to large medical infrastructures, rural outlying areas will suffer more as they must travel to metropolitan centers to receive urological care due to “urban flight” of urologists. For example, Colli, Sartor, Thomas, and Lee (2011) indicates that poorer and rural areas tend to experience greater renal cancer mortality rates, thus increasing their burden even more and emphasizing the notion that those with the greatest risk and need are affected the most by this urologic care deficit.
Observing the current trends in men’s health care in the state of Florida is overall a call to the fact that there needs to be more health care resources and services for men suffering from urological conditions and diseases. Neglecting these issues will only lead to further health problems in the future, creating a domino effect in health care as a whole. One such concern would be that due to the lack of available urologic health care services, other physicians and health practitioners might see an increase in their patient panel sizes due in large part to males seeking urologic services. This, as discussed previously, could lead to burnout among these clinicians, this exacerbating the problem even further.
The urologic care ratios at the national and state levels are currently well below the estimates of appropriate care by nearly 75%, with this figure forecasted to decline even further over the next 15 years. This analysis attempts to call attention to this issue in order to prevent an increase in PCa mortality and a decrease in overall quality of life due to possible future shortages of urologic health care services. With the proper awareness, resources, education, and training it may be possible to prevent the deficit from growing and eventually, reverse it until it reaches the ideal urologic care ratio.
Limitations
The prognostications of this article are limited in some ways. Primarily, the suggested ideal urologic care ratio is a generous educated estimate. The area of urologic care panel sizes is in need of more attention to make more precise estimates of the appropriate urologic care ratio. To abate this limitation, our ideal is purposefully broad and generous.
The urologic care ratios in this article are also calculated from the total population, as with the previous point, little is known about what proportions of the population, specifically between males and females, typically require urologic care. Beyond known trends that the elderly population is the group with the highest per capita usage of urologic care, little else can be said with any degree of certainty regarding the demographics of urologist’s patient panels. Using the entire population could introduce threats to external validity of findings.
The use of population and urologist projections, which are inherently uncertain, is also a limitation. As such the predictions of this article should be taken with the same amount of uncertainty as the projections it is based on. This is particularly true regarding the future state of urologic care at the state level. National projections had to be used at the state level, given no state-level projections of that nature have been conducted. It is entirely possible that Florida follows a similar but not exact trend as the national decline in the number of urologists.
Acknowledgments
We would like to acknowledge the Fellows, student interns, and supporters of the Men’s Health Initiative, Inc. and the Behavioral Health Research Group for their tireless work in the field of male health promotion and the behavioral health sciences.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Albarrak J. S., Ho M. Y., Cheung W. Y. (2011, February). Associations between county-level surgeon density and colorectal cancer (CRC) mortality. Journal of Clinical Oncology, 29, 4 Retrieved from http://meeting.ascopubs.org/cgi/content/abstract/29/15_suppl/601821115867 [Google Scholar]
- Altschuler J., Margolius D., Bodenheimer T., Grumbach K. (2012). Estimating a reasonable patient panel size for primary care physicians with team-based task delegation. Annals of Family Medicine, 10, 396-400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach D. (n.d.). United States, State of Florida, Florida Department of Elder Affairs. Retrieved from http://www.myfloridahouse.gov/FileStores/Web/HouseContent/Approved/MinorityLeader/Resources/Senior_FactSheet.pdf
- Benson G. S. (1994). The decline of urological education in United States medical schools. Journal of Urology, 152(1), 169-170. [DOI] [PubMed] [Google Scholar]
- Brott A., Dougherty A., Williams S. T., Matope J. H., Fadich A., Taddelle M. (2011). The economic burden shouldered by public and private entities as a consequence of health disparities between men and women. American Journal of Men’s Health, 5, 528-539. [DOI] [PubMed] [Google Scholar]
- Colli J., Sartor O., Thomas R., Lee B. R. (2011). Does urological cancer mortality increase with low population density of physicians? Journal of Urology, 186, 2342-2346. [DOI] [PubMed] [Google Scholar]
- Collins M. M., Stafford R. S., O’Leary M. P., Barry M. J. (1998). How common is prostatitis? A national survey of physician visits. Journal of Urology, 159, 1224-1228. [PubMed] [Google Scholar]
- Conway K. S., Rork J. C. (2016). How has elderly migration changed in the twenty-first century? What the data can—and cannot—tell us. Demography. Advance online publication. doi: 10.1007/s13524-016-0477-7 [DOI] [PubMed] [Google Scholar]
- Flynn C. B., Longino C. F., Wiseman R. F., Biggar J. C. (1985). The redistribution of America’s older population: Major national migration patterns for three census decades, 1960–1980. The Gerontologist, 25, 292-296. [DOI] [PubMed] [Google Scholar]
- Frye T., Sadowski D., Zahnd W., Jenkins W., Dynda D., Mueller G., . . . McVary K. (2015). Impact of county rurality and urologist density on urological cancer mortality in Illinois. Journal of Urology, 193, 1608-1614. [DOI] [PubMed] [Google Scholar]
- Holmes J. A., Carpenter W. R., Wu Y., Hendrix L. H., Peacock S., Massing M., . . . Chen R. C. (2012). Impact of distance to a urologist on early diagnosis of prostate cancer among black and white patients. Journal of Urology, 187, 883-888. [DOI] [PubMed] [Google Scholar]
- Issa M. M., Fenter T. C., Black L., Grogg A. L., Kruep E. J. (2006). An assessment of the diagnosed prevalence of diseases in men 50 years of age or older. American Journal of Managed Care, 12(4 Suppl.), S83-S89. [PubMed] [Google Scholar]
- Jemal A., Fedewa S. A., Ma J., Siegel R., Lin C. C., Brawley O., Ward E. M. (2015). Prostate cancer incidence and PSA testing patterns in relation to USPSTF screening recommendations. Journal of the American Medical Association, 314, 2054-2061. [DOI] [PubMed] [Google Scholar]
- Juraschek S. P., Zhang X., Ranganathan V., Lin V. W. (2012). United States registered nurse workforce report card and shortage forecast. American Journal of Medical Quality, 27, 241-249. [DOI] [PubMed] [Google Scholar]
- Kerfoot B. P., Masser B. A., DeWolf W. C. (2006). The continued decline of formal urological education of medical students in the United States: Does it matter? Journal of Urology, 175, 2243-2248. [DOI] [PubMed] [Google Scholar]
- Klein E. (2013, June 13). Men over 40: Start seeing a urologist regularly. Health Essentials. Retrieved from https://health.clevelandclinic.org/2013/06/men-over-40-start-seeing-a-urologist-regularly/
- Marschall J. G., Karimuddin A. A. (2003). Decline in popularity of general surgery as a career choice in North America: Review of postgraduate residency training selection in Canada, 1996–2001. World Journal of Surgery, 27, 249-252. [DOI] [PubMed] [Google Scholar]
- Milsom I., Kaplan S. A., Coyne K. S., Sexton C. C., Kopp Z. S. (2012). Effect of bothersome overactive bladder symptoms on health-related quality of life, anxiety, depression, and treatment seeking in the United States: Results from EpiLUTS. Journal of Urology, 80, 90-96. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. (2015). Health, United States, 2014: With special feature on adults aged 55–64. Hyattsville, MD: Author. [PubMed] [Google Scholar]
- Odisho A., Cooperberg M., Fradet V., Ahmad A., Carroll P. (2010). Urologist density and county-level urologic cancer mortality. Journal of Clinical Oncology, 28, 2499-2504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passel J. S., Cohn D. (2008). U.S. population projections: 2005-2050. Retrieved from http://www.pewhispanic.org/files/reports/85.pdf
- Passiment E. (2006). Update on the laboratory workforce-shortage crisis. MLO: Medical Laboratory Observer, 38, 64, 38. [PubMed] [Google Scholar]
- Pruthi R., Neuwahl S., Nielsen M., Fraher E. (2013). Recent trends in the urology workforce in the United States. Urology, 82, 987-994. [DOI] [PubMed] [Google Scholar]
- Siegel R. L., Miller K. D., Jemal A. (2015). Cancer statistics, 2015. CA: A Cancer Journal for Clinicians, 65, 5-29. [DOI] [PubMed] [Google Scholar]
- Shanafelt T. D., Boone S., Tan L., Dyrbye L. N., Sotile W., Satele D., . . . Oreskovich M. R. (2012). Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Archives of Internal Medicine, 172, 1377-1385. [DOI] [PubMed] [Google Scholar]
- Shanafelt T. D., Mungo M., Schmitgen J., Storz K. A., Reeves D., Hayes S. N., . . . Buskirk S. J. (2016). Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clinic Proceedings, 91, 422-431. [DOI] [PubMed] [Google Scholar]
- Smith C. V., Bauer J. J., Connelly R. R., Seay T., Kane C., Foley J., . . . Moul J. W. (2000). Prostate cancer in men age 50 years or younger: A review of the Department of Defense Center for Prostate Disease Research multicenter prostate cancer database. Journal of Urology, 164, 1964-1967. [DOI] [PubMed] [Google Scholar]
- Smith S. K., Rayer S. (2013). Projections of Florida population by county, 2015-2040, with estimates for 2012. Florida Population Studies, 46, Bulletin 165 Retrieved from https://www.bebr.ufl.edu/sites/default/files/Research%20Reports/projections_2013.pdf [Google Scholar]
- U.S. Census Bureau. (2011). Population distribution and change: 2000 to 2010. Retrieved from http://www.census.gov/prod/cen2010/briefs/c2010br-01.pdf
- U.S. Census Bureau (2015). United States Quick Facts. Retrieved from http://www.census.gov/quickfacts/table/PST045215/00
- Williams T., Satiani B., Thomas A., Ellison E. (2009). The impending shortage and the estimated cost of training the future surgical workforce. Annals of Surgery, 250, 590-597. [DOI] [PubMed] [Google Scholar]
- Yao N., Foltz S., Odisho A., Wheeler D. (2015). Geographic analysis of urologist density and prostate cancer mortality in the United States. PLoS ONE, 10, 6. doi: 10.1371/journal.pone.0131578 [DOI] [PMC free article] [PubMed] [Google Scholar]


