Abstract
Background
Genetic cascade screening is the most cost-effective method for the identification of individuals with familial hypercholesterolemia (FH), but the best strategies for the enrollment of at-risk individuals in a FH screening program are not fully known.
Objective
The aim of this study is to identify the best predictors of familial enrollment into genetic screening, using features derived from tested probands.
Methods
One hundred and eighty-three index-cases (ICs) with a positive genetic result that had relatives screened from 01/2011 to 07/2015 were included. The response variable was the number of relatives for each enrolled IC. All variables in the study were based on ICs’ derived clinical and socioeconomical features. The effect size of predictor variables were obtained through a general linear model using a negative binomial regression link function. Significance was considered with a p < 0.05.
Results
Mean IC age when enrolling into the program was 50 years old; 78.1% of individuals reported knowledge of relatives with dyslipidemia. Mean baseline LDL-cholesterol level was 316 ± 90 mg/dL. Referral origin through the cascade program website vs. tertiary care, IC LDL-cholesterol and familial history of high LDL-cholesterol levels were independent predictors associated with a higher number of enrolled relatives.
Conclusions
Our data suggest that FH cascade screening programs can predict family enrollment based on IC features. This information may be useful for devising better and more effective screening approaches for at-risk individuals.
Keywords: Hypelipoproteinemia Type II/genetics, Mass Screening, Dyslipidemias/genetics, Hypercholesterolemia, Genetic Testing, Cholesterol
Introduction
Familial hypercholesterolemia (FH) is a genetic disease characterized by elevated blood LDL cholesterol (LDL-C) levels. FH is usually caused by mutations in the gene encoding the LDL receptor (LDLR) and less frequently (~5% of cases) by mutations in genes coding for apolipoprotein-B (APOB) or proprotein convertase subtilisin/kexin type 9 (PCSK9). Individuals carrying these mutations are exposed to high lipid levels and, thus, have a higher risk of developing early atherosclerotic cardiovascular disease and mortality.1,2
The worldwide prevalence of heterozygous FH ranges between 1:200 and 1:500 individuals, varying in a few countries.3,4 FH is an underdiagnosed disease and, therefore, most affected individuals do not have access to proper treatment until later in life.5
FH diagnosis usually involves the identification of typical clinical signs of the disease such as high levels of LDL-C (> 190 mg/dL), tissue cholesterol deposition (e.g. tendon xanthomas and corneal arcus when detected in individuals less than 45 years old), a family history of high blood cholesterol and or early atherosclerotic disease.6
In many instances, a typical FH index case (IC) is clinically diagnosed after the onset of an atherosclerotic cardiovascular event. Due to its autosomal dominant transmission, FH can and must be diagnosed early in asymptomatic relatives to start LDL-C lowering treatment with the aim of preventing cardiovascular disease onset. Genetic testing is important not only for diagnostic confirmation of index cases and in relatives, but also as a prognostic tool since recent evidence confirmed that the presence of FH-causing mutations implicates in higher cardiovascular risk even in comparison with other hypercholesterolemic individuals.7,8
Currently, cascade genetic screening is the most cost-effective method for FH diagnosis.9-12 The screening begins with the clinical and genetic diagnosis of an IC, of which all first-degree relatives are screened for the same mutation. After the identification of all affected relatives, the cascade gives sequence to all 2nd-degree relatives, and then successively. Most importantly, the higher the number of screened relatives, the more cost-effective the cascade becomes.13,14
Interestingly, despite being recognized as the most cost-effective strategy for population-wide FH identification, little is known about the best strategies for maximizing the enrollment of at-risk individuals in a cascade screening program. One can argue that this information is even more important than devising ways to identify index-cases to be tested from the overall population.. Therefore, the aim of this study is to identify the main predictors of family enrollment into cascade screening using the IC as a starting point.
Methods
The Brazilian FH screening program (HipercolBrasil) is performed by the Laboratory of Genetics and Molecular Cardiology at the Heart Institute (InCor) of the University of São Paulo Medical School Hospital. This study was approved by the institutional ethics committee (CAPPesq 3757/12/013). All participants read and signed an informed consent form authorizing the study.
Participants included in our analysis were previously registered in the HipercolBrasil Program and were referred to the program by institutional physicians or by other collaborators. Individuals that spontaneously contacted the program by phone or website were also included. Once the inclusion criteria were met, participants were referred to molecular genetic testing.
Study population and inclusion criteria
The inclusion criterion for program enrollment was the presence of a baseline LDL-C value ≥ 210 mg/dL. However, some individuals with LDL-C < 210 mg/dL were also enrolled when suggestive signs of FH were detected by the physicians. All genetic positive ICs (individuals in which a pathogenic or likely pathogenic mutations were identified) who authorized the screening of relatives from January 2011 to July 2015 were included in the present study.
Whole blood was collected after a physical exam was performed and a standardized questionnaire was applied by trained personnel from the HipercolBrasil team. In case of a positive genetic result, the IC was contacted and informed about the importance of the genetic results and the possibility of free family screening. After a comprehensive explanation of the disease risks and early diagnosis benefits, the IC was asked to provide information on all at-risk first-degree relatives. These were then contacted by phone and invited to join the cascade program by trained specialized health professionals. The screening in relatives is restricted to the same mutation found in the IC, despite the presence or not of FH clinical features. All relatives also signed the informed consent form and were submitted to the same standardized questionnaire application.
Study variables
Possible predictor variables from ICs were obtained before the genetic test results were available. The standardized questionnaire consisted of socioeconomic, clinical and biochemical variables.
Information regarding employment status consisted of three categories: employed (working age, individual currently working); unemployed (working age, individual not currently working) and inactive (students, elderly and/or retired individuals and those with special needs unable to work). Educational level was defined as: illiterate, elementary education, high-school education, and college/university.
IC origin was defined according to whom or from where the patient was referred to the program. ICs could have been referred by physicians from the Lipid Clinic of the Heart Institute (the lipids referral center closely associated with the HipercolBrasil program); from partner centers located at other tertiary care institutions; from private physicians; by the patient itself through the program website (www.hipercolesterolemia.com.br); or by a primary health care unit. Enrollment criteria were the same for all ICs regardless of origin. The participation of other partner centers in the study was approved by the institutional ethics committee (CAAE 00594212.0.0000.0068/nº:1.213.994).
Required clinical information was: occurrence of atherosclerotic or familial history of early atherosclerotic cardiovascular disease and/or altered lipid levels; clinical stigmata such as corneal arcus, xanthelasmas or xanthomas. Biochemical exams were obtained from medical records or from previous exams brought by the patient. The following values were recorded: total cholesterol (TC), LDL-C, HDL-C, triglycerides (TG) and fasting glucose. The Dutch Lipid Clinic Network (DLNC) score and Simon Broome criteria were calculated using the available information at the baseline visit. Whenever possible, the baseline value of LDL-C was used. In case of a patient receiving lipid-lowering treatment with unavailable baseline LDL-C values, the current value was used to calculate the score. Those clinical scores were applied only with the intention of collecting and storing data and were not used as criteria for program enrollment.
Genetic testing
IC samples were sequenced for six FH-related genes: LDLR, APOB, PCSK9, LDLRAP1, LIPA and APOE. Target regions were considered as coding exons plus 10bp of introns up and downstream and captured using a specially designed enrichment reagent. Templates were prepared on Ion One Touch System and sequenced in Ion Torrent PGM® platform, with 32 samples per run in a 316v2 Ion Chip. Bioinformatics analyses were performed in CLC Genomics Workbench 9.5 (QIAGEN) in a custom pipeline. Minimum quality requirements for variant call were: Base quality of PhredQ ≥ 20; Target-region coverage ≥ 10x; Frequency of variant allele ≥ 20% and bidirectional presence of variant allele.
After filtering for a MAF ≤ 0.002 with control populations (NHLBI-ESP6500, AbraOM, ExAC and 1000Genomes), all potential mutations were consulted for previous description in ClinVar, Human Genome Mutation Database (HGMD), British Heart Foundation and Jojo Genetics databases. Functional impact prediction was performed with SIFT, PROVEAN and PolyPhen-2 and mutations without a previous description should be indicated as damaging in at least two algorithms to be considered as potentially pathogenic. Individuals with negative results were also screened for large insertions and deletions via MLPA (MRC-Holland). Point mutations found in ICs were screened in relatives through Sanger sequencing, and large insertions/deletions via MLPA.
Statistical analysis
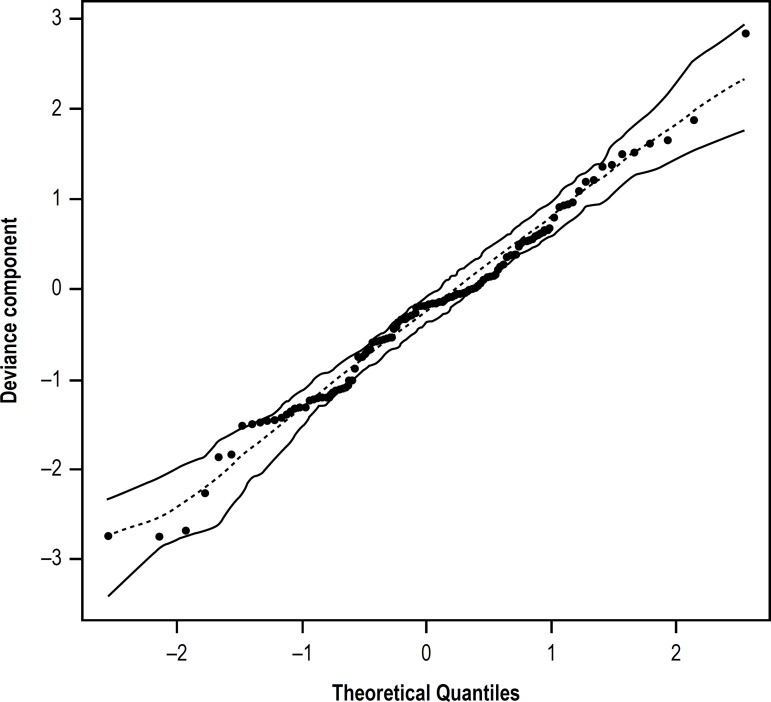
The response variable of this study consisted in the number of family members enrolled in the program by each family, starting from a positive IC. The response variable consists of count data, which would suggest the application of a Poisson model. However, as the dependent variable variance was higher than the mean value, the most adequate model in this situation was the negative binomial model, due to data overdispersion (Figure 1). Predictive variables were based on the IC’s clinical and socioeconomic characteristics. We initially performed a distribution analysis on the response variable and the model that appropriately fit this variable was one using a negative binomial distribution. Thus, the estimate for predictor variables for the number of enrolled relatives was derived through a general linear model using a negative binomial regression link function. The following variables were included in the initial model: age, family history of high cholesterol levels, DLNC score, Simon Broome Score, baseline lipid-lowering treatment, employment situation, baseline LDL-C or highest level during treatment, educational level and origin. The mean and standard deviation were calculated for continuous variables. Significance was considered at a p < 0.05. Statistical analyses were performed with SPSS v19.0 (IBM) and R software (Package gamlss, version 3.3.1).
Figure 1.
QQ Plot for the general linear model using a negative binomial distribution.
Results
A total of 183 ICs were analyzed, of which 2316 relatives were contacted and 1605 agreed to enroll in the program (overall enrollment rate of 69.3%). Eighty-seven families were excluded from the study after model adjustment for multiple regression analysis. These were related to 87 ICs that had missing data in at least one of the variables included in the final model. Clinical characteristics of the ICs are shown in Table 1.
Table 1.
Clinical characteristics of Index cases
| Variables | n | |
|---|---|---|
| Age (Mean ± SD) | 183 | 47 ± 18 |
| Male sex (%) | 84 | 45.9 |
| Tendon xanthomas (%) | 26 | 14.2 |
| Corneal Arcus (%) | 49 | 26.8 |
| Early coronary disease (%)* | 54 | 29.5 |
| Family history of early coronary disease (%)† | 72 | 39.3 |
| Family history of increased LDL-C levels(%)‡ | 98 | 53.6 |
| Current pharmacological treatment (%)§ | 145 | 79.2 |
| DLCN Score (%) | ||
| Definitive | 74 | 40.4 |
| Probable | 48 | 26.2 |
| Possible | 33 | 18.0 |
| Simon Broome (%) | ||
| Definitive | 29 | 15.8 |
| Probable | 124 | 67.8 |
| Baseline TC// mg/dL (Mean ± SD) | 104 | 405 ± 112 |
| TC mg/dL (Mean±SD) highest level during treatment | 64 | 305 ± 124 |
| Baseline LDL-C mg/dL (Mean ± SD) | 104 | 326 ± 111 |
| LDL-C mg/dL (Mean ± SD) highest level during treatment | 64 | 238 ± 122 |
| Baseline HDL-C mg/dL (Mean ± SD) | 102 | 47 ± 15 |
| HDL-C mg/dL (Mean±SD) highest level during treatment | 64 | 43 ± 10 |
| Baseline TG¶ mg/dL (Mean ± SD) | 99 | 144 ± 63 |
| TG mg/dL (Mean ± SD) highest level during treatment | 32 | 132 ± 77 |
Coronary disease in men aged < 55 years or women aged < 60 years.
Family history of coronary disease (e.g.. heart attack) in first or second degree relatives (men aged < 55 years and women < 60 years).
First or second degree relatives with TC > 260 mg/dl or LDL > 160 mg/dL in children (> 16 years old) or TC > 290 mg/dL or LDL > 190 mg/dL in adults (pre-treatment levels or the highest level during treatment).
Current use of lipid-lowering drugs (e.g. statins).
TC: total cholesterol; TG: triglycerides. SD:standard deviation; DLCN: Dutch Lipid Clinic Network; HDL-C: high-density lipoprotein cholesterol; LDL-C: Low-density lipoprotein cholesterol.
Regarding the educational level, 30.6% of ICs had college, 25.1% high-school, 22.4% elementary education and 4.9% were illiterate. The greatest percentage of ICs is currently employed (41.0%). Most of ICs were referred by local physicians (81.4%), followed by 7.7% of patients that reached the program via the website. The other 5% were referred from partner centers located at other tertiary care institutions and 3.3% from private physicians.
Table 2 shows the univariate negative binomial regression calculated for all the variables in the study. Only family history of altered lipid levels and referral of patients via the website were significantly associated with the number of relatives brought into the program.
Table 2.
Parameters associated with relatives’ inclusion in the cascade screening according to univariate negative binomial regression analysis
| Predictors | Estimate | Std. Error | p value* |
|---|---|---|---|
| Age (years) | 0.005 | 0.003 | 0.141 |
| Early coronary disease† | -0.024 | 0.143 | 0.867 |
| DLCN‡ Score (Probable) | 0.117 | 0.415 | 0.777 |
| DLCN Score (Possible) | -0.158 | 0.600 | 0.792 |
| Family history of early coronary disease | 0.136 | 0.171 | 0.425 |
| Family history of increased LDL-C levels | 0.395 | 0.201 | 0.048 |
| Educational level (Elementary) | 0.460 | 0.326 | 0.159 |
| Educational level (High School) | 0.355 | 0.324 | 0.273 |
| Educational level (College) | 0.219 | 0.320 | 0.494 |
| Employment Situation (Unemployed) | -0.175 | 0.247 | 0.479 |
| Employment Situation (Inactive) | -0.204 | 0.150 | 0.174 |
| Origin§ (Rio de Janeiro) | -0.751 | 0.400 | 0.060 |
| Origin (website//) | -0.745 | 0.245 | 0.002 |
| Current pharmacological treatment | 0.179 | 0.190 | 0.346 |
| LDL-C | 0.001 | 0.000 | 0.112 |
p value < 0.05.
Coronary disease in men aged < 55 years or women aged < 60 years.
DLCN: Dutch Lipid Clinic Network.
IC origin was defined according to whom or from where the patient was referred to the program.
Website: by the patient itself via the program website. LDL-C: Low-density lipoprotein cholesterol.
Results after model adjustment are outlined in Table 3. Family history of high LDL-C levels was an independent predictor associated with a higher number of enrolled relatives, with an increasing estimate of 1.76-fold when comparing ICs with and without family history of dyslipidemia. IC baseline LDL-Cvalues were also associated with a higher number of enrolled relatives.
Table 3.
Parameters associated with relatives’ inclusion in the cascade screening according to multiple negative binomial regression analysis
| Predictors | Estimate | Std. Error | p value* |
|---|---|---|---|
| Origin (website)† | -0.846 | 0.339 | 0.012 |
| Family history of increased LDL-C levels | 0.565 | 0.210 | 0.007 |
| LDL-C | 0.002 | 0.000 | 0.004 |
p value < 0.05.
IC origin was defined according to whom or from where the patient was referred to the program. Website: by the patient itself via the program website. LDL-C: Low-density lipoprotein cholesterol.
The IC referral origin also significantly influenced the number of relatives in the program. When comparing the origin of ICs, for those enrolled via website the expected number of relatives decreased by 0.42-fold when compared to ICs referred from inside a referral center.
Discussion
The present study is, to the best of our knowledge, the first to assess the predictors that might influence enrollment of relatives in a genetic FH cascade screening program, considering clinical, demographic and socioeconomic features of ICs as the main source. Currently, for every IC with a pathogenic variant identified by molecular genetic testing, around 69.3% of eligible relatives are enrolled in our cascade screening program. For each positive IC we identified 1.8 affected relatives.13
Based on ICs’ characteristics, the factor that most influences the inclusion of relatives in the program is a reported family history of dyslipidemia. High levels of LDL-C in ICs also contributed to the enrollment of relatives in the cohort, suggesting that some measure of the IC dyslipidemia severity also modulates the relatives’ willingness to enroll in disease screening.
Once enrolled in the program, ICs are provided with systematic recommendations about the importance of family screening, mainly due to the possible identification of at-risk individuals, which makes genetic testing of great importance. Genetic testing not only confirms the ICs’ clinical diagnosis, but also elucidates the family history of dyslipidemia and the existence of at-risk relatives.15
Relatives frequently underestimate the disease risks and are not aware of their condition, increasing the chance of early atherosclerotic cardiovascular event onset.16-18 Sometimes, even though embodied with knowledge of the importance of genetic testing, they remain reluctant to participate due to the lack of motivation.19
The cascade effectiveness depends on the ICs’ agreement to recruit relatives through the program and on the actual enrollment of these relatives, so that the ideal scenario is the enrolment of all eligible individuals.20,21 To find the best strategy for familial enrollment in a cascade screening program is relevant and impacts the overall cascade’s cost-effectiveness. The Dutch FH cohort reported the obstacles in recruiting relatives after 5 years of cascade screening,22 even with a relatively efficient rate of enrollment. Some of the most important raised points are the social and ethical questions surrounding genetic testing, but also the fact that many participants died before having the chance to enroll in the cascade. Many countries have already implemented this form of detection, revealing its feasibility9,13,14,22 which is considered the gold-standard method referred by the NICE guidelines.16
Recruiting ICs via website was a factor that decreased the chance of familial enrollment when compared to ICs referred from the Lipid Clinic of the Heart Institute, a tertiary referral center. This result is probably related to both the amount of information that ICs receive and the severity of the ICs’ condition. Those recruited by specialists of tertiary health centers are more conscious about their risks as well as for their relatives. On the other hand, those recruited via website are only guided by the screening program. Therefore, the amount of information delivered by the screening program only might not be enough for the ICs to understand the importance of family enrollment, suggesting that awareness should be emphasized even after several visits.
Unexpectedly, we did not observe a significant effect of the educational level on family enrollment prediction. This observation deserves further study, since it may suggest new ways for educational and awareness programs to be developed.
One limitation of our study is that it is based on a genetic-screening cascade and that the identified predictors may not apply to biochemical-based cascades, since the genetic cascade is only performed for those individuals with a pathogenic variant of FH.
Conclusions
Early diagnosis through cascade screening is important for the prevention of risk factors, because over time individuals would be diagnosed early in their lives or even in childhood, thus allowing adequate treatment and prevention of additional risks. With cascade screening, the relatives are diagnosed at a younger age, which is the main factor that characterizes the effectiveness of this diagnostic method. We conclude that after four years of screening, family history of dyslipidemia, as well as high LDL-C levels are the factors that most influenced the inclusion of relatives in the genetic cascade. A professional approach certainly plays an important role in family adherence and our results laid the foundations for the planning of specific intervention trials designed to test new approaches for increasing family enrollment.
The funding of Sociedade Hospital Samaritano and Ministério da Saúde (PROADI-SUS; SIPAR: 25000.180.672/2011-81) and FAPESP (grant n. 2013/17368-0) are gratefully acknowledged.
Acknowledgments
The authors would like to thank all the patients who participated in the cohort and the entire professional staff of Laboratory of Genetics and Molecular Cardiology of the Heart Institute (InCor)/University of São Paulo Medical School Hospital.
References
- 1.Santos RD, Gidding SS, Hegele RA, Cuchel MA, Barter PJ, Watts GF, et al. Defining severe familial hypercholesterolaemia and the implications for clinical management : a consensus statement from the International Atherosclerosis Society Severe Familial Hypercholesterolemia Panel. Lancet Diabetes Endocrinol. 2016;4(10):850–861. doi: 10.1016/S2213-8587(16)30041-9. [DOI] [PubMed] [Google Scholar]
- 2.Silva P, Jannes CE, Marsiglia JDC, Krieger JE, Santos RD, Pereira AC. Predictors of cardiovascular events after one year of molecular screening for Familial hypercholesterolemia. Atherosclerosis. 2016 Jul;250:144–150. doi: 10.1016/j.atherosclerosis.2016.05.023. [DOI] [PubMed] [Google Scholar]
- 3.Nordestgaard BG, Chapman MJ, Humphries SE, Ginsberg HN, Masana L, Descamps OS, et al. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: Guidance for clinicians to prevent coronary heart disease. Eur Heart J. 2013;34(45):3478a–3490a. doi: 10.1093/eurheartj/eht273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pajak A, Szafraniec K, Polak M, Drygas W, Piotrowski W, Zdrojewski T, et al. Prevalence of familial hypercholesterolemia: A meta-analysis of six large, observational, population-based studies in Poland. Arch Med Sci. 2016;12(4):687–696. doi: 10.5114/aoms.2016.59700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benn M, Watts GF, Tybjaerg-Hansen A, Nordestgaard BG. Familial hypercholesterolemia in the danish general population: prevalence, coronary artery disease, and cholesterol-lowering medication. J Clin Endocrinol Metab. 2012;97(11):3956–3964. doi: 10.1210/jc.2012-1563. [DOI] [PubMed] [Google Scholar]
- 6.Santos RD, Gagliardi AC, Xavier HT, Casella Filho A, Araujo DB, Cesena FY, et al. First Brazilian Guidelines for Familial Hypercholesterolemia. Arq Bras Cardiol. 2012;99(2) Suppl 2:1–28. doi: 10.5935/abc.20120202. [DOI] [PubMed] [Google Scholar]
- 7.Brautbar A, Leary E, Rasmussen K, Wilson DP, Steiner RD, Virani S. Genetics of familial hypercholesterolemia. Curr Atheroscler Rep. 2015;17(4):491–491. doi: 10.1007/s11883-015-0491-z. [DOI] [PubMed] [Google Scholar]
- 8.Khera A V, Won HH, Peloso GM, Lawson KS, Bartz TM, Deng X, et al. Diagnostic yield and clinical utility of sequencing familial hypercholesterolemia genes in patients with severe hypercholesterolemia. J Am Coll Cardiol. 2016;67(22):2578–2589. doi: 10.1016/j.jacc.2016.03.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Santos RD, Bourbon M, Alonso R, Cuevas A, Vásquez-Cárdenas A, Pereira AC, et al. Clinical and molecular aspects of familial hypercholesterolemia in Ibero-American countries. J Clin Lipidol. 2016;11(1):160–166. doi: 10.1016/j.jacl.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 10.Henderson R, O’Kane M, McGilligan V, Watterson S. The genetics and screening of familial hypercholesterolaemia. J Biomed Sci. 2016 Apr 16;23:39–39. doi: 10.1186/s12929-016-0256-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kerr M, Pears R, Miedzybrodzka Z, Haralambos K, Cather M, Watson M, et al. Cost effectiveness of cascade testing for familial hypercholesterolaemia, based on data from familial hypercholesterolaemia services in the UK. Eur Heart J. 2017;38(23):1832–1839. doi: 10.1093/eurheartj/ehx111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lázaro P, Pérez de Isla L, Watts GF, Alonso R, Norman R, Muñiz O, et al. Cost-effectiveness of a cascade screening program for the early detection of familial hypercholesterolemia. J Clin Lipidol. 2017;11(1):260–271. doi: 10.1016/j.jacl.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 13.Jannes CE, Santos RD, de Souza Silva PR, Turolla L, Gagliardi ACM, Marsiglia JDC, et al. Familial hypercholesterolemia in Brazil: Cascade screening program, clinical and genetic aspects. Atherosclerosis. 2015;238(1):101–107. doi: 10.1016/j.atherosclerosis.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 14.Bell DA, Pang J, Burrows S, Bates TR, van Bockxmeer FM, Hooper AJ, et al. Effectiveness of genetic cascade screening for familial hypercholesterolaemia using a centrally co-ordinated clinical service: an Australian experience. Atherosclerosis. 2015;239(1):93–100. doi: 10.1016/j.atherosclerosis.2014.12.036. [DOI] [PubMed] [Google Scholar]
- 15.Hallowell N, Jenkins N, Douglas M, Walker S, Finnie R, Porteous M, et al. Patients’ experiences and views of cascade screening for familial hypercholesterolemia (FH): A qualitative study. J Community Genet. 2011;2(4):249–257. doi: 10.1007/s12687-011-0064-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Institute for Health and Clinical Excellence . Familial Hypercholesterolaemia - Costing Report: Implementing NICE guidance. London: 2009. pp. 1–42. [Google Scholar]
- 17.Finnie RM. Cascade screening for familial hypercholesterolaemia in Scotland. Br J Diabetes Vasc Dis. 2010;10(3):123–125. [Google Scholar]
- 18.Neal WA, Knowles J, Wilemon K. Underutilization of cascade screening for familial hypercholesterolemia. Clin Lipidol. 2014;9(3):291–293. [Google Scholar]
- 19.Hardcastle SJ, Legge E, Laundy CS, Egan SJ, French R, Watts GF, et al. Patients’ perceptions and experiences of familial hypercholesterolemia, cascade genetic screening and treatment. Int J Behav Med. 2015;22(1):92–100. doi: 10.1007/s12529-014-9402-x. [DOI] [PubMed] [Google Scholar]
- 20.Watts GF, Sullivan DR, Poplawski N, van Bockxmeer F, Hamilton-Craig I, Clifton PM, et al. Familial hypercholesterolaemia: A model of care for Australasia. Atheroscler Suppl. 2011;12(2):221–263. doi: 10.1016/j.atherosclerosissup.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 21.Newson AJ, Humphries SE. Cascade testing in familial hypercholesterolaemia: how should family members be contacted? Eur J Hum Genet. 2005;13(4):401–408. doi: 10.1038/sj.ejhg.5201360. [DOI] [PubMed] [Google Scholar]
- 22.Umans-Eckenhausen MAW, Defesche JC, Sijbrands EJG, Scheerder RLJM, Kastelein JJP. Review of first 5 years of screening for familial hypercholesterolaemia in the Netherlands. Lancet. 2001;357(9251):165–168. doi: 10.1016/S0140-6736(00)03587-X. [DOI] [PubMed] [Google Scholar]