Abstract
Objective
The hidden curriculum is a set of influences that function at the level of organizational structure and culture which fall outside the formal curriculum, and are often unarticulated or unexplored. Learning associated with the hidden curriculum may have negative consequences on trainee educational development. The study goal was to examine how aspects of the hidden curriculum were enacted during ward rounds on a tertiary care general paediatrics clinical teaching unit (CTU).
Methods
We conducted an ethnographic case study on a CTU of a tertiary care paediatric hospital and observed interactions between medical students, residents and attending staff on rounds. Detailed field notes were collected and inductive analysis was used to inform descriptions and identify themes regarding the hidden curriculum.
Results
Twenty-two hours of observation were performed. Two major themes emerged: the hierarchical nature of team dynamics and engagement mediated by perceptions of relevance of the rotation. The hierarchical nature of team dynamics reflected the reinforcement of the rules of rank and ‘who to respect’; it contained three subthemes including ‘rules of the game’, positioning and questioning order. Engagement mediated by perceptions of relevance of the rotation concerned the finding that active participation and attentiveness during rounds varied by home discipline.
Conclusions
We were able to identify representations of the hidden curriculum during observations on a tertiary care paediatric CTU. Interest appears to be a determinant in student level of engagement and observed hierarchies have the potential to impact this engagement either positively or negatively.
Keywords: Clinical teaching units, Hidden curriculum, Hierarchy
All physicians in training are educated in the knowledge, skills and attitudes for medical practice via the formal curricula delivered at undergraduate and postgraduate levels. However, the informal and hidden curricula also exert influence on learners throughout their training.
The informal curriculum consists of unscripted, ad hoc and interpersonal forms of teaching and learning that take place among faculty and students (1). The informal curriculum should not necessarily imply a negative connotation, as positive interactions can occur in these settings.
The hidden curriculum, in contrast, is a set of influences that function at the level of organizational structure and culture (1), essentially representing what an institution teaches without intending to, or being aware it is taught (2).
Learning associated with the hidden curriculum can have negative consequences on trainee educational development, including loss of idealism, adoption of a ‘ritualized’ professional identity, emotional neutralization, change of ethical integrity, acceptance of hierarchy, learning less formal aspects of ‘good doctoring’ (2,3) and decline in moral reasoning (4). Hafferty and Franks (1) hypothesize that conflicts between the formal and hidden curricula may contribute to these negative consequences. The need to investigate and address the hidden curriculum has been emphasized by the medical community (5–9).
Qualitative and ethnographic studies have proven to be effective approaches in examining the informal and hidden curriculum (10). Martimianakis et al. have encouraged discipline-specific examination of the hidden curriculum to help set a research agenda for pursuing evidence-based educational and health practice in relation to issues of the hidden curriculum and humanism (11). As compared to the classroom setting, the hidden curriculum is not as well studied in applied learning contexts. In one such study examining paediatric ward rounds, Balmer and colleagues (12–14) performed ethnographic observations of rounds. They examined what they termed the ‘implicit curriculum’ and examined clinical learning on ward rounds and specifically how the learning mapped to the Accreditation Council for Graduate Medical Education (ACGME) competencies. The hidden curriculum, however, was not explicitly examined.
Thus, the goal of our study was to examine how aspects of the hidden curriculum were enacted during ward rounds on a tertiary care general paediatrics clinical teaching unit (CTU).
METHODS
Design
This study was formally reviewed and approved by The Children’s Hospital of Eastern Ontario (CHEO) Institutional Research Ethics Board.
Our qualitative, exploratory study was informed by an ethnographic approach that was used to describe and interpret learning related to the hidden curriculum. As such, we examined the observable and learned patterns (15) of a convenience sample of physicians and trainees as they conducted daily rounds on an inpatient CTU. Fieldwork included participant observations that focused primarily on interactions between our key informants: attending physicians and physicians in training (i.e., medical students and residents). Other members of the interdisciplinary team, including nurses and pharmacists, would participate in rounds periodically but were not consistently present during group interactions.
Participants
Attending physicians were invited to participate in the study via an e-mail message distributed to faculty in the Division of General Pediatrics at the University of Ottawa. Following their agreement to participate, we approached the trainees on their respective teams. Written, informed consent was obtained from all team members prior to fieldwork commencement. Patients and their families were informed about the study via a written script delivered to each patient and their family prior to rounds commencing.
Setting
The field site for this study was an inpatient general paediatrics CTU at CHEO. CHEO is a 167-bed tertiary care paediatric hospital associated with the University of Ottawa. The University of Ottawa offers a 4-year undergraduate medicine program in either English or French. The core paediatrics rotation for medical students is a 6-week mandatory rotation during the clerkship year of undergraduate medical training. The academic year for medical students runs from September to August and for residents runs from July to June.
Residents from general paediatrics and other specialty programs such as family medicine also complete rotations on the paediatric wards. These rotations are 1 month in duration.
Typically, rounds occur in the hallway outside of patient rooms. The Division of General Paediatrics adheres to a philosophy of patient and family centred rounds (16). As such, the parents and/or patient are invited to participate in rounds while the CTU team discusses their case in the hallway outside of the patient room. The team member assigned to the patient (typically a medical student or R1) presents the case to the team and summarizes the plan for the patient. The trainee may then be asked questions or for clarification by the senior resident or attending staff. Family members are then asked if they have any questions and have understood the medical plan.
Data collection
Data collection occurred in two phases, and different observers were used for the first and second phase of data collection. In the first phase, we performed descriptive observations using field notes and diagrams with no a priori assumptions regarding interactions pertinent to the hidden curriculum. These observations were completed by a research assistant with experience in medical education. This data, as well as a review of the literature and expert opinion, informed the development of a structured observation field guide that was used in the second phase of data collection. The observational field guide was piloted by two team members with qualitative experience, to refine the tool and establish consistent observational procedures. The remainder of the second phase of observation was conducted by the research assistant using the field guide. The field guide was structured to document the following elements: type of participants; location and context of interactions; descriptive notes of directly observable behaviors including body language, group positioning, quotes and tones and reflective notes to capture any inferences made by the researcher. Reflective notes were frequently completed at the end of the observation session to collect the observer’s emergent perceptions and insights. Data collection and analysis were concurrent and data collection was ended when saturation was reached. This was determined when no new ideas or patterns emerged.
In both phases of data collection, the researcher-observers had no prior relationships with the study participants, remained separate from the group during rounds aside from initial introductions, and were not in a position of authority in comparison to the participants. The researcher-observers did not assume an active role as participants and it is not anticipated that their backgrounds influenced the study results. Additionally, they were instructed to make note of instances where they felt their presence influenced group dynamics and document evidence of possible Hawthorne effect in their field notes.
Data analysis
Observational data was first synthesized by the observer, during which time raw field notes, observational field guides and reflective notes were compiled into a cohesive, descriptive, summary of each observation day. Following this step, data were analyzed via an iterative process, using thematic analysis. This involved reading and rereading of observational data to identify themes in the data, clustering of themes, interpretation of content and structure of themes and development of coding schemes. Two members of the research team familiar with the topic area and trained in qualitative research methods independently reviewed the descriptive summaries, observations and diagrams collected in the field. This involved reading, memoing, grouping and organizing the data to inform initial codes. They met to discuss their interpretations of the data and initial codes, and to develop a coding scheme to apply to the data set. This preliminary phase of coding informed more complex thematic generation.
The entire research team, including physicians, nonphysician clinicians and nonclinicians then assembled to discuss and review the preliminary coding. Areas of incongruence in interpretations were examined and debated until consensus was reached on the coding scheme, themes and definitions. The data set was then reclassified with attention paid to recurrent themes. See Table 1 for a description of how the key determinants of trustworthiness of qualitative studies (17–20) (credibility, transferability, dependability and confirmability) were addressed in our study.
Table 1.
Methods employed in our study to address the key determinants of trustworthiness of qualitative data
| Determinant | Method of addressing determinant in our study |
|---|---|
| Credibility | Enhanced using investigator triangulation, and by comparing observation data collected by two independent observers and analyzed by two research team members. Credibility was also strengthened through peer review. Preliminary results were presented at a local medical education conference as a way of soliciting peer review. Feedback from the audience of healthcare professionals with expertise in medical education indicated that the concepts identified were relevant, and that issues described in this study were common to other settings. |
| Transferability | Enhanced using rich descriptions, allowing the reader to judge the reliability of the data and interpretation of findings and the extent to which these findings can be transferred to other settings. |
| Dependability | Enhanced through the maintenance of a detailed audit trail comprising raw data, logs, and field notes; data reduction memos and analysis notes; and process notes. |
| Confirmability | Enhanced through the maintenance of an audit trail of coding decisions and data analysis procedures, as well as copies of evolving coding schemes. |
RESULTS
Twenty-two hours of observation (14 hours in Phase 1, 8 hours in Phase 2) of 11 sets of CTU rounds were performed. Phase 1 occurred in April to May 2012 and Phase 2 in April to May 2014. April to May was considered a time of year when trainees would have been quite experienced in the basic process of rounding on inpatients; i.e., for medical students, the timing of the study would have coincided to be halfway through their clerkship. Rounds typically occurred between 9:00 am and noon and length of rounds ranged between 100 and 200 minutes. Parents or caregivers participated in rounds in the majority of cases.
Teams were most commonly comprised of one staff attending physician (S) one senior 3rd year resident (R3), several 1st year residents (R1) and 3rd year medical students (MS3). R1s could either be paediatric residents or residents from other disciplines rotating on the paediatrics ward. Nurses were present and participated in rounds during approximately half of the observations. Attending staff did not always round on a daily basis with the CTU team. Only rarely would rounds occur in the absence of both the attending staff and R3. All attending staff were practicing general paediatricians and none had further subspecialty training. No examples of possible Hawthorne effect were documented in the field notes.
Two major themes emerged regarding the enactment of the hidden curriculum: 1) the hierarchical nature of team dynamics and 2) engagement as mediated by perceptions of relevance of the rotation.
The hierarchical nature of team dynamics
The existing rank among participants (MS3s, R1-3s, S) was readily observable during rounds. This hierarchy manifested in many ways including an awareness of the ‘rules’ of when and who to pay attention to, physical positioning of participants, and questioning order.
‘Rules of the game’
We noted whether active engagement was or was not noted when certain team members were speaking. Active engagement was observed through the use of reinforcing and mimicking body language, including nods of agreement, eye contact with the speaker and note taking. Junior team members (MS3s and R1s) appeared more engaged and attentive when the R3s or attendings were presenting a case. In contrast MS3s would only sometimes give full attention to R1s, and R1s only rarely gave their full attention to MS3s.
Positioning of participants during rounds
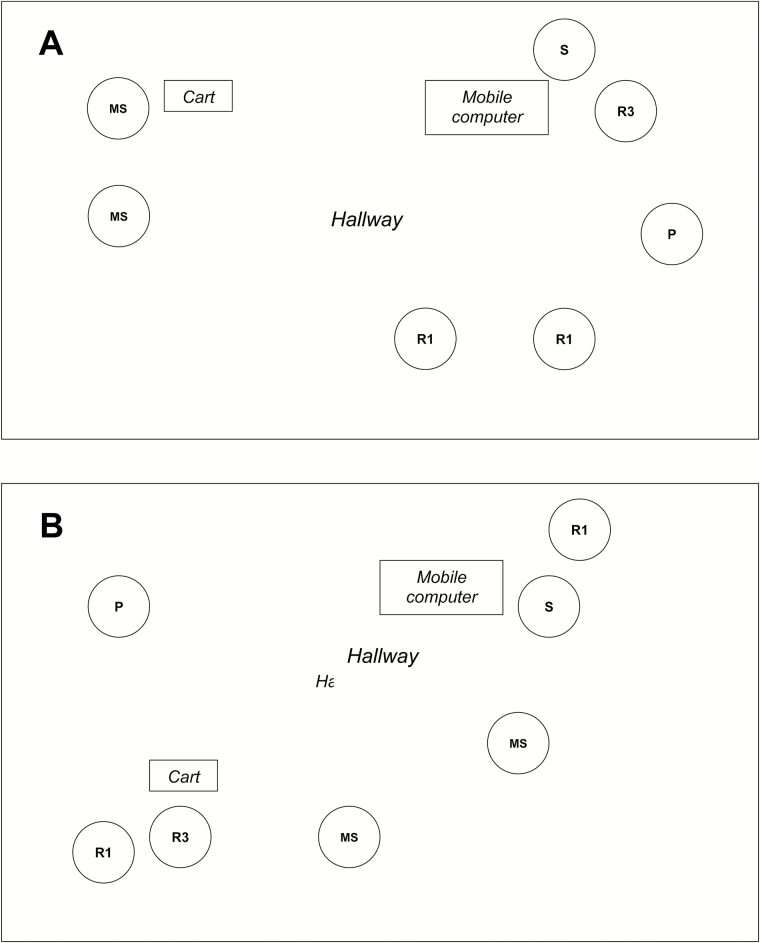
Physical positioning during rounds also reinforced participants’ hierarchical position within the team. This included elements such as physical proximity to one another, to the mobile computer, and to the most senior member of the team. Physical positioning remained fairly consistent throughout rounds, irrespective of the location of rounds (hallway versus bedside). Attending staff and R3s tended to be physically distanced from the more junior trainees. We used the analogy of the attending staff and/or R3s as ‘planets’ with the R1s and MS3s in varying degrees of orbit (Figure 1A and 1B). Sometimes the R3 and attending would be positioned together as a ‘single planet’ (Figure 1A); at other times, they would be separated as ‘double planets’, each with their own trainees in orbit around them (Figure 1B). Often, MS3s would be the most separated physically from the entire team with the R1s standing closer to the attending and R3 (Figure 1A and 1B). A notable exception to this separation was when the attending staff and R3 were both absent; in these cases, the participants were in close proximity to one another.
Figure 1.
Positioning of team members during rounds. (A) ‘Single planet model’ with trainees in orbit around senior team members and (B) ‘Double planet model’ with senior resident and attending acting as separate ‘planets’ with trainees in orbit. S, staff; R3, Senior Resident; R1, First year resident; MS, medical student; P, parent.
Questioning order
During rounds, attendings and R3s posed questions broadly to the team. There was a discernable order imposed when questions were asked, starting with the most senior member of the team (apart from the R3) and, if unanswered, deferring to the other trainees in order of rank. When a question was posed to the group it was, for example, extremely uncommon for MS3s to offer an answer before residents had the opportunity to reply to the question. Though the order was never explicitly set, this pattern was consistent across rounding groups and appeared to be a learned behavior of trainees.
It was also noted that MS3s actively competed to answer questions if no residents were present, but did not do this if residents were present. Direct questioning of trainees appeared to only occur in the situation where the R3 was doing the questioning, and in this case they would often direct questions to individual MS3s, but not to R1s.
Engagement as mediated by perceptions of relevance of the rotation
The level of engagement and attention of R1s appeared to be dependent on home discipline. For example, R1s whose home program was general paediatrics often participated most in rounds discussions. They were also the most likely team members to assume a leadership position when the R3s and attendings were absent from rounds. Equally, the R1s from other disciplines often appeared less attentive and engaged during rounds.
There appeared to be a perception of a lower rank of nonpaediatric R1s on the team, as evidenced by the fact MS3s and R1s would rarely give their full attention to non-paediatric residents when said trainees were presenting a case.
DISCUSSION
One of our key themes was the hierarchical nature of team dynamics. Literature has shown that paediatric team members acknowledge that expected roles exist (14). Our study adds to this by identifying hierarchies within these roles. The hierarchical structure of medicine has been described in previous studies of the hidden curriculum (21–23). Gaufberg et al. (24) have emphasized that hierarchy in medicine is complicated by the fact that expected behaviors in medicine are rarely made explicit, and that the accountability of superiors is not always defined. Our study findings underscore the effect hierarchies have in the clinical teaching setting. In particular, we found that trainees preferentially direct their attention to certain individuals while directing less attention to others. The hierarchical nature of the team extended to the positioning of trainees during rounds, with the staff attending and R3s being physically distanced from the other more junior trainees. These findings have implications for teaching. Ideally one would like to construct an open and interactive teaching environment; the hierarchical nature of the paediatric team structure may represent a barrier to achieving this.
Although questioning (or ‘pimping’) in medicine has been discussed previously in the literature (25–31), our unique study finding concerned exactly how teaching and in particular, questioning occurred on rounds by the attendings or R3s. We found a clear hierarchy of questioning was observable. Another interesting aspect noted is how MS3s will actively compete to answer questions if no residents are present, but will not do this if residents are present. Clearly, the students have learned the implicit rules of when to speak up during rounds and when to remain quiet.
We observed differential engagement with the learning process depending on a resident’s home discipline and this has not been previously described in the literature. While paediatric residents appear to be very engaged in learning on rounds, nonpaediatric residents would often appear less engaged. The reasons for this remain unclear. We theorize that some residents may filter what they are learning though a preconceived notion of relevance to them, namely that they may be chiefly concerned with learning directly applicable to their home discipline and less engaged with learning that is perceived as less pertinent. Another possible explanation relates to team dynamics and the perceived lower rank of nonpaediatric trainees on the team. Finally, nonpaediatric trainees may be less engaged because they feel less comfortable with the subject matter. These possibilities would need to be further examined with interviews and focus groups to obtain the perspective of these trainees.
One strength of our study was our diverse team and the use of a collaborative approach to data analysis. Although there was a time gap between when Phases 1 and 2 of the study were performed, there was no significant change in how rounds were conducted in the two phases of data collection. Other potential limitations of the study include that data was collected at a single site, the fact that a convenience sample was used, and data authenticity. As mentioned, we attempted to minimize the Hawthorne effect by having the observers note any occurrences when they felt that their presence influenced group dynamics, interactions or behaviors. Study team members also discussed the observation data to determine whether they seemed authentic; of note, no data were discarded as a result of these team-debriefing discussions.
However, the presence of family members may also have affected the nature of the interactions observed. Certainly, family members’ presence may affect how various team members engage with one another, and the patterns observed in our study may not necessarily be seen in other specialties that do not use this family centred approach. For example, it is conceivable that team members were polite and present in their interactions with one another due to the presence of family members. As such, our findings may be uniquely generalizable to specialties who incorporate a similar family centred approach.
As such, the exploratory utility of these findings can be used to enhance further research at different centres and in different specialties.
CONCLUSIONS
We were able to demonstrate specific aspects of the hidden curriculum during observations on a tertiary care paediatric CTU. Interest appears to be a key determinant in student level of engagement and observed hierarchies have the potential to impact this engagement either positively or negatively. As a result, it may be advisable to address issues pertaining to the hidden curriculum during teaching on rounds in order to ensure optimal engagement of all trainees. Further qualitative studies could be performed to further expand upon the perception trainees have in the rounds process and how it links to clinical learning.
Acknowledgments
The authors would like to thank Ms. Kathy Day and Ms. Francine Hart for their help in the data collection, as well as Dr. Stephanie Sutherland for her help in the conceptualization of the study.
Funding Source: This study was supported by a grant from the Department of Innovation in Medical Education, University of Ottawa, Ottawa, Ontario, Canada.
Ethical Approval: Research Ethics Board, Children’s Hospital of Eastern Ontario
References
- 1. Hafferty FW, Franks R. The hidden curriculum, ethics teaching, and the structure of medical education. Acad Med 1994;69(11):861–71. [DOI] [PubMed] [Google Scholar]
- 2. Lempp H, Seale C. The hidden curriculum in undergraduate medical education: Qualitative study of medical students’ perceptions of teaching. BMJ 2004;329(7469):770–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Griffith CH, Wilson JF. The loss of student idealism in the 3rd-year clinical clerkships. Eval Health Prof 2001;24(1):61–71. [DOI] [PubMed] [Google Scholar]
- 4. Patenaude J, Niyonsenga T, Fafard D. Changes in students’ moral development during medical school: A cohort study. CMAJ 2003;168(7):840–4. [PMC free article] [PubMed] [Google Scholar]
- 5. Doja A, Horsley T, Sampson M. Productivity in medical education research: An examination of countries of origin. BMC Med Educ 2014;14:243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Marinker M. Myth, paradox and the hidden curriculum. Med Educ 1997;31(4):293–8. [DOI] [PubMed] [Google Scholar]
- 7. Reisman AB. Outing the hidden curriculum. Hastings Cent Rep 2006;36(4):9. [DOI] [PubMed] [Google Scholar]
- 8. Tekian A. Must the hidden curriculum be the “black box” for unspoken truth?Med Educ 2009;43(9):822–3. [DOI] [PubMed] [Google Scholar]
- 9. MacLeod A. The hidden curriculum: Is it time to re-consider the concept?Med Teach 2014;36(6):539–40. [DOI] [PubMed] [Google Scholar]
- 10. Stern DT. Practicing what we preach? An analysis of the curriculum of values in medical education. Am J Med 1998;104 (6):569–75. [DOI] [PubMed] [Google Scholar]
- 11. Martimianakis MAT, Michalec B, Lam J, Cartmill C, Taylor JS, Hafferty FW. Humanism, the hidden curriculum, and educational reform: A scoping review and thematic analysis. Acad Med 2015;90(11 Suppl):S5–13. [DOI] [PubMed] [Google Scholar]
- 12. Balmer DF, Richards BF, Giardino AP. “Just be respectful of the primary doc”: Teaching mutual respect as a dimension of teamwork in general pediatrics. Acad Pediatr 2010;10(6):372–5. [DOI] [PubMed] [Google Scholar]
- 13. Balmer DF, Giardino AP, Richards BF. The dance between attending physicians and senior residents as teachers and supervisors. Pediatrics 2012;129(5):910–5. [DOI] [PubMed] [Google Scholar]
- 14. Balmer DF, Master CL, Richards BF, Serwint JR, Giardino AP. An ethnographic study of attending rounds in general paediatrics: Understanding the ritual. Med Educ 2010;44(11):1105–16. [DOI] [PubMed] [Google Scholar]
- 15. Creswell JW. Qualitative Inquiry and Research Design. 3rd edition. Thousand Oaks, CA: SAGE Publications, 2007. (cited March 29, 2016]. Available from: https://uk.sagepub.com/en-gb/eur/qualitative-inquiry-and-research-design/book235677. [Google Scholar]
- 16. Muething SE, Kotagal UR, Schoettker PJ, Gonzalez del Rey J, DeWitt TG. Family-centered bedside rounds: A new approach to patient care and teaching. Pediatrics 2007;119(4): 829–32. [DOI] [PubMed] [Google Scholar]
- 17. Lincoln YS, Guba EG.. Naturalistic Inquiry. New York: SAGE, 1985. [Google Scholar]
- 18. Krefting L. Rigor in qualitative research: The assessment of trustworthiness. Am J Occup Ther 1991;45(3):214–22. [DOI] [PubMed] [Google Scholar]
- 19. Barbour RS. Checklists for improving rigour in qualitative research: A case of the tail wagging the dog?BMJ 2001;322(7294): 1115–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Horsburgh D. Evaluation of qualitative research. J Clin Nurs 2003;12(2):307–12. [DOI] [PubMed] [Google Scholar]
- 21. Bould MD, Sutherland S, Sydor DT, Naik V, Friedman Z. Residents’ reluctance to challenge negative hierarchy in the operating room: A qualitative study. Can J Anaesth 2015;62(6):576–86. [DOI] [PubMed] [Google Scholar]
- 22. Basabe N, Ros M. Cultural dimensions and social behavior correlates : Individualism-collectivism and power distance. Int J Psychol 2005;18(1):189–225. [Google Scholar]
- 23. Freytag J. Barriers that define a genre of shared decision making in palliative care communication. J Commun Healthc 2012;5(2):140–6. [Google Scholar]
- 24. Gaufberg EH, Batalden M, Sands R, Bell SK. The hidden curriculum: What can we learn from third-year medical student narrative reflections?Acad Med 2010;85(11):1709–16. [DOI] [PubMed] [Google Scholar]
- 25. Wear D, Kokinova M, Keck-McNulty C, Aultman J. Pimping: Perspectives of 4th year medical students. Teach Learn Med 2005;17(2):184–91. [DOI] [PubMed] [Google Scholar]
- 26. Kost A, Chen FM. Socrates was not a pimp. Acad Med 2015;90(1):20–4. [DOI] [PubMed] [Google Scholar]
- 27. Healy JM, Yoo PS. In defense of “Pimping.” J Surg Educ 2015;72(1):176–7. [DOI] [PubMed] [Google Scholar]
- 28. Brancati FL. The art of pimping. JAMA 1989;262(1):89. [PubMed] [Google Scholar]
- 29. Detsky AS. The art of pimping. JAMA 2009;301(13):1379–81. [DOI] [PubMed] [Google Scholar]
- 30. Reifler DR. The pedagogy of pimping educational rigor or mistreatment?JAMA 2016;314(22):2355–6. [DOI] [PubMed] [Google Scholar]
- 31. McCarthy CP, McEvoy JW. Pimping in medical education lacking evidence and under threat. JAMA 2015;314(22):2347. [DOI] [PubMed] [Google Scholar]