Abstract
Objectives:
Antidepressant use increases as age rises. Moreover, older patients are more sensitive to side effects and drug interactions. This descriptive study aims to map antidepressant use among patients at the geriatrics department of a university hospital and to evaluate whether prescribing happens in an evidence-based manner.
Methods:
Patients aged 75 years and over, admitted to the geriatrics department of the Middelheim Hospital in Antwerp between February and July 2017 were included. We checked whether they took antidepressants, which types and doses were prescribed, who prescribed the antidepressants, and whether prescribing was in concordance with the revised STOPP (Screening Tool of Older People’s Prescriptions) criteria.
Results:
Out of the 239 included patients, 61 were found to use antidepressants, with depression being the most important indication. General practitioners appeared to be the most frequent prescribers. Trazodone was the most prescribed antidepressant and was often used for sleeping disorders. Antidepressants were taken longer than recommended in almost one out of five cases. Patients with diabetes and renal insufficiency were prescribed antidepressants less frequently. Only 2.8% of the study participants were prescribed antidepressants for anxiety disorders.
Conclusion:
We can conclude that prescription of antidepressants in older patients at the geriatrics department is often not evidence based. Clear guidelines may offer a solution; therefore more studies are needed on antidepressant use in older patients.
Keywords: antidepressants, elderly, polypharmacy, revised Screening Tool of Older People’s Prescriptions criteria
Introduction
The use of antidepressants increases with age. Figures obtained through Farmanet, the pharmaceutical database of the ‘Rijksinstituut voor Ziekte- en Invaliditeitsverzekering’ (RIZIV) (National Sickness and Invalidity Insurance Institute), show that in 2016 in Belgium, 22.8% of older people aged 75 years and over received a refundable antidepressant at least once compared with 10.8% of the total population. Previous studies showed that these figures are even higher in hospitalized older patients (25%), and increase to 40% in institutionalized older people.1,2 Nevertheless, these patients are more sensitive to side effects and drug interactions, given the frequent comorbidities they suffer, and related polypharmacy, defined as the chronic use of five or more drugs.3,4 Therefore, it is even more important to prescribe antidepressants only following the specific indications and to take the correct treatment duration into account when treating older people.5
In addition to the use of antidepressants rising with age, the number of patients with polypharmacy also increases in the older age categories. Figures from 2016 obtained through Farmanet show the chronic (at least 3 months) use of at least five different drugs in 24.2% of older people aged 75 years and over in Belgium. Importantly, this percentage is only 5.6 in the total population. Polypharmacy increases the risk of drug interactions and side effects, and is often associated with reduced autonomy to perform the ‘activities of daily living’ (ADL), an increased risk of cognitive decline, and an increasing incidence of geriatric syndromes, such as delirium, falls and urinary incontinence.4 Several instruments have already been developed to detect the potentially inappropriate use of drugs in older people, both implicit (based on clinical judgment) and explicit (based on criteria).6 An example of the latter are the STOPP (Screening Tool of Older People’s Prescriptions)/START (Screening Tool to Alert to Right Treatment) criteria, developed in 2008 by O’Mahony and coworkers, with a revised version published in 2015.7 This screening tool contains a list of 80 STOPP and 34 START criteria. Several studies have already shown that the use of these criteria in the context of a more extensive evaluation leads to a higher quality of drug prescriptions, resulting in a reduction of the number of falls, episodes of delirium, duration of hospitalization, number of visits to general practitioners/emergency departments and drug costs.8
Antidepressants are among the top 10 most frequently prescribed drugs in patients with polypharmacy.9 This descriptive study aims to map antidepressant use among patients hospitalized at the geriatric department of a university hospital, and to evaluate whether prescription happens in an evidence-based manner, taking into account the revised STOPP criteria.7
Methods
Study design, setting and study population
This descriptive, retrospective study took place in the Middelheim Hospital in Antwerp, part of the ‘Ziekenhuis Netwerk Antwerpen’ (ZNA) (Hospital Network Antwerp) group. The geriatric services at ZNA are brought together as the University Center of Geriatrics (UCG). Files of all patients aged 75 years or older, hospitalized on ward ‘6D’ (one of the three wards of the acute geriatrics department) between February 2017 and July 2017 were screened for inclusion in this study. The first author was the treating physician of all screened patients. Exclusion criteria were a hospital stay of less than 5 days and a palliative setting.
Measurements and measuring instruments
For each patient, it was determined whether he or she took antidepressant drugs. If so, the type and dosage was documented, as well as the prescribing physician.
Using the revised STOPP criteria,7 we determined whether or not these drugs were prescribed in an evidence-based manner.
Section A of the STOPP criteria (drug indication criteria) was used to check whether the medication was prescribed for the correct indication. The first STOPP criterion of this section is: ‘Any drug prescribed without an evidence-based clinical indication’. Four scientifically based indications for the use of antidepressants in older people were defined: depression, anxiety and panic disorder, neuropathic pain and behavioral disorders in dementia (although current evidence is limited in the latter). All other indications were considered invalid due to lack of a scientific basis, although sometimes very commonly used to prescribe antidepressant drugs. If no clear indication could be found, this was classified under ‘no indication’. The second STOPP criterion of section A is: ‘Any drug prescribed beyond the recommended duration, where treatment duration is well defined’. Guidelines are available on the duration of treatment with antidepressant drugs in older people: for a first episode of depression, a treatment duration of at least 1 to a maximum of 2 years is recommended.10 For patients with recurrent depression or a very severe episode, a lifetime treatment is recommended.10 No specific guidelines are available concerning treatment duration of anxiety disorders in an older population. The general guidelines recommend at least 1 to a maximum of 2 years of treatment for a first episode, and a lifetime treatment for recurrent episodes.11,12 For neuropathic pain, behavioral disorders in dementia, and other, nonevidence-based indications of antidepressant use, no guidelines on treatment duration are available.
Finally, section D (central nervous system criteria) mentions three STOPP criteria specifically concerning antidepressants: ‘Tricyclic antidepressants with dementia, narrow angle glaucoma, cardiac conduction abnormalities, prostatism, or prior history of urinary retention’, ‘Initiation of tricyclic antidepressants as first-line antidepressant treatment’ and ‘Selective serotonin re-uptake inhibitors (SSRI’s) with current or recent significant hyponatraemia i.e. serum Na+ <130 mmol/l’. The use of antidepressants in our study participants was also tested against these three criteria.
Data collection
We used the medication list at admission (as mentioned in the hospitalization report) to determine whether or not patients were currently on antidepressant drugs, and if so, what type and which dosage. The electronic patient file was screened to identify the prescriber, the indication and the duration of taking the antidepressant drug. If this information could not be retrieved, the general practitioner was contacted. For the STOPP criteria from section D, the above-mentioned comorbidities and the sodium level on admission were looked up in the electronic patient file. Furthermore, we included the following variables: age, sex, origin (home, service flat, residential care center, other hospital, transfer from intensive care), cognitive status (mini-mental state examination, MMSE),13 ADL (Katz scale),14 and total number of chronic drugs. The items of the Charlson Comorbidity Index15 were used as comorbidities, with the exclusion of AIDS, because this is less relevant in a geriatric population. These were documented together with the comorbidities that have a specific contraindication for the use of tricyclic antidepressants (TCAs), according to the STOPP criteria.
Statistics
The characteristics of the total study population and the subgroups (using antidepressants versus not using antidepressants) were presented as frequencies (number, %) for the categorical variables, and as the median for the continuous variables. Comparison of the characteristics between the two subgroups was done according to Fisher’s exact test for the categorical variables, and according to the Mann–Whitney U test for the continuous variables. A p value less than 0.05 was considered statistically significant. For the description of antidepressant use within the group of patients taking antidepressants, frequencies were used. The median was used only for the doses of the antidepressants. To compare the classes of antidepressants versus the prescribers, the indications versus the prescribers, the duration of treatment versus the prescribers and the indications versus the classes of antidepressants, we used the Fisher Freeman Halton test. Again, a p value of less than 0.05 was considered statistically significant. For the statistical processing of the results, IBM SPSS Statistics (version 24) was used.
Results
Between February 2017 and July 2017, 263 patients (⩾75 years) were admitted to ward 6D at ZNA Middelheim Hospital. Of these, 239 patients met the inclusion criteria; 19 patients were not included due to a hospital stay less than 5 days, and five due to a palliative setting. Sixty-one (25.5%) of the 239 patients used antidepressants. Table 1 gives an overview of the characteristics of the total study population and the two subgroups (intake antidepressants/no intake antidepressants). Compared with the group not taking antidepressants, patients taking antidepressants were more likely to be women and to use a larger number of chronic drugs. Fewer patients had diabetes mellitus and moderate to severe renal insufficiency compared with patients with no antidepressant drug use.
Table 1.
Characteristics of the study population.
|
Total
(N = 239) |
No intake antidepressants
(N = 178) |
Intake antidepressants
(N = 61) |
p value | |
|---|---|---|---|---|
|
Age in years
Median (min–max) |
85 (75–101) | 85.5 (75–101) | 84 (75–97) | 0.125‡ |
|
Sex
N (%) | ||||
| Male | 80 (33.5) | 67 (37.6) | 13 (21.3) | 0.027 § |
| Female | 159 (66.5) | 111 (62.4) | 48 (78.7) | |
|
Number of medications
Median (min–max) |
8 (1–22) | 7 (1–20) | 10 (3–22) | <0.001 ‡ |
|
Length of hospital stay in days
Median (min–max) |
15 (5–104) | 15 (5–104) | 16 (5–43) | 0.973‡ |
|
MMSE*
Median (min–max) |
24 (0–30) | 25 (0–30) | 23 (0–30) | 0.294‡ |
|
Origin
N (%) | ||||
| Residential care center | 59 (24.7) | 42 (23.6) | 17 (27.9) | 0.640§ |
| Service flat | 13 (5.4) | 11 (6.2) | 2 (3.3) | |
| Home | 158 (66.1) | 118 (66.3) | 40 (65.6) | |
| Other hospital, geriatric department | 2 (0.8) | 2 (1.1) | 0 (0) | |
| Other hospital, revalidation department | 3 (1.3) | 3 (1.7) | 0 (0) | |
| ICU | 4 (1.7) | 2 (1.1) | 2 (3.3) | |
|
ADL$
N (%) | ||||
| O | 68 (28.5) | 57 (32.2) | 11 (18) | 0.025 § |
| A | 47 (19.7) | 29 (16.4) | 18 (29.5) | |
| B | 19 (7.9) | 15 (8.5) | 4 (6.6) | |
| C | 6 (2.5) | 4 (2.3) | 2 (3.3) | |
| Cd | 36 (15.1) | 31 (17.5) | 5 (8.2) | |
| D | 62 (25.9) | 41 (23.2) | 21 (34.4) | |
|
Comorbidities
N (%) |
||||
| Cardiovascular disease | 129 (54) | 95 (53.4) | 34 (55.7) | 0.768§ |
| Chronic obstructive pulmonary disease | 34 (14.2) | 26 (14.6) | 8 (13.1) | 0.835§ |
| Conjunctive tissue disease | 18 (7.5) | 13 (7.3) | 5 (8.2) | 0.784§ |
| Peptic ulcer disease | 27 (11.3) | 22 (12.4) | 5 (8.2) | 0.485§ |
| Diabetes mellitus | 56 (23.4) | 48 (27) | 8 (13.1) | 0.035 § |
| Moderate or severe renal disease | 57 (23.8) | 49 (27.5) | 8 (13.1) | 0.024 § |
| Malignancy | 42 (17.6) | 34 (19.1) | 8 (13.1) | 0.335§ |
| Liver disease | 4 (1.7) | 3 (1.7) | 1 (1.6) | 1.000§ |
ADL (Katz scale): O: physically completely independent and not demented; A: physically dependent for bathing or dressing; B: physically dependent for washing and dressing; and for transferring or toileting; C: physically dependent for washing and dressing, for transferring and toileting; and for feeding or because of incontinence; D: diagnosis of dementia (based on specialist report); Cd: diagnosis of dementia, and dependent for bathing and dressing, and dependent because of incontinence; and dependent for transferring or toileting or eating.
N = 216, 23 missing data.
N = 238, 1 missing data.
Mann–Whitney U test.
Fisher’s exact test.
ADL, activities of daily living; MMSE, mini-mental state examination.
Bold text represents statistically significant results, defined as a p value < 0.05
Within the study population taking antidepressants, antidepressants directly affecting the neuroreceptors are prescribed most, with trazodone being the most commonly prescribed drug in this class. Table 2 provides a further overview of the prescribed classes of antidepressants, type of products and doses.
Table 2.
Prescribed classes of antidepressants, type of products and doses.
| Antidepressant classes and type of products | N (%) |
Dose in mg
Median (min–max) |
|---|---|---|
| SSRI | 18 (25.4) | |
| Paroxetine | 1 (5.6) | 20 |
| Sertraline | 6 (33.3) | 50 (25–100) |
| Citalopram | 2 (11.1) | 20 |
| Escitalopram | 9 (50) | 10 (5–20) |
| TCA | 15 (21.1) | |
| Amitriptyline | 8 (53.3) | 25 (10–75) |
| Melitracen | 7 (46.7) | 10 (10–20) |
| SNRI | 11 (15.5) | |
| Duloxetine | 3 (27.3) | 60 |
| Venlafaxine | 8 (72.7) | 75 (75–150) |
| Antidepressants directly affecting the neuroreceptors | 27 (38) | |
| Mirtazapine | 9 (33.3) | 15 (7.5–30) |
| Trazodon | 18 (66.7) | 100 (25–200) |
SNRI, serotonin and noradrenalin reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant.
General practitioners (GPs) appear to be the most frequent (43.7%) prescribers of antidepressants, followed by geriatricians (14.1%), neurologists (11.3%) and psychiatrists (8.5%). The prescriber was unknown in 22.5% of cases.
Figure 1 shows the different indications for which antidepressant drugs were prescribed. The main indication remained depression (56.3%), with sleeping disorders (12.7%) in second place. In 8.5% of the cases no clear indication was documented.
Figure 1.
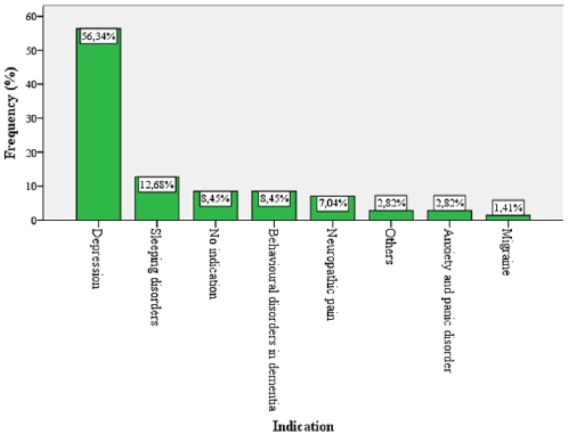
Indication of antidepressant drugs.
Furthermore, it was determined whether the antidepressants in our study population were prescribed according to the current guidelines, using the revised STOPP criteria. These results can be found in Table 3. More than 25% of the patients took antidepressant drugs for a nonevidence-based indication (also taking into account whether the right type of antidepressant drug was prescribed for the correct indication). Almost one in five patients in the study population were taking the antidepressant drugs longer than recommended according to the current guidelines. In a third of the cases, there were no clear guidelines on the duration of treatment. Also, 80% of patients taking TCA drugs took this as a first-choice preparation, so without taking other classes of antidepressants before.
Table 3.
Application of the STOPP criteria (second version) on antidepressant use.
| STOPP criterion | N (%) |
|---|---|
| Incorrect indication | 18 (25.4) |
| Incorrect treatment duration | |
| Longer than guideline | 12 (16.9) |
| No guideline | 24 (33.8) |
| Unknown treatment duration | 9 (12.7) |
| Contraindication SSRI if Na+ <130 meq/liter | 1 (5.6) |
| Contraindication TCA | |
| TCA as first-choice preparation | 12 (80) |
| Dementia | 2 (13) |
| Cardiac conduction disorders | 1 (6.7) |
SSRI, selective serotonin reuptake inhibitor; STOPP, Screening Tool of Older People’s Prescriptions; TCA, tricyclic antidepressant.
Table 4 shows that there is no significant difference between the different prescribers with regard to the class of prescribed antidepressant drugs. There is, however, a difference when we look at the indications for which the antidepressant drugs were prescribed. More specifically, GPs and psychiatrists mainly prescribe antidepressants in the context of depression (74.2% and 100%, respectively), while geriatricians mainly do this to treat sleeping disorders (40%) and behavioral disorders in dementia (30%).
Table 4.
Prescriber versus antidepressant classes/indication/treatment duration.
| Prescriber | ||||||
|---|---|---|---|---|---|---|
|
General practitioner
N (%) |
Geriatrician
N (%) |
Psychiatrist
N (%) |
Neurologist
N (%) |
Unknown
N (%) |
||
|
AD
Classes |
SSRI | 8 (25.8) | 0 (0) | 3 (50) | 1 (12.5) | 6 (37.5) |
| TCA | 9 (29) | 1 (10) | 1 (16.7) | 1 (12.5) | 3 (18.8) | |
| SNRI | 4 (12.9) | 1 (10) | 0 (0) | 4 (50) | 2 (12.5) | |
| AD directly affecting NR | 10 (32.3) | 8 (80) | 2 (33.2) | 2 (25) | 5 (31.3) | |
| Indication | Depression | 23 (74.2) | 1 (10) | 6 (100) | 4 (50) | 6 (37.5) |
| Anxiety and panic disorder | 1 (3.2) | 0 (0) | 0 (0) | 1 (12.5) | 0 (0) | |
| Neuropathic pain | 1 (3.2) | 2 (20) | 0 (0) | 1 (12.5) | 1 (6.3) | |
| Behavioral disorders in dementia | 1 (3.2) | 3 (30) | 0 (0) | 1 (12.5) | 1 (6.3) | |
| Migraine | 0 (0) | 0 (0) | 0 (0) | 1 (12.5) | 0 (0) | |
| Sleeping disorders | 3 (9.7) | 4 (40) | 0 (0) | 0 (0) | 2 (12.5) | |
| Others | 2 (6.5) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| No indication | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 6 (37.5) | |
| Treatment duration | According guideline | 12 (38.7) | 1 (10) | 6 (100) | 4 (50) | 3 (18.8) |
| Longer than guideline | 12 (38.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Unknown | 0 (0) | 0 (0) | 0 (0) | 1 (12.5) | 8 (50) | |
| No guideline | 7 (22.6) | 9 (90) | 0 (0) | 3 (37.5) | 5 (31.3) | |
Prescriber versus antidepressant classes: p = 0.118, Fisher Freeman Halton test; prescriber versus antidepressant indication: p < 0.001, Fisher Freeman Halton test; prescriber versus treatment duration: p < 0.001, Fisher Freeman Halton test.
AD, antidepressant; NR, neuroreceptor; SNRI, serotonin and noradrenalin reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant.
Table 4 also shows that there is a significant difference between the different prescribers and whether or not the correct treatment duration is respected. For example, GPs seem to prescribe antidepressant drugs for a longer period of time than is recommended following the current guidelines.
Finally, Table 5 shows that there is a significant difference between the different classes of antidepressant drugs and the indications for which they are prescribed. All classes were found to be prescribed most frequently for depression, especially the selective serotonin reuptake inhibitors (SSRIs) (83.3%). The TCAs were also often used (26.7%) for neuropathic pain. The antidepressant drugs directly affecting the neuroreceptors were frequently prescribed for indications other than depression. If we make a further dissection within this group, as shown in Table 6, we see that especially trazodone is prescribed for these other indications, like sleeping disorders (50%) and behavioral disorders in dementia (33.3%). Mirtazapine is prescribed predominantly in the context of depression (88.9%).
Table 5.
Indication versus antidepressant classes.
| Indication | Antidepressant classes | |||
|---|---|---|---|---|
|
SSRI
N (%) |
TCA
N (%) |
SNRI
N (%) |
AD directly affecting NR
N (%) |
|
| Depression | 15 (83.3) | 7 (46.7) | 7 (63.6) | 11 (40.7) |
| Anxiety and panic disorder | 0 (0) | 1 (6.7) | 1 (9.1) | 0 (0) |
| Neuropathic pain | 0 (0) | 4 (26.7) | 1 (9.1) | 0 (0) |
| Behavioral disorders in dementia | 0 (0) | 0 (0) | 0 (0) | 6 (22) |
| Migraine | 0 (0) | 0 (0) | 0 (0) | 1 (3.7) |
| Sleeping disorders | 0 (0) | 0 (0) | 0 (0) | 9 (33.3) |
| Others | 0 (0) | 2 (13.3) | 0 (0) | 0 (0) |
| No indication | 3 (16.7) | 1 (6.7) | 2 (18.2) | 0 (0) |
p < 0.001, Fisher Freeman Halton test.
AD, antidepressant; NR, neurotransmitter; SNRI, serotonin and noradrenalin reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant.
Table 6.
Indication versus antidepressant classes and type of products.
| Indication | AD classes and type of products | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| SSRI | AD directly affecting NR | SNRI | TCA | |||||||
| Sertraline N (%) |
Escitalopram N (%) |
Citalopram N (%) |
Paroxetine N (%) |
Trazodon N (%) |
Mirtazapine N (%) |
Venlafaxine N (%) |
Duloxetine N (%) |
Amitryptiline N (%) |
Melitracen N (%) |
|
| Depression | 6 (100) | 7 (77.8) | 1 (50) | 1 (100) | 3 (16.7) | 8 (88.9) | 6 (75) | 1 (33.3) | 4 (50) | 3 (42.9) |
| Anxiety and panic disorder | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (33.3) | 0 (0) | 1 (14.3) |
|
Neuropathic
pain |
0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (33.3) | 4 (50) | 0 (0) |
| Behavioral disorders in dementia | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 6 (33.3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Migraine | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (11.1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Sleeping disorders | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 9 (50) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Others | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2 (28.6) |
| No indication | 0 (0) | 2 (22.2) | 1 (50) | 0 (0) | 0 (0) | 0 (0) | 2 (25) | 0 (0) | 0 (0) | 1 (14.3) |
AD, antidepressant; NR, neuroreceptor; SNRI, serotonin and noradrenalin reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant.
Discussion
This study confirms that the use of antidepressants in older people is frequent. In our study population, more than 25% of the patients took antidepressant drugs (25.5%). These figures are comparable with those of Farmanet in 2016 (22.8%).
When we apply the revised STOPP criteria to our study population, antidepressants appear to be prescribed for an incorrect indication in more than 25% of the cases. This is probably still an underestimation, given that in this study, ‘depression’ was always considered a correct indication, although treatment with antidepressants is only indicated in cases of major depression and not in the milder cases. Primary sleeping disorders were a frequent indication for the prescription of antidepressants (especially trazodone) in our study population, although this is not an evidence-based indication.16 There is some evidence for the use of trazodone in secondary sleep disorders, for example in sleeping disorders accompanying depression and in reversal of the day/night rhythm in Alzheimer’s disease dementia.17–19 Sleeping disorders in this context were mentioned in our study under ‘depression’ and ‘behavioral disorders in dementia’, respectively. Migraine prophylaxis was also considered as a nonevidence-based indication for the use of (tricyclic) antidepressants because of the availability of multiple safer preparations for this indication.20 All indications that did not fall under the four evidence-based indications (depression, anxiety and panic disorder, neuropathic pain and behavioral disorders in dementia) or the two nonevidence-based indications mentioned above were considered as ‘other indications’. These included, for example, ‘psychosomatic complaints’ and ‘generally unwell being’.
It is remarkable that antidepressants were prescribed for anxiety and panic disorders in only 2.8% of cases, while this is a clear evidence-based indication for prescribing an SSRI or serotonin and noradrenalin reuptake inhibitor (SNRI). Of the two patients in our study treated for this indication, one received duloxetine (SNRI), and one melitracen (TCA, as a combination preparation with flupentixol). The latter is mainly used off label as a sedative drug. Melitracen is under dosed as an antidepressant in this product.21 Previous studies have already shown that older people with anxiety and panic disorders are mainly treated with benzodiazepines (25.3%) instead of antidepressants (3.8%).22
The correct treatment duration was not respected in about 20% of the cases; this means that the drug use was continued longer than recommended. It should be noted that the current guidelines on this subject are based on ‘expert consensus’ and that there are few studies available concerning the discontinuation of antidepressants in older people, which can explain the reluctance of doctors to stop this medication in older patients. However, in patients with dementia in residential care centers, one double-blind and one open-label randomized controlled study on discontinuation of antidepressants were performed, reporting positive results.5 When the decision is made to stop an antidepressant, the current guidelines recommend gradually discontinuing the dose over a period of 4 weeks to prevent withdrawal symptoms and relapse.5
Finally, patients taking TCAs were found to use this as a first-choice preparation in 80% of cases, which should be avoided because of the unfavorable adverse effects compared with, for example, the SSRIs.23 If a TCA is chosen in older people, nortriptyline is preferred because of the lower anticholinergic burden.23 It is however remarkable that in our study population, not nortriptyline but amitriptyline, known for its high anticholinergic burden, was frequently prescribed (i.e. in 53.3% of the patients taking TCAs).
Both the female sex and an increasing number of chronic disorders are risk factors for depression and anxiety disorders in the older population.24 This may explain why in our population, women more often took antidepressants, and that patients taking antidepressants also took a greater number of chronic drugs.
In our study population, patients with diabetes mellitus took antidepressants less often. Importantly, diabetes increases the risk of depression,25 just as depression increases the risk of developing diabetes mellitus type 2.26 Certain antidepressants are also indicated for neuropathic pain in the context of diabetes.27 Perhaps the fear of doctors for inducing weight gain or drug interactions explains this difference. However, studies show that a pharmacological treatment of major depression in patients with diabetes leads to better glycemic control.28
Similar results are found in patients with moderate to severe renal insufficiency. Previous studies have already shown that patients with poorer renal function more often show depressive symptoms, but got antidepressant drugs prescribed less frequently.29 Depression is associated with increased morbidity and mortality in patients with chronic renal insufficiency.30 However, few data are available on the safety and efficacy of antidepressants in severe renal insufficiency, which explains the potential reluctance of clinicians to prescribe this drug.30
The antidepressants directly affecting the neuroreceptors were the most frequently prescribed class of antidepressants in our study population, with trazodone as the most prescribed product (25.4% in total). This corresponds with data from the RIZIV in 2016.31 As mentioned above, it is striking that in half of the cases trazodone is prescribed for primary sleeping disorders, an indication for which little scientific evidence exists.16
In our study population, trazodone is also prescribed for behavioral disorders in dementia in one third of cases, for which only a few small studies have shown a positive effect in very specific indications (sleeping disorders in Alzheimer’s disease, behavioral disorders in frontal dementia).18,19,32 The SSRIs, for which a limited benefit was demonstrated in large studies in this indication, were not prescribed in our study population in this context.33
This may be explained by the fact that trazodone is considered a safer product. However, it must be taken into account that trazodone is a substrate of cytochrome P450, which can lead to drug interactions, and it can cause orthostatism in older patients.32 Heart rhythm disorders and priapism are also documented as rare side effects.32
GPs are the most frequent prescribers of antidepressants in our study population. In about 75% of cases they prescribed these drugs in the context of depression. The most frequently prescribed classes of antidepressants by GPs are the antidepressants directly affecting the neuroreceptors (32%), TCAs (29%) and SSRIs (25.8%). In almost 40% of cases, they prescribed antidepressants for a longer period of time than is recommended according to current guidelines.
The above data show that clear guidelines on antidepressant use in older people, especially aimed at primary care, are essential. Efforts have already been made on this subject: recently, a guideline on the management of depression in adults was published by Domus Medica, containing an important section on depression in older patients.34 However, only the treatment of depression was discussed, and not the other indications, for which GPs prescribe antidepressant drugs (25% of the cases in our study). Moreover, nothing is mentioned about the recommended duration of treatment. In order to be able to provide clear guidelines, further studies are certainly needed on antidepressant use in older people, mainly concerning the use in sleeping disorders and behavioral disorders in dementia, and concerning the correct treatment duration of depressive episodes.
To our knowledge, this is the first study to identify antidepressant use by the over 75s admitted to the geriatrics department of a university hospital and to compare them with the revised STOPP criteria. A strength of the study is that we used the electronic patient file and direct contact with the GP combined to collect the correct information about the indication, the prescriber and the duration of the medication.
On the other hand, a limitation of our study is that the population includes a small group of patients from one hospital, which means that the data may not be generalized. However, several findings (prevalence of antidepressant use in older people, trazodone as the most frequently used antidepressant), as indicated before, correspond with recent figures from the RIZIV.31 As already mentioned, on the basis of the available data, no distinction could be made between mild, moderate and major depression as the indication. Nor could it be verified whether the diagnosis was correct. A multicenter study, including more patients, but using the same approach, is essential.
In this study, we specifically assessed the prescribing of antidepressants against the STOPP criteria. However, a similar approach to other medications that are frequently prescribed in older patients with polypharmacy might be useful as well. For example, specific STOPP criteria are available for the 10 most frequently prescribed drug classes in Belgium among older patients with polypharmacy (e.g. proton pump inhibitors, statins, β blockers).7,9 Additionally, general criteria regarding the indication and the treatment duration could also be applied.
Conclusion
This descriptive retrospective study shows that antidepressant use in an older population is frequent, but that prescription of antidepressants in older patients is often not evidence based. For example, older people are often treated too long with antidepressants, and these medications are often prescribed for off-label indications such as sleeping disorders, without much scientific evidence. However, there appears to be too great a reluctance to prescribe antidepressants in some comorbidities and indications. Therefore more studies are essential to describe antidepressant use in older patients, with the goal of formulating clear guidelines.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: The authors declare that there is no conflict of interest.
Contributor Information
Lynn Gers, Department of Geriatric Medicine, University of Antwerp, Antwerp, Belgium.
Mirko Petrovic, Department of Geriatric Medicine, University Hospital Ghent, Ghent, Belgium.
Stany Perkisas, Department of Geriatric Medicine, University of Antwerp, Antwerp, Belgium.
Maurits Vandewoude, Department of Geriatric Medicine, University of Antwerp, ZNA Sint-Elisabeth, Leopoldstraat 26, Antwerp, Antwerp 2000, Belgium.
References
- 1. Vander Stichele R, Van de Voorde C, Elseviers M, et al. Geneesmiddelengebruik in de Belgische rusthuizen en rust- en verzorgingstehuizen. KCE Report 47A, Federaal Kenniscentrum voor de Gezondheidszorg, Brussel, 2006. [Google Scholar]
- 2. Pavon JM, Zhao YZ, McConnell E, et al. Identifying risk of readmission in hospitalized elderly adults through inpatient medication exposure. JAGS 2014; 62: 1116–1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Petrovic M, De Paepe P, Van Bortel L. Pharmacotherapy of depression in old age. Acta Clin Belg 2005; 60: 150–156. [DOI] [PubMed] [Google Scholar]
- 4. Löffler C, Drewelow E, Paschka SD, et al. Optimizing polypharmacy among elderly hospital patients witch chronic diseases - study protocol of the cluster randomized controlled POLITE-RCT trail. Implement Sci 2014; 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kok FM, Reynolds CF. Management of depression in older adults. JAMA 2017; 317: 2114–2122. [DOI] [PubMed] [Google Scholar]
- 6. Kaufmann CP. Inappropriate prescribing: a systematic overview of published assessment tools. Eur J Clin Pharmacol 2014; 70: 1–11. [DOI] [PubMed] [Google Scholar]
- 7. O’Mahony D, O’Sullivan D, Byrne S, et al. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing 2015; 44: 213–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hill-Taylor B, Walsh KA, Stewart S, et al. Effectiveness of STOPP/START (Screening tool of Older Persons’ potentially inappropriate Prescriptions/Screening tool to Alert doctors to the Right Treatment) criteria: systematic review and meta-analysis of randomised controlled studies. J Clin Pharm Ther 2016; 41: 158–169. [DOI] [PubMed] [Google Scholar]
- 9. De Cock J. Polyfarmacie bij ouderen. Website RIZIV, http://www.riziv.fgov.be/nl/publicaties/Paginas/infospot-polyfarmacie.aspx#.WWC6eI9OKUk (2014, accessed 8 July 2017).
- 10. Buchanan D, Tourigny-Rivard MF, Cappeliez P, et al. National guidelines for senior’s mental health: the assessment and treatment of depression. Can J Geriatrics 2006; 9: S52–S58. [Google Scholar]
- 11. Katzman MA, Bleau P, Blier P, et al. Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and OCD. BMC Psychiatry 2014; 14: S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bystriststsky A. Pharmacotherapy for generalized anxiety disorders in adults, http://www.uptodate.com/contents/pharmacotherapy-for-generalized-anxiety-disorder-in-adults?source:search_results&search=anxiety+disorder&selectedTitle=2%7E150#H303453001 (2016, accessed 8 September 2016).
- 13. Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental State.’ A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12: 189–198. [DOI] [PubMed] [Google Scholar]
- 14. Katz S, Ford AB, Moskowitz RW, et al. Studies of Illness in the aged: the Index of ADL: a standardized measure of biological and psychosocial function. JAMA 1963; 185: 914–919. [DOI] [PubMed] [Google Scholar]
- 15. Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–383. [DOI] [PubMed] [Google Scholar]
- 16. Fagiolini A, Comandini A, Catena Dell’Osso M, et al. Rediscovering trazodone for the treatment of major depressive disorder. CNS Drugs 2012; 26: 1033–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nierenberg AA, Alder LA, Peselow E, et al. Trazodone for antidepressant-associated insomnia. Am J Psychiatry 1994; 151: 1069–1072. [DOI] [PubMed] [Google Scholar]
- 18. Grippe TC, Gonçalves BS, Louzada LL, et al. Circadian rhythm in Alzheimer disease after trazodone use. Chronobiol Int 2015; 32: 1311–1314. [DOI] [PubMed] [Google Scholar]
- 19. Camargos EF, Louzada LL, Quintas JL, et al. Trazodone improves sleep parameters in Alzheimer disease patients: a randomized, double-blind, and placebo-controlled study. Am J Geriatr Psychiatry 2014; 22: 1565–1574. [DOI] [PubMed] [Google Scholar]
- 20. Haan J, Hollander J, Ferrari MD. Migraine in the elderly: a review. Cephalalgia 2006; 27: 97–106. [DOI] [PubMed] [Google Scholar]
- 21. Belgisch Centrum voor Farmacotherapeutische Informatie. Gecommentarieerd geneesmiddelenrepertorium, www.bcfi.be (2017, accessed 18 November 2017).
- 22. Cassidy KL, Rector NA. The silent geriatric giant: anxiety disorders in late life. Geriatr Aging 2008; 11: 150–156. [Google Scholar]
- 23. Wiese BS. Geriatric depression: the use of antidepressants in the elderly. BD Med J 2001; 53: 341–347. [Google Scholar]
- 24. Vink D, Aartsen MJ, Schoevers RA. Risk factors for anxiety and depression in the elderly: a review. J Affect Disord 2008; 106: 29–44. [DOI] [PubMed] [Google Scholar]
- 25. Anderson RJ, Freedland KE, Clouse RE, et al. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care 2001; 24: 1069–1078. [DOI] [PubMed] [Google Scholar]
- 26. Rotella F, Mannucci E. Depression is a risk factor for diabetes: a meta-analysis of longitudinal studies. J Clin Psychiatry 2013; 74: 31–37. [DOI] [PubMed] [Google Scholar]
- 27. Haslam C, Nurmikko T. Pharmacological treatment of neuropathic pain in older persons. Clin Interv Aging 2008; 3: 111–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Brieler JA, Lustman PJ, Scherrer JF, et al. Antidepressant medication use and glycaemic control in co-morbid type 2 diabetes and depression. Fam Pract 2016; 33: 30–36. [DOI] [PubMed] [Google Scholar]
- 29. Fischer MJ, Xie D, Jordan N, et al. Factors associated with depressive symptoms and use of antidepressant medications among participants in the chronic renal insufficiency cohort (CRIC) and Hispanic-CRIC studies. Am J Kidney Dis 2012; 60: 27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hedayati SS, Yalamanchili V, Finkelstein FO. A practical approach to the treatment of depression in patients with chronic kidney disease and end-stage renal disease. Kidney Int 2012; 81: 247–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. De Cock J. De antidepressiva – Infospot. Website RIZIV, http://www.riziv.fgov.be/nl/publicaties/Paginas/infospot-antidepressiva.aspx#.WV5G9I9OKUk (2014, accessed 7 June 2017).
- 32. Florence L. Behavioral benefits of trazodone are sustained for the long term in frontotemporal dementia. Therapy 2006; 3: 93–96. [Google Scholar]
- 33. Seitz DP, Adunuri N, Gill SS, et al. Antidepressants for agitation and psychosis in dementia. Cochrane Database of Syst Rev 2011; (2). Art. No.: CD008191. doi: 10.1002/14651858.CD008191.pub2. [DOI] [PubMed] [Google Scholar]
- 34. Declercq T, Habraken H, Van Den Ameele H, et al. Richtlijn depressie bij volwassenen. Domus Medica 2016. [Google Scholar]


