Abstract
The effectiveness of annual mailed fecal immunochemical testing (FIT) outreach is highest when return rates are optimized, which is aided by patient reminders. In a pilot patient-randomized controlled trial in two western Washington clinics of the Sea Mar Community Health Centers, we compared the effectiveness of two phone-based approaches to mailed FIT outreach reminders. In fall 2016, patients ages 50–75, due for colorectal cancer screening, and with a visit in the previous year at either of two clinics, were mailed an introductory letter and FIT. Those who did not return the FIT within 3 weeks (N = 427) were randomized to receive either: a) a series of up to 6 automated phone reminders; or b) the combination of automated and live phone reminders (up to 6 in total). The sole outcome was FIT return within 6 months after the FIT mailing. FIT completion rates were similar in the groups assigned to receive automated calls vs automated plus live calls (40% vs 39%; p = 0.89). The effectiveness of FIT reminder mode differed by language preference (p for interaction = 0.03): among Spanish-preferring patients (n = 106), FIT return rates were higher in the automated-only group than to the auto- plus live-call group (62% vs 39%, p = 0.02). Among English-preferring patients, no difference in modes was observed (n = 279, 32% vs 34%, p = 0.74). We observed no added benefit of live reminder calls in a mailed FIT plus automated call reminder program; our findings may inform efforts to efficiently optimize mailed-FIT outreach programs.
ClinicalTrials.gov identifier NCT01742065
Keywords: Colorectal neoplasms, Early detection of cancer, Community health centers, Language
1. Introduction
Colorectal cancer remains one of the most common cancers among adults over age 50, although its incidence has declined in the past decade (Siegel et al., 2017). The declining disease burden is at least partially attributable to effective screening. Annual screening by FIT reduces CRC mortality (Zhang et al., 2017), and the US Multi-Society Task Force on Colorectal Cancer has recommended targeting a ≥60% completion rate for those offered FIT testing (Robertson et al., 2017). Interventions that include directly mailing FIT kits and providing return postage are highly effective at increasing access to screening, and most of these interventions include patient reminders to increase FIT return rates (Davis et al., 2018; Singal et al., 2017).
The Community Preventive Services Task Force has recommended the use of reminders for FIT return (Community Preventive Services Task Force, 2012). Mailed reminders have been demonstrated to improve FIT return rates (e.g., from 48% to 65% in a Veterans Administration study (Lee et al., 2009)), as have automated phone reminders (e.g., from 16% to 23% in Kaiser Permanente patients (Mosen et al., 2010)). In some studies that compared reminder modes, phone reminders have resulted in higher return rates than mail alone (Cha et al., 2011; Vinker et al., 2002). Furthermore, the optimal reminder modes may differ by age, sex, or racial/ethnic background (Albright et al., 2014; Brandzel et al., 2017; Mosen et al., 2010).
We previously reported that patients in the Sea Mar Community Health Centers were about 50% more likely to return their FIT when reminders were provided by live call than by reminder letter (Coronado et al., 2018). We also reported that among patients who preferred to speak Spanish, the combination of automated and live reminder calls resulted in the highest FIT return rate (49%) (Coronado et al., 2018). In that study, because patients in the combined automated plus live reminder call group received a higher number of reminders (up to 6), compared to those in either the automated or live call group alone (up to 3), we designed the current study to test the hypothesis that return rates differed by automated vs a combination of automated and live phone call reminders when the total number of call attempts was held constant (up to 6). In addition, we tested the hypothesis that delivery mode effectiveness differed by language preference (Spanish or English).
2. Methods
Sea Mar Community Health Centers is a community-based health center specializing in serving Latinos in western Washington. Two clinics participated in the pilot study. This patient-randomized controlled trial (RCT) compared the effectiveness of two modes for delivering telephone reminders to patients who had been mailed a FIT kit.
Eligible patients were 50 to 75 years old and due for colorectal cancer screening; i.e., they had not had a colonoscopy in the last 10 years, flexible sigmoidoscopy in the last 5 years, or FIT in the previous year. Patients were excluded if they had a previous colon cancer diagnosis or colectomy.
The introductory letter and FIT kit packets used templates developed for the Strategies and Opportunities to Stop Colorectal Cancer (STOP CRC) program (Coronado et al., 2018). The letters were developed in English and translated into Spanish and Russian. FIT packets contained a single-specimen FIT kit (Polymedco OC FIT-Chek, Polymedco, Inc., Cortlandt Manor, NY), pictorial wordless and written instructions (in English and Spanish), and a postage-paid envelope for returning the kit to the health center's centralized laboratory.
Research and clinic staff developed reminders as previously described (Coronado et al., 2018). A script for the calls was developed in English and translated into Spanish by bilingual staff. Patients who returned their FIT within 3 weeks (n = 3) were not randomized to receive reminder calls. The 3-week interval was consistent with our prior research on mailed FIT outreach programs and based on patient preferences (Thompson et al., 2017). The remaining 427 were stratified by clinic and randomized prior to the first reminder using a computer-generated list (in a 1:1 ratio). The sole outcome was FIT completion within six months after the FIT mailing. Evidence of a resulted FIT was derived from the electronic health record; therefore, any FIT that lacked a result (e.g., due to a processing failure) was not captured. A post-hoc power analysis for this pilot demonstrated that with a sample size of 420 (50% in each treatment group), the minimum detectable odds ratio was 1.74, assuming 80% power and a two-sided alpha of 0.05 (Demidenko, 2007).
All procedures and intervention materials were approved by the institutional review board of Kaiser Permanente Northwest. The study was approved by the Sea Mar Community Health Centers research committee. Informed consent was waived.
Patient characteristics were described overall and by randomization group. In the intention-to-treat analysis, we calculated the percent of patients overall and by language preference who returned a FIT within 6 months from the date of FIT mailing. Differences in percentages of FIT return between randomization groups were tested using chi-squared or Fisher's exact tests. We used logistic regression to test the association between randomization group and FIT return, and we tested the interaction between randomization group and language preference among those who preferred English or Spanish. The overall and language-specific odds ratios (OR) and 95% confidence intervals (CI) were calculated. Per-protocol analyses excluded randomized patients who had died, transferred care outside of Sea Mar Community Health Centers, had non-working phone numbers, or could not be reached by phone after 6 attempts (n = 141). The percentages of patients who were reached by automated or live phone call in each arm were calculated. All tests were two-sided; analyses were performed in SAS 9.4 (SAS Institute Inc., Cary, NC).
3. Results
Of the 427 patients randomized to receive either of the two modes of reminder calls, the majority (78%) was 50–64 years old, and 80% had Medicaid or Medicare coverage (Table 1). Nearly one-third of participants were Hispanic, and one-quarter preferred Spanish. Patient characteristics were similar between the two reminder modes (Table 1).
Table 1.
Baseline characteristics of patients and FIT return in the intention-to-treat analysis in Sea Mar Community Health Centers, mean (SD) or n (%).
| Overall N = 427 |
Automated calls only n = 218 |
Automated and live calls n = 209 |
|
|---|---|---|---|
| Age (years) | |||
| Mean (SD) | 59.07 (6.67) | 59.59 (6.82) | 58.53 (6.49) |
| Age | |||
| 50–64 | 334 (78.2) | 166 (76.1) | 168 (80.4) |
| 65–74 | 93 (21.8) | 52 (23.9) | 41 (19.6) |
| Sex | |||
| Male | 198 (46.4) | 96 (44.0) | 102 (48.8) |
| Female | 229 (53.6) | 122 (56.0) | 107 (51.2) |
| Ethnicity | |||
| Hispanic | 135 (31.6) | 66 (30.3) | 69 (33.0) |
| Non-Hispanic | 289 (67.7) | 149 (68.3) | 140 (67.0) |
| Unknown | 3 (0.7) | 3 (1.4) | 0 |
| Preferred language | |||
| English | 279 (65.3) | 148 (67.9) | 131 (62.7) |
| Spanish | 106 (24.8) | 55 (25.2) | 51 (24.4) |
| Other | 42 (9.8) | 15 (6.9) | 27 (12.9) |
| Insurance | |||
| Medicaid or medicare | 342 (80.1) | 174 (79.8) | 168 (80.4) |
| Commercial | 14 (3.3) | 7 (3.2) | 7 (3.3) |
| Other | 71 (16.6) | 37 (17.0) | 34 (16.3) |
| Family income | |||
| <$20,000 | 224 (52.5) | 118 (54.1) | 106 (50.7) |
| $20,000+ | 73 (17.1) | 34 (15.6) | 39 (18.7) |
| Unknown | 130 (30.4) | 66 (30.3) | 64 (30.6) |
| Clinic | |||
| 1 | 186 (43.6) | 98 (45.0) | 88 (42.1) |
| 2 | 241 (56.4) | 120 (55.0) | 121 (57.9) |
| FIT returned | 169 (40%) | 87 (40%) | 82 (39%) |
| English preference | 91 (33%) | 47 (32%) | 44 (34%) |
| Spanish preference | 54 (51%) | 34 (62%) | 20 (39%)⁎ |
| Other language preference | 24 (57%) | 6 (40%) | 18 (67%) |
p for χ2 = 0.02 for reminder group comparison. For all other χ2 or Fisher's exact tests of differences in FIT return, p ≥ 0.12.
In intention-to-treat analyses, 40% of participants returned a FIT within 6 months of their FIT mailing. There was no difference in FIT completion between reminder modes (p = 0.89, Table 1). There was a significant interaction between language preference and reminder mode (p = 0.03): the OR for automated + live calls (vs automated only) was 1.09 (95% CI: 0.66–1.79) for those who preferred English and was 0.40 (95% CI: 0.18–0.87) for those who preferred Spanish (Fig. 1). This difference was driven by a high FIT return rate (62%) for Spanish-speakers in the automated call group, compared to 39% in the automated + live comparison group (Table 1).
Fig. 1.
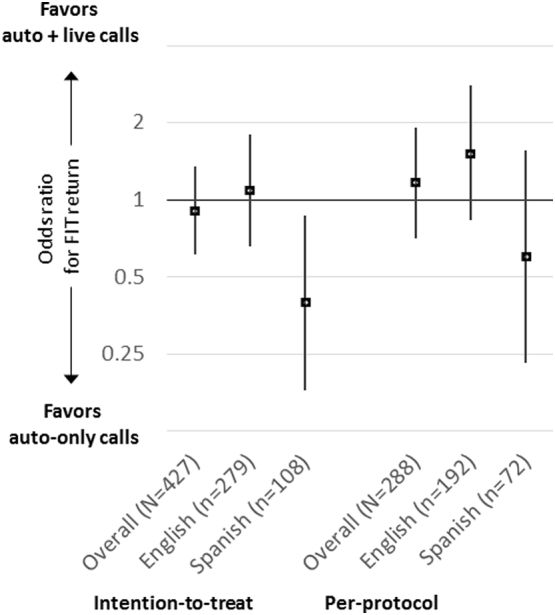
Associations between reminder mode and FIT return, overall and by language preference* in Sea Mar Community Health Centers (odds ratios and 95% confidence intervals).
* For the interaction between language preference (Spanish or English) and reminder mode in the intention-to-treat analysis, p = 0.03. In the per-protocol analysis, p for interaction = 0.11.
In the automated-only arm, 67% of patients were reached. In the automated + live call arm, 67% were reached by either automated or live call: 65% were reached by automated call, 26% were reached by live call, and 24% were reached by both methods.
In the per-protocol analyses, 141 (33%) of participants were excluded, and the pattern of return rates was similar to that in the intention-to-treat analysis (Supplemental Table 1). The interaction between language preference and reminder mode persisted in the same direction (p = 0.11, Fig. 1), with 45% of Spanish-speakers in the automated calls group returning a FIT, compared to 37% in the automated + live group (Supplemental Table 1).
4. Discussion
In this trial comparing two modes of phone reminders in a mailed-FIT outreach program in a community health center, we observed no benefit of combining live phone calls with automated calls over using automated calls alone. The 6-month FIT-return rate was 40%, and the only treatment-group difference was among those who preferred Spanish language. In that group, there was a higher return rate in those assigned to receive automated calls only (62% FIT return rate) than among those assigned to receive the combination of auto + live calls (45%). However, these results should be interpreted cautiously. The number in the Spanish-language group was small (n = 108), and multiple comparisons were tested, leaving room for chance as an explanation. In the per-protocol analysis, which excluded patients who were never reached by the reminder mode to which they were assigned, there were no significant differences in return rate overall or for either language-preference group.
In our previous study of multiple reminder methods for mailed FITs, we reported that modes that included a phone call (automated or live) resulted in higher return rates than a mailed reminder letter did. In that study, Spanish-preferring patients had the highest return rates if they were assigned to the combination of automated and live phone calls (49% vs 25% in the automated call group) (Coronado et al., 2018). However, the total number of calls in the two groups differed: patients in the automated call group received three calls, whereas patients in the combined automated plus live group received up to six calls. Our new findings suggest that when the total number of calls is held constant, the live phone call offered no added benefit.
The limited reach of live calls (26%) was likely a contributor to finding no difference from automated-only calls. The low proportion of patients randomized to receive a live call who actually did receive one was likely a result of competing demands on clinic staff members' time in a busy health center setting. Even if a high reach could have been achieved, this pilot study was not powered to detect odds ratios below 1.74. Although the observed effect sizes in the intention-to-treat analysis were consistently small and not supportive of higher response rates in the auto + live group, it is possible that statistically significant effects with OR < 1.74 would be detectable in a larger study.
Our finding might also suggest that reminders interact with patient characteristics in complex ways to drive FIT return. For example, age, sex, and patient preference may modify the effectiveness of interventions and may have been confounded with patients' language preference in our studies. Studies have shown that older participants prefer phone calls over other reminder modes and that phone-reminder effectiveness might be higher in older patients. Among Kaiser Permanente members, older participants more often requested phone calls regarding screening reminders so that they could ask questions and make follow-up appointments; younger participants chose electronic reminders, such as texts and e-mails (Albright et al., 2014). Moreover, an auto-call was more effective among older than younger patients (Mosen et al., 2010). In a study of phone-delivered colorectal cancer screening messages, African-American patients strongly preferred African-American voices over white and Latina options and suggested that messages include tailored information about the relevance of screening for African Americans (Albright et al., 2014).
Phone reminders after mailed-FIT outreach are effective (Coronado et al., 2018; Mosen et al., 2010; Vinker et al., 2002; Walsh et al., 2010). However, baseline (or control) return rates vary widely, and return rate improvements following phone reminders have been small in some studies, for example, when they followed an educational DVD mailing (Levy et al., 2012) or multiple auto-call and text reminders (Baker et al., 2014). Heterogeneity in the combinations and timing of multi-component reminders prohibits direct comparisons of reminder modes across published studies.
Nevertheless, the effectiveness of reminders overall is not disputed; hence the recommendation for reminders after FIT delivery (Community Preventive Services Task Force, 2012). In addition to effectiveness, costs of implementation are a concern. In a Kaiser Permanente study, automated call reminders raised screening rates by about 6% and increased costs by $3 per patient (Smith et al., 2012). In a VA study, the cost of implementing a high-intensity reminder system (including live calls before and after the FIT mailing) was offset by the savings from fewer wasted FITs (Schlichting et al., 2014). In the current study, automated calls were less expensive than the estimated personnel costs for live calls. However, a precise comparison of costs would require collecting person-time and wage data for training and delivery of calls, costs of the auto-call service, and costs of future FIT kit mailing for non-respondents. Given the similar FIT return rates, automated calls may be optimal for this patient population.
The following is the supplementary data related to this article.
FIT test completion by reminder mode in the per-protocol analysis, n (%).
Conflict of interest statement
Dr. Coronado served as a co-investigator on a study funded by Epigenomics and as a principal investigator on a study funded by Quidel Corporation. The studies had no influence on the design, conduct, or reporting of the present study. All other authors declare that they have no conflict of interest.
Acknowledgments
Research reported in this publication was supported by the National Cancer Institute, Award Number UH3CA188640. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The study sponsor had no role in study design; collection, analysis, and interpretation of data; writing the report; or the decision to submit the report for publication.
References
- Albright K., Richardson T., Kempe K.L., Wallace K. Toward a trustworthy voice: increasing the effectiveness of automated outreach calls to promote colorectal cancer screening among African Americans. Perm. J. 2014;18:33–37. doi: 10.7812/TPP/13-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker D.W., Brown T., Buchanan D.R. Comparative effectiveness of a multifaceted intervention to improve adherence to annual colorectal cancer screening in community health centers: a randomized clinical trial. JAMA Intern. Med. 2014;174:1235–1241. doi: 10.1001/jamainternmed.2014.2352. [DOI] [PubMed] [Google Scholar]
- Brandzel S.D., Bowles E.J.A., Wieneke A. Cancer screening reminders: addressing the spectrum of patient preferences. Perm. J. 2017;21 doi: 10.7812/TPP/17-051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cha J.M., Lee J.I., Joo K.R., Shin H.P., Park J.J. Telephone reminder call in addition to mailing notification improved the acceptance rate of colonoscopy in patients with a positive fecal immunochemical test. Dig. Dis. Sci. 2011;56:3137–3142. doi: 10.1007/s10620-011-1720-0. [DOI] [PubMed] [Google Scholar]
- Community Preventive Services Task Force Updated recommendations for client- and provider-oriented interventions to increase breast, cervical, and colorectal cancer screening. Am. J. Prev. Med. 2012;43:92–96. doi: 10.1016/j.amepre.2012.04.008. [DOI] [PubMed] [Google Scholar]
- Coronado G.D., Rivelli J.S., Fuoco M.J. Effect of reminding patients to complete fecal immunochemical testing: a comparative effectiveness study of automated and live approaches. J. Gen. Intern. Med. 2018;33:72–78. doi: 10.1007/s11606-017-4184-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis M.M., Freeman M., Shannon J. A systematic review of clinic and community intervention to increase fecal testing for colorectal cancer in rural and low-income populations in the United States - how, what and when? BMC Cancer. 2018;18:40. doi: 10.1186/s12885-017-3813-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demidenko E. Sample size determination for logistic regression revisited. Stat. Med. 2007;26:3385–3397. doi: 10.1002/sim.2771. [DOI] [PubMed] [Google Scholar]
- Lee J.K., Reis V., Liu S. Improving fecal occult blood testing compliance using a mailed educational reminder. J. Gen. Intern. Med. 2009;24:1192–1197. doi: 10.1007/s11606-009-1087-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy B.T., Daly J.M., Xu Y., Ely J.W. Mailed fecal immunochemical tests plus educational materials to improve colon cancer screening rates in Iowa Research Network (IRENE) practices. J. Am. Board Fam. Med. 2012;25:73–82. doi: 10.3122/jabfm.2012.01.110055. [DOI] [PubMed] [Google Scholar]
- Mosen D.M., Feldstein A.C., Perrin N. Automated telephone calls improved completion of fecal occult blood testing. Med. Care. 2010;48:604–610. doi: 10.1097/MLR.0b013e3181dbdce7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson D.J., Lee J.K., Boland C.R. Recommendations on fecal immunochemical testing to screen for colorectal neoplasia: a consensus statement by the US multi-society task force on colorectal cancer. Gastroenterology. 2017;152:1217–1237. doi: 10.1053/j.gastro.2016.08.053. [DOI] [PubMed] [Google Scholar]
- Schlichting J.A., Mengeling M.A., Makki N.M. Increasing colorectal cancer screening in an overdue population: participation and cost impacts of adding telephone calls to a FIT mailing program. J. Community Health. 2014;39:239–247. doi: 10.1007/s10900-014-9830-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel R.L., Miller K.D., Fedewa S.A. Colorectal cancer statistics, 2017. CA Cancer J. Clin. 2017;67:177–193. doi: 10.3322/caac.21395. [DOI] [PubMed] [Google Scholar]
- Singal A.G., Gupta S., Skinner C.S. Effect of colonoscopy outreach vs fecal immunochemical test outreach on colorectal cancer screening completion: a randomized clinical trial. JAMA. 2017;318:806–815. doi: 10.1001/jama.2017.11389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith D.H., Feldstein A.C., Perrin N. Automated telephone calls to enhance colorectal cancer screening: economic analysis. Am. J. Manag. Care. 2012;18:691–699. [PMC free article] [PubMed] [Google Scholar]
- Thompson J., Davis M., Michaels L., Rivelli J., Castro M., Escaron A., Younger B., Castillo M., Reich S. Using boot camp translation to design a system-based intervention to improve rates of colon cancer screening using fecal immunochemical testing among Latino patients in community health centers. Cancer Epidemiol. Biomarkers Prev. 2017;27:A13. [Google Scholar]
- Vinker S., Nakar S., Rosenberg E., Kitai E. The role of family physicians in increasing annual fecal occult blood test screening coverage: a prospective intervention study. Isr. Med. Assoc. J. 2002;4:424–425. [PubMed] [Google Scholar]
- Walsh J.M., Salazar R., Nguyen T.T. Healthy colon, healthy life: a novel colorectal cancer screening intervention. Am. J. Prev. Med. 2010;39:1–14. doi: 10.1016/j.amepre.2010.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Cheng Z., Ma Y. Effectiveness of screening modalities in colorectal cancer: a network meta-analysis. Clin. Colorectal Cancer. 2017;16:252–263. doi: 10.1016/j.clcc.2017.03.018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
FIT test completion by reminder mode in the per-protocol analysis, n (%).


