Abstract
Objectives
There is substantial lack of guidance when it comes to the implementation of non-technical skills (NTS) in undergraduate medical education. This review aimed to identify and critically evaluate published literature on learning strategies for NTS in undergraduate medical education and to derive a training framework targeted towards standardizing future training interventions.
Methods
A systematic review of the MEDLINE database was performed using a prospective protocol following PRISMA guidelines. Studies evaluating undergraduate medical students exposed to NTS interventions, which measured subjective or objective outcomes in selected attributes, were included.
Results
Initial systematic search yielded a total of 5079 articles, out of which 68 fulfilled the inclusion criteria. A total of 24 NTS were identified, with communication skills being the most commonly reported skill evaluated (n = 37). A variety of educational tools were used (n = 32), noteworthy being the use of simulated patients. Great heterogeneity was also observed in measured outcomes and methods of assessment. A ‘triad of outcomes’ in NTS training was devised (knowledge, skill performance and attitude towards skills) and used for classification of all reported outcomes. Extracted data were used to design a non-technical skill training framework.
Conclusions
The existing literature describes a plethora of NTS interventions in undergraduate medical education, with varied outcomes and assessments. We hereby propose the ‘NTS Training Framework’, in an attempt to coordinate future research and catalyze the identification of an ideal NTS course structure to form tomorrow's physicians.
Keywords: Non-technical skills, Communication skills, Undergraduate medical education, Framework, Learning
Highlights
-
•
Initial systematic search yielded a total of 5079 articles, out of which 68 fulfilled the inclusion criteria.
-
•
A total of 24 non-technical skills (NTS) were identified, with communication skills being the most commonly reported skill.
-
•
A ‘triad of outcomes’ in NTS training was devised (knowledge, skill performance and attitude towards skills).
-
•
We propose a unified framework for NTS training, with the objective of guiding future research.
1. Introduction
In an era of globalized medicine and increased public pressure for high-quality care, the need to form medical professionals with greater adaptability to social environments is ever-growing. Whilst knowledge and technical skills remain indispensable pillars of medical education, non-technical skills (NTS) training has attracted considerable attention in recent decades [1], aiming to contribute to a more holistic model of medical education. NTS can be defined as a mélange of ‘soft skills’ allowing doctors to self-evolve as part of a ‘learning organization’ capable of adapting in volatile environments [[2], [3], [4]]. Increasing use of the term “soft skills” pertains to a paradigm shift from the medical profession's traditional notions of internalized norms and implicit standards towards a culture of audits, transparency and self-surveillance.
Inspired by its original application in the aviation sector and air safety, NTS training implementation has expanded to many multidisciplinary fields, including healthcare, to prevent adverse outcome related to human factors errors [5,6]. NTS training aspires to resolve healthcare failures precipitated by errors often conceived at the organizational level. For instance, narratives surrounding failures such as the Mid-Staffordshire scandal, revealed conditions that often lay the groundwork for errors, favouring quick fixes and ‘blame games’ over learning and transparency within teams [7,8]. Such systemic ‘defects’ have been the focus of numerous high-impact reports such as ‘To Err is Human’ and ‘A promise to learn–a commitment to act’ [7,9]. Yet preventable harm continues to occur, exacerbating both patient suffering and healthcare costs [10]. Even at the undergraduate level, lack of practice, anxiety and reduced confidence are all factors contributing to students' under performance when interacting with patients or operating within multidisciplinary environments [11]. These shortcomings may be traceable to the lack of a universal NTS training framework, highlighting the need for a unified and focused training approach part of medical school curricula [[12], [13], [14]].
NTS training efforts are the product of two main driving forces. The first, arising in the 1970s and based on the concept of ‘dehumanization’, sustains that medical students become progressively ‘estranged’ and detached from patients throughout their training, leading to compromised patient care - a theory also supported by more recent studies [15,16]. The second relates to the potential of NTS to influence clinical outcomes independently of technical skills [17]. Indeed, studies suggest that NTS, such as effective doctor-patient communication, ensure better health outcomes, patient safety, satisfaction and compliance [18], and decreased patient distress [19]. Equally, doctors benefit from a gratifying work environment and reduced malpractice lawsuits [20,21].
Despite the widely recognized advantages of comprehensive NTS training, research surrounding its implementation remains elusive. Whilst many studies evaluate NTS interventions, at present there are no clear guidelines for implementing NTS learning strategies. With this in mind, we performed a systematic review (SR) to identify and critically evaluate published literature on learning strategies for NTS in undergraduate medical education. Additionally, we outline comprehensive NTS intervention outcomes and derive a NTS training framework targeted for standardizing future training interventions.
2. Methods
We performed a SR following PRISMA guidelines to identify studies evaluating NTS interventions in undergraduate medical education. Studies were hand-searched to find additional papers not included in the initial search.
2.1. Registration
This systematic review has been registered with Research Registry (registration code: reviewregistry608).
2.2. Assessment of methodological quality of the systematic review (AMSTAR 2)
We completed the AMSTAR 2 checklist to assess the quality of our methodology [22].
2.3. Search strategy
The search strategy focused on pooling studies published on the MEDLINE database, including targeted ‘non-technical skills’ intervention strategies. We utilized an extensive list of keywords obtained from MeSH terms pertaining to all qualities and skills-other than technical proficiency-believed to play a role in the development of future doctors; a complete list of all included keywords can be viewed in Appendix 1. This list was compiled following detailed review of key precedent studies [14,23] as well as the General Medical Council's (GMC) “Outcomes for graduates” guidelines, outlining key competencies expected of newly qualified doctors [24].
2.4. Selection criteria
As part of the SR protocol we agreed to a “Population, Intervention, Comparison, Outcome – PICO” strategy (Fig. 1). Inclusion criteria limited selected studies to only those exposing primarily undergraduate medical students or mixed medical with other healthcare students (P, population) to any non-technical skills training approach incorporated within the curriculum of, or offered by, a Medical Institution or any other provider (I, intervention). Included studies were furtherly limited to those measuring perceived or actual changes in attributes such as skills, knowledge or attitudes in randomized or quasi-experimental study designs (C, comparison). Outcomes sought were the objective or perceived improvement in participants' attributes. In borderline cases, study inclusion was made by default. Exclusively qualitative studies, reporting students’ perceptions towards intervention (NTS module) were not considered. Such studies did not seem to affect any of our primary results. We also excluded studies not reporting baseline performance of the subjects, and therefore unable to comment on the impact of the intervention (performance improvement).
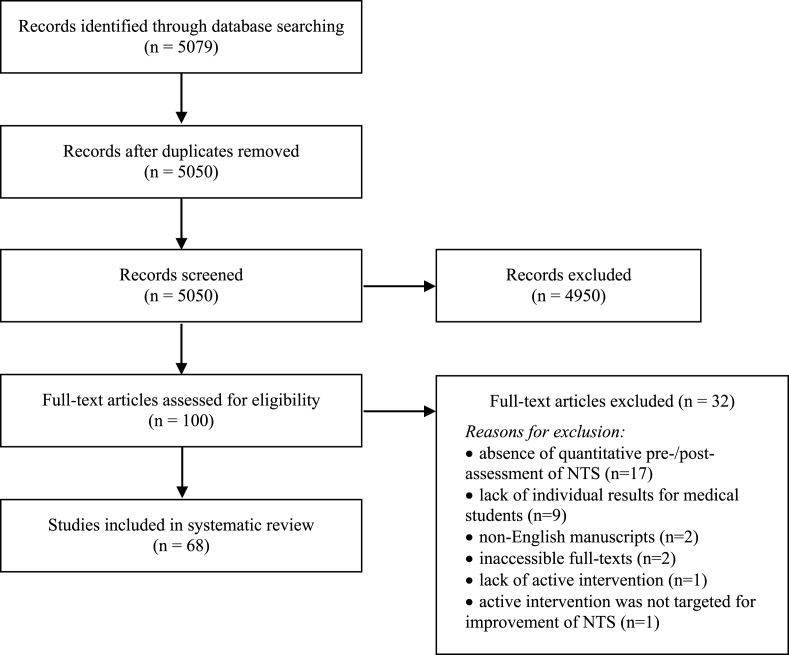
Fig. 1.
PRISMA flow diagram [25].
2.5. Data extraction
To maximize the homogeneity of extracted information from shortlisted studies, we used a pilot, prospectively designed worksheet, structured around the PICO headings. Extracted fields were based on the subheadings as indicated in Table 1. Whenever study location was not provided, the presumed location was the corresponding authors’ affiliation country. A third reviewer (I.T.) was involved in the full-text articles assessment and resolved any disagreement between the two reviewers (M.N., L.C.), cross-checking and confirming the validity of extracted data. Any further disagreement was discussed and dissolved by the senior authors (M.S., A.P.). The final extraction sheet was standardized to provide refined results amenable to more accurate qualitative analysis and subsequent synthesis of results.
Table 1.
PICO data extraction fields.
| PICO Criteria | Extracted fields |
|---|---|
| General | Aim, Year and Location of study |
| Population | Intervention/Control group sizes |
| Demographic details | |
| Tutor/Facilitator background | |
| Recruitment method | |
| Year of study | |
| Intervention/Control | Non-technical skill assessed |
| Educational tool used | |
| Use of simulated patients | |
| Duration of intervention | |
| Outcomes | Attribute assessed |
| Tool of assessment | |
| Conclusion of study | |
| Other | Study limitations |
3. Results
3.1. Selected studies
The initial systematic search yielded a total of 5079 records from MEDLINE. Following removal of duplicates, 5050 records were screened against our inclusion criteria. A total of 100 studies were selected from primary screening, and the full-text articles retrieved for eligibility assessment. A total of 68 studies were eligible for inclusion in our SR. (Fig. 1).
3.2. Study characteristics
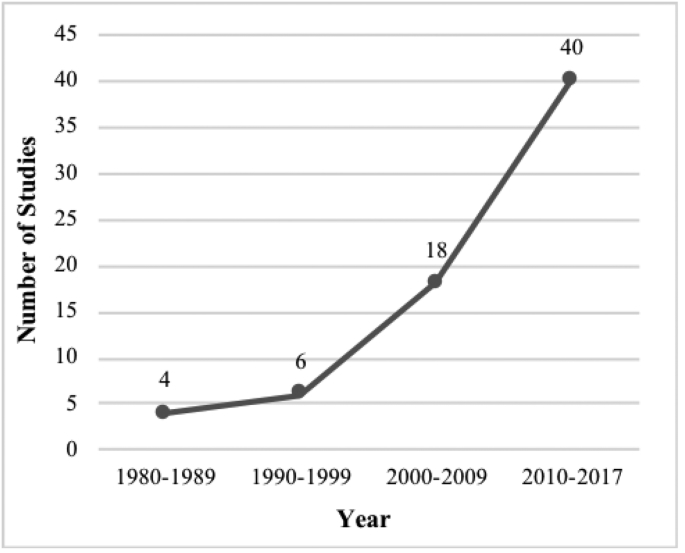
Fig. 2 shows a remarkable increase in the number of studies available per year since 1980, with a striking increase of 122% between periods 2000–2009 and 2010–2017. Most studies were featured in the Americas (n = 25) [[26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50]], followed closely by Europe (n = 24) [[51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74]]. Specifically, the majority were carried out in the United States (US) (n = 23) [[26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48]], whereas the United Kingdom (UK) ranked second with 10 studies [[51], [52], [53], [54], [55], [56], [57], [58], [59], [60]]. Of 68 included studies, 48 reported both qualitative and quantitative measures, whilst the remainder were solely quantitative.
Fig. 2.
Studies assessing NTS interventions, 1980-Present.
3.3. Study population
Study population was homogeneous, with medical students forming the main participant group in selected studies. 11 studies also involved other healthcare students [28,32,34,39,46,47,56,57,62,66,75], with nursing students being the most represented group (n = 7) [28,39,47,56,57,66,75]. As summarized in Table 3, the total sample size ranged from 7 to 373 medical students, with an average of 111 ± 87.1 per study. Two papers were not considered for such average given that participant number was not provided. Indeed, tutors' number and profession were provided by only 24 and 22 studies respectively; both of these factors were considered while designing the ‘NTS Training Framework’.
Table 3.
Summary of interventions in eligible studies.
| Author | Non-technical skill | Length of Intervention | Simulated Patient (SP) used | Sample size (Medical students) | Year groups |
|
|---|---|---|---|---|---|---|
| Pre-clinical (1–2) | Clinical (3–6) | |||||
| Aboumatar et al. [44] | Communication skills Teamwork skills | Short | No | 120 | ✓ | |
| Alroy et al. [79] | Interpersonal skills | Short | No | n/a | ✓ | |
| Ayuob et al. [84] | Communication skills | Short | No | 293 | ✓ | |
| Betson et al. [85] | Breaking bad news | Short | No | 160 | ✓ | |
| Blatt & Greenberg [36] | Teaching skills | Short | No | 103 | ✓ | |
| Communication skills | ||||||
| Feedback-giving skills | ||||||
| Bonnaud-Antignac et al. [72] | Breaking bad news | Long | Yes | 108 | ✓ | |
| Braniff et al. [51] | Communication skills | Long | No | 240 | ✓ | |
| Teaching skills | ||||||
| Understanding the work environment | ||||||
| Teamwork skills | ||||||
| Learning skills | ||||||
| Buczacki et al. [52] | Interprofessional collaboration | Short | No | 331 | ✓ | |
| Cämmerer et al. [70] | Communication skills | Long | Yes | 84 | ✓ | |
| Carpenter [56] | Interprofessional collaboration | Short | No | 23 | ✓ | |
| Carter et al. [31] | Cross-cultural training | Short | No | 196 | ✓ | |
| Chun & Lee [86] | Debating skills | Long | No | 45 | ✓ | |
| Dixon-Woods et al. [60] | Communication skills | Long | No | 173 | ✓ | |
| Doherty et al. [65] | Communication skills | Short | Yes | 127 | ✓ | |
| Efstathiou & Walker [57] | Communication skills | Short | No | 14 | ✓ | |
| Engerer et al. [69] | Communication skills | Short | Yes | 34 | ✓ | |
| Engler et al. [43] | Communication skills | Long | No | 46 | ✓ | |
| Erickson et al. [26] | Communication skills | Short | Yes | 118 | ✓ | |
| Teamwork skills | ||||||
| Fadlon & Pessah [87] | Interviewing skills | Long | No | 56 | ✓ | |
| Empathy skills | ||||||
| Communication skills | ||||||
| Fernández-Olano et al. [62] | Empathy skills | Short | No | 137 | ✓ | |
| Fletcher et al. [58] | Emotional Intelligence | Long | No | 86 | ✓ | |
| Forsgren et al. [61] | Communication skills | Short | Yes | 69 | ✓ | |
| Franco et al. [64] | Communication skills | Short | Yes | 69 | ✓ | |
| Hagemann [68] | Situation awareness | Short | No | 77 | ✓ | |
| Teamwork skills | ||||||
| Task management | ||||||
| Decision-making | ||||||
| Hagemeier et al. [39] | Communication skills | Short | Yes | 73 | ✓ | |
| Haidet et al. [29] | Communication skills | Short | No | 34 | ✓ | |
| Hammer & Rian [48] | Presentation skills | Short | No | 7 | ✓ | ✓ |
| Harlak et al. [88] | Communication skills | Long | No | 59 | ✓ | |
| Heiman et al. [33] | Presentation skills | Long | Yes | 132 | ✓ | |
| Hess et al. [46] | Communication skills | Long | Yes | 67 | ✓ | |
| Hobgood et al. [47] | Teamwork skills | Short | No | 235 | ✓ | |
| Hobgood et al. [47] | Breaking bad news | Short | Yes | 138 | ✓ | |
| Joekes et al. [54] | Communication skills | Long | Yes | 82 | ✓ | |
| Karnieli-Miller et al. [89] | Interpersonal communication skills | Short | Yes | 19 | ✓ | |
| Humor | ||||||
| Knox and Bouchier [53] | Communication skills | Long | Yes | n/a | ✓ | |
| Konopasek et al. [27] | Communication skills | Short | Yes | 90 | ✓ | |
| Feedback-giving skills | ||||||
| Koponen et al. [73] | Communication skills | Long | Yes | 129 | ✓ | |
| Kushner et al. [30] | Empathy skills | Short | Yes | 127 | ✓ | |
| Communication skills | ||||||
| Lanken et al. [34] | Communication skills | Long | No | 370 | ✓ | ✓ |
| Lau et al. [81] | Communication skills | Short | No | 160 | ✓ | |
| Lie et al. [42] | Interpreter interaction skills | Short | No | 304 | ✓ | |
| Lim et al. [83] | Empathy skills | Long | No | 77 | ✓ | |
| Lim et al. [77] | Empathy skills | Short | No | 72 | ✓ | |
| LoSasso et al. [35] | Empathy skills | Short | No | 70 | ✓ | |
| Loureiro et al. [63] | Communication skills | Long | No | 115 | ✓ | |
| Ludwig et al. [38] | Teamwork skills | Short | Yes | 373 | ✓ | |
| Lukman et al. [82] | Communication skills | Long | Yes | 189 | ✓ | |
| Martino et al. [45] | Brief Motivational Interviewing | Short | Yes | 45 | ✓ | |
| Mauksch et al. [32] | Communication skills | Long | No | 22 | ✓ | |
| Moorhead & Winefield [90] | Empathy skills | Short | No | 63 | ✓ | |
| Ozcan et al. [75] | Empathy skills | Short | No | 143 | ✓ | |
| Poole & Sanson-Fisher [78] | Empathy skills | Short | No | 45 | ✓ | |
| Rees & Sheard [55] | Communication skills | Long | Yes | 216 | ✓ | |
| Robertson et al. [28] | Teamwork skills | Short | Yes | 104 | ✓ | |
| Rosen et al. [40] | Cross-cultural training | Short | Yes | 32 | ✓ | |
| Saab et al. [91] | Communication skills | Short | No | 75 | ✓ | |
| Schildmann et al. [66] | Breaking bad news | Short | Yes | 23 | ✓ | |
| Shapiro et al. [50] | Communication skills | Long | Yes | 79 | ✓ | |
| Simmenroth-Nayda et al. [67] | Communication skills | Long | Yes | 32 | ✓ | |
| Tiuraniemi et al. [74] | Communication skills | Short | No | 126 | ✓ | |
| Todisco et al. [76] | Interviewing skills | Long | Yes | 60 | ✓ | |
| Tsai et al. [92] | Interviewing skills | Short | Yes | 27 | ✓ | |
| Usherwood [59] | Interviewing skills | Short | No | 44 | ✓ | |
| von Lengerke & Kursch [71] | Communication skills | Short | Yes | 267 | ✓ | |
| Wiese et al. [41] | Presentation skills | Short | No | 62 | ✓ | |
| Yeung et al. [49] | Teaching skills | Long | No | 18 | ✓ | |
| Communication skills | ||||||
| Yu et al. [93] | Non-verbal communication skills | Short | No | 82 | ✓ | |
| Zgheib et al. [80] | Communication skills | Long | No | 102 | ✓ | |
| Professionalism | ||||||
| Personal Development | ||||||
Variability was observed in the disclosure of further participant demographic information, specifically concerning first language, gender and mean age. Only 24 papers specified whether students had previous experience in NTS learning [26,28,32,35,39,41,44,45,52,55,61,63,64,[67], [68], [69],[74], [75], [76], [77], [78], [79], [80], [81]].
3.4. Intervention
After exploring the learning outcomes of the included studies, we defined an NTS intervention as ‘any teaching strategy aiming to improve an individual's performance, knowledge and attitude towards a non-technical skill’. A total of 24 discrete NTS interventions were identified, with communication and empathy skills being featured a total of 37 and 9 times respectively (Table 3). We described studies as either long or short, based on intervention duration greater than 40 hours (active time) or 12 weeks (total time). When duration was defined in days, we assumed one working day equals to 8 hours. Considering these parameters, we computed an average study duration of 33 ± 94.1 hours and described 25 studies as long (Table 3). Of the 68 studies, 15 did not specify the exact intervention time and were therefore omitted from the aforementioned calculations [30,32,33,38,42,43,50,53,54,57,72,77,82,83]. Courses were either (a) implemented in the medical schools' core curricula and made compulsory to all attending students (n = 46) or (b) optional to internal medical students (n = 22).
As anticipated, a variety of educational tools were utilized (32 in total). Simulated patients (SP) were used in 31 studies and of those, 16 (52%) utilized SP feedback either as an educational tool or as a method of assessment. Didactic lectures, video-assisted learning and role play were recurrently integrated in the courses generating a combination of both traditional (didactic lectures) and non-traditional methods of teaching in most NTS courses. Table 2 summarizes the 16 most commonly used educational tools with corresponding frequency, whilst the remaining (n = 16) were only utilized once each.
Table 2.
Educational tools used with corresponding frequency.
| Educational Tool | Number of times used |
|---|---|
| Didactic lecture | 25 |
| Role play | 25 |
| Video assisted learning | 25 |
| Simulated Patients | 21 |
| Workshop | 21 |
| Feedback | 20 |
| Other | 16 |
| Group discussion | 11 |
| Clinical placement | 9 |
| Seminar | 7 |
| Case Based Learning | 4 |
| E-learning | 4 |
| Audio record feedback | 3 |
| Practical | 2 |
| Problem Based Learning | 2 |
| tOSCE | 2 |
| Tutorial | 2 |
3.5. Learning outcomes
We noted an extensive variation in learning outcomes amongst selected studies, possibly owing to the broad pool of courses, each one assessing different NTS. Inspired by the apparent gap in literature concerning universal NTS outcomes, we devised a ‘triad of outcomes’. This approach encapsulates a step-wise model by which students potentially acquire new NTS, with 1) knowledge of the NTS providing the initial context and scaffolding to the subsequent 2) performance of the NTS, followed by 3) self-reflection on the learning accomplished. Indeed, our ‘triad’ represents three potentially overlapping, albeit distinct, steps which both medical students and educators should focus upon when reflecting on their performance and designing interventions, respectively (Fig. 3). An overlap between assessed outcomes is inevitable as some skills impact various improvement areas.
Fig. 3.
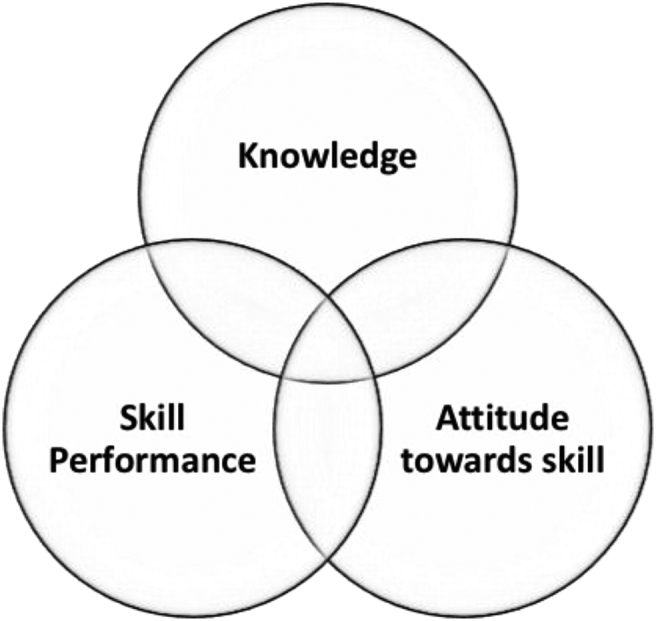
Triad of outcomes in a NTS intervention.
We used the following definitions for classification of the reported triad of outcomes:
-
1.
Knowledge: theoretical understanding of the principles surrounding a specific NTS.
-
2.
Skill performance: quantifiable adeptness in a specific NTS.
-
3.
Attitude towards skill: subjective perception about the usefulness and purpose of a specific NTS.
By qualitatively synthesizing (Table 4) the reported outcomes in accordance with the aforementioned ‘improvement areas’, we were able to deduce some descriptive statistics. For example, skill performance was encountered most frequently, amounting to 60 times, while attitude towards skill and knowledge appeared on 31 and 16 occasions, respectively.
Table 4.
Summary of study outcomes and assessment.
| Author | Outcome |
Assessment |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Skill Performance | Knowledge | Attitude towards skills | Assessment Method 1 | Assessment Method 2 | Assessment Method 3 | Assessment Method 4 | Validated method | Results | |
| Aboumatar et al. [44] | ✓ | ✓ | Likert scale questionnaire | System thinking scale | ✓ | + | |||
| Alroy et al. [79] | ✓ | Rating scale | ✓ | + | |||||
| Ayuob et al. [84] | ✓ | ✓ | Multiple-choice questionnaire | Checklist based assessment | + | ||||
| Betson et al. [85] | ✓ | Likert scale questionnaire | + | ||||||
| Blatt & Greenberg [36] | ✓ | ✓ | ✓ | Learners' rating | Likert scale questionnaire | Interaction analysis data | + | ||
| Bonnaud-Antignac et al. [72] | ✓ | ✓ | Likert scale questionnaire | 6-point protocol | ✓ | + | |||
| Braniff et al. [51] | ✓ | Likert scale questionnaire | + | ||||||
| Buczacki et al. [52] | ✓ | Likert scale questionnaire | + | ||||||
| Cämmerer et al. [70] | ✓ | Likert scale questionnaire | + | ||||||
| Carpenter [56] | ✓ | ✓ | Likert scale questionnaire | + | |||||
| Carter et al. [31] | ✓ | CABSa | + | ||||||
| Chun & Lee [86] | ✓ | Debate Competence Scale | ✓ | + | |||||
| Dixon-Woods et al. [60] | ✓ | ✓ | Likert scale questionnaire | + | |||||
| Doherty et al. [65] | ✓ | ✓ | Likert scale questionnaire | + | |||||
| Efstathiou & Walker [57] | ✓ | ✓ | Likert scale questionnaire | + | |||||
| Engerer et al. [69] | ✓ | Likert scale questionnaire | + | ||||||
| Engler et al. [43] | ✓ | CSICb | ✓ | + | |||||
| Erickson et al. [26] | ✓ | ✓ | SCSc | JSAPNCd | ATHCTe | ✓ | + | ||
| Fadlon & Pessah [87] | ✓ | ✓ | Likert scale questionnaire | Focus groups | + | ||||
| Fernández-Olano et al. [62] | ✓ | JSPEf | ✓ | + | |||||
| Fletcher et al. [58] | ✓ | Bar-On EQ-i | ✓ | + | |||||
| Forsgren et al. [61] | ✓ | ✓ | Likert scale questionnaire | Checklist-based assessment | + | ||||
| Franco et al. [64] | ✓ | ✓ | Multiple-choice questionnaire | CCPQC-CCg | CSASh | Likert scale questionnaire | ✓ | + | |
| Hagemann [68] | ✓ | ✓ | ANTS Observation Systemi | Likert scale questionnaire | ✓ | + | |||
| Hagemeier et al. [39] | ✓ | Likert scale questionnaire | + | ||||||
| Haidet et al. [29] | ✓ | ✓ | Likert scale questionnaire | MAASj | PPOSk | ✓ | + | ||
| Hammer & Rian [48] | ✓ | ✓ | Likert scale questionnaire | + | |||||
| Harlak et al. [88] | ✓ | ✓ | CSASh | Empathic Tendency Scale | ✓ | - | |||
| Heiman et al. [33] | ✓ | Checklist based assessment | + | ||||||
| Hess et al. [46] | ✓ | Common Ground Rating Scale | OSCEl | ✓ | + | ||||
| Hobgood et al. [47] | ✓ | ✓ | ✓ | Teamwork attitudes instrument | Teamwork knowledge test | ✓ | + | ||
| Hobgood et al. [47] | ✓ | ✓ | Likert scale questionnaire | + | |||||
| Joekes et al. [54] | ✓ | ✓ | Doctor-Patient (DP) Scale | Likert scale questionnaire | Interview Rating Scale | OSCEl | ✓ | + | |
| Karnieli-Miller et al. [89] | ✓ | ✓ | Patient–Practitioner Orientation Scale | Lavie Scale | RCSm | ✓ | + | ||
| Knox and Bouchier [53] | ✓ | Modified essay question | + | ||||||
| Konopasek et al. [27] | ✓ | ✓ | Likert scale questionnaire | + | |||||
| Koponen et al. [73] | ✓ | CSASh | ✓ | + | |||||
| Kushner et al. [30] | ✓ | ✓ | Likert scale questionnaire | + | |||||
| Lanken et al. [34] | ✓ | ✓ | ✓ | Likert scale questionnaire | JSPEf | ✓ | + | ||
| Lau et al. [81] | ✓ | Likert scale questionnaire | + | ||||||
| Lie et al. [42] | ✓ | Multiple-choice questionnaire | + | ||||||
| Lim et al. [83] | ✓ | ✓ | JSPEf | OSCEl | ✓ | + | |||
| Lim et al. [77] | ✓ | ✓ | Behaviour Change Counselling Index | ✓ | - | ||||
| LoSasso et al. [35] | ✓ | ✓ | JSPEf | ✓ | + | ||||
| Loureiro et al. [63] | ✓ | ✓ | STAIn | Interpersonal Behaviour Survey | CSASh | ✓ | - | ||
| Ludwig et al. [38] | ✓ | Likert scale questionnaire | + | ||||||
| Lukman et al. [82] | ✓ | ✓ | ✓ | General Information questionnaire | ICIo | CSAMp | CSVAq | ✓ | + |
| Martino et al. [45] | ✓ | ✓ | Likert scale questionnaire | Multiple-choice questionnaire | + | ||||
| Mauksch et al. [32] | ✓ | Likert scale questionnaire | + | ||||||
| Moorhead & Winefield [90] | ✓ | Empathy Rating Scale | - | ||||||
| Ozcan et al. [75] | ✓ | ✓ | ECSSr | Empatic Tendency Scale | ✓ | + | |||
| Poole & Sanson-Fisher [78] | ✓ | Accurate Empathy Scale | ✓ | + | |||||
| Rees & Sheard [55] | ✓ | CSASh | ✓ | - | |||||
| Robertson et al. [28] | ✓ | ✓ | ✓ | Teamwork knowledge test | CHIRP Scales | Team skills checklist video rating | ✓ | + | |
| Rosen et al. [40] | ✓ | ✓ | ✓ | Likert scale questionnaire | + | ||||
| Saab et al. [91] | ✓ | Rating scale | + | ||||||
| Schildmann et al. [66] | ✓ | Likert scale questionnaire | + | ||||||
| Shapiro et al. [50] | ✓ | ✓ | SAICQt | SPIRu | ISRSv | ✓ | - | ||
| Simmenroth-Nayda et al. [67] | ✓ | CCOGw | ✓ | + | |||||
| Tiuraniemi et al. [74] | ✓ | Likert scale questionnaire | Global self-appraisal of competency | + | |||||
| Todisco et al. [76] | ✓ | Likert scale questionnaire | Videotaped interview rating scale | + | |||||
| Tsai et al. [92] | ✓ | Videotaped interview rating scale | + | ||||||
| Usherwood [59] | ✓ | Likert scale questionnaire | + | ||||||
| von Lengerke & Kursch [71] | ✓ | Likert scale questionnaire | + | ||||||
| Wiese et al. [41] | ✓ | Videotaped interview rating scale | + | ||||||
| Yeung et al. [49] | ✓ | Likert scale questionnaire | + | ||||||
| Yu et al. [93] | ✓ | METTx | SETTy | + | |||||
| Zgheib et al. [80] |
✓ |
TPSz |
✓ |
+ |
|||||
| TOTAL | 60 | 16 | 31 | 30 | |||||
Abbreviations: a: Cultural Attitudes and Beliefs Scale, b: Carkhuff's Standard Index of Communication, c: Self-efficacy in Communication Scale, d: Jefferson Scale of Attitudes toward Physician-Nurse Collaboration, e: Attitudes toward Health Care Team, f: Jefferson Scale of Physician Empathy, g:Clinical Communication and Professionalism Questionnaire of Capability – Communication Competencies, h: Communication Skills Attitude Scale, i: Anaesthesia Non-Technical Skills Observation System, j: Mindful Attention Awareness Scale, k: Patient Practitioner Orientation Scale, l: Objective Structured Clinical Examination, m: Relational Communication Scale n: Speilberger's State-Trait Anxiety Inventory, o: Interpersonal Communication Inventory, p: Communication Skills Attitude Measure q: Communication Skills Video Assessment, r: Empathic Communication Skill Scale, s: Collaborative Healthcare Interdisciplinary Relationship Planning, t: Self-Assessment of Interpersonal Competence Questionnaire, u: The Staff-Patient Interaction Rating Scale, v: Interpersonal Skills Rating, Scale, w: Calgary-Cambridge Observation-Guide, x: Micro Expression Training Tool, y: Subtle Expression Training Tool, z: Team Performance Scale.
3.6. Assessment
Our analysis yielded a total of 49 individual methods of assessment (Table 4), which we classified as either objective or subjective. Objective methods of assessment reflect the actual performance (n = 23), whilst subjective methods of assessment reflect the perceived competence of the participant in the relevant skill (n = 26). Of the 68 studies, 53 included a subjective method, either on its own or in conjunction with an objective one. In 30 studies (44%), a validated method of assessment was used, nevertheless many of the remaining studies failed to report whether methods used were validated.
Overall study results after NTS intervention were classified as having either a positive or negative impact on the study population, based upon the provided data and conclusions drawn by the authors (Table 4). Only six papers reported negative findings, with a decline in measured outcomes following the intervention enacted. This may suggest the presence of publication bias towards positive results.
3.7. Limitations of the included studies
Included studies reported several limitations, the most common being the absence of a control group (n = 19). This was followed by a small sample size (n = 16) and the application of the NTS intervention in question to a single institution only (n = 12). Few studies reported on the long-term retention of the intervention undertaken, and this was mentioned as a limitation to 10 studies. Further to this, based on AMSTAR 2 checklist the methodological quality is low, which can be attributed to significant heterogeneity in the studies included.
4. Discussion
The modern shift of patient care to the biopsychosocial approach demands a coincident change in medical education, particularly in non-technical skills teaching [94,95]. This review has compiled substantial evidence supporting early exposure of undergraduate medical students to NTS training. Evaluation of included studies has been complicated by the heterogeneity of reported participant and educator demographics, interventions, outcomes, and their assessment. This underscores the need to unify NTS teaching implementation and reporting. To this effect, we propose a singular NTS teaching framework.
4.1. Parameter 1: Participants and educators
NTS training was compulsory in the majority of studies included, and we suggest it be a mandatory element of medical school curricula (Table 5). Results showed participants were mostly in the clinical years of their studies, however it is unclear whether introduction of NTS training in clinical versus pre-clinical years has particular advantages. Few studies specified students’ socio-demographics and previous experience in NTS, complicating appraisal of the important link between such and NTS acquisition [[96], [97], [98]]. This hinders our efforts to optimize future course designs, particularly if neglected student minorities exist undetected by the current literature. Similarly, the optimum number of students per intervention cannot be established reliably due to: 1) variation in group size dependent on the educational tool used and 2) variation in the student to tutor ratio. Acknowledging these ambiguities, our framework helps overcome them by standardizing the reporting of results such that future studies can be compared more accurately (Table 5).
Table 5.
Parameters of NTS training framework.
| Parameter | Suggestions | |
|---|---|---|
| Course | Participants |
|
| Educators |
|
|
| Intervention |
|
|
| Outcomes |
|
|
| Assessment | Nature |
|
| Methods |
|
|
Educator information is also poorly represented, with most studies failing to provide sufficient analyzable data. Given the pivotal role of educators in NTS training, we propose to alleviate any potential disparities in educators’ backgrounds with a uniform pre-course training (Table 5).
4.2. Parameter 2: Intervention
The vast number of different NTS intervened for in the analyzed studies reinforces our argument to unify training by defining a core set of NTS for the undergraduate curriculum. To accomplish this, we propose a ‘frequency-based’ approach, selecting the most common NTS and training strategies from the existing evidence base. This assumes educational demand has spurred coincidental development of relevant NTS study interventions. For example, the frequent use of communication skills interventions (37 times) may suggest recognition of the importance of this NTS and students' need for improvement in this domain. Indeed, the literature demonstrates a shift away from ‘classic’ areas of intervention previously incorporated in surgical, anesthetic and health education frameworks, towards skills such as empathy and breaking bad news [3,4,99]. Whilst this approach guarantees catering for the current educational needs, it's effectiveness is dependent upon continued monitoring of NTS learning.
Currently, the majority of reported interventions are limited to domain-specific training, focusing on singular aspects of the medical profession such as the operating room (OR) [3,4,100]. This observation highlights a future pathway for NTS training, where movement out of the OR and into surgical wards can be mirrored in other areas of the medical profession [101].
Present educational methods combine traditional and novel training tools. Simulation-Based Learning (SBL) has been implemented in a variety of medical disciplines [102,103], with recent evidence of its role in NTS training [[104], [105], [106], [107], [108], [109]]. Despite its sparse use in the selected studies, evaluating its time advantages and high fidelity, we consider SBL a fundamental part for all future NTS interventions [103,110,111]. Also, we appraise the increasing use of feedback from SP noted in our study. Though a recent review [112] was inconclusive regarding feedbacks’ effectiveness in aiding medical students, it has been suggested that feedback can positively affect communication skills when used in conjunction with other education tools, warranting further investigation [113]. Taking into consideration the above points, we encourage use of simulation in NTS training in conjunction with other widely-accepted traditional or non-traditional methods of teaching (Table 5).
To the best of our knowledge, no existing studies correlate NTS active intervention duration to participant outcomes. However, most authors support a longitudinal model, involving a course extending over weeks or months as opposed to singular timepoints [114,115]. Positive outcomes for participants are generally reported by studies, independently of intervention time or frequency. This may indicate that duration and frequency are not pivotal factors towards the success of NTS training. However, we exercise caution when drawing scheduling suggestions, as our calculation of study duration was based on assumptions (see results), whilst publication bias towards positively-skewed results may also exist. Nonetheless, due to the time constraints pre-existing in medical school curricula, we propose that the ideal NTS intervention duration should verge towards our average of 20–30 hours, distributed longitudinally.
Whilst most studies show NTS training leads to participant learning, retention of skills can degrade over time [43,78,116]. Maintenance of high quality NTS throughout a physician's career has the potential to improve clinical outcomes and care standards; hence, we argue it is vital to periodically revisit NTS throughout undergraduate education. This also addresses the natural decline in students' NTS, including empathy, experienced over the duration of medical school [[117], [118], [119]]. This can be achieved by scheduling regular NTS training over the academic years, building upon previous NTS taught, whilst increasing student proficiency through further, more complex exercises [120].
4.3. Parameter 3: Outcomes
The extensive variation in learning outcomes reported in the reviewed studies constituted a barrier to interpreting the relative impact of the NTS interventions on students. To simplify this, we developed a “triad of outcomes”, unifying measured outcomes in three areas: 1) knowledge, 2) skill performance, 3) attitude towards skill. Whilst this provides some basis for analysis, it is inherently limited in attempting to normalize outcomes disparate as the NTS they refer to. To eliminate this in future studies, we propose the ecumenical utilization of unified outcomes such as our “triad”, on the footsteps of the subdivision of NTS in tools such as the surgeons' NOTSS and anesthetists’ ANTS [2,3].
4.4. Parameter 4: Nature and method of assessment
The commonest rationale for study exclusion in this review was the lack of student assessment before and after the NTS intervention (Fig. 1). Also, many studies failed to utilize a control group not participating in any NTS intervention (n = 50). These limitations denote the inherent complexity of implementing a well-designed and controlled NTS intervention trial to a cohort of medical students. This is chiefly impeded by preexisting time constraints and the educational disadvantage of offering NTS training to only a cohort of students. Hence, variables such as students’ previous exposure to NTS training and to other curricular activities that may contribute to their NTS development cannot be compounded for. To obviate this shortcoming in future studies, we suggest the use of baseline and post-intervention assessments, which can also be “formative” assessments to students [121,122]. We also suggest the use of control groups, which can receive the NTS intervention subsequently, thus also permitting improved tutor to student ratios (Table 5).
Whilst many studies evaluated the same NTS, different assessment methods were often used, complicating the comparison of training effectiveness. To address this, we propose that future studies utilize unified assessment methods. A possible solution is to reaffirm assessment methods already commonly utilized, such as the Communication Skills Attitude Scale and the Jefferson Scale of Physician Empathy [123,124]. Amongst the reviewed studies these tools were the most frequently occurring, suggesting they may be easily extended to all future NTS intervention studies [4]. Importantly, these scales have been extensively validated, demonstrating good test-retest reliability and internal consistency, both in their English and non-English translations [88,[123], [124], [125], [126], [127], [128], [129], [130], [131]]. Likert scales were also utilized by a majority of the included studies. This suggests a second route to implement a common NTS assessment method, mimicking tools such as the NOTSS and the ANTS, grading NTS by Likert scales in key domains [2,3]. Whilst an attractive option, the success of this unifying method is dependent on reaching a consensus on the domains to be included. Moreover, subdivision of NTS into domains could allow assessment through feedback and self-evaluation, methods invaluable to capture the social skills involved in many NTS [4]. Applied to our proposed “triad” of outcomes, attitude towards skill could be best assessed via a subjective scale, such as a Likert scale or one of the validated tools aforementioned, whilst skill performance and knowledge could be measured via more objective tools, including multiple-choice questions, as exemplified by some included studies [42,45,64,84] (Table 5).
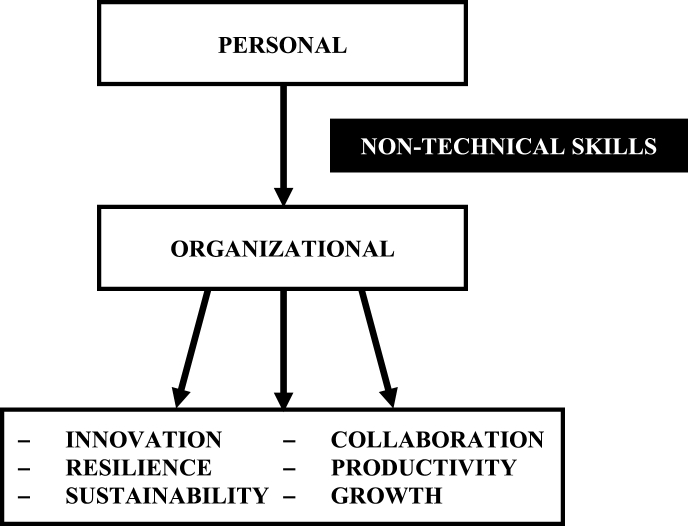
4.5. NTS in the transition from a personal to an organizational level
NTS should be viewed as a catalyst for improving personal competence and performance in multi-disciplinary teams and settings. Such personal gains lead to improved organizational performance and allow the individual to ‘mature’ and form a key prerequisite for organizational gains. We suggest that effective plurality can lead to innovation, resilience, sustainability, collaboration, productivity and growth (Fig. 4) – all key principles of high quality and cost-efficient care. On the basis of evidence from the compiled studies, and considering the damaging repercussions in the absence of such elements, we strongly support the early introduction of NTS training in undergraduate medical education.
Fig. 4.
Transition from a personal to an organizational proficiency level depends upon competence in non-technical skills.
4.6. Limitations
We have performed a systematic review of the literature on the MEDLINE database only. Albeit 68 articles were included for full text retrieval, this is a restriction of our study, and future work should include studies in other databases. Furthermore, the intrinsic diversity of NTS teaching studies included prejudiced the use of currently approved tools for appraisal of quality of evidence. Whilst we believe this would not have altered our conclusions, we recognize this as a limitation which should be addressed in further developments of our framework.
5. Conclusion
It is evident that integration of NTS training in undergraduate education continues to face challenges, illustrated in part by the huge increase in emerging studies but more importantly by the striking inconsistency between them. We propose a unified framework for NTS training, with the objective of guiding future research, facilitating comparison between interventions, and spurring the creation of a standardized NTS course. Although this review focuses solely on personal gains from the medical perspective, coordinated efforts to achieve similar gains in allied healthcare professionals are expected to trigger multiplier effects. Future studies will be required to elucidate the current theories on NTS teaching, in the endeavor to enhance the education of tomorrow's doctors.
Provenance and peer review
Not commissioned, externally peer reviewed.
Ethical approval
Not required.
Sources of funding
Self funded.
Author contribution
MN drafted the manuscript and is the lead author; parts of the manuscript have been drafted and edited by LC and IT. MN, LC, IT, JH performed data extraction and synthesis of evidence. MS, AP GT, TA are the senior authors with input in several steps of the authorship. MS, MN and AP conceived study, search strategy and data synthesis. All authors have approved final manuscript.
Conflicts of interest
None declared.
Trial registry number
NA.
Research registration number
reviewregistry608.
Guarantor
MS and AP are the guarantors of this work. MN is the lead author.
Availability of data and material
The datasets supporting the conclusions of this article are included within the article (and its additional files). The raw data extraction from the reviewed studies can be shared by the corresponding author upon reasonable request.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2018.10.005.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Epstein R.M., Hundert E.M. Defining and assessing professional competence. Jama. 2002;287(2):226–235. doi: 10.1001/jama.287.2.226. [DOI] [PubMed] [Google Scholar]
- 2.Flin R., Yule S., Paterson-Brown S., Rowley D., Maran N. University of Aberdeen; Scotland: 2006. The Non-technical Skills for Surgeons (NOTSS) System Handbook V1. 2. [Google Scholar]
- 3.Flin R., Patey R., Glavin R., Maran N. Anaesthetists' non-technical skills. Br. J. Anaesth. 2010;105(1):38–44. doi: 10.1093/bja/aeq134. [DOI] [PubMed] [Google Scholar]
- 4.Youngson G.G. Teaching and assessing non-technical skills. Surgeon. 2011;9:S35–S37. doi: 10.1016/j.surge.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 5.Christian C.K., Gustafson M.L., Roth E.M., Sheridan T.B., Gandhi T.K., Dwyer K., Zinner M.J., Dierks M.M. A prospective study of patient safety in the operating room. Surgery. 2006;139(2):159–173. doi: 10.1016/j.surg.2005.07.037. [DOI] [PubMed] [Google Scholar]
- 6.Greenberg C.C., Regenbogen S.E., Studdert D.M., Lipsitz S.R., Rogers S.O., Zinner M.J., Gawande A.A. Patterns of communication breakdowns resulting in injury to surgical patients. J. Am. Coll. Surg. 2007;204(4):533–540. doi: 10.1016/j.jamcollsurg.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 7.Berwick D. vol. 6. Department of Health; London: 2013. (A Promise to Learn–a Commitment to Act: Improving the Safety of Patients in England). [Google Scholar]
- 8.Leape L.L. Error in medicine. Jama. 1994;272(23):1851–1857. [PubMed] [Google Scholar]
- 9.Donaldson M.S., Corrigan J.M., Kohn L.T. National Academies Press; 2000. To Err Is Human: Building a Safer Health System. [PubMed] [Google Scholar]
- 10.Landrigan C.P., Parry G.J., Bones C.B., Hackbarth A.D., Goldmann D.A., Sharek P.J. Temporal trends in rates of patient harm resulting from medical care. N. Engl. J. Med. 2010;363(22):2124–2134. doi: 10.1056/NEJMsa1004404. [DOI] [PubMed] [Google Scholar]
- 11.Laidlaw A.H. Social anxiety in medical students: implications for communication skills teaching. Med. Teach. 2009;31(7):649–654. doi: 10.1080/01421590802208867. [DOI] [PubMed] [Google Scholar]
- 12.Cannon-Bowers J.A., Salas E. Team performance and training in complex environments: recent findings from applied research. Curr. Dir. Psychol. Sci. 1998;7(3):83–87. [Google Scholar]
- 13.Flin R., Patey R. British Medical Journal Publishing Group; 2009. Improving Patient Safety through Training in Non-technical Skills. [DOI] [PubMed] [Google Scholar]
- 14.Gordon M., Darbyshire D., Baker P. Non‐technical skills training to enhance patient safety: a systematic review. Med. Educ. 2012;46(11):1042–1054. doi: 10.1111/j.1365-2923.2012.04343.x. [DOI] [PubMed] [Google Scholar]
- 15.Mumford E. Harvard University Press; 1970. Interns: from Students to Physicians. [Google Scholar]
- 16.Anvik T., Grimstad H., Baerheim A., Bernt Fasmer O., Gude T., Hjortdahl P., Holen A., Risberg T., Vaglum P. Medical students' cognitive and affective attitudes towards learning and using communication skills–a nationwide cross-sectional study. Med. Teach. 2008;30(3):272–279. doi: 10.1080/01421590701784356. [DOI] [PubMed] [Google Scholar]
- 17.Stewart M.A. Effective physician-patient communication and health outcomes: a review. CMAJ (Can. Med. Assoc. J.) 1995;152(9):1423. [PMC free article] [PubMed] [Google Scholar]
- 18.Deveugele M., Derese A., De Maesschalck S., Willems S., Van Driel M., De Maeseneer J. Teaching communication skills to medical students, a challenge in the curriculum? Patient Educ. Counsel. 2005;58(3):265–270. doi: 10.1016/j.pec.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 19.Ramirez A.J., Graham J., Richards M., Gregory W., Cull A. Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet. 1996;347(9003):724–728. doi: 10.1016/s0140-6736(96)90077-x. [DOI] [PubMed] [Google Scholar]
- 20.Stewart M. Radcliffe Publishing; 2003. Patient-centered Medicine: Transforming the Clinical Method. [Google Scholar]
- 21.Levinson W., Roter D.L., Mullooly J.P., Dull V.T., Frankel R.M. Physician-patient communication: the relationship with malpractice claims among primary care physicians and surgeons. Jama. 1997;277(7):553–559. doi: 10.1001/jama.277.7.553. [DOI] [PubMed] [Google Scholar]
- 22.Shea B.J., Reeves B.C., Wells G., Thuku M., Hamel C., Moran J., Moher D., Tugwell P., Welch V., Kristjansson E. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dalaya M., Ishaquddin S., GHaDaGe M., Hatte G. An interesting review on soft skills and dental practice. J. Clin. Diagn. Res.: JCDR. 2015;9(3):ZE19. doi: 10.7860/JCDR/2015/12725.5719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Outcomes for Graduates (Tomorrow's Doctors) General Medical Council; 2015. [Google Scholar]
- 25.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Erickson J.M., Blackhall L., Brashers V., Varhegyi N. An interprofessional workshop for students to improve communication and collaboration skills in end-of-life care. Am. J. Hospice Palliat. Med. 2015;32(8):876–880. doi: 10.1177/1049909114549954. [DOI] [PubMed] [Google Scholar]
- 27.Konopasek L., Kelly K.V., Bylund C.L., Wenderoth S., Storey-Johnson C. The group objective structured clinical experience: building communication skills in the clinical reasoning context. Patient Educ. Counsel. 2014;96(1):79–85. doi: 10.1016/j.pec.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 28.Robertson B., Kaplan B., Atallah H., Higgins M., Lewitt M.J., Ander D.S. The use of simulation and a modified Team STEPPS curriculum for medical and nursing student team training. Simulat. Healthc. J. Soc. Med. Simulat. 2010;5(6):332–337. doi: 10.1097/SIH.0b013e3181f008ad. [DOI] [PubMed] [Google Scholar]
- 29.Haidet P., Jarecke J., Yang C., Teal C.R., Street R.L., Stuckey H. Multidisciplinary Digital Publishing Institute; 2017. Using Jazz as a Metaphor to Teach Improvisational Communication Skills, Healthcare; p. 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kushner R.F., Zeiss D.M., Feinglass J.M., Yelen M. An obesity educational intervention for medical students addressing weight bias and communication skills using standardized patients. BMC Med. Educ. 2014;14(1):53. doi: 10.1186/1472-6920-14-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carter M.M., Lewis E.L., Sbrocco T., Tanenbaum R., Oswald J.C., Sykora W., Williams P., Hill L.D. Cultural competency training for third-year clerkship students: effects of an interactive workshop on student attitudes. J. Natl. Med. Assoc. 2006;98(11):1772. [PMC free article] [PubMed] [Google Scholar]
- 32.Mauksch L., Farber S., Greer H.T. Design, dissemination, and evaluation of an advanced communication elective at seven US medical schools. Acad. Med. 2013;88(6):843–851. doi: 10.1097/ACM.0b013e31828fd5ed. [DOI] [PubMed] [Google Scholar]
- 33.Heiman H.L., Uchida T., Adams C., Butter J., Cohen E., Persell S.D., Pribaz P., McGaghie W.C., Martin G.J. E-learning and deliberate practice for oral case presentation skills: a randomized trial. Med. Teach. 2012;34(12):e820–e826. doi: 10.3109/0142159X.2012.714879. [DOI] [PubMed] [Google Scholar]
- 34.Lanken P.N., Novack D.H., Daetwyler C., Gallop R., Landis J.R., Lapin J., Subramaniam G.A., Schindler B.A. Efficacy of an internet-based learning module and small-group debriefing on trainees' attitudes and communication skills toward patients with substance use disorders: results of a cluster randomized controlled trial. Acad. Med. 2015;90(3):345–354. doi: 10.1097/ACM.0000000000000506. [DOI] [PubMed] [Google Scholar]
- 35.LoSasso A.A., Lamberton C.E., Sammon M., Berg K.T., Caruso J.W., Cass J., Hojat M. Enhancing student empathetic engagement, history-taking, and communication skills during electronic medical record use in patient care. Acad. Med. 2017;92(7):1022–1027. doi: 10.1097/ACM.0000000000001476. [DOI] [PubMed] [Google Scholar]
- 36.Blatt B., Greenberg L. A multi-level assessment of a program to teach medical students to teach. Adv. Health Sci. Educ. 2007;12(1):7–18. doi: 10.1007/s10459-005-3053-2. [DOI] [PubMed] [Google Scholar]
- 37.Hobgood C.D., Tamayo-Sarver J.H., Hollar D.W., Jr., Sawning S. Griev_Ing: death notification skills and applications for fourth-year medical students. Teach. Learn. Med. 2009;21(3):207–219. doi: 10.1080/10401330903018450. [DOI] [PubMed] [Google Scholar]
- 38.Ludwig A.B., Raff A.C., Lin J., Schoenbaum E. Group observed structured encounter (GOSCE) for third-year medical students improves self-assessment of clinical communication. Med. Teach. 2017:1–5. doi: 10.1080/0142159X.2017.1332361. [DOI] [PubMed] [Google Scholar]
- 39.Hagemeier N.E., Hess R., Jr., Hagen K.S., Sorah E.L. Impact of an interprofessional communication course on nursing, medical, and pharmacy students' communication skill self-efficacy beliefs. Am. J. Pharmaceut. Educ. 2014;78(10):186. doi: 10.5688/ajpe7810186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rosen J., Spatz E.S., Gaaserud A.M., Abramovitch H., Weinreb B., Wenger N.S., Margolis C.Z. A new approach to developing cross-cultural communication skills. Med. Teach. 2004;26(2):126–132. doi: 10.1080/01421590310001653946. [DOI] [PubMed] [Google Scholar]
- 41.Wiese J., Varosy P., Tierney L. Improving oral presentation skills with a clinical reasoning curriculum: a prospective controlled study. Am. J. Med. 2002;112(3):212–218. doi: 10.1016/s0002-9343(01)01085-3. [DOI] [PubMed] [Google Scholar]
- 42.Lie D., Bereknyei S., Kalet A., Braddock C., 3rd Learning outcomes of a web module for teaching interpreter interaction skills to pre-clerkship students. Fam. Med. 2009;41(4) [PubMed] [Google Scholar]
- 43.Engler C.M., Saltzman G.A., Walker M.L., Wolf F.M. Medical student acquisition and retention of communication and interviewing skills. Acad. Med. 1981;56(7):572–579. doi: 10.1097/00001888-198107000-00005. [DOI] [PubMed] [Google Scholar]
- 44.Aboumatar H.J., Thompson D., Wu A., Dawson P., Colbert J., Marsteller J., Kent P., Lubomski L.H., Paine L., Pronovost P. Republished: development and evaluation of a 3-day patient safety curriculum to advance knowledge, self-efficacy and system thinking among medical students. Postgrad. Med. 2012;88(1043):545–551. doi: 10.1136/postgradmedj-2011-000463rep. [DOI] [PubMed] [Google Scholar]
- 45.Martino S., Haeseler F., Belitsky R., Pantalon M., Fortin A.H. Teaching brief motivational interviewing to year three medical students. Med. Educ. 2007;41(2):160–167. doi: 10.1111/j.1365-2929.2006.02673.x. [DOI] [PubMed] [Google Scholar]
- 46.Hess R., Hagemeier N.E., Blackwelder R., Rose D., Ansari N., Branham T. Teaching communication skills to medical and pharmacy students through a blended learning course. Am. J. Pharmaceut. Educ. 2016;80(4):64. doi: 10.5688/ajpe80464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hobgood C., Sherwood G., Frush K., Hollar D., Maynard L., Foster B., Sawning S., Woodyard D., Durham C., Wright M. 2010. Teamwork Training with Nursing and Medical Students: Does the Method Matter? Results of an Interinstitutional, Interdisciplinary Collaboration, Quality and Safety in Health Care. qshc.2007.031732. [DOI] [PubMed] [Google Scholar]
- 48.Hammer R.R., Rian J.D., Gregory J.K., Bostwick J.M., Birk C.B., Chalfant L., Scanlon P.D., Hall-Flavin D.K. Medical humanities; 2011. Telling the Patient's Story: Using Theatre Training to Improve Case Presentation Skills. jmh.2010.006429. [DOI] [PubMed] [Google Scholar]
- 49.Yeung C., Friesen F., Farr S., Law M., Albert L. Development and implementation of a longitudinal students as teachers program: participant satisfaction and implications for medical student teaching and learning. BMC Med. Educ. 2017;17(1):28. doi: 10.1186/s12909-017-0857-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shapiro S.M., Lancee W.J., Richards-Bentley C.M. Evaluation of a communication skills program for first-year medical students at the University of Toronto. BMC Med. Educ. 2009;9(1):11. doi: 10.1186/1472-6920-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Braniff C., Spence R.A., Stevenson M., Boohan M., Watson P. Assistantship improves medical students' perception of their preparedness for starting work. Med. Teach. 2016;38(1):51–58. doi: 10.3109/0142159X.2015.1045843. [DOI] [PubMed] [Google Scholar]
- 52.Buczacki S., Shalhoub J., George P.M., Vearncombe L.M., Byrne P.D., Alazawi W. Benefits of knowledge-based interprofessional communication skills training in medical undergraduate education. JRSM Short Rep. 2011;2(8):1–8. doi: 10.1258/shorts.2011.011065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Knox J., Bouchier I. Communication skills teaching, learning and assessment. Med. Educ. 1985;19(4):285–289. doi: 10.1111/j.1365-2923.1985.tb01322.x. [DOI] [PubMed] [Google Scholar]
- 54.Joekes K., Noble L.M., Kubacki A.M., Potts H.W., Lloyd M. Does the inclusion of'professional development'teaching improve medical students' communication skills? BMC Med. Educ. 2011;11(1):41. doi: 10.1186/1472-6920-11-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rees C., Sheard C. Evaluating first-year medical students' attitudes to learning communication skills before and after a communication skills course. Med. Teach. 2003;25(3):302–307. doi: 10.1080/0142159031000100409. [DOI] [PubMed] [Google Scholar]
- 56.Carpenter J. Interprofessional education for medical and nursing students: evaluation of a programme. Med. Educ. 1995;29(4):265–272. doi: 10.1111/j.1365-2923.1995.tb02847.x. [DOI] [PubMed] [Google Scholar]
- 57.Efstathiou N., Walker W.M. Interprofessional, simulation-based training in end of life care communication: a pilot study. J. Interprof. Care. 2014;28(1):68–70. doi: 10.3109/13561820.2013.827163. [DOI] [PubMed] [Google Scholar]
- 58.Fletcher I., Leadbetter P., Curran A., O'Sullivan H. A pilot study assessing emotional intelligence training and communication skills with 3rd year medical students. Patient Educ. Counsel. 2009;76(3):376–379. doi: 10.1016/j.pec.2009.07.019. [DOI] [PubMed] [Google Scholar]
- 59.Usherwood T. Subjective and behavioural evaluation of the teaching of patient interview skills. Med. Educ. 1993;27(1):41–47. doi: 10.1111/j.1365-2923.1993.tb00227.x. [DOI] [PubMed] [Google Scholar]
- 60.Dixon‐Woods M., Regan J., Robertson N., Young B., Cordle C., Tobin M. Teaching and learning about human sexuality in undergraduate medical education. Med. Educ. 2002;36(5):432–440. doi: 10.1046/j.1365-2923.2002.01198.x. [DOI] [PubMed] [Google Scholar]
- 61.Forsgren E., Hartelius L., Saldert C. Improving medical students' knowledge and skill in communicating with people with acquired communication disorders. Int. J. Speech Lang. Pathol. 2017;19(6):541–550. doi: 10.1080/17549507.2016.1216602. [DOI] [PubMed] [Google Scholar]
- 62.Fernández-Olano C., Montoya-Fernández J., Salinas-Sánchez A.S. Impact of clinical interview training on the empathy level of medical students and medical residents. Med. Teach. 2008;30(3):322–324. doi: 10.1080/01421590701802299. [DOI] [PubMed] [Google Scholar]
- 63.Loureiro E.M., Severo M., Bettencourt P., Ferreira M.A. Attitudes and anxiety levels of medical students towards the acquisition of competencies in communication skills. Patient Educ. Counsel. 2011;85(3):e272–e277. doi: 10.1016/j.pec.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 64.Franco C., Franco R., Severo M., Ferreira M.A. A brief course on clinical communication skills: a multi centered study. Acta Med. Port. 2016;29(12):809–818. doi: 10.20344/amp.8393. [DOI] [PubMed] [Google Scholar]
- 65.Doherty E.M., McGee H., O'Boyle C., Shannon W., Bury G., Williams A. 1992. Communication Skills Training in Undergraduate Medicine: Attitudes and Attitude Change. [PubMed] [Google Scholar]
- 66.Schildmann J., Härlein J., Burchardi N., Schlögl M., Vollmann J. Breaking bad news: evaluation study on self-perceived competences and views of medical and nursing students taking part in a collaborative workshop. Support. Care Canc. 2006;14(11):1157–1161. doi: 10.1007/s00520-006-0064-3. [DOI] [PubMed] [Google Scholar]
- 67.Simmenroth-Nayda A., Weiss C., Fischer T., Himmel W. Do communication training programs improve students' communication skills?-a follow-up study. BMC Res. Notes. 2012;5(1):486. doi: 10.1186/1756-0500-5-486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hagemann V., Herbstreit F., Kehren C., Chittamadathil J., Wolfertz S., Dirkmann D., Kluge A., Peters J. Does teaching non-technical skills to medical students improve those skills and simulated patient outcome? Int. J. Med. Educ. 2017;8:101. doi: 10.5116/ijme.58c1.9f0d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Engerer C., Berberat P.O., Dinkel A., Rudolph B., Sattel H., Wuensch A. Integrating 360 behavior-orientated feedback in communication skills training for medical undergraduates: concept, acceptance and students' self-ratings of communication competence. BMC Med. Educ. 2016;16(1):271. doi: 10.1186/s12909-016-0792-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cämmerer J., Martin O., Rockenbauch K. Learning Doctor-Patient Communication–Evaluating the effectiveness of the communication training course at Leipzig University from the students' point of view. GMS J. Med. Educ. 2016;33(3) doi: 10.3205/zma001042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.von Lengerke T., Kursch A., Lange K., MHH A.-L. The communication skills course for second year medical students at Hannover Medical School: an evaluation study based on students' self-assessments. GMS Z. Med. Ausbild. 2011;28(4) doi: 10.3205/zma000766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bonnaud‐Antignac A., Campion L., Pottier P., Supiot S. Videotaped simulated interviews to improve medical students' skills in disclosing a diagnosis of cancer. Psycho Oncol. 2010;19(9):975–981. doi: 10.1002/pon.1649. [DOI] [PubMed] [Google Scholar]
- 73.Koponen J., Pyörälä E., Isotalus P. Comparing three experiential learning methods and their effect on medical students' attitudes to learning communication skills. Med. Teach. 2012;34(3):e198–e207. doi: 10.3109/0142159X.2012.642828. [DOI] [PubMed] [Google Scholar]
- 74.Tiuraniemi J., Läärä R., Kyrö T., Lindeman S. Medical and psychology students' self-assessed communication skills: a pilot study. Patient Educ. Counsel. 2011;83(2):152–157. doi: 10.1016/j.pec.2010.05.013. [DOI] [PubMed] [Google Scholar]
- 75.Ozcan C., Oflaz F., Bakir B. The effect of a structured empathy course on the students of a medical and a nursing school. Int. Nurs. Rev. 2012;59(4):532–538. doi: 10.1111/j.1466-7657.2012.01019.x. [DOI] [PubMed] [Google Scholar]
- 76.Farnill D., Todisco J., Hayes S., Bartlett D. Videotaped interviewing of non‐English speakers: training for medical students with volunteer clients. Med. Educ. 1997;31(2):87–93. doi: 10.1111/j.1365-2923.1997.tb02464.x. [DOI] [PubMed] [Google Scholar]
- 77.Lim B.T., Moriarty H., Huthwaite M., Gray L., Pullon S., Gallagher P. How well do medical students rate and communicate clinical empathy? Med. Teach. 2013;35(2):e946–e951. doi: 10.3109/0142159X.2012.715783. [DOI] [PubMed] [Google Scholar]
- 78.Poole A.D., Sanson-Fisher R. Long-term effects of empathy training on the interview skills of medical students. Patient Counsell. Health Educ. 1980;2(3):125–127. doi: 10.1016/s0738-3991(80)80053-x. [DOI] [PubMed] [Google Scholar]
- 79.Alroy G., Ber R., Kramer D. An evaluation of the short‐term effects of an interpersonal skills course. Med. Educ. 1984;18(2):85–89. doi: 10.1111/j.1365-2923.1984.tb00978.x. [DOI] [PubMed] [Google Scholar]
- 80.Zgheib N.K., Dimassi Z., Bou Akl I., Badr K.F., Sabra R. The long-term impact of team-based learning on medical students' team performance scores and on their peer evaluation scores. Med. Teach. 2016;38(10):1017–1024. doi: 10.3109/0142159X.2016.1147537. [DOI] [PubMed] [Google Scholar]
- 81.Lau K.C.J., Stewart S., Fielding R. Preliminary evaluation of ‘interpreter’role plays in teaching communication skills to medical undergraduates. Med. Educ. 2001;35(3):217–221. doi: 10.1046/j.1365-2923.2001.00731.x. [DOI] [PubMed] [Google Scholar]
- 82.Lukman H., Beevi Z., Yeap R. Training future doctors to be patient-centred: efficacy of a communication skills training (CST) programme in a Malaysian medical institution. Med. J. Malaysia. 2009;64(1):52–55. [PubMed] [Google Scholar]
- 83.Lim B.T., Moriarty H., Huthwaite M. “Being-in-role”: a teaching innovation to enhance empathic communication skills in medical students. Med. Teach. 2011;33(12):e663–e669. doi: 10.3109/0142159X.2011.611193. [DOI] [PubMed] [Google Scholar]
- 84.Ayuob N.N., Qadi M.A., El Deek B.S., Boker A.M. Evaluation of a communication skills training course for medical students using peer role-play. JPMA J. Pakistan Med. Assoc. 2017;67(5):745. [PubMed] [Google Scholar]
- 85.Betson C., Fielding R., Wong G., Chung S., Nestel D. Evaluation of two videotape instruction programmes on how to break bad news—for Cantonese-speaking medical students in Hong Kong. J. Audiov. Media Med. 1997;20(4):172–177. doi: 10.3109/17453059709063101. [DOI] [PubMed] [Google Scholar]
- 86.Chun K.H., Lee Y.H. Improvement of debate competence: an outcome of an introductory course for medical humanities. Korean J. Med. Educ. 2016;28(1):87. doi: 10.3946/kjme.2016.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Fadlon J., Pessach I., Toker A. Teaching medical students what they think they already know. Educ. Health. 2004;17(1):35–41. doi: 10.1080/13576280310001656132. [DOI] [PubMed] [Google Scholar]
- 88.Harlak H., Gemalmaz A., Gurel F., Dereboy C., Ertekin K. Communication skills training: effects on attitudes toward communication skills and empathic tendency. Educ. Health. 2008;21(2):62. [PubMed] [Google Scholar]
- 89.Karnieli-Miller O., Michael K., Segal O., Steinberger A. Health communication; 2017. Assessing an Intervention Focused on Enhancing Interpersonal Communication Skills and Humor: a Multi-method Quasi-experiential Study Among Medical Students; pp. 1–13. [DOI] [PubMed] [Google Scholar]
- 90.Moorhead R., Winefield H. Teaching counselling skills to fourth-year medical students: a dilemma concerning goals. Fam. Pract. 1991;8(4):343–346. doi: 10.1093/fampra/8.4.343. [DOI] [PubMed] [Google Scholar]
- 91.Saab B., Usta J., Major S., Antoun J. Impact of a communication skills audiovisual package on medical students' knowledge, Le Journal medical libanais. Leban. Med. J. 2009;57(4):226–230. [PubMed] [Google Scholar]
- 92.Tsai M.-H., Lu F.-H., Frankel R.M. Learning to listen: effects of using conversational transcripts to help medical students improve their use of open questions in soliciting patient problems. Patient Educ. Counsel. 2013;93(1):48–55. doi: 10.1016/j.pec.2013.03.022. [DOI] [PubMed] [Google Scholar]
- 93.Yu E.H., Choi E.J., Lee S.Y., Im S.J., Yune S.J., Baek S.Y. Effects of micro-and subtle-expression reading skill training in medical students: a randomized trial. Patient Educ. Counsel. 2016;99(10):1670–1675. doi: 10.1016/j.pec.2016.04.013. [DOI] [PubMed] [Google Scholar]
- 94.Smith R.C. The biopsychosocial revolution. J. Gen. Intern. Med. 2002;17(4):309–310. [Google Scholar]
- 95.Chin J.J. Doctor-patient relationship: from medical paternalism to enhanced autonomy. Singap. Med. J. 2002;43(3):152–155. [PubMed] [Google Scholar]
- 96.Huang C.-C., Huang C.-C., Yang Y.-Y., Lin S.-J., Chen J.-W. The influence of gender on the communication skills assessment of medical students. Eur. J. Intern. Med. 2015;26(9):670–674. doi: 10.1016/j.ejim.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 97.Salem R.O., Al-Mously N., Nabil N.M., Al-Zalabani A.H., Al-Dhawi A.F., Al-Hamdan N. Academic and socio-demographic factors influencing students' performance in a new Saudi medical school. Med. Teach. 2013;35(sup1):S83–S89. doi: 10.3109/0142159X.2013.765551. [DOI] [PubMed] [Google Scholar]
- 98.Haist S.A., Wilson J.F., Elam C.L., Blue A.V., Fosson S.E. The effect of gender and age on medical school performance: an important interaction. Adv. Health Sci. Educ. 2000;5(3):197–205. doi: 10.1023/A:1009829611335. [DOI] [PubMed] [Google Scholar]
- 99.Gordon M., Baker P., Catchpole K., Darbyshire D., Schocken D. Devising a consensus definition and framework for non-technical skills in healthcare to support educational design: a modified Delphi study. Med. Teach. 2015;37(6):572–577. doi: 10.3109/0142159X.2014.959910. [DOI] [PubMed] [Google Scholar]
- 100.Mitchell L., Flin R. Ashgate; Farnham, UK: 2009. Scrub Practitioners' List of Intra-operative Nontechnical Skills-SPLINTS, Safer Surgery: Analysing Behaviour in the Operating Theatre; pp. 67–81. [Google Scholar]
- 101.Hull L., Sevdalis N. Advances in teaching and assessing nontechnical skills. Surg. Clin. 2015;95(4):869–884. doi: 10.1016/j.suc.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 102.Chakravarthy B., ter Haar E., Bhat S.S., McCoy C.E., Denmark T.K., Lotfipour S. Simulation in medical school education: review for emergency medicine. West. J. Emerg. Med. 2011;12(4):461. doi: 10.5811/westjem.2010.10.1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lateef F. Simulation-based learning: just like the real thing. J. Emergencies, Trauma, Shock. 2010;3(4):348. doi: 10.4103/0974-2700.70743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Coggins A., Desai M., Nguyen K., Moore N. Early acquisition of non-technical skills using a blended approach to simulation-based medical education. Adv. Simulat. 2017;2(1):12. doi: 10.1186/s41077-017-0045-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Bagnasco A., Pagnucci N., Tolotti A., Rosa F., Torre G., Sasso L. The role of simulation in developing communication and gestural skills in medical students. BMC Med. Educ. 2014;14(1):106. doi: 10.1186/1472-6920-14-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Subramanian P., Sathanandan K. Improving communication skills using simulation training. Br. J. Med. Pract. 2016;9(2):40–43. [Google Scholar]
- 107.Gordon M., Box H., Farrell M., Stewrt A. 2015. Non-technical Skills Learning in Healthcare through Simulation Education: Integrating the SECTORS Learning Model and Complexity Theory, BMJ Simulation and Technology Enhanced Learning. bmjstel-2015-000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Baile W.F., Blatner A. Teaching communication skills: using action methods to enhance role-play in problem-based learning. Simulat. Healthc. J. Soc. Med. Simulat. 2014;9(4):220–227. doi: 10.1097/SIH.0000000000000019. [DOI] [PubMed] [Google Scholar]
- 109.Harnof S., Hadani M., Ziv A., Berkenstadt H. Simulation-based interpersonal communication skills training for neurosurgical residents. Isr. Med. Assoc. J. 2013;15(9):489–492. [PubMed] [Google Scholar]
- 110.Nuzhat A., Salem R.O., Al Shehri F.N., Al Hamdan N. Role and challenges of simulation in undergraduate curriculum. Med. Teach. 2014;36(sup1):S69–S73. doi: 10.3109/0142159X.2014.886017. [DOI] [PubMed] [Google Scholar]
- 111.Keskitalo T., Ruokamo H., Gaba D. Towards meaningful simulation-based learning with medical students and junior physicians. Med. Teach. 2014;36(3):230–239. doi: 10.3109/0142159X.2013.853116. [DOI] [PubMed] [Google Scholar]
- 112.Bokken L., Linssen T., Scherpbier A., Van Der Vleuten C., Rethans J.J. Feedback by simulated patients in undergraduate medical education: a systematic review of the literature. Med. Educ. 2009;43(3):202–210. doi: 10.1111/j.1365-2923.2008.03268.x. [DOI] [PubMed] [Google Scholar]
- 113.Labaf A., Jamali K., Jalili M., Baradaran H.R., Eizadi P. Effect of repetitive feedback on residents' communication skills improvement. Acta Med. Iran. 2014;52(7):557. [PubMed] [Google Scholar]
- 114.Van Dalen J., Kerkhofs E., van Knippenberg-Van Den Berg B., van Den Hout H., Scherpbier A., Van der Vleuten C. Longitudinal and concentrated communication skills programmes: two Dutch medical schools compared. Adv. Health Sci. Educ. 2002;7(1):29–40. doi: 10.1023/a:1014576900127. [DOI] [PubMed] [Google Scholar]
- 115.Malhotra A., Gregory I., Darvill E., Goble E., Pryce-Roberts A., Lundberg K., Konradsen S., Hafstad H. Mind the gap: learners' perspectives on what they learn in communication compared to how they and others behave in the real world. Patient Educ. Counsel. 2009;76(3):385–390. doi: 10.1016/j.pec.2009.07.024. [DOI] [PubMed] [Google Scholar]
- 116.Craig J. Retention of interviewing skills learned by first‐year medical students: a longitudinal study. Med. Educ. 1992;26(4):276–281. doi: 10.1111/j.1365-2923.1992.tb00169.x. [DOI] [PubMed] [Google Scholar]
- 117.Diseker R.A., Michielutte R. An analysis of empathy in medical students before and following clinical experience. J. Med. Educ. 1981;56(12):1004–1010. doi: 10.1097/00001888-198112000-00004. [DOI] [PubMed] [Google Scholar]
- 118.Hojat M., Mangione S., Nasca T.J., Rattner S., Erdmann J.B., Gonnella J.S., Magee M. An empirical study of decline in empathy in medical school. Med. Educ. 2004;38(9):934–941. doi: 10.1111/j.1365-2929.2004.01911.x. [DOI] [PubMed] [Google Scholar]
- 119.Chen D., Lew R., Hershman W., Orlander J. A cross-sectional measurement of medical student empathy. J. Gen. Intern. Med. 2007;22(10):1434–1438. doi: 10.1007/s11606-007-0298-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Harden R.M. What is a spiral curriculum? Med. Teach. 1999;21(2):141–143. doi: 10.1080/01421599979752. [DOI] [PubMed] [Google Scholar]
- 121.Rushton A. Formative assessment: a key to deep learning? Med. Teach. 2005;27(6):509–513. doi: 10.1080/01421590500129159. [DOI] [PubMed] [Google Scholar]
- 122.Ben-David M.F. The role of assessment in expanding professional horizons. Med. Teach. 2000;22(5):472–477. doi: 10.1080/01421590050110731. [DOI] [PubMed] [Google Scholar]
- 123.Rees C., Sheard C., Davies S. The development of a scale to measure medical students' attitudes towards communication skills learning: the Communication Skills Attitude Scale (CSAS) Med. Educ. 2002;36(2):141–147. doi: 10.1046/j.1365-2923.2002.01072.x. [DOI] [PubMed] [Google Scholar]
- 124.Hojat M., Mangione S., Nasca T.J., Cohen M.J., Gonnella J.S., Erdmann J.B., Veloski J., Magee M. The Jefferson Scale of Physician Empathy: development and preliminary psychometric data. Educ. Psychol. Meas. 2001;61(2):349–365. [Google Scholar]
- 125.Hojat M., Gonnella J.S., Nasca T.J., Mangione S., Veloksi J.J., Magee M. The Jefferson Scale of Physician Empathy: further psychometric data and differences by gender and specialty at item level. Acad. Med. 2002;77(10):S58–S60. doi: 10.1097/00001888-200210001-00019. [DOI] [PubMed] [Google Scholar]
- 126.Roh M.-S., Hahm B.-J., Lee D.H., Suh D.H. Evaluation of empathy among Korean medical students: a cross-sectional study using the Korean Version of the Jefferson Scale of Physician Empathy. Teach. Learn. Med. 2010;22(3):167–171. doi: 10.1080/10401334.2010.488191. [DOI] [PubMed] [Google Scholar]
- 127.Kliszcz J., Nowicka-Sauer K., Trzeciak B., Nowak P., Sadowska A. Empathy in health care providers–validation study of the Polish version of the Jefferson Scale of Empathy. Adv. Med. Sci. 2006;51 [PubMed] [Google Scholar]
- 128.Alcorta-Garza A., Gonzalez-Guerrero J., Tavitas-Herrera S., Rodríguez-Lara F., Hojat M. Validity and reliability of the Jefferson scale of physician empathy in Mexican medial students. Salud Ment. 2005;28(5):57–63. [Google Scholar]
- 129.Ahn S., Yi Y.H., Ahn D.S. Developing a Korean communication skills attitude scale: comparing attitudes between Korea and the West. Med. Educ. 2009;43(3):246–253. doi: 10.1111/j.1365-2923.2008.03271.x. [DOI] [PubMed] [Google Scholar]
- 130.Harlak H., Dereboy C., Gemalmaz A. Validation of a Turkish translation of the communication skills attitude scale with Turkish medical students. Educ. Health. 2008;21(1):55. [PubMed] [Google Scholar]
- 131.Molinuevo B., Torrubia R. Validation of the Catalan version of the communication skills attitude scale (CSAS) in a cohort of south European medical and nursing students. Educ. Health. 2011;24(1):499. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.