Keywords: nerve regeneration, spinal cord injury, flavonoids, Scutellaria baicalensis, neurofilament, brain-derived neurotrophic factor, astrocytes, microglia, neural regeneration
Abstract
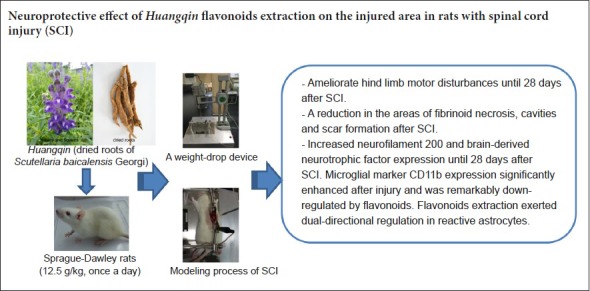
Flavonoids from Huangqin (dried roots of Scutellaria baicalensis Georgi) have anti-inflammatory effects, and are considered useful for treatment of spinal cord injury. To verify this hypothesis, the T9–10 spinal cord segments of rats were damaged using Allen's method to establish a rat spinal cord injury model. Before model establishment, Huangqin flavonoid extraction (12.5 g/kg) was administered intragastrically for 1 week until 28 days after model establishment. Methylprednisolone (30 mg/kg) was injected into the tail vein at 30 minutes after model establishment as a positive control. Basso, Beattie, and Bresnahan locomotor scale scores were used to assess hind limb motor function. Hematoxylin-eosin staining was used to detect pathological changes in the injured spinal cord. Immunofluorescence and western blot assays were performed to measure immunoreactivity and expression levels of brain-derived neurotrophic factor, neuronal marker neurofilament protein, microglial marker CD11b and astrocyte marker glial fibrillary acidic protein in the injured spinal cord. Huangqin flavonoid extraction markedly reduced spinal cord hematoma, inflammatory cell infiltration and cavities and scars, and increased the Basso, Beattie, and Bresnahan locomotor scale scores; these effects were identical to those of methylprednisolone. Huangqin flavonoid extraction also increased immunoreactivity and expression levels of brain-derived neurotrophic factor and neurofilament protein, and reduced immunoreactivity and expression levels of CD11b and glial fibrillary acidic protein, in the injured spinal cord. Overall, these data suggest that Huangqin flavonoid extraction can promote recovery of spinal cord injury by inducing brain-derived neurotrophic factor and neurofilament protein expression, reducing microglia activation and regulating reactive astrocytes.
Introduction
Spinal cord injury (SCI) is caused by a severe insult or progressive neurodegeneration, and frequently leads to neurological deficits and disabilities. The prevalence of SCI ranges from 250 to 906 cases per million, with an annual incidence of acute SCI of 8–49.1 per million worldwide, while the global prevalence is expected to increase over the next few years (Singh et al., 2014). Although there have been significant advances in the treatment of SCI, many patients still suffer substantial neurological disabilities (Michailidou et al., 2014). The major obstacle of SCI therapy is neuronal survival and axonal regeneration, which are usually inhibited by multiple chemical and physical factors in the damaged microenvironment (Colón and Miranda, 2016; Hachem et al., 2017). Thus, treatments are required to eliminate inhibitory factors, but enhance neuronal survival, after SCI.
Scutellaria baicalensis (Chinese skullcap) is the dry root of Scutellaria baicalensis Georgi (Lamiaceae) (see http://www.theplantlist.org). Scutellaria baicalensis is one of the most commonly used traditional Chinese herbs, and it is typically referred to as Huangqin. Huangqin is widely distributed in China, Russia, Mongolia, Korea, and Japan, and is officially listed in the Chinese Pharmacopoeia. The major phytochemicals of Huangqin have been confirmed as flavonoids, which possess anti-inflammatory, anti-tumor, anti-apoptosis, free radical scavenging, and anti-human immunodeficiency virus activities (Li et al., 2011; Gaire et al., 2014). Recently, the neuroprotective effects of Huangqin extraction and its isolated flavonoids have also been examined in various in vivo and in vitro models, suggesting a protective action against neurodegenerative diseases (Gasiorowski et al., 2011; Cheng et al., 2012; Xu et al., 2015).
The aim of the present study was to investigate the neuroprotective effect of the Huangqin flavonoid extraction in terms of recovery of motor function and histomorphological changes following SCI in rats. The therapeutic effects of Huangqin flavonoid extraction were compared with the positive control drug methylprednisolone (MP), a routine clinical therapy for early stage SCI. We also used immunofluorescence and western blot to evaluate changes in axonal regeneration, brain-derived neurotrophic factor (BDNF), activation of microglia and proliferation of reactive astrocytes.
Materials and Methods
Animals
Animals used in this study were maintained in accordance with the Guide for Care and Use of Laboratory Animals published by the U.S. National Institutes of Health (NIH publication No. 85-23, revised 1996). The experiments were approved by the Animal Ethics Committee of College of Medicine, Xi’an Jiaotong University, China. The 48 female specific-pathogen-free Sprague-Dawley rats aged 12 weeks and weighing 200 ± 20 g were provided by College of Medicine, Xi’an Jiaotong University, China (license No. SCXK [Shaanxi] 2007-001). The rats were housed at 22 ± 2°C in a 12-hour dark/light cycle, and allowed free access to food and water. Rats were randomly divided into four groups (n = 12 per group): normal, model (SCI), MP (positive control; SCI + MP) and Huangqin (SCI + Huangqin flavonoid extraction) groups.
Preparation and separation of Huangqin flavonoid extract
Huangqin was purchased from Sichuan Xinhehua Medicinal Materials Electuary Co., Ltd. (Sichuan, China), and the plant material was identified by Dr. Li-Xin Zhang. A voucher specimen was deposited at the Herbarium of Translational Medicine Center, Hong Hui Hospital, Xi’an Jiaotong University, China.
Huangqin flavonoid extraction was prepared from the dried roots of Scutellaria baicalensis Georgi by three rounds of reflux with 75% ethanol, with reflux times of 3 hours, 2 hours and 1 hour, respectively. All the extracted liquid was filtered, combined and concentrated under vacuum, and then stored at 4°C. Using this extraction preparation, 1 g extraction contains 1 g of dry root of Scutellaria baicalensis Georgi (Yune et al., 2009). Results of chemical fingerprint of Huangqin flavonoid extraction are shown in Additional file 1 (342.4KB, pdf) . Identification and measurement of the major constituents in Huangqin (Scutellaria baicalensis Georgi) are shown in Additional file 2 (190.1KB, pdf) .
Chemical fingerprint of huangqin flavonoids extraction
Identification and measurement of major constituents in huangqin
Drug dose determination of flavonoid extraction
In preliminary experiments, different doses (2.5, 7.5 and 12.5 g/kg) of Huangqin flavonoid extraction were administered by intragastric gavage to SCI rats. According to behavioral scores and hematoxylin and eosin staining (data not shown), there was a dose-dependent treatment effect. However, considering the viscosity of extraction and stomach volume of rats, we selected 12.5 g/kg as the optimal dosage for the present study.
SCI model establishment
Rats in model and Huangqin groups were anesthetized with pentobarbital sodium (40 mg/kg) intraperitoneally. A laminectomy was performed at the T9–10 levels, exposing the underlying spinal cord without destroying the spinal dura mater. The spine was clamped to stabilization at the T8–11 levels. A moderate contusion was induced using a weight-drop device (RWD G124-138; RWD Life Science Co., Ltd., Shenzhen, China) by dropping a 10 g rod (2.5 mm in diameter) from a height of 50 mm onto the exposed cord. The skin and musculature were then sutured (Allen, 1911). Spastic swinging of the tail and flaccid paralysis of the posterior limb are considered signs of a successful SCI model. All SCI rats received bladder evacuation twice daily until sphincter control had recovered, and gentamicin (80,000 U in each rat, via intramuscular injection) was administered to prevent urinary tract infection. The cages were cleaned daily to prevent wound infection, and rats were provided free access to water and food.
Drug administration
Rats in the Huangqin group received intragastric gavage of the flavonoid extraction (12.5 g/kg, once daily) for 1 week before surgery, and then after SCI until sacrifice. Rats in the normal, MP, and model groups received free access to food and water. Rats in MP group were administered MP injection via the caudal vein at 30 minutes after surgery (30 mg/kg).
Basso, Beattie, and Bresnahan locomotor scale
Two researchers blinded to the groupings independently assessed the functional recovery of all 48 rats (12 rats per group) at each time point using the Basso, Beattie, and Bresnahan (BBB) locomotor scale. After SCI, the average BBB scores were recorded on days 0, 3 and 7, and then every week until the fourth week. The score was assigned from a range of 0 (flat paralysis) to 21 (normal gait) based on limb movement, gait, coordination and paw placement (Basso et al., 1995).
Tissue collecting and processing
At 3, 14 and 28 days after surgery, 12 rats in each group (6 rats for immunofluorescence staining, 6 rats for western blot assay) were sacrificed by pentobarbital sodium (40 mg/kg intraperitoneal), and the spinal cords collected.
For hematoxylin and eosin staining and immunofluorescence, rats were transcardially perfused with normal saline (100 mL) then 4% paraformaldehyde (100 mL). The spinal cords were removed and fixed in 4% paraformaldehyde overnight, and then transferred to 30% sucrose solutions for cryoprotection. Each spinal cord was cut into 20 mm lengths with the lesion site at the center. The tissues were then frozen, embedded in optimal cutting temperature compound and cut into 14-μm thick longitudinal sections with a freezing microtome (Leica, Germany).
For western blot assay, the spinal cords were freshly collected and frozen at −20°C without perfusion.
Hematoxylin and eosin staining
To examine the cavities and damage to the spinal cord, the longitudinal sections were stained with hematoxylin and eosin. The sections were stained with hematoxylin and rinsed, and placed in acid-alcohol (1% hydrochloric acid). The sections were then counterstained with eosin and rinsed, and treated with distilled water, alcohol and xylene. The sections were air-dried, cover slipped with neutral balsam and examined under a light microscope (DM1000; Leica, Wetzlar, Germany). Areas of cavities on the photographs were calculated using ImageJ software (V1.8.0; National Institutes of Health, Bethesda, MD, USA).
Immunofluorescence assay
For the immunofluorescence assay, sections were washed with phosphate buffered saline (PBS), and then exposed to bovine serum albumin solution (0.5%) for 1 hour at room temperature. Next, the sections were incubated overnight at 4°C with solution A or solution B. Solution A contained the following primary antibodies: goat anti-BDNF polyclonal antibody (1:400; Santa Cruz Biotechnology, Dallas, TX, USA) and mouse anti-neurofilament-H (NF-H; axonal marker (He and Nan, 2016)) polyclonal antibody (1:400; Cell Signaling Technology Inc., Danvers, MA, USA). Solution B contained the following primary antibodies: mouse anti-glial fibrillary acidic protein (GFAP; marker for astroglia (Yuan and He, 2013)) polyclonal antibody (1:400; Cell Signaling Technology Inc.) and rabbit anti-CD11b (microglia marker (Norden et al., 2015)) polyclonal antibody (1:400; Novus, New York, NY, USA). After washing with PBS, the sections were incubated for 1 hour with solution C or solution D at room temperature. Solution C contained the following secondary antibodies: rabbit anti-goat antibody (1:200; FITC; Boster, Wuhan, China) against BDNF, and goat anti-mouse antibody (1:200; TRITC; Boster) against NF-H. Solution D contained the following secondary antibodies: goat anti-mouse antibody (1:200; DyLight 594; Boster) against GFAP, and donkey anti-rabbit antibody (1:200; DyLight 488; Boster) against CD11b. Excess secondary antibody was washed off. Next, sections were incubated in 4′,6-diamidino-2-phenylindole for 5 minutes at room temperature, and then washed three times with PBS. Sections were coverslipped and immediately observed under a fluorescence microscope (DM1000; Leica, Wetzlar, Germany).
The intensity of BDNF, NF-H, GFAP and CD11b expression was quantified by the sum of integrated optical density values obtained from the threshold pixels for all signals measured in each image. ImageJ (National Institutes of Health) was used to analyze optical densities. From each section, eight representative visual fields were chosen to calculate the mean optical density value. The integrated optical density was equal to neutral area in the immunofluorescence image × optical density.
Western blot assay
Protein was extracted from spinal cord tissue and heated with loading buffer at 95°C for 5 minutes for denaturation. A 50 mg of each protein sample was then separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis with 8% (NF-H and CD11b) or 15% (BDNF and GFAP) gels. Protein bands were electroblotted onto polyvinylidene difluoride membranes and blocked with non-fat dried milk for 1 hour. The blots were then probed with mouse anti-NF-H polyclonal antibody (1:1000; Cell Signaling Technology Inc.), goat anti-BDNF polyclonal antibody (1:1000; Santa Cruz Biotechnology), mouse anti-GFAP polyclonal antibody (1:1000; Cell Signaling Technology Inc.), rabbit anti-CD11b polyclonal antibody (1:1000; Novus) and goat anti-β-actin monoclonal antibody (1:1000; Cell Signaling Technology Inc.) overnight at room temperature. After washing with Tris buffered saline tween, sections were incubated with peroxidase anti-mouse, anti-goat and anti-rabbit IgG (1:5000) secondary antibodies for 1 hour at room temperature. Immunoreactivity was detected by enhanced chemiluminescence assay. Autoradiograms were exposed for 5–15 minutes. The micrographs were analyzed by Image Pro Plus 6 (Media Cybernetics, Sliver Spring, MD, USA). After defining a threshold for background correction, relative optical density of NF-H, BDNF, GFAP and CD11b in the grey matter was calculated.
Statistical analysis
All data are expressed as the mean ± SD. Statistical significances between groups were evaluated using statistical software (IBM SPSS Statistics version 22; IBM Co., Armonk, NY, USA) by one-way analysis of variance followed by Student-Newman-Keuls post hoc test. A P-value < 0.05 was considered statistically significant.
Results
Flavonoid extraction improves the morphology of the injured spinal cord in SCI model rats
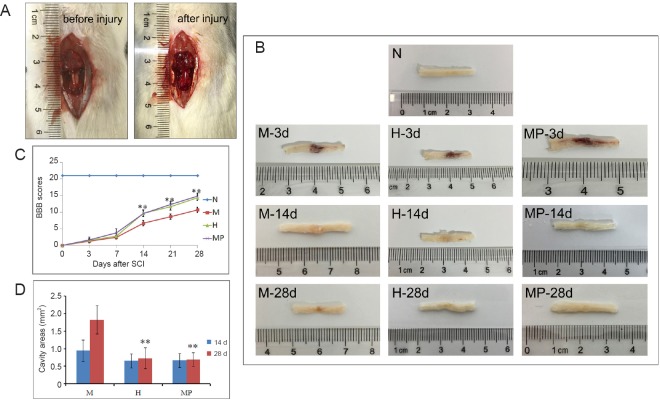
In the normal group without SCI, the spinal cord tissue was smooth and intact (Figure 1B). During SCI model establishment, a visible edema and hemorrhage occurred within a few seconds (Figure 1A), and a visible spinal cord hematoma was observed on the spinal cord at 3 days after surgery. The hematoma then disappeared and was replaced by a clear wound at 14 and 28 days after SCI. In the MP and Huangqin groups, the hematoma severity at 3 days was similar to that of the model group, but was reduced at 14 and 28 days compared with the model group.
Figure 1.
Effect of Huangqin flavonoid extraction on motor function of rats after spinal cord injury (SCI).
(A) The exposed spinal cord before and after the contusion injury induced with a weight-drop device. Hemorrhages and spinal cord edema are labeled with white arrows. (B) The stripped spinal cord tissue of different groups. (C) Effect of flavonoid extraction on motor function, as assessed using the Basso, Beattie, and Bresnahan (BBB) scoring system up to 4 weeks after SCI (n = 6 per group). (D) Effect of flavonoid extraction on cavities areas at 14 and 28 d after SCI. Data are presented as the mean ± SD, and analyzed by one-way analysis of variance followed by the Student-Newman-Keuls post hoc test. **P < 0.01, vs. model group. N: Normal group; M: model group; H: Huangqin group; d: days.
Flavonoid extraction improves motor function of SCI rats
The BBB scores of all rats in the model and Huangqin groups were 0 on the day of surgery (Figure 1C), which indicated complete loss of motor ability in the posterior limbs. From 14 to 28 days after SCI, the BBB scores indicated that flavonoid extraction intervention significantly ameliorated the hind limb motor disturbances (P < 0.01).
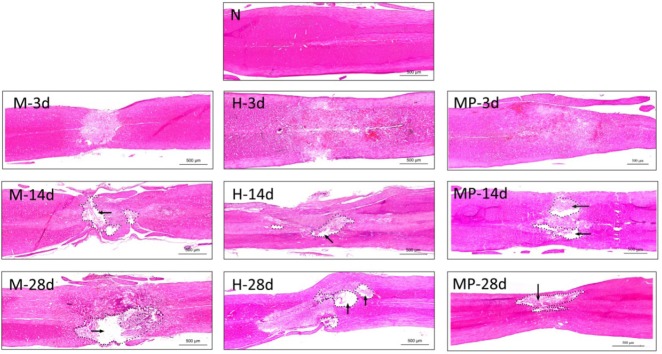
Flavonoid extraction improves the morphological features of the lesion site in the injured spinal cord
Hematoxylin and eosin staining was used to examine the morphological changes at the lesion site in SCI rats. After SCI, there was evidence of disorganization of the lesion site, inflammatory cell infiltration and formation of a cavity and scar in the model, MP and Huangqin groups (Figure 2). At 3 days after SCI, hemorrhages scattered throughout the injured area and diffuse degeneration were observed in the model, MP and Huangqin groups.
Figure 2.
Effect of Huangqin flavonoid extraction on the histomorphological changes of the injured spinal cord.
Assessment of injury in spinal cord sections using hematoxylin and eosin staining (original magnification, 4×). All cell nuclei were stained dark purple, and the cytoplasm was stained pink. The cavities (arrows) are labeled with a dotted line. Scale bars: 500 μm. N: Normal group; M: model group; H: Huangqin group; d: days.
However, at 14 days after SCI, there was a marked increase in cell infiltration and structural disturbances at the injury site in the model group, which was not observed in the MP and Huangqin groups. Further, at 28 days after SCI, there was clear evidence of extended areas of fibrinoid necrosis, and cavities and scar formation, at the lesion site in the model group, which was less severe in the MP and Huangqin groups. The cavity areas in the Huangqin group and MP groups at 28 days after SCI were also significantly smaller than that of model group (P < 0.05), while there were no differences between the groups at 14 days (P > 0.05; Figure 1D).
Overall, data from the BBB scores and hematoxylin and eosin staining suggest that Huangqin flavonoid extraction showed protective effects against SCI, which were similar to that for MP. Previous studies also reported that MP can upregulate NF-H and BDNF expression, while down-regulate GFAP and CD11b expression, after SCI (Donnelly and Popovich, 2008). Thus, immunofluorescence and western blot data of the MP group were not shown in the present study.
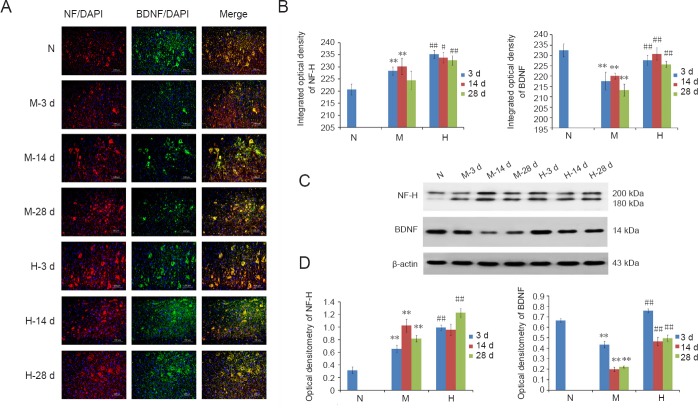
Flavonoid extraction increases neurofilament expression at the lesion site of SCI rats
In the normal group, there were low levels of NF-H detected in axons and cell bodies of neurons. By contrast, the clear funicular structure of axons disappeared after SCI, with evidence of severe diffuse axonal injury, which was particularly high at 3 and 14 days after SCI (Figure 3A). In model group, there was a progressive increase in NF-H staining up to 2 weeks, while NF-H staining was significantly lower at 4 weeks recovery (P < 0.01; Figure 3B). In the Huangqin group, there was less evidence of changes in the funicular structure of the axons, and NF-H expression was significantly higher than that in the model group at all time points (P < 0.05, P < 0.01; Figure 3B).
Figure 3.
Effect of Huangqin flavonoid extraction on the expression of neurofilament-H (NF-H) and brain-derived neurotrophic factor (BDNF) in neurons in the injured spinal cord of SCI rats.
(A) NF-H (TRITC, red) and BDNF (FITC, green) expression with double-immunofluorescence labeling, and 4′,6-diamidino-2-phenylindole (DAPI) counterstaining, of the injured spinal cord at 3, 14 and 28 d of recovery in each group. (B) The integrated optical density of NF-H and BDNF double-immunofluorescence expression at 3, 14 and 28 d of recovery in each group (n = 8 per group). Western blot results (C) and bar graphs (D) showing NF-H and BDNF expression at 3, 14 and 28 d of recovery in each group (n = 6 per group). Data are presented as the mean ± SD, and analyzed by one-way analysis of variance followed by the Student-Newman-Keuls post hoc test. **P < 0.01, vs. normal group; #P < 0.05, ##P < 0.01, vs. model group. N: Normal group; M: model group; H: Huangqin group; BDNF: brain-derived neurotrophic factor; NF-H: neurofilament-H; DAPI: 4′,6-diamidino-2-phenylindole; d: days.
Results of western blot assay showed a significant increase in NF-H (200 kDa) expression in the model group (P < 0.01) compared with controls, which was further increased in the Huangqin group at all time points (P < 0.01; Figure 3C and D).
Flavonoid extraction increases BDNF expression at the lesion site of SCI rats
BDNF is an important neurotrophic factor, and is co-expressed with NF-H in neurons and axons (Hodgetts and Harvey, 2017). As shown in Figure 3B, BDNF expression was significantly reduced in the model group compared with the normal group (P < 0.01). Flavonoid extraction was associated with a significant increase in BNDF content in the Huangqin group compared with the model group (P < 0.01).
By western blot, there was a significant decrease in BDNF expression at all time points in the model group compared with controls (P < 0.01; Figure 3C). By contrast, BDNF expression was significantly increased in the Huangqin group compared with the model group at all time points (P < 0.01).
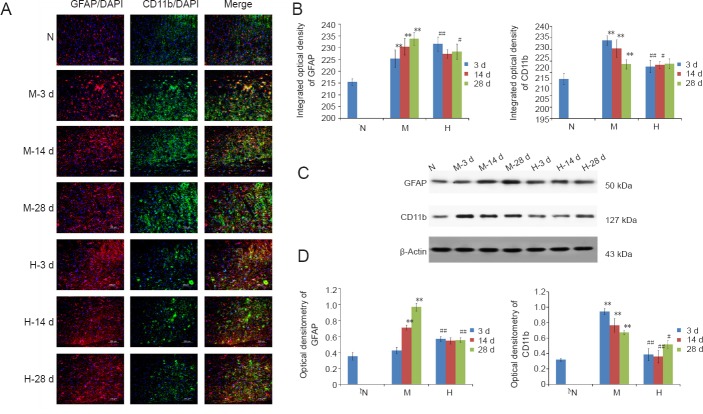
Flavonoid extraction increases microglial marker expression at the lesion site of SCI rats
Microglia labeled by CD11b are activated after injury and distributed closely around the injury site (Smith et al., 2012). There was a significant increase in CD11b staining in the model group compared with controls, which peaked at 3 days recovery, and then progressively decreased until 28 days (P < 0.01; Figure 4B). In the Huangqin group, CD11b staining was significantly less than that in the model group at 3 days after injury, but remained significantly higher than controls at 28 days (P < 0.01). Western blot data for CD11b expression showed a similar pattern (Figure 4D).
Figure 4.
Effect of Huangqin flavonoid extraction on the expression of glial fibrillary acidic protein (GFAP) and CD11b in astrocytes and microglia in the injured spinal cord of SCI rats.
(A) GFAP (DyLight 594, red) and CD11b (Dylight 488, green) expression with double-immunofluorescence labeling, and DAPI counterstaining, of the injured spinal cord at 3, 14 and 28 d of recovery in each group. (B) The integrated optical density of GFAP and CD11b double-immunofluorescence expression at 3, 14 and 28 d recovery in each group (n = 8 per group). Western blot results (C) and bar graphs (D) showing GFAP (50 kDa) and CD11b (127 kDa) expression at 3, 14 and 28 d of recovery in each group (n = 6 per group). Data are presented as the mean ± SD, and analyzed by one-way analysis of variance followed by the Student-Newman-Keuls post hoc test. **P < 0.01, vs. normal group; #P < 0.05, ##P < 0.01, vs. model group. N: Normal group; M: model group; H: Huangqin group; GFAP: glial fibrillary acidic protein; DAPI: 4′,6-diamidino-2-phenylindole; d: days.
Flavonoid extraction exerts bi-directional regulation of GFAP expression at the lesion site of SCI rats
GFAP expression in astrocytes is indicative of glial scar formation (Oberheim et al., 2009). Immunofluorescence studies showed a significant increase in GFAP staining surrounding the injury epicenter at 28 days after SCI in the model group (P < 0.01; Figure 4B). Western blot assay results confirmed these findings at 28 days (P < 0.01; Figure 4D). Interestingly, in the Huangqin group there was a significant increase in GFAP expression at 3 days after SCI compared with the model group, but which was significantly lower at 28 days after SCI (P < 0.05, P < 0.01, respectively; Figure 4). Thus, flavonoid extraction initially upregulated GFAP expression, and then down-regulated GFAP expression a few weeks later. These data suggest that flavonoid extraction can exert bi-directional regulation of GFAP expression after SCI, thereby maintaining GFAP at a relatively stable level.
Discussion
As the active ingredients and most studied flavonoids in Huangqin, baicalein, baicalin, wogonin and wogonoside have shown neuroprotective effects in multiple neurodegeneration diseases in vitro and in vivo (Chen et al., 2015a; Ding et al., 2015; Zhou et al., 2017), and via a range of mechanisms including scavenging peroxynitrite to reduce neurotoxicity (Xu et al., 2013b), ameliorating Aβ1–42 protein-related pathology and cognitive dysfunction (Chen et al., 2015a), modulating stress-responsive genes (Xu et al., 2015) and helping dorsal root ganglion neurons prevent tunicamycin induced endoplasmic reticulum stress (Chen et al., 2015b). Importantly, baicalin can pass through the blood-brain barrier and is detected in cerebrospinal fluid (Huang et al., 2008), and as such, is considered a novel and promising therapeutic agent for SCI.
Interestingly, using in vivo and in vitro experiments, Yune et al. (2009) reported that total flavonoid extraction of Huangqin produced better recovery of motor function after SCI compared with any specific flavonoid isolated from the herb. It should be noted that other flavonoids than baicalein, baicalin, wogonin and wogonoside, and other chemical components, may also provide synergistic neuroprotective actions (Wang et al., 2013; Gaire et al., 2014). As such, we utilized the flavonoid extraction for our study, rather than an individual flavonoid.
MP is a routine clinical therapy used in combination with surgery in the early stage of SCI (Bowers et al., 2016; Liu et al., 2017). Although its use remains controversial because of side effects, MP can inhibit lipid peroxidation, maintain the blood-spinal cord barrier, enhance spinal cord blow flow, inhibit endorphin release and limit the inflammatory response (Suberviola et al., 2008; Evaniew et al., 2015; Lu et al., 2016). In the present study, the Huangqin flavonoid extraction produced a similar in vivo effect on the morphology of spinal cord tissues, the BBB score and hematoxylin and eosin pathology to that observed with MP. However, further studies are required to determine the specific mechanisms of action.
Regulation of axonal regeneration
NF-H is an accepted marker of mature neuronal cells in the central nervous system. Under normal conditions, NF-H content in the cell body is low (Yang et al., 2018). After SCI, nerve cells in the lesion area are directly destroyed by the trauma, and show degeneration necrosis, structural damage, cell disruption and loss of responsiveness. However, neurons adjacent to the lesion area begin to synthesize NF-H, which is deposited in cell bodies (He and Nan, 2016; Yang et al., 2018).
Interestingly, the number of NF-H-positive neurons and the degree of NF-H staining on neuron cell bodies was strongly associated with functional recovery in the posterior limb (Wang et al., 2014; He and Nan, 2016). In the present study, we found a marked increase in NF-H levels in neuronal cell bodies after SCI, likely as a response to promote axonal regeneration. Further, administration of flavonoid extraction was associated with further upregulation the NF-H levels in the lesion area, and recovery of locomotor function, in SCI rats.
Regulation of BDNF content
BDNF is the most important neurotrophic factor in experimental SCI, and can promote neurogenesis, neuroprotection, axonal sprouting, myelination, adaptive synaptic plasticity and synaptic transmission (Kovalchuk et al., 2004; Hodgetts and Harvey, 2017). As such, a number of studies have shown that addition of exogenous BDNF, such as with gene delivery and transplant combined with cellular grafts, can promote motor recovery after SCI (Brock et al., 2010; Zhao et al., 2013; Ollivier-Lanvin et al., 2015).
In the present study, BDNF expression was decreased after SCI, as reported (Ying et al., 2008; Jung et al., 2016). Further, administration of flavonoid extraction was associated with a significant increase in BDNF expression, and an improvement in the BBB score and hematoxylin and eosin staining pathology, in the injured spinal cord.
Regulation of microglial activation
Uncontrolled microglial activation is thought to play an important pathogenic role in a range of neurodegenerative diseases. Activated microglia undergo hypertrophy and rapid proliferation, then migrate to inflammatory sites and produce neurotoxic and proinflammatory mediators that can injure neurons (Smith et al., 2012; Dursun et al., 2015; Li et al., 2016). Several studies have reported that baicalin and wogonin can reduce microglia activation in the central nervous system, via reduced expression of CD11b, suppressed phagocytosis (Xu et al., 2013a) and decreased production of proinflammatory cytokines (interleukin-6, tumor necrosis factor-α, inducible nitric oxide synthase and nitric oxide) and chemokines (Lee et al., 2003; Li et al., 2005; Xu et al., 2013a; Yeh et al., 2015). This was confirmed in vitro in primary microglia and the microglial BV2 cell line (Lee et al., 2003; Xu et al., 2013a; Yeh et al., 2015). In the present study, administration of flavonoid extraction also suppressed microglial activation, as indicated by reduced CD11b expression. However, the specific signaling pathways remain to be determined.
Proliferation of reactive astrocytes
There is increasing evidence for a role of astrocytes in blood-spinal cord barrier formation and maintenance of neuronal homeostasis (Oberheim et al., 2006; Oberheim et al., 2009). Astrocytes were also suggested to constitute an extra neuronal signaling system in the central nervous system, and play important roles in information processing during brain development, adulthood, aging and injury (Bazargani and Attwell, 2016).
In the present study, administration of flavonoid extraction increased GFAP expression at 3 days after SCI. In the primary lesion stage of SCI, the upregulation of GFAP provides beneficial support to the injured area, including maintenance of the blood-spinal cord barrier, secretion of cytokines such as interleukin-6, interleukin-10, interferon-b, tumor necrosis factor-a and monocyte chemotactic protein 1, prevention of excitotoxicity and modulation of synaptic transmission. Together with microglia, their immune responses play a ‘housekeeper’ role in the central nervous system (Radford et al., 2015; Sun et al., 2016).
In the secondary lesion stage, astrocytes become hypertrophic. The synthesis of a number of intermediate filaments (e.g., GFAP and vimentin) and proteoglycans are increased, and the glial scar is formed weeks after injury. This molecular and physical barrier isolates the injured area from adjacent normal tissue, which prevents re-establishing the integrity of the central nervous system (Silver and Miller, 2004; Gao et al., 2013; Yuan and He, 2013). Thus, reactive astrogliosis is considered an important therapeutic target for axonal regeneration (Zhang et al., 2007; Fitch and Silver, 2008). Importantly, in the present study, administration of flavonoid extraction significantly decreased GFAP expression at 28 days after SCI, suggestive of decreased glial scar formation and removal of the physical and molecular barrier for axonal regeneration.
Conclusion
The present study provides new evidence that Huangqin flavonoid extraction can promote recovery of locomotor function following SCI in rats. Further, this effect was associated with promotion of axonal regeneration, up-regulation of BDNF, suppression of microglia and bi-directional regulation of reactive astrocytes. Future studies are required to examine the specific signaling pathways underlying these protective effects.
Additional files:
Additional file 1 (342.4KB, pdf) : Chemical fingerprint of Huangqin flavonoids extraction.
Additional file 2 (190.1KB, pdf) : Identification and measurement of major constituents in Huangqin (Scutellaria baicalensis Georgi).
Additional file 3: Open peer review reports 1 (14KB, pdf) and 2 (20.7KB, pdf) .
Footnotes
Conflicts of interest: The authors declare no competing financial interests.
Financial support: This study was supported by the National Natural Science Foundation of China, No. 81403278 (to QZ); the Natural Science Foundation of Shaanxi Province of China, No. 2017JM8058 (to QZ); the Shaanxi Administration of Traditional Chinese Medicine in China, No. 15-ZY038 (to QZ). The funding bodies played no role in the study design, collection, analysis and interpretation of data, in the writing of the report, or in the decision to submit the paper for publication.
Institutional review board statement: The experiments were approved by the Animal Ethics Committee of College of Medicine, Xi’an Jiaotong University, China.
Copyright license agreement: The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement: Datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
Open peer reviewers: Mengliang Zhang, Lunds Universitet, Sweden; Syoichi Tashiro, Keio University School of Medicine, Japan.
Funding: This study was supported by the National Natural Science Foundation of China, No. 81403278 (to QZ); the Natural Science Foundation of Shaanxi Province of China, No. 2017JM8058 (to QZ); the Shaanxi Administration of Traditional Chinese Medicine in China, No. 15-ZY038 (to QZ).
P-Reviewer: Zhang M, Tashiro S; C-Editor: Zhao M; S-Editor: Yu J, Li CH; L-Editor: Qiu Y, Song LP; T-Editor: Liu XL
References
- 1.Allen AR. Surgery of experimental lesion of spinal cord equivalent to crush injury of fracture dislocation of spinal column. JAMA. 1911;57:878–880. [Google Scholar]
- 2.Basso DM, Beattie MS, Bresnahan JC. A sensitive and reliable locomotor rating scale for open field testing in rats. J Neurotrauma. 1995;12:1–21. doi: 10.1089/neu.1995.12.1. [DOI] [PubMed] [Google Scholar]
- 3.Bazargani N, Attwell D. Astrocyte calcium signaling: the third wave. Nat Neurosci. 2016;19:182–189. doi: 10.1038/nn.4201. [DOI] [PubMed] [Google Scholar]
- 4.Bowers CA, Kundu B, Hawryluk GW. Methylprednisolone for acute spinal cord injury: an increasingly philosophical debate. Neural Regen Res. 2016;11:882–885. doi: 10.4103/1673-5374.184450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brock JH, Rosenzweig ES, Blesch A, Moseanko R, Havton LA, Edgerton VR, Tuszynski MH. Local and remote growth factor effects after primate spinal cord injury. J Neurosci. 2010;30:9728–9737. doi: 10.1523/JNEUROSCI.1924-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen C, Li X, Gao P, Tu Y, Zhao M, Li J, Zhang S, Liang H. Baicalin attenuates alzheimer-like pathological changes and memory deficits induced by amyloid beta1-42 protein. Metab Brain Dis. 2015a;30:537–544. doi: 10.1007/s11011-014-9601-9. [DOI] [PubMed] [Google Scholar]
- 7.Chen F, Wu R, Zhu Z, Yin W, Xiong M, Sun J, Ni M, Cai G, Zhang X. Wogonin protects rat dorsal root ganglion neurons against tunicamycin-induced ER stress through the PERK-eIF2alpha-ATF4 signaling pathway. J Mol Neurosci. 2015b;55:995–1005. doi: 10.1007/s12031-014-0456-7. [DOI] [PubMed] [Google Scholar]
- 8.Cheng O, Li Z, Han Y, Jiang Q, Yan Y, Cheng K. Baicalin improved the spatial learning ability of global ischemia/reperfusion rats by reducing hippocampal apoptosis. Brain Res. 2012;1470:111–118. doi: 10.1016/j.brainres.2012.06.026. [DOI] [PubMed] [Google Scholar]
- 9.Colón JM, Miranda JD. Tamoxifen: an FDA approved drug with neuroprotective effects for spinal cord injury recovery. Neural Regen Res. 2016;11:1208–1211. doi: 10.4103/1673-5374.189164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ding H, Wang H, Zhao Y, Sun D, Zhai X. Protective effects of Baicalin on Abeta(1)(-)(4)(2)-induced learning and memory deficit, oxidative stress, and apoptosis in rat. Cell Mol Neurobiol. 2015;35:623–632. doi: 10.1007/s10571-015-0156-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Donnelly DJ, Popovich PG. Inflammation and its role in neuroprotection, axonal regeneration and functional recovery after spinal cord injury. Exp Neurol. 2008;209:378–388. doi: 10.1016/j.expneurol.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dursun E, Gezen-Ak D, Hanağası H, Bilgic B, Lohmann E, Ertan S, Atasoy IL, Alaylıoğlu M, Araz ÖS, Önal B, Gunduz A, Apaydin H, Kiziltan G, Ulutin T, Gurvit H, Yilmazer S. The interleukin 1 alpha, interleukin 1 beta, interleukin 6 and alpha-2-macroglobulin serum levels in patients with early or late onset Alzheimer's disease, mild cognitive impairment or Parkinson's disease. J Neuroimmunol. 2015;283:50–57. doi: 10.1016/j.jneuroim.2015.04.014. [DOI] [PubMed] [Google Scholar]
- 13.Evaniew N, Noonan VK, Fallah N, Kwon BK, Rivers CS, Ahn H, Bailey CS, Christie SD, Fourney DR, Hurlbert RJ, Linassi AG, Fehlings MG, Dvorak MF RHSCIR Network. Methylprednisolone for the treatment of patients with acute spinal cord injuries: a propensity score-matched cohort study from a Canadian multi-center spinal cord injury registry. J Neurotrauma. 2015;32:1674–1683. doi: 10.1089/neu.2015.3963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fitch MT, Silver J. CNS injury, glial scar, and inflammation: Inhibitory extracellular matrices and regeneration failure. Exp Neurol. 2008;209:294–301. doi: 10.1016/j.expneurol.2007.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gaire BP, Moon SK, Kim H. Scutellaria baicalensis in stroke management: nature's blessing in traditional Eastern medicine. Chin J Integr Med. 2014;20:712–720. doi: 10.1007/s11655-014-1347-9. [DOI] [PubMed] [Google Scholar]
- 16.Gao Z, Zhu Q, Zhang Y, Zhao Y, Cai L, Shields CB, Cai J. Reciprocal modulation between microglia and astrocyte in reactive gliosis following the CNS injury. Mol Neurobiol. 2013;48:690–701. doi: 10.1007/s12035-013-8460-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gasiorowski K, Lamer-Zarawska E, Leszek J, Parvathaneni K, Yendluri BB, Blach-Olszewska Z, Aliev G. Flavones from root of Scutellaria baicalensis Georgi: drugs of the future in neurodegeneration? CNS Neurol Disord Drug Targets. 2011;10:184–191. doi: 10.2174/187152711794480384. [DOI] [PubMed] [Google Scholar]
- 18.Hachem LD, Ahuja CS, Fehlings MG. Assessment and management of acute spinal cord injury: From point of injury to rehabilitation. J Spinal Cord Med. 2017;40:665–675. doi: 10.1080/10790268.2017.1329076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.He B, Nan G. Neuronal regeneration after acute spinal cord injury in adult rats. Spine J. 2016;16:1459–1467. doi: 10.1016/j.spinee.2016.06.020. [DOI] [PubMed] [Google Scholar]
- 20.Hodgetts SI, Harvey AR. Neurotrophic factors used to treat spinal cord injury. Vitam Horm. 2017;104:405–457. doi: 10.1016/bs.vh.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 21.Huang H, Zhang Y, Yang R, Tang X. Determination of baicalin in rat cerebrospinal fluid and blood using microdialysis coupled with ultra-performance liquid chromatography-tandem mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci. 2008;874:77–83. doi: 10.1016/j.jchromb.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 22.Jung SY, Seo TB, Kim DY. Treadmill exercise facilitates recovery of locomotor function through axonal regeneration following spinal cord injury in rats. J Exerc Rehabil. 2016;12:284–292. doi: 10.12965/jer.1632698.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kovalchuk Y, Holthoff K, Konnerth A. Neurotrophin action on a rapid timescale. Curr Opin Neurobiol. 2004;14:558–563. doi: 10.1016/j.conb.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 24.Lee H, Kim YO, Kim H, Kim SY, Noh HS, Kang SS, Cho GJ, Choi WS, Suk K. Flavonoid wogonin from medicinal herb is neuroprotective by inhibiting inflammatory activation of microglia. FASEB J. 2003;17:1943–1944. doi: 10.1096/fj.03-0057fje. [DOI] [PubMed] [Google Scholar]
- 25.Li C, Lin G, Zuo Z. Pharmacological effects and pharmacokinetics properties of Radix Scutellariae and its bioactive flavones. Biopharm Drug Dispos. 2011;32:427–445. doi: 10.1002/bdd.771. [DOI] [PubMed] [Google Scholar]
- 26.Li FQ, Wang T, Pei Z, Liu B, Hong JS. Inhibition of microglial activation by the herbal flavonoid baicalein attenuates inflammation-mediated degeneration of dopaminergic neurons. J Neural Transm (Vienna) 2005;112:331–347. doi: 10.1007/s00702-004-0213-0. [DOI] [PubMed] [Google Scholar]
- 27.Li JF, Yan JY, Xia RF, Zhang X, Tan XH, Guan J, Ye Z, Zhang SL. Glial scar formation and astrocyte role in spinal cord injury. Zhongguo Zuzhi Gongcheng Yanjiu. 2016;20:5609–5616. [Google Scholar]
- 28.Liu JT, Zhang S, Gu B, Li HN, Wang SY, Zhang SY. Methotrexate combined with methylprednisolone for the recovery of motor function and differential gene expression in rats with spinal cord injury. Neural Regen Res. 2017;12:1507–1518. doi: 10.4103/1673-5374.215263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lu GB, Niu FW, Zhang YC, Du L, Liang ZY, Gao Y, Yan TZ, Nie ZK, Gao K. Methylprednisolone promotes recovery of neurological function after spinal cord injury: association with Wnt/β-catenin signaling pathway activation. Neural Regen Res. 2016;11:1816–1823. doi: 10.4103/1673-5374.194753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Michailidou C, Marston L, De Souza LH, Sutherland I. A systematic review of the prevalence of musculoskeletal pain, back and low back pain in people with spinal cord injury. Disabil Rehabil. 2014;36:705–715. doi: 10.3109/09638288.2013.808708. [DOI] [PubMed] [Google Scholar]
- 31.Norden DM, Muccigrosso MM, Godbout JP. Microglial priming and enhanced reactivity to secondary insult in aging, and traumatic CNS injury, and neurodegenerative disease. Neuropharmacology. 2015;96:29–41. doi: 10.1016/j.neuropharm.2014.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oberheim NA, Wang X, Goldman S, Nedergaard M. Astrocytic complexity distinguishes the human brain. Trends Neurosci. 2006;29:547–553. doi: 10.1016/j.tins.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 33.Oberheim NA, Takano T, Han X, He W, Lin JH, Wang F, Xu Q, Wyatt JD, Pilcher W, Ojemann JG, Ransom BR, Goldman SA, Nedergaard M. Uniquely hominid features of adult human astrocytes. J Neurosci. 2009;29:3276–3287. doi: 10.1523/JNEUROSCI.4707-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ollivier-Lanvin K, Fischer I, Tom V, Houle JD, Lemay MA. Either brain-derived neurotrophic factor or neurotrophin-3 only neurotrophin-producing grafts promote locomotor recovery in untrained spinalized cats. Neurorehabil Neural Repair. 2015;29:90–100. doi: 10.1177/1545968314532834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Radford RA, Morsch M, Rayner SL, Cole NJ, Pountney DL, Chung RS. The established and emerging roles of astrocytes and microglia in amyotrophic lateral sclerosis and frontotemporal dementia. Front Cell Neurosci. 2015;9:414. doi: 10.3389/fncel.2015.00414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Silver J, Miller JH. Regeneration beyond the glial scar. Nat Rev Neurosci. 2004;5:146–156. doi: 10.1038/nrn1326. [DOI] [PubMed] [Google Scholar]
- 37.Singh A, Tetreault L, Kalsi-Ryan S, Nouri A, Fehlings MG. Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol. 2014;6:309–331. doi: 10.2147/CLEP.S68889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Smith JA, Das A, Ray SK, Banik NL. Role of pro-inflammatory cytokines released from microglia in neurodegenerative diseases. Brain Res Bull. 2012;87:10–20. doi: 10.1016/j.brainresbull.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Suberviola B, González-Castro A, Llorca J, Ortiz-Melón F, Miñambres E. Early complications of high-dose methylprednisolone in acute spinal cord injury patients. Injury. 2008;39:748–752. doi: 10.1016/j.injury.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 40.Sun H, Liang R, Yang B, Zhou Y, Liu M, Fang F, Ding J, Fan Y, Hu G. Aquaporin-4 mediates communication between astrocyte and microglia: Implications of neuroinflammation in experimental Parkinson's disease. Neuroscience. 2016;317:65–75. doi: 10.1016/j.neuroscience.2016.01.003. [DOI] [PubMed] [Google Scholar]
- 41.Wang LJ, Zhang RP, Li JD. Transplantation of neurotrophin-3-expressing bone mesenchymal stem cells improves recovery in a rat model of spinal cord injury. Acta Neurochir (Wien) 2014;156:1409–1418. doi: 10.1007/s00701-014-2089-6. [DOI] [PubMed] [Google Scholar]
- 42.Wang R, Shen X, Xing E, Guan L, Xin L. Scutellaria baicalensis stem-leaf total flavonoid reduces neuronal apoptosis induced by amyloid beta-peptide (25-35) Neural Regen Res. 2013;8:1081–1090. doi: 10.3969/j.issn.1673-5374.2013.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xu J, Zhang Y, Xiao Y, Ma S, Liu Q, Dang S, Jin M, Shi Y, Wan B, Zhang Y. Inhibition of 12/15-lipoxygenase by baicalein induces microglia PPARbeta/delta: a potential therapeutic role for CNS autoimmune disease. Cell Death Dis. 2013a;4:e569. doi: 10.1038/cddis.2013.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xu M, Chen X, Gu Y, Peng T, Yang D, Chang RC, So KF, Liu K, Shen J. Baicalin can scavenge peroxynitrite and ameliorate endogenous peroxynitrite-mediated neurotoxicity in cerebral ischemia-reperfusion injury. J Ethnopharmacol. 2013b;150:116–124. doi: 10.1016/j.jep.2013.08.020. [DOI] [PubMed] [Google Scholar]
- 45.Xu S, Zhao X, Zhao Q, Zheng Q, Fang Z, Yang X, Wang H, Liu P, Xu H. Wogonin prevents rat dorsal root ganglion neurons death via inhibiting tunicamycin-induced ER stress in vitro. Cell Mol Neurobiol. 2015;35:389–398. doi: 10.1007/s10571-014-0134-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yang Z, Bramlett HM, Moghieb A, Yu D, Wang P, Lin F, Bauer C, Selig TM, Jaalouk E, Weissman AS, Rathore DS, Romo P, Zhang Z, Hayes RL, Wang MY, Dietrich WD, Wang KKW. Temporal profile and severity correlation of a panel of rat spinal cord injury protein biomarkers. Mol Neurobiol. 2018;55:2174–2184. doi: 10.1007/s12035-017-0424-7. [DOI] [PubMed] [Google Scholar]
- 47.Yeh CH, Shih HC, Hong HM, Lee SS, Yang ML, Chen CJ, Kuan YH. Protective effect of wogonin on proinflammatory cytokine generation via Jak1/3-STAT1/3 pathway in lipopolysaccharide stimulated BV2 microglial cells. Toxicol Ind Health. 2015;31:960–966. doi: 10.1177/0748233713485886. [DOI] [PubMed] [Google Scholar]
- 48.Ying Z, Roy RR, Zhong H, Zdunowski S, Edgerton VR, Gomez-Pinilla F. BDNF-exercise interactions in the recovery of symmetrical stepping after a cervical hemisection in rats. Neuroscience. 2008;155:1070–1078. doi: 10.1016/j.neuroscience.2008.06.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yuan YM, He C. The glial scar in spinal cord injury and repair. Neurosci Bull. 2013;29:421–435. doi: 10.1007/s12264-013-1358-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yune TY, Lee JY, Cui CM, Kim HC, Oh TH. Neuroprotective effect of Scutellaria baicalensis on spinal cord injury in rats. J Neurochem. 2009;110:1276–1287. doi: 10.1111/j.1471-4159.2009.06214.x. [DOI] [PubMed] [Google Scholar]
- 51.Zhang L, Zhang WP, Chen KD, Qian XD, Fang SH, Wei EQ. Caffeic acid attenuates neuronal damage, astrogliosis and glial scar formation in mouse brain with cryoinjury. Life Sci. 2007;80:530–537. doi: 10.1016/j.lfs.2006.09.039. [DOI] [PubMed] [Google Scholar]
- 52.Zhao T, Yan W, Xu K, Qi Y, Dai X, Shi Z. Combined treatment with platelet-rich plasma and brain-derived neurotrophic factor-overexpressing bone marrow stromal cells supports axonal remyelination in a rat spinal cord hemi-section model. Cytotherapy. 2013;15:792–804. doi: 10.1016/j.jcyt.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 53.Zhou ZQ, Li YL, Ao ZB, Wen ZL, Chen QW, Huang ZG, Xiao B, Yan XH. Baicalin protects neonatal rat brains against hypoxic-ischemic injury by upregulating glutamate transporter 1 via the phosphoinositide 3-kinase/protein kinase B signaling pathway. Neural Regen Res. 2017;12:1625–1631. doi: 10.4103/1673-5374.217335. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Chemical fingerprint of huangqin flavonoids extraction
Identification and measurement of major constituents in huangqin