Abstract
Background and Objectives
Lower-body muscular power and movement velocity (MV) are associated with balance and physical function. The Tendo power analyzer (Tendo) is a portable device that calculates functional lower body power (FLBP) and MV. This reliable (Cronbach’s α = .98) method is validated against motion capture analysis of functional lower body sit-to-stand power and velocity (r = .76). However, the Tendo has not been utilized in discrimination or prediction of falls. We determined the discriminant validity of FLBP and MV among older adults based on the history of falls. These results lay the framework for longitudinal research in FLBP and MV in fall prediction/prevention.
Research Design and Methods
Cross-sectional investigation examining differences between FLBP and MV during 5 sit-to-stands of 98 community-dwelling older adults (aged 77.5 years, 61% female) classified by the history of fall (no = 59, yes = 39). Participants completed 5 consecutive sit-to-stands (60-second rest between each) with FLBP and MV measured by the Tendo. Multivariate analysis of variance modeling determined between-group differences in functional lower body sit-to-stand average velocity, peak velocity, relative average power, and relative peak power. Binary and forward conditional logistic regression models determined the ability of each measure to discriminate fall history.
Results
FLBP and MV were significantly lower in older adults with a fall history (p < .05). Relative average power and peak power were 15% and 16% lower and average and peak velocity were 18% and 14% slower, respectively among fallers. Logistic regression indicated average velocity was the best discriminator of fall history (p < .05).
Discussion and Implications
The Tendo detects differences in FLBP and MV during a sit-to-stand while discriminating fall history. Future longitudinal studies should determine efficacy in fall prediction and applicability toward clinically relevant interventions for fall prevention.
Keywords: Clinical practice, Function/mobility, Assessment, Muscle performance, Chair stand
Translational Significance: This pilot study lays the framework for the clinical use of a portable device to measure functional lower body power and velocity, which are essential in preventing falls.
One in three adults over the age of 65 experiences a fall annually, increasing to one in two after the age of 80 (1). With the exponential increase in the older adult population and the associated health care costs and ramifications, researchers and health care professionals are tasked with the development of assessments and intervention strategies to predict and prevent falls (2).
To determine proper prevention strategies, it is first important to understand the major risk factors associated with falls in older adults. Traditionally, physical risk factors associated with falling include decreased muscular strength, limitations in functional mobility, and decreased balance (3,4). Specifically regarding balance, adequate force and velocity are necessary to prevent a slip, trip, or fall (5). As a result, muscle power and more recently, velocity of movement, are considered better predictors of functional mobility than traditional measures of muscular strength and more recent studies have highlighted the stronger relationships of movement velocity (MV) to functional mobility and balance (3,6,7).
Traditional clinical assessment tools, such as sit-to-stand tests, the Berg Balance Scale, Functional Reach, or Dynamic Gait Index, are validated to quantify balance, mobility, and fall risk but are limited by ceiling effects. Additionally, none of the aforementioned clinical assessments quantify functional power or MV; neuromuscular attributes necessary to prevent a fall (8). As a result, there is a need to develop clinically applicable measures to quantify functional lower body power (FLBP) and MV in relation to falls.
Few studies have investigated power and MV among community-dwelling older adults with a history of falls. In regards to muscular power, seated knee extension power is lower in older women with a history of falls (9) and maximal sit-to-stand power analyzed with a force plate is discriminatory of fall history among older adults (10). In regards to velocity, the seated MV of the upper and lower extremities and trunk is significantly slower among high-functioning older adults with a history of falls compared to individuals without (11). Of additional interest, although velocity was slower among individuals with a history of falls, other measures related to falls (falls efficacy, maximum gait speed, and timed up and go) were not significantly different between groups; further supporting the importance of MV in fall risk, especially among higher functioning or community-dwelling older adults. Additionally, MV and muscular power are more discriminant than postural sway among older adults with functional impairments. Among nursing home residents with a history of falls, power measured through a force platform and MV measured by a linear transducer during a sit-to-stand task were 50% lower among individuals with a history of falls yet there were no differences in postural sway (12). These studies highlight the need for investigation of the unique relationship of functional (sit-to-stand) power and MV in relation to falls among older adults.
As previously mentioned, researchers and health care professionals are tasked with developing assessment and intervention strategies to better predict and prevent falls due to the ramifications of a fall on the individual and public (2). Although the few studies on power and velocity among older adults with a history of falls or with fall risk are promising, there are barriers to current state-of-the-art measurements of power and velocity. The few tools used to measure muscular power and MV (ie, Nottingham Power Rig, isokinetic dynamometer, leg press) are not portable and measure power and velocity in a seated, nonfunctional position (6,9,11). Furthermore, while force plates have been utilized to measure sit-so-stand performance, extensive data management and technical expertise are necessary to obtain accurate values. Hence, there is a significant need for methods evaluating power and MV during functional tasks in relation to prediction and prevention of falls that are portable and provide immediate results.
The Tendo Weightlifting Analyzer (Tendo; Trencin, Slovac Republic; Figures 1–3) is a validated tool used to measure FLBP and MV during a sit-to-stand task (13,14). This method of measuring lower-body functional power is highly correlated (r = .76) to changes in center of mass as assessed with 2D motion capture (Vicon Peak Motus) and test–retest reliability is high (Cronbach’s α = .98) between repeated chair stands (14). Additionally, muscular power measured with Tendo is positively associated with functional mobility performance among older adults (15). More importantly, Tendo is highly functional and portable compared with traditional methods of measuring muscular power and velocity and provides an instantaneous output of power and velocity results. Based on its functionality, portability, and immediate data output, Tendo is well primed for investigations into the longitudinal ability to predict falls in at-risk older adults. However, before this novel technique can be used longitudinally to evaluate the efficacy of assessment and prediction of fall risk, it is necessary to first determine the Tendo’s baseline utility to discern differences among FLBP and MV during a sit-to-stand task and its initial ability to properly discriminate between current fallers and nonfallers. The ability to successfully measure and delineate individual baseline differences in FLBP and MV is critical if future investigations are to properly model and evaluate long-term efficacy with regard to fall risk and prevention. As such, the purpose of this investigation was (i) to determine the ability of a clinically practical assessment tool (Tendo) to differentiate functional lower body muscular power and velocity during a sit-to-stand among older adults with and without a history of falls and (ii) to evaluate Tendo’s ability to accurately discriminate fall history among older adults. The results of this investigation will allow for longitudinal investigations utilizing Tendo to successfully model, predict, and prevent falls in aging individuals.
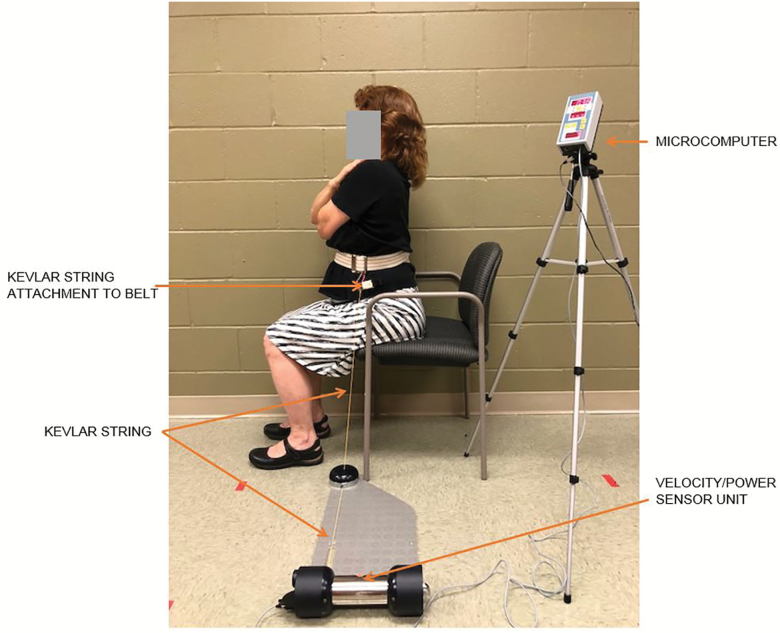
Figure 1.
Part 1 of assessment—seated set-up for using Tendo to measure movement velocity and power.
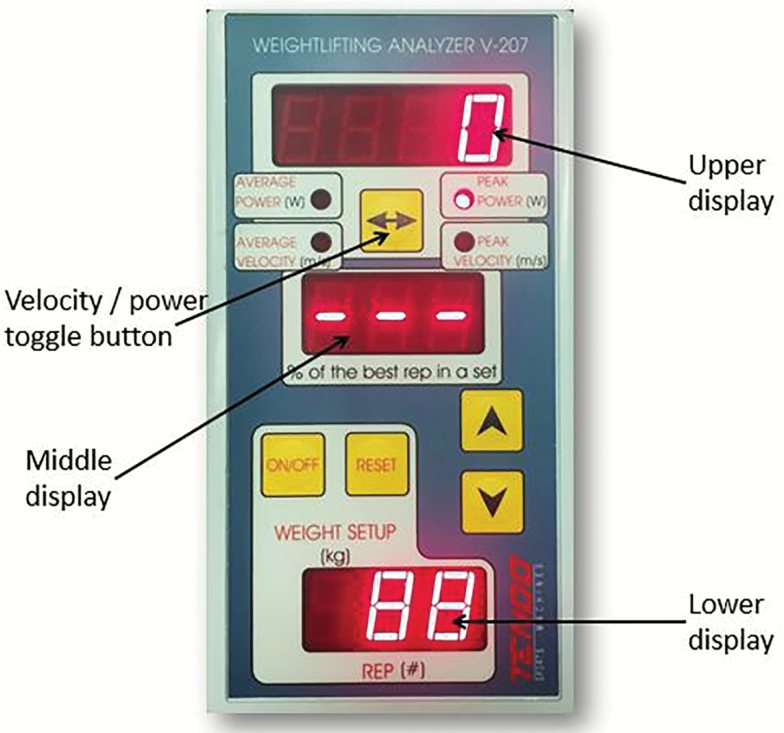
Figure 3.
Tendo microcomputer.
Research Design and Methods
Study Design
The University Institutional Review Board approved all measures and procedures associated with this project, and informed consent was obtained from all participants before testing. This study employed a cross-sectional, between-subjects analysis. Subjects were evaluated on average/peak relative (to body weight) power, and average/peak velocity during a sit-to-stand task. Differences and discriminatory ability of the variables were analyzed.
Participants
Participants (n = 98; males = 36, females = 62) were recruited via flyers placed in adult wellness centers, independent living facilities, and word of mouth. Fifty-nine participants reported no falls within the previous year while 39 reported experiencing at least one fall in the previous year. Inclusion criteria were over the age of 65 years, able to execute an informed consent, and able to complete a chair stand without upper extremity support. Subjects also completed a Mini-Mental State Exam and health and fall history questionnaire to screen for inclusion and exclusion criteria (described later). Height and weight were measured using a Detecto Physician’s Scale (Webb City, MO); measurements were recorded to the nearest 0.1 cm and 0.1 kg, respectively. Subjects also completed the sit-to-stand power and velocity assessment measured with Tendo (described in detail later).
Measures
Health and fall history questionnaire
All subjects completed the Mini-Mental State Exam to screen for cognitive impairment. A score of ≤23/30 resulted in exclusion from the study (16). Subjects also completed a health and fall history questionnaire to prescreen for exclusion criteria such as unstable diabetes, neurologic issues, cardiovascular disease, or hypertension and identify confounders. Potential confounders associated with falls recorded included hypertension, osteoarthritis, cardiac issues, cerebrovascular accidents, and number of medications. Polypharmacy was defined as taking five or more medications (17). As in prior studies, a history of a fall was defined by self-report of inadvertently coming to rest on a lower object within the prior 12 months (18).
FLBP and velocity
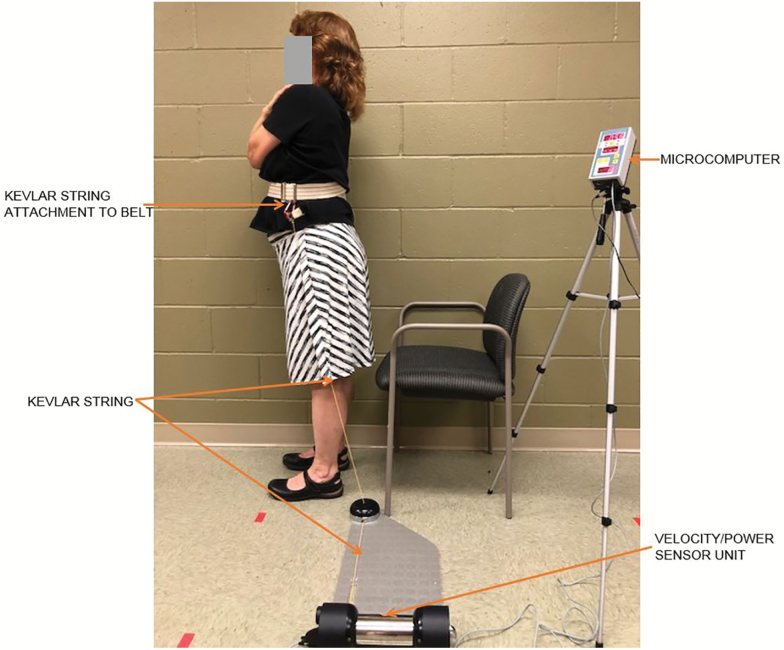
FLBP and MV achieved during a sit-to-stand were analyzed using the Tendo Weightlifting Analyzer (Trencin, Slovac Republic) as previously described (13–15,19). Briefly, this method has been validated against motion capture analysis to measure functional sit-to-stand power and velocity of the lower extremities (13–15,19). Participant’s weight (kg) was entered into the Tendo software to enable appropriate power calculations. The Tendo was attached with the Kevlar string in the sagittal plane on a belt secured around the waist. Starting from the seated position with arms across the chest (Figure 1), participants stood up as quickly and safely as possible (Figure 2) before returning to the initial seated position. As the participant stood the Kevlar string of the Tendo was pulled, measuring linear displacement and time (14). As previously described (19), five repetitions were recorded with 60 seconds rest provided between each repetition. Average/peak power (W) and velocity (m/s) for each stand were recorded from the microcomputer (Figure 3). The recorded power is calculated by the software relatively by utilizing the vertical velocity along with the mass moved (body mass in kg) and time to perform the movement. Relative average power was calculated as the mean power generated among all five repetitions. Relative peak power was considered the highest power output achieved among all repetitions. Average velocity was calculated as the mean velocity generated among all five repetitions. Peak velocity was considered the highest velocity achieved of the five repetitions. Tendo is a reliable and valid measure of lower extremity power in adults (14). When compared with motion capture analysis, sit-to-stand muscular power is highly correlated (r = .76), and Cronbach’s alpha is .98 for repeated measures (14).
Figure 2.
Part 2 of assessment—participant stand while using Tendo to measure movement velocity and power.
Statistical Analyses
Statistical Package for the Social Sciences (20) was used to conduct all analyses. Normal distribution of data was assessed using box plots, and homogeneity of variance was analyzed with Levene’s test. Descriptive statistics were calculated for subject demographics and sit-to-stand lower-body power and velocity variables. Frequencies were calculated for medical history variables. Chi-square was employed to analyze differences by sex in velocity and power measures as well as differences in confounders between groups based on fall history. One-way analysis of variance (ANOVA) was utilized to determine if there were differences in age, height, weight, or body mass index between participants with and without a history of falls. Multivariate analysis of variance (MANOVA) modeling was utilized to determine between group (fall history vs no fall history) differences in sit-to-stand average velocity, peak velocity, relative average power, and relative peak power. Separate binary logistic regression models were conducted to determine the ability of each measure (peak velocity, average velocity, relative average power, and relative peak power) to discriminate fall history. Forward conditional logistic regression models were conducted to ascertain which variables were the best discriminators of fall history when considered together. Post hoc effect size (Cohen’s d), sensitivity and specificity, and statistical power were calculated. Statistical significance was set as α <.05 for all analyses. Data are presented as mean (SD).
Results
This study included 98 community-dwelling older adults (61% female) classified into two groups based on the history of a fall in the previous year (no falls = 59, fall history = 39). Participant age, on average, was 77.5 (7.3) years old, ranging from 65 to 92 years of age. Forty percent of the entire sample had a history of a fall in the previous year. Model assumptions were met. Chi-square indicated there were no differences by sex in fall history, MV, or relative muscular power measures (p > .05). There were no differences between groups delineated by fall history in prevalence of hypertension, cardiac issues, stroke, osteoarthritis, or polypharmacy (p > .05, Table 1). Due to no baseline differences in potential confounders, all subjects were analyzed together, and no variables were entered as covariates in analyses. MANOVA analysis revealed a significant effect of group (falls vs no falls) for all FLBP and velocity variables [Wilk’s Λ = .90, F(4, 93) = 2.59, p = .04]. Post hoc statistical power was 0.71 for the dependent variables. Follow-up univariate ANOVA results are described later.
Table 1.
Demographics and Medical History Based on Fall History
| Variable | No Falls (n = 59) | Fall History (n = 39) | p Value |
|---|---|---|---|
| Age (years) | 77.8 (6.8) | 77.1 (8.0) | .67 |
| Height (cm) | 164.3 (15.8) | 161.1 (19.5) | .38 |
| Weight (kg) | 77.0 (15.5) | 73.9 (18.9) | .39 |
| Hypertension, n (%) | 32 (54%) | 25 (64%) | .33 |
| Body mass index | 27.62 (4.86) | 27.51 (5.35) | .92 |
| Cardiac issues, n (%) | 22 (37%) | 13 (33%) | .69 |
| Stroke, n (%) | 4 (7%) | 4 (10%) | .54 |
| Osteoarthritis, n (%) | 35 (59%) | 19 (49%) | .30 |
| Polypharmacy, n (%) | 19 (33%) | 19 (49%) | .11 |
Note: No significant differences between groups on all measures.
Power
ANOVA revealed relative average power during the chair stand was 16% (0.77 W/kg) lower among individuals with a positive fall history [F(1, 97) = 6.64, p = .011]. Sensitivity and specificity were 72% and 52%, respectively, in discriminating fall history. Relative peak power was 15% (1.10 W/kg) lower among individuals with a history of falls [F(1, 97) = 6.22, p = .014; Table 2] with similar sensitivity (72%) and slightly higher specificity (59%). Effect sizes for both average and peak power were moderate, d = 0.52 and 0.50, respectively. Logistic regression analyses indicated relative average power [χ2(1) = 6.34, B = −0.38, odds ratio [OR] = 0.69 (95% CI = 0.51–0.93), p = .012] and relative peak power [χ2(1) = 6.17, B = −0.25, OR = 0.78 (95% CI = 0.63–0.96), p = .013] both discriminated fall history.
Table 2.
Sit-to-Stand Power and Velocity Measures
| Tendo measurement | No Falls (n = 59) | Falls (n = 39) | Effect Size (d) | p Value |
|---|---|---|---|---|
| Relative average power (W/kg) | 4.83 (1.54), CI {4.46–5.20} | 4.06 (1.27), CI {3.61–4.52} | 0.52 | .011* |
| Relative peak power (W/kg) | 7.32 (2.24), CI {6.77–7.86} | 6.22 (1.92), CI {5.55–6.90} | 0.50 | .014* |
| Average velocity (m/s) | 0.50 (0.16), CI {0.46–0.53} | 0.41 (0.13), CI {0.37–0.46} | 0.60 | .007* |
| Peak velocity (m/s) | 0.74 (0.23), CI {0.69–0.80} | 0.64 (0.20), CI {0.57–0.71} | 0.45 | .017* |
Note: All data are expressed as mean (SD). CI {95 % confidence interval}. Asterisks indicate a significant difference between groups, (p < .05).
Velocity
ANOVA indicated average velocity was significantly different between groups based on fall history [F(1, 97) = 7.47, p = .007]. Individuals who experienced at least one fall within the previous year were 18% (0.09 m/s) slower in the average MV during the sit-to-stand task. Sensitivity and specificity of 72% and 52%, respectively were noted for fall discrimination. Similarly, peak velocity was significantly slower [14%; F(1, 97) = 5.92, p = .017) among individuals suffering from previous falls (Table 2) and sensitivity and specificity were marginally higher (77% and 54%, respectively). Effect sizes for both average and peak velocity were moderate, d = 0.60 and 0.45, respectively. Logistic regression analyses indicated average velocity was a significant independent discriminator of fall history [χ2(1) = 7.29, B = −3.91, OR = 0.02 (95% CI = 0.001–0.39), p = .007] as was peak velocity [χ2(1) = 5.85, B = −2.37, OR = 0.09 (95% CI = 0.01–0.69), p = .017]. Parameter estimates and ORs were the greatest among average velocity, indicating a much lower likelihood of having a history of a fall among subjects who achieved a higher average velocity of movement across five chair stands.
Forward conditional stepwise logistic regression was employed to determine which sit-to-stand measure best discriminated fall history. Results indicated that average velocity was the only significant discriminator variable in the full model [χ2(1) = 9.73, p = .002].
Discussion and Implications
The purpose of this investigation was (i) to determine the ability of a clinically practical assessment tool (Tendo) to differentiate FLBP and velocity during a sit-to-stand among older adults with and without a history of falls and (ii) to evaluate Tendo’s ability to accurately discriminate fall history among older adults. This investigation was conducted to determine the baseline efficacy of the sit-to-stand technique as measured by Tendo with regards to differentiating lower-body muscular power, MV, and fall history among older adults to design future, longitudinal investigations on fall prediction and prevention. We found that all FLBP and MV measures achieved during a sit-to-stand were significantly lower among older adults with a history of falls and each measure (average velocity, peak velocity, relative average power, and relative peak power) significantly discriminated fall history in individual models (when combined, average velocity was the only significant discriminator of fall history). Although this was not a prospective study, sensitivities and specificities for all measures were in line with other functional measures of fall risk in the literature (8). Sensitivity to accurately classify people with a fall history was moderate (72%–77%), while specificity to rule out a history of a fall was poor (52%–59%) (8). The most protective factor against having a fall history was average velocity; older adults who achieved a faster average velocity of movement across five sit-so-stands had the lowest odds (0.02) of having a history of fall (21). Interestingly, other known fall risk factors, such as polypharmacy or cardiac issues (1) were not different between groups in this investigation. These results signify the importance and utility of FLBP and MV in potential fall prediction and prevention and warranting prospective and interventional investigations.
Power, the product of force and velocity, is an important determinant of functional mobility among older adults (7). Seated knee extension power is lower in older women with a history of falls (9) and maximal sit-to-stand power analyzed with a force plate is discriminatory of fall history among older adults (10). In our investigation, we found that both relative peak and average muscular power measured with the Tendo during a sit-to-stand are discriminatory of fall history among older adults. Differences in both relative average and peak power between older adults with and without a fall history were 16% and 15%, respectively. Although we did not test the effects of an intervention, differences are notably in line with substantial clinically meaningful improvement (18%) for lower extremity extensor power measured with a bilateral leg press among mobility-limited older adults (22).
MV is a critical, independent component of power and independently related to functional performance and mobility limitations among older adults (7,13,23). Furthermore, quick movements are essential in preventing a trip, slip, or fall (5). We found that peak and average velocity were significantly slower in individuals with a history of falls and average velocity was the most significant discriminator of fall history based on results from a stepwise logistic regression analysis. Individuals with a fall history had 14% (0.10 m/s) slower peak and 18% (0.09 m/s) slower average velocity during the sit-to-stand. Importantly, average velocity yielded the greatest differences between groups based on fall history. Although this was not an intervention, it is notable that differences between groups are consistent with substantial clinical improvement [15% (0.05 m/s)] established from a prior study analyzing lower extremity power and velocity during a bilateral leg press (22).
There is a dearth of information on the relationship between MV and falls. Although we only found two previous publications relating to this concept, the results of both investigations support the current findings that power and MV are lower among people with increased fall risk or history of falls. However, prior studies yielded varying magnitudes of differences. Álvarez-Barbosa and colleagues (12) found that nursing home residents over the age of 80 years at risk of falls had 50% lower power and slower MV during the 30-second chair stand but no differences in postural sway (12). Comparatively, power and velocity ranged between 14% and 18% lower in our study among people with a history of falls. Differences in results are likely due to the dissimilar sample populations and group stratifications. We studied community-dwelling older adults aged 65 and older and stratified groups by fall history whereas Álvarez-Barbosa and colleagues (12) studied nursing home residents over the age of 80 stratified by fall risk. Taken together, these data imply that there may be greater discrepancies in MV with advancing age and further research is needed to evaluate this concept.
In another related investigation, Iwata and colleagues (11) analyzed seated MV of the upper and lower extremities and trunk among 112 high-functioning older adults, of which 28 had a history of falls. Despite differences in measurement methodologies and magnitudes, results were similar to our investigation. MV of the lower extremities and trunk were 6% and 8%, respectively, significantly slower among older adults with a fall history (11). Comparatively, we found MV was 14%–18% slower among people with a fall history. Of additional interest, both studies found no differences in other measures traditionally related to fall risk. We found no differences between groups on polypharmacy or cardiac disease and Iwata and colleagues (11) found falls efficacy, maximum gait speed, and timed up and go were not significantly different between groups. These findings further support the notion that traditional measures of fall risk may not be sufficient for discriminating functional performance differences among higher-level older adults.
Based on the previous investigations and our current results, it can be postulated that the older adults in our investigation had a history of falls due to lower functional power and slower MV (24). Quick, powerful movements are necessary to stop a trip or a slip from becoming a fall (5). The clinical implications of these data suggest targeted training should be conducted for older adults at risk of falls and/or with decreased MV and power. Research supports power training and high-velocity training as an effective means to improve physical function among older adults (25,26). Conversely, few studies evaluate the role of muscular power, and high-velocity training in falls and exercise programs are often implemented using machines rather functional or transitional movements (27). The InVEST pilot study found promising results that velocity specific mobility exercises with a weighted vest improved leg power, balance, and mobility among community-dwelling older women (28). However, to our knowledge, similar studies have not been conducted investigating the role of functional power and velocity training in fall prevention.
This cross-sectional study does have limitations. First, Tendo captures lower-limb muscular power and MV through the Kevlar string attached to a belt around the participant’s waist on one side. There potentially may be a small amount of resistance provided through this movement on one side of the body, which may change the mechanics of the sit-to-stand. Further studies are necessary to determine this impact, if any. Second, the nature of a cross-sectional study relies on the one-time performance of a task and is a “snapshot” of an individuals’ abilities at that day and time; however, collecting these baseline data were a necessary step to develop future investigations evaluating long-term fall risk and prediction. Third, participant grouping was based on self-report of falls, which may have been inaccurate or unreliable with regards to participant recall or willingness to report a prior fall. Finally, while our sample size was adequate for this investigation, it consisted of community-dwelling older adults who could perform a chair stand without upper extremity support; therefore, results may not be generalizable to other populations with underlying conditions or diseases.
Conclusion
This study supports the importance and independent role functional MV may play in fall prediction and possibly prevention, especially among higher functioning or community-dwelling older adults. Results also support the clinical utility of assessment of functional MV and need for future studies on the impact interventions to improve functional power and/or MV may have on falls in older adults. The data from this investigation confirm Tendo’s utility to successfully measure differences in power and velocity achieved during a sit-to-stand and discriminate fall history among older adults. Compared with seated isokinetic machines, leg presses, and the Nottingham Power Rig, the Tendo is a more portable, functional tool which is also validated in measuring sit-to-stand lower extremity power and MV. With this concept established, future investigations can utilize this technique to determine if interventions resulting in clinical changes in power or MV measured during a sit-to-stand impact function or prevent future falls. This study also lays the framework for longitudinal studies to develop more robust prediction models for fall risk. Our findings suggest functional MV has important implications for researchers and clinicians in the public health issue of falls in older adults. In addition to our lab’s direction for pursuing fall risk prediction, future studies should investigate the sensitivity and specificity of MV and power in predicting prospective falls compared with other gold standard measures of fall prediction.
Funding
None reported.
Acknowledgments
The authors would like to thank Stephanie Gray Chunn, the Rogers Adult Wellness Center staff, and Butterfield Trail Village fitness staff for their support during the conduct of this research.
Consent for Publication
Written informed consent for publication of the clinical image was obtained from the patient. A copy of the consent form is available for review by the Editor of this journal.
Conflict of Interest
None reported.
References
- 1. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75:51–61. doi: 10.1016/j.maturitas.2013.02.009 [DOI] [PubMed] [Google Scholar]
- 2. Houry D, Florence C, Baldwin G, Stevens J, McClure R. The CDC injury center’s response to the growing public health problem of falls among older adults. Am J Lifestyle Med. 2016;10:74–77. doi: 10.1177/1559827615600137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ward RE, Beauchamp MK, Latham NK, et al. Neuromuscular impairments contributing to persistently poor and declining lower-extremity mobility among older adults: new findings informing geriatric rehabilitation. Arch Phys Med Rehabil. 2016;97:1316–1322. doi: 10.1016/j.apmr.2016.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(Suppl. 2):ii37–ii41. doi: 10.1093/ageing/afl084 [DOI] [PubMed] [Google Scholar]
- 5. Bhatt T, Yang F, Pai Y. Learning to resist gait-slip falls: long-term retention in community-dwelling older adults. Arch Phys Med Rehabil. 2012;93:557–564. doi: 10.1016/j.apmr.2011.10.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Byrne C, Faure C, Keene DJ, Lamb SE. Ageing, muscle power and physical function: a systematic review and implications for pragmatic training interventions. J Sports Med. 2016;46:1311–1332. doi: 10.1097/jes.0b013e31823b5f13 [DOI] [PubMed] [Google Scholar]
- 7. Reid KF, Fielding RA. Skeletal muscle power: a critical determinant of physical functioning in older adults. Exerc Sport Sci Rev. 2012;40:4–12. doi: 10.1097/JES.0b013e31823b5f13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lusardi MM, Fritz S, Middleton A, et al. Determining risk of falls in community dwelling older adults: a systematic review and meta-analysis using posttest probability. J Geriatr Phys Ther. 2017;40:1–36. doi: 10.1519/jpt.0000000000000099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Crozara LF, Morcelli MH, Hallal CZ, et al. Effect of age and fall status on lower-extremity muscle activation and joint torque and power in physically active women. Isokinet Exerc Sci. 2016;24:67–77. doi: 10.3233/ies-150602 [DOI] [Google Scholar]
- 10. Cheng Y, Wei S, Chen P, et al. Can sit-to-stand lower limb muscle power predict fall status?Gait Posture. 2014;40:403–407. doi: 10.1016/j.gaitpost.2014.05.064 [DOI] [PubMed] [Google Scholar]
- 11. Iwata A, Higuchi Y, Sano Y, et al. Movement velocity is a sensitive risk factor of falls in high-functioning older adults. J Am Geriatr Soc. 2014;62:1595–1596. doi: 10.1111/jgs.12959 [DOI] [PubMed] [Google Scholar]
- 12. Álvarez Barbosa F, Pozo‐Cruz B, Pozo‐Cruz J, Alfonso‐Rosa RM, Sanudo Corrales B, Rogers ME. Factors associated with the risk of falls of nursing home residents aged 80 or older. Rehabil Nurs. 2016;41:16–25. doi: 10.1002/rnj.229 [DOI] [PubMed] [Google Scholar]
- 13. Glenn JM, Gray M, Vincenzo J, Paulson S, Powers M. An evaluation of functional sit-to-stand power in cohorts of healthy adults aged 18–97 years. J Aging Phys Act. 2017;25:305–310. doi: 10.1123/japa.2016-0031 [DOI] [PubMed] [Google Scholar]
- 14. Gray M, Paulson S. Developing a measure of muscular power during a functional task for older adults. BMC Geriatr. 2014;14:145–150. doi: 10.1186/1471-2318-14-145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Glenn JM, Gray M, Binns A. Relationship of sit-to-stand lower-body power with functional fitness measures among older adults with and without sarcopenia. J Geriatr Phys Ther. 2017;40:42–50. doi: 10.1519/jpt.0000000000000072 [DOI] [PubMed] [Google Scholar]
- 16. Herman T, Mirelman A, Giladi N, Schweiger A, Hausdorff JM. Executive control deficits as a prodrome to falls in healthy older adults: a prospective study linking thinking, walking, and falling. J Gerontol A Biol Sci Med Sci. 2010;65:1086–1092. doi: 10.1093/gerona/glq077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gnjidic D, Hilmer SN, Blyth FM, et al. Polypharmacy cutoff and outcomes: five or more medicines were used to identify community-dwelling older men at risk of different adverse outcomes. J Clin Epidemiol. 2012;65:989–995. doi: 10.1016/j.jclinepi.2012.02.018 [DOI] [PubMed] [Google Scholar]
- 18. Vincenzo JL, Glenn JM, Gray SM, Gray M. Balance measured by the sway balance smart-device application does not discriminate between older persons with and without a fall history. Aging Clin Exp Res. 2016;28:679–686. doi: 10.1007/s40520-015-0471-8 [DOI] [PubMed] [Google Scholar]
- 19. Glenn JM, Gray M, Vincenzo JL, Stone MS. Functional lower-body power: a comparison study between physically inactive, recreationally active, and masters athlete late-middle-aged adults. J Aging Phys Act. 2016;24:501–507. doi: 10.1123/japa.2015-0208 [DOI] [PubMed] [Google Scholar]
- 20. IBM SPSS (for Windows). Version 24. Armonk, NY: IBM Corp; 2016. http://www-01.ibm.com/support/docview.wss?uid=swg21476197 [Google Scholar]
- 21. Hannaford PC, Owen-Smith V. Using epidemiological data to guide clinical practice: review of studies on cardiovascular disease and use of combined oral contraceptives. BMJ. 1998;316:984–987. doi: 10.1136/bmj.316.7136.984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kirn DR, Reid KF, Hau C, Phillips EM, Fielding RA. What is a clinically meaningful improvement in leg-extensor power for mobility-limited older adults?J Gerontol A Biol Sci Med Sci. 2016;71:632–636. doi: 10.1093/gerona/glv207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mayson DJ, Kiely DK, LaRose SI, Bean JF. Leg strength or velocity of movement: which is more influential on the balance of mobility limited elders?Am J Phys Med Rehabil. 2008;87:969–976. doi: 10.1097/phm.0b013e31818dfee5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. McKinnon NB, Connelly DM, Rice CL, Hunter SW, Doherty TJ. Neuromuscular contributions to the age-related reduction in muscle power: mechanisms and potential role of high velocity power training. Ageing Res Rev. 2017;35:147–154. doi: 10.1016/j.arr.2016.09.003 [DOI] [PubMed] [Google Scholar]
- 25. Reid KF, Martin KI, Doros G, et al. Comparative effects of light or heavy resistance power training for improving lower extremity power and physical performance in mobility-limited older adults. J Gerontol A Biol Sci Med Sci. 2015;70:374–380. doi: 10.1093/gerona/glu156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Glenn JM, Gray M, Binns A. The effects of loaded and unloaded high-velocity resistance training on functional fitness among community-dwelling older adults. Age Ageing. 2015;44:926–931. doi: 10.1093/ageing/afv081 [DOI] [PubMed] [Google Scholar]
- 27. Straight CR, Lindheimer JB, Brady AO, Dishman RK, Evans EM. Effects of resistance training on lower-extremity muscle power in middle-aged and older adults: a systematic review and meta-analysis of randomized controlled trials. Sports Med. 2016;46:353–364. doi: 10.1007/s40279-015-0418-4 [DOI] [PubMed] [Google Scholar]
- 28. Bean JF, Herman S, Kiely DK, et al. Increased velocity exercise specific to task (InVEST) training: a pilot study exploring effects on leg power, balance, and mobility in community‐dwelling older women. J Am Geriatr Soc. 2004;52:799–804. doi: 10.1111/j.1532-5415.2004.52222.x [DOI] [PubMed] [Google Scholar]