Abstract
In 2002, the Institute of Medicine highlighted community partnerships as important in strategies for assuring the public’s health in the 21st Century. Whether defined narrowly as the neighborhood or more broadly as the whole nation, communities represent settings where health is supported and protected by healthy social connections and environments or risked and damaged by detrimental social, environmental, and policy determinants, as well as adverse behavioral and lifestyle choices. In this article, cardiovascular disease in African Americans is used as an example to highlight the successes achieved over the last half-century in reducing mortality rates; the persisting challenge of suboptimal adoption of evidence-based practices to promote community health and prevent disease; and the still widespread and pervasive health disparities. The article concludes with a call for the scientific community to embrace implementation research in strategic partnership with community stakeholders to stem the tide of cardiovascular disease and reduce related cardiovascular health disparities.
Keywords: Cardiovascular disease, heart disease, stroke, community, partnerships, disparities, implementation research, health disparities, public health, environment, lifestyle, risk, residence characteristics, African Americans, review
Introduction
Cardiovascular diseases (CVD), principally ischemic heart disease and stroke, remain the leading cause of global deaths and a major cause of health loss in all regions of the world.2 In 2015, there were nearly 423 million cases and an estimated 18 million deaths attributed to CVD.2 In the US alone, the most recent national vital statistics show 774,165 deaths from CVD, nearly 29% of all deaths in 2015.3 Although the national age-adjusted mortality rates for heart disease and stroke continued their long-term trends, declining 61% and 70%, respectively since 1975, rates for African Americans remained 20% higher for heart disease and 40% higher for stroke, compared to rates in Whites.3,4 In fact, the age-adjusted mortality rates for heart disease and stroke remain highest in African American men and women among all race/ethnic groups in the US.
Compounding this disease burden are the pervasive disparities in access to high-quality cardiovascular health care experienced by African Americans and other underserved racial and ethnic minorities.5–8 Although adverse clinical, behavioral, and lifestyle-mediated risk factors contribute to the excess burden of CVD in African Americans, it has become increasingly clear that neighborhood, place of residence, and geography matter;9–11 and that community and neighborhood factors have a role in the disparities seen in cardiovascular outcomes.12 In this review, the importance of leveraging strategic community partnerships that go beyond the biomedical sector to address community determinants of cardiovascular health and reduce excess CVD burden and related health disparities in African Americans is addressed.
Excess Burden of Cardiovascular Disease in African Americans
A recent American Heart Association scientific statement on the cardiovascular health of African Americans nicely summarizes the high burden of CVD and the role it plays as a primary driver of disparities between black and white Americans.13 For example, the report highlights the greater incidence, prevalence, and/or mortality of heart failure, sudden cardiac arrest, sudden cardiac death, transient ischemic attacks, ischemic stroke, and intracerebral hemorrhage in African Americans compared to Whites.13 Additionally, these CVD and their major risk factors such as hypertension, diabetes mellitus (both diagnosed and undiagnosed), and obesity often have an earlier age of onset and greater prevalence in African Americans than Whites.13 The report also highlights the greater target organ damage associated with hypertension and diabetes in African Americans and the profound excess of diabetes-related retinopathy, nephropathy, and lower-extremity amputations.13 Comorbid conditions such as chronic kidney disease and sickle cell disease that predispose to CVD are also more prevalent in African Americans compared to Whites.13
The greater prevalence of adverse health behaviors such as poor diet quality, low adherence to recommended physical activity, insufficient or poor-quality sleep, and untreated sleep disorders in African Americans compared to Whites contributes to the greater burden of CVD and related risk factors in the former. These risk factors often cluster in African American adults13; for example, Baruth et al. showed in a sample of adult African Americans in community-based faith settings that the prevalence of hypertension, obesity, hypercholesterolemia, and diabetes was 64%, 62%, 39%, and 23% respectively.14 Importantly, however, as many as 22% had 3 risk factors while 10% had 4 risk factors.14 These adverse risk factor findings are also strongly associated with social and environmental determinants of health and community or neighborhood charateristics.15–18
Neighborhood and Community Characteristics and Cardiovascular Health
Adverse health risks that contribute to a greater burden of disease often result from individual behavioral and lifestyle choices as well as institutional, socioeconomic, policy, and environmental influences. Important among these influences are community or neighborhood characteristics that include joblessness, poverty, educational attainment, housing quality, environmental pollution, availability of nutritious foods, neighborhood walkability, neighborhood violence, access to green spaces, social connectedness, other social and environmental determinants of health, and access to quality health care.15–19 For example, the proportion of African Americans who live in poverty is twice that of non-Hispanic Whites and the level of educational attainment, on average, is lower in African Americans.13 Krueger et al.20 have shown that mortality that can be attributed to limited education is similar in magnitude to the mortality that can be attributed to being a current rather than a former smoker.20 In fact, as pointed out by Wong et al,21 mortality resulting from all causes is greater for individuals who have fewer years of education and for those who are African American.
Independent of education and income, residential segregation based on race and ethnicity in the US may lead to adverse CVD outcomes for African Americans and other racial and ethnic minority populations. In fact, Williams and Collins have argued that racial residential segregation is a fundamental cause of racial disparities in health and that any efforts to end racial disparities in health must make a serious effort to address segregation and its long-lasting consequences.22 An analysis of the Multi-Ethnic Study of Atherosclerosis (MESA) showed that in African Americans, each standard deviation increase in black segregation was associated with a 12% higher hazard of incident CVD (first definite angina, probable angina followed by revascularization, myocardial infarction, resuscitated cardiac arrest, coronary heart disease death, stroke, or stroke death) over 10.2 median years of follow-up, after adjusting for demographics.23 In African Americans, this adverse association between racial residential segregation and CVD risk persisted after adjustment for neighborhood-level characteristics, individual socioeconomic position, and traditional CVD risk factors.23 In contrast, residential segregation was associated with lower CVD risk in Whites in the MESA study.23
The crucial role that racial residential segregation plays in CVD disparities can be surmised from the fact that racial residential segregation is high in the US, as demonstrated by the US201 Project.24 Logan and Stults show in their analysis of 367 metropolitan areas that the average black person lives in a neighborhood that is 45% black, 35% white, 15% Hispanic, and 4% Asian whereas the average white person lives in a neighborhood that is 75% white, 8% black, 11% Hispanic, and 5% Asian.24 Table 1 shows black-white segregation in 50 metropolitan areas with the largest black populations in 2010. As demonstrated in Figure 1, Whites live in neighborhoods with low minority representation while Blacks and Hispanics live in neighborhoods with high minority representation, and relatively few white neighbors.24 It has been suggested that predominantly racial and ethnic minority neighborhoods are disproportionately higher in poverty than predominantly white neighborhoods and that the association with increased CVD risk may be mediated by multiple mechanisms including poor access to health-promoting resources, less exposure to safe areas, and reduced opportunities to obtain high-quality health care.23
Table 1:
Black-White Segregation in 50 Metropolitan Areas with Largest Black Populations in 2010.
| 2010 Rank |
Area Name | 2010 Segregation |
2000 Segregation |
1990 Segregation |
1980 Segregation |
|---|---|---|---|---|---|
| 1 | Detroit-Livonia-Dearborn, MI | 79.6 | 85.9 | 85.6 | 83.0 |
| 2 | Milwaukee-Waukesha-West Allis, WI |
79.6 | 82.2 | 82.8 | 83.9 |
| 3 | New York-White Plains- Wayne, NY-NJ |
79.1 | 81.3 | 82.0 | 81.7 |
| 4 | Newark-Union, NJ-PA | 78.0 | 80.4 | 82.7 | 82.8 |
| 5 | Chicago-Joliet-Naperville, IL | 75.9 | 80.8 | 84.6 | 88.6 |
| 6 | Philadelphia, PA | 73.7 | 76.5 | 81.4 | 82.6 |
| 7 | Miami-Miami Beach- Kendall, FL |
73.0 | 72.4 | 71.8 | 79.3 |
| 8 | Cleveland-Elyria-Mentor, OH | 72.6 | 77.2 | 82.8 | 85.8 |
| 9 | St. Louis, MO-IL | 70.6 | 73.4 | 77.2 | 81.6 |
| 10 | Nassau-Suffolk, NY | 69.2 | 73.6 | 76.4 | 76.9 |
| 11 | Boston-Quincy, MA | 67.8 | 71.5 | 73.7 | 79.8 |
| 12 | Cincinnati-Middletown, OH- KY-IN |
66.9 | 72.6 | 75.9 | 78.2 |
| 13 | Birmingham-Hoover, AL | 65.2 | 68.0 | 70.3 | 72.2 |
| 14 | Los Angeles-Long Beach- Glendale, CA |
65.0 | 67.4 | 73.1 | 81.1 |
| 15 | Indianapolis-Carmel, IN | 64.5 | 71.0 | 74.4 | 78.8 |
| 16 | Baltimore-Towson, MD | 64.3 | 67.6 | 71.4 | 74.4 |
| 17 | Washington-Arlington- Alexandria, DC-VA-MD-WV |
64.1 | 65.9 | 68.4 | 71.4 |
| 18 | New Orleans-Metairie- Kenner, LA |
63.3 | 69.0 | 68.3 | 70.0 |
| 19 | Pittsburgh, PA | 63.1 | 67.4 | 70.8 | 73.3 |
| 20 | Memphis, TN-MS-AR | 62.2 | 65.7 | 65.5 | 68.8 |
| 21 | Houston-Sugar Land- Baytown, TX |
60.6 | 65.1 | 65.5 | 73.7 |
| 22 | Columbus, OH | 59.9 | 62.2 | 67.6 | 72.9 |
| 23 | Kansas City, MO-KS | 58.6 | 69.3 | 72.9 | 77.7 |
| 24 | Atlanta-Sandy Springs- Marietta, GA |
58.3 | 63.9 | 66.3 | 76.9 |
| 25 | Warren-Troy-Farmington Hills, MI |
57.9 | 68.1 | 76.7 | 80.5 |
Reproduced from JR Logan and B Stults24
Figure 1:
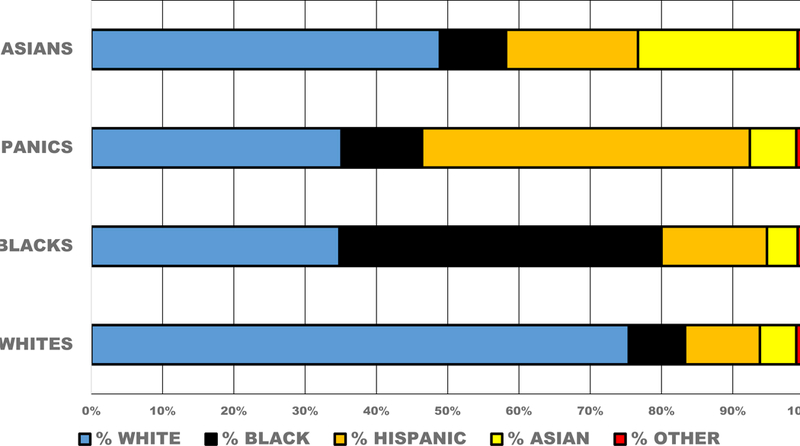
The extent of diversity experienced in each racial/ethnic group’s typical neighborhood, National Metropolitan Average, 2010 Census. Reproduced from JR Logan and B Stults24
Taken collectively, these social, environmental, community, and neighborhood characteristics and determinants of health play important roles in the continuing high burden of CVD and related health disparities in African Americans. Strategies to address the burden of CVD and disparities must involve active engagement of and strategic partnerships with the community to be successful. Until recently however, the crucial role of strategic partnerships with communities as a legitimate strategy for cardiovascular health promotion and disparities reduction had been underrecognized. Importance of Community Partnerships for Health
In 2002, the US Institute of Medicine (now the National Academy of Medicine) highlighted community partnerships as important in strategies for assuring the public’s health in the 21st Century.25 Whether defined narrowly as the neighborhood or more broadly to encompass the whole nation, communities represent the settings where health is “supported and protected” or “risked and damaged”.25 Active engagement of communities and strategic partnerships with community residents, institutions, and resources beyond the health sector is crucial. As the Institute of Medicine correctly emphasized, communities are “both the physical and cultural settings for … action to promote the public’s health”.25 They are ideally seen as “points of convergence” for the interests of multiple stakeholders, including individuals, families, employers, businesses, schools, healthcare settings, health care providers, media outlets, and governmental and non-governmental organizations. These stakeholders can and should be engaged to contribute to supporting and promoting cardiovascular health and reducing related health disparities.
An important starting point for strategic partnerships is a recognition of community norms, values, resources, and most importantly, community needs and challenges. Thus, a community needs assessment can be an invaluable tool for forging partnerships, identifying health priorities, as well as supporting a true community culture of health.26 Fostering strategic partnerships with communities is crucial for sustained success in stemming the tide of CVD and related disparities.27 Active engagement of community stakeholders is essential and should ideally include community thought-leaders, diverse governmental and non-governmental organizations, large corporations and small businesses, sororities and fraternities, other civic organizations, academic health centers and their research investigators, State and local health departments, and most importantly, community residents and their families. The National Academies of Sciences, Engineering, and Medicine (NASEM) report on communities in action has provided a conceptual model to inform community success in implementing community-driven solutions to promote health equity (Figure 2).28
Figure 2:
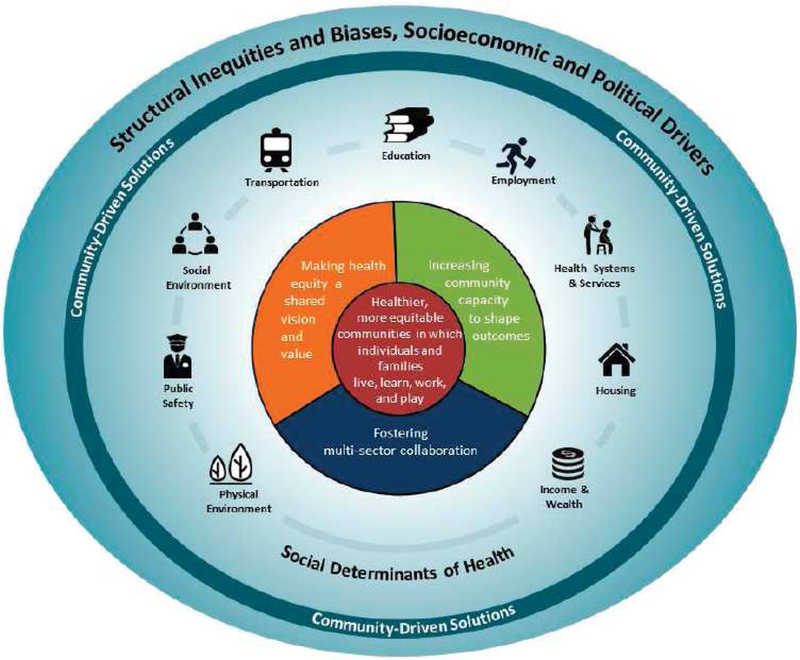
The three elements of community success in implementing community-driven solutions to promote health equity. Image is © 2017 National Academy of the Sciences and is reproduced from28 with permission of the copyright holder.
The three important elements of the conceptual model include “(1) Multi-sector collaboration; (2) Health equity as a shared vision and value; and (3) Community capacity to shape outcomes”.28 Developing strong, strategic, multi-sector, community collaboration is an essential first step that takes time and commitment of stakeholders. A strong collaboration without a shared vision for the reduction and elimination of disparities is not likely to be successful. As the NASEM report astutely points out, the shared vision is the “glue” that holds the multi-sector collaboration together, permitting the collective vision to rise above individual stakeholder interests.28 Finally, the community’s likelihood of succeeding in its efforts depends on its ability to leverage its residents, thought leaders, local businesses, and elected officials to develop its prioritized needs and the capacity to intervene.
All the above require a high degree of community engagement with committed community leadership. As the NASEM report emphasizes, there have to be “conversations at kitchen tables, in church basements, in little meeting rooms,” across the community.28 This is hard, painstaking work; but we have evidence from two of the longest-running CVD prevention and control programs with active community engagement that success is attainable.29,30 For example, Record et al.29 demonstrated in a county in Maine that sustained, community-wide interventions addressing cardiovascular risk factors and behavior changes were associated with reductions in hospitalization and mortality rates over 40 years. Similarly, the community-based North Karelia Project led to dramatic declines in cardiovascular mortality (82% in men aged 35 to 64 years and 84% in similarly aged women) over a 40-year period.30 The need and the challenge is to also demonstrate that these principles can be used to tackle the reduction and eventual elimination of CVD disparities. Given the hard work of engaging community stakeholders and the need for long-term relationships, it would be important to explore appropriate funding models for sustaining these partnerships, especially when research funding grants end. There is a role for governmental, private sector, and philanthropic organizations in helping sustain these community partnerships.
Embracing Implementation Research
There is some good news in the efforts to promote cardiovascular health and reduce CVD disparities. In the US, substantial declines in CVD mortality have been seen in all race/ethnic groups, including African Americans, with significant improvements in life expectancy.31 For example, in both African American men and women, life expectancy has increased from 60 and 68 years, respectively in 1970 to 72 and 78 years, respectively in 2014.4 In addition, the life expectancy gap between blacks and whites has continued to decline;32 and has been eliminated in adults aged 65 years or older.33 The largest contributor to the decrease in the black-white life expectancy gap between 1999 and 2013 was heart disease, which, together with contributions from cancer, HIV, unintentional injuries, and perinatal conditions accounted for nearly 60% of the 2.3-year decrease in the gap.32
Additional good news includes the availability of safe and effective interventions for the treatment and control of CVD risk factors such as hypertension. We have recent evidence suggesting that hypertension control rates of 80–90% are achievable and racial/ethnic disparities in hypertension control rates can be eliminated, especially in integrated health systems that implement systematic strategies to manage hypertension.34–36 What these findings suggest is that continued success in improving cardiovascular health and reducing CVD disparities is possible but it will require embracing dissemination and implementation research and accelerating widespread and sustained adoption of proven-effective interventions.37 In fact, embracing dissemination and implementation research in hypertension treatment and control is needed more now, given the lower blood pressure treatment goal recommended in the 2017 high blood pressure clinical practice guideline.38,39 Continued success in reducing CVD disparities also requires interventions to be tailored to community context with active community engagement to address social and environmental determinants of health, to improve neighborhood characteristics, and to enhance access to quality health care for all.
Conclusions
As the Victoria Declaration stated 25 years ago, “cardiovascular disease is largely preventable.40 We know enough to maximize health impact for all and eliminate related CVD disparities. But we cannot do so by working only in the biomedical arena because of the important influences of social determinants of health and neighborhood and community characteristics.19 The crucial role of the community in health could not have been more eloquently captured by William James.1 The time has come to redouble our efforts in fully embracing strategic partnerships with community stakeholders to turn research discoveries into health and assure a future free of CVD and related disparities. The time for action is now!
Acknowledgements:
The author thanks Jazmine R. Mensah for edits to the manuscript and assistance with table, figures, and references.
Support: This article is part of a supplement that arose from the Frank M. Norfleet Forum for Advancement of Health: African Americans and Kidney Disease in the 21st Century, held March 24, 2017 in Memphis, TN. The Forum and the publication of this supplement were funded by the Frank M. Norfleet Forum for Advancement of Health, the Community Foundation of Greater Memphis, and the University of Tennessee Health Science Center.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The community stagnates without the impulse of the individual.
The impulse dies away without the sympathy of the community.
William James1
Financial Disclosure: The author declares that he has no relevant financial interests.
Publisher's Disclaimer: Disclaimer: The views expressed in this article are the author’s and do not necessarily represent the views of the National Institutes of Health or the United States Department of Health and Human Services.
References
- 1.James W. Great Men, Great Thoughts, and the Environment. Lecture delivered before the Harvard Natural History Society. Published in the Atlantic Monthly, October, 1880. https://www.uky.edu/~eushe2/Pajares/jgreatmen.html Accessed October 31, 2017.
- 2.Roth GA, Johnson C, Abajobir A, et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J Am Coll Cardiol 2017;70(1):1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Center for Health Statistics. Health, United States, 2016: With Chartbook on Long-term Trends in Health 2017. https://www.cdc.gov/nchs/data/hus/hus16.pdf. [PubMed]
- 4.Kochanek KD, Murphy SL, Xu J, Tejada-Vera B. Deaths: Final Data for 2014. National vital statistics reports : from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System 2016;65(4):1–122. [PubMed] [Google Scholar]
- 5.Agency for Health Research and Quality. 2016 National Healthcare Quality and Disparities Report. Rockville, MD: AHRQ; Pub. No. 17–0001; 2017. [Google Scholar]
- 6.Dong L, Fakeye OA, Graham G, Gaskin DJ. Racial/Ethnic Disparities in Quality of Care for Cardiovascular Disease in Ambulatory Settings: A Review. Med Care Res Rev 2018;75(3):263–291. [DOI] [PubMed] [Google Scholar]
- 7.Shi L, Chen CC, Nie X, Zhu J, Hu R. Racial and socioeconomic disparities in access to primary care among people with chronic conditions. Journal of the American Board of Family Medicine : JABFM 2014;27(2):189–198. [DOI] [PubMed] [Google Scholar]
- 8.Rangrass G, Ghaferi AA, Dimick JB. Explaining racial disparities in outcomes after cardiac surgery: the role of hospital quality. JAMA Surg 2014;149(3):223–227. [DOI] [PubMed] [Google Scholar]
- 9.LaVeist T, Pollack K, Thorpe R Jr., Fesahazion R, Gaskin D. Place, not race: disparities dissipate in southwest Baltimore when blacks and whites live under similar conditions. Health Aff (Millwood) 2011;30(10):1880–1887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mensah GA, Goff DC, Gibbons GH. Cardiovascular Mortality Differences-Place Matters. JAMA 2017;317(19):1955–1957. [DOI] [PubMed] [Google Scholar]
- 11.Limdi NA, Howard VJ, Higginbotham J, Parton J, Safford MM, Howard G. US Mortality: Influence of Race, Geography and Cardiovascular Risk Among Participants in the Population-Based REGARDS Cohort. J Racial Ethn Health Disparities 2016;3(4):599–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liao Y, Bang D, Cosgrove S, et al. Surveillance of health status in minority communities - Racial and Ethnic Approaches to Community Health Across the U.S. (REACH U.S.) Risk Factor Survey, United States, 2009. MMWR Surveill Summ 2011;60(6):1–44. [PubMed] [Google Scholar]
- 13.Carnethon MR, Pu J, Howard G, et al. Cardiovascular Health in African Americans: A Scientific Statement From the American Heart Association. Circulation 2017;136(21):e393–e423. [DOI] [PubMed] [Google Scholar]
- 14.Baruth M, Wilcox S, Egan BM, Dowda M, Laken M, Warren TY. Cardiovascular disease risk factor clustering among African American adults. Ethn Dis 2011;21(2):129–134. [PMC free article] [PubMed] [Google Scholar]
- 15.Havranek EP, Mujahid MS, Barr DA, et al. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation 2015;132(9):873–898. [DOI] [PubMed] [Google Scholar]
- 16.Diez Roux AV. Neighborhoods and Health: What Do We Know? What Should We Do? Am J Public Health 2016;106(3):430–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Muennig P, Cohen AK, Palmer A, Zhu W. The relationship between five different measures of structural social capital, medical examination outcomes, and mortality. Soc Sci Med 2013;85:18–26. [DOI] [PubMed] [Google Scholar]
- 18.Barber S, Hickson DA, Wang X, Sims M, Nelson C, Diez-Roux AV. Neighborhood Disadvantage, Poor Social Conditions, and Cardiovascular Disease Incidence Among African American Adults in the Jackson Heart Study. Am J Public Health 2016;106(12):2219–2226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hall YN. Social Determinants of Health: Addressing Unmet Needs in Nephrology. American Journal of Kidney Diseases 2018;72(4): 10.1053/j.ajkd.2017.12.016 [DOI] [PubMed] [Google Scholar]
- 20.Krueger PM, Tran MK, Hummer RA, Chang VW. Mortality Attributable to Low Levels of Education in the United States. PloS one 2015;10(7):e0131809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. N Engl J Med 2002;347(20):1585–1592. [DOI] [PubMed] [Google Scholar]
- 22.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep 2001;116(5):404–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kershaw KN, Osypuk TL, Do DP, De Chavez PJ, Diez Roux AV. Neighborhood-level racial/ethnic residential segregation and incident cardiovascular disease: the multi-ethnic study of atherosclerosis. Circulation 2015;131(2):141–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Logan JR, Stults BM. The Persistence of Segregation in the Metropolis: New Findings from the 2010 Census 2011. https://s4.ad.brown.edu/Projects/Diversity/Data/Report/report2.pdf Accessed October 31, 2017.
- 25.Institute of Medicine. The Community. The Future of the Public’s Health in the 21st Century Washington, DD: National Academies Press (US); 2003:178 – 211. [Google Scholar]
- 26.Chandra A, Acosta JD, Carman KG, et al. Building a National Culture of Health: Background, Action Framework, Measures, and Next Steps Santa Monica, CA: Rand Corporation; 2016. [PMC free article] [PubMed] [Google Scholar]
- 27.National Academies of Sciences, Engineering, and Medicine. The Role of Communities in Promoting Health Equity. Communities in action: Pathways to health equity Washington, DC: The National Academies Press; 2017:185 – 210. [PubMed] [Google Scholar]
- 28.National Academies of Sciences, Engineering, and Medicine. Communities in action: Pathways to health equity Washington, D.C.: National Academies Press; 2017. [PubMed] [Google Scholar]
- 29.Record NB, Onion DK, Prior RE, et al. Community-wide cardiovascular disease prevention programs and health outcomes in a rural county, 1970–2010. JAMA 2015;313(2):147–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jousilahti P, Laatikainen T, Salomaa V, Pietila A, Vartiainen E, Puska P. 40-Year CHD Mortality Trends and the Role of Risk Factors in Mortality Decline: The North Karelia Project Experience. Glob Heart 2016;11(2):207–212. [DOI] [PubMed] [Google Scholar]
- 31.Mensah GA, Wei GS, Sorlie PD, et al. Decline in Cardiovascular Mortality: Possible Causes and Implications. Circ Res 2017;120(2):366–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kochanek KD, Anderson RN, Arias E. Leading Causes of Death Contributing to Decrease in Life Expectancy Gap Between Black and White Populations: United States, 1999–2013. NCHS Data Brief 2015(218):1–8. [PubMed] [Google Scholar]
- 33.Cunningham TJ, Croft JB, Liu Y, Lu H, Eke PI, Giles WH. Vital Signs: Racial Disparities in Age-Specific Mortality Among Blacks or African Americans - United States, 1999–2015. MMWR Morb Mortal Wkly Rep 2017;66(17):444–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sim JJ, Handler J, Jacobsen SJ, Kanter MH. Systemic implementation strategies to improve hypertension: the Kaiser Permanente Southern California experience. The Canadian journal of cardiology 2014;30(5):544–552. [DOI] [PubMed] [Google Scholar]
- 35.Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved blood pressure control associated with a large-scale hypertension program. Jama 2013;310(7):699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shaw KM, Handler J, Wall HK, Kanter MH. Improving blood pressure control in a large multiethnic California population through changes in health care delivery, 2004–2012. Preventing chronic disease 2014;11:E191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mensah GA. Embracing dissemination and implementation research in cardiac critical care. Glob Heart 2014;9(4):363–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018;71(6):1269–1324. [DOI] [PubMed] [Google Scholar]
- 39.Muntner P, Carey RM, Gidding S, et al. Potential U.S. Population Impact of the 2017 American College of Cardiology/American Heart Association High Blood Pressure Guideline. Circulation 2018;137(2):109–118.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.O’Connor B. The Victoria Declaration--a unifying force. Can J Cardiol 1995;11 Suppl A:12A–13A. [PubMed] [Google Scholar]


