Abstract
End-stage kidney disease (ESKD) and earlier stages of chronic kidney disease (CKD) represent one of the most dramatic examples of racial/ethnic disparities in health in our nation. African Americans are three times more likely to require renal replacement therapy then their non-Hispanic White counterparts. This article describes CKD-related disparities linked to a variety of clinical, socio-economic, and cultural factors, as well as to select social determinants of health that are defined by social positioning and often by race within the United States. Our advancing understanding of these issues has led to improvements in patient outcomes and is narrowing the gap in disparities across most aspects of CKD and CKD risk factors. There are also extensive data indicating similar improvements in quality measures for patients on dialysis. This article also reviews the state of CKD in African Americans from a population perspective and provides recommendations for the way forward.
Keywords: chronic kidney disease (CKD), race, disparities, social determinants, African American, population health, health beliefs, health behaviors, ethnicity, socioeconomic status (SES), risk factor, review
INTRODUCTION
Chronic kidney disease (CKD) is a major public health problem that disproportionally affects minority and low-income persons.1,2 In the United States African-Americans suffer from some of the highest rates of end stage kidney disease (ESKD) in comparison to other racial ethnic groups.3,4 This appears to be related to multiple factors, including the number of and degree of control of CKD risk factors, access to and receipt of high-quality care, health beliefs and health behaviors, social determinants of health and other factors that combine to create a nearly 3 fold greater incidence of treated ESKD for African-Americans in comparison to their White peers (Figure 1).1,2,5,6 This report will focus on the non-biological factors that contribute to CKD in African Americans, while biological factors such as APOL1 gene variants are discussed elsewhere in this journal supplement.5B
Figure 1.
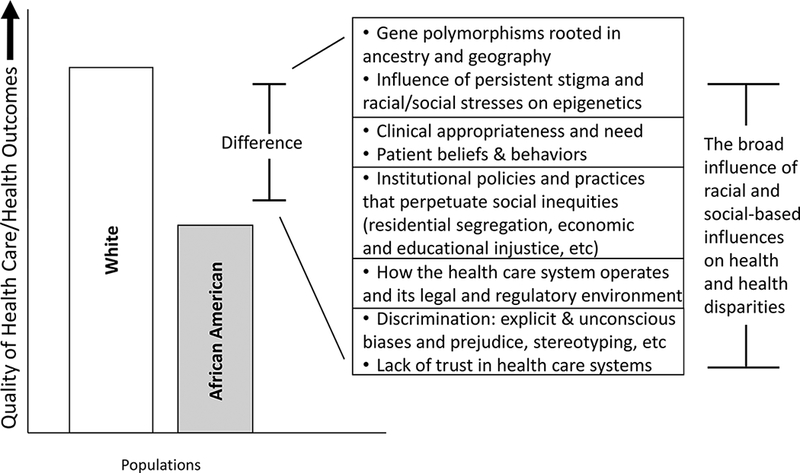
Major domains contributing to racial differences and disparities in quality of care and clinical outcomes for patients with chronic kidney disease. Based on a conceptual model in Smedley et al5A.
Race and Health in the U.S.
African-Americans represent approximately 13% of the US population, and along with Native Americans suffer from the highest rates of premature morbidity and mortality in the United States for most medical conditions.7 Although the terms “race” and “ethnicity” are social constructs created by society, they represent a collection of people organized around shared ancestry and history, shared cultural norms, language, and social identity as well as shared biological characteristics due to differing frequencies of select gene variants that reflect important linkages to ancestral geographic origins.8,9 They also reflect variations in gene expression (epigenetics) due to the varying social, physical, and psychological environments driven by the social structure.8 Probably the most direct impact of race on health for African Americans is being relegated to a dramatic and persistent degree of low socio-economic status due to institutionalized policies and practices that perpetuate residential segregation, low-quality public school systems, and greater risk of violent death.2,6,10–12
Major Chronic Kidney Disease Risk Factors
Diabetes and hypertension are the most common risk factors for developing ESKD,13 with obesity/overweight being an important co-morbid condition. Compared to their White counterparts, African Americans have a higher prevalence of obesity/overweight (76.3% vs 68.5%), diabetes (18% vs 9.6%, including both physician-diagnosed and undiagnosed disease), and hypertension (43.3% vs 29.1%).7 Also, African Americans have a more than 2 fold greater odds than Whites of having elevated albuminuria, another important CKD progression factor.14
Impact of Health Beliefs and Behaviors on Chronic Kidney Disease
Variation in health beliefs and behaviors by race can have an impact on CKD screening, CKD risk factor control, and adherence to CKD therapies. The early identification and management of CKD can “(1) limit or prevent CKD progression, (2) ensure appropriate drug dosing, (3) limit drug-related nephrotoxic injury, (4) minimize the risk of drug-related and other causes of acute kidney injury, and (5) reduce the increased rate of CV events in patients with CKD”.15 Of note Umeukeje et al. recently attempted to identify the key barriers and facilitators influencing the likelihood of African Americans participating in community-based CKD screenings.16 Guided by the Health Belief Model, they found several consistent barriers such as limited understanding of CKD and CKD risk factors, low trust in health care systems, and financial burden. They also noted several facilitators, including the critical role of physicians as communicators, peer pressure, and church health leaders.16 These factors seem to be relevant not only for screening, but for engagement in clinical trials17 and accessing care.5,10,18
Social Determinants of Health
Common examples of the influence of the social determinants of health, which disproportionally affect minority and low-income populations, include educational attainment, income, insurance, and community-level assets and deficits.2,19 Nationally, 20% of African Americans are below the federal poverty level compared to only 9% of Whites,20 only 76% of African Americans graduated high school vs. 88% of Whites,21 and in 2016 the uninsured rate for Blacks was 10.5% vs 6.3% for Whites.21 An analysis of uninsured persons who participated in the National Kidney Foundation screening program for persons with or at risk for CKD, the Kidney Early Evaluation Program (KEEP), found uninsured KEEP participants were 72% more likely to develop ESKD and 82% more likely to die than those with private insurance.23 Similarly, Choi et al. reported a nearly 20% higher adjusted relative risk of death over a mean follow-up period of 3.9 years for KEEP participants with CKD and less than a high school education compared to those with CKD and high school education or greater.24
Closely linked to educational attainment is literacy, and limited health literacy in CKD is especially common among African Americans and/or persons of low socioeconomic status.25 Among patients in the Chronic Renal Insufficiency Cohort (CRC) Study, limited health literacy was found in 28% of African American and 5% of White participants.26 Limited health literacy in patients with CKD has been associated with increased hospitalizations, emergency department use, cardiovascular events, and mortality.27 Health literacy is defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions”.27A,28 The use of plain language is a strategy for simplifying complex health information to improve health literacy. This led to the Federal Plain Language Action and Information Network (PLAIN) Writing Act being signed into law in 2010, mandating that all government agencies use written communication that is accessible and comprehensible to all citizens.20 The use of plain language for educational materials relevant for patients with or at risk for CKD still has room for improvement as it has remained at about a 9th grade reading level (above the desired 6th grade reading level) over the last 10 years.29,30 A recent review estimated the overall prevalence of limited health literacy to be 25% among patients with CKD not on dialysis, 27% among patients treated with dialysis, and 14% among patients with kidney transplants.25 Cavanaugh et al. reported that limited health literacy among 480 dialysis patients is more likely in be present in males, non-Whites and those with fewer years of education, and is associated with a 54% higher risk for death.31 However, these and similar reports may underestimate health literacy given the even higher estimated rates of functional literacy of 45% among adults in the U.S.32
In addition to high rates of low health literacy, many patients with CKD have multiple medical conditions and multiple medications that may impact their cognitive function and ability to grasp clinical descriptions of disease status, complications, and expectations.33,34 With an increasing number of immigrants who speak English as a second language, an aging population, and an exponential rise in social media, there are vastly more competing linguistic, generational, and cultural issues that can create barriers to effective communication. Improving patient-provider communication can assist in engaging patients in health care decisions and enhance patient activation.35,36 However, communication is an area that will need close attention going forward as those with limited resources, education, and health literacy may suffer from even more disparities as our society has an increasing reliance on social media and the internet, with a certain level of sophistication being needed to obtain accurate digital health information and/or to effectively communicate with health care providers. To improve communication it will be more and more important to not only convey messages but to confirm understanding. Confirming understanding is not merely asking a patient to respond to “do you understand” and waiting for an affirmative response or a nod, but to have them explain or “teach back” the treatment plan and any other aspects of care.37 For many patients with ESKD and earlier stages of CKD, this may require constant reinforcement by many health care providers, but the gains can be substantial. Finally, other social determinants such as neighborhood and the built environment and the social and community context can markedly influence socioeconomic status, health behaviors, social networks, peer pressure, and many other domains that ultimately impact CKD and CKD risk factors.10
Population Level Health
The Agency for Healthcare Research and Quality reported that when comparing 182 national quality measures between Black and White patients, Blacks had improvement across 23 measures, no difference in 82 measures and worsening quality of care in 77 measures.38 However, for CKD and major CKD risk factors there has been more substantial improvement in many key quality of care measures, as noted by Healthy People 2020 (table 1).13,39 The Healthy People 2020 program has monitored the health of the nation over the last several years at a population level, by both the disease condition and subgroups, to assess any changes in healthcare disparities.40 These assessments include select aspects of CKD and CKD risk factors.
Table 1:
Select Healthy People 2020 Indicators of CKD Care, by Race/Ethnicity
| Black/African American | White | HP 2020 Target | |||
|---|---|---|---|---|---|
| 2006 | 2015* | 2006 | 2015* | ||
| % of persons with diagnosed DM who obtain an annual urinary albumin measurement | 29.5% | 46.0% | 31.4 | 47.5%*** | 37% |
| % of persons with DM and CKD who receive medical evaluation with measurement of Scr, urinary albumin, HbA1c, lipids, and eye exam | 18.8% | 27.6% | 21.4% | 30.2% | 25.3% |
| % of persons with DM and CKD who receive recommended medical treatment with ACEi or ARBs | 66.7% | 72.3% | 62.2% | 70.2% | 76.3% |
| % CKD patients receiving care from a nephrologist at least 12 mo before RRT start | 23.2% | 32% | 27.9% | 37% | 30.4% |
| Rate of new cases of ESKD per million population | 1114 | 895 | 294 | 312.1 | 352 |
| % patients receiving a kidney transplant within 3 y of ESKD | 9.1% | 7%** | 21% | 16.2** | 20.1 |
| No. of deaths per 1,000 patient-years for persons on dialysis | 170.9 | 135.8 | 258.1 | 207.4 | 187.4 |
Unless otherwise indicated
2012
2014
DM – diabetes mellitus; ESKD – end-stage kidney disease; angiotensin-converting enzyme inhibitors (ACEi) or angiotensin II receptor blocker (ARB); Scr, serum creatinine; HbA1c, hemoglobin A1c. HP 2020, Healthy People 2020; RRT, renatl replacement therap
Source: USRDS 2017 Annual Data Report13
Healthy People 2020 found a substantial increase in the percent of African-Americans diagnosed with diabetes mellitus (DM) who obtained an annual urinary albumin measure in 2015 (46%) as compared to 2006 (29.5%). This increase is similar to the gains seen in their white peers over the same time period (47.5% versus 31.4%), with both groups now exceeding the Healthy People 2020 target rate of 37% (Table 1). Similar findings were noted in the percent of persons with DM and CKD who received a more comprehensive medical assessment and recommended medical treatment with inhibitors of the renin angiotensin system (Table 1).
Regarding the advanced stages of CKD, the percent of patients receiving care from a nephrologist at least 12 months prior to the start of renal replacement therapy rose from 26.4% in 2006 to 35.6% in 2015, but African Americans continue to trail Whites by about 5% (Table 1). African Americans have seen a substantial drop in the rate of new cases of ESKD per million population, possibly related to improved quality of care over time, but still fall far short of the Healthy People 2020 target rate (Table 1). While the number of patients receiving renal replacement therapy has increased, the number of kidney transplants has remained stable, leading to a progressive decline in the percent of all patients receiving a kidney transplant within three years of starting dialysis (Table 1).
Interestingly, despite an overall reduction in the death rate for dialysis patients, the death rate for White dialysis patients (207.4) remains above the Healthy People 2020 target level of 187.4 per 1000 patient years in contrast to only 135.8 per 1000 patient years for African Americans (Table 1). The reason for this observation remains unknown and is an area of intense research interest, but survival bias leading to healthier minorities reaching dialysis or other factors leading to a relative increase in resilience appear to contribute to the observed differences.41–46
Conclusions and Future Directions
In summary there has been a marked improvement in CKD and ESKD metrics for African Americans over time, with continuing reduction in the level of racial/ethnic disparities for multiple CKD metrics. African Americans still lag behind on most metrics, but overall have seen marked improvements in the quality of care for ESKD and earlier stages of CKD. These lingering disparities chart a path for the next generation of investigators to better understand the many nuances of racial/ethnic outcomes in CKD.
Racial and ethnic inequalities remain an indictment of the moral compass of our society. There is an increasing recognition of the important role of the social determinants of health as drivers of not only disparities, but of major factors influencing access to care and adherence to treatment for many patients with or at risk for CKD. As noted by Hall, there is an increasing need for a greater integration of social science, public health, and clinical policy approaches to better understand the causal mechanisms between social determinants and health, and their interactions on health outcomes within nephrology.10 There are also key action steps that can be taken immediately such as implementing strategies to address low health literacy in patients with or at risk for CKD using translators, videos and/or novellas, increasing the role of social networks and community organizations/institutions such as churches, and primary intervention strategies including the use of lay health workers and peer patient navigators.2 Finally, we should not miss the opportunity to advance the necessary policies to advance equity in society, eliminate health inequities and reduce the unacceptably high morbidity and mortality associated with CKD.47
Acknowledgments
Support: This article is part of a supplement that arose from the Frank M. Norfleet Forum for Advancement of Health: African Americans and Kidney Disease in the 21st Century, held March 24, 2017 in Memphis, TN. The Forum and the publication of this supplement were funded by the Frank M. Norfleet Forum for Advancement of Health, the Community Foundation of Greater Memphis, and the University of Tennessee Health Science Center. This article was also supported by the following institutes at the National Institute of Health: National Institute of Diabetes, Digestive and Kidney Disease-T32-DK104687 (ML), K23DK103972–03 (JS), R25DK113659 (KN) R13DK098961 (KN), and U54GM119024 (KN).
Footnotes
Financial Disclosure: The authors declare that they have no relevant financial interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Nicholas SB, Kalantar-Zadeh K, Norris KC. Racial disparities in kidney disease outcomes. Seminars in Nephrology. 2013;33(5):409–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nicholas SB, Kalantar-Zadeh K, Norris KC. Socioeconomic disparities in chronic kidney disease. Advances in Chronic Kidney Disease. 2015;22(1):6–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saran R, Li Y, Robinson B, et al. US Renal Data System 2015 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2016;67(3)(suppl 1):SVII–SVIII. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hsu CY, Lin F, Vittinghoff E, Shlipak MG. Racial differences in the progression from chronic renal insufficiency to end-stage renal disease in the United States. Journal of the American Society of Nephrology. 2003;14(11):2902–2907. [DOI] [PubMed] [Google Scholar]
- 5.Norris K, Nissenson AR. Race, gender, and socioeconomic disparities in CKD in the United States. Journal of the American Society of Nephrology. 2008;19(7): 1261–1270. [DOI] [PubMed] [Google Scholar]
- 6.Norton JM, Moxey-Mims MM, Eggers PW, Narva AS, Star RA, Kimmel PL, Rodgers GP. Social Determinants of Racial Disparities in CKD. Journal of the American Society of Nephrology. 2016;27(9):2576–2595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Center for Health Statistics. Health, United States, 2015: With Special Feature on Racial and Ethnic Health Disparities. Hyattsville, MD; 2016. [PubMed] [Google Scholar]
- 8.Norris KC, Williams SF, Rhee CM, Nicholas SB, Kovesdy CP, Kalantar-Zadeh K, Ebony Boulware L. Hemodialysis Disparities in African Americans: The Deeply Integrated Concept of Race in the Social Fabric of Our Society. Seminars in Dialysis. 2017;30(3):213–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Collins FS. What we do and don’t know about ‘race’, ‘ethnicity’, genetics and health at the dawn of the genome era. Nature Genetics. 2004;36(11 Suppl):S13–15. [DOI] [PubMed] [Google Scholar]
- 10.Hall YN. Social Determinants of Health: Addressing Unmet Needs in Nephrology. American Journal of Kidney Diseases. 2018;72(4):***-***. doi: 10.1053/j.ajkd.2017.12.016 [DOI] [PubMed] [Google Scholar]
- 11.Popescu I, Duffy E, Mendelsohn J, Escarce JJ. Racial residential segregation, socioeconomic disparities, and the White-Black survival gap. PloS One. 2018;13(2):e0193222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mesic A, Franklin L, Cansever A, Potter F, Sharma A, Knopov A, Siegel M. The Relationship Between Structural Racism and Black-White Disparities in Fatal Police Shootings at the State Level. Journal of the National Medical Association. 2018;110(2):106–116. [DOI] [PubMed] [Google Scholar]
- 13.Saran R, Robinson B, Abbott KC, et al. US Renal Data System 2017 Annual Data Report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2018;71(3)(suppl 1):S1–S672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bryson CL, Ross HJ, Boyko EJ, Young BA. Racial and ethnic variations in albuminuria in the US Third National Health and Nutrition Examination Survey (NHANES III) population: associations with diabetes and level of CKD. American Journal of Kidney Diseases. 2006;48(5):720–726. [DOI] [PubMed] [Google Scholar]
- 15.Norris KC, Nicholas SB. Community-Based CKD Screening in Black Americans. Clinical journal of the American Society of Nephrology. 2018;13(4):521–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Umeukeje EM, Wild MG, Maripuri S, Davidson T, Rutherford M, Abdel-Kader K, Lewis J, Wilkins CH, Cavanaugh K. Black Americans’ Perspectives of Barriers and Facilitators of Community Screening for Kidney Disease. Clinical Journal of the American Society of Nephrology. 2018;13(4):551–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.George S, Duran N, Norris K. A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. American Journal of Public Health. 2014;104(2):e16–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Powe NR. Let’s get serious about racial and ethnic disparities. Journal of the American Society of Nephrology. 2008;19(7):1271–1275. [DOI] [PubMed] [Google Scholar]
- 19.National Center for Health Statistics. Health, United States, 2015: With Special Feature on Racial and Ethnic Health Disparities. Hyattsville, MD: 2016. [PubMed] [Google Scholar]
- 20.Kaiser Family Foundation. State Health Facts. 2018. https://www.kff.org/state-category/minority-health/ Accessed on 20 May 2018.
- 21.National Center for Education Statistics Public High School Graduation Rates - 2018. https://nces.ed.gov/programs/coe/indicator_coi.asp> accessed 20 May 2018.
- 22.Barnett Jessica C. and Berchick Edward R., Current Population Reports, P60–260, Health Insurance Coverage in the United States: 2016, U.S. Government Printing Office, Washington, DC, 2017. [Google Scholar]
- 23.Jurkovitz CT, Li S, Norris KC, Saab G, Bomback AS, Whaley-Connell AT, McCullough PA, Investigators K. Association between lack of health insurance and risk of death and ESRD: results from the Kidney Early Evaluation Program (KEEP). American Journal of Kidney Diseases. 2013;61(4 Suppl 2):S24–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Choi AI, Weekley CC, Chen SC, Li S, Tamura MK, Norris KC, Shlipak MG. Association of educational attainment with chronic disease and mortality: the Kidney Early Evaluation Program (KEEP). American Journal of Kidney Diseases. 2011;58(2):228–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taylor DM, Fraser SDS, Bradley JA, Bradley C, Draper H, Metcalfe W, Oniscu GC, Tomson CRV, Ravanan R, Roderick PJ. A Systematic Review of the Prevalence and Associations of Limited Health Literacy in CKD. Clinical Journal of the American Society of Nephrology. 2017;12(7):1070–1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ricardo AC, Yang W, Lora CM, Gordon EJ, Diamantidis CJ, Ford V, Kusek JW, Lopez A, Lustigova E, Nessel L, Rosas SE, Steigerwalt S, Theurer J, Zhang X, Fischer MJ, Lash JP. Limited health literacy is associated with low glomerular filtration in the Chronic Renal Insufficiency Cohort (CRIC) study. Clinical Nephrology. 2014;81(1):30–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taylor DM, Fraser S, Dudley C, Oniscu GC, Tomson C, Ravanan R, Roderick P. Health literacy and patient outcomes in chronic kidney disease: a systematic review. Nephrology, Dialysis, Transplantation. 2017;November 20 doi: 10.1093/ndt/gfx293 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 28.Ratzan SC. The national health literacy action plan: the time has come for action. J Health Commun. 2010;15(6):575–577. [DOI] [PubMed] [Google Scholar]
- 29.Calderon JL, Zadshir A, Norris K. A survey of kidney disease and risk-factor information on the World Wide Web. MedGenMed : Medscape General Medicine. 2004;6(4):3. [PMC free article] [PubMed] [Google Scholar]
- 30.Morony S, Flynn M, McCaffery KJ, Jansen J, Webster AC. Readability of Written Materials for CKD Patients: A Systematic Review. American Journal of Kidney Diseases. 2015;65(6):842–850. [DOI] [PubMed] [Google Scholar]
- 31.Cavanaugh KL, Wingard RL, Hakim RM, Eden S, Shintani A, Wallston KA, Huizinga MM, Elasy TA, Rothman RL, Ikizler TA. Low health literacy associates with increased mortality in ESRD. Journal of the American Society of Nephrology. 2010;21(11):1979–1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kirsch IS, United S, Office of Educational R, Improvement, Educational Testing S, National Center for Education S. Adult literacy in America : a first look at the results of the National Adult Literacy Survey; 2002. [Google Scholar]
- 33.Weiner DE, Seliger SL. Cognitive and physical function in chronic kidney disease. Current Opinion in Nephrology and Hypertension. 2014;23(3):291–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Murray AM, Knopman DS. Cognitive impairment in CKD: no longer an occult burden. American Journal of Kidney Diseases. 2010;56(4):615–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barry MJ, Edgman-Levitan S. Shared decision making--pinnacle of patient-centered care. The New England journal of Medicine. 2012;366(9):780–781. [DOI] [PubMed] [Google Scholar]
- 36.Eneanya ND, Winter M, Cabral H, Waite K, Henault L, Bickmore T, Hanchate A, Wolf M, Paasche-Orlow MK. Health Literacy and Education as Mediators of Racial Disparities in Patient Activation Within an Elderly Patient Cohort. Journal of Health Care for the Poor and Underserved. 2016;27(3):1427–1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kripalani S, Weiss BD. Teaching about health literacy and clear communication. J Gen Intern Med. 2006;21(8):888–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.2016 National Healthcare Quality and Disparities Report. Rockville, MD: Agency for Healthcare Research and Quality; October 2017. AHRQ Pub. No. 17–0001. [PubMed] [Google Scholar]
- 39.Healthy People - Development of the National Health Promotion and Disease Prevention Objectives for 2030. https://www.healthypeople.gov/2020/About-Healthy-People/Development-Healthy-People-2030 Accessed 11–6-17.
- 40.Koh HK, Piotrowski JJ, Kumanyika S, Fielding JE. Healthy People a 2020 vision for the social determinants approach. Health Education & Behavior. 2011;38(6):551–557. [DOI] [PubMed] [Google Scholar]
- 41.Kucirka LM, Grams ME, Lessler J, Hall EC, James N, Massie AB, Montgomery RA, Segev DL. Association of race and age with survival among patients undergoing dialysis. JAMA. 2011;306(6):620–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yan G, Norris KC, Yu AJ, Ma JZ, Greene T, Yu W, Cheung AK. The relationship of age, race, and ethnicity with survival in dialysis patients. Clinical Journal of the American Society of Nephrology. 2013;8(6):953–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kalantar-Zadeh K, Kovesdy CP, Norris KC. Racial survival paradox of dialysis patients: robust and resilient. American Journal of Kidney Diseases. 2012;60(2): 182–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rhee CM, Lertdumrongluk P, Streja E, Park J, Moradi H, Lau WL, Norris KC, Nissenson AR, Amin AN, Kovesdy CP, Kalantar-Zadeh K. Impact of age, race and ethnicity on dialysis patient survival and kidney transplantation disparities. American Journal of Nephrology. 2014;39(3):183–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Laster M, Norris KC. Lessons Learned in Mortality and Kidney Transplant Outcomes Among Pediatric Dialysis Patients. Journal of the American Society of Nephrology. 2017;28(5):1334–1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mehrotra R, Kermah D, Fried L, Adler S, Norris K. Racial differences in mortality among those with CKD. Journal of the American Society of Nephrology. 2008;19(7):1403–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Norris K, Nissenson A. Racial disparities in chronic kidney disease: tragedy, opportunity, or both? Clinical Journal of the American Society of Nephrology. 2008;3(2):314–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5A.Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Washington (DC): National Academies Press (US); 2003. [PubMed] [Google Scholar]
- 5B.Freedman BI, Limou S, Ma L, Kopp JB. APOLl-Associated Nephropathy: A Key Contributor to Racial Disparities in CKD. Am JKidney Dis 2018;72(suppl 1):●●●-●●●. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27A.U.S. Department of Health and Human Services. 2000. Healthy People 2010. Washington, DC: U.S. Government Printing Office. [Google Scholar]; Originally developed for Ratzan SC, Parker RM. 2000. Introduction In National Library of Medicine Current Bibliographies in Medicine: Health Literacy. Selden CR, Zorn M, Ratzan SC, Parker RM, Editors. NLM Pub. No. CBM 2000–1 Bethesda, MD: National Institutes of Health, U.S. Department of Health and Human Services. [Google Scholar]


