Abstract
Background
Intimate partner violence directed at women by men continues to be a global concern. However, little is known about the factors associated with perpetrating intimate partner violence among heterosexual men.
Purpose
History of childhood sexual abuse and other sociodemographic variables were examined as potential factors associated with severe intimate partner violence perpetration toward women in a sample of heterosexual men in South Africa.
Methods
Longitudinal logistic generalized estimating equations examined associations of childhood sexual abuse and sociodemographic variables at baseline with intimate partner violence perpetration at subsequent time points.
Results
Among participants with a steady female partner, 21.81 % (190/871) reported perpetrating intimate partner violence in the past year at baseline. Having a history of childhood sexual abuse (p<.001), binge drinking (p=.002), being employed (p=.050), and more difficulty controlling sexual impulses in order to use a condom (p=.006) at baseline were associated with self-reported intimate partner violence perpetration in the past year at subsequent time points.
Conclusions
With high levels of recent severe physical and/or sexual intimate partner violence perpetration in South Africa, comprehensive interventions are urgently needed. To more fully address gender-based violence, it is important to address associated factors, including exposure to childhood sexual abuse that could impact behavior later in life and that have long-lasting and deleterious effects on men and their female partners.
Keywords: Partner abuse, Africa, Risk factors, Sexual abuse, Men
Introduction
Male-perpetrated intimate partner violence is the most common form of gender-based violence and continues to be a growing public health concern worldwide [1,2]. According to the World Health Organization, intimate partner violence is behavior by an intimate partner or ex partner that causes physical, sexual, or psychological harm, including physical aggression, sexual coercion, psychological abuse, and controlling behaviors [3]. Globally, on average, 30 % of women ages 15–49 years report experiencing physical or sexual violence by intimate partners [3] with estimates varying widely between 15 and 71 % among countries [4]. It is well established that intimate partner violence has serious implications for women who experience it, having been associated with many detrimental outcomes, including HIV [5, 6], mental health issues [2], and death due to partner perpetrated homicide [7]. In South Africa, the rates of intimate partner violence experienced by women are among the highest in the world based on data including a nationally representative sample [8], among adolescent and young adult women [9], and among women attending antenatal clinics [5]. These findings are consistent with high prevalence rates in multiple studies of male perpetration of intimate partner violence toward female partners in South Africa [6, 10, 11]. For example, one population-based study in South Africa found that the prevalence of male perpetration of lifetime physical partner violence was 42 % [12, 13].
While several important studies have examined factors that place women at risk for experiencing intimate partner violence in South Africa [5, 14, 15], there is a need to better understand characteristics of men who perpetrate intimate partner violence against women. Such an understanding will contribute to global comparisons of explanatory factors and help to develop context-specific public health prevention initiatives that have substantive impact. There is a growing body of literature that has identified men’s characteristics associated with male intimate partner violence perpetration, including having multiple sexual partners [11, 16] or concurrent sexual partners [17], inconsistent condom use [11], problem alcohol use [18], having less education [17], and child maltreatment [19, 20].
To situate the phenomenon of intimate partner violence perpetration and possible associated factors, it is important to recognize that there are several pathways of influence that may interact. Social gender norms that justify unequal, controlling, and often violent relationships with women are one explanatory pathway. The context of South Africa is marked by high levels of gender inequality and violence against women [8, 12]. Furthermore, emerging research in neuroscience suggests that traumatic events experienced in childhood, especially those that are recurrent or that are not addressed with support, can alter brain pathways that regulate emotion and social behavior and involve stress reactivity with long-lasting impact [21]. Additionally, environments of poverty and disadvantage and other life stressors can compound the negative impact of early adversity [21, 22].
One such life stressor is childhood sexual abuse, which is an understudied potential predictor of intimate partner violence perpetration. Impulse control may be protective for intimate partner violence perpetration. Older age may result in more relationship experience and maturity in resolving interpersonal differences that not only may reduce the likelihood of intimate partner violence but also may be associated with more traditional gender norms that may reinforce justifications for intimate partner violence. High religiosity may be associated with reduced violence given teachings of respect for others common to many religions but alternatively could be associated with traditional gender role norms that require enforcement possibly including intimate partner violence. Partner communication may be associated with less intimate partner violence perpetration if partners take time to talk through differences but may be more related to emotional abuse than physical or sexual intimate partner violence [13]. Binge drinking may be accompanied by disinhibition and greater intimate partner violence perpetration. Education and employment may be protective toward intimate partner violence perpetration, but greater income may exacerbate gender power differentials. In this article, we examined the history of childhood sexual abuse, age, impulse control, religiosity, partner communication, binge drinking, education, and employment as potential factors associated with intimate partner violence perpetration toward women in a sample of heterosexual men in South Africa.
Methods
Participants and Procedures
The article presents a secondary data analysis of the original 1181 men from a randomized controlled trial of an HIV risk reduction intervention whose details are described elsewhere [23]. The analytic cohort of n=871 included men with a recorded intimate partner violence outcome with a steady partner at any assessment time (e.g., baseline, 6 months, or 12 months). We compared basic demographic characteristics of those retained (n=779) and those lost to follow-up (n=92) for the analytic sample of 871. Specifically, lost to follow-up was operationalized as those who reported a response to the primary outcome at baseline only and no response at either the 6- or 12-month follow-up visit. Specifically, men lost to follow-up and men retained were similar in terms of random intervention assignment (p=.506), age (p=.078), matriculation status (p=.437), employment status (p=.286), marital status (p=.294), and residence (p=.546).
The participants were residents of townships near East London in Eastern Cape Province, South Africa, who completed questions at baseline and 6- and 12-month post-intervention. More than 98 % of the residents in these areas are Black Africans whose first language is isiXhosa. Men aged 18 to 45 years who lived in selected neighborhoods reported vaginal intercourse in the previous 3 months, did not report plans to relocate beyond a reasonable distance from the study site within the next 15 months, and had a photo ID or were willing to have their picture taken for identification purposes were eligible. Appropriate Institutional Review Board (IRB) approval was received for this study.
Measures
We analyzed data from confidential questionnaires that were completed via audio computer-assisted selfinterviewing (ACASI), which provided both audio and video presentation of the questions and response options on a laptop computer. The measures were available in isiXhosa (following translation and back translation from English), English, and a combination of isiXhosa (audio) and English (visual). For this article, we analyzed data from 871 participants who reported having a steady partner (“A main or steady partner is your wife or a woman with whom you have had a serious relationship for at least 6 months, e.g., wife, girlfriend”) in the past year.
Intimate partner violence was assessed among participants who indicated that they had a steady partner. Self-reported history of perpetrating intimate partner violence with a steady partner in the past year was assessed with three items assessing severe physical assault and sexual coercion drawn from the Revised Conflict Tactics Scale (physical violence subscale alpha=0.86; sexual coercion subscale alpha=0.87) [24]. The Conflict Tactics Scale and Revised Conflict Tactics Scale have been used in many studies with diverse populations [24] including South Africans, assessing assault perpetration among men (alpha=0.96) [25]. In this study, two items assessed various types of severe physical assault (kick; beat up; slam against a wall; hit with something that could hurt or scald or burn on purpose; and choke or use a knife, gun, or other weapon, or threatened to do so) and one item assessed severe sexual coercion (use any force to make your steady partner have sex). The responses from these three items were combined into one dichotomous variable (any intimate partner violence: yes/no) indicating the presence of severe intimate partner violence toward a steady partner in the past year if participants reported yes to any of the three questions. Because this item was operationalized to assess behavior in the past year and assessed at each time point as described above, we characterized intimate partner violence prevalence at baseline and incidence at 6 and 12 months. Specifically, men responding “yes” to any intimate partner violence denote baseline prevalence of intimate partner violence, whereas those who respond yes at 6 months, but not at baseline, denote 6-month incidence, and those who respond yes at 12 months and not at baseline or 6 months denote 12- month incidence. In short, prevalence/incidence was operationalized as the first affirmative response to any intimate partner violence.
Self-reported sociodemographic and selected health characteristics, including age, employment, marital status, housing situation and urban vs. rural location, multiple partners, and unprotected sex with main and casual partners in the past 3 months, were obtained. We assessed education and determined if they had completed matric (i.e., the 12th grade) or not. In addition, we measured binge drinking with the question, “In the past month (30 days), on how many days did you have five or more drinks of alcohol (e.g., beer, wine, brandy, or hard liquor) on the same occasion? (by occasion, we mean at the same time or within a couple of hours of each other).” Those who indicated one or more days were categorized as having engaged in binge drinking. Partner communication about condom use was assessed with one item, “Did you and a main or steady partner discuss using condoms in the past 3 months?” Self-efficacy impulse control to use condoms was derived as the mean response of three items, each measured on a five-point Likert agreement scale, assessing the participants’ ability to pause before sex in order to use a condom, even if sexually aroused; to say no to sex if neither they or their partner have a condom; and to stop sex in order to get a condom if they do not have one. Religiosity was the mean response of the reported frequency of participating in several activities including going to church or other religious activities, reading the Bible or other religious works, listening to worship music, listening to religious radio, and watching religious television programs. This measure of religiosity has been used previously in another South African sample with an alpha=0.80 [26]. Childhood sexual abuse was measured with five questions: Before you were 16 years of age, did anyone have intercourse with you against your will; did anyone force you to lick of suck her vagina or his penis; did anyone put his or her mouth on your penis against your will; did anyone force you to put your finger or an object in her vagina; did anyone put his penis or an object in your bottom or behind or rectum? A yes response to any of the five questions was categorized as having a history of childhood sexual abuse. Those who participated in the HIV risk reduction intervention vs. those who participated in the attention control intervention during the randomized controlled trial were also identified.
We took several steps to increase the validity of self-report measures that have been used in previous HIV/STD risk reduction intervention studies [27–31]. To reduce problems with memory, we asked respondents to recall sexual behaviors over a relatively brief period (i.e., 90 days), wrote the dates comprising that period on a whiteboard, and gave them calendars clearly highlighting the dates. We emphasized the importance of responding honestly, informing them that their responses would be used to create programs for South African men like themselves. We assured the participants that we would keep their responses confidential. The use of ACASI may also serve to increase participants’ motivation to respond accurately [32–34].
Data Analysis
Baseline categorical participant characteristics comparing those who were and were not intimate partner violence perpetrators were summarized using frequencies, percentages, and corresponding chi-square tests, while baseline continuous characteristics comparing those who were and were not intimate partner violence perpetrators were summarized using means, standard errors, and corresponding t tests (Table 1).
Table 1.
Baseline comparisons of SAM participants who did and did not report IPV perpetration in the past year
| No IPV perpetration in past year (n = 681) |
IPV perpetration in past year (n = 190) |
Test statistica (p value) |
|
|---|---|---|---|
| Age | 26.49 ± 0.25 | 26.33 ± 0.44 | 0.31 (.759) |
| Religiosity | 3.40 ± 0.04 | 3.18 ±0.08 | 2.37 (.018) |
| Self-efficacy impulse control to use condoms | 3.56 ± 0.04 | 3.27 ± 0.07 | 3.62 (<.01) |
| RR intervention | 353 (51.84 %) | 111 (58.42 %) | 6.14 (.046) |
| Matric | 307 (45.08 %) | 86 (45.26 %) | 0.44 (.803) |
| Employed | 201 (29.52 %) | 69 (36.32 %) | 9.06 (.011) |
| Any CSA | 114 (16.74 %) | 59 (31.05 %) | 21.14 (<.001) |
| Binge drinking | 358 (52.57 %) | 125 (65.79 %) | 13.09 (.001) |
| Partner communication | 421 (61.82 %) | 115 (60.53 %) | 36.20 (<.001) |
| Married | 42 (6.17 %) | 12 (6.32 %) | 1.01 (.604) |
| Urban | 164 (24.08 %) | 57 (30.00 %) | 5.25 (.073) |
| Live where? | |||
| In my own house/flat | 138 (20.26 %) | 31 (16.32 %) | 15.31 (.053) |
| In my family’s house | 427 (62.70 %) | 124 (65.26 %) | |
| In my partner’s house | 14 (2.06 %) | 8 (4.21 %) | |
| I rent a room | 18(2.64 %) | 4 (2.11 %) | |
| I live in a shack in someone else’s yard | 84 (12.33 %) | 23 (12.11 %) | |
| Multiple partners | 233 (34.21 %) | 95 (50.00 %) | 19.81 (<.001) |
| Any unprotected sex with main partner | 337 (49.49 %) | 113 (59.47 %) | 43.28 (<.001) |
| Any unprotected sex with casual partner | 108 (15.86 %) | 45 (23.68 %) | 8.32 (.081) |
Cell values are mean ± standard errors or frequency (%)
Test statistic p value from t test for continuous variables or chi-square comparisons among participants who do and do not report IPV
Longitudinal logistic generalized estimating equations (GEE) were employed to simultaneously examine associations of potential baseline factors and intimate partner violence perpetration at subsequent time points (i.e., 6- and 12-month follow-ups) [35]. These factors included participants’ age, religiosity, condom-use impulse-con- trol self-efficacy, matriculation, employment status, any childhood sexual abuse history, binge drinking, and partner communication. The model included intervention arm as a control variable. Model estimates were expressed as adjusted odds ratios and 95 % confidence intervals (CI) along with corresponding p values (Fig. 1). All analyses were completed using SAS version 9.4.
Fig. 1.
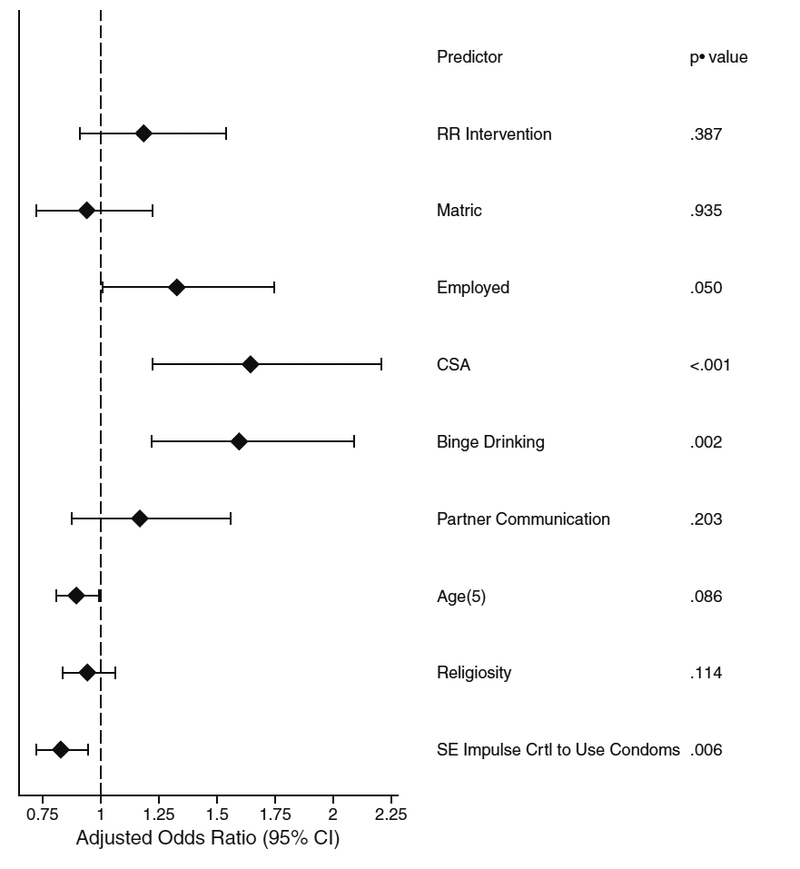
Association (odds ratios) of baseline factors on intimate partner violence (IPV) perpetration in the past year (at both the 6- and 12-month time points). Note that this figure is a graphical representation of the previous table
Results
Among participants who reported having a steady female partner, intimate partner violence prevalence at baseline was 21.81 % (190/871) and incidence at 6 and 12 months, respectively, was 7.23 % (63/871) and 5.17 % (45/871). As shown in Table 1, there were significant univariate associations between intimate partner violence perpetration and lower religiosity, lower self-efficacy impulse control to use condoms, being randomized to the HIV risk reduction intervention, being employed, history of childhood sexual abuse, binge drinking, and partner communication at baseline. Additionally, intimate partner violence perpetrators were more likely to have multiple partners and have unprotected sex with their main partner and casual partners.
Table 2 and Fig. 1 summarize the longitudinal logistic GEE analysis of intimate partner violence amongmen who reported having a steady partner in the past 3 months at the 6- and 12-month follow-up, simultaneously on time, age, religiosity, self-efficacy for sexual impulse control in order to use condoms, matriculation, employment status, any childhood sexual abuse history, binge drinking, partner communication, and intervention study arm. Participants who were employed, who had a history of childhood sexual abuse, or who were binge drinkers had significantly higher odds of being intimate partner violence perpetrators, while those who had higher self-efficacy for impulse control to use condoms had significantly lower odds of being intimate partner violence perpetrators.
Table 2.
Association (odds ratios) of baseline factors on intimate partner violence (IPV) perpetration in the past year (at both the 6- and 12-month time points)
| Predictor | OR estimate | OR confidence | limits | p value |
|---|---|---|---|---|
| RR intervention | 1.133 | 0.854 | 1.504 | .387 |
| Matric | 0.988 | 0.744 | 1.313 | .935 |
| Employed | 1.351 | 1.003 | 1.820 | .050 |
| CSA | 1.787 | 1.300 | 2.456 | <.001 |
| Binge drinking | 1.588 | 1.189 | 2.121 | .002 |
| Partner communication | 1.222 | 0.897 | 1.666 | .203 |
| Age (5 years) | 0.907 | 0.811 | 1.014 | .086 |
| Religiosity | 0.810 | 0.789 | 1.026 | .114 |
| Self-efficacy impulse control to use condoms |
0.815 | 0.706 | 0.942 | .006 |
Discussion
Our findings indicate high levels of male perpetration of severe physical and/or sexual intimate partner violence (22 %) toward female partners in the past year within steady relationships in this region in South Africa. These findings are comparable with other studies in South Africa which report rates of male intimate partner violence perpetration of 9 to 42 % depending on the time frame (lifetime vs past year), sample (general population vs those who had certain risk factors), and type of violence measured (physical, sexual, psychological, or some combination). For example, Abrahams et al. (2006) found that, in a sample of employed men, 8.8 % had perpetrated physical intimate partner violence in the past year, while 42 % had perpetrated physical intimate partner violence within the past 10 years [18]. Townsend et al. (2011) found that 41.5 % of their sample of 25–55-year-old South African men who had multiple concurrent partners perpetrated physical or sexual violence in the past 12 months with any of their partners [11]. In another study, Dunkle et al. (2006) found that 31.8 % of their sample of 15–26-year-old South African men perpetrated either physical or sexual intimate partner violence ever in their lives [6]. Given that we assessed intimate partner violence in the past year in steady relationships only, we may have underestimated the incidence of intimate partner violence since it can also occur in casual relationships as well.
In our study, we found that more binge drinking was associated with intimate partner violence perpetration. Several studies have found that problematic alcohol use is a predictor of intimate partner violence perpetration [11, 17, 36]. Abrahams found that problem drinking was associated with any sexual intimate partner violence (2004) and any physical intimate partner violence (2006) perpetrated within the past 10 years. Townsend et al. (2011) found that problem alcohol use was associated with any intimate partner violence perpetrated in the past 12 months and more specifically with physical intimate partner violence, but not just sexual intimate partner violence toward any sexual partner among men who had multiple concurrent partners.
Contrary to our finding that employed men were more likely to perpetrate intimate partner violence, research in the USA indicates that men who are unemployed are more likely to perpetrate intimate partner violence [37], and this factor is compounded when living in communities experiencing economic distress. In a US study, the rate of intimate partner violence perpetration was 4.7 % among consistently employed men compared to 7.5 % among men who experienced one period of unemployment and rose to 12.3 % when the male partner experienced two or more periods of unemployment. We did not find any studies that examined the association between employment and intimate partner violence perpetration among men in South Africa. Perhaps, men in South Africa who are employed have greater ability to purchase alcohol and/or to entertain multiple partners, compared to non-employed peers, both of which are factors associated with intimate partner violence perpetration in South Africa [11, 16, 38]. Employed men may also feel more entitled to greater gender power in relation to their female partners, which may be associated with intimate partner violence perpetration. Further exploration of the link between employment status and intimate partner violence perpetration is needed. Furthermore, contrary to prior studies among men in South Africa and elsewhere in the world, which have found that less education was associated with perpetration of intimate partner violence [13, 18], we did not find that education was associated with intimate partner violence perpetration.
We also found that men in our sample who had lower condom-use impulse-control self-efficacy were also more likely to perpetrate intimate partner violence. Lee (2012) found that men with a history of childhood family violence exposure (physical or emotional maltreatment or witnessing intraparental violence) were more likely to report difficulty in self-control in relation to violence toward a partner in particular situations compared to men without that exposure [39]. We also found that men with a history of childhood sexual abuse were more likely to perpetrate intimate partner violence. Several studies have examined composite exposures of childhood adversity (such as physical or sexual abuse, neglect, witnessing interparental violence) in relation to intimate partner violence perpetration among men [10, 17, 22, 40–44], and most found significant associations. The baseline prevalence of childhood sexual abuse in our sample was 21.81 %, which may account for our robust finding and is consistent with a global meta-analysis of childhood sexual abuse that reported a 19.3 % rate of childhood sexual abuse for boys in Africa, which was the highest rate of childhood sexual abuse for boys in the world [45]. This is the first study to our knowledge that indicates a history of childhood sexual abuse specifically associated with later intimate partner violence perpetration among men.
Other important factors to consider in understanding intimate partner violence perpetration are social gender norms, masculine identity, and power dynamics within relationships, particularly as they are influenced by early adversity and social hardship. Several studies have documented that men who perpetrate intimate partner violence are also more likely to hold adversarial beliefs about women and adhere to gender norms that are unfavorable to women [6, 46–48], and these negative views are heightened among men exposed to childhood family violence [39]. Furthermore, there is some evidence that exposure to childhood adversity may lead men to adopt violent forms of masculinities to overcome feelings of insecurity and powerlessness, as suggested by findings from a study of South African men in prison for killing their intimate partners [49]. Likewise, men who have been subject to human rights violations may interpret these experiences as a challenge to their masculinity and in turn try to exert power and control over their female partner(s) through violence [50]. Social and structural gender norms that are disadvantageous toward women may serve to reinforce these adversarial interpersonal dynamics.
There is a growing body of research that suggests that exposure to traumatic events early in childhood can effect brain development, leading to diminished capacity to inhibit a variety of impulsive behaviors [21]. Viewed from that perspective, it could be that men in our study who were exposed to childhood sexual abuse early in life may have consequently engaged in binge drinking and had difficulty with impulse control and both contributed to a greater likelihood of perpetrating intimate partner violence. This perspective is bolstered by recent findings by Roberts et al. [22] indicating that men who had a history of childhood adversity and who were exposed to stressors as adults had an elevated rate of perpetrating intimate partner violence compared with men only exposed to adult stressors. Additional research is needed to further explore the biopsychosocial pathways linking childhood sexual abuse and intimate partner violence perpetration, which likely involve compounding effects of several factors. Preventing male intimate partner violence perpetration toward women is not only important to reduce the impact of these traumatic exposures for women but also especially relevant for prevention of HIV and other sexually transmitted infections (STIs). We found that men in our study who perpetrated intimate partner violence were more likely to have multiple partners and unprotected sex with both steady and casual partners, compared with men who did not perpetrate intimate partner violence. Similar to the current study, several other studies conducted in South Africa and globally have found that perpetrating sexual and/or physical intimate partner violence is associated with having multiple partners including more casual partners [6, 11, 17,18]. In addition, the literature also shows that inconsistent condom use and coercive condom practices such as anger or condom refusal in response to a condom request are more common among men who perpetrate intimate partner violence [11, 51].
The findings need to be considered in light of several limitations. We measured severe physical and sexual intimate partner violence but not the full spectrum of intimate partner violence, which includes physical violence, psychological/emotional abuse, and coercive control. We also do not know whether the childhood sexual abuse was recurrent or occurred only one time, and we did not assess other types of childhood violence or witnessing of intimate partner violence during childhood. In addition, only men with a steady female sexual partner were included in the study; therefore, we do not know whether our findings would apply to violence perpetration among men who have sex with men. We did not find an association between intimate partner violence perpetration and partner communication, but the assessment of partner communication was limited by our use of a single-item measure. Finally, we did not assess gender norms of attitudes toward women among the men in this study, which also is an important consideration. These areas should be addressed in future research. This paper, however, has several notable strengths including measuring intimate partner violence at several time points and examining childhood sexual abuse, an important and widespread problem in an emerging area of study.
The high level of recent severe physical and/or sexual intimate partner violence perpetration among men toward their steady female partners in South Africa is alarming. These findings point to multiple avenues of intervention to reduce intimate partner violence perpetration among men, beginning with the urgent need to identify and address sexual violence perpetration against boys. Binge drinking and impulsivity especially in relation to condom use within the context of promoting more equitable gender norms also need to be addressed. Effective community-wide campaigns are needed to discourage interpersonal violence across the lifespan. To effectively address the epidemic of gender-based violence in South Africa and globally, it will be important to focus on identified risk factors for intimate partner violence perpetration.
Compliance with Ethical Standards
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards Authors Teitelman, Bellamy, Jemmott, Icard, O’Leary, Al, Ngwane, and Makiwane declare that they have no conflict of interest. All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Financial Disclosure None reported.
Funding This research was supported by the National Institutes of Health grants R01 HD053270 to John B. Jemmott III and K01 MH080649 to Anne M. Teitelman from the National Institute of Mental Health, with additional support from the Penn Center for AIDS Research, funded by grant P30 AI045008 from the National Institute of Allergy and Infectious Diseases.
Role of the Sponsors The National Institute had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Publisher's Disclaimer: Disclaimer The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Watts C, Zimmerman C. Violence against women: Global scope and magnitude. Lancet. 2002;359(9313):1232–1237. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization/London School of Hygiene and Tropical Medicine. Preventing intimate partner and sexual violence against women: Taking action and generating evidence. Geneva, Switzerland: World Health Organization; 2010. http://whqlibdoc.who.int/publications/2010/9789241564007_eng.pdf. Accessibility verified July 5, 2016.
- 3.World Health Organization. Violence against women. Geneva, Switzerland; 2013. http://www.who.int/mediacentre/factsheets/fs239/en/ Accessibility verified July 5, 2016.
- 4.Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH, WHO Multi-country Study on Women’s Health and Domestic Violence against Women Study Team,. Prevalence of intimate partner violence: Findings from the WHO multi-country study on women’s health and domestic violence. Lancet. 2006;368(9543): 1260–1269. [DOI] [PubMed] [Google Scholar]
- 5.Dunkle KL, Jewkes RK, Brown HC, Gray GE, Mclntryre JA, Harlow SD. Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. Lancet. 2004;363(9419):1415–1421. [DOI] [PubMed] [Google Scholar]
- 6.Dunkle KL, Jewkes RK, Nduna M, et al. Perpetration of partner violence and HIV risk behaviour among young men in the rural Eastern Cape, South Africa. AIDS (London, England). 2006;20(16):2107–2114. [DOI] [PubMed] [Google Scholar]
- 7.Seedat M, Van Niekerk A, Jewkes R, Suffla S, Ratele K. Violence and injuries in South Africa: Prioritising an agenda for prevention. Lancet. 2009;374(9694):1011–1022. [DOI] [PubMed] [Google Scholar]
- 8.Gass JD, Stein DJ, Williams DR, Seedat S. Intimate partner violence, health behaviours, and chronic physical illness among South African women. South African medical journal=Suid-Afrikaanse tydskrif vir geneeskunde. 2010;100(9):582–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Swart LA, Seedat M, Stevens G, Ricardo I. Violence in adolescents’ romantic relationships: Findings from a survey amongst school- going youth in a South African community. J Adolesc 2002;25(4):385–395. [DOI] [PubMed] [Google Scholar]
- 10.Gupta J, Silverman JG, Hemenway D, Acevedo-Garcia D, Stein DJ, Williams DR. Physical violence against intimate partners and related exposures to violence among South African men. CMAJ : Canadian Medical Association journal=journal de l’Association medicale canadienne 2008;179(6):535–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Townsend L, Jewkes R, Mathews C, et al. HIV risk behaviours and their relationship to intimate partner violence (intimate partner violence) among men who have multiple female sexual partners in Cape Town, South Africa. AIDS Behav 2011;15(1):132–141. [DOI] [PubMed] [Google Scholar]
- 12.Jewkes R, Sikweyiya Y, Morrell R, Dunkle K. Gender inequitable masculinity and sexual entitlement in rape perpetration South Africa: Findings of a cross-sectional study. PloS one. 2011;6(12): e29590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fulu E, Jewkes R, Roselli T, Garcia-Moreno C. Prevalence of and factors associated with male perpetration of intimate partner violence: Findings from the UN multi-country cross-sectional study on men and violence in Asia and the Pacific. Lancet Glob Health. 2013;1(4):e187–207. [DOI] [PubMed] [Google Scholar]
- 14.Jewkes R, Dunkle K, Nduna M, et al. Factors associated with HIV sero-status in young rural south African women: Connections between intimate partner violence and HIV Int J Epidemiol 2006;35(6):1461–1468. [DOI] [PubMed] [Google Scholar]
- 15.Kalichman SC, Simbayi LC, Kaufman M, et al. Gender attitudes, sexual violence, and HIV/AIDS risks among men and women in Cape Town, South Africa. J. Sex Res 2005;42(4):299–305. [DOI] [PubMed] [Google Scholar]
- 16.Jewkes R, Dunkle K, Koss MP, et al. Rape perpetration by young, rural South African men: Prevalence, patterns and risk factors.Soc Sci Med (1982). 2006;63(11):2949–2961. [DOI] [PubMed] [Google Scholar]
- 17.Abrahams N, Jewkes R, Hoffman M, Laubsher R. Sexual violence against intimate partners in Cape Town: Prevalence and risk factors reported by men. Bull World Health Organ 2004;82:330–337. [PMC free article] [PubMed] [Google Scholar]
- 18.Abrahams N, Jewkes R, Laubscher R, Hoffman M. Intimate partner violence: Prevalence and risk factors for men in Cape Town, South Africa. Violence Vict 2006;21(2):247–264. [DOI] [PubMed] [Google Scholar]
- 19.Millett LS, Kohl PL, Jonson-Reid M, Drake B, Petra M. Child maltreatment victimization and subsequent perpetration of young adult intimate partner violence: An exploration of mediating factors. Child Maltreatment. 2013;18(2):71–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McKinney C, Caetano R, Ramisetty-Mikler S, Nelson S. Childhood family violence and perpetration and victimization of intimate partner violence: Findings from a national population based study of couples. Ann Epidemiol 2009;19(1):25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jemmott JB 3rd, Jemmott LS, O’Leary A, et al. Cluster-randomized controlled trial of an HIV/sexually transmitted infection risk-reduction intervention for South African men. Am J Public Health 2014;104(3):467–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Strauss M, Hamby S, Boney-McCoy S, Sugerman DB. The revised conflict tactics scale (CTS2). J Fam Issues 1996;17(3):283–316. [Google Scholar]
- 23.Straus MA, Mickey EL. Reliability, validity, and prevalence of partner violence measured by the conflict tactics scales in male-dominant nations. Aggress Violent Behav 2012;17:463–474. [Google Scholar]
- 24.O’Leary A, Jemmott JB 3rd, Jemmott LS, et al. Moderation and mediation of an effective HIV risk-reduction intervention for South African adolescents. Ann Behav Med 2012;44(2):181–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jemmott JB 3rd, Jemmott LS, Fong GT, Morales KH. Effectiveness of an HIV/STD risk-reduction intervention for adolescents when implemented by community-based organizations: A cluster-randomized controlled trial. Am J Public Health 2010;100(4): 720–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jemmott LS, Jemmott JB 3rd, O’Leary A. Effects on sexual risk behavior and STD rate of brief HIV/STD prevention interventions for African American women in primary care settings. Am J Public Health 2007;97(6):1034–1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jemmott JB 3rd, Jemmott LS, Braverman PK, Fong GT. HIV/STD risk reduction interventions for African American and Latino adolescent girls at an adolescent medicine clinic: A randomized controlled trial. Arch Pediatr Adolesc Med 2005;159(5):440–449. [DOI] [PubMed] [Google Scholar]
- 28.Jemmott JB 3rd, Jemmott LS, Fong GT. Abstinence and safer sex HIV risk-reduction interventions for African American adolescents: A randomized controlled trial. J Am Med Assoc 1998;279(19): 1529–1536. [DOI] [PubMed] [Google Scholar]
- 29.Jemmott JB 3rd, Jemmott LS, Fong GT. Reductions in HIV risk- associated sexual behaviors among black male adolescents: Effects of an AIDS prevention intervention. Am J Public Health 1992;82(3):372–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Metzger DS, Koblin B, Turner C, et al. Randomized controlled trial of audio computer-assisted self-interviewing: Utility and acceptability in longitudinal studies. HIVNET vaccine preparedness study protocol team. Am J Epidemiol 2000;152(2):99–106. [DOI] [PubMed] [Google Scholar]
- 31.Hewett PC, Mensch BS, Erulkar AS. Consistency in the reporting of sexual behaviour by adolescent girls in Kenya: A comparison of interviewing methods. Sex Transm Infect, 80 (Suppl 2). 2004, p. ii43–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Johnson TP, Fendrich M, Mackesy-Amiti ME. Computer literacy and the accuracy of substance use reporting in an ACASI survey. Soc Sci Comput Rev 2010;28(4):515–523. [Google Scholar]
- 33.Liang K-Y, Zeger S. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22. [Google Scholar]
- 34.Foran HM, O’Leary KD. Alcohol and intimate partner violence: A meta-analytic review. Clin Psychol Rev 2008;28(7):1222–1234. [DOI] [PubMed] [Google Scholar]
- 35.Benson ML, Fox GL. When violence hits home: How economics and neighborhood play a role. Washington, DC: U.S. Department of Justice, National Institute of Justice;2004. [Google Scholar]
- 36.Tsai AC, Leiter K, Heisler M, et al. Prevalence and correlates of forced sex perpetration and victimization in Botswana and Swaziland. Am J Public Health 2011;101(6):1068–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim HK, Laurent HK, Capaldi DM, Feingold A. Men’s aggression toward women: A 10-year panel study. J Marriage Fam 2008;70(5):1169–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee RD, Walters ML, Hall JE, Basile KC. Behavioral and attitu- dinal factors differentiating male intimate partner violence perpetrators with and without a history of childhood family violence. J Fam Violence 2012;28(1):85–94. [Google Scholar]
- 39.Watt ME, Scrandis DA. Traumatic childhood exposures in the lives of male perpetrators of female intimate partner violence. J Interpers Violence 2013;28(14):2813–2830. [DOI] [PubMed] [Google Scholar]
- 40.Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: Building a new framework for health promotion and disease prevention. JAMA. 2009;301(21):2252–2259. [DOI] [PubMed] [Google Scholar]
- 41.Roberts AL, McLaughlin KA, Conron KJ, Koenen KC. Adulthood stressors, history of childhood adversity, and risk of perpetration of intimate partner violence. Am J Prev Med 2011;40(2):128–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Welles SL, Corbin TJ, Rich JA, Reed E, Raj A. Intimate partner violence among men having sex with men, women, or both: Earlylife sexual and physical abuse as antecedents. J Community Health 2011;36(3):477–485. [DOI] [PubMed] [Google Scholar]
- 43.White H, Widom C. Intimate partner violence among abused and neglected children in young adulthood: The mediating effects of early aggression, antisocial personality, hostility and alcohol problems. Aggress Behav 2003;29(4):332–345. [Google Scholar]
- 44.Widom CS, Czaja S, Dutton MA. Child abuse and neglect and intimate partner violence victimization and perpetration: A prospective investigation. Child Abuse Negl 2014;38(4): 650–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stoltenborgh M, van Ijzendoorn MH, Euser EM, Bakermans-Kranenburg MJ A global perspective on child sexual abuse: Meta-analysis of prevalence around the world. Child Maltreatment. 2011;16(2):79–101. [DOI] [PubMed] [Google Scholar]
- 46.Santana MC, Raj A, Decker MR, La Marche A, Silverman JG. Masculine gender roles associated with increased sexual risk and intimate partner violence perpetration among young adult men. J Urban Health 2006;83(4):575–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Krishnan S, Rocca C, Hubbard A, et al. Do changes in spousal employment status lead to domestic violence? Insights from a prospective study in Bangalore, India. Soc Sci Med 2010;70(136):e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kalichman S, Simbay LC, Cain D, et al. Sexual assault, sexual risks and gender attitudes in a community sample of South African men. AIDS Care. 2007;19(20):e7. [DOI] [PubMed] [Google Scholar]
- 49.Mathews S, Jewkes R, Abrahams N. ‘I had a hard life’ exploring childhood adversity in the shaping of masculinities among men who killed an intimate partner in South Africa. Brit J Criminol 2011;51(6):960–977. [Google Scholar]
- 50.Gupta J, Reed E, Kelly J, Stein DJ, Williams DR. Men’s exposure to human rights violations and relations with perpetration of intimate partner violence in South Africa. J Epidemiol Community Health 2012;66(6):e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Decker M, Seage G, Hemenway D, et al. Intimate partner violence functions as both a risk marker and risk factor for women’s HIV infection: Findings from Indian husband-wife dyads. J Acquir Immune Defic Syndr 2009;51 593–600. [DOI] [PMC free article] [PubMed] [Google Scholar]


