Abstract
Total hip replacement (THR) and, particularly, total knee replacement (TKR), are painful surgical procedures. Effective postoperative pain management leads to a better and earlier functional recovery and prevents chronic pain. Studies on the control of pain during the postoperative rehabilitation period are not common. The aim of this study is to present results of a perioperative anesthetic protocol, and a pain treatment protocol in use in the Orthopaedic and the Rehabilitation intensive units of our Hospital. 100 patients (50 THR and 50 TKR) were retrospectively included in this observational study. Numeric Rating Scale (NRS) for pain at rest registered in the clinical sheet was retrieved for all patients and analyzed with respect to the spinal anaesthesia given for the surgery, local analgesia, analgesia protocol adopted during the postoperative days in the Orthopaedic Unit, the antalgic treatment given during the stay within the Rehabilitation Unit, the postoperative consumption of rescue pain medication, and any collateral effect due to the analgesic therapy. Patients reached standard functional abilities (walking at least 50 meters and climbing/descending stairs) at a mean length of 8 days without medication-related complications. Mean NRS during the time of stay was 1.3 ± 0.3 for THR and 1.3 ± 0.2 for TKR) and maximum mean NRS was 1.8 ± 0.5 for TKR and 1.8 ± 0.6 for THR. The use of rescue therapy in the rehabilitation guard was correlated with the mean NRS pain and the maximum NRS pain. A very good control of pain with the perioperative anesthetic protocol and pain treatment protocol in use was obtained.
Keywords: multimodal analgesic protocol, pain, rehabilitation, total joint replacement
1. Introduction
It is well documented in literature that effective pain management leads to a better and earlier functional recovery after hip or knee prosthetic surgery and prevents chronic pain.[1–3] However, some reports demonstrate that in more than 50% of the total hip replacement (THR) cases, postoperative pain management strategies adopted were not successful, and after total knee replacement (TKR), 75% of patients complained of moderate to severe chronic pain.[4,5] The critical role of postoperative pain within orthopedic surgery procedures is demonstrated by the fact that the effectiveness of a THR or TKR is often limited by the postoperative pain management itself.[6] In fact, intensive post-surgical rehabilitation, which has a fundamental role in recovering and maintaining the patient's complete movement abilities, can be hindered when a proper analgesia is not delivered to the patient, leading to worse patients’ satisfaction with their surgery. As additional consequence, risks of thromboembolic disorders and infections can be intensified, which can lead to delays in hospital discharge, thus causing an increase in healthcare costs.[7–8] Nevertheless, the existence of a possible transition between acute pain due to intraoperative tissue damage and long-term postoperative pain, which is now referred to as central sensitization, has been documented.[9–10] If left untreated, acute pain can lead to long-term emotional and psychological distress that has the potential to develop into a chronic pain state which is even much more difficult to manage.[4,9,11]
In order to best manage postoperative pain, several protocols have been studied and adopted in literature.[12–17] To reduce the occurrence of collateral effects, the analgesia protocol should be multimodal[18–20] which consists of the employment of more than 2 different drugs or modalities with different mechanisms or sites of action for synergistic effects on pain and should block pain at its origin.[6] Horlocker[8] demonstrated that, in order to minimize the use of opioid analgesics, employing peripheral nerve blockages (PNB) together with a combination of analgesic agents allows early mobilization and helps patient's rehabilitation, reducing hospitalization times and costs. The use of regional analgesic techniques was found to improve early rehabilitation after major knee surgery by effectively controlling pain during continuous passive motion, thus hastening the convalescence.[21]
Based on these assumptions, in order to obtain optimal control of postoperative pain and facilitating early rehabilitation in THR and TKR patients, at the Rizzoli-Sicilia Department in Bagheria an apposite perioperative anesthetic protocol, and a pain treatment protocol during the rehabilitation period was established. The aim of this study is to present the effectiveness of such protocols on postoperative pain throughout patient's stay in the Orthopaedic Unit and the Rehabilitation Intensive Unit of the Department.
2. Methods
2.1. Study design
The study is an observational retrospective cohort-study carried out through the retrieval of information on hospital medical records. The study was approved by the local ethical committee (N. 0007675).
2.2. Patient sample
Numeric Rating Scale (NRS) for pain reduction was defined as a primary endpoint. In order to identify a statistical meaningful sample of patients a power analysis was conducted, according to the available literature,[22] reporting that the NRS value of patients receiving a total joint replacement is around 7.9 ± 1.7 (mean and standard deviation), and the minimum improvement clinically accepted requires a pain reduction of 20%. Considering these factors, the least clinically significant difference is 1.58 NRS points. If a two-sided error of 0.05 and a power of 0.9 are assumed, together with a minimal clinically significant difference of 1.58 NRS points with a standard deviation of 1.7 points, the resulting minimal number of cases to be studied is 25. To evaluate the data as precisely as possible, and taking in consideration some missing NRS values within medical archives, medical records of 50 patients who underwent THR and 50 on TKR hospitalized within the Intensive Rehabilitation Unit from January 2017 to December 2017 were retrospectively evaluated, and included in the study. All patients underwent a primary THR or TKR for osteoarthritis (OA) in the Orthopaedic Unit of the same Department. They were then admitted to the intensive rehabilitation Unit from the second postoperative day (POD), according to hospital standards. Those patients that experienced complications during their hospital stay, such as vein thrombosis, severe anemia, cardiovascular problems, acute psychiatric disorders, or who had previous history of drug addiction, medication-related allergies, cerebral infarction, or severe neurological lesions, acute heart or renal diseases or rheumatic diseases, were excluded from this study. Any medical records with missing values of NRS were also excluded.
On the same day of surgery, patients initiated a conventional rehabilitation training, consisting of two 30 minutes daily sessions at the Orthopaedic Unit, and then they continued two 90 minutes daily sessions at the Intensive Rehabilitation Unit.
The discharge criteria included patients demonstrating independent transfer, walking with crutches with partial weight bearing on the operated limb for at least 50 meters, and stair ambulation.
2.3. Evaluation criteria
Pain intensity at rest, as measured by the NRS (0 = no pain-10 = worst pain) registered in the clinical sheet by nurses 3 times a day (morning, afternoon, and night), was retrieved for all patients during both their hospital stay in the Orthopedic Surgery and the Rehabilitation Unit.
The following variables were also retrieved: hospitalization duration, kind of anaesthesia given for the surgery, local analgesia (if given), analgesia protocol adopted during the first few days immediately after surgery until the admittance of patients to the Rehabilitation Unit, antalgic treatment given during the stay within the Rehabilitation Unit, postoperative consumption of rescue pain medication, and any collateral effect due to the analgesic therapy. Moreover, the modified Barthel Index[23] of patients upon discharge from the Rehabilitation Unit was calculated. Other values, such as age, gender, and BMI were recorded as well.
2.4. Anesthetic protocol for surgical intervention and for postoperative pain control
In all the cases, Fentanyl (1–2 mcg/kg-1) and Midazolam (0,02 mg/kg) were used for anesthetic premedication. Patients undergoing to total joint replacement received subarachnoid anesthesia with levobupivacaine 0.5% 15 mg after identifying L4/L5 level for knee replacements, and after identifying L3/L4 level for hip replacement.
In patients undergone TKR a femoral nerve block (FNB) or an adductor canal block (ACB) was performed during the intervention, while in some patients undergone THR a lumbar plexus block (LPB) was performed.
This procedure was always performed using a single shot under ultrasound guidance— electrical nerve stimulation (ENS) guidance through the atraumatic 18 gauge needle with an in-plane lateromedial approach, inserting a 20 gauge catheter with levobupivacaine 0.5% 10 to 15 mg in 20 ml NaCl 0.9%. The correct positioning was verified with the ultrasound view of the 10 ml spread of levobupivacaine 5 mg/ml. Peripheral blocks both in TKR and THR were removed before the patients’ admission at the Rehabilitation Unit.
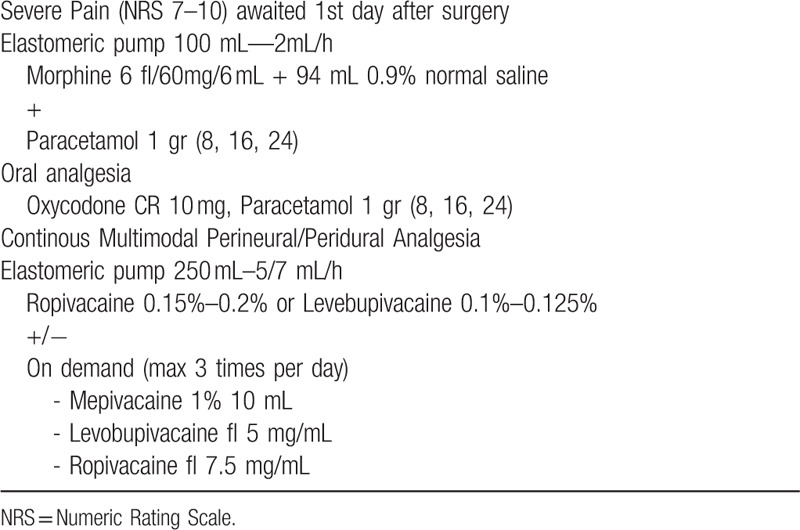
In all cases, oral therapy and intravenous patient-controlled analgesia were used postoperatively, according to the specific protocols illustrated in Table 1.
Table 1.
Postoperative analgesic protocol.
2.5. Pain control protocol in the Rehabilitation Unit
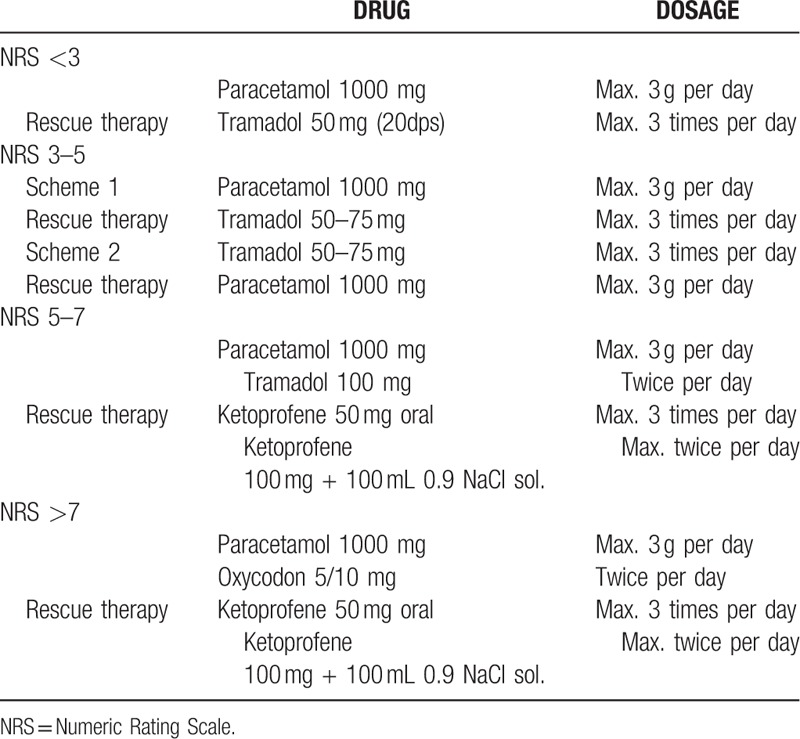
Regarding the postoperative pain management, all patients were given regular oral or parenteral painkillers following a protocol established in the operative Unit in agreement with hospital anesthesiologists, and based on the World Health Organization, 1986 pain relief ladder.[24] Rescue analgesics were used when needed according to the protocol, as reported in Table 2.
Table 2.
Pain control protocol in the Rehabilitation Unit.
2.6. Statistical analysis
Continuous data were expressed as mean and the standard deviation of the mean, categorical data were expressed as frequency and percentage. The Kolmogorov–Smirnov test was performed to test normality of continuous variables. Because of non-normality of NRS score, differences in patients who received a peripheral nerve block and those who did not receive it were explored by means of the Mann–Whitney test calculated by exact method for small samples.
The Mann–Whitney test was also used to assess the influence of gender on the NRS score. Patients’ age and BMI were correlated to the NRS values through the Spearman rank correlation.
The Fisher Chi-square test was performed to investigate the balance of gender between the groups (PNB and not PNB, and between FNB and ACB). The T-test was performed to investigate the balance of age and BMI between the groups (PNB and not PNB, and between FNB and ACB). For the evaluation of the pain level evolution along the hospitalization, the Wilcoxon repeated measures non parametric test evaluated by exact methods for small samples was used. The Wilcoxon test with Bonferroni correction for multiple comparison was used for the evaluation of the possible differences within the 3 NRS values recorded daily.
All statistical analyses were considered significant for P < .05 and were performed using SPSS v.19.0 (IBM Corp, Armonk, NY).
3. Results
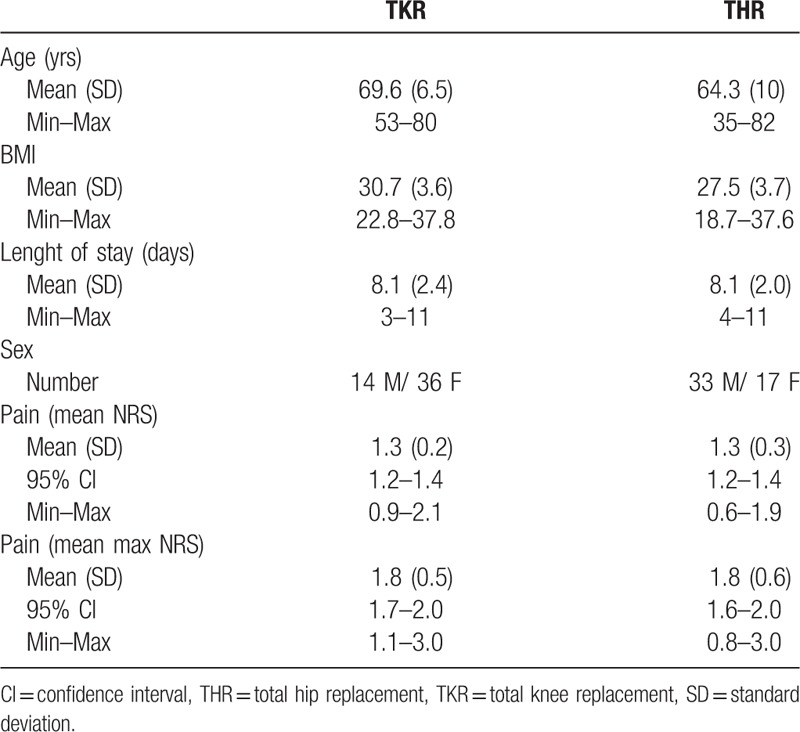
The average age of the patients was 64.26 ± 10 years for the THR Group and 69.7 ± 6.5 years for the TKR Group. General data of patients are reported in Table 3. The mean hospital stay was 8.1 ± 2.0 days for the THR Group and 8.1 ± 2.4 days for the TKR Group. At discharge, all patients reached the standard goals of rehabilitation after TKR and THR, such as walking with crutches with partial weight bearing on the operated limb, and stair ambulation. Modified Barthel Index was 87.6 ± 9.4 for TKR and 86.3 ± 13.5, for THR respectively, at discharge from the Rehabilitation Unit.
Table 3.
General data on patients.
A PNB was positioned in all the TKR patients (32 FNB, 18 ACB) and in 25 THR patients (LPB). No difference between THR patients with or without PNB and between TKR patients who received FNB or ACB was found in terms of mean and maximum value of pain in the postoperative period.
3.1. NRS for pain
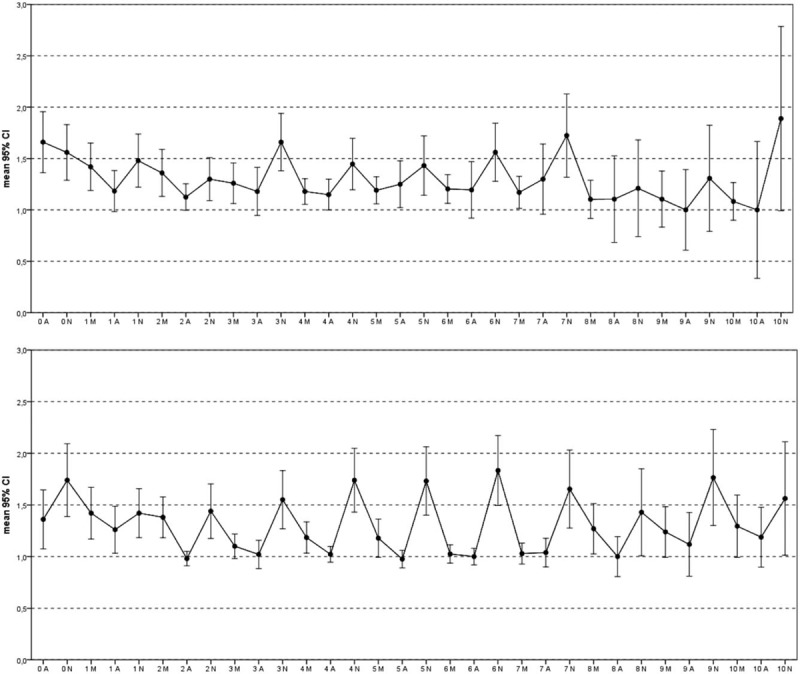
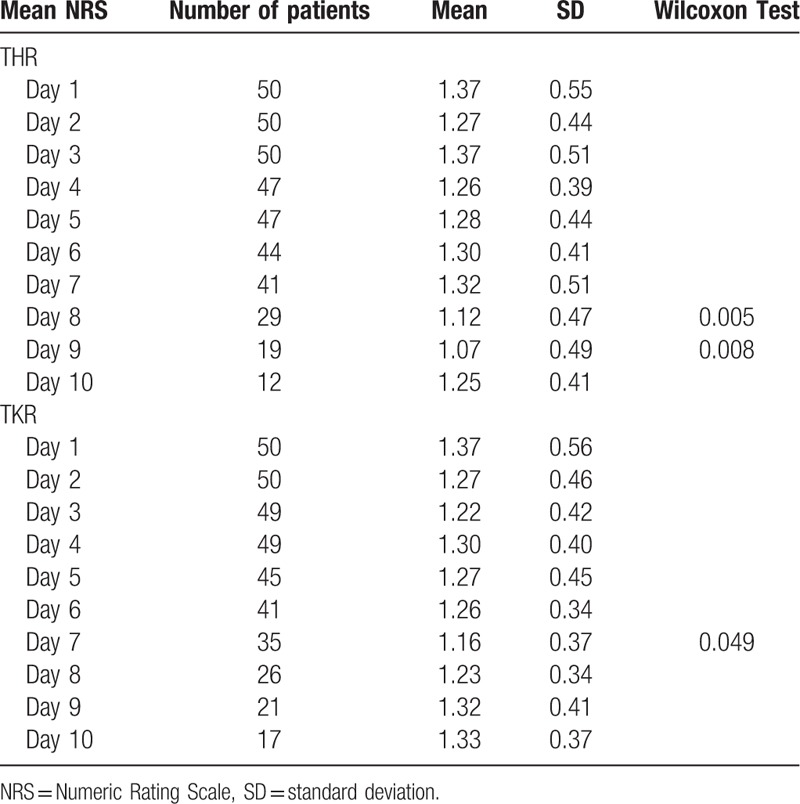
Mean pain during the time of stay as measured by NRS was 1.3 ± 0.3 for THR and 1.3 ± 0.2 for TKR (Fig. 1). The maximum pain registered during the hospital stay was 1.8 ± 0.5 for TKR and 1.8 ± 0.6 for THR. The trend of pain for both groups along the hospitalization period is reported in Figure 2. Mean NRS reduced throughout the hospitalization: for THR the difference between NRS value at POD 1 was significantly different from the NRS value at day 8 (P = .005) and 9 (P = .008), for TKR it was different between day 1 and day 7 (P = .049) (Table 4). An increase of pain was always noted in the night both for THR and TKR (P < .017). At discharge mean pain was respectively 1.9 ± 1.2 for THR and 1.6 ± 1 for TKR. Sex, BMI and age were not correlated to the amount of pain and to the type of PNB.
Figure 1.
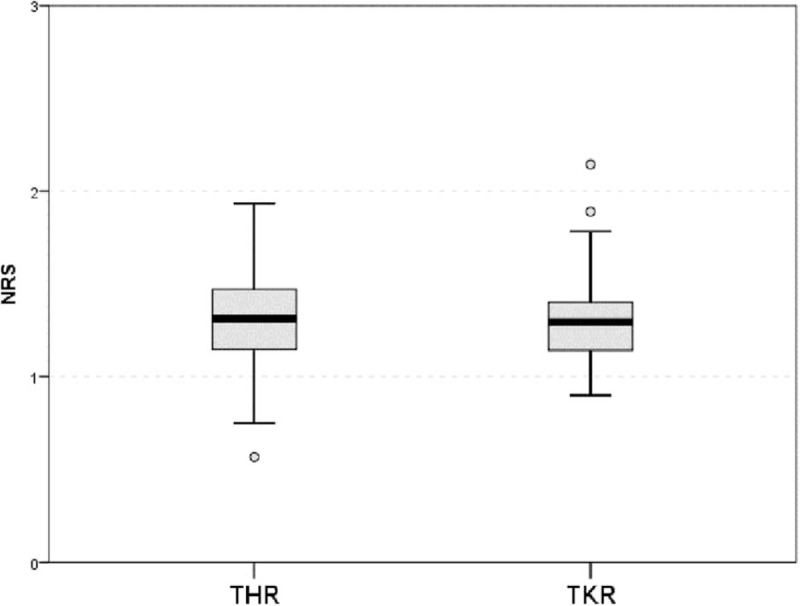
Mean and 95% CI NRS along the entire hospital stay for THR and TKR. CI = confidence interval, NRS = Numeric Rating Scale, THR = total hip replacement, TKR = total knee replacement.
Figure 2.
Daily (morning, afternoon, and night) NRS measurement (mean and 95% CI) along the hospital stay respectively for THR (upper graph) and TKR (lower graph). CI = confidence interval, NRS = Numeric Rating Scale, THR = total hip replacement, TKR = total knee replacement.
Table 4.
NRS for pain along the hospitalization.
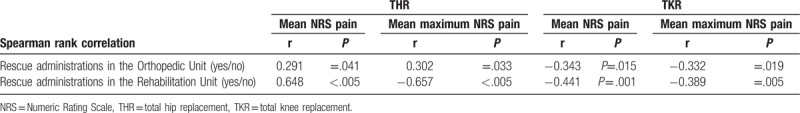
3.2. Additional consumption of analgesics and complication rate
The 2 groups consumed a similar amount of additional analgesics as a rescue supplement to the regular intake of painkillers prescribed until discharge. There were no medication-related complications, such as nausea and vomiting. There were no cases of wound infection or a delay in wound healing. In the THR Group, age was correlated with a greater consumption of rescue therapy in the orthopaedic guard (r = 0.315, 0 = 0.26). In both groups, the use of rescue therapy in the rehabilitation guard was correlated with the mean NRS pain and the maximum NRS pain (Table 5).
Table 5.
Rescue therapy consumption.
4. Discussion
THR and, particularly, TKR, have a reputation for being especially painful procedures from which to recover. Recently, great attention has been paid to postoperative pain control, particularly in the context of the so-called “fast track” protocols in which the accelerated rehabilitation for fast recovery requires pain-free patients, obtained with multimodal anesthetic protocols.[25] However, also in standard protocols for patients who undergo THR or TKR and not included in “fast track” protocols, perioperative, and postoperative pain control, particularly during the rehabilitation phase, is currently mandatory. Since main reviews have concluded that, as a result of low quality of evidence, small sample sizes and heterogeneity of trial designs, as well as the designation of optimal procedure-specific analgesic regimen after THR and TKR is not possible,[26–27] we designed our own multimodal anesthetic protocol.
The Italian Decree Law n. 38 adopted on March 15, 2010, known as the “Anti-pain Law”, was one of the first decrees in Europe devoted to guaranteeing access to palliative care and pain therapies to patients, within the public health system. In order to promptly dispense the most appropriate antalgic treatment, both the pain characteristics and their evolution during the admittance time must be registered in medical records used in all healthcare facilities. This is generally carried out through recording 3 daily scores by means of NRS, a score of established validity and reliability for assessing postoperative pain.[28] In the present study, NRS values recorded in the medical files were retrieved and associated to the anesthesiological protocol used both for surgery and during rehabilitative hospital stay.
The results of this retrospective study on a cohort of patients who underwent uncomplicated THR and TKR demonstrated well-controlled pain both in the early postoperative period and in the intensive rehabilitation phase, with a mean NRS score of 1.3 ± 0.3 and 1.3 ± 0.2 respectively for THR and for TKR. Unfortunately, there are not many studies available in which the amount of pain is measured after the first 72 postoperative hours, and particularly during the postoperative rehabilitation period.
Among available data in TKR, Lisi[29] reported a NRS value under 3, at POD 2 in a mininvasive protocol for TKR, Snyder[30] a mean NRS value ranging between 3.24 (POD 0) and 4 (POD 3), and Gerbershagen[31] a mean maximum pain at POD 1 of 5.56. Rakel[32] reported a median resting pain NRS intensity of 4 at POD 2, and Choi[33] reported a mean NRS value of 4.6 in patients who underwent TKR and were treated with FNB at POD 2. Castorina,[34] comparing a fast track protocol versus a standard protocol in TKR, reported a level of Visual Analogic Scale (VAS) pain at POD 3 of 3.38 and 4.40, respectively. Benditz[5] in a prospective study over 2 years in which they increased the quality of pain management in TKR, reported a reduction of NRS maximum pain from 6.45 to 5.44 at POD 1.
Only 1 study reporting NRS along the course of a 21-day rehabilitation stay was retrieved,[35] reporting a decrease of the NRS from 5.2 at the baseline to 0.9 in patients treated with Tapentadol and from 5 to 2.6 in patients treated with Paracetamol.
As regards THR, Gerbershagen[31] reported an NRS maxim score of 4.95 at POD 1, and Johnson[36] a median maximum NRS pain score across 3 groups (posterior LPB, periarticular infiltration with ropivacaine, ketorolac, and epinephrine and periarticular infiltration with liposomal bupivacaine, ketorolac, and epinephrine) at POD 1 respectively of 3.0, 4.0, and 3.0.
NRS scores in the present study were far below most of these findings, demonstrating the effectiveness of the analgesic protocol proposed both for surgery and for postoperative management of pain in THR and TKR, without medical-related conditions, such as nausea and vomiting. Furthermore, patients functionality and participation to rehabilitation session was not influenced by the effects of the pharmacological therapies.
The consumption of rescue analgesics on demand was, as expected, related to the mean and the maximum NRS value and it was, however, effective in containing pain throughout the hospital stay.
PNB was included in the multimodal protocol in all TKR patients and in a subgroup of THR patients. Being the LPB of recent introduction in our hospital at the time of this retrospective study, not all the patients had the procedure. Moreover, based on the surgeon choice, some TKR patients received an ACB and others a FNB. With the number of patients included, no differences were found between THR patients who received a PNB and those who did not. While there is evidence that PNB as adjunctive techniques to systemic analgesia reduced pain intensity when compared with systemic analgesia alone after major knee surgery and in THR, at the moment there are no strong evidences confirming our findings on the effects of the association of PNB and spinal analgesia.[36–38]
Furthermore, as concerns the absence of postoperative pain differences between the FNB and the ACB in TKR patients, this result confirms previous studies which demonstrated no difference concerning analgesia quality with the 2 procedures.[39–42]
There are some limitations in the present study. First, the preoperative pain level was not reported. Actually, preoperative pain intensity (NRS) was found to be a significant predictor of high pain (at rest and during movement) following TKR,[32] and an independent risk indicator for poor function at 6 months after surgery, slowing down rehabilitation in the immediate postoperative period.[4] However, since the objective of our study was to monitor pain during the postoperative rehabilitation period in relation to the protocols in use, this point was not considered. A further prospective study is going to be planned to evaluate chronic neuropathic pain after TKR that takes into account, in addition to the drugs used, also the effects of preoperative pain and all the individual psychosocial and clinical factors considered responsible for the central sensitization.
Second, pain level was measured only at rest, considering only the nursing registration, without taking into account possible pain related to the physiotherapy or to movement. To this purpose, Ernlewein et al, 2017[4] reports interesting findings after hip surgery in terms of pain during motion and pain at rest. In his study, pain did not continuously decrease over the course of the first postoperative week, but, after an early decrease, pain increased again and this was associated with the progress of mobilization, particularly in patients with chronic pain before surgery. These findings suggest that the temporal dimension of pain (e.g. time pattern of pain intensity in response to recovery and mobilization) requires greater consideration. Further studies are guaranteed to overcome these limitations. Furthermore, the inclusion in the study only of patients with a complete dataset of NRS in the medical records during the hospital stay could be considered a potential selection bias.
In conclusion, the present study reports a very good control of pain with the perioperative anesthetic protocols, and pain treatment protocols in use after primary uncomplicated THR and TKR throughout the Orthopaedic and the Rehabilitation Unit stay. Patients reached standard functional abilities (walking at least 50 meters and climbing/descending stairs) at a mean length of 8 days with a mean NRS pain at discharge of about 1.9 points for THR and 1.6 for TKR without medication-related complications.
Acknowledgments
The authors wish to thanks Elettra Pignotti, biostatistician, for the support in the statistical analysis of data.
Author contributions
Conceptualization: Marcello Ciccarello, Giulia Letizia Mauro, Stefano Bonarelli, Maria Grazia Benedetti.
Data curation: Maria Laura De Luca, Marcello Ciccarello, Manfredi Martorana, Davide Infantino, Maria Grazia Benedetti.
Methodology: Marcello Ciccarello, Maria Grazia Benedetti.
Supervision: Giulia Letizia Mauro, Stefano Bonarelli.
Writing – original draft: Manfredi Martorana, Maria Grazia Benedetti.
Writing – review & editing: Maria Grazia Benedetti.
Footnotes
Abbreviations: ACB = adductor canal block, FNB = femoral nerve block, LPB = lumbar plexus block, NRS = Numeric Rating Scale, POD = postoperative day, THR = total hip replacement, TKR = total knee replacement.
The authors have no conflicts of interest to disclose.
References
- [1].Fu PL, Xiao J, Zhu YL, et al. Efficacy of a multimodal analgesia protocol in total knee arthroplasty: a randomized, controlled trial. J Int Med Res 2010;38:1404–12. [DOI] [PubMed] [Google Scholar]
- [2].Macfarlane JR, Prasad GA, Chan VWS, et al. Does regional anaesthesia improve outcome after total hip arthroplasty? A systematic review. Br J Anaesth 2009;103:335–45. [DOI] [PubMed] [Google Scholar]
- [3].Ibrahim MS, Khan MA, Nizam I, et al. Peri-operative interventions producing better functional outcomes and enhanced recovery following total hip and knee arthroplasty: an evidence-based review. BMC Med 2013;11:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Erlenwein J, Müller M, Falla D, et al. Clinical relevance of persistent postoperative pain after total hip replacement—a prospective observational cohort study. J Pain Res 2017;10:2183–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Benditz A, Drescher J, Greimel F, et al. Implementing a benchmarking and feedback concept decreases postoperative pain after total knee arthroplasty: a prospective study including 256 patients. Sci Rep 2016;6:38218doi:10.1038/srep38218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Lee KJ, Min BW, Bae KC, et al. Efficacy of multimodal pain control protocol in the setting of total hip arthroplasty. Clin Orthop Surg 2009;1:155–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Kethy JEM, Goon AK, Westrich GH, et al. Patient-controlled epidural analgesia or multimodal pain regimen with periarticular injection after total hip arthroplasty: a randomized, double-blind, placebo-controlled study. J Bone Joint Surg Am 2015;97:789–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Horlocker TT. Pain management in total joint arthroplasty: a historical review. Orthopedics 2010;33(suppl 9):14–9. [DOI] [PubMed] [Google Scholar]
- [9].Meissner W, Coluzzi F, Fletcher D, et al. Improving the management of post-operative acute pain: priorities for change. Curr Med Res Opin 2015;31:2131–43. [DOI] [PubMed] [Google Scholar]
- [10].Korean Knee Society. Guidelines for the management of postoperative pain after total knee arthroplasty. Knee Surg Relat Res 2012;24:201–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Cohen P, Raja SN. Prevention of chronic postsurgical pain. The ongoing search for the holy grail of anesthesiology. Anesthesiology 2013;118:241–3. [DOI] [PubMed] [Google Scholar]
- [12].Min BW, Kim Y, Cho HM, et al. Perioperative pain management in total hip arthroplasty: Korean hip society guidelines. Hip Pelvis 2016;28:15–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Clarke H, Poon M, Weinrib A, et al. Preventive analgesia and novel strategies for the prevention of chronic post-surgical pain. Drugs 2015;75:339–51. [DOI] [PubMed] [Google Scholar]
- [14].Kelley TC, Adams MJ, Mulliken BD, et al. Efficacy of multimodal perioperative analgesia protocol with periarticular medication injection in total knee arthroplasty: a randomized, double-blinded study. J Arthrop 2013;28:1274–7. [DOI] [PubMed] [Google Scholar]
- [15].Gaffney CJ, Pelt CE, Gililland JM, et al. Perioperative pain management in hip and knee arthroplasty. Orthop Clin North Am 2017;48:407–19. [DOI] [PubMed] [Google Scholar]
- [16].Russo MW, Parks NL, Hamilton WG. Perioperative pain management and anesthesia: a critical component to rapid recovery total joint arthroplasty. Orthop Clin North Am 2017;48:401–5. [DOI] [PubMed] [Google Scholar]
- [17].Stevenson KL, Neuwirth AL, Sheth N. Perioperative pain management following total joint arthroplasty: a review and update to an institutional pain protocol. J Clin Orthop Trauma 2018;9:40–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].McDonald LT, Corbiere NC, DeLisle JA, et al. Pain management after total joint arthroplasty. AORN J 2016;103:605–16. [DOI] [PubMed] [Google Scholar]
- [19].Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg 2017;152:691–7. [DOI] [PubMed] [Google Scholar]
- [20].Parvizi J, Miller AG, Gandhi K. Multimodal pain management after total joint arthroplasty. J Bone Joint Surg Am 2011;93:1075–84. [DOI] [PubMed] [Google Scholar]
- [21].Capdevila X, Barthejet Y, Biboulet P, et al. Effects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgery. Anesthesiology 1999;91:8–15. [DOI] [PubMed] [Google Scholar]
- [22].Soledad-Cepedaa M, Africanoa JM, Poloa R, et al. What decline in pain intensity is meaningful to patients with acute pain. Pain 2003;105:151–7. [DOI] [PubMed] [Google Scholar]
- [23].Collin C, Wade DT, Davies S, et al. The Barthel ADL Index: a reliability study. Int Disabil Stud 1988;10:61–3. [DOI] [PubMed] [Google Scholar]
- [24].World Health Organization. Cancer Pain Relief. Geneva, Switzeland: World Health Press; 1986. [Google Scholar]
- [25].Kehlet H, Aasvang EK. Regional or general anesthesia for fast-track hip and knee replacement - what is the evidence? F1000Research 2015;(F1000 Faculty Rev):1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Karlsen AP, Wetterslev M, Hansen SE4, et al. Postoperative pain treatment after total knee arthroplasty: a systematic review. PLoS One 2017;12:e0173107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Højer Karlsen AP, Geisler A, Petersen PL, et al. Postoperative pain treatment after total hip arthroplasty: a systematic review. Pain 2015;156:8–30. [DOI] [PubMed] [Google Scholar]
- [28].Gagliese L, Weizblit N, Ellis W, et al. The measurement of postoperative pain: a comparison of intensity scales in younger and older surgical patients. Pain 2005;117:412–20. [DOI] [PubMed] [Google Scholar]
- [29].Lisi C, Caspani P, Bruggi M, et al. Early rehabilitation after elective total knee arthroplasty. Acta Biomed 2017;88(suppl 4):56–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Snyder MA, Scheuerman CM, Gregg JL, et al. Improving total knee arthroplasty perioperative pain management using a periarticular injection with bupivacaine liposomal suspension. Arthroplast Today 2016;2:37–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Gerbershagen HJ, Pogatzki-Zahn E, Aduckathil S, et al. Procedure-specific risk factor analysis for the development of severe postoperative pain. Anesthesiology 2014;120:1237–45. [DOI] [PubMed] [Google Scholar]
- [32].Rakel BA, Blodgett NP, Bridget Zimmerman M, et al. Predictors of postoperative movement and resting pain following total knee replacement. Pain 2012;153:2192–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Choi S, O’Hare T, Gollish J, et al. Optimizing pain and rehabilitation after knee arthroplasty: a two-center, randomized trial. Anesth Analg 2016;123:1316–24. [DOI] [PubMed] [Google Scholar]
- [34].Castorina S, Guglielmino C, Castrogiovanni P, et al. Clinical evidence of traditional fast track recovery methodologies after total arthroplasty for osteoarthritic knee treatment. A retrospective observational study. MLTJ 2018;7:504–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Panella L, Caserta AV, Ballarati R, et al. Control of post-operative pain and rehabilitation compliance of patients undergoing knee replacement. Clin Pract 2016;132:39–45. [Google Scholar]
- [36].Johnson RL, Amundson AW, Abdel MP, et al. Continuous posterior lumbar plexus nerve block versus periarticular injection with ropivacaine or liposomal bupivacaine for total hip arthroplasty: a three-arm randomized clinical trial. J Bone Joint Surg Am 2017;99:1836–45. [DOI] [PubMed] [Google Scholar]
- [37].Xu J, Chen XM, Ma CK, et al. Peripheral nerve blocks for postoperative pain after major knee surgery. Cochrane Database Syst Rev 2014;12:CD010937. [DOI] [PubMed] [Google Scholar]
- [38].Guay J, Johnson RL, Kopp S. Nerve blocks or no nerve blocks for pain control after elective hip replacement (arthroplasty) surgery in adults. Cochrane Database Syst Rev 2017;31; 10:CD011608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Wiesmann T, Piechowiak K, Duderstadt S, et al. Continuous adductor canal block versus continuous femoral nerve block after total knee arthroplasty for mobilisation capability and pain treatment: a randomised and blinded clinical trial. Arch Orthop Trauma Surg 2016;136:397–406. [DOI] [PubMed] [Google Scholar]
- [40].Koh IJ, Choi YJ, Kim MS, et al. Femoral nerve block versus adductor canal block for analgesia after total knee arthroplasty. Knee Surg Relat Res 2017;29:87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Shah NA, Jain NP. Is continuous adductor canal block better than continuous femoral nerve block after total knee arthroplasty? Effect on ambulation ability, early functional recovery and pain control: a randomized controlled trial. J Arthrop 2014;29:2224–9. [DOI] [PubMed] [Google Scholar]
- [42].Zhao XQ, Jiang N, Yuan FF, et al. The comparison of adductor canal block with femoral nerve block following total knee arthroplasty: a systematic review with meta-analysis. J Anesth 2016;30:745–54. [DOI] [PubMed] [Google Scholar]


