Abstract
The Global Registry of Acute Coronary Events (GRACE) risk score independently predicts major adverse cardiac events (MACEs) in patients with acute coronary syndrome (ACS). This study aims to evaluate whether the level of plasma homocysteine in addition to the GRACE score enhances the predictive value for MACEs in patients with acute coronary syndrome.
A total of 361 patients with ACS evaluated at our hospital were included in the study and tested for blood homocysteine levels. We recorded 40 (11.1%) instances of MACE during a median follow-up of 43.3 months (quartile 40.6–44.4 months), including 29 cases (8.0%) of all-cause death and 11 cases (3.1%) of nonfatal myocardial infarction.
The GRACE score was significantly associated with homocysteine levels, and multivariate Cox regression analysis showed that both the GRACE risk score and homocysteine content were independent predictors of MACEs (HR 2.63; 95% confidence interval (CI) 1.54 to 4.49; P < .001 and 2.27; 1.06 to 4.86; P = .035, respectively). Moreover, meta-analysis showed that as the homocysteine level increased, the incidence of MACEs also increased (log-rank 8.41; P = .015). GRACE scores adjusted by homocysteine level increased the area under the curve (AUC) from 0.78 to 0.83 (P = 0.006).
Blood homocysteine levels are significantly associated with the GRACE risk score, and using both parameters can further improve risk stratification in patients with acute coronary syndrome.
Keywords: acute coronary syndrome, coronary artery disease, homocysteine
1. Introduction
Patients with acute coronary syndrome (ACS) have diverse clinical manifestations and a high risk of death. Outcomes in high-risk cases can be improved by accurate clinical decisions made following a thorough patient assessment. To identify high-risk patients with acute coronary syndrome, current guidelines recommend using a standardized and useful grading system such as the Global Registry of Acute Coronary Events (GRACE) score.[1] Although the GRACE score has been clinically adopted, it does not include some important biomarkers.[2] Therefore, whether GRACE scores combined with other biomarkers provide a more accurate risk score for people with acute coronary syndrome remains to be explored.
Homocysteine (Hcy) is a detrimental intermediate of cellular metabolism in the human body. An increased level of Hcy in the blood is an indicator of a high risk of stroke. Even more dangerous is the increased risk of stroke compared with the normal population when both blood pressure and Hcy increase.[3,4] Clinical scholars consider “hypertension with elevated homocysteine levels” as “H-type hypertension.”[5,6] Due to genetic background, the interaction of diet and other factors, the level of homocysteine in the Chinese population is elevated and the folic acid level is low, which in turn leads to a high incidence of stroke. A total of 300 million hypertensive patients have been identified in China, and roughly two-thirds have H-type hypertension.[7,8] It has been found that high levels of homocysteine increase the risk of cardiovascular events.[9–11] However, there are few reports in the literature detailing the relationship of homocysteine combined with GRACE scores in patients with ACS.
In the present study, we found that homocysteine levels and GRACE scores independently predicted MACE in patients with acute coronary syndrome, and considering homocysteine levels can potentially augment estimates based upon the GRACE score values alone. This relationship has rarely been reported in the literature.
2. Patients and methods
2.1. Patients
This was a single-center observational study that continuously collected data from patients diagnosed with acute coronary syndrome from January 2013 to August 2014 in our hospital. Those with unstable angina pectoris, non-ST-segment elevation myocardial infarction, and ST-segment elevated myocardial infarction were included. Exclusion criteria included advanced liver disease, kidney failure, cancer, valvular heart disease, stroke, idiopathic dilated cardiomyopathy or hypertrophic cardiomyopathy, peripheral arterial disease, pregnancy, anti-inflammatory drug treatment, acute or chronic infection, autoimmune disease, and hematological or thyroid disease.
Clinical data were collected and analyzed from the patients’ medical records, included demographic data, cardiovascular risk factors and cardiovascular-related medications used. Enrollment was conducted in accordance with the Declaration of Helsinki (2008) of the World Medical Association. This study was approved by the ethics committee and institutional review board of the First Hospital of Xi’an, Jiaotong University, and all patients provided written informed consent.
2.2. Blood tests
EDTA anticoagulated plasma samples were measured by ELISA. After patients had fasted for 12 hours, blood samples were drawn between 8:00 and 10:00 AM the next morning. Plasma and whole blood were immediately separated by centrifugation (1000×g/15 min, 4°C). Plasma aliquots were stored at −70°C and thawed before testing. Homocysteine concentration was measured with a commercially available ELISA kit (Ortho-Clinical Diagnostics, Inc., Rochester, New York) according to the manufacturer's instructions. Standard measurements of blood parameters and serum biochemistry were performed with a DIRUI CS 400 Analyzer (Dirui, Changchun, China). Venous plasma glucose, blood lipids, lipoproteins, serum creatinine, NT-proBNP, leukocytes, and platelet count were assessed.
2.3. GRACE score calculation
The GRACE score was derived from the values calculated for cardiovascular variables.[1,12] These variables included age, heart rate, systolic blood pressure, serum creatinine, congestive heart failure, PCI and coronary bypass surgery procedures, a history of myocardial infarction, the magnitude of ST-depression, and the elevation of myocardial enzymes. The GRACE risk score was originally used to predict lethality 6 months after discharge from the hospital and more than 4 years after myocardial ischemic events. According to ESC guidelines, patients can be divided into 3 categories based on GRACE scores: low risk (1–88), moderate risk (89–118), and high risk (>118).
2.4. Follow-up
MACEs were defined as all-cause death or nonfatal myocardial infarction. All patients were followed-up by telephone and at outpatient visits. The end event was defined as the first MACE occurrence.
2.5. Statistical analysis
All data were analyzed using SPSS version 11.0 (SPSS, 127 Chicago, IL). Continuity variables were expressed as the mean ± standard deviation, and categorical variables were expressed as frequency and percentage. The Kolmogorov–Smirnov test was used to describe the normal distribution of quantitative variables. An independent-samples t-test was used to compare the 2 groups and the Chi-square test was used to compare categorical variables. One-way ANOVA was used to compare the differences among multiple groups. Correlation analysis was performed using Spearman's correlation. Univariate and multivariate survival analysis included COX regression analysis. A Kaplan–Meier survival curve was used to assess the predictive value of homocysteine for risk of death in patients with acute coronary syndrome. The predictive value of homocysteine alone and the value combined with the GRACE score were expressed as the area under the ROC curve. P < .05 was defined as statistically significant.
3. Results
3.1. Baseline data
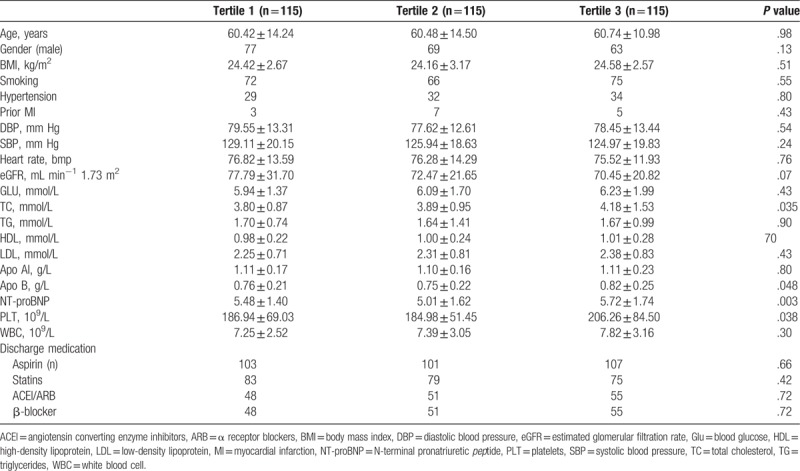
As shown in Table 1, of the 361 eligible patients enrolled in this study, 12 were lost to follow-up (3.4%) by study end at approximately 43.3 months. The remaining 347 patients were divided into 3 groups based on homocysteine values as follows: Group 1 <16 μmol / L, Group 2 = 16 to 30 μmol/L, and Group 3 > 30 μmol/L (Table 1). As the homocysteine value increased, the total cholesterol value also increased (P < .05). Platelet count, NT-proBNP level and ApoB in Group 3 were higher than in Groups 1 and 2 (P < .05, P = 0.003 and P = 0.048).
Table 1.
The demographic characteristics data in the study.
3.2. Clinical characteristics of patients with and without MACEs
Of all 347 patients enrolled, 40 (11.5%) suffered MACEs, including 29 all-cause deaths and 11 nonfatal MI. According to the GRACE score, the incidence of MACEs was greater in the high-risk group than in the low-risk and intermediate-risk groups. We performed a correlation analysis between GRACE score and Hcy level as a continuous variable which revealed a significant correlation between the 2 (R = 0.172, P = .001).
3.3. Hcy level was an independent predictor of MACE rates
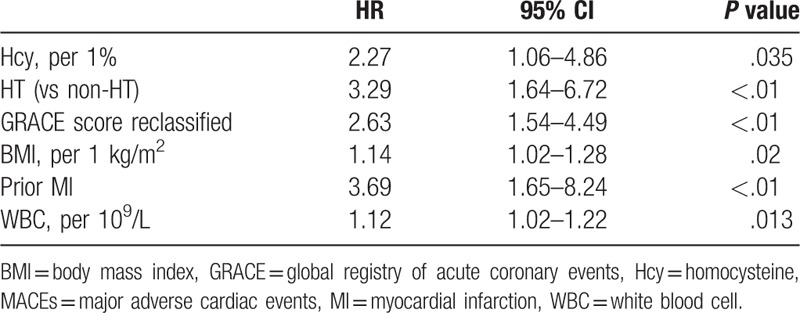
As determined by univariate Cox regression analysis, the most significant predictors of MACE were age, body mass index (BMI), history of hypertension, history of myocardial infarction, leukocyte and platelet count, homocysteine levels, and GRACE scores (Table 2). In multivariate COX regression analysis, Hcy levels were an independent factor shown to be significantly predictive of MACEs (HR 2.270; 95% CI 1.061 to 4.856; P < .05), as well as GRACE scores (HR 2.634; 95% CI 1.544 to 4.493; P < .001) (Table 3).
Table 2.
Univariate COX regression analysis of MACEs events.
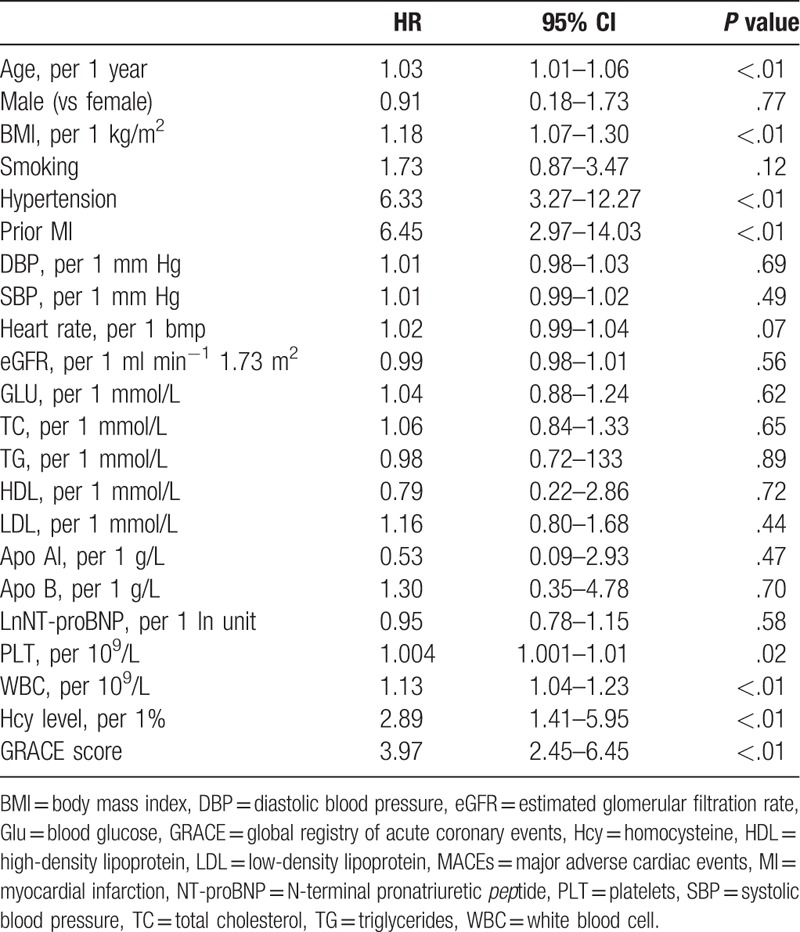
Table 3.
Multivariate cox regression analysis of MACEs events.
3.4. The combination effect of Hcy and GRACE on the incidence of MACE
Since Hcy levels and GRACE scores are both independent risk factors for MACE, we evaluated the combination effect on the prediction of long-term MACE. The AUC for the GRACE score alone was 0.78 (95% CI 0.73–0.83), which increased to 0.83 (95% CI 0.80–0.88) with the addition of Hcy. The change in AUC was statistically significant (P = 0.006) when both measures were combined, suggesting that the combination of Hcy level with the GRACE score contributes to the estimation of MACE.
4. Discussion
Homocysteine is a sulfur-containing amino acid formed after methionine demethylation, belonging to the intermediate product of the methionine cycle. The earliest reports of metabolic disorders originated from observations of homocystinuria in patients with congenital cystathionine synthase deficiency.[13] Since then, scientists have also found several other metabolic changes in HCY metabolism of enzymes or coenzymes caused by metabolic disorders. In recent years, with improvements in measurement techniques, HCY in various forms has been measured in normal human plasma and found to be a potential effective factor in the treatment of several ailments including cardiovascular, cerebrovascular and peripheral vascular diseases. HCY metabolic disorders have been found in patients suffering from chronic renal insufficiency, psoriasis and vitamin B12 deficiency as well.[12,14–18]
Subsequent clinical and experimental studies have shown that high levels of HCY can cause vascular damage, and lead to lesions in the coronary arteries, peripheral vasculature, and cerebrovasculature.[19] Plasma HCY levels in patients with peripheral vascular disease and those with intermittent claudication confirmed by angiography were higher than those in normal subjects. Plasma homocysteine levels in patients with thickened carotid intima and myometrium confirmed by B ultrasound were also higher than those in normal subjects.[20] These clinical studies of plasma HCY in relation to various vascular diseases indicate that HCY may be an independent risk factor for the development of such lesions.
The clinical management of patients with acute coronary syndrome should be based on risk stratification. In this study, the GRACE score provided a valid independent predictor of MACE in ACS patients, consistent with previous findings. However, the AUC for the GRACE score alone was only 0.78, possibly because underlying risk factors were not included in the scoring system. Furthermore, different scoring systems combine other clinical parameters indicating different clinical predictive values for patients with ACS or myocardial infarction. A previous study revealed that 3-dimensional global peak longitudinal strain (GPLS) could be a reproducible and efficient method to evaluate complex coronary artery disease in patients with non-ST-segment elevation acute coronary syndrome, and the value of GPLS was significantly associated with the complexity of coronary artery lesions.[21] Other authors described 3-dimensional global longitudinal strain as an excellent predictor with the highest predictive value for future left ventricular remodeling after acute myocardial infarction,[22] and the waist circumference could be more accurate to assess the cardiac function through the changes of let ventricular structure on the cardiac rehabilitation program ater ACS patients.[23] Moreover, other authors considered that the combination of computer-tomography-based fractional flow reserve pullback curve and wall shear stress distributions can provide more accurate evaluation the clinical outcome of the patients suffer from coronary stenoses,[24] and the non-invasive fractional low reserve derived from coronary computed tomographic angiography may be an simplified method to assess the hemodynamic characteristics for coronary stenosis.[25] These reports demonstrate that many potential questions remain in relation to the selection of optimal prognostic predictive factors for ACS.
Epidemiological data demonstrate that Hcy level is a risk factors for independent cardiovascular events (including myocardial infarction) in both general and hypertensive populations.[2,9–11] However, previous studies did not include Hcy in the GRACE scoring system. In the present study, the value of the GRACE score increased with increasing Hcy levels, and both correlated with MACE. Furthermore, the combination of Hcy and GRACE enhanced the predictive value for MACE in patients with ACS and no DM comorbidity (AUC 0.78 for the GRACE score alone and 0.83 for Hcy and GRACE). In patients with ACS, whether or not Hcy levels are independent predictors of cardiovascular events is uncertain. In this study, Hcy levels were independently predictive of long-term MACE in patients with ACS and those with comorbidities.
A previous study found that the addition of C-reactive protein (CRP), NT-proBNP, fatty acids, growth-differentiation factor-15, cystatin C, Dickkopf protein, RDW/PDW, troponin, mean platelet volume (MPV), and other factors to the scoring system can increase the predictive value of major cardiac adverse events in patients with ACS.[26–33] Even the functional assessment and computational fluid dynamics of a hemodynamic significant stenosis base on blood pressure variation has been applied for the evaluation of the myocardial ischemic event,[34–36] and the alterations of these parameters under pathological conditions are important indicators for diagnosis of cardiovascular disease. However, the effect of Hcy combined with GRACE scores was unclear. Our results demonstrate that the GRACE score was significantly associated with baseline Hcy levels, and the combination effect between Hcy and GRACE scores could improve the predictive value. However, whether or not the combination effect could further improve the clinical prognosis of patients with ACS still needs further investigation in clinical practice.
In conclusion, Hcy levels predict the occurrence of MACE in patients with ACS, and Hcy levels correlate significantly with GRACE scores. Combining the predictive effect of the 2 could improve risk stratification of the ACS population. However, this study was a retrospective study at a single center conducted in a select patient population and thus may be subject to some bias, and the pathophysiological mechanism of this effect remains known. The results of the study therefore, should be confirmed via RCTs study in the future.
Acknowledgments
The language of this article was edited by the American Journal Experts (AJE) group.
Author contributions
Conceptualization: Jianlin Liu, Jianjun Quan, Yanzi Li, Yue Wu, Lin Yang.
Data curation: Jianlin Liu, Jianjun Quan, Yanzi Li, Yue Wu, Lin Yang.
Formal analysis: Jianlin Liu, Jianjun Quan, Yanzi Li, Yue Wu, Lin Yang.
Investigation: Jianlin Liu, Jianjun Quan, Yanzi Li, Yue Wu, Lin Yang.
Methodology: Jianlin Liu, Jianjun Quan, Yanzi Li, Yue Wu, Lin Yang.
Project administration: Jianlin Liu, Yanzi Li, Yue Wu, Lin Yang.
Resources: Jianlin Liu, Yue Wu, Lin Yang.
Software: Yanzi Li, Yue Wu, Lin Yang.
Supervision: Jianlin Liu, Yue Wu, Lin Yang.
Validation: Yue Wu, Lin Yang.
Visualization: Lin Yang.
Writing – original draft: Lin Yang.
Writing – review & editing: Jianlin Liu, Yue Wu, Lin Yang.
Footnotes
Abbreviations: ACS = acute coronary syndrome, BMI = body mass index, DBP = diastolic blood pressure, eGFR = estimated glomerular filtration rate, Glu = blood glucose, GRACE = global registry of acute coronary events, HCY = homocysteine, HDL = high-density lipoprotein, LDL = low-density lipoprotein, MACEs = major adverse cardiac events, MI = myocardial infarction, NT-proBNP = N-terminal pronatriuretic peptide, SBP = systolic blood pressure, TC = total cholesterol, TG = triglycerides.
The authors have no conflicts of interest to disclose.
References
- [1].Aragam KG, Tamhane UU, Kline-Rogers E, et al. Does simplicity compromise accuracy in ACS risk prediction? A retrospective analysis of the TIMI and GRACE risk scores. PLoS One 2009;4:e7947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Wan ZF, Zhou D, Xue JH, et al. Combination of mean platelet volume and the GRACE risk score better predicts future cardiovascular events in patients with acute coronary syndrome. Platelets 2014;25:447–51. [DOI] [PubMed] [Google Scholar]
- [3].Eagle H, Washington C, Friedman SM. The synthesis of homocystine, cystathionine, and cystine by cultured diploid and heteroploid human cells. Proc Natl Acad Sci USA 1966;56:156–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Biswas A, Ranjan R, Meena A, et al. Homocystine levels, polymorphisms and the risk of ischemic stroke in young Asian Indians. J Stroke Cerebrovasc Dis 2009;18:103–10. [DOI] [PubMed] [Google Scholar]
- [5].Li J, Jiang S, Zhang Y, et al. H-type hypertension and risk of stroke in Chinese adults: a prospective, nested case-control study. J Transl Int Med 2015;3:171–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Zhang Q, Qiu DX, Fu RL, et al. H-type hypertension and c reactive protein in recurrence of ischemic stroke. Int J Environ Res Public Health 2016;13:E477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Ma L, Li L, Tang Z. Epidemiological characteristics of hyperhomocysteinemia and H-type hypertension in the elderly in Beijing, China. Clin Exp Hypertens 2017;39:640–4. [DOI] [PubMed] [Google Scholar]
- [8].Qin X, Huo Y. H-Type hypertension, stroke and diabetes in China: opportunities for primary prevention. J Diabetes 2016;8:38–40. [DOI] [PubMed] [Google Scholar]
- [9].Ganguly P, Alam SF. Role of homocysteine in the development of cardiovascular disease. Nutr J 2015;14:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Leal AA, Palmeira AC, Castro GM, et al. Homocysteine: cardiovascular risk factor in children and adolescents? Rev Assoc Med Bras (1992) 2013;59:622–8. [DOI] [PubMed] [Google Scholar]
- [11].Cianciolo G, De Pascalis A, Di Lullo L, et al. Folic acid and homocysteine in chronic kidney disease and cardiovascular disease progression: which comes first? Cardiorenal Med 2017;7:255–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Anderson JL, Adams CD, Antman EM, et al. 2012 ACCF/AHA focused update incorporated into the ACCF/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2013;127:e663–828. [DOI] [PubMed] [Google Scholar]
- [13].Sakamoto A, Sakura N. Limited effectiveness of betaine therapy for cystathionine beta synthase deficiency. Pediatr Int 2003;45:333–8. [DOI] [PubMed] [Google Scholar]
- [14].Fava M, Borus JS, Alpert JE, et al. Folate, vitamin B12, and homocysteine in major depressive disorder. Am J Psychiatry 1997;154:426–8. [DOI] [PubMed] [Google Scholar]
- [15].Ogawa M, Abe S, Saigo M, et al. Homocysteine and hemostatic disorder as a risk factor for myocardial infarction at a young age. Thromb Res 2003;109:253–8. [DOI] [PubMed] [Google Scholar]
- [16].Awara MA, Zahid S, Elnenaei MO. Rapid cycling bipolar affective disorder and recurrent strokes secondary to high blood homocysteine. J Ment Health 2014;23:276–9. [DOI] [PubMed] [Google Scholar]
- [17].Chen J, Li G, Xu Z, et al. Elevated plasma homocysteine level increased the risk of early renal impairment in acute ischemic stroke patients. Cell Mol Neurobiol 2017;37:1399–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Giannoni M, Consales V, Campanati A, et al. Homocysteine plasma levels in psoriasis patients: our experience and review of the literature. J Eur Acad Dermatol Venereol 2015;29:1781–5. [DOI] [PubMed] [Google Scholar]
- [19].Li T, Yu B, Liu Z, et al. Homocysteine directly interacts and activates the angiotensin II type I receptor to aggravate vascular injury. Nat Commun 2018;9:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Potter K, Hankey GJ, Green DJ, et al. The effect of long-term homocysteine-lowering on carotid intima-media thickness and flow-mediated vasodilation in stroke patients: a randomized controlled trial and meta-analysis. BMC Cardiovasc Disord 2008;8:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Cai Z, Dai J, Wu D, et al. The value of 3-dimensional longitudinal strain in the evaluation of complex coronary lesions in non-ST-segment elevation acute coronary syndrome patient. Medicine 2016;95:e4667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Xu L, Huang X, Ma J, et al. Value of three-dimensional strain parameters for predicting left ventricular remodeling after ST-elevation myocardial infarction. Int J Cardiovasc Imaging 2017;33:663–73. [DOI] [PubMed] [Google Scholar]
- [23].Xu L, Zhao H, Qiu J, et al. The different effects of BMI and WC on organ damage in patients from a cardiac rehabilitation program after acute coronary syndrome. Biomed Res Int 2015;2015:942695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Liu X, Peng C, Xia Y, et al. Hemodynamics analysis of the serial stenotic coronary arteries. Biomed Eng Online 2017;16:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Shi C, Zhang D, Cao K, et al. A study of noninvasive fractional flow reserve derived from a simplified method based on coronary computed tomography angiography in suspected coronary artery. Biomed Eng Online 2017;16:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Schiele F, Meneveau N, Seronde MF, et al. C-reactive protein improves risk prediction in patients with acute coronary syndromes. Eur Heart J 2010;31:290–7. [DOI] [PubMed] [Google Scholar]
- [27].Ang DS, Wei L, Kao MP, et al. A comparison between B-type natriuretic peptide, global registry of acute coronary events (GRACE) score and their combination in ACS risk stratification. Heart 2009;95:1836–42. [DOI] [PubMed] [Google Scholar]
- [28].Harris WS, Kennedy KF, O’Keefe JH, Jr, et al. Red blood cell fatty acid levels improve GRACE score prediction of 2-yr mortality in patients with myocardial infarction. Int J Cardiol 2013;168:53–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Widera C, Pencina MJ, Meisner A, et al. Adjustment of the GRACE score by growth differentiation factor 15 enables a more accurate appreciation of risk in non-ST-elevation acute coronary syndrome. Eur Heart J 2012;33:1095–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Eggers KM, Kempf T, Venge P, et al. Improving long-term risk prediction in patients with acute chest pain: the Global Registry of Acute Coronary Events (GRACE) risk score is enhanced by selected nonnecrosis biomarkers. Am Heart J 2010;160:88–94. [DOI] [PubMed] [Google Scholar]
- [31].Wang L, Hu XB, Zhang W, et al. Dickkopf-1 as a novel predictor is associated with risk stratification by GRACE risk scores for predictive value in patients with acute coronary syndrome: a retrospective research. PLoS One 2013;8:e54731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Timoteo AT, Papoila AL, Lousinha A, et al. Predictive impact on mediumterm mortality of hematological parameters in acute coronary syndromes: added value on top of GRACE risk score. Eur Heart J Acute Cardiovasc Care 2015;4:172–9. [DOI] [PubMed] [Google Scholar]
- [33].Stahli BE, Yonekawa K, Altwegg LA, et al. Clinical criteria replenish high-sensitive troponin and inflammatory markers in the stratification of patients with suspected acute coronary syndrome. PLoS One 2014;9:e98626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Liu X, Zhang H, Ren L, et al. Functional assessment of the stenotic carotid artery by CFD-based pressure gradient evaluation. Am J Physiol Heart Circ Physiol 2016;311:H645–53. [DOI] [PubMed] [Google Scholar]
- [35].Liu X, Gao Z, Xiong H, et al. Three-dimensional hemodynamics analysis of the circle of Willis in the patient-specific nonintegral arterial structures. Biomech Model Mechanobiol 2016;15:1439–56. [DOI] [PubMed] [Google Scholar]
- [36].Xu P, Liu X, Zhang H, et al. Assessment of boundary conditions for CFD simulation in human carotid artery. Biomech Model Mechanobiol 2018;7: doi: 10.1007/s10237-018-1045-4. [DOI] [PubMed] [Google Scholar]


