Abstract
Background:
Securing the airway and enabling adequate oxygenation and ventilation is essential during cardiopulmonary resuscitation (CPR). The aim of the study was to evaluate the success rate of blind intubation via the I-Gel and the Air-Q compared with direct laryngoscopy guided endotracheal intubation by inexperienced physician and to measure time to successful intubation.
Methods:
The study was designed as a randomized, cross-over simulation study. A total of 134 physicians, from specialties other than Anesthesia or Emergency Medicine, who considered themselves skilled in endotracheal intubation but who have never used any kind of supraglottic airway device performed blind intubation via the I-Gel and Air-Q and direct laryngoscopy guided endotracheal intubation in 3 randomized scenarios: normal airway without chest compression during intubation attempt; normal airway with continuous chest compression during intubation attempt; difficult airway with continuous chest compression.
Results:
Scenario A: Success rate with initial intubation attempt was 72% for endotracheal intubation, 75% in Air-Q, and 81% in I-Gel. Time to endotracheal intubation and ease of intubation was comparable with all 3 airway devices used. Scenario B: Success rate with the initial intubation attempt was 42% for endotracheal intubation, compared with 75% in Air-Q and 80% in I-Gel. Time for endotracheal intubation was significantly prolonged in endotracheal intubation (42 seconds, 35–49), compared with Air-Q (21 seconds, 18–32) and I-Gel (19 seconds, 17–27). Scenario C: The success rate with the initial intubation attempt was 23% in endotracheal intubation, compared with 65% in Air-Q and 74% in I-Gel. Time to intubation was comparable with both supraglottic airway devices (20 vs 22 seconds) but was significantly shorter compared with endotracheal intubation (50 seconds, P < .001).
Conclusions:
Less to moderately experienced providers are able to perform endotracheal intubation in easy airways but fail during ongoing chest compressions and simulated difficult airway. Consequently, less to moderately experienced providers should refrain from endotracheal intubation during ongoing chest compressions during CPR and in expected difficult airways. Supraglottic airway devices are reliable alternatives and blind intubation through these devices is a valuable airway management strategy.
Keywords: blind intubation, cardiopulmonary resuscitation, endotracheal intubation, medical simulation, physician
1. Introduction
More than 350,000 people suffer an out-of-hospital cardiac arrest in the united states annually and early initiation of advanced cardio-pulmonary resuscitation (CPR) is the key to favorable outcomes.[1–4] High-quality chest compressions are the most single important component of CPR. Even minor interruptions of chest compressions during CPR, represented by the so-called hands-off time, reduces systemic blood flow and increases morbidity and mortality.[5] Consequently, international CPR guidelines advocate to keep the hands-off time as short as possible.[2,6]
Securing the airway and enabling adequate oxygenation and ventilation is essential during CPR, and although controversially discussed, endotracheal intubation is considered the airway of choice, at least by experienced providers.[7,8] Endotracheal intubation requires regular training and high level of individual skills and experience.[9–11] Supraglottic airway devices are less invasive, are easier to place, and have previously been reported to decrease the time needed to intubate, even by unexperienced providers and during ongoing chest compression during CPR.[12–14] Supraglottic airway devices do not prevent pulmonary aspiration of gastric content, a common and serious clinical concern.[15] However, once the airway is secured by a supraglottic airway and ventilation is restored, the trachea can be intubated through some types of supraglottic airway devices. Intubation through these devices can be performed using a fiberoptic bronchoscope or blindly, meaning that the tube is inserted through the supraglottic airway device without direct visualization of the airway.[16,17] Success rate of blind intubation ranges between 15% and 97%, mostly depending on the type of the supraglottic airway device used, patient characteristics and operator skills.[18,19]
The I-Gel and the Air-Q are recently introduced supraglottic airway devices designed to permit fiberoptic-guided and blind endotracheal intubation.[19,20] Whether these airway devices can be used successfully by non-experienced providers like physicians within acceptable time frame remains currently unclear. We, therefore, performed this manikin study to evaluate the success rate of blind intubation via the I-Gel and the Air-Q compared with direct laryngoscopy guided endotracheal intubation by unexperienced physician. Additionally, we investigated the number of intubation attempts and the time to successful intubation. In particular, we tested the hypothesis, that success rates of blind-intubation via I-Gel and Air-Q are non-inferior to direct laryngoscopy guided endotracheal intubation.
2. Material and methods
The study was designed as a randomized, cross-over simulation study. The study protocol was approved by the Institutional Review Board of the Polish Society of Disaster Medicine (Approval no. 43.12.2017.IRB) and was performed at the International Institute of Rescue Research and Education (Warsaw, Poland) between December 2017 and April 2018.
2.1. Participants
After informed written consent was obtained, 134 physicians voluntarily participated in the study (Table 1). All participating physicians considered themselves as skilled in endotracheal intubation, but never used any kind of supraglottic airway device. Physicians were excluded in case of pregnancy or any physical injury, affecting probability to perform endotracheal intubation. Anesthesiologists or emergency physicians were excluded from the study.
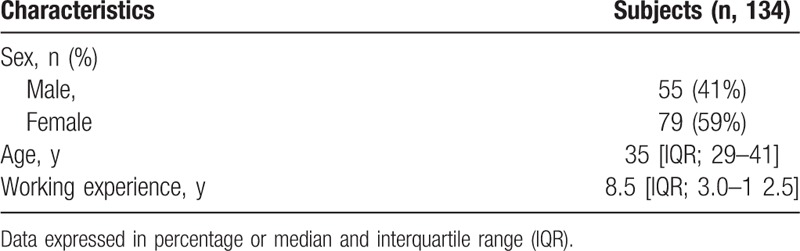
Table 1.
Baseline characteristics.
2.2. Protocol
Prior to the study, participating physicians received a standardized audio-visual lecture lasting 30 minutes covering fundamental airway anatomy, physiology, and pathophysiology, and common methods of airway management including several supraglottic airway devices used for blind intubation. This lecture was followed by a 30 minutes lasting hands-on training. Blind intubation via the I-Gel and Air-Q and direct laryngoscopy guided endotracheal intubation were demonstrated and physicians were able to practice the devices on an airway manikin. Endotracheal intubation was performed by using a laryngoscope with a Macintosh's blade size 3 (HEINE Optotechnik GmbH & Co. KG, Herrsching, Germany). Blind intubation was performed using an I-Gel supraglottic airway size 4 (Intersurgical Ltd., Wokingham, UK), and Air-Q supraglottic airway device size 4.5 (Mercury Medical, Florida) (Fig. 1). A standard single lumen endotracheal tube with 7.0 mm internal diameter (ID) was used for all intubation attempts. Both, the endotracheal tube and respective supraglottic airway devices were thoroughly lubricated with a lubricant recommended by the producer of the manikin.
Figure 1.
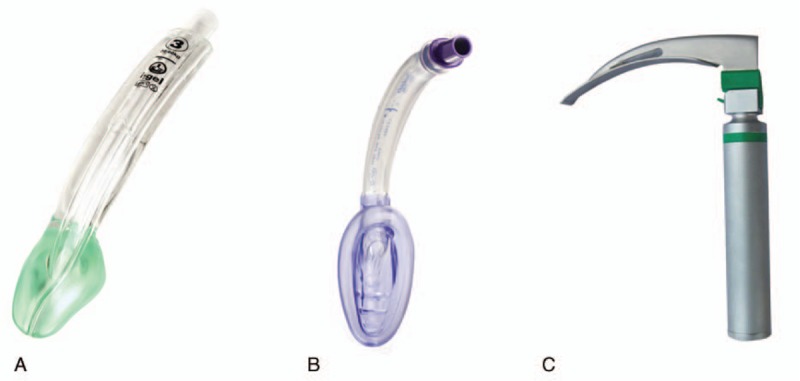
Devices used in the study: (A) iGEL mas; (B) Air-Q maks; (C) Macintosh laryngoscope.
A Resusci Anne QCPR (Laerdal, Stavanger, Norway) simulator was placed on the floor in a well-lit room. Subjects were asked to perform airway management with all 3 airway devices in 3 separate scenarios:
-
(1)
Scenario A: normal airway without chest compression during intubation attempt.
-
(2)
Scenario B: normal airway with continuous chest compression during intubation attempt.
-
(3)
Scenario C: difficult airway with continuous chest compression. The simulator control software generated a Mallampati grade 3 through tongue edema.
The physicians were asked to perform airway management as fast as possible. Chest compressions were performed at a rate of 100 compressions per minute, and compression depth of 5 cm by using the CORPULS CPR (GS Elektromedizinische Geräte G. Stemple GmbH, Kaufering, Germany) chest compression system.
Both, the intubation methods and scenarios sequence were randomized by using a Research Randomizer program (randomizer.org) (Fig. 2). Physicians performed airway management with all 3 devices in each scenario. Afterwards, physicians rested for about 10 minutes, before they were asked to handle the second, respectively the third airway scenario.
Figure 2.
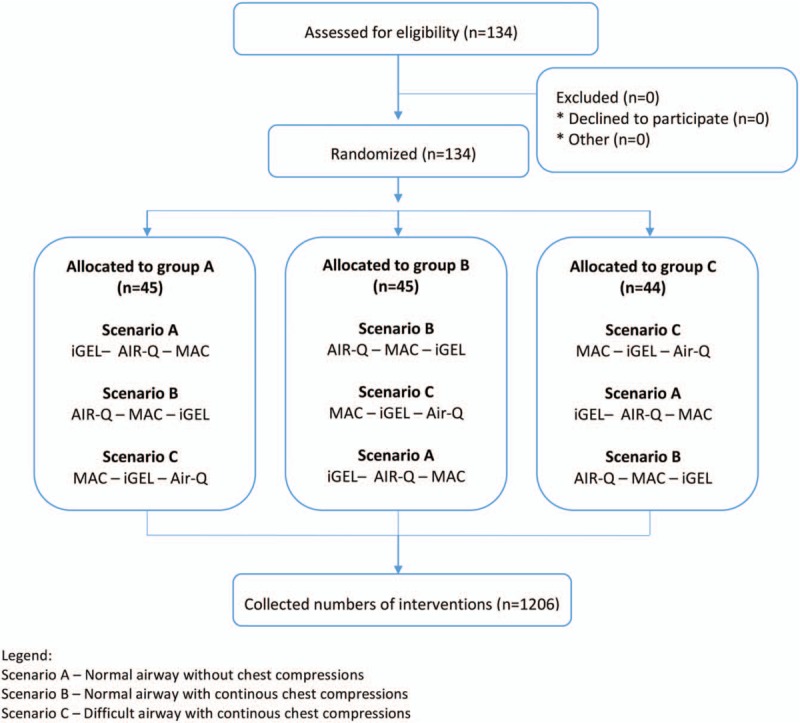
Randomization flow chart.
2.3. Data collection
Primary endpoint was overall rate of successful intubation, defined as successful placement of an endotracheal tube in the simulators trachea. Correct placement was confirmed by successful ventilation of the manikin's lungs with an anesthesia bag. Intubation attempts lasting longer than 120 seconds, or unrecognized esophageal intubation were defined as failure.
Secondary endpoints included: rate of successful intubation with 1 single intubation attempt. Time to successful supraglottic airway device (SAD) placement, defined as the time from the initial insertion of the SADs in the manikin's mouth until stabilization of the supraglottic airway device. Time to successful endotracheal intubation was defined as time from the initial insertion of the laryngoscope or SAD in the manikin's mouth to confirmation of lung inflation with positive pressure breaths through the endotracheal tube. Time to successful blind intubation was defines as time from the initial insertion of the Supraglottic airways (SGAs) in the manikin's mouth to confirmation of lung inflation with positive pressure breaths through the tracheal tube.
Once physicians performed all 3 intubations during a scenario, physicians were asked to rate difficulty of intubation of each device using a visual analog scale (VAS) ranging from 1 (extremely easy) to 100 (extremely difficult).
2.4. Statistical analysis
The statistical package Statistica 13.0 EN (Tibico, Tulusa, OK) was used for all statistical analysis. The type I error was set to a = 0.05. To account for multiple testing, critical was adjusted using the Bonferroni method (a = 0.0125). To detect possible differences in procedure time and success rate of endotracheal intubation, the analysis of variance (ANOVA) Kruskal Wallis was used. The participants’ subjective opinions were compared with the use of the Stuart–Maxwell test. Data were presented as medians and interquartile range (IQR), or percentages (%). The α-error level for all analyses was set at P < .05.
3. Results
One hundred and thirty-four physicians (79 women) with a median age 35 [IQR; 29–41] years and work experience of 8.5 [3.0–12.5] years participated in this study. All physicians declared the ability to perform endotracheal intubation using direct laryngoscopy but had not used any form of any supraglottic airway device beforehand.
3.1. Scenario A: normal airway without chest compression
Success rate with initial intubation attempt was 72% for endotracheal intubation, 75% in Air-Q, and 81% in I-Gel (Table 2). The final success rate within 3 intubation attempts was 95% in endotracheal intubation, 99% in Air-Q, and 100% in I-Gel (Table 2). Time to endotracheal intubation and ease of intubation was comparable with all 3 airway devices used (Figs. 3A and 4A, respectively).
Table 2.
Study outcomes by supraglottic airway devices with unexperienced physician (N = 134).
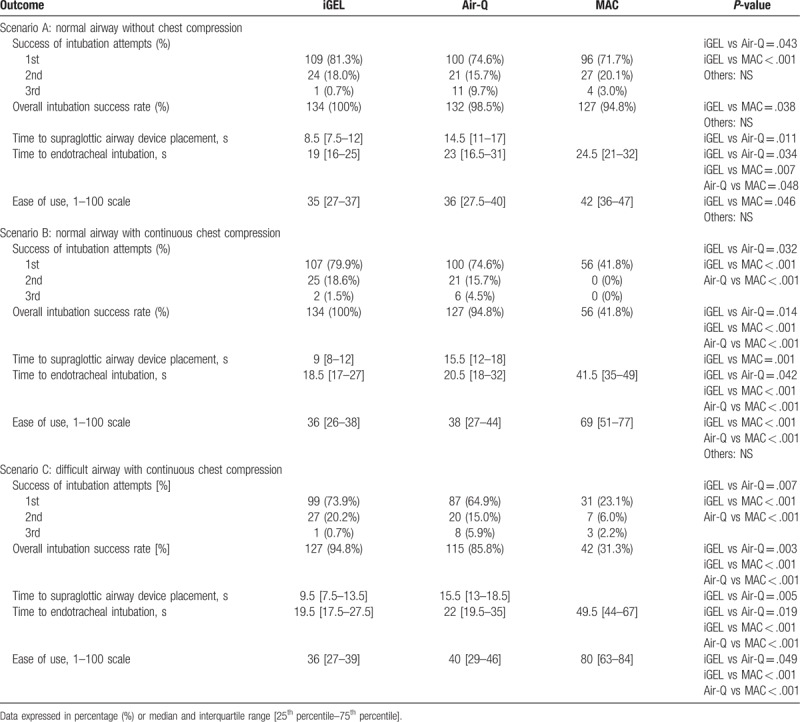
Figure 3.
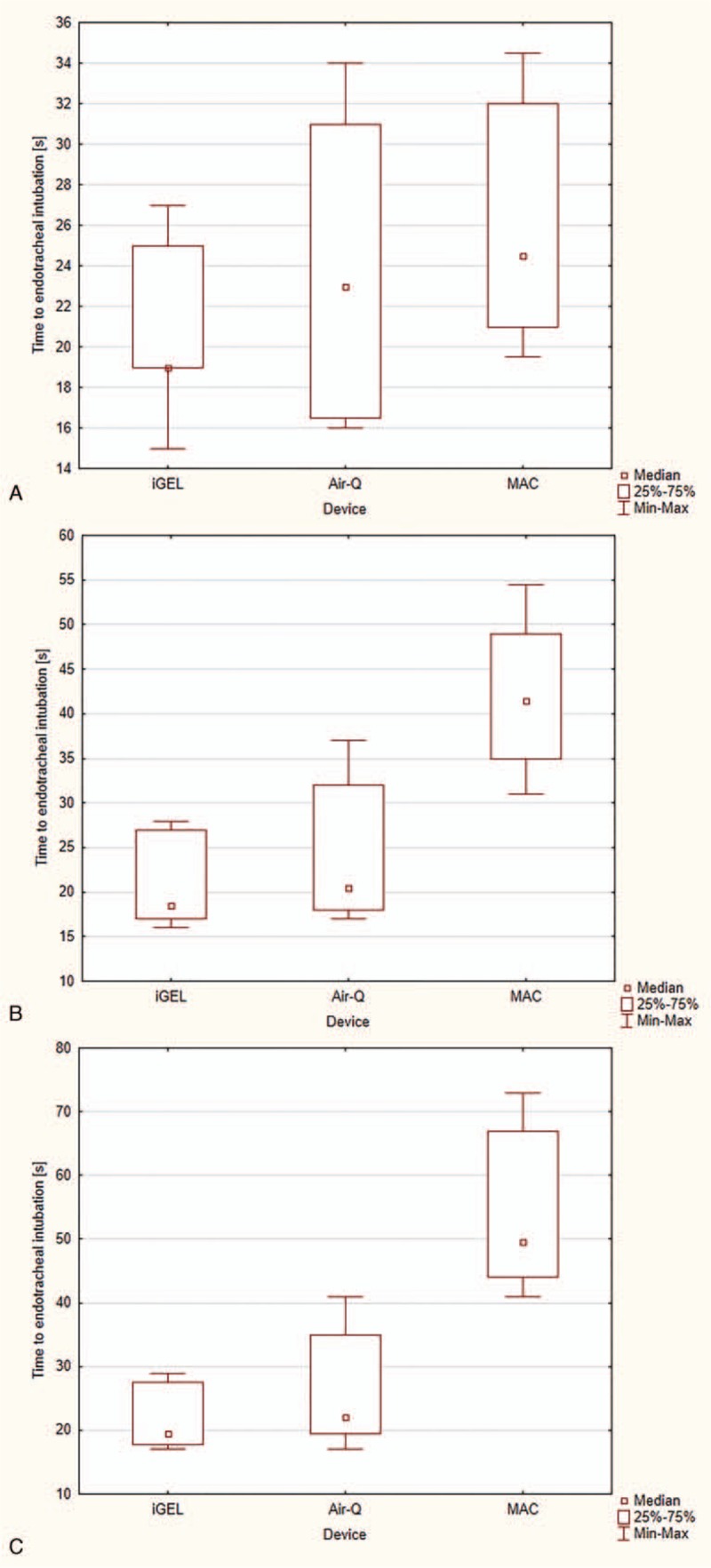
Time to endotracheal intubation during: (A) Scenario A; (B) Scenario B; (C) Scenario C).
Figure 4.
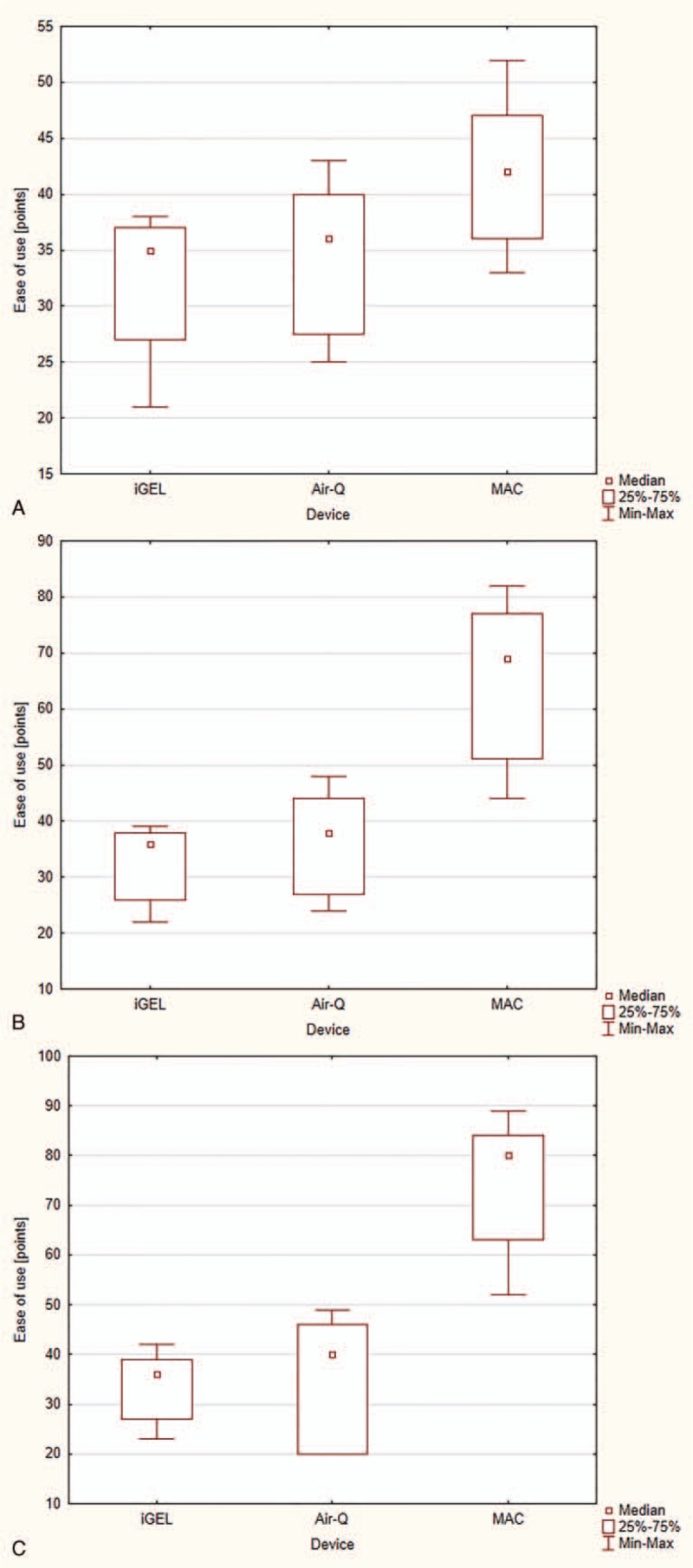
Ease of use during: (A) Scenario A; (B) Scenario B; (C) Scenario C).
3.2. Scenario B: normal airway with continuous chest compression
Success rate with the initial intubation attempt was 42% for endotracheal intubation, compared with 75% in Air-Q and 80% in I-Gel (Table 2). Overall success rate was 42% for endotracheal intubation, 95% in Air-Q, and 100% in I-Gel (Table 2). Time for endotracheal intubation was significantly prolonged in endotracheal intubation (42 seconds, 35–49), compared with Air-Q (21 seconds, 18–32) and I-Gel (19 seconds, 17–27) (Fig. 3B). Endotracheal intubation was also rated to be significantly more difficult compared with both supraglottic airway devices (69 vs 38 for Air-Q and 36 for I-Gel; Fig. 4B).
3.3. Scenario C: difficult airway with continuous chest compression
During this scenario, the success rate with the initial intubation attempt was 23% in endotracheal intubation, compared with 65% in Air-Q and 74% in I-Gel (Table 2). Overall success rate was significantly higher in I-Gel compared with Air-Q (95% vs 86%, P = .003). Both supraglottic airway devices offered significant better overall success rate, compared with endotracheal intubation (95% vs 86% vs 31%, P < .001). Time to intubation was comparable with both supraglottic airway devices (20 vs 22 seconds) but was significantly shorter compared with endotracheal intubation (50 seconds, P < .001; Fig. 3C). Again, both supraglottic airway devices were rated comparable (36 vs 40), but significantly easier compared with endotracheal intubation (80, P < .001; Fig. 4C)
4. Discussion
Results of this manikin study indicate, that relatively skilled and experienced providers were able to intubate a manikin with an easy regular airway. However, these providers failed during ongoing chest compressions or with a simulated difficult airway (success rate of 42% and 31%, respectively). Contrary, placement of supraglottic airway devices was easy, and success rate of blind intubation via these supraglottic airway devices were between 86% and 100% in all intubation attempts and all 3 airway scenarios.
The I-Gel as well as the Air-Q devices have been previously reported to be easy to insert and providing adequate ventilation in several clinical scenarios.[20–23] Placement of both supraglottic airway devices were possible in all intubation attempts in all 3 intubation scenarios. The corresponding success rate of 100% is in line with several previous reports.[19,20,24] Placement of supraglottic airway devices are easy to place, quickly inserted, and nearly always provide adequate ventilation.[14,20,25,26] However, supraglottic airway devices are generally limited due their ability to prevent pulmonary aspiration of gastric content, a significant clinical concern in patients undergoing both, regular anesthesia for a surgical procedure or CPR.[8,27,28]
Once the airway is secured with a supraglottic airway device, several devices including the I-Gel and the Air-Q offer the possibility to intubate the trachea through the supraglottic airway device. This can be done without direct visualization of the airway, the so called blind intubation, or guided by using a fiberoptic bronchoscope. Especially in the emergency setting, blind intubation might be more reasonable, as it is much less time consuming and a fiberoptic might not be regularly available.
Success rate of blind intubation via the supraglottic airway devices with the initial intubation attempt differed between the 2 different devices used in this study and within the 3 airway scenarios. As expected, success rate was highest in scenario 1 with an easy airway anatomy (81% in I-Gel and 75% in Air-Q), and somewhat decreased during ongoing chest compression (scenario 2, 80% in I-Gel and 75% in Air-Q) and difficult airway (scenario 3, 74% in I-Gel and 64% in Air-Q). Overall, the success rate with initial intubation attempt is well within the previously reported range of success rates ranging between 57% and 70%.[18,20,29] The obvious reason is the use of airway manikins in this study instead of patients undergoing real-world intubations.
Previous studies reported an overall success rate of blind-intubation via a supraglottic airway devices, ranging from 24% to 97%.[19,20] Results of our study indicate, that blind intubation via a supraglottic airway devices with a maximum of 3 intubation attempt is highly success full in easy airways (scenario 1, 100% in I-Gel and 99% in Air-Q) and is relatively not altered by ongoing chest compression (scenario 2, 100% in I-Gel and 95% in Air-Q). Blind intubation in difficult airways is less successful (scenario 3, 95% in I-Gel and 86% in Air-Q). In general, blind intubation is often considered an airway technique, potentially associated with serious complications including airway trauma and trachea rupture. Although, complications were not investigated in this study, a most recent large clinical trial did not report any major complication.[20] Given the fact, that success rate of insertion of the supraglottic airway devices was promising and even success rate of blind intubation was acceptable high, less experienced providers should refrain from endotracheal intubation and should place a supraglottic airway device instead.
Ease of intubation, as determined by subjective evaluation of the physicians participating in this study, was comparable with both supraglottic airway devices throughout all 3 airway scenarios. In contrast, direct laryngoscopy guided endotracheal intubation was rated much more difficult.
Participating physicians classified themselves as experienced with direct laryngoscopy guided endotracheal intubation however anesthesiologists or emergency physicians were excluded from the study. In Poland endotracheal intubation is performed mainly by anesthesiologists and emergency physicians. Physicians of other specialties or specialists in other fields of medicine are not experienced in endotracheal intubation but in several clinical situation may decide to perform endotracheal intubation especially in sudden cardiac arrest. This is especially important, as success rate in the easy airway scenario was 95%, but significantly dropped during scenario 2 and 3 (42% and 24%, respectively). This finding is significant, as success rate during easy airway indicates, that physicians were truly at least moderately experienced with this technic. Success rates during chest compressions or difficult airway scenario confirm previous findings, that moderately physicians should refrain from endotracheal intubation during CPR and should consider a supraglottic airway devices instead.[12,13,24,30]
Our study has several limitations. First, this study was performed in airway manikins, which might not mimic real conditions during real CPR. However, airway manikins are considered reliable airway teaching tools, and based on ethical considerations, cross-over studies like that might not be feasible in real patients undergoing real CPR. Nevertheless, results of airway manikin's studies are generally considered reliable.[31,32] Second, our participating physicians considered themselves are skilled in endotracheal intubation. We were not able to assess the number of endotracheal intubations in real patients. Consequently, this opens the possibility for self-overestimating of personal skills and experience.
5. Conclusions
In summary, our study indicates, that less to moderately experienced providers are able to perform endotracheal intubation in easy airways but fail during ongoing chest compressions and simulated difficult airway. Consequently, less to moderately experienced providers should refrain from endotracheal intubation during ongoing chest compressions during CPR and in expected difficult airways. Supraglottic airway devices are reliable alternatives and blind intubation through these devices is a valuable airway management strategy.
Author contributions
Conceptualization: Andrzej Bielski, Lukasz Szarpak.
Data curation: Lukasz Szarpak.
Formal analysis: Andrzej Bielski, Eva Rivas, Kurt Ruetzler, Oliver Robak, Lukasz Szarpak.
Investigation: Andrzej Bielski, Jacek Smereka, Mateusz Puslecki, Marek Dabrowski, Togay Evrin, Lukasz Szarpak.
Methodology: Andrzej Bielski, Jerzy Robert Ladny, Oliver Robak, Lukasz Szarpak.
Project administration: Lukasz Szarpak.
Resources: Mateusz Puslecki, Lukasz Szarpak.
Software: Michael Frass, Lukasz Szarpak.
Supervision: Kurt Ruetzler, Lukasz Szarpak.
Validation: Michael Frass, Lukasz Szarpak.
Visualization: Jacek Smereka, Jerzy Robert Ladny, Lukasz Szarpak.
Writing – original draft: Andrzej Bielski, Eva Rivas, Kurt Ruetzler, Jacek Smereka, Jerzy Robert Ladny, Oliver Robak, Lukasz Szarpak.
Writing – review & editing: Andrzej Bielski, Eva Rivas, Kurt Ruetzler, Jacek Smereka, Mateusz Puslecki, Marek Dabrowski, Jerzy Robert Ladny, Michael Frass, Oliver Robak, Togay Evrin, Lukasz Szarpak.
Footnotes
Abbreviations: CPR = cardiopulmonary resuscitation, ID = internal diameter, IQR = interquartile range, IRB = Institutional Review Board, SAD = supraglottic airway device, VAS = Visual Analog Scale.
Ethical approval: The study protocol was approved by the Institutional Review Board of the Polish Society of Disaster Medicine (Approval no. 43.12.2017.IRB).
Informed consent: Informed consent was obtained from all individual participants included in the study.
The authors have no conflicts of interest to disclose.
References
- [1].McCarthy JJ, Carr B, Sasson C, et al. Out-of-Hospital Cardiac arrest resuscitation systems of care: a scientific statement from the American Heart Association. Circulation 2018;137:e645–60. [DOI] [PubMed] [Google Scholar]
- [2].Link MS, Berkow LC, Kudenchuk PJ, et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015;132(18 suppl 2):S444–64. [DOI] [PubMed] [Google Scholar]
- [3].Freund B, Kaplan PW. A review of the utility of a hypothermia protocol in cardiac arrests due to non-shockable rhythms. Cardiol J 2017;24:324–33. [DOI] [PubMed] [Google Scholar]
- [4].Soar J, Nolan JP, Bottiger BW, et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult advanced life support. Resuscitation 2015;95:100–47. [DOI] [PubMed] [Google Scholar]
- [5].Telec W, Klosiewicz T, Zalewski R, et al. Chain of survival used for a victim of sudden cardiac arrest in a public place. Disaster Emerg Med J 2017;2:135–6. [Google Scholar]
- [6].Perkins GD, Travers AH, Berg RA, et al. Part 3: Adult basic life support and automated external defibrillation: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation 2015;95:e43–69. [DOI] [PubMed] [Google Scholar]
- [7].Benoit JL, Gerecht RB, Steuerwald MT, et al. Endotracheal intubation versus supraglottic airway placement in out-of-hospital cardiac arrest: a meta-analysis. Resuscitation 2015;93:20–6. [DOI] [PubMed] [Google Scholar]
- [8].Piegeler T, Roessler B, Goliasch G, et al. Evaluation of six different airway devices regarding regurgitation and pulmonary aspiration during cardio-pulmonary resuscitation (CPR) - a human cadaver pilot study. Resuscitation 2016;102:70–4. [DOI] [PubMed] [Google Scholar]
- [9].Piegeler T, Neth P, Schlaepfer M, et al. Advanced airway management in an anaesthesiologist-staffed Helicopter Emergency Medical Service (HEMS): a retrospective analysis of 1047 out-of-hospital intubations. Resuscitation 2016;105:66–9. [DOI] [PubMed] [Google Scholar]
- [10].Mulcaster JT, Mills J, Hung OR, et al. Laryngoscopic intubation: learning and performance. Anesthesiology 2003;98:23–7. [DOI] [PubMed] [Google Scholar]
- [11].Thoeni N, Piegeler T, Brueesch M, et al. Incidence of difficult airway situations during prehospital airway management by emergency physicians--a retrospective analysis of 692 consecutive patients. Resuscitation 2015;90:42–5. [DOI] [PubMed] [Google Scholar]
- [12].Gruber C, Nabecker S, Wohlfarth P, et al. Evaluation of airway management associated hands-off time during cardiopulmonary resuscitation: a randomised manikin follow-up study. Scand J Trauma Resusc Emerg Med 2013;21:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Goliasch G, Ruetzler A, Fischer H, et al. Evaluation of advanced airway management in absolutely inexperienced hands: a randomized manikin trial. Eur J Emerg Med 2013;20:310–4. [DOI] [PubMed] [Google Scholar]
- [14].Robak O, Leonardelli M, Zedtwitz-Liebenstein K, et al. Feasibility and speed of insertion of seven supraglottic airway devices under simulated airway conditions. CJEM 2012;14:330–4. [DOI] [PubMed] [Google Scholar]
- [15].Sip M, Dabrowska A, Prucnal K, et al. Supraglottic devices — future or everyday life? Disaster Emerg Med J 2017;2:74–83. [Google Scholar]
- [16].Kurowski A, Hryniewicki T, Czyżewski L, et al. Simulation of blind tracheal intubation during pediatric cardiopulmonary resuscitation. Am J Respir Crit Care Med 2014;190:1315. [DOI] [PubMed] [Google Scholar]
- [17].Ladny JR, Bielski K, Szarpak L, et al. Are nurses able to perform blind intubation? Randomized comparison of I-gel and laryngeal mask airway. Am J Emerg Med 2017;35:786–7. [DOI] [PubMed] [Google Scholar]
- [18].Bakker EJ, Valkenburg M, Galvin EM. Pilot study of the air-Q intubating laryngeal airway in clinical use. Anaesth Intensive Care 2010;38:346–8. [DOI] [PubMed] [Google Scholar]
- [19].Erlacher W, Tiefenbrunner H, Kastenbauer T, et al. CobraPLUS and Cookgas air-Q versus Fastrach for blind endotracheal intubation: a randomised controlled trial. Eur J Anaesthesiol 2011;28:181–6. [DOI] [PubMed] [Google Scholar]
- [20].Ruetzler K, Guzzella SE, Tscholl DW, et al. Blind intubation through self-pressurized, disposable supraglottic airway laryngeal intubation masks: an International, Multicenter, Prospective Cohort Study. Anesthesiology 2017;127:307–16. [DOI] [PubMed] [Google Scholar]
- [21].Kim MH, Lee JH, Choi YS, et al. Comparison of the laryngeal mask airway supreme and the i-gel in paralysed elderly patients: a randomised controlled trial. Eur J Anaesthesiol 2018;35:598–604. [DOI] [PubMed] [Google Scholar]
- [22].Haske D, Schempf B, Gaier G, et al. Performance of the i-gel during pre-hospital cardiopulmonary resuscitation. Resuscitation 2013;84:1229–32. [DOI] [PubMed] [Google Scholar]
- [23].Larkin C, King B, D’Agapeyeff A, et al. iGel supraglottic airway use during hospital cardiopulmonary resuscitation. Resuscitation 2012;83:e141. [DOI] [PubMed] [Google Scholar]
- [24].Ruetzler K, Roessler B, Potura L, et al. Performance and skill retention of intubation by paramedics using seven different airway devices--a manikin study. Resuscitation 2011;82:593–7. [DOI] [PubMed] [Google Scholar]
- [25].Park SK, Ko G, Choi GJ, et al. Comparison between supraglottic airway devices and endotracheal tubes in patients undergoing laparoscopic surgery: a systematic review and meta-analysis. Medicine (Baltimore) 2016;95:e4598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Ramachandran SK, Kumar AM. Supraglottic airway devices. Respir Care 2014;59:920–31. [DOI] [PubMed] [Google Scholar]
- [27].Beck-Schimmer B, Bonvini JM. Bronchoaspiration: incidence, consequences and management. Eur J Anaesthesiol 2011;28:78–84. [DOI] [PubMed] [Google Scholar]
- [28].Radu RR, Kaserer A, Seifert B, et al. Prevalence and in-hospital outcome of aspiration in out-of-hospital intubated trauma patients. Eur J Emerg Med 2018;25:362–7. [DOI] [PubMed] [Google Scholar]
- [29].Karim YM, Swanson DE. Comparison of blind tracheal intubation through the intubating laryngeal mask airway (LMA Fastrach) and the Air-Q. Anaesthesia 2011;66:185–90. [DOI] [PubMed] [Google Scholar]
- [30].Ruetzler K, Gruber C, Nabecker S, et al. Hands-off time during insertion of six airway devices during cardiopulmonary resuscitation: a randomised manikin trial. Resuscitation 2011;82:1060–3. [DOI] [PubMed] [Google Scholar]
- [31].Smereka J, Ladny JR, Naylor A, et al. C-MAC compared with direct laryngoscopy for intubation in patients with cervical spine immobilization: A manikin trial. Am J Emerg Med 2017;35:1142–6. [DOI] [PubMed] [Google Scholar]
- [32].Truszewski Z, Szarpak L, Czyzewski L, et al. A comparison of the ETView VivaSight SL against a fiberoptic bronchoscope for nasotracheal intubation of multitrauma patients during resuscitation. A randomized, crossover, manikin study. Am J Emerg Med 2015;33:1097–9. [DOI] [PubMed] [Google Scholar]


