Abstract
Background:
This study aims to evaluate the effectiveness and safety of lower limb nerve block combined with slow induction of light general anesthesia and tracheal intubation in hip surgery in the elderly.
Methods:
Thirty elderly patients who underwent hip surgery under the lower limb nerve block were randomly divided into 2 groups: slow induction of light general anesthesia and tracheal intubation group (group M), and laryngeal mask light general anesthesia group (group H). After undergoing total intravenous anesthesia without muscle relaxants, all patients received sciatic nerve, lumbar plexus, and paravertebral nerve blocks. The hemodynamic situations, dosage of anesthetics, time for awakening and extubation (or laryngeal mask removal), and incidence of respiratory adverse reactions in the induction period were recorded.
Results:
Compared with baseline levels, the difference in mean arterial pressure (MAP) value at each time point after intubation/laryngeal mask removal in both groups was not statistically significant (P > .05). Furthermore, the time for awakening and extubation/laryngeal mask removal, and anesthetic dosage were significantly decreased in group M, when compared with group H (P < .05). For the incidence of adverse reactions, the incidence of poor sealing and hypoxia was significantly lower in group M than in group H (P < .05), and the incidence of sore throat was significantly lower in group H than in group M (P < .05).
Conclusion:
Lower limb nerve block combined with slow induction of light general anesthesia and tracheal intubation was associated with smaller anesthetic dosage, and shorter duration of anesthesia induction and extubation/laryngeal mask after surgery.
Keywords: elderly patient, hip surgery, laryngeal mask, lower limb nerve block, slow induction of tracheal intubation
1. Introduction
As the aging of the society intensifies, more and more elderly patients with multisystem complications need to receive hip replacement. Hence, the risk of anesthesia and mortality in the perioperative period has significantly increased.[1,2] Studies have revealed that the anesthesia procedure is an independent factor that affects the mortality of elderly patients in orthopedics, and that peripheral nerve blocks can reduce the incidence of perioperative complications and mortality.[3–6] Common lumbar plexus and sciatic nerve block anesthesia has the advantages of small hemodynamic impact and good postoperative analgesic effect. However, it does not meet the requirements of hip replacement and requirements for general anesthesia.[7] The cause may be that in terms of nerve distribution, the range of the hip replacement exceeds the range innervated by the lumbar plexus and sciatic nerve. The combination of the lumbar plexus and sciatic nerve block and paravertebral nerve block can further increase the effect of peripheral nerve block in hip replacement. However, there are many controversies in the diffusion mode of local anesthetics in the paravertebral space,[8] and there are imperfect situations in clinic. Therefore, general anesthesia and laryngeal masks are used to remedy the shortcomings of nerve blocks in this kind of operation. The sealing effect of the laryngeal mask airway (LMA) is not as good as that of the endotracheal tube. Therefore, the use of a laryngeal mask increases the risk of gastrointestinal reflux, or even aspiration.[9] Furthermore, the shape and size of the airway in the pharynx of the elderly are different from those in the young, and these changes may affect the role of the supraglottic airway.[10,11] Complications related to the use of laryngeal masks have been frequently reported. As it is known, older people tend to have several other diseases, such as coronary heart disease, hypertension, chronic obstructive pulmonary disease (COPD), kidney dysfunction, and so on. Therefore, light anesthesia is preferred to reduce these risks in older patients. In view of the above situations, in order to solve key problems, such as the air tightness, safety and effectiveness of mechanical ventilation during the operation, slow induction of light general anesthesia and tracheal intubation (SILGA-TI) combined with lower limb nerve block was used during hip surgery in elderly patients, and its safety and effectiveness were assessed, providing a reference for the selection of clinical anesthetic methods.
2. Materials and methods
2.1. General information
The present study was conducted in accordance with the declaration of Helsinki and was approval by the Ethics Committee of our hospital. A written informed consent was obtained from all participants.
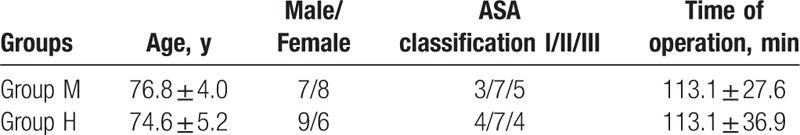
Thirty patients with ASA I-III, who underwent hip replacement in our hospital between November 2017 and March 2018, were included into the present study. Among these patients, 14 patients were male and 16 patients were female; the age of these patients ranged within 65 to 88 years. These patients were randomly divided into 2 groups: laryngeal mask light general anesthesia group (group H, n = 15) and slow induction of light general anesthesia and tracheal intubation group (group M, n = 15). The differences in age, ASA grade, and operation duration between these 2 groups were not statistically significant (Table 1). All patients were confirmed to have no local anesthetic allergy, block site infection, peripheral nerve disease, bradycardia, airway hyper-reactivity, and pulmonary infection. In group M, 7 patients had hypertension (2 patients were complicated with coronary heart disease), 2 patients had COPD, 2 patients had cardiac arrhythmia, 2 patients had cognitive impairment before the operation, and 2 patients had diabetes mellitus (1 patient was complicated with cerebral infarction). In group H, 5 patients had hypertension, 1 patient had hyperthyroidism, 1 patient had cardiac arrhythmia, and 1 patient had diabetes mellitus. Before the operation, all patients received medical treatments, and had no absolute surgical and anesthetic contraindications.
Table 1.
Comparison of general data between 2 groups ( , n = 15).
, n = 15).
2.1.1 Anesthesia protocol
All patients underwent preoperative fluid deprivation and fasting. Electrocardiogram (ECG), blood oxygen saturation (SPO2), bispectral index (BIS), and invasive arterial blood pressure were monitored after the patient was transferred to the operation room, and venous channels were established. During the operation, the BIS was kept within 40 to 60.
In group M, patients received an intravenous infusion of dexmedetomidine within 10 minutes (loading rate, 1 μg/kg). At the same time, the surface and root of the tongue and throat were sprayed with 2% lidocaine 2 to 3 times. Stepwise intravenous bolus injection of fentanyl was given (2 μg/kg). Then, pure oxygen was inhaled through a face mask. Five minutes before intubation, thyrocricoid puncture was performed, and 3 mL of 2% lidocaine was injected. Afterwards, tracheal intubation was performed after full surface anesthesia, and the corresponding device was connected to monitor end-tidal carbon dioxide (PETCO2), in which the position of the catheter was determined. The patients in group H were intravenously induced with 1 to 2 mg/kg of propofol and 1 to 2 μg/kg of fentanyl. Then, the LMA was placed. Patients in both groups were treated with single intravenous anesthesia without muscle relaxant, their spontaneous breathing was maintained, oxygen was continuously given at a rate of 2 L/min, and positive pressure ventilation was intermittently given to maintain PETCO2 within 30 to 45 mm Hg. Then, the intravenous infusion of propofol and remifentanil was continuously given during the operation, the pump rate was adjusted according to changes in blood pressure, heart rate (HR), and BIS, and fentanyl was added at the right time to maintain BIS within 45 to 60. Next, patients in both groups were placed in the lateral position, with their diseased limb stretching upward. The sciatic nerve (transgluteal approach), the lumbar plexus (the psoas interspace), and T12 paravertebral nerve were blocked under the guidance of a nerve stimulator and ultrasound machine. The initial stimulation current of the nerve stimulator (model: HNS12; Omnitest, Melsungen, Germany) was set at 1 mA and the frequency was set at 2 Hz. Under the guidance of the ultrasound machine (model: GE LOLIQ P6, GE Healthcare, USA), when the puncture needle (model: 4894235N; Omnitest, Melsungen, Germany) traveled near the target nerve, muscle contraction was induced. The sciatic nerve corresponds to the contraction of the gastrocnemius muscle, which manifests as the plantar flexion or dorsal flexure of the foot, while the lumbar plexus nerve corresponds to the contraction of the femoral quadriceps, which manifests as “kneecap dance.” The current intensity was adjusted to 0.3 to 0.5 mA. If the corresponding muscle group continued to present with contraction and blood was not observed during the withdrawal of the needle, 0.5% ropivacaine was injected. Then, 30 mL was injected to the sciatic nerve, and 20 mL was injected to the lumbar plexus. For the paravertebral nerve block, the puncturing point was set at a point 2 cm apart from the T12 spinous process on the affected side. An epidural needle was vertically inserted until it touched the transverse process, and the needle was slightly withdrawn obliquely toward the caudal direction. Then, the needle was pushed forward along the lower margin of the transverse process by 1.5 to 2.0 cm. At that time, the needle was felt to break through something and enter an empty space. When the connecting syringe revealed that the resistance disappeared, and blood or cerebrospinal fluid was not observed during the withdrawal of the needle, 10 mL of 0.5% ropivacaine was slowly injected.
2.1.2 Assessment of the block
When the quadriceps femoris contracted strongly, then the current intensity was 0.5 mA, and the block was considered successful.
2.2. Observation indexes
MAP and HR were recorded before anesthesia induction (T1), immediately before tracheal intubation/laryngeal mask placement (T2), at 1 minute after tracheal intubation/laryngeal mask placement (T3), at 3 minutes after tracheal intubation/laryngeal mask placement (T4), and at 5 minutes after tracheal intubation/laryngeal mask placement (T5). The dosage for general anesthesia, the awakening time after the operation, and the time of removal of the tracheal catheter and laryngeal mask were recorded. The following adverse reactions were observed: poor sealing, hypoxia, reflux and saspiration, the incidence of sore throat, and the patient's tolerance to the tracheal tube.
2.3. Statistical methods
The IBM SPSS Statistics 21.0 (the United States, California) was used to conduct the statistical analysis. All results were expressed as mean ± standard deviation (SD). Shapiro–Wilk test was used to analyze the normal distribution of data. Intragroup comparison was conducted using analysis of variance, and intergroup comparison was conducted using t test. For multiple comparisons, each value was compared by 1-way analysis of variance (ANOVA) following Dunnett test when each datum was normally distributed, while non-normally distributed continuous data were compared using nonparametric tests. A value of P < .05 was considered statistically significant.
3. Results
3.1 Hemodynamic situations
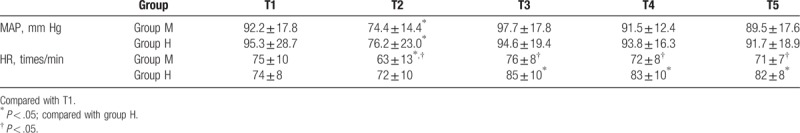
Compared with time point T1, MAP values in the 2 groups from anesthesia induction to intubation (T2) decreased to varying degrees, and the differences were statistically significant (P < .05). The MAP values in these 2 groups increased after tracheal intubation/laryngeal mask placement (T3), and the amplitudes of the fluctuation were within the normal range. The differences in MAP values between T3-T5 and T1 were not statistically significant (P > .05). In group M, HR was significantly lower at T2 than before induction (T1) (P < .05), and no serious bradycardia occurred. In group H, HR was significantly higher at T3, T4, and T5 than before induction (T1) (P < .05). Furthermore, HR at the T2-T5 time points was significantly lower in group M, when compared with group H (P < .05, Table 2).
Table 2.
Comparison of MAP and HR at each time point between the 2 groups ( , n = 15).
, n = 15).
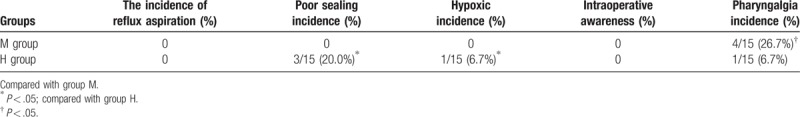
3.2 Incidence of adverse reactions
All patients in group M were successfully intubated in one time. In group H, 3 patients needed to receive a second replacement or adjustment.
3.3 Lateral position
All patients in group M were well-ventilated and oxygenated. SPO2 was maintained within 96% to 100%, and no hypoxia occurred. In group H, poor sealing, air leak, and a decrease in SPO2 occurred in 3 patients, and the minimum was 88%. Ventilation was improved after replacing the laryngeal mask, and adjusting the head and neck, the position of the laryngeal mask and the pressure of the laryngeal mask gasbag. No reflux or aspiration occurred in any patient.
3.4 Incidence of sore throat
In the postoperative follow-up, sore throat occurred in 4 patients in group M and in 1 patient in group H. The sore throat of all patients was spontaneously relieved within 48 hours after the operation. The 2 groups of patients had good tolerance to tube/laryngeal mask during the operation. No intraoperative awareness occurred (Table 3).
Table 3.
The comparison of incidence of adverse reactions between 2 groups.
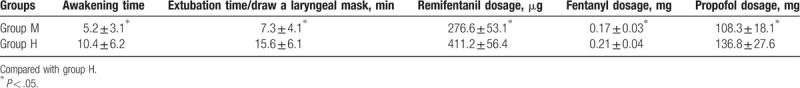
3.5 Comparison of the time of awakening and extubation/laryngeal mask removal, and the dosage of anesthetics
The time for awakening and the time for extubation/laryngeal mask removal, and the dosage of anesthetics were significantly lower in group M than in group H (P < .05, Table 4).
Table 4.
Two groups of patients awaken and extubation time/draw a laryngeal mask anesthetics dosage of contrast (X ± S, n = 15).
4. Discussion
As elderly patients have degenerative changes in all organs, and are often combined with endocrine, cardiovascular, neurological, and respiratory diseases before the operation, most of them have slow reactions and low autonomic nerve regulatory function. During the operation, if accidents such as anoxia and low perfusion occur, they can be induced to develop complications, such as myocardial ischemia, arrhythmia, and nerve dysfunction, which would directly influence the survival and prognosis of the patient. Therefore, it is essential to choose an appropriate anesthesia procedure. For hip surgery in the elderly, hemodynamic fluctuations caused by intraspinal anesthesia used in the past have been unavoidable, and the use of anticoagulants has also become a risk for intraspinal anesthesia. Traditional general anesthesia and tracheal intubation are also unable to avoid disadvantages, such as hemodynamic fluctuations, slow recovery of respiratory function, delayed awakening, imperfect postoperative analgesia, and high incidence of postoperative cognitive dysfunction. Peripheral nerve blocks can be used for patients with poor cardiopulmonary function, allowing them to safely ride out the perioperative period.[4] However, it also has the shortcoming of incomplete block, which has often been solved through the additional use of intravenous anesthesia or laryngeal mask general anesthesia. In the process of laryngeal mask use, complications such as reflux and aspiration, oropharyngeal cavity tissue damage, and ventilation failure would occur. Particularly in the lateral position, the success rate of a 1-stop operation is reduced, the position needs to be adjusted again, and the preparation of conversion to the supine position and tracheal intubation should be made. Therefore, a laryngeal mask cannot replace tracheal intubation under any condition. The subjects in the present study were mainly elderly patients who underwent hip surgery, and usually chose the lateral position, which belongs to the compulsory position. Once complications, such as reflux, aspiration, and hypoxia, occurred during the operation, serious consequences can be induced. Therefore, it is essential to maintain good airway management and hemodynamic stability. Laryngeal mask light general anesthesia and SILGA-TI were performed before the nerve block to avoid the pain caused by the placement of position during anesthesia. The combination of an ultrasound machine and nerve stimulator was used to assist in peripheral nerve block, which resulted in accurate positioning and a good analgesic effect, and the operation was simple to perform. This was beneficial for systemic circulation stability. In particular, it had the advantages of rapid onset, long duration of analgesia, and stable hemodynamics during anesthesia in elderly patients.[12] Furthermore, the success rate of the operation greatly improved, and the incidence of complications was reduced. The main purpose of the present study was to observe the safety and reliability of SILGA-TI combined with lower limb nerve block in elderly patients.
Previous literatures have reported that[13–15] dexmedetomidine can reduce the stress response caused by endotracheal intubation, and that it can be used for conscious tracheal intubation in combination with opioids. An infusion of 0.6 μg/kg of dexmedetomidine followed by a small dose at 0.2 μg/kg/h could produce a good sedation and amnesic effect. Furthermore, a loading rate of 1 μg of dexmedetomidine (completed within 10 minutes) for conscious tracheal intubation has a low and mild influence on the hemodynamics. In recent years, many studies at home and abroad have reported that dexmedetomidine has a certain intervention effect on postoperative cognitive impairment after general anesthesia in elderly patients. In the present study, the research subjects were mainly elderly patients, and elderly patients can extremely easily develop brain dysfunction after an operation, especially after general anesthesia, that is, elderly postoperative cognitive dysfunction.[16] Therefore, in the present study, dexmedetomidine and fentanyl were chosen as intravenous inducers to reduce the incidence of cognitive impairment in the perioperative period, and fully inhibit the stress response caused by tracheal intubation.
For a long time, tracheal intubation has been the gold standard for the maintenance of respiratory tract management in patients with general anesthesia during an operation. It can effectively send anaesthetizing gas into the trachea and effectively control the ventilation and oxygen supply. However, complications associated with tracheal intubation, such as injury of the tooth and soft tissue of the oral cavity, and cardiovascular reactions associated with the insertion/removal of the tracheal tube, have hindered the application of tracheal intubation in elderly patients during the perioperative period.[17] As a device used on the glottis, compared with tracheal intubation, a laryngeal mask has the advantages of simple operation, rapid placement, low depth of anesthesia, slight injury, good tolerance, small cardiovascular response, and low body stress response.[18–20] In the present study, it was observed that in the process of induction and intubation, the amplitude of blood pressure fluctuation was slight and the hemodynamics was stable in group M. This is consistent with that reported in a previous study.[15] Compared with group H, the difference was not statistically significant. Due to the anti-sympathetic effect of dexmedetomidin, HR significantly decreased in group M, and no serious bradycardia occurred. Both applications of tracheal intubation and laryngeal mask need a certain depth of anesthesia or sedation to inhibit the sympathetic and parasympathetic excitation caused by the operation. However, excessive sedation or excessive anesthesia would inevitably lead to a series of risk factors, such as cardiovascular system inhibition and respiratory depression. The present study revealed that patients in group M were in a state of shallow sleep, in which the patient could easily be woken up, and had spontaneous respiration and good tube tolerance. The reason may be the large dose of dexmedetomidine and the good superficial anesthesia of the tracheal mucosa and pharynx.[21] The slow response and lower stress ability of elderly patients was also one of the reasons. The time for awakening and extubation was significantly shorter in group M than in group H, and the dose for general anesthesia significantly decreased in group M, when compared with group H. The result revealed that less dosage of anesthetics can better inhibit the hemodynamic fluctuations and stress responses caused by SILGA-TI in elderly patients, and effectively maintain the appropriate depth of anesthesia during the operation.
Due to strict fasting and fluid deprivation before the operation, no reflux or aspiration occurred in any of the patients. However, air leakage occurred in 3 patients in group H. Among these patients, SPO2 decreased to 88% in 1 patient, which was improved after adjustment, and the operation was successfully completed. Although no situations, such as airway obstruction and ventilation failure, occurred during this period, elderly patients had poor cardiopulmonary function reserve, and they especially had poor tolerance to hypoxia. When elderly patients have hypoxic manifestations during the operation, the risk of anesthesia management must be increased. In group M, no similar situation occurred in any of the patients during the operation. These results revealed that tracheal intubation was more safe and reliable in the management of ventilation. However, the incidence of postoperative sore throat was significantly higher in group M than in group H. These results reveal that group H was superior to group M in avoiding the complications of intubation.
In the present study, the combination of a nerve stimulator and ultrasound machine was used to guide the lumbar plexus and sciatic nerve block and paravertebral nerve block, which greatly increased the success rate of the peripheral nerve block in hip replacement. Laryngeal mask anesthesia or SILGA-TI was additionally used to avoid the adverse consequences caused by possible respiratory depression when the block was not perfect, and analgesic and sedative drugs must be used for remedy. In the present study, the operation in both groups was successfully completed, and the effect of anesthesia was satisfactory. The increase in the incidences of air leakage and hypoxia in group H may be associated with the type of laryngeal mask, proficiency in practice, management experience, and sample size. Tracheal intubation is undoubtedly a more reliable tool for airway management. The respiratory tract can be forwardly controlled through tracheal intubation, and respiration and circulation are easily regulated. When an emergency occurs during the operation, such as circulation fluctuations caused by fat embolism, shedding of the thrombus in deep veins and bleeding, the surgeon must perform circulatory resuscitation. This would be helpful to reduce risk in anesthetic management and ensure the safety of elderly patients in the perioperative period.
For elderly patients, anesthesia procedures are absolutely not safe. The results of the present study revealed that when lower limb nerve block combined with SILGA-TI was applied in hip surgery in elderly patients, the time for awakening and extubation was shortened, and the dose for general anesthesia was small, but hemodynamic stability in the induction period could be maintained and safe and reliable airway conditions could be achieved. Compared with the combined use of general anesthesia and laryngeal masks, lower limb nerve block combined with SILGA-TI can reduce complications caused by airway management, such as poor sealing, hypoxia, and reflux and aspiration, during anesthesia, and can more safely and reliably remedy the incomplete nerve block of the lower limbs. Although it induces a higher incidence of postoperative sore throat, it remains a worthwhile anesthesia procedure for elderly patients with poor preoperative basic conditions and high anesthesia management requirements.
Author contributions
Data curation: Zhengyuan Shi.
Formal analysis: Zhengyuan Shi, ChunNan Jiang.
Writing – original draft: Zhengyuan Shi, ChunNan Jiang.
Writing – review & editing: Zhengyuan Shi, ChunNan Jiang, Gang Shao.
Footnotes
Abbreviations: BIS = bispectral index, COPD = chronic obstructive pulmonary disease, ECG = electrocardiogram, LMA = laryngeal mask airway, MAP = mean arterial pressure, PETCO2 = end-tidal carbon dioxide, SILGA-TI = slow induction of light general anesthesia and Tracheal intubation, SPO2 = blood oxygen saturation.
The authors report no conflict of interest.
The author(s) of this work have nothing to disclose.
References
- [1].Liu XW, Zi Y, Xiang LB, et al. Total hip arthroplasty: a review of advances, advantages and limitations. Int J Clin Exp Med 2015;8:27–36. [PMC free article] [PubMed] [Google Scholar]
- [2].Bilsel K, Erdil M, Gulabi D, et al. Factors affecting mortality after hip fracture surgery: a retrospective analysis of 578 patients. Eur J Orthop Surg Traumatol 2013;23:895–900. [DOI] [PubMed] [Google Scholar]
- [3].Karaca S, Ayhan E, Kesmezacar H, et al. Hip fracture mortality: is it affected by anesthesia techniques. Anesthesiol Res Pract 2012;2012:708754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Gamli M, Sacan O, Baskan S, et al. Combined lumbar plexus and sciatic nerve block for hip fracture surgery in a patient with severe aortic stenosis. J Anesth 2011;25:784–5. [DOI] [PubMed] [Google Scholar]
- [5].Asao Y, Higuchi T, Tsubaki N, et al. [Combined paravertebral lumbar plexus and parasacral sciatic nerve block for reduction of hip fracture in four patients with severe heart failure]. Masui 2005;54:648–52. [PubMed] [Google Scholar]
- [6].Flack S, Anderson C. Ultrasound guided lower extremity blocks. Paediatr Anaesth 2012;22:72–80. [DOI] [PubMed] [Google Scholar]
- [7].Amiri HR, Zamani MM, Safari S. Lumbar plexus block for management of hip surgeries. Anesth Pain Med 2014;4:e19407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Marhofer D, Marhofer P, Kettner SC, et al. Magnetic resonance imaging analysis of the spread of local anesthetic solution after ultrasound-guided lateral thoracic paravertebral blockade: a volunteer study. Anesthesiology 2013;118:1106–12. [DOI] [PubMed] [Google Scholar]
- [9].Wang HE, Szydlo D, Stouffer JA, et al. Endotracheal intubation versus supraglottic airway insertion in out-of-hospital cardiac arrest. Resuscitation 2012;83:1061–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Lin BC, Wu RS, Chen KB, et al. A comparison of the classic and a modified laryngeal mask airway (OPLAC™) in adult patients. Anesth Analg 2011;112:539–44. [DOI] [PubMed] [Google Scholar]
- [11].Alexiev V, Ochana A, Abdelrahman D, et al. Comparison of the Baska(®) mask with the single-use laryngeal mask airway in low-risk female patients undergoing ambulatory surgery. Anaesthesia 2013;68:1026–32. [DOI] [PubMed] [Google Scholar]
- [12].Shaw A, Mohyeldin A, Zibly Z, et al. Novel tunneling system for implantation of percutaneous nerve field stimulator electrodes: a technical note. Neuromodulation 2015;18:313–6. discussion 316. [DOI] [PubMed] [Google Scholar]
- [13].El-Shmaa NS, El-Baradey GF. The efficacy of labetalol vs dexmedetomidine for attenuation of hemodynamic stress response to laryngoscopy and endotracheal intubation. J Clin Anesth 2016;31:267–73. [DOI] [PubMed] [Google Scholar]
- [14].Shen SL, Xie YH, Wang WY, et al. Comparison of dexmedetomidine and sufentanil for conscious sedation in patients undergoing awake fibreoptic nasotracheal intubation: a prospective, randomised and controlled clinical trial. Clin Respir J 2014;8:100–7. [DOI] [PubMed] [Google Scholar]
- [15].Tsai CJ, Chu KS, Chen TI, et al. A comparison of the effectiveness of dexmedetomidine versus propofol target-controlled infusion for sedation during fibreoptic nasotracheal intubation. Anaesthesia 2010;65:254–9. [DOI] [PubMed] [Google Scholar]
- [16].Parikh SS, Chung F. Postoperative delirium in the elderly. Anesth Analg 1995;80:1223–32. [DOI] [PubMed] [Google Scholar]
- [17].Zoremba M, Aust H, Eberhart L, et al. Comparison between intubation and the laryngeal mask airway in moderately obese adults. Acta Anaesthesiol Scand 2009;53:436–42. [DOI] [PubMed] [Google Scholar]
- [18].Lu W, Zheng J, Gao L, et al. A comparison of classic laryngeal mask airway insertion between lightwand- and standard index finger-guided techniques. J Clin Anesth 2016;33:309–14. [DOI] [PubMed] [Google Scholar]
- [19].Polat R, Aydin GB, Ergil J, et al. Comparison of the i-gel™ and the Laryngeal Mask Airway Classic™ in terms of clinical performance. Rev Bras Anestesiol 2015;65:343–8. [DOI] [PubMed] [Google Scholar]
- [20].Kim MS, Lee JS, Nam SB, et al. Randomized comparison of actual and ideal body weight for size selection of the laryngeal mask airway classic in overweight patients. J Korean Med Sci 2015;30:1197–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Chopra P, Dixit MB, Dang A, et al. Dexmedetomidine provides optimum conditions during awake fiberoptic intubation in simulated cervical spine injury patients. J Anaesthesiol Clin Pharmacol 2016;32:54–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


