Abstract
Background:
Men who have sex with men with histories of homophobic victimization bear heightened risk of unstable housing and methamphetamine use. However, it is unclear whether unstable housing explains the link between homophobic victimization and methamphetamine use in this group. The present study aims to test associations between homophobic victimization, unstable housing, and recent methamphetamine use across 24 months in a cohort of men of color who have sex with men (MoCSM).
Methods:
Our analysis stems from data of 1,342 person-visits from 401 MoCSM participating in an ongoing cohort study. We performed a lagged multilevel negative binominal regression to test the association between past homophobic victimization and recent unstable housing, and a lagged multilevel ordered logistic regression to test the association between past homophobic victimization recent methamphetamine use. We then performed a path analysis to test whether recent unstable housing mediates the association between past homophobic victimization and recent methamphetamine use.
Results:
Findings showed homophobic victimization associated significantly with increased odds of unstable housing (IRR = 1.70, 95% CI [1.35, 2.14], p < .001) and recent methamphetamine use (OR = 1.40, 95% CI [1.15, 1.71], p = .001). Mediation analysis indicated that past homophobic victimization was indirectly associated with recent methamphetamine use via unstable housing (OR = 1.06 (95% CI [1.01, 1.11], p = .010).
Conclusion:
Our findings suggest that homophobic victimization and unstable housing should be addressed alongside treatment and prevention of methamphetamine use in MoCSM.
Keywords: methamphetamine, homophobia, victimization, Black, Latino, unstable housing, men who have sex with men
1. Introduction
A growing body of literature recognizes that men who have sex with men (MSM) are often burdened with concurrent and interacting health threats and conditions (e.g., homophobia, unstable housing, substance abuse, HIV infection), that can synergistically affect each other (Friedman, 2015; Herrick, 2012; Stall, 2008). Men of color who have sex with men (MoCSM) (Buttram, 2015; Dyer, 2012), may experience even more of these “syndemic” health problems due to the intersectional challenges of having both a racial and sexual minority status (Dyer, 2012; Mereish and Bradford, 2014). In Los Angeles and other areas along the urban West Coast, MoCSM report high rates of methamphetamine use (Reback, 2008; Reback et al., 2013), which in turn can interact with syndemic conditions that include HIV acquisition (Plankey, 2007), HIV disease progression, psychiatric symptoms (Cruickshank and Dyer, 2009), and chronic health problems, especially cardiovascular diseases (Darke et al., 2017; Hassan et al., 2016; Kaye et al., 2007).
Multiple studies have found that minority stress—the excess stress of minority status (e.g., racial or sexuality-based)—is associated with abuse of substances, such as methamphetamine, in sexual minority communities (Hughes et al., 2010; McCabe et al., 2010). Compared to heterosexual persons, MSM are burdened by higher rates of victimization (e.g., verbal harassment, violence, threats), unstable housing (Choi et al., 2015; Durso and Gates, 2012), and of substance abuse (Goldbach et al., 2015; Hughes et al., 2010; McCabe et al., 2010; Slater et al., 2017), all which are foundational to experiences of minority stress. In large national samples, MoCSM have greater odds of mental health problems compared to White MSM, who are already at heightened risk of mental health problems compared to their heterosexual peers (Bostwick et al., 2014). Furthermore, experiences of both homophobia and racism appear to contribute to greater levels of distress in MoCSM, suggesting that minority stress can be additive (McConnell et al., 2018).
Underlying these syndemic experiences of minority stress is the role of macro-level or structural level stigma related to sexual orientation on the health of MSM. Structural level stigma which can manifest in the forms of societal level policies, community-level attitudes, cultural norms and institutional policies that marginalize or alienate sexual minorities and people of color and are linked to adverse health outcomes (Hatzenbuehler, 2014). For instance, the prevalence of psychiatric disorders among sexual minority adults was significantly higher in states that did not have a hate-crime statute and employment nondiscrimination policy that include sexual orientation as a protected class (Hatzenbuehler et al., 2010). Those living in neighborhoods with high hate-crime rates were significantly more likely to report suicidal ideation than those in lowhate crime areas (Duncan and Hatzenbuehler, 2014). However, the mechanisms that potentially link minority stress to substance use—particularly methamphetamine use—among racial minority MSM remain relatively underexplored.
Among MSM, homophobic victimization can enhance already high risks for unstable housing (the lack of a regular place of residence). According to a nationwide survey of homeless agencies by the Williams Institute of the University of California, Los Angeles, about 40% of homeless persons—specifically those who have no housing or residence—identify as lesbian, gay, bisexual, transgender, or queer (LGBTQ) (Durso and Gates, 2012). The vast majority of homeless LGBTQ clients reported histories of homophobic victimization and family rejection, and 55–60% claimed the primary reason for their homelessness was being forced from their homes or of fleeing homophobia from family members (Choi et al., 2015). Among LGBTQ homeless individuals, persons of color are disproportionately represented, with 31% identifying as Black and 14% Latino (Choi et al., 2015).
Unstable housing and methamphetamine use can be reciprocally associated (Johnson and Chamberlain, 2008). In Los Angeles, 23–25% of homeless individuals report using methamphetamine (23–25%) (Nyamathi et al., 2008; Yoshioka-Maxwell et al., 2015), a rate that far exceeds the general adult population in Los Angeles (2–7%) (County of Los Angeles Public Health, 2016). People who are homeless are more vulnerable to using methamphetamine due to constrained social networks, to conforming to drug culture to gain trust within the homeless community, and to cope with the suffering associated with being homeless (Barman-Adhikari et al., 2016; Bungay et al., 2006; Nyamathi et al., 2008; Yoshioka-Maxwell et al., 2015). Likewise, chronic methamphetamine use is a risk factor for financial problems and unstable housing (Johnson and Chamberlain, 2008). However, the majority of homeless people using methamphetamine report being homeless prior to initiating methamphetamine (66%) rather than the converse (15%) (Johnson and Chamberlain, 2008), and longitudinal research has demonstrated that substance abuse did not independently predict subsequent homelessness (Fertig and Reingold, 2008; McVicar et al., 2015).
Experiences of homophobia may directly contribute to methamphetamine use in MSM who have stable housing. Some researchers suggest that homophobia and other forms of stigmatization may trigger mental health problems associated with substance abuse or a desire to misuse methamphetamine to relieve feelings of distress (McCabe et al., 2010; Roy and Perry, 2009; Wilton, 2008). Being HIV-positive may further complicate risk or severity of methamphetamine use for MoCSM who struggle with experiences of homophobic victimization and unstable housing (Durvasula and Miller, 2014; Plankey, 2007). Living with HIV can be fraught with struggles that exacerbate substance abuse such as psychosocial problems, HIV-specific traumatic stress, and experiences of violence and stigma, all of which can be medicated with methamphetamine (Argento et al., 2017; Carrico et al., 2010; Chartier et al., 2009; Durvasula and Miller, 2014). Elucidating the degree to which homophobic victimization, unstable housing, and methamphetamine use among HIV-negative and HIV-positive MoCSM, would help to identify needs of MoCSM vulnerable to homophobia and related consequences. Therefore, the aim of this analysis is to test whether severity of homophobic victimization is associated with a corresponding increase in levels of methamphetamine use in MoCSM, and to estimate the degree to which unstable housing mediates this association.
2. Methods
2.1. Study design
Data for the present study comes from [blinded cohort name]—an ongoing National Institute on Drug Abuse (NIDA)-sponsored longitudinal cohort study of HIV-negative and HIVpositive MSM with varied substance use behaviors. Additional details of the [blinded cohort name] are published elsewhere (Aralis et al., 2018; Okafor et al., 2017). Briefly, the [blinded cohort name] is focused on enrolling Black/African American and Latino/Hispanic MSM between 18 and 45 years of age who were born male. In addition, HIV-negative MSM were eligible if they reported unprotected anal intercourse with a man in the past 6 months. The primary goal of the [blinded cohort name] is to explore the direct and indirect effects of substance use on the immune system and on behavior and to identify links to HIV transmission dynamics. Recruitment of participants began in July 2014. Participants in the [blinded cohort name] return every 6 months for physical examinations, laboratory testing, specimen collection, and completion of a survey collecting sociodemographic, psychosocial, psychological and behavioral data. All behavioral questions were assessed using computer-assisted self-interview (CASI) (Gribble et al., 2000). The total analytic sample consisted of 1,342 person-visits from 401 participants. All study procedures have been approved by the Institutional Review Board of the authors’ home institution.
2.2. Measures
In the computer assisted self-interview (CASI), homophobic victimization in the past 12 months was measured using five items from the National Health, Aging, and Sexuality/Gender Study (NHAS) (Fredriksen-Goldsen and Kim, 2017). Responses were dichotomous—(0) “No” to (1) “Yes”—to items such as “I was threatened with physical violence because I am, or was thought to be, gay or bisexual” and “I was verbally insulted (yelled at, criticized) because I am, or was thought to be, gay or bisexual.” These five items were summed to make a composite score of homophobic victimization with a possible range from 0 to 5, with greater scores representing greater severity. To specify that the homophobic victimization score precedes unstable housing and homophobic victimization, this score was lagged by one observation.
To measure duration of unstable housing, the CASI asked “Approximately how many days have you not had a regular place to stay in the last six months?” We converted the units of this variable from days to weeks of unstable housing to allow for more meaningful interpretation of results.
The measure of methamphetamine use in the past six months was adapted from the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) (WHO, 2010) on an ordinal scale ranging from (0) “None,” (1) “Once,” (2) “Less often,” (3) “Monthly,” (4) “Weekly,” and (5) “Daily” to the question “In the past 6 months, how often have you used methamphetamine (speed, crystal meth, ice, etc.)” administered via CASI.
HIV status was determined from HIV tests taken at clinic visit. Sociodemographics including age, race, education level, employment status, and history of incarceration were obtained via CASI.
2.3. Analyses
All statistical analysis was conducted in Stata 15 (StataCorp, 2017). To preserve the temporal order between homophobic victimization and unstable housing, the homophobic victimization variable was lagged by one time-point, so that the model evaluated associations between homophobic victimization at a specific time-point and unstable housing at a subsequent time-point (Bhargava and Sargan, 1983; Rabe-Hesketh and Skrondal, 2008). We computed the mean age of participants at study entry, and tabulated frequencies and percentages of past homophobic victimization score (lagged), unstable housing, methamphetamine use, HIV status, race, education level, employment status, and history of incarceration. We computed Spearman’s rank correlations of unstable housing by homophobic victimization, unstable housing, age, and education level. We computed Spearman’s rank correlations of methamphetamine use on the same variables, as well as on unstable housing. We tested HIV status and history of incarceration on unstable housing and methamphetamine use using Wilcoxon-Mann-Whitney tests, as well as race and employment status on unstable housing and methamphetamine use using KruskallWallis tests.
We conducted a lagged random intercept negative binomial regression to test whether past homophobic victimization (lagged one observation) was associated with recent duration of unstable housing (weeks). We then conducted a lagged random intercept ordered logistic regression to test whether past homophobic victimization was associated with recent methamphetamine use, an ordinal outcome. In both multilevel models, we adjusted for HIV status, age, race, education level, employment status, history of incarceration, and time elapsed since study entry (in days). We also explored whether HIV-positive serostatus for interaction with homophobic victimization using a product term of the two variables in initial modeling. Retention of the product term in the final model depended on whether it was significant. Both models adjusted for the correlations of repeated measurements of the outcome within participants.
To test whether the association between homophobic victimization and methamphetamine use was mediated by unstable housing, we conducted a multilevel mediation analysis, modeling direct paths from past homophobic victimization (lagged) to recent unstable housing and to methamphetamine use, and from unstable housing to methamphetamine use. We used Mplus 6 (Muthén and Muthén, 2010) within the Stata 15 interface via the “runmplus” extension (Jones, 2015) for the multilevel mediation analysis. Associations with methamphetamine use were estimated using the ordinal logistic regression.
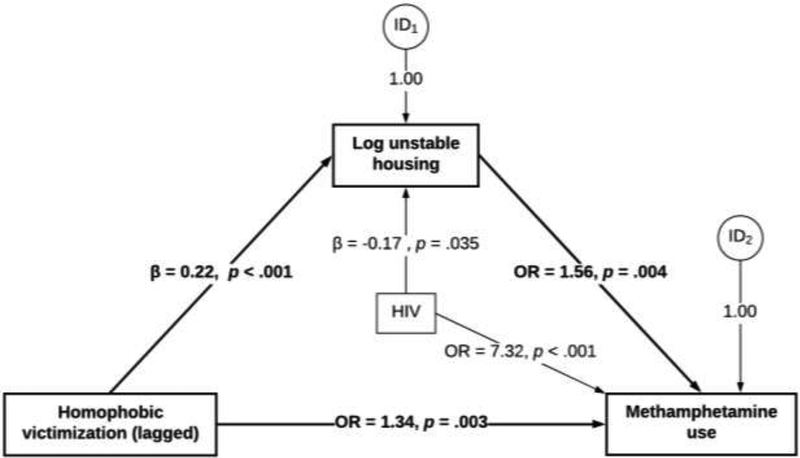
Current estimation approaches of mediation can only handle numerical mediators as continuous variables but not count variables (MacKinnon, 2012; Muthén, 2011). Therefore, we transformed unstable housing, originally a count variable (number of weeks), by computing its natural logarithm. Mediation, or indirect association, between homophobic victimization and methamphetamine use (via log unstable housing) was the exponentiated product term of the linear regression slope estimate of homophobic victimization on log unstable housing multiplied by the log odds ratio of log unstable housing on methamphetamine use (see Figure 1) (MacKinnon, 2012; Muthén, 2011).
Figure 1.
Multilevel mediation model of past homophobic victimization, recent unstable housing, and recent methamphetamine use (Nvisits = 1,342, n = 401)
Notes: All estimates adjust for HIV status, age at study entry, race, education, employment status, incarceration, time elapsed, and clustering on participant ID number; indirect association between prior homophobic victimization and methamphetamine use was OR = 1.06 (95% CI [1.01, 1.11], p = .010); total association was OR = 1.42 (95% CI [1.17, 1.72], p < .001); percent mediated = 16.6%
3. Results
3.1. Participant characteristics
The mean age of our sample at study entry was 31.7 years. Half of participants were HIV-positive by study design. Most participants were Black (39.8%) or Latino (47.9%), while the remainder White (7.59%) or other (4.81%). At baseline (second observation), 51.7% of participants held a high school degree or lower, and 43.8% were unemployed. About 36% of participants reported having ever been incarcerated for more than 24 hours. Nearly 20% (n = 78) of participants reported one experience of homophobic victimization in the past 12 months, while 27.3% (n = 108) of participants reported two or more experiences of homophobic victimization in the past 12 months. Again, the past homophobic victimization variable was lagged to reflect responses from the prior observation. Nearly 25% of participants reported unstable housing for least one day during the past six months. Greater than 20% of participants reported using methamphetamine between once to monthly in the past six months, and 15.9% of participants reported using methamphetamine weekly or more in the past six months.
3.2. Univariate associations
Table 1 displays bivariate nonparametric statistics for the outcomes unstable housing and methamphetamine use at baseline. Greater homophobic victimization was correlated with greater duration unstably housed (Spearman’s rho (ρ) = .19, p < .001), while greater education level was correlated with lower duration unstably housed ρ = −.15, p < .003). Both full- and part-time employment were associated with significantly less weeks unstably housed (p = .003), while having a history of incarceration was associated with significantly more weeks unstably housed (p < .001).
Table 1.
Baseline non-parametric bivariate tests of past homophobic victimization (lagged) and other characteristics on recent unstable housing and methamphetamine use (n = 401)
| Unstable housing | Methamphetamine use | |||
|---|---|---|---|---|
| Spearman’s ρ | p | Spearman’s ρ | p | |
| Past homophobic victimization a | .19 | <. 001 | .13 | < .001 |
| Unstable housing a† | -- | .29 | < .001 < | |
| Age (in years) at study entry a | .01 | .977 | .19 | < .001 |
| Education level a | -0.15 | .003 | -.16 | .002 |
| Mean rank sum | p | Mean rank sum | p | |
| Race b | .749 | .046 | ||
| White | 213.12 | 212.60 | ||
| Black | 200.77 | 188.00 | ||
| Latino | 192.34 | 209.51 | ||
| Other | 207.58 | 143.08 | ||
| Employment status b | .003 | < .001 | ||
| Unemployed | 221.11 | 232.08 | ||
| Part-time | 190.44 | 199.03 | ||
| Full-time | 173.68 | 156.41 | ||
| Student | 177.60 | 157.00 | ||
| History of incarceration c | < .001 | < .001 | ||
| No | 186.85 | 177.70 | ||
| Yes | 217.43 | 228.67 | ||
| HIV status c | .524 | < .001 | ||
| Negative | 200.80 | 166.55 | ||
| Positive | 195.27 | 228.67 | ||
Note: Past homophobic victimization was lagged by 1 observation; therefore, all bivariate tests use the second observation as baseline data.
# of weeks not having a regular place to stay in the last six months
Spearman’s rank correlation
Kruskall-Wallis test
Wilcoxon-Mann-Whitney test
Greater homophobic victimization (Spearman’s rho (ρ) = .13, p < .001), duration unstably housed (ρ = .29, p < .001), and age (ρ = .19, p < .001) were all correlated with greater methamphetamine use at baseline, while greater education level (ρ = −.16, p = .002) was correlated with lower methamphetamine use. Unemployment (p < .001), having a history of incarceration (p < .001), HIV-positive serostatus (p < .001) were associated with greater methamphetamine use at baseline. There were no significant differences in baseline methamphetamine use by race.
3.3. Multilevel models
Table 2 displays the incidence rate ratios (IRRs) for the lagged multilevel negative binomial regression of past homophobic victimization and its association with recent unstable housing. While adjusting for covariates and repeated measurements within the individual participant, a 1-unit increase in the past homophobic victimization score was significantly associated with a 70% increase (95% CI [1.35, 2.14], p = .001) in the number of weeks unstably housed. The lagged multilevel ordered logistic model of recent methamphetamine on past homophobic victimization is also displayed on Table 2. While adjusting for covariates and repeated measurements within the individual participant, a 1-unit increase in the past homophobic victimization score was significantly associated with 1.40 times the odds (95% CI [1.15, 1.71], p = .001) of greater levels of recent methamphetamine use. Note that HIV status was retained in the final model as a control variable rather than a moderator, as there was no significant interaction by HIV status in initial modeling.
Table 2.
Lagged multilevel ordered logistic models of recent unstable housing and methamphetamine use on past homophobic victimization (Nvisits = 1,342, n = 401)
| Unstable housing | Methamphetamine use | |||||
|---|---|---|---|---|---|---|
| IRRa | 95% CI | p | ORb | 95% CI | p | |
| Within-person | ||||||
| Homophobic victimization | 1.70 | 1.35 – 2.14 | < .001 | 1.40 | 1.15 – 1.71 | .001 |
| HIV status | ||||||
| Negative | 1.00 | 1.00 | ||||
| Positive | 0.49 | 0.29 – 1.23 | .128 | 7.02 | 2.88 – 17.13 | < .001 |
| Age at study entry | 1.02 | 0.96 – 1.09 | .540 | 1.06 | 0.99 – 1.12 | .082 |
| Race | ||||||
| White | 1.00 | 1.00 | ||||
| Black | 0.43 | 0.09 – 1.94 | .272 | 0.50 | 0.12 – 2.03 | .331 |
| Latino | 0.27 | 0.06 – 1.24 | .093 | 0.80 | 0.20 – 3.26 | .759 |
| Other | 0.54 | 0.07 – 3.97 | .543 | 0.18 | 0.02 – 1.30 | .088 |
| Education | ||||||
| Less than high school | 1.00 | 1.00 | ||||
| High school | 0.52 | 0.17 – 1.55 | .239 | 1.22 | 0.48 – 3.12 | .674 |
| diploma/GED | 0.61 | 0.18 – 2.08 | .433 | 1.29 | 0.41 – 3.40 | .752 |
| Some college | 0.15 | 0.04 – 0.61 | .009 | 0.45 | 0.13 – 1.65 | .231 |
| College degree or more | ||||||
| Employment | ||||||
| Unemployed | 1.00 | 1.00 | ||||
| Part-time | 0.79 | 0.29 – 2.13 | .643 | 0.35 | 0.16–0.78 | .010 |
| Full-time | 0.30 | 0.11 – 0.82 | .019 | 0.08 | 0.03–0.20 | < .001 |
| Student | 0.61 | 0.13 – 2.86 | .532 | 0.17 | 0.04–0.77 | .022 |
| History of incarceration | ||||||
| No | 1.00 | 1.00 | ||||
| Yes | 1.95 | 0.88 – 4.33 | .100 | 3.92 | 1.99 – 7.73 | < .001 |
| Time elapsed (days) | 0.99 | 0.99 – 1.00 | .015 | 1.00 | 1.00 – 1.00 | .621 |
| Between-person | ||||||
| Variance component | 8.81 | 6.02 – 12.89 | 9.22 | 5.55 – 15.33 | ||
Estimates are incidence rate ratios from random intercept negative binomial regression
Estimates are odds ratios from random intercept ordered logistic regression
3.4. Mediation model of homophobic victimization, unstable housing, and methamphetamine use
Figure 1 displays the estimates for direct paths between past homophobic victimization, recent unstable housing, and recent methamphetamine use from multilevel path analysis, adjusting for covariates and repeated measurements within the individual participant. The direct effects of past homophobic victimization on recent methamphetamine use was OR = 1.34 (95% CI [1.10, 1.62]) and significant (p = .003) while adjusting for mediation by unstable housing. The indirect effects of past homophobic victimization on recent methamphetamine use— mediated by unstable housing—was also OR = 1.06 (95% CI [1.01, 1.11], p = .010) and accounted for approximately 17% of its total effect OR = 1.42 (95% CI [1.17, 1.72], p < .001).
4. Discussion
In this analysis of predominantly men of color who have sex with men (MoCSM) in Los Angeles County, homophobic victimization was associated with greater levels of unstable housing and methamphetamine. Greater levels of unstable housing in those who experienced homophobic victimization in the past partially explained the association between homophobic victimization and methamphetamine use. In addition to this indirect association, past homophobic victimization was directly associated with recent methamphetamine use.
Our findings are consistent with prior research indicating that homophobic victimization is associated with both unstable housing (Choi et al., 2015; Durso and Gates, 2012) and substance use problems (Goldbach et al., 2015; Hughes et al., 2010; Paul et al., 2014; Slater et al., 2017) in MSM and other sexual minorities. Prior research linking homophobic victimization with substance use problems are predominantly cross-sectional (Goldbach et al., 2015; Hughes et al., 2010; Paul et al., 2014) Our study expands upon extant literature by utilizing longitudinal data and addressing temporal order between past homophobic victimization and recent methamphetamine use – via lagged-models. Furthermore, the present study is among the first to quantify the degree to which unstable housing partially mediates (~12%) this association. This suggests that unstable housing may be one reason that MSM who experience homophobic victimization are at greater risk of methamphetamine use. This finding corresponds with national data indicating that LGBTQ persons are disproportionately at risk of unstable housing compared to the general population, and majority of unstably housed LGBTQ persons attribute their lack of housing to being forced out of their prior homes due to homophobia (Choi et al., 2015; Durso and Gates, 2012). In turn, methamphetamine is commonly used in the context of unstable housing as a means of survival or emotional coping (Barman-Adhikari et al., 2016; Bungay et al., 2006; Johnson and Chamberlain, 2008; Nyamathi et al., 2008; Yoshioka-Maxwell et al., 2015).
Even after accounting for this mediated pathway and adjusting for sociodemographic variables and HIV status, our analysis showed a direct association between past homophobic victimization and methamphetamine use. This may be explained by the Minority Stress Model, which indicates that exposure to minority stressors such as discrimination, harassment, or violence can directly harm the mental health of minority individuals (Meyer, 2003). Therefore, it is plausible that mental health problems arising from homophobic victimization can take the form of methamphetamine or other substance use (Goldbach et al., 2015; Hughes et al., 2010; McCabe et al., 2010; Roy and Perry, 2009). Qualitative research has elucidated that methamphetamine and other social drugs are used in the context of loneliness, isolation, and fear that comes with being a sexual minority (Aguilar and Sen, 2013; Reback, 1997). Therefore, the fundamental motivation for methamphetamine use in MSM may not be recreation, but the drive to escape from stress, sexual stigma, and oppression and poor self-esteem (Reback, 1997; Roy and Perry, 2009; Semple et al., 2002).
In all multilevel models, HIV status did not significantly moderate associations between past homophobic victimization, recent unstable housing, and recent methamphetamine use, but it was a significant covariate. It is unclear whether this association due to the involvement of methamphetamine use in HIV infection prior to study entry (Plankey, 2007), or due to motivations to cope with HIV through methamphetamine use (Argento et al., 2017; Carrico et al., 2010; Chartier et al., 2009; Durvasula and Miller, 2014).
Our findings highlight the syndemic nature of these minority stress conditions and suggest the need to approach to prevention and treatment at multiple levels. Substance abuse intervention research has found contingency management (CM) to be efficacious in reducing methamphetamine use in MSM, especially those who are homeless or resource-deprived, as such incentives can also benefit basic survival needs such as food and shelter (Bourne and Weatherburn, 2017; Carrico et al., 2016; Reback et al., 2010; Shoptaw et al., 2017). In light of the current findings, CM approaches that incorporate psychosocial sessions that help MoCSM copy with homophobic victimization, provide linkages to community and economic resources tailored for MoCSM can have greater impact on reducing these adverse syndemic factors.
The complication of psychosocial harm from homophobic stigma on substance use disorders may require treatment therapies that address these burdens (Bourne and Weatherburn, 2017; Garcia et al., 2015) while adhering to LGBTQ-affirming national guidelines for substance abuse treatment (American Psychological Association, 2009; SAMHSA, 2012). Alongside these intervention approaches, there remains the need to prevent and protect against homophobia, which underlies these health problems in MSM. Structural factors such as oppressive social norms and lack of institutional support for sexual minorities can create unsafe and unsupportive social environments for sexual minorities, and in turn, perpetuate for cycles of minority stress syndemics at the individual level (Hatzenbuehler, 2014). Therefore, current research on preventing homophobic victimization have taken social ecological approaches to promote respect for diversity and support from authority figures, though these efforts have largely been limited to school settings (Espelage, 2014; Espelage et al., 2018). In order to specifically address homophobia-driven driven homelessness in students, Tierney and Ward (2017) suggest training school district homeless liaisons—assigned per the McKinney-Vento Homeless Education Assistance Improvement Act of 2001—in LGBTQ sensitivity as well as McKinney-Vento protections of relevant need to this population.
Our analysis has some limitations that warrant mention. Methamphetamine use in this analysis was assessed via self-report and not with biological verification of use. However, self-report of methamphetamine use was assessed using CASI—an approach previously shown to improve reporting of sensitive behaviors (Gribble et al., 2000). The recall period for homophobic victimization includes the past 12 months, whereas, unstable housing and methamphetamine use were assessed in the past six months, and as such, the temporal ordering of these variables cannot be confirmed. Although, we attempted to address these issues by lagging the homophobic victimization variable by one time-point, we cannot say definitively, that homophobic victimization at a specific time point influenced unstable housing at a subsequent time point and thus precluding causal interpretations of our findings. There may be other potential meditators of the relationship between homophobic victimization and methamphetamine use, and confounding factors not addressed in our analysis. Nevertheless, our study has many strengths, including our use of data from MoCSM—a sociodemographic group predominantly affected by HIV and substance use. Further, our use of longitudinal data addressed many of the issues of cross-sectional data, which prior studies have mostly relied on.
In sum, our analysis of predominantly MoCSM in LAC indicate an independent, negative impact of past homophobic victimization and an indirect effect via unstable housing on methamphetamine use. Together, our findings emphasize the need to address factors of minority stress holistically, in particular, dissuading or protecting against homophobic victimization and enhancing socioeconomic resources for MoCSM experiencing victimization alongside prevention and treatment of methamphetamine use.
Highlights.
Homophobic victimization (HV) was associated with greater severity of methamphetamine use across 24 months.
HV was associated with greater duration of unstable housing across 24 months.
Unstable housing partially explained the association between HV and methamphetamine use.
Acknowledgements
This research was supported by the MSM and Substances Cohort at UCLA Linking Infections Noting Effects (MASCULINE) (National Institute on Drug Abuse, #5U01DA036267, PI: Gorbach, Shoptaw), the Center for HIV Identification Prevention and Treatment Services (CHIPTS) (National Institute of Mental Health, #P30MH058107, PI: Shoptaw), and the UCLA Postdoctoral Fellowship Training Program in Global HIV Prevention Research grant T32MH080634 (PI: Currier, Gorbach).
Role of the Funding Source No role declared.
Footnotes
Conflict of Interest
No conflict declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aguilar JP, Sen S, 2013. The culture of methamphetamine: Reframing gay men’s methamphetamine use. J. Hum. Behav. Soc. Environ 23, 370–382. [Google Scholar]
- American Psychological Association, 2009. Report of the Task Force on Appropriate Therapeutic Responses to Sexual Orientation. American Psychological Association, Washington, D.C. [Google Scholar]
- Argento E, Strathdee SA, Goldenberg S, Braschel M, Montaner J, Shannon K, 2017. Violence, trauma and living with HIV: Longitudinal predictors of initiating crystal methamphetamine injection among sex workers. Drug Alcohol Depend. 175, 198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barman-Adhikari A, Begun S, Rice E, Yoshioka-Maxwell A, Perez-Portillo A, 2016. Sociometric network structure and its association with methamphetamine use norms among homeless youth. Soc. Sci. Res 58, 292–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhargava A, Sargan JD, 1983. Estimating dynamic random effects models from panel data covering short time periods. Econometrica 51, 1635–1659. [Google Scholar]
- Bostwick WB, Meyer I, Aranda F, Russell S, Hughes T, Birkett M, Mustanski B, 2014. Mental health and suicidality among racially/ethnically diverse sexual minority youths. Am. J. Public Health 104, 1129–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourne A, Weatherburn P, 2017. Substance use among men who have sex with men: Patterns, motivations, impacts and intervention development need. Sex. Trans. Inf 93, 342. [DOI] [PubMed] [Google Scholar]
- Bungay V, Malchy L, Buxton JA, Johnson J, MacPherson D, Rosenfeld T, 2006. Life with jib: A snapshot of street youth’s use of crystal methamphetamine. Addict. Res. Theory 14(3), 235–251. [Google Scholar]
- Buttram ME, Kurtz SP, 2015. A mixed methods study of health and social disparities among substance-using African American/Black men who have sex with men. J. Racial Ethn. Health Disparities 2, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrico AW, Jain J, Discepola MV, Olem D, Andrews R, Woods WJ, Neilands TB, Shoptaw S, Gómez W, Dilworth SE, Moskowitz JT, 2016. A community-engaged randomized controlled trial of an integrative intervention with HIV-positive, methamphetamine-using men who have sex with men. BMC Public Health 16, 673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrico AW, Johnson MO, Colfax GN, Moskowitz JT, 2010. Affective correlates of stimulant use and adherence to anti-retroviral therapy among HIV-positive methamphetamine users. AIDS Behav. 14, 769–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chartier M, Araneta A, Duca L, McGlynn LM, Gore-Felton C, Goldblum P, Koopman C, 2009. Personal values and meaning in the use of methamphetamine among HIV-positive men who have sex with men. Qual. Health Res 19, 504–518. [DOI] [PubMed] [Google Scholar]
- Choi SK, Wilson BDM, Shelton J, Gates GJ, 2015. Serving our youth 2015: The needs and experiences of lesbian, gay, bisexual, transgender, and questioning youth experiencing homelessness. The Williams Institute with True Colors Fund and The Palette Fund, Los Angeles, CA. [Google Scholar]
- County of Los Angeles Public Health, 2016. Methamphetamine Misuse/Abuse and Consequences, Substance Abuse Prevention and Control, Medical Director’s Brief. [Google Scholar]
- Cruickshank Christopher C, Dyer Kyle R, 2009. A review of the clinical pharmacology of methamphetamine. Addiction 104, 1085–1099. [DOI] [PubMed] [Google Scholar]
- Darke S, Duflou J, Kaye S, 2017. Prevalence and nature of cardiovascular disease in methamphetamine-related death: A national study. Drug Alcohol Depend. 179, 174–179. [DOI] [PubMed] [Google Scholar]
- Durso LE, Gates GJ, 2012. Serving our youth: Findings from a national survey of services providers working with the lesbian, gay, bisexual, and transgender youth who are homeless or at risk of becoming homeless. The Williams Institute with True Colors Fund and The Palette Fund, Los Angeles, CA. [Google Scholar]
- Durvasula R, Miller TR, 2014. Substance abuse treatment in persons with HIV/AIDS: Challenges in managing triple diagnosis. Behav. Med 40, 43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyer TP, Shoptaw S, Guadamuz TE, Plankey M, Kao U, Ostrow D, Chmiel JS, Herrick A, Stall R, 2012. Application of syndemic theory to black men who have sex with men in the Multicenter AIDS Cohort Study. J. Urban Health 89, 697–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espelage DL, 2014. Ecological theory: preventing youth bullying, aggression, and victimization. Theory Pract. 53, 257–264. [Google Scholar]
- Espelage DL, Valido A, Hatchel T, Ingram KM, Huang Y, Torgal C, 2018. A literature review of protective factors associated with homophobic bullying and its consequences among children and adolescents. Aggr. Violent Behav In Press. [Google Scholar]
- Fertig Angela R., Reingold David A., 2008. Homelessness among at‐risk families with children in twenty american cities. Soc. Serv. Rev 82, 485–510. [Google Scholar]
- Fredriksen-Goldsen KI, Kim H-J, 2017. The science of conducting research with LGBT older adults- an introduction to aging with pride: National Health, Aging, and Sexuality/Gender Study (NHAS). Gerontol. 57(Suppl. 1), S1–S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman MR, Stall R, Silvestre AJ, Wei C, Shoptaw S, Herrick A, Surkan PJ, Teplin L, Plankey MW, 2015. Effects of syndemics on HIV viral load and medication adherence in the multicentre AIDS cohort study. AIDS 29, 1087–1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia J, Parker C, Parker RG, Wilson PA, Philbin M, Hirsch JS, 2015. Psychosocial implications of homophobia and hiv stigma in social support networks: Insights for highimpact HIV prevention among black men who have sex with men. Health Educ. Behav 43, 217–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldbach J, Fisher BW, Dunlap S, 2015. Traumatic experiences and drug use by LGB adolescents: A critical review of minority stress. J. Soc. Work Pract. Addict 15, 90–113. [Google Scholar]
- Gribble JN, Miller HG, Cooley PC, Catania JA, Pollack L, Turner CF, 2000. The impact of T-ACASI interviewing on reported drug use among men who have sex with men. Subst. Use Misuse 35, 869–890. [DOI] [PubMed] [Google Scholar]
- Hassan SF, Wearne TA, Cornish JL, Goodchild AK, 2016. Effects of acute and chronic systemic methamphetamine on respiratory, cardiovascular and metabolic function, and cardiorespiratory reflexes. J. Physiol 594, 763–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, 2014. Structural stigma and the health of lesbian, gay, and bisexual populations. Curr. Dir. Psychol. Sci 23, 127–132. [Google Scholar]
- Herrick AL, Lim SH, Plankey MW, Chmiel JS, Guadamuz TT, Kao U, Shoptaw S, Carrico A, Ostrow D, Stall R, 2012. Adversity and syndemic production among men participating in the Multicenter AIDS Cohort Study: A life-course approach. Am. J. Public Health 103, e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes T, McCabe SE, Wilsnack SC, West BT, Boyd CJ, 2010. Victimization and substance use disorders in a national sample of heterosexual and sexual minority women and men. Addiction 105, 2130–2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson G, Chamberlain C, 2008. Homelessness and substance abuse: Which comes first? Aust. Social Work 61, 342–356. [Google Scholar]
- Jones RN, 2015. RUNMPLUS: Stata module to run Mplus from Stata. Latent Variable Methods Workshop, Brown University, Providence, RI. [Google Scholar]
- Kaye S, McKetin R, Duflou J, Darke S, 2007. Methamphetamine and cardiovascular pathology: A review of the evidence. Addiction 102, 1204–1211. [DOI] [PubMed] [Google Scholar]
- MacKinnon D, 2012. Introduction to Statistical Mediation Analysis Taylor and Francis, New York, NY. [Google Scholar]
- McCabe SE, Bostwick WB, Hughes TL, West BT, Boyd CJ, 2010. The relationship between discrimination and substance use disorders among lesbian, gay, and bisexual adults in the United States. Am. J. Public Health 100, 1946–1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConnell EA, Janulis P, Phillips G II, Truong R, Birkett M, 2018. Multiple minority stress and LGBT community resilience among sexual minority men. Psychol. Sex. Orient. Gender Div 5, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McVicar D, Moschion J, van Ours JC, 2015. From substance use to homelessness or vice versa? Soc. Sci. Med 136–137, 89–98. [DOI] [PubMed] [Google Scholar]
- Mereish EH, Bradford JB, 2014. Intersecting identities and substance use problems: Sexual orientation, gender, race, and lifetime substance use problems. J. Stud. Alcohol Drugs 75, 179–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, 2003. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychol. Bull 129, 674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén BO, 2011. Applications of causally defined direct and indirect effects in mediation analysis using SEM in Mplus. Muthén and Muthén, Los Angeles, CA. [Google Scholar]
- Muthén LK, Muthén BO, 2010. Mplus: Statistical analysis with latent variables, 6 ed. Muthén and Muthén, Los Angeles, CA. [Google Scholar]
- Nyamathi A, Dixon EL, Shoptaw S, Marfisee M, Gelberg L, Williams S, Dominick S, Leake B, 2008. Profile of lifetime methamphetamine use among homeless adults in Los Angeles. Drug Alcohol Depend. 92, 277–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul JP, Boylan R, Gregorich S, Ayala G, Choi K-H, 2014. Substance use and experienced stigmatization among ethnic minority men who have sex with men in the United States. J. Ethn. Subst. Abuse 13, 430–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plankey MW, Ostrow DG, Stall R, Cox C, Li X, Peck JA, Jacobson LP, 2007. The relationship between methamphetamine and popper use and risk of HIV seroconversion in the multicenter AIDS cohort study. J. Acquir. Immune Defic. Syndr 45, 85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabe-Hesketh S, Skrondal A, 2008. Multilevel and longitudinal modeling using Stata. STATA press. [Google Scholar]
- Reback CJ, 1997. The social construction of a gay drug: Methamphetamine use among gay and bisexual males in Los Angeles: Report for the City of Los Angeles, in: City of Los Angeles, A.C. (Ed.). Los Angeles, CA.
- Reback CJ, Fletcher JB, Shoptaw S, Grella CE, 2013. Methamphetamine and other substance use trends among street-recruited men who have sex with men, from 2008 to 2011. Drug Alcohol Depend. 133, 262–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reback CJ, Peck JA, Dierst-Davies R, Nuno M, Kamien JB, Amass L, 2010. Contingency management among homeless, out-of-treatment men who have sex with men. J. Subst. Abuse Treat 39, 255–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reback CJ, Shoptaw S, Grella CE, 2008. Methamphetamine use trends among streetrecruited gay and bisexual males, from 1999 to 2007. J. Urban Health 85, 874–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy CJ, Perry NH, 2009. Stigmatization, stress, and the search for belonging in black men who have sex with men who use methamphetamine. J. Black Psychol 35, 343–365. [Google Scholar]
- Semple SJ, Patterson TL, Grant I, 2002. Motivations associated with methamphetamine use among HIV men who have sex with men. J. Subst. Abuse Treat 22, 149–156. [DOI] [PubMed] [Google Scholar]
- Shoptaw S, Landovitz RJ, Reback CJ, 2017. Contingent vs. non-contingent rewards: Time-Based Intervention response patterns among stimulant-using men who have sex with men. J. Subst. Abuse Treat 72, 19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slater ME, Godette D, Huang B, Ruan WJ, Kerridge BT, 2017. Sexual orientation-based discrimination, excessive alcohol use, and substance use disorders among sexual minority adults. LGBT Health 4, 337–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stall R, Friedman M, Catania JA, 2008. Intersecting epidemics and gay men’s health: A theory of syndemic production among urban gay men, in: Wolitski Richard J., R.S., Valdeserri Ronald O. (Ed.) Unequal Opportunity: Health Disparities Affecting Gay and Bisexual Men in the United States. Oxford, New York: NY, pp. 251–274. [Google Scholar]
- StataCorp, 2017. Stata, 15 ed. StataCorp LLC, College Station, TX. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA), 2012. A Provider’s Introduction to Substance Abuse Treatment for Lesbian, Gay, Bisexual, and Transgender Individuals. U.S. Department for Health and Human Services, Rockville, MD. [Google Scholar]
- Tierney WG, Ward JD, 2017. Coming out and leaving home: A policy and research agenda for LGBT homeless students. Educ. Res 46, 498–507. [Google Scholar]
- Wilton L, 2008. Correlates of substance use in relation to sexual behavior in black gay and bisexual men: Implications for HIV prevention. J. Black Psychol 34, 70–93. [Google Scholar]
- World Health; Organization (WHO), 2010. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Manual for use in primary care in: Humeniuk R, Henry-Edwards S, Ali R, Poznyak V, Monteiro MG (Eds.). World Health Organization, Geneva, Switzerland. [Google Scholar]
- Yoshioka-Maxwell A, Rice E, Rhoades H, Winetrobe H, 2015. Methamphetamine use among homeless former foster youth: The mediating role of social networks. J. Alcohol. Drug Depend 3, 197. [DOI] [PMC free article] [PubMed] [Google Scholar]