Abstract
Venous thromboembolism (VTE) is a major healthcare problem that results in significant mortality, morbidity, and expenditure of resources. It compounds with pulmonary embolism (PE) and deep vein thrombosis (DVT). Phlegmasia cerulea dolens (PCD) is an uncommon but potentially life-threatening complication of acute DVT characterized by marked swelling of the extremities with pain and cyanosis, which in turn may lead to arterial ischemia and ultimately gangrene with high amputation and mortality rates. The key in treating such patients is to provide quick and effective treatment to save the limbs and the patient.
Keywords: phlegmasia cerulea dolens, compartment syndrome, acute deep vein thrombosis
Introduction
The complications of acute venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE), are the most common preventable causes of hospital death and a source of substantial long-term morbidity.1)
Phlegmasia cerulea dolens (PCD) is an uncommon but potentially life-threatening complication of acute DVT characterized by marked swelling of the extremities with pain and cyanosis, which in turn may lead to arterial ischemia and ultimately cause gangrene with high amputation and mortality rates. There is no consensus on its treatment, and the reported treatment methods are usually suboptimal.2) The key in treating such patients is to provide quick and effective treatment to save the limbs and the patient. Treatments of PCD have many modalities, which include conservative management and intervention or surgery. These have both risks and benefits.3) Here, we present a patient who developed the severe form of lower extremity DVT (i.e., PCD) that resulted in compartment syndrome.
Case Report
A 74-year-old man presented to the emergency department after a motorcycle accident. He had a deformity in the right leg. His comorbidities were chronic obstructive pulmonary disease, ischemic cardiomyopathy due to myocardial infarction, atrial fibrillation, hypertension, and dyslipidemia. His medications included aspirin and clopidogrel. Following investigations in this admission, a brain computed tomography (CT) revealed that he had acute traumatic subdural hematoma that was managed with nonoperative treatment. His right leg was broken, which was diagnosed as a closed fracture of the tibia and fibula, and was managed conservatively. He had fractures at the left iliac crest and the left superior pubic rami. The neurovascular conditions were normal. During admission, he had acute dyspnea with desaturation but no chest pain at ten days after admission. On examination, his blood pressure was 102/78 mmHg, pulse rate was 100/min, respiratory rate was 24/min, and blood oxygen saturation (SpO2) was 90% in room air, which was not corrected with oxygen supplement. He had crepitation at his left lower lung but no wheezing. CT angiography of the chest was performed and showed acute PEs at the right superior and inferior trunk. He was found to have acute respiratory failure and hypotension after the chest CT angiography was finished. He was scheduled for an emergency operation for surgical pulmonary embolectomy.
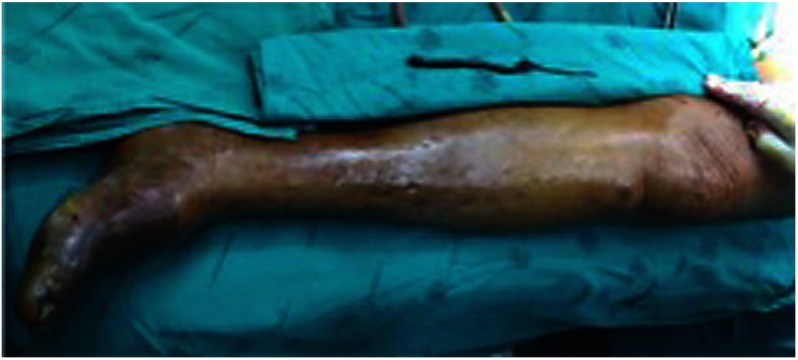
On the next day at the surgical intensive care unit (ICU), he developed progressive left leg edema with cyanosis. He had no fever and he could still move his leg, but his pain could not be evaluated since he was delirious. On examination, his left lower limb exhibited discoloration at his left foot without any ulcer or bleb, moist skin, or pitting edema, and the left dorsalis pedis and posterior tibial pulse could be palpated (1+) but were diminished (Fig. 1). The motor functions remained intact. Doppler ultrasonography was performed and revealed an uncompressible vein along the midsuperior femoral vein to the popliteal vein. His laboratory investigation showed that the leukocytosis and creatinine level rose from 1.04 mg% to 1.62 mg% and creatinine phosphokinase (CPK) was 322 U/L. He was diagnosed with PCD at the left femoral vein. The intervention radiologist attempted a catheter-directed thrombectomy, but it failed because the guider could not pass through the intraluminal clot. The patient was scheduled for emergency operation again for surgical thrombectomy with fasciotomy of the left leg (Fig. 2). The operative finding was a thrombus in the femoral vein that was 10 cm in length (Fig. 3). The compartment pressures before performing the fasciotomy at the anterior, lateral, and superficial posterior compartments were 43 mmHg, 37 mmHg, and 47 mmHg, respectively. The deep posterior compartment pressure was not measured. After the operation, his pain was relieved and the left dorsalis pedis and posterior tibial pulse were normal. He continued on wound dressings and the fasciotomy was closed by split-thickness skin graft. He continued on oral anticoagulant drugs for six months and underwent elective ray amputation at five months after the PCD for a dry gangrenous left big toe.
Fig. 1 Left foot of the patient diagnosed with phlegmasia cerulea dolens.
Fig. 2 Venous clot in the femoral vein.
Fig. 3 Venous clot, 10 cm in length.
Discussion
VTE is a major healthcare problem that results in significant mortality, morbidity, and expenditure of resources. Approximately 1% of hospital admissions in the United States are for VTE. The incidence of VTE is approximately 100 per 100,000 people per year in the general population. Of the symptomatic patients, one-third present with PE and two-thirds with DVT.4) The risk factor of DVT is compounded by many factors. Traumatic hospitalization was associated with acute DVT (odds ratio [OR]=12.69). In addition, age (OR=1.05 for each one-year increment), blood transfusion (OR=1.74), surgery (OR=2.30), and fracture of the femur or tibia (OR=4.82) were significantly associated with the development of DVT in this population.5) Other reported risk factors were a hospital stay longer than seven days, increased Injury Severity Score, pelvic fractures, and duration of immobilization.5) Since this patient was 74 years old with pelvic fractures and was immobilized in the hospital for ten days, he was at risk for VTE.
Extensive DVT of the major axial deep venous channels of the lower extremity with relative sparing of collateral veins causes a condition called PCD. Phlegmasia (phlegma) means inflammation. The first description was given by Gregoire in 1938.5) It is a rare life-threatening complication of acute proximal DVT. It can lead to impairment of the arterial circulation, which results in tissue ischemia or limb gangrene. The major amputation rate is 20–50% and the death rate is 25–40%.6) PCD extends the thrombosis to collateral veins, resulting in severe venous congestion with massive fluid sequestration and more significant edema.7) If gangrene is not established, it is reversible. But 40–60% of PCD cases can have capillary involvement resulting in irreversible venous gangrene, which can occur in two days after the onset of symptoms of ischemia.2) The symptoms of PCD are compounded with severe pain, edema, and pathognomonic cyanosis (blue or cerulea).7) When the thrombosis extends to the collateral veins, massive fluid sequestration and a greater amount of edema ensue, which results in the condition known as phlegmasia alba dolens (PAD).2) The affected extremity in PAD is extremely painful and is edematous and pale secondary to arterial insufficiency from dramatically elevated compartment pressures below the knee. Both PCD and PAD can be complicated by venous gangrene and the need for amputation. The differential diagnosis includes venous gangrene, lymphatic obstruction, acute cellulitis, PAD, and acute arterial occlusion. Diagnosis of PCD can be made clinically.7) Doppler ultrasound can identify occlusion in both the arteries and the veins of the lower extremities, which is a good first choice for imaging. The main sonographic finding is the presence of extensive thrombus in the deep and superficial venous system of the affected lower extremity. In compression sonography, the inability to compress the vein lumen entirely is pathognomonic for a thrombus in the vein.7) Usually, sonography is the only imaging modality required, with no need for magnetic resonance venography or arteriography.7) Catheter venography and arteriography remain the gold standard and can be therapeutic.6)
The goals of treatment in PCD are thrombus removal to improve venous patency, valve function, and decrease risk of recurrence and postthrombotic syndrome. The treatment in PCD has many modalities that include conservative treatment, systemic or local thrombolysis, pharmacomechanical thrombolysis (PMT), and surgical thrombectomy.6) PMT is the best treatment in PCD from the two cohort studies.6) A study by Vedantham8) on 28 patients with acute DVT revealed that PMT had a clot removal rate of 82% compared with 26% in thrombectomy alone. Another study9) of catheter-directed thrombolysis versus PMT for the treatment of acute DVT in 93 patients revealed that the PMT group had lower rates of ICU stay, length of stay, and packed red cells transfusion than the catheter-directed thrombolysis group. However, PMT has the disadvantage of major bleeding, microemboli, or bleeding at intervention sites. Our patient who had intracranial bleeding was probably not suitable for thrombolysis combined with thrombectomy, although it is the treatment of choice at present. The last option is surgical thrombectomy in patients who are not candidates for thrombolysis, but it is less effective than thrombolysis since it cannot address clots in small veins involved in the progression to venous gangrene. Nevertheless, the ten-year patency rate after surgical thrombectomy is as high as 80% with the valvular competence.
Fasciotomies to treat compartment syndrome secondary to PCD or PAD are rarely reported. To our knowledge, there are reports on only 15 patients.10) There is a markedly increased intramuscular pressure (>30 mmHg) in iliofemoral thrombosis with PCD that causes compartment syndrome. In these cases, intramuscular pressure measurements are suggested to evaluate the need for fasciotomy, which may help decrease the amputation rate. Our patient had high compartment pressures and underwent fasciotomy. Even though we saved his limb, he later had a minor amputation.
Conclusion
In conclusion, PCD with compartment syndrome is a rare condition. Timely restoration of the venous circulation is important in order to save the limbs. Besides revascularization, compartment syndrome is a concomitant condition that requires vigilance.
Disclosure Statement
All authors have no conflict of interest.
Author Contributions
Study conception: all aurhors
Writing: WC
Critical review and revision: all authors
Final approval of the article: all authors
Accountability for all aspects of the work: all authors
References
- 1).Hull RD, Raskob GE, Hirsh J. Prophylaxis of venous thromboembolism. An overview. Chest 1986; 89 Suppl: 374S-83S. [PubMed] [Google Scholar]
- 2).Brockman SK, Vasko JS. Phlegmasia cerulean dolens. Surg Gynecol Obstet 1965; 121: 1347-56. [PubMed] [Google Scholar]
- 3).Oguzkurt L, Tercan F, Ozkan U. Manual aspiration thrombectomy with stent placement: rapid and effective treatment for phlegmasia cerulea dolens with impending venous gangrene. Cardiovasc Intervent Radiol 2008; 31: 205-8. [DOI] [PubMed] [Google Scholar]
- 4).Spyropoulos AC, Hussein M, Lin J, et al. Rates of symptomatic venous thromboembolism in US surgical patients: a retrospective administrative database study. J Thromb Thrombolysis 2009; 28: 458. [DOI] [PubMed] [Google Scholar]
- 5).Knepper JP, Wakefield TW. Acute deep venous thrombosis: pathophysiology and natural history. In: Cronenwett JL, Johnston KW eds. Rutherford’s Vascular Surgery 1, 8th ed. Philadelphia: Elsevier, 2014: 745-9.
- 6).Chinsakchai K, ten Duis K, Moll FL, et al. Trends in management of phlegmasia cerulea dolens. Vasc Endovascular Surg 2011; 45: 5-14. [DOI] [PubMed] [Google Scholar]
- 7).Bazan HA, Reiner E, Sumpio B. Management of bilateral phlegmasia cerulea dolens in a patient with subacute splenic laceration. Ann Vasc Dis 2008; 1: 45-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).Vedantham S, Vesely TM, Parti N, et al. Lower extremity venous thrombolysis with adjunctive mechanical thrombectomy. J Vasc Interv Radiol 2002; 13: 1001-8. [DOI] [PubMed] [Google Scholar]
- 9).Lin PH, Zhou W, Dardik A, et al. Catheter-direct thrombolysis versus pharmacomechanical thrombectomy for treatment of symptomatic lower extremity deep venous thrombosis. Am J Surg 2006; 192: 782-8. [DOI] [PubMed] [Google Scholar]
- 10).Mesfin A, Lum YW, Nayfeh T, et al. Compartment syndrome in patients with massive venous thrombosis after inferior vena cava filter placement. Orthopedics 2011; 34: 229. [DOI] [PubMed] [Google Scholar]