Abstract
Objectives:
To summarize available peer-reviewed publications about public knowledge and awareness of diabetes mellitus (DM) among the population of Saudi Arabia.
Methods:
We followed the standard reporting guidelines outlined in the PRISMA statement for the preparation of this systematic review. In February 2018 we conducted literature searches of PubMed, Scopus, BIOSIS Citation Index, and Web of Science using the following keywords: “Knowledge” OR “Awareness” AND “Diabetes Mellitus” AND “Saudi Arabia.” Records were screened, and relevant studies were selected and synthesized narratively.
Results:
Nineteen articles are included in our systematic review. These studies included the following populations: DM patients (n=13), healthcare workers (n=3), medical students (n=1), secondary school students (n=1), and general population (n=1). Most studies found a lack of public awareness of the risk factors and complications of DM. Among medical students and healthcare workers, knowledge about the epidemiology of the disease and angle of insulin injection was deficient.
Conclusion:
This review highlights the need for increased knowledge and awareness of DM among the Saudi population. The means of improving knowledge and awareness of DM needs to be integrated into existing healthcare systems and processes to better inform patients, families, and communities about this chronic disease.
PROSPERO REG. NO: CRD: 42018098787
Diabetes mellitus (DM) is a metabolic disorder characterized by a deficit in insulin secretion or action resulting in hyperglycemia. Diabetes mellitus is classified into 3 major types: type 1 (T1DM), type 2 (T2DM) and gestational diabetes. Type 1 DM results from autoimmune destruction of beta cells in the islets of Langerhans, resulting in a decrease in insulin secretion. Type 2 DM results from a decrease in insulin action due to insulin resistance by body tissues, leading to disturbed glucose entry to body cells. Obesity has been found to increase insulin resistance and has therefore been linked to T2DM. This paper will focus on a systematic review of the literature about education and prevention of T1DM and T2DM in Saudi Arabia.
According to the International Diabetes Federation,1 DM affects about 8.8% of the worldwide population over 20 years of age. Middle Eastern and North African (MENA) countries have a higher prevalence of DM compared to other regions in the world; the prevalence rate was 9.6% in 2017, and the rate is expected to increase to 12.1% by 2045.1 The high prevalence of DM in the MENA region is attributed to the urbanization process, high obesity rates and the increase in the aging population in these countries.2 As DM is the most prevalent disease in Saudi Arabia, carrying a substantial economic burden, it is essential that public health interventions consider how to influence behavior in the Saudi population to better prevent and control this disease.
According to the International Diabetes Federation,1 Saudi Arabia has the highest rate of DM in the MENA region (prevalence rate of 17.7%). The prevalence of T1DM in Saudi Arabia was investigated by Al-Herbish et al3 in 2008 using a cross-sectional study of 45,682 children and adolescents. They reported a rate of 109.5 patients per 100,000 people. Saudi Arabia has the fourth highest incidence of T1DM in the world, at about 33.5/100,000 persons per year.1 In 2011, Al-Daghri et al3 performed a cross-sectional study of 9149 citizens reported a 31.6% prevalence rate for T2DM in Saudi Arabia. Alqurashi et al4 performed another cross-sectional study in Saudi Arabia to determine the prevalence rate of T2DM using a convenience sampling method. In this study, they reported a prevalence rate for T2DM of 30% in 2009.4 Approximately 0.78 billion dollars of the total healthcare expenditure of Saudi Arabia was dedicated to managing DM.5 Given that DM is so prevalent in Saudi Arabia, it is important to ensure that the community has sufficient knowledge and awareness of this disease to enable further promotion of public health interventions to control its prevalence. It is also important for DM patients to better understand medication and lifestyle modification that may allow for better management of their glucose levels and delay the onset of DM complications. To help DM patients achieve this goal, patients, families, nurses and healthcare physicians need high levels of knowledge and awareness about DM pathology, risk factors, management, and complications. In this article, the literature is systemically reviewed to better understand what is known about DM among the Saudi population.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and Meta-analyses of Observational Studies in Epidemiology (MOOSE) statement guidelines were followed during the preparation of this systematic review.6,7 All steps were performed in strict accordance with the Cochrane Handbook of Systematic Review and Meta-analysis.8
Literature search strategy
Throughout February 2018, literature searches of PubMed, Scopus, Biosciences Information Service (BIOSIS) and the Institute for Scientific Information (ISI) Web of Science was conducted using the following keywords (knowledge OR awareness) AND diabetes mellitus AND Saudi Arabia. These keywords used were relevant to the topic area and were the most appropriate terms for the review. The search outcomes from the databases were then limited to English language, peer reviewed, and research articles with no time frame limit.
Study selection
Two researchers independently screened the literature search results for relevant studies. They first performed computerized searches on medical databases as described above, producing 401 potential articles. Four hundred and one articles were screened for duplicates resulting in the elimination of 118 articles. The researchers then assessed the titles and abstracts of the remaining 283 articles and determined that 253 of those were not relevant to the present study, leaving 30 potential articles. In the final stage, the researchers carefully reviewed the full text of all articles selected during previous step and remove those not relevant to the topic. Disagreement between researchers about the relevance on an article was resolved through discussion with a third researcher. After this review process, 19 articles were determined to be relevant and were included in the systemic review (Figure 1).
Figure 1.
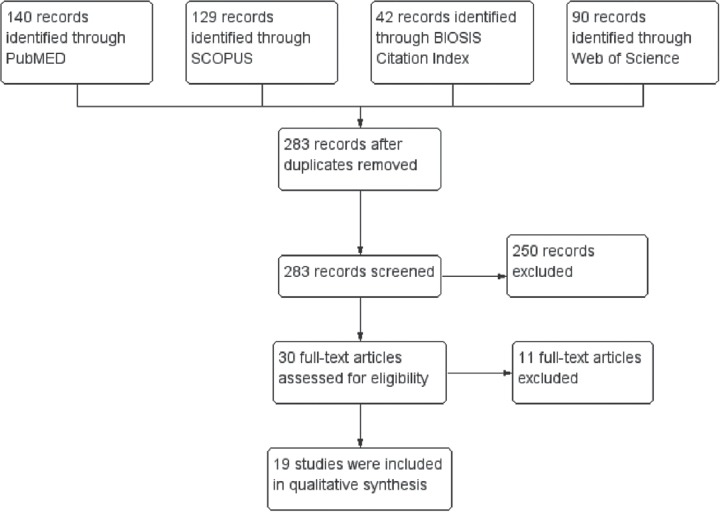
PRISMA flow diagram for the literature search and study selection process.
Eligibility criteria
Studies satisfying the following criteria were chosen for inclusion in this review: 1) studies that were described as cross-sectional studies, 2) studies in which Saudi Arabia was the population of interest and 3) studies evaluating the knowledge and awareness of the population about T1DM, T2DM or both. We excluded articles that were 1) in a country other than Saudi Arabia, 2) academic thesis, and 3) conference abstracts.
Data extraction
Data were extracted independently by the 2 researchers to a uniform data extraction sheet. The extracted data included: 1) characteristics of the study design, 2) features of the study population and 3) data of the study outcomes.
Synthesis of results
Included studies were classified according to the type of the population: 1) studies on the general population, 2) studies on health care professionals and 3) studies on DM patients. Extracted data from each study were tabulated and reviewed narratively.
Results
Characteristics of included studies
The search strategy retrieved 283 unique articles. Following eligibility screening, 19 articles met the inclusion criteria and were included in the systematic review. The population of these studies were as follows: DM patients (n=13), healthcare workers (n=3), medical students (n=1), secondary school students (n=1) and general population (n=1). The flow diagram of the study selection process is shown in Figure 1.
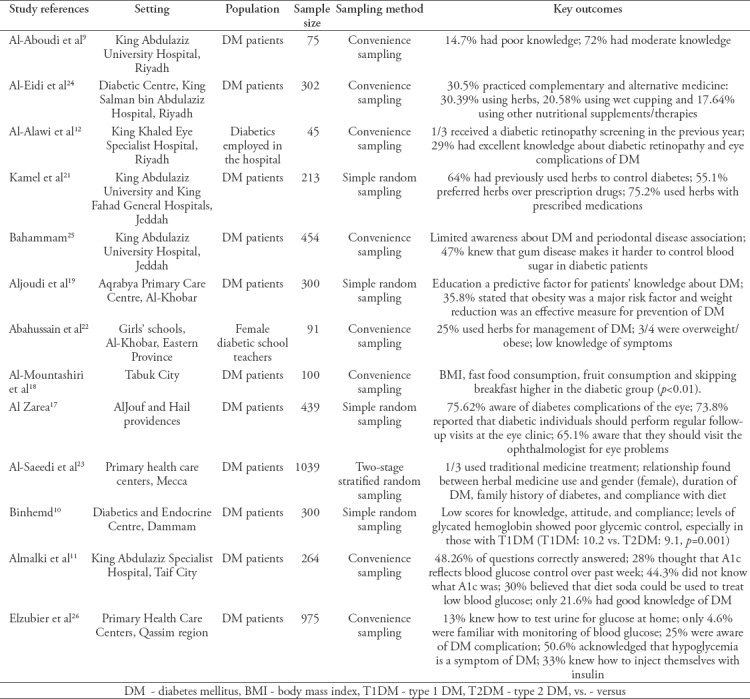
Level of knowledge about DM
Most studies found a poor level of knowledge of the disease among DM patients in Saudi Arabia. Al-Aboudi et al9 found that 15% of DM patients had inadequate knowledge of DM while 72% has moderate knowledge. In a study by Binhemd,10 DM patients in Dammam received low scores regarding knowledge and attitudes towards DM. In another survey of DM patients by Al Malki et al,11 the percentage of correct answers to questions about DM was 49%, highlighting a gap in DM knowledge among the population. A summary of cross-sectional studies about DM knowledge among DM patients in Saudi Arabia is shown in Table 1.
Table 1.
Summary of cross-sectional studies performed in Saudi Arabia about knowledge and awareness of DM among diabetic patients.
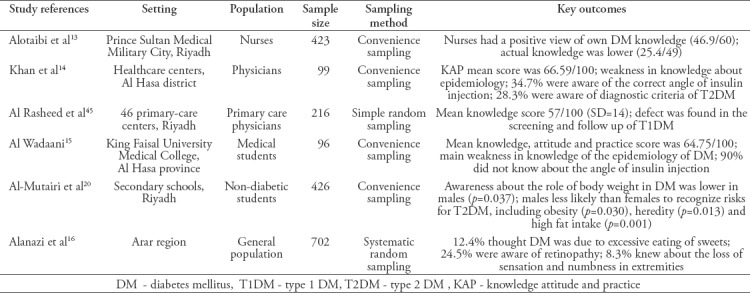
Only one third of healthcare staff with a DM diagnosis participated in retinopathy screening in the study by Al-Alawi et al12 Among health professionals, nurses at Prince Sultan Medical Military City in Riyadh had low knowledge scores about DM (25.5/49), despite having positive views about their level of knowledge (46.9/60), highlighting a gap between their perceived and actual knowledge about DM.13 Unexpectedly, in the Al Hasa district, physicians also had low knowledge scores (66.6/100), with the biggest weakness in physicians’ knowledge being disease epidemiology.14 Only one third of the physicians surveyed were aware of the correct angle at which to administer insulin injections, and only 28.3% of them were aware of the diagnostic criteria for DM.14 Similarly, medical students had low scores regarding knowledge about DM, with the main weakness being epidemiology, and 90% of the students were not aware of the correct angle required for administering insulin injections.15
Citizens of the Arar region had relatively low knowledge about DM,16 with only 12.4% acknowledged excess consumption of sweets and obesity as risk factors.16 A summary of studies focused on the knowledge of health professionals, students, and the general population is shown in Table 2.
Table 2.
Summary of cross-sectional studies performed in Saudi Arabia about knowledge and awareness of DM among healthcare workers, students, and the general population.
Knowledge about complications of DM
Three studies were found that evaluated population knowledge about DM complications.12,16,17 Al Zarea17 performed a cross-sectional study on 439 diabetic patients in the cities of AlJouf and Hail and found that most of the patients (75.62%) were aware of diabetes complications of the eyes. Al-Alawi et al12 conducted a cross-sectional descriptive study on 45 healthcare staff with DM at a tertiary eye hospital in central Saudi Arabia. They found that in the previous year, only one third of the study population received a diabetic retinopathy screening. Of the participants, 29% had excellent knowledge about diabetic retinopathy and eye complications of DM. However, lack of gender-specific health professionals, the distance to the health center and lack of referral from the health care professionals and family were the main barriers towards not receiving a diabetic retinopathy screening on a regular basis. Menwer et al’s16 cross-sectional study to assess knowledge of risk factors of DM among diabetic patients in the Arar region selected 702 participants by using a systematic random sample method. Of those, 12.4% thought that DM was due to excessive eating of sweets. The knowledge about DM complications was relatively low; only 24.5% were aware of retinopathy, while only 8.3% knew about the loss of sensation and numbness in extremities.
Knowledge about risk factors of DM
In the city of Tabuk, Al-Mountashiri et al18 conducted a cross-sectional study on 100 DM patients; they found that high body mass index (BMI), fast food consumption, fruit consumption and skipping breakfast occurred significantly more frequently among DM patients when compared to the non-DM population. Aljoudi and Taha19 performed a cross-sectional study on a sample of 300 patients attending the Aqrabya Primary Care Centre in Saudi Arabia. They randomly selected those patients from the attendees to complete surveys about the knowledge of DM risk factors and preventive measures. This study found that age, gender, and education level were associated with the knowledge of DM risk factors and preventive measures (p<0.001). Education level was found to be a statistically significant predictive factor for patients’ knowledge about DM, and 35.8% of the participants stated that obesity was a significant risk factors for DM and that weight reduction was an effective measure for the prevention of DM. In a cross-sectional study of 426 non-diabetic secondary school students, the authors found higher obesity rates in males than females (p=0.013).20 The male students were also less aware of the risks of T2DM, such as obesity, family history, and high fat intake. The students acknowledged obesity as the most important risk factor, while weight reduction was recognized as the key preventive measure.
Use of herbs and alternative medicine
Beside assessing patients’ knowledge and awareness about DM, 3 studies assessed patients’ use of herbs and alternative medicine products in relation to DM. One study was conducted in Jeddah, where the investigators found that 64% of DM patients had used herbs as a course of treatment for their condition.21 Another study was conducted in Al-Khobar, where 25% of diabetic female teachers reported using herbs and about one third were obese.22 A study carried out in Mecca found that about one third of DM patients used herbal medicine.23 These studies concluded that the use of herbs was associated with both female gender and longer duration of DM.
Discussion
Summary of results
This systematic review has shown that there is generally low knowledge about DM, its risk factors and its complications among the Saudi population. Most DM patients had low to moderate knowledge scores in Riyadh, Jeddah, Al Hasa, Al-Khobar, and Mecca. Obesity was understood to be the most important risk factor, while weight reduction was acknowledged as a preventive measure. Unexpectedly, health professionals in Saudi Arabia also had low knowledge scores about DM, with physicians, nurses and medical students receiving low scores for knowledge about the epidemiology of the disease and the correct angle to administer insulin injections.
Critical appraisal of the studies included in our review
It does not escape our notice that the included studies from published literature suffer from some methodological limitations. Some studies had relatively small sample sizes. For example, Al-Aboudi et al9 included 75 participants and Al-Alawi et al12 included 45. In addition, most researchers employed a convenience sampling method, rather than a random sampling method, which resulted in limited generalizability to the target population.9,11,13,18,22,24-26 Kamel et al,21 Aljoudi et al,19 and Alzarea17 selected a random sampling of DM patients at their treatment centers. Alsaeedi et al23 worked in multiple primary health care centers in Mecca; therefore, they employed a 2-stage stratified random sampling strategy.
Another methodological limitation arises from different outcomes assessed across the studies. Alsaeedi et al,23 Al-Eidi et al,12 Abahussain et al,22 and Kamel et al21 aimed to evaluate the knowledge and use of complementary and alternative medicine products. Alzarea17 and Al-Alawi et al12 assess knowledge about eye complications of DM. Bahammam assessed the knowledge about periodontal diseases in association with DM.25 Binhemd evaluated the knowledge about DM and glycemic control.10
Moreover, all the studies assessed the knowledge about DM using different questionnaires, while in the survey used by Aljoudi et al,19 data were collected using a structured face-to-face interview. In most cases, these studies developed their questionnaires and piloted them among the study participants before use. The questionnaires included open-ended questions about the DM risk factors and prevention methods. In the study by Binhemd,10 participants were interviewed using a pre-structured questionnaire developed by the researchers based on earlier work about the misconceptions of DM among Saudi Arabia population. The most commonly used questionnaire was the brief diabetic knowledge test developed by the University of Michigan Diabetes Research and Training Centre.27 This questionnaire has been validated in the Saudi Arabian population28 and has been used by many studies to assess the knowledge of Saudi Arabia population about DM.9,29-31
Importance of DM Education in Saudi Arabia
This systematic review has identified a considerable gap in knowledge about DM in the Saudi population, including among healthcare workers, medical students, and DM patients themselves. Therefore, more efforts are required to increase knowledge and awareness of DM in Saudi Arabia, especially regarding epidemiology.
As has been shown in other countries, better health education is a powerful tool to control chronic health problems such as DM. For examples, 2 studies carried out in the United Kingdom by Christie et al32 and Deeb,33 reported better education among diabetic patients improves their ability to control the disease, resulting in better patient outcomes and reduced complications.
Therefore, increasing knowledge and awareness of DM in the population will contribute to better community health outcomes. Increased knowledge about DM is needed for patients to optimize their lifestyles and improve their medication habits to get the optimum benefits and delay the onset of long-term complications. Education is also essential to help DM patients’ families cope with the necessary lifestyle modifications and provide psychological and dietary support. For healthcare workers, higher levels of knowledge are needed because they provide the first direct source of information and education for patients. Additionally, clinical information, such as the correct angle for insulin injections, is essential for improving clinical outcomes. Therefore, improving knowledge about DM among physicians is imperative, given the prevalence of the disease in Saudi Arabia. Public health centers are considered the best place to provide health education interventions for citizens both with and without DM.
Risk Factors for DM in Saudi Arabia
The risk factors of DM can be classified into 2 categories: modifiable and non-modifiable. Modifiable risk factors include diets rich in fat, low physical activity, high BMI, high blood pressure (above 140/90), metabolic syndrome and high plasma levels of triglycerides. Non-modifiable risk factors include age (above 40 years) and family history of DM. The high prevalence of T2DM in the Saudi population is attributed to high levels of obesity as the rapid urbanization of the country has led to physical inactivity and the adoption of a more western diet rich in fat. Midhet et al34 performed a case-control study to investigate lifestyle-related risk factors of T2DM in Saudi Arabia. They found a strong association between lifestyle and T2DM: a maternal history of diabetes, education level, lack of exercise and dietary habits were significant risk factors. The adjusted odds ratios for these risk factors were: regular eating of Kabsa OR = 5.5 (95% CI 2.3 to 13.5), eating vegetables OR = 0.4 (95% Cl 0.2 to 0.7), eating dates OR = 1.8 (95% Cl 1.0 to 3.3) and sedentary lifestyle OR = 2.5 (95% Cl 1.2 to 5.0).
Murad et al35 performed a case-control study in Jeddah to investigate the risk factors of T2DM. They found that smoking, hypertension, increased weight/obesity and age (above 40 years) were significant risk factors for T2DM among the studied population. Alfadhli et al36 found that older maternal age, high BMI, high blood pressure, previous gestational diabetes (GDM), history of delivering a malformed child and family history of diabetes were the main risk factors for GDM.
Complications of DM
Complications of DM involve many body systems. Diabetic neuropathy, nephropathy, retinopathy and coronary artery disease are long-term severe complications of DM that require management and medical treatment.35-39 A study by Algeffari37 found that 35% of DM patients in Saudi Arabia suffer diabetic neuropathy. The odds of experiencing diabetic neuropathy was higher in those patients with poor compliance with their treatment plan. Diabetic foot is another major complication and economic burden of DM, as it results in partial disability of the patient.38 A cross-sectional study of 62,681 DM patients from the Saudi National Diabetes Registry (SNDR) found that about 3.3% of DM patients had diabetic foot complications. Risk factors for diabetic foot include male gender, cerebral vascular disease, poor glycemic control, insulin use and old age.38
Diabetic retinopathy is a result of macular edema due to vascular changes in retinal vessels. A study of 690 randomly selected DM patients from King Fahd Hospital at Al-Madinah showed that about 36% of T2DM patients had microalbuminuria.40 Another cross-sectional study examining 50,464 DM patients from the SNDR showed that about 20% of DM patients had diabetic retinopathy.39 According to the SNDR, about 10.8% of DM patients in Saudi Arabia had diabetic nephropathy.39 Diabetic nephropathy starts with microalbuminuria and progresses to end-stage renal disease.41 Age and DM duration were the most important risk factors for diabetic nephropathy.41
Role of physical activity in DM
Multiple studies have linked low physical activity with DM in the Saudi population.42-44 Exercise and physical activity help glucose entry into body cells, which improves the functions of insulin and enhances glucose metabolism. Exercise can indirectly reduce the risk of DM by decreasing body weight and burning fat cells which resist insulin. Midhet et al34 found that a healthy diet combined with physical activity can reduce the risk of T2DM by 45%, despite having a family history of diabetes. Therefore, health education programs need to promote a healthy lifestyle in the Saudi population to minimize the burden of the disease.
Strengths and limitations of this review
This systematic review has multiple strength: First, we followed the PRISMA statement guidelines during the preparation of this review to ensure a robust process, to explore knowledge of DM in the Saudi population. This is the first attempt to integrate the results of multiple studies about this topic. Second, we included epidemiological studies assessing the knowledge and awareness of the Saudi Arabia population in different geographical locations. Also, these studies represent a wide array of the population groups including DM patients, healthcare professionals, and school children. However, our review is limited by the differences in the outcomes reported by individual studies. Also, the questionnaires used to assess the knowledge and awareness of participants were heterogeneous. Many researchers developed their surveys based on the literature search while others use the validated DKT-2 developed by Michigan University. Finally, the low sample size of some studies and the non-probability sampling methods employed by several studies might limit the generalizability of their findings.
Implications for health policy
This systematic review highlighted the lack of knowledge and awareness of DM among the Saudi population. To improve public knowledge and awareness, it is necessary to enhance the education of health professionals regarding the pathology, etiology, risk factors, prevention, management and complications of DM. A greater focus is needed on the responsibility of health professionals in educating patients, families and the community about how a healthy lifestyle can reduce the risk of developing DM and the complications of those living with this chronic disease.
In conclusion, this review highlighted a gap in the knowledge about DM and its risk factors among the Saudi population. Further public health interventions are needed in Saudi Arabia to address the lack of knowledge about DM and its preventive measures.
Footnotes
References
- 1.International Diabetes Federation. IDF diabetes atlas - 2017 Atlas. [[Update 2017; cited 2018 February 19]]. Available from: http://www.diabetesatlas.org/resources/2017-atlas.html .
- 2.Kearns K, Dee A, Fitzgerald AP, Doherty E, Perry IJ. Chronic disease burden associated with overweight and obesity in Ireland: the effects of a small BMI reduction at population level. BMC Public Health. 2014;14:143. doi: 10.1186/1471-2458-14-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al-Daghri NM, Al-Attas OS, Alokail MS, Alkharfy KM, Yousef M, Sabico SL, et al. Diabetes mellitus type 2 and other chronic non-communicable diseases in the central region, Saudi Arabia (riyadh cohort 2): A decade of an epidemic. BMC Med. 2011;9:76. doi: 10.1186/1741-7015-9-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alqurashi KA, Aljabri KS, Bokhari SA. Prevalence of diabetes mellitus in a Saudi community. Ann Saudi Med. 2011;31:19–23. doi: 10.4103/0256-4947.75773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Naeem Z. Burden of diabetes mellitus in Saudi Arabia. Int J Health Sci (Qassim) 2015;9:V–VI. doi: 10.12816/0024690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 8.Higgins JPT, Green S, Series CB. Cochrane handbook for systematic reviews of interventions [Internet] Vol. 5. Wiley Online Library; 2008. [[cited 2014 Jun 1]]. p. 672. Available from: http://books.google.com/books?id=NKMg9sMM6GUC&pgis=1 . [Google Scholar]
- 9.Al-Aboudi I, Hassali M, Shafie A. Knowledge, attitudes, and quality of life of type 2 diabetes patients in Riyadh, Saudi Arabia. J Pharm Bioallied Sci. 2016;8:195. doi: 10.4103/0975-7406.171683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Binhemd TA. Diabetes mellitus: Knowledge, attitude, practice and their relation to diabetes control in female diabetics. Ann Saudi Med. 1992;12:247–251. doi: 10.5144/0256-4947.1992.247. [DOI] [PubMed] [Google Scholar]
- 11.Almalki TM, Almalki NR, Balbaid K, Alswat K. Assessment of diabetes knowledge using the Michigan brief diabetes knowledge test among patients with type 2 diabetes mellitus. J Endocrinol Metab. 2017;7:185–189. [Google Scholar]
- 12.Al-Alawi A, Al-Hassan A, Chauhan D, Al-Futais M, Khandekar R. Knowledge, attitude, and perception of barriers for eye care among diabetic persons registered at Employee Health Department of a Tertiary Eye Hospital of Central Saudi Arabia. Middle East Afr J Ophthalmol. 2016;23:71. doi: 10.4103/0974-9233.164629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alotaibi A, Gholizadeh L, Al-Ganmi A, Perry L. Examining perceived and actual diabetes knowledge among nurses working in a tertiary hospital. Appl Nurs Res. 2017;35:24–29. doi: 10.1016/j.apnr.2017.02.014. [DOI] [PubMed] [Google Scholar]
- 14.Khan A, Khamseen M, Al Aithan M, Khan S, Al Ibrahim I, Al Abdul Lateef Zn. Knowledge, attitude and practice of ministry of health primary health care physicians in the management of type 2 diabetes mellitus: A cross-sectional study in the Al Hasa District of Saudi Arabia 2010. Niger J Clin Pract. 2011;14:52. doi: 10.4103/1119-3077.79241. [DOI] [PubMed] [Google Scholar]
- 15.Al Wadaani F. The knowledge attitude and practice regarding diabetes and diabetic retinopathy among the final year medical students of King Faisal University Medical College of Al Hasa region of Saudi Arabia: A cross sectional survey. Niger J Clin Pract. 2013;16:164. doi: 10.4103/1119-3077.110133. [DOI] [PubMed] [Google Scholar]
- 16.Menwer Alanazi A, Mohamed Abo el-Fetoh N, Khalid Alotaibi H, Ayed Alanazi K, Khalid Alotaibi B, Majed Alshammari S, et al. Survey of awareness of diabetes mellitus among the Arar population, Northern Border Region of Saudi Arabia. Electron Physician. 2017;9:5369–5374. doi: 10.19082/5369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al Zarea BK. Knowledge, Attitude and Practice of Diabetic Retinopathy amongst the Diabetic Patients of AlJouf and Hail Province of Saudi Arabia. J Clin Diagn Res. 2016;10:NC05–NC08. doi: 10.7860/JCDR/2016/19568.7862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Mountashiri NA, Al-Zhrani AM, Ibrahim SFH, Mirghani HO. Dietary habits, physical activity and diabetes perception among patients with type 2 diabetes mellitus in Tabuk City, Saudi Arabia. Electron Physician. 2017;9:5179–5184. doi: 10.19082/5179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aljoudi AS, Taha AZA. Knowledge of diabetes risk factors and preventive measures among attendees of a primary care center in eastern Saudi Arabia. Ann Saudi Med. 2009;9:15–19. doi: 10.4103/0256-4947.51813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Al-Mutairi RL, Bawazir AA, Ahmed AE, Jradi H. Health beliefs related to diabetes mellitus prevention among adolescents in Saudi Arabia. Sultan Qaboos Univ Med J. 2015;15:e398–e404. doi: 10.18295/squmj.2015.15.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kamel FO, Magadmi RM, Hagras MM, Magadmi B, AlAhmad RA. Knowledge, attitude, and beliefs toward traditional herbal medicine use among diabetics in Jeddah Saudi Arabia. Complement Ther Clin Pract. 2017;29:207–212. doi: 10.1016/j.ctcp.2017.10.007. [DOI] [PubMed] [Google Scholar]
- 22.Abahussain NA, El-Zubier AG. Diabetes knowledge among self reported diabetic female teachers: Al-khobar, Saudi Arabia. J Family Community Med. 2005;12:43–48. [PMC free article] [PubMed] [Google Scholar]
- 23.Al-Saeedi M, Elzubier AG, Bahnassi AA, Al-Dawood KM. Patterns of belief and use of traditional remedies by diabetic patients in Mecca, Saudi Arabia. East Mediterr Health J. 2003;9:99–107. [PubMed] [Google Scholar]
- 24.Al-Eidi S, Tayel S, Al-Slail F, Qureshi NA, Sohaibani I, Khalil M, et al. Knowledge, attitude and practice of patients with type 2 diabetes mellitus towards complementary and alternative medicine. J Integr Med. 2016;14:187–196. doi: 10.1016/S2095-4964(16)60244-3. [DOI] [PubMed] [Google Scholar]
- 25.Bahammam M. Periodontal health and diabetes awareness among Saudi diabetes patients. Patient Prefer Adherence. 2015:225. doi: 10.2147/PPA.S79543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Elzubier AG, AlAmri ADA, AlHaraka EA, AbuSamara IO. Self-care, self-reliance and knowledge of diabetes among diabetics in Qassim Region, Saudi Arabia. Saudi Med J. 1996;17:598–603. [Google Scholar]
- 27.Fitzgerald JT, Funnell MM, Anderson RM, Nwankwo R, Stansfield RB, Piatt GA. Validation of the revised brief diabetes knowledge test (DKT2) Diabetes Educ. 2016;42:178–187. doi: 10.1177/0145721715624968. [DOI] [PubMed] [Google Scholar]
- 28.Alhaiti AH, Alotaibi AR, Jones LK, DaCosta C, Lenon GB. Psychometric evaluation of the revised Michigan diabetes knowledge test (v.2016) in arabic: translation and Validation. J Diabetes Res. 2016;2016:1–7. doi: 10.1155/2016/9643714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Almalki TM, Almalki NR, Balbaid K, Alswat K. Assessment of diabetes knowledge using the michigan brief diabetes knowledge test among patients with type 2 diabetes mellitus. J Endocrinol Metab. 2017;7:185–189. [Google Scholar]
- 30.Moawad S. Assessment of Knowledge among Saudi Diabetic Children/ Adolescent at Riyadh City. Am J Nurs Sci. 2014;3:5. [Google Scholar]
- 31.Zowgar AM, Siddiqui MI, Alattas KM. Level of diabetes knowledge among adult patients with diabetes using diabetes knowledge test. Saudi Med J. 2018;39:161–168. doi: 10.15537/smj.2017.2.21343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Christie D, Strange V, Allen E, Oliver S, Wong IC, Smith F, et al. Maximising engagement, motivation and long term change in a Structured Intensive Education Programme in Diabetes for children, young people and their families: Child and Adolescent Structured Competencies Approach to Diabetes Education(CASCADE) BMC Paediatr. 2009;9:1–10. doi: 10.1186/1471-2431-9-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Deeb LC. Diabetes technology during the past 30 years: a lot of changes and mostly for the better. Diabetes Spectr. 2008;21:78–83. [Google Scholar]
- 34.Midhet FM, Al-Mohaimeed a a Sharaf FK. Lifestyle related risk factors of type 2 diabetes mellitus in Saudi Arabia. Saudi Med J. 2010;31:768–774. [PubMed] [Google Scholar]
- 35.Murad MA, Abdulmageed SS, Iftikhar R, Sagga BK. Assessment of the common risk factors associated with type 2 diabetes mellitus in Jeddah. Int J Endocrinol. 2014;2014:1–9. doi: 10.1155/2014/616145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alfadhli EM, Osman EN, Basri TH, Mansuri NS, Youssef MH, Assaaedi SA, et al. Gestational diabetes among Saudi women: prevalence, risk factors and pregnancy outcomes. Ann Saudi Med. 2015;35:222–230. doi: 10.5144/0256-4947.2015.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Algeffari MA. Painful Diabetic Peripheral Neuropathy among Saudi Diabetic Patients is Common but Under-recognized: Multicenter Cross-sectional study at primary health care setting. J Family Community Med. 2018;25:43–47. doi: 10.4103/jfcm.JFCM_145_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Al-Rubeaan K, Al Derwish M, Ouizi S, Youssef AM, Subhani SN, Ibrahim HM, et al. Diabetic foot complications and their risk factors from a large retrospective cohort study. PLoS One. 2015;10:e0124446. doi: 10.1371/journal.pone.0124446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Al-Rubeaan K, Abu El-Asrar AM, Youssef AM, Subhani SN, Ahmad NA, Al-Sharqawi AH, et al. Diabetic retinopathy and its risk factors in a society with a type 2 diabetes epidemic: a Saudi National Diabetes Registry-based study. Acta Ophthalmol. 2015;93:e140–e147. doi: 10.1111/aos.12532. [DOI] [PubMed] [Google Scholar]
- 40.El-Bab MF, Shawky N, Al-Sisi A, Akhtar M. Retinopathy and risk factors in diabetic patients from Al-Madinah Al-Munawarah in the Kingdom of Saudi Arabia. Clin Ophthalmol. 2012;6:269–276. doi: 10.2147/OPTH.S27363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Al-Rubeaan K, Youssef AM, Subhani SN, Ahmad NA, Al-Sharqawi AH, Al-Mutlaq HM, et al. Diabetic nephropathy and its risk factors in a society with a type 2 diabetes epidemic: a Saudi National Diabetes Registry-based study. PLoS One. 2014;9:e88956. doi: 10.1371/journal.pone.0088956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Al-Baghli NA, Al-Turki KA, Al-Ghamdi AJ, El-Zubaier AG, Al-Ameer MM, Al-Baghli FA. Control of diabetes mellitus in the Eastern Province of Saudi Arabia: results of screening campaign. East Mediterr Health J. 2010;16:621–629. [PubMed] [Google Scholar]
- 43.Alzaheb RA, Altemani AH. The prevalence and determinants of poor glycemic control among adults with type 2 diabetes mellitus in Saudi Arabia. Diabetes Metab Syndr Obes. 2018;11:15–21. doi: 10.2147/DMSO.S156214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mokabel F, Aboulazm S, Hassan H, Al-Qahtani M, Alrashedi S, Zainuddin F. The efficacy of a diabetic educational program and predictors of compliance of patients with noninsulin-dependent (type 2) diabetes mellitus in Al-Khobar, Saudi Arabia. J Fam Community Med. 2017;24:164. doi: 10.4103/jfcm.JFCM_45_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Al Rasheed R, Al Adel F. Diabetic retinopathy: Knowledge, awareness and practices of physicians in primary-care centers in Riyadh, Saudi Arabia. Saudi J Ophthalmol. 2017;31:2–6. doi: 10.1016/j.sjopt.2017.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


