Abstract
Dermoscopy is an important in-vivo, non-invasive diagnostic technique that allows visualization of morphological features not macroscopic visible. It has a major contribution in enhancing the diagnostic accuracy for pigmented skin lesions. Recent studies have shown that it also aids in the diagnosis of non-pigmented keratinizing skin lesions, including actinic keratosis and Bowen’s disease. We performed a retrospective study in Dermamed Clinic Craiova, between January and June 2014, with the aim to correlate the dermoscopic and histopathological aspect of skin tumors. This study included a total of 74 patients, aged between 16 and 76 years. The dermatoscopic examination revealed 12 skin cancers, 51 precancerous lesions and 11 benign tumors. Those 12 subjects diagnosed with malignant tumors by dermatoscopic examination, had also histopathological examination and confirmation of the diagnosis, also 11 patients identified with benign tumors with dermatoscopic examination were subsequently confirmed by histopathological assesment. Out of the 51 patients with premalignant tumors, 48 patients had histopatological confirmation of it, and for 3 patients the result was squamous cell carcinoma. Thus dermatoscopic examination identified the malignant lesions with a specificity of 100% and a sensitivity of 80% with a positive predictive value of 100% and a negative predictive value of 94.12%, p<0.000.
Keywords: dermoscopy, melanoma, basal cell carcinoma, squamous cell carcinoma
Introduction
Dermoscopy or dermatoscopy[1, 2] is a noninvasive technique that consists of viewing pigmented skin lesions through a hand-held lens, a dermatoscope or a video imaging system. Dermoscopy has considerably developed, becoming a routine technique in many countries in the mid-1980s.
Patients and Methods
We performed a retrospective study in Dermamed Clinic Craiova, between January and June 2014, with the aim to correlate the dermoscopic and histopathological aspect of tumors. Our study included 74 patients with premalignant skin tumors and skin cancers. The study was approved by the local ethics committee and written informed consent was obtained from all patients.
Results
This study included a total of 74 patients (48 women and 26 men), aged between 16 and 76 years. Considering the regions 26 of them were from rural areas and 48 from urban areas (Table 1).
Table 1.
Distribution of patients - environment, sex
| Urban areas | Rural areas | Women | Men |
| 48 | 26 | 48 | 26 |
The dermatoscopic examination revealed 12 skin cancers (6 basal cell carcinomas, 3 squamous cell carcinomas and 3 melanomas), 51 precancerous lesions (38 nevi, 12 actinic keratosis and a keratoacanthoma) and 11 benign tumors (11 seborrheic keratosis).
Those 12 subjects diagnosed with malignant tumors by dermatoscopic examination, had also histopathological examination and confirmation of the diagnosis (6 basal cell carcinomas - Figure 1,2,3, 3 squamous cell carcinomas - Figure 4,5,6, and 3 melanomas Figure 7,8,9,107-10), also 11 patients identified with benign tumors with dermatoscopic examination were subsequently confirmed by histopathological assesment (Fig. 11,12).
Figure 1.
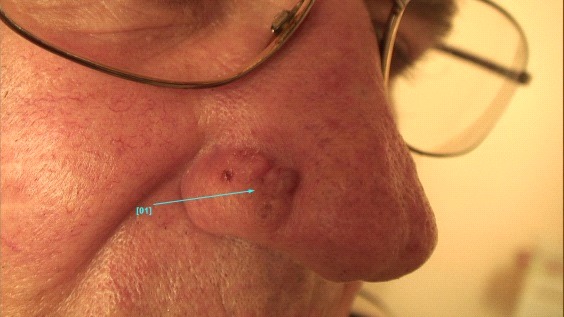
Clinical aspect of Basal cell carcinoma
Figure 2.

Dermatoscopic aspect of Basal cell carcinoma
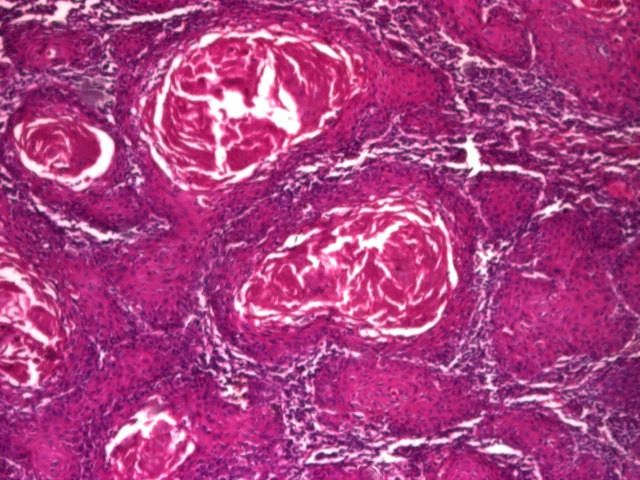
Figure 3.
Basal cell carcinoma adenoid form
Figure 4.

Clinical aspect of Squamous cell carcinoma
Figure 5.

Dermatoscopic aspect of Squamous cell carcinoma
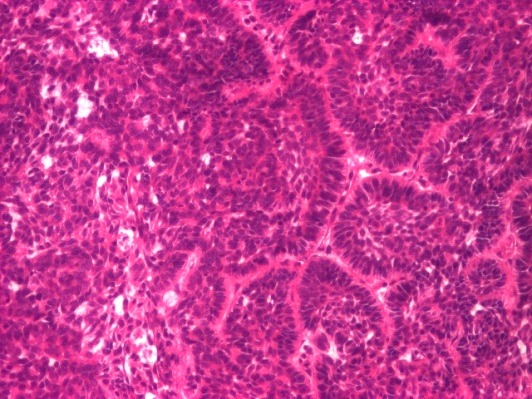
Figure 6.
Histopatological aspect of Squamous cell carcinoma
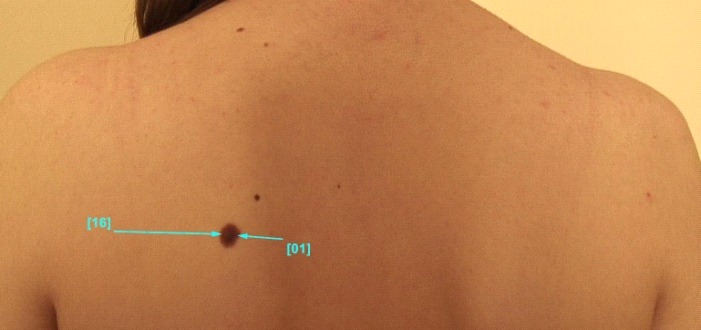
Figure 7.

Clinical aspect of melanoma
Figure 8.

Dermatoscopic aspect of melanoma
Figure 9.

Dermatoscopic aspect of melanoma
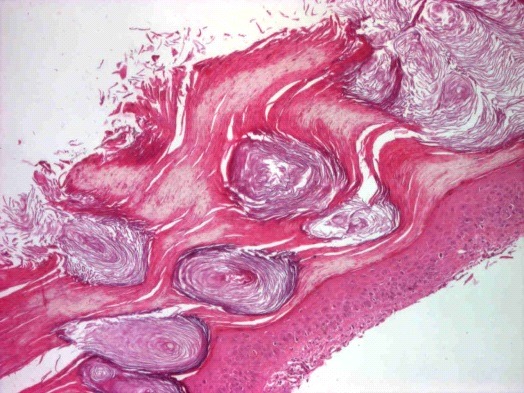
Figure 10.
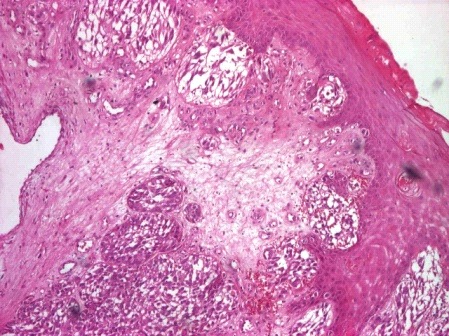
Histopatological aspect of melanoma
Figure 11.

Clinical aspect Seborrheic keratosis
Figure 12.

Dermatoscopic aspect of Seborrheic keratosis
After dermatoscopic assessment we identified 22 nevi with dysplasia (central hypopigmentation, hyperpigmentation, peripheral hyper/hypopigmentation, multifocal blue areas, epidermal cysts).
Out of the 51 patients with premalignant tumors, 48 patients were confirmed by histopatological examination with this type of lesions (38 nevi - Fig. 13,14,15,16, 10 actinic keratoses - Fig. 17,18,19), and at 3 patients (2 actinic keratoses and 1 keratoacanthoma - Fig. 20, 21) skin biopsy revealed squamous cell carcinoma.
Figure 13.

Clinical aspect of common nev
Figure 14.

Dermatoscopic aspect of common nev
Figure 15.
Clinical aspect of dysplastic nev
Figure 16.

Dermatoscopic aspect of dysplastic nev
Figure 17.

Clinical aspect of Actinic keratosis
Figure 18.

Dermatoscopic aspect of Actinic keratosis
Figure 19.
Histopatological aspect of Actinic keratosis
Figure 20.

Clinical aspect of Keratoacanthoma
Figure 21.

Dermatoscopic aspect of Keratoacanthoma
Thus dermatoscopic examination identified the malignant lesions with a specificity of 100% and a sensitivity of 80% with a positive predictive value of 100% and a negative predictive value of 94.12%, p<0.000 (Table 2).
Table 2.
Distribution of the lesions according to dermatoscopic and histopathological examination
| Skin biopsy</p> | Skin biopsy precancerous lesions | Skin biopsy</p> | |
| <p>malignant tumors | <p>benign tumors | ||
| Dermatoscopy – malignant tumors | 12 | 0 | 0 |
| Dermatoscopy – precancerous lesions | 3 | 48 | 0 |
| Dermatoscopy – benign tumors | 0 | 0 | 11 |
Discussion
Dermoscopic findings have been formulated into diagnostic criteria that assist experienced clinicians in differentiating benign and malignant skin tumors. In essence, dermoscopy can help identify cutaneous malignancies, while at the same time minimizing the frequency of unnecessary biopsies of benign cutaneous lesions.
Nonmelanocytic Lesions
Among nonmelanocitic lesions, that we met in our group of patients, 11 were represented by seborrheic keratoses and for those dermatoscopic exam was in absolute relationship with histopathological examination. The dermatoscopic aspect we met is in relationship with the ones published in dermatology journals.
In seborrheic keratosis are starry and cloudy milia-like cysts, comedo-like openings (keratin-filled invaginations of the epidermis with blackhead-like plugs) and fissures and ridges sometimes giving a brain-like appearance.[3,4,5] Comedo-like openings and fissures and ridges may rarely be seen also in papillomatous dermal nevi. Particularly, starry milia-like cysts can be detected with high prevalence in both seborrheic keratosis and melanoma; conversely, cloudy milia-like cysts have a specificity of 99% for seborrheic keratosis in respect to melanoma and have been considered the hallmark of seborrheic keratosis. Also, another dermoscopic structure, typical but not exclusive of seborrheic keratosis is represented by hairpin vessels. Linear irregular, hairpin, glomerular and arborizing vessels are vascular structures commonly observed in nonmelanocytic lesions.
Actinic keratosis
Our study included a total of 12 actinic keratosis diagnosed by dermatoscopic examination. Histopathology revealed two squamous cell carcinoma.
The usual dermoscopic aspect of actinic keratosis (AK) is an erythema forming a marked pink-to-red pseudonetwork surrounding the follicular openings defined as 'strawberry' pattern.[6] Follicles are typically keratin-filled and appear as yellowish to white ovoid structures sometimes with a targetoid aspect with a darker inner part and a lighter one around. Fine linear or coiled vessels can be seen at higher magnification in the spaces around follicles. Surface scales are often present, representing a further diagnostic element.[6,7] Zalaudek et al. proposed an interesting dermoscopic progression model of facial AK developing into SCC. Conversely, pigmented AK are characterized by slate-grey to black dots and globules around the follicular ostia, annular-granular and rhomboidal structures and less frequently by brown-to-grey pseudonetwork (high specificity for a diagnosis of pigmented AK).
Basal Cell Carcinoma (BCC)
Basal cell carcinomas can be dermoscopic classified as pigmented and nonpigmented lesions, a classification which does not always correspond to the clinical aspect – dermatoscopic examination increases the sensitivity of pigment detection (marked out by nuances of black, brown, blue and gray). Some authors still divide pigmented tumors according to pigment quantifying, into lesions slightly pigmented (<30 per cent of the tumor contains pigment), pigmented (30 to 70 per cent of the surface contains pigment) and intensely pigmented (>70 per cent of the tumor surface contains pigment).
Dermatoscopic structures that we encountered in the 6 cases of basal cell carcinoma were suggestive of the diagnosis. The non pigmented elements were pink-reddish or bluish areas, arborescent, pearly homogeneous areas, branching vascular elements asymmetrically disposed on the lesions and clearly present in the image (in focus), ulceration (often covered with hematic crust – red, black or serous-orange, yellow), to which may be added vascular elements such as fine, short capillaries. Relevant for pigmented tumors are: the absence of the pigmentary network, variously sized gray-bluish globules, peripheral foliaceous structures, granulations of brown and gray pigments, wheel arm-like structures. [8]
Squamous Cell Carcinoma (SCC)
Dermatoscopic aspects that we encountered for SCC does not fit into a specific pattern. The vascular pattern represents the main dermoscopic feature. SCC is poor in dermoscopic structures, a polymorphous vascular pattern is the hallmark of the lesion and it consists of irregularly shaped and distributed hairpin vessels, irregularly distributed dotted, glomerular and linear vessels. Ulceration, keratin crust and surface scales may be present.
The dermatoscopic features of SCC are a non-specific pattern with scales and grouped glomerular blood vessels surrounded by a whitish halo. A scaly surface, brown globules and glomerular vessels can be seen in the dermatoscopic examination of pigmented Bowen’s disease. In SCC the vascular pattern represents the main dermoscopic feature. Conversely, SCC is poor in dermoscopic structures but a polymorphous vascular pattern is the hallmark of the lesion and it consists of irregularly shaped and distributed hairpin vessels, irregularly distributed dotted, glomerular and linear vessels. Ulceration, keratin crust and surface scales may be present.
In our study we had a patient with keratoacanthoma at dermatoscopic examination, but the histopathological examination, for the same lesion, showed SCC.
In keratoacanthoma, hairpin vessels are the main vascular structure. They are distributed peripherally and they surround a mass of keratin localized in the central part of the lesion, ranging in color from yellowish to brown.
Melanocytic Lesions
Melanocytic Nevi
This study found 38 types of nevi: 9 common nevi, 22 dysplastic nevi, 6 halo and one blue nevi. The dermatoscopic aspect we met, after assesing the skin lesions, is in relationship with the one found at the cases reported in dermatological literature.
From a histopathological point of view, common (or Clark) nevi can be classified into three main categories: junctional, dermal and compound nevi. The prototypic dermoscopic aspect of each type of nevus is a brownish (light to dark) reticular pattern (pigmented network with or without an overlying “black lamella” of melanin pigment), globular or a combination of pigmented network and globules, respectively.
In common nevi the pigment network is composed of regularly meshed uniform brown lines, gradually thinning out at the periphery. Globules are characterized by uniformity of size and shape and regularly distributed. A combination of network and globules usually results in a homogeneous distribution of globules in the central part, regularly at the periphery or throughout the holes of the entire pigment network.
Atypical nevi display the same dermoscopic structures of common nevi but are frequently irregular in size and/or shape and/or irregularly disseminated. [3,4] Pigmented network may be characterized by areas of darkening, interruptions, irregular sizes of the holes and irregular borders. Globules may be not homogenous in shape, size and distribution. A gray-white veil can be observed. These lesions present heterogeneity of colors. [3,4]
Halo nevi are characterized by an association of homogeneous and globular pattern followed by the homogeneous and the globular pattern alone, surrounded by a fair rim of depigmentation. The reticular pattern has been seen in a minority of cases.
The dermosopic features of blue nevi are considered to have high specificity for the diagnosis of this type of nevus. The authors observed blue nevi to be often characterized by a blue or white-blue homogeneous pigmentation and less commonly by brown structureless (combined blue nevus) or polychromatic (deep penetrating blue nevus) appearance.
Melanoma
Out of 74 patients, 3 skin tumors were melanomas after dermatoscopic and histopathological assessment. The dermatoscopic examination showed general features representing asymmetry and polychrome aspect. Structural elements were atypical pigmented network, blue vale, atypical vessels and irregular pigmentation.
Superficial melanomas usually have one or more of the following dermoscopic features: blue-white veil, multiple brown dots, pseudopods, radial streaming, scar-like depigmentation, peripheral black dots/globules, multiple (5-6) colors, especially red and blue, broad network, focal sharply cut-off border, negative network, irregular vascularity.
The blue-white veil is described as an irregular structure-less area of confluent blue pigmen,t with a ground glass haze, as if the image were out of focus. It is due to hyperkeratinisation over dense epidermal pigment. Uniform blue-white structures may be observed over some blue nevi and hemangiomas, but in melanoma they are focal, asymmetrical and irregular.
Scar-like depigmentation, due to regression of melanoma, results in irregular white areas that must be distinguished from the uniform peripheral loss of pigment seen in benign halo nevi. It arises in about 50% of melanomas.
In a study of Pizzichetta et al., the dermoscopic description observed for in situ melanoma were blue-whitish veil, grey-blue areas and black dots. White scar-like areas and atypical vessels were found in thicker lesions. Similarly, invasive melanomas with a thickness less than 0.75 mm showed basically the similar criteria but with a lower frequency of irregular pigment network and pseudopods and a higher frequency of blue-whitish veil with respect to in situ melanomas. Incidence of blue-whitish veil increases in melanomas thicker than 0.75 mm. [9]
Conclusion
The combination of clinical assessment, dermoscopic and histopathologic examination improves the accuracy of the diagnosis of skin tumors and at the same time minimizes unnecessary excisions of benign skin tumors.
Acknowledgments
This paper was published under the frame of European Social Found, Human Resources Development Operational Programme POSCCE 2003-2014, project no. 580/19.09.2013
References
- 1.Vestergaard ME, Macaskill P, Holt PE, Menzies SW. Dermoscopy compared with naked eye examination for the diagnosis of primary melanoma: a meta-analysis of studies performed in a clinical setting. Br J Dermatol. 2008;159(3):669–676. doi: 10.1111/j.1365-2133.2008.08713.x. [DOI] [PubMed] [Google Scholar]
- 2.Malvehy J, Puig S, Argenziano G, Marghoob AA, Soyer HP. International Dermoscopy Society Board members. Dermoscopy report: proposal for standardization. Results of a consensus meeting of the International Dermoscopy Society. J Am Acad Dermatol. 2007;57(1):84–95. doi: 10.1016/j.jaad.2006.02.051. [DOI] [PubMed] [Google Scholar]
- 3.Argenziano G, Soyer HP, Chimenti S, et al. Dermoscopy of pigmented skin lesions: results of a consensus meeting via the Internet. J Am Acad Dermatol. 2003;48(5):679–693. doi: 10.1067/mjd.2003.281. [DOI] [PubMed] [Google Scholar]
- 4.Braun RP, Rabinovitz HS, Oliviero M, Kopf AW, Saurat JH. Dermoscopy of pigmented skin lesions. J Am Acad Dermatol. 2005;52(1):109–121. doi: 10.1016/j.jaad.2001.11.001. [DOI] [PubMed] [Google Scholar]
- 5.Stricklin SM, Stoecker WV, Oliviero MC, Rabinovitz HS, Mahajan SK. Cloudy and starry milia-like cysts: how well do they distinguish seborrheic keratoses from malignant melanomas? J Eur Acad Dermatol Venereol. 2011;25(10):1222–1224. doi: 10.1111/j.1468-3083.2010.03920.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zalaudek I, Giacomel J, Argenziano G, et al. Dermoscopy of facial nonpigmented actinic keratosis. Br J Dermatol. 2006;155(5):951–956. doi: 10.1111/j.1365-2133.2006.07426.x. [DOI] [PubMed] [Google Scholar]
- 7.Zalaudek I, Kreusch J, Giacomel J, Ferrara G, Catricalà C, Argenziano G. How to diagnose nonpigmented skin tumors: a review of vascular structures seen with dermoscopy: part II. Nonmelanocytic skin tumors. J Am Acad Dermatol. 2010;63(3):377–386. doi: 10.1016/j.jaad.2009.11.697. [DOI] [PubMed] [Google Scholar]
- 8.Altamura D, Menzies SW, Argenziano G, Zalaudek I, Soyer HP, Sera F, Avramidis M, DeAmbrosis K, Fargnoli MC, Peris K. Dermatoscopy of basal cell carcinoma: morphologic variability of global and local features and accuracy of diagnosis. J Am Acad Dermatol. 2010;62:67–75. doi: 10.1016/j.jaad.2009.05.035. [DOI] [PubMed] [Google Scholar]
- 9!!!Pizzichetta MA, Argenziano G, Talamini R, et al. Dermoscopic criteria for melanoma in situ are similar to those for early invasive melanoma. Cancer. 2011;91(5):992–997. [PubMed] [Google Scholar]


