Abstract
The association between vitamin D and cancer has long been studied, but the results have been variable. Thus, there does not seem to be a consensus on whether vitamin D has a beneficial anti-cancer effect. This review not only summarizes the association between vitamin D and cancer risk and results of clinical trials involving vitamin D, but explores some of the reasons that contribute to the variability of study outcomes. Highlighted are single nucleotide polymorphisms (SNPs) that contribute to variability in the efficacy of vitamin D supplementation. Understanding these differences can personalize approaches to optimize the effectiveness of vitamin D in limiting cancer risk.
Keywords: l,25(OH)2D; cancer; polymorphisms; SNPs; vitamin D
Introduction
Multiple studies have assessed whether vitamin D can prevent cancer or if it can improve cancer treatment outcomes. This includes original studies and meta-analyses. Most studies on its preventive roles have correlated plasma levels of the vitamin D metabolites with cancer risk. Typically, 25(OH)D, the stable metabolite of vitamin D in the circulation, is measured and subjects are considered as vitamin D sufficient (30–100 ng/ml), insufficient (21–29 ng/ml) or deficient (<20 ng/ml). Below is a summary of studies demonstrating beneficial effects of vitamin D supplementation as well as studies showing the absence of vitamin D effects.
Beneficial effects of increased circulating levels of vitamin D metabolites
Many, although not all, studies that associate vitamin D levels with cancer risk measure serum levels of 25(OH)D to determine if the subjects are deficient. For example, a greater proportion of melanoma patients had deficient or insufficient levels of 25(OH)D than healthy controls [1]. Similarly, vitamin D levels were lower in patients with thyroid cancer compared to matched controls [2]. Women with breast cancer that were deficient in 25(OH)D had larger tumors, more advanced stage and reduced survival than those that were not deficient [3]. For glioblastoma, serum 25(OH)D was inversely associated with risk, although there was no association for non-glioblastoma glioma [4]. Using annual ambient ultraviolet B exposure as a surrogate for vitamin D levels, an inverse association with risk for esophageal and gastric cancers has been reported [5]. In a prospective Japanese population study with a 15 year follow-up, the incidence of liver and pre-menopausal breast cancers was greater in subjects with lower 25(OH)D levels at the study onset [6].
Vitamin D can also indirectly prevent cancer. Patients that failed treatment to eradicate Helicobacter pylori, which is associated with gastric cancer, had a higher prevalence of 25(OH)D deficiency than those that were successfully treated [7]. Indirect anti-cancer effects of vitamin D can also be due to its anti-inflammatory properties. Men with prostate cancer had reduced 25(OH)D and increased inflammatory mediator levels compared to controls [8]. Similarly, inflammatory mediators were increased in colorectal cancer patients that had lower levels of 25(OH)D [9].
Several meta-analyses have assessed the relationship between circulating 25(OH)D levels and cancer risk, with meta-analyses being able to assemble larger datasets than can individual studies. One such analysis of 25 prospective and retrospective studies associated reduced pancreatic cancer risk with increased vitamin D consumption [10]. An analysis of 17 prospective studies linked reduced 25(OH)D levels with increased lung cancer risk, although overall survival was not associated with 25(OH)D levels [11]. A combined case-control study and meta-analysis inversely correlated 25(OH)D levels and papillary thyroid cancer risk [12]. Finally, a meta-analysis of 22 studies showed reduced lung cancer risk and improved lung cancer patient survival when serum 25(OH)D levels were increased [13].
Fewer studies have examined links between vitamin D levels and lymphoproliferative diseases, although the active metabolite has been shown in vitro to stimulate differentiation of human leukemia HL-60 cells into monocytic cells [14]. A study of patients with lymphoid malignancies showed those with severe 25(OH)D deficiency had a shorter time to cancer progression [15]. Patients with newly diagnosed acute myeloid leukemia were typically 25(OH)D deficient (<20 ng/ml) [16]. However, those with 25(OH)D levels >20 ng/ml had a reduced length of hospitalization and higher complete remission rates following induction chemotherapy.
The absence of association between blood levels of vitamin D metabolites and cancer
Not all studies have shown beneficial effects of vitamin D. An epidemiological survey with a 7 year follow-up showed no association between 25(OH)D levels and cancers development [17]. Similarly, there was no beneficial effect of higher circulating vitamin D levels and pancreatic cancer risk in a large European prospective study [18]. An analysis of 20 prospective cohort studies involving over 5,000 case-control subjects found no association between 25(OH)D levels and lung cancer risk [19]. Similar results were found in a prospective study of subjects undergoing colonoscopy screening [20]. Neither insufficient nor deficient vitamin D levels were associated with the incidence of adenomatous polyps.
A few studies showed increased cancer risk with increased 25(OH)D levels. A meta-analysis of 19 prospective cohort studies associated increased 25(OH)D levels with an increased prostate cancer risk [21]. Possible reasons for why some studies show beneficial anti-cancer effects of vitamin D while others show no or detrimental effects to cancer risk are discussed toward the end of this review.
Relationship of vitamin D-associated pathways with cancer risk and progression
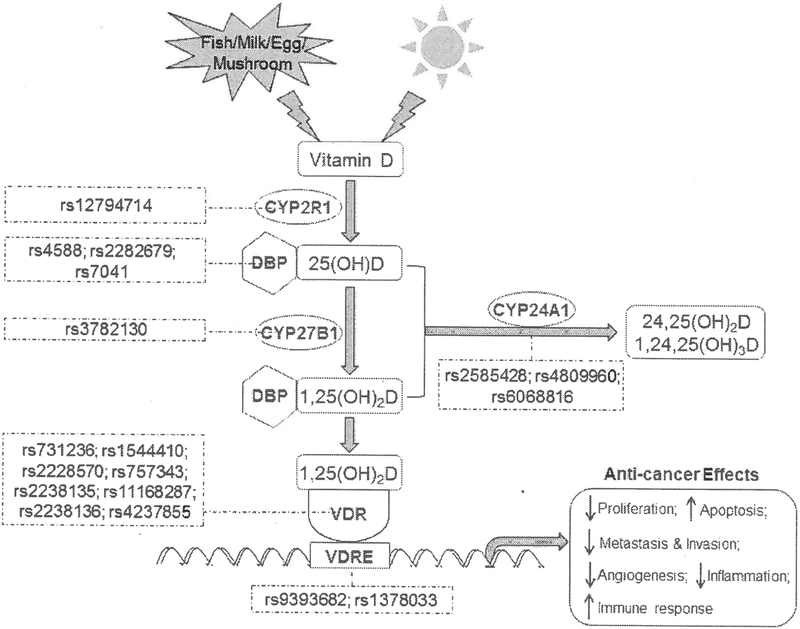
The association between vitamin D metabolites and cancer risk need to take into consideration the vitamin D pathway (summary in Figure 1). The actions of the active metabolite l,25(OH)2D are mediated by its binding to the vitamin D receptor (VDR) to, in turn, regulate multiple genes in a cell-specific manner. However, cancers such as human esophageal squamous cell carcinoma have less VDR expression than do normal tissues [22]. The survival of these cancer patients is lower when tumor stromal expression of VDR is reduced.
Figure 1.
Overview of the vitamin D-associated pathways and potential influences.
There are multiple single nucleotide polymorphisms (SNPs) for components of the vitamin D pathway (summary in Table 1). Among the most widely studied VDR SNPs is the rs731236 (TaqI) polymorphism. In a meta-analysis, this SNP was associated with increased prostate cancer risk, particularly in Asians [23]. The mutation could reduce stability of VDR mRNA and, thus, reduce receptor binding by l,25(OH)2D. A separate metaanalysis of 39 publications associated colorectal cancer risk with the VDR rs 1544410 (BsmI) polymorphism, and near significance of the rs2228570 (Fokl) SNP with colorectal cancer risk [24]. In Caucasians, the Fokl rs2228570 polymorphism was predictive of prostate cancer risk [25]. This same VDR polymorphism was associated with ovarian cancer risk in Caucasian women [26]. It was also predictive of hepatocellular carcinoma development in patients with chronic hepatitis C infection [27]. A different low penetrance rs757343 (Tru9I) SNP was associated in a case-control study with premenopausal breast cancer in Pakistani women [28]. A large case-control study of U.S. women linked increased breast cancer risk with the VDR rs2238135, rsl 1168287, rs2238136 and rs4237855 SNPs [29].
Table 1.
Association of SNPs with cancers.
| Molecules | Function | SNPs | Consequence | Refs |
|---|---|---|---|---|
| VDR | receptor for 1,25(OH)2D | rs731236 | ↑ prostate cancer in Asians | [23] |
| rs1544410 | ↑ colorectal cancer | [24] | ||
| rs2228570 | ↑ prostate cancer | [25] | ||
| ↑ ovarian cancer in Caucasian | [26] | |||
| ↑ hepatocellular carcinoma | [27] | |||
| rs757343 | ↑ breast cancer in Pakistani | [28] | ||
| rs2238135 | ↑ breast cancer | [29] | ||
| rs11168287 | ||||
| rs2238136 | ||||
| rs4237855 | ||||
| GC/DBP | bind and transport 25(OH)D | rs2282679 | ↓ colorectal cancer patient survival | [36] |
| rs7041 | ↓ non-small cell lung cancer | [38] | ||
| rs4588 | ↓ survival of colorectal cancer patients treated with chemo/bevacizumab | [39] | ||
| ↑ survival of colorectal cancer patients treated with chemo/cetuximab | [39] | |||
| CYP2R1 | hydroxylate vitamin D to 25(OH)D | rs12794714 | ↓ 25(OH)D levels ↑ ovarian cancer in European-ancestry |
[40] |
| ↑ colorectal cancer in African American | [41] | |||
| CYP27B1 | Convert 25(OH)D to active 1,25(OH)2D | rs28934604 | ↓ enzyme activity ↓ 1,25(OH)2D levels in colon cancer cells |
[42] |
| rs58915677 | ||||
| rs13377933 | ||||
| rs2229103 | ||||
| rs3782130 | ↑ non-small cell lung cancer | [38] | ||
| CYP24A1 | catabolize active 1,25(OH)2D to inactive metabolites | rs35051736 | ↓ enzyme activity ↑ 1,25(OH)2D levels in colon cancer cells |
[42] |
| rsl6999131 | ||||
| rs6022990 | ||||
| rs6068812 | ||||
| rs2585428 | ↓ pancreatic cancer in Caucasian | [43] | ||
| rs4809960 | ↓ breast cancer in Caucasian | [43] | ||
| rs6068816 | ↓ non-small cell lung carcinoma | [38] | ||
| VDRE | vitamin D response element | rs9393682 | ↑ prostate cancer | [45] |
| rs1378033 |
↑ = increases and ↓, = decreases consequence (i.e. cancer risk or progression).
Polymorphisms have also been described in the GC gene (group-specific component) encoding the vitamin D binding protein (DBP). DBP impacts the bioavailability of vitamin D metabolites, by binding to 25(OH)D with high affinity and l,25(OH)2D with lower affinity to transport them to target organs [30]. The association of 25(OH)D with DBP is critical for synthesis of l,25(OH)2D in the kidney, but can limit the bioavailability of 25(OH)D to non-renal sites. Polymorphisms in GC, including rs4588 and rs2282679, have been associated with lower systemic 25(OH)D levels [31–33]. For example, the GC rs4588 polymorphism yields a 3.5 ng/ml decrease in serum 25(OH)D levels per copy of the minor allele [34]. Not clear, however, is how this impacts on bioavailable 25(OH)D or l,25(OH)2D.
Polymorphisms in the GC gene have clinical implications. Restoration of 25(OH)D sufficiency by supplementation with 2,000 IU vitamin D were less effective in colorectal cancer patients with the GC rs4588 and rs2282679 polymorphisms [35]. The GC rs2282679 SNP was associated with reduced disease-free survival of colorectal cancer patients following cancer diagnosis, although it had no impact on cancer risk [36]. In contrast, no association was found in a Mendelian randomization study between the GC rs2282679 SNP and prostate cancer progression, as measured by prostate-specific antigen (PSA) levels, or patient mortality following radiation therapy [37]. The GC rs7041 SNP is associated with reduced non-small cell lung carcinoma risk, presumably because of the bioavailability of 25(OH)D and l,25(OH)2D [38]. Survival of metastatic colorectal cancer patients following treatment with chemotherapy plus either antibody to epidermal growth factor receptor (EGFR) or vascular endothelial growth factor (VEGF) was influenced by the GC rs4588 polymorphism [39]. Patients with this SNP had a shorter survival time following chemotherapy plus bevacizumab (anti-VEGF) but had a longer survival time following chemotherapy plus cetuximab (anti-EGFR). It was suggested that lower levels of vitamin D metabolites would have different impacts on the anti-angiogenic effect of bevacizumab and immune-associated effects of cetuximab.
Polymorphisms have been found in genes involved in vitamin D synthetic and catabolic pathways. The rsl2794714 polymorphism at CYP2R1, which encodes an enzyme that hydroxylates vitamin D to 25(OH)D, was associated with a 1.8 ng/ml decrease in serum 25(OH)D levels per minor allele [34]. A separate Mendel ian randomization study associated this rsl2794714 SNP with a reduction in 25(OH)D by 1.2 ng/ml for each risk allele [40]. This, in turn was linked to increased ovarian cancer risk among European-ancestry women. This SNP was also associated with increased colorectal cancer risk in African Americans [41].
SNPs in CYP27B1, which encodes the enzyme that converts 25(OH)D to l,25(OH)2D, have been associated with cancer risk. A case-control study associated the CYP27B1 rs3782130 SNP with increased non-small cell lung carcinoma risk [38]. This SNP was linked to reduced CYP27B1 mRNA expression and, in turn, reduced patient survival. Using in vitro analyses, 4 of 5 tested CYP27B1 SNPs (rs28934604, rs58915677, rsl3377933 and rs2229103) reduced CYP27B1 enzyme activity, indicating reduced availability of l,25(OH)2D [42].
SNPs in CYP24A1, encoding the primary enzyme that catabolizes 25(OH)D, have been linked to reduced cancer risk. In Caucasians, the CYP24A1 rs2585428 SNP decreased pancreas cancer risk, while the rs4809960 SNP decreased the breast cancer risk [43]. The rs6068816 SNP was associated with reduced non-small cell lung carcinoma risk [38]. In in vitro analyses to assess enzyme activity, all four of the tested CYP24A1 SNPs (rs35051736, rs 16999131, rs6022990 and rs6068812) reduced CYP24A1 hydroxylase activity, indicating reduced l,25(OH)2D degradation [42]. Assessment of CYP24A1 expression showed mRNA and protein were higher in non-small cell lung cancer compared to levels in non-cancerous tissues [44]. Higher CYP24A1 expression, suggesting increased degradation of l,25(OH)2D, was associated with reduced cancer differentiation and reduced patient survival.
Less extensively studied are polymorphisms in vitamin D response elements (VDRE) and their biological impacts. A study of prostate cancers associated rs9393682 with progression of localized prostate cancer while rsl378033 was associated with reduced progression for advanced prostate cancer [45]. Assessment of expression of nearby genes associated rs9393682 with expression of HFE (hemochromatosis) and rsl378033 with expression of TUSC3 (tumor suppressor candidate). These related genes have biological impacts since, in response to l,25(OH)2D, prostate cancer cells downregulated HFE expression, which, in turn, inhibits prostate cancer cell proliferation. l,25(OH)2D treatment also induced TUSC3 expression, which is important limiting cancer cell growth and migration.
Overall, the above studies of polymorphisms of the vitamin D-associated pathways, including VDR, GC, CYP2R1, CYP27B1, and CYP24A1 show SNP heritability could regulate the activity and levels of l,25(OH)2D and can impact on cancer risk. However, not all vitamin D-associated SNPs have been linked to cancer risk and those that have do not predict risk to all cancers. For example, a study of SNPs in women showed that polymorphism in the DHCR7 gene (rs11234027) encoding an enzyme that diverts metabolism from vitamin D to cholesterol, CYP2R1 (rs7944926) and in GC (rs2282679) were not associated with an increased risk of breast, colorectal or lung cancer [46].
Clinical trials involving treatment with vitamin D metabolites
Chronic inflammation is considered to be protumorigenic such as for cancers of the prostate, lung, liver and esophagus [47–50]. Vitamin D can temper inflammation and, thus, has been examined for efficacy in inflammation-associated disorders [51, 52]. This includes cancer chemoprevention. In a randomized, double-blind placebo-controlled trial involving women with cervical intraepithelial neoplasia grade 1 (CIN1), supplementation with 50,000 lU vitamin D every two weeks for 6 months increased the percentage of women having CIN1 regression [53]. Vitamin D supplementation also reduced markers of inflammation and oxidative stress, suggesting this was a mechanism for the observed regressions of CIN Is and, in turn, reduced progression to cervical cancer. However, there are also conflicting results. A randomized doubleblind study demonstrated no effect of the relatively low dose of 1,000 IU/day vitamin D in preventing recurrent pre-cancerous polyps in subjects whose adenomatous polyps were removed during colonoscopy [54].
The immune-modulatory effects of vitamin D in patients with cancer have also been examined. An analysis of the prostate transcriptome showed that vitamin D supplementation (4,000 IU/day) for 2 months prior to undergoing prostatectomy altered expression of inflammatory genes [55]. This was particularly evident in African Americans, a population with an increased prostate cancer risk and a higher incidence of vitamin D deficiency. In a separate prospective study, these investigators showed that supplementing low-risk prostate cancer patients that were under active surveillance with 4,000 IU/day vitamin D for one year decreased their Gleason scores and reduced the number of positive cores upon repeated biopsy [56]. Immune regulatory activity of vitamin D was also demonstrated in patients with head and neck squamous cell carcinoma (HNSCC). In a randomized prospective study, HNSCC patients receiving l,25(OH)2D for 3 weeks prior to surgical treatment had a significantly longer time to cancer recurrence than patients that were untreated prior to surgery [57, 58]. The l,25(OH)2D treatment diminished circulating levels of immune inhibitory cells while increasing intratumoral levels of immune reactive CD4+ T-cells and mature dendritic cells.
Other anti-tumor mechanisms were demonstrated in breast cancer patients in which high-dose vitamin D supplementation (10,000 IU/day) decreased levels of the CYP24A1 product 27-hydroxycholesterol (27HC), which is an estrogen receptor modulator that supports breast cancer growth [59]. Lower doses of 400 IU/day did not increase serum 25(OH)D levels and did not reduce 27HC levels, indicating that high vitamin D dose levels, but not the low dose, could have breast cancer-inhibitory effects. In a study of patients with aggressive B-cell lymphomas, patients were placed on chemoimmunotherapy along with an aggressive vitamin D loading phase of either one or two weeks of 25,000 IU daily and then a maintenance weekly dose of 25,000 IU [60]. Patients that achieved serum concentrations of >30 ng/ml 25(OH)D had a better event-free survival than those that did not.
Improvement in the quality of life of cancer patients receiving vitamin D supplementation has been documented in several studies. Patients with advanced or unresectable oral cancer had lower serum levels of 25(OH)D than healthy controls, but supplementation with twice daily 1,000 IU vitamin D increased the 25(OH)D levels [61]. These patients had reduced chemoradiation-related toxicities and greater improvement in the quality of life assessments (swallowing, pain and chewing difficulties) than those not receiving vitamin D. While not a tightly controlled study, similar types of results were found with esophageal cancer patients that self-reported to take vitamin D supplementation (200–400 IU daily over one year) following esophagectomy [62]. Despite the low dose of supplementation, patients taking vitamin D reported improved quality of life, including physical function, social functioning, fatigue, and appetite loss. In this study, the vitamin D supplementation also prolonged disease-free survival. In a matched control study of palliative care patients with various cancers, supplementation with 4,000 IU/day vitamin D improved the quality of life, diminished antibiotic use and the amount of opioid (fentanyl) used [63].
Not all studies have shown beneficial effects of vitamin D supplementation with cancer treatment. Vitamin D insufficient patients that were randomized to receive standard chemotherapy alone or also 2,000 IU vitamin D daily for 2 years were followed for almost 4 years [64]. No difference was seen in overall survival or progression-free survival. However, the authors stated that the absence of a vitamin D treatment effect could have been due to poor compliance and this study had no verifications of whether serum 25(OH)D levels were increased as a result of the supplementation.
Conclusion: possible reasons for variability among studies
While some studies have reported positive anticancer effects of vitamin D supplementation, others have shown no effect or even increased cancer risk. Reasons for such variability are multiple and often can be attributed to differences in study design. For example, studies have differed profoundly in the amounts of vitamin D being supplemented, which can range from levels in the hundreds of IUs to treatments in the tens of thousands of units [53, 60, 62]. The study designs also varied from vitamin D supplementation being self-reported to studies measuring increases in serum 25(OH)D levels [59, 65].
Baseline levels of serum 25(OH)D also impact on responsiveness to supplementation. A placebo-controlled randomized colorectal adenoma chemoprevention trial showed variability in how much serum 25(OH)D levels increased after supplementation with 1,000 IU vitamin D for one year [66]. The amount of increase was impacted by the starting serum 25(OH)D levels. Subjects with lower starting levels had greater proportional increases in serum 25(OH)D levels than those with higher baseline levels. A separate analysis of vitamin D supplementation trials showed that trials that stratified subjects, including cancer patients, by their serum 25(OH)D insufficiency or deficiency demonstrated vitamin D supplementation effects on mortality [67]. Thus, more rigorous analysis involving patient subpopulations may limit some of the differences among study results.
Study designs that focus on gender-selective cancers such as breast or prostate cancers inherently bring variability that may influence conclusions as to the effectiveness of vitamin D supplementation. This is not simply due to differences in cancer types. Studies have shown that responses to vitamin D supplementation can be affected by gender of the cancer patient. In response to vitamin D supplementation, increases in serum 25(OH)D levels were greater in females than in males [66]. In postmenopausal women, the result of vitamin D supplementation can be further affected by whether they are using menopausal hormone therapy [65]. Vitamin D supplementation (self-reported) decreased cancer risk in women that used hormone therapy. However, cancer risk increased in women that did not use menopausal hormone therapy, but only in women with a body mass index of less than 25 kg/m2. A greater BMI has separately been shown to temper the capacity of vitamin D supplementation to increase 25(OH)D levels. To achieve the same serum 25(OH)D levels, higher doses were needed for overweight (7,000 IU/day) and obese (8,000 IU/day) individuals than for normal weight (6,000 IU/day) individuals [68].
Assessments of whether or not vitamin D can reduce cancer risk also need to consider genotypes of vitamin D-associated genes. This was discussed at length above, but further supported by results of a randomized placebo-controlled study that showed vitamin D supplementation (1,000 IU/day) significantly reduced development of advanced colorectal adenomas in subjects with the VDR rs7968585 AA genotype, but increased the risk in those with AG or GG genotype [69].
Finally, it has to be acknowledged that not all cancer types or stages of cancer progression need to be influenced in the same way by vitamin D supplementation. While studies described in the preceding sections have examined how vitamin D supplementation impacts on risk of various cancers, there have not been strong analyses to determine which cancer types are more likely to be prevented or have better clinical outcome by vitamin D supplementation.
Acknowledgments
FUNDING
This work was supported by the Clinical Sciences Research and Development Program of the Department of Veterans Affairs (I01-CX000851).
Footnotes
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
REFERENCES
- 1.Cattaruzza MS, Pisani D, Fidanza L, Gandini S, Marmo G, Narcisi A, Bartolazzi A and Carlesimo M 2018, Eur. J. Cancer Prev, Epub 2018/02/14. [DOI] [PubMed] [Google Scholar]
- 2.Heidari Z, Nikbakht M, Mashhadi MA, Jahantigh M, Mansoumia N, Sheikhi V and Mansoumia MA 2017, Asian Pac. J. Cancer Prev, 18, 3419–3422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ismail A, El-Awady R, Mohamed G, Hussein M and Ramadan SS 2018, Asian Pac. J. Cancer Prev, 19, 571–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Takahashi H, Cornish AJ, Sud A, Law PJ, Kinnersley B, Ostrom QT, Labreche K, Eckel-Passow JE, Armstrong GN, Claus EB, Ll’yasova D, Schildkraut J, Bamholtz-Sloan JS, Olson SH, Bernstein JL, Lai RK, Schoemaker MJ, Simon M, Hoffmann P, Nothen MM, Jockel KH, Chanock S, Rajaraman P, Johansen C, Jenkins RB, Melin BS, Wrensch MR, Sanson M, Bondy ML, Turnbull C and Houlston RS 2018, Sci. Rep, 8, 2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Sullivan F, van Geffen J, van Weele M and Zgaga L 2018, Photochem. Photobiol, 94, 797–806. [DOI] [PubMed] [Google Scholar]
- 6.Budhathoki S, Hidaka A, Yamaji T, Sawada N, Tanaka-Mizuno S, Kuchiba A, Charvat H, Goto A, Kojima S, Sudo N, Shimazu T, Sasazuki S, Inoue M, Tsugane S and Iwasaki M 2018, B.M.J, 360, k671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yildirim O, Yildirim T, Seckin Y, Osanmaz P, Bilgic Y and Mete R 2017, Adv. Clin. Exp. Med, 26, 1377–1381. [DOI] [PubMed] [Google Scholar]
- 8.Xie DD, Chen YH, Xu S, Zhang C, Wang DM, Wang H, Chen L, Zhang ZH, Xia MZ, Xu DX and Yu DX 2017, Oncotarget, 8, 22076–22085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vayrynen JP, Mutt SJ, Herzig KH, Vayrynen SA, Kantola T, Karhu T, Karttunen TJ, Klintrup K, Makela J, Makinen MJ and Tuomisto A 2016, Sci. Rep, 6,36519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu Y, Wang X, Sun X, Lu S and Liu S 2018, Medicine, 97, e0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Feng Q, Zhang H, Dong Z, Zhou Y and Ma J 2017, Medicine, 96, e8613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hu MJ, Zhang Q, Liang L, Wang SY, Zheng XC, Zhou MM, Yang YW, Zhong Q and Huang F 2018, J. Endocrinol. Invest, Epub 2018/02/22. [DOI] [PubMed] [Google Scholar]
- 13.Liu J, Dong Y, Lu C, Wang Y, Peng L, Jiang M, Tang Y and Zhao Q 2017, Oncotarget, 8, 81040–81051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Supnick HT, Bunaciu RP and Yen A 2018, Oncotarget, 9, 9808–9824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Djurasinovic VT, Mihaljevic BS, Sipetic Grujicic SB, Ignjatovic SD, Trajkovic G, Todorovic-Balint MR, Antic DA, Bila JS, Andjelic BM, Jelicic JJ, Vukovic VM, Nikolic AM and Klek S 2018, Support. Care Cancer, 26,2825–2832. [DOI] [PubMed] [Google Scholar]
- 16.Seyedalipour F, Mansouri A, Vaezi M, Gholami K, Heidari K, Hadjibabaie M and Ghavamzadeh A 2017, Int. J. Hematol. Oncol. Stem Cell Res, 11, 209–216. [PMC free article] [PubMed] [Google Scholar]
- 17.Cheney CP, Thorand B, Huth C, Berger K, Peters A, Seifert-Klauss V, Kiechle M, Strauch K and Quante AS 2018, Oncol. Res. Treat, 41, 117–121. [DOI] [PubMed] [Google Scholar]
- 18.van Duijnhoven FJB, Jenab M, Hveem K, Siersema PD, Fedirko V, Duell EJ, Kampman E, Halfweeg A, van Kranen HJ, van den Ouweland JMW, Weiderpass E, Murphy N, Langhammer A, Ness-Jensen E, Olsen A, Tjonneland A, Overvad K, Cadeau C, Kvaskoff M, Boutron-Ruault MC, Katzke VA, Kuhn T, Boeing H, Trichopoulou A, Kotanidou A, Kritikou M, Palli D, Agnoli C, Tumino R, Panico S, Matullo G, Peeters P, Brustad M, Olsen KS, Lasheras C, Obon-Santacana M, Sanchez MJ, Dorronsoro M, Chirlaque MD, Barricarte A, Manjer J, Almquist M, Renstrom F, Ye W, Wareham N, Khaw KT, Bradbury KE, Freisling H, Aune D, Norat T, Riboli E and Buenode-Mesquita HBA 2018, Int. J. Cancer, 142, 1189–1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muller DC, Hodge AM, Fanidi A, Albanes D, Mai XM, Shu XO, Weinstein SJ, Larose TL, Zhang X, Han J, Stampfer MJ, Smith-Wamer SA, Ma J, Gaziano JM, Sesso HD, Stevens VL, McCullough ML, Layne TM, Prentice R, Pettinger M, Thomson CA, Zheng W, Gao YT, Rothman N, Xiang YB, Cai H, Wang R, Yuan JM, Koh WP, Butler LM, Cai Q, Blot WJ, Wu J, Ueland PM, Midttun O, Langhammer A, Hveem K, Johansson M, Hultdin J, Grankvist K, Arslan AA, Le Marchand L, Severi G, Johansson M and Brennan P 2018, Ann. Oncol, 29, 1468–1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bryce C 2018, Mil. Med, 183, 547–551. [DOI] [PubMed] [Google Scholar]
- 21.Gao J, Wei W, Wang G, Zhou H, Fu Y and Liu N 2018, Ther. Clin. Risk Manag, 14, 95–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bao Y, Zhang S, Guo Y, Wei X, Zhang Y, Yang Y, Zhang H, Ma M and Yang W 2018, Clin. Transl. Oncol, 2018/02/10. [DOI] [PubMed] [Google Scholar]
- 23.Kang S, Zhao Y, Wang L, Liu J, Chen X, Liu X, Shi Z, Gao W and Cao F 2018, Oncotarget, 9, 7136–7147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pan Z, Chen M, Hu X, Wang H, Yang J, Zhang C, Pan F and Sun G 2018, Oncotarget, 9, 13068–13076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mi YY, Chen YZ, Chen J, Zhang LF, Zuo L and Zou JG 2017, Arch. Med. Sci, 13, 1449–1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen H and Zhu J 2018, J. Obstet. Gynaecol. Res, 44, 556–565. [DOI] [PubMed] [Google Scholar]
- 27.Cusato J, Boglione L, De Nicolo A, Favata F, Ariaudo A, Momese Pinna S, Guido F, Avataneo V, Cantu M, Carcieri C, Cariti G, Di Perri G and D’Avolio A 2018, Cancer Chemother. Pharmacol, 81, 615–620. [DOI] [PubMed] [Google Scholar]
- 28.Iqbal MUN, Maqbool SA and Khan TA 2018, J. Int. Med. Res, 46, 1801–1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O’Brien KM, Sandler DP, Kinyamu HK, Taylor JA and Weinberg CR 2017, Cancer Epidemiol. Biomarkers Prev, 26, 1761–1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chun RF, Peercy BE, Orwoll ES, Nielson CM, Adams JS and Hewison M 2014, J. Steroid. Biochem. Mol. Biol, 144 Pt A, 132–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang TJ, Zhang F, Richards JB, Kestenbaum B, van Meurs JB, Berry D, Kiel DP, Streeten EA, Ohlsson C, Koller DL, Peltonen L, Cooper JD, O’Reilly PF, Houston DK, Glazer NL, Vandenput L, Peacock M, Shi J, Rivadeneira F, McCarthy MI, Anneli P, de Boer IH, Mangino M, Kato B, Smyth DJ, Booth SL, Jacques PF, Burke GL, Goodarzi M, Cheung CL, Wolf M, Rice K, Goltzman D, Hidiroglou N, Ladouceur M, Wareham NJ, Hocking LJ, Hart D, Arden NK, Cooper C, Malik S, Fraser WD, Hartikainen AL, Zhai G, Macdonald HM, Forouhi NG, Loos RJ, Reid DM, Hakim A, Dennison E, Liu Y, Power C, Stevens HE, Jaana L, Vasan RS, Soranzo N, Bojunga J, Psaty BM, Lorentzon M, Foroud T, Harris TB, Hofman A, Jansson JO, Cauley JA, Uitterlinden AG, Gibson Q, Jarvelin MR, Karasik D, Siscovick DS, Econs MJ, Kritchevsky SB, Florez JC, Todd JA, Dupuis J, Hypponen E and Spector TD 2010, Lancet, 376, 180–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li LH, Yin XY, Wu XH, Zhang L, Pan SY, Zheng ZJ and Wang JG 2014, Endocr. J, 61, 133–41. [DOI] [PubMed] [Google Scholar]
- 33.Huss L, Butt ST, Almgren P, Borgquist S, Brandt J, Forsti A, Melander O and Manjer J 2018, Breast Cancer Res, 20, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O’Brien KM, Sandler DP, Shi M, Harmon QE, Taylor JA and Weinberg CR 2018, Front. Genet, 9, 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Muindi JR, Adjei AA, Wu ZR, Olson I, Huang H, Groman A, Tian L, Singh PK, Sucheston LE, Johnson CS, Trump DL and Fakih MG 2013, Horm. Cancer, 4, 242–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhu Y, Wang PP, Zhai G, Bapat B, Savas S, Woodrow JR, Campbell PT, Li Y, Yang N, Zhou X, Dicks E, McLaughlin JR and Parfrey PS 2018, BMC Cancer, 18, 155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Trummer O, Langsenlehner U, Krenn-Pilko S, Pieber TR, Obermayer-Pietsch B, Gerger A, Renner W and Langsenlehner T 2016, World J. Urol, 34, 607–11. [DOI] [PubMed] [Google Scholar]
- 38.Kong J, Xu F, Qu J, Wang Y, Gao M, Yu H and Qian B 2015, Oncotarget, 6,2573–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Berger MD, Stintzing S, Heinemann V, Cao S, Yang D, Sunakawa Y, Matsusaka S, Ning Y, Okazaki S, Miyamoto Y, Suenaga M, Schirripa M, Hanna DL, Soni S, Puccini A, Zhang W, Cremolini C, Falcone A, Loupakis F and Lenz HJ 2018, Clin. Cancer Res, 24, 784–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ong JS, Cuellar-Partida G, Lu Y, Fasching PA, Hein A, Burghaus S, Beckmann MW, Lambrechts D, Van Nieuwenhuysen E, Vergote I, Vanderstichele A, Anne Doherty J, Anne Rossing M, Chang-Claude J, Eilber U, Rudolph A, Wang-Gohrke S, Goodman MT, Bogdanova N, Dork T, Durst M, Hillemanns P, Runnebaum IB, Antonenkova N, Butzow R, Leminen A, Nevanlinna H, Pelttari LM, Edwards RP, Kelley JL, Modugno F, Moysich KB, Ness RB, Cannioto R, Hogdall E, Hogdall CK, Jensen A, Giles GG, Bruinsma F, Kjaer SK, Hildebrandt MA, Liang D, Lu KH, Wu X, Bisogna M, Dao F, Levine DA, Cramer DW, Terry KL, Tworoger SS, Stampfer M, Missmer S, Bjorge L, Salvesen HB, Kopperud RK, Bischof K, Aben KK, Kiemeney LA, Massuger LF, Brooks-Wilson A, Olson SH, McGuire V, Rothstein JH, Sieh W, Whittemore AS, Cook LS, Le ND, Gilks CB, Gronwald J, Jakubowska A, Lubinski J, Kluz T, Song H, Tyrer JP, Wentzensen N, Brinton L, Trabert B, Lissowska J, McLaughlin JR, Narod SA, Phelan C, Anton-Culver H, Ziogas A, Eccles D, Campbell I, Gayther SA, Gentiy-Maharaj A, Menon U, Ramus SJ, Wu AH, Dansonka-Mieszkowska A, Kupryjanczyk J, Timorek A, Szafron L, Cunningham JM, Fridley BL, Winham SJ, Bandera EV, Poole EM, Morgan TK, Risch HA, Goode EL, Schildkraut JM, Pearce CL, Berchuck A, Pharoah PD, Chenevix-Trench G, Gharahkhani P, Neale RE, Webb PM and MacGregor S 2016, Int. J. Epidemiol, 45, 1619–1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pibiri F, Kittles RA, Sandler RS, Keku TO, Kupfer SS, Xicola RM, Llor X and Ellis NA 2014, Cancer Causes Control, 25, 561–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jacobs ET, Van Pelt C, Forster RE, Zaidi W, Hibler EA, Galligan MA, Haussler MR and Jurutka PW 2013, Cancer Res, 73, 2563–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhu M, Qiu S, Zhang X, Wang Y, Souraka TDM, Wen X, Liang C and Tu J 2018, Pathol. Res. Pract, 214, 53–63. [DOI] [PubMed] [Google Scholar]
- 44.Ge N, Chu XM, Xuan YP, Ren DQ, Wang Y, Ma K, Gao HJ and Jiao WJ 2017, Oncol. Lett, 14, 7538–7544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lin VC, Huang SP, Ting HJ, Ma WL, Yu CC, Huang CY, Yin HL, Huang TY, Lee CH, Chang TY, Lu TL and Bao BY 2017, Oncotarget, 8, 74119–74128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chandler PD, Tobias DK, Wang L, Smith-Wamer SA, Chasman DI, Rose L, Giovannucci EL, Buring JE, Ridker PM, Cook NR, Manson JE and Sesso HD 2018, Nutrients, 10,55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhang Q, Liu S, Ge D, Cunningham DM, Huang F, Ma L, Burris TP and You Z 2017, Prostate, 77, 888–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Akbay EA, Koyama S, Liu Y, Dries R, Bufe LE, Silkes M, Alam MM, Magee DM, Jones R, Jinushi M, Kulkami M, Carretero J, Wang X, Wamer-Hatten T, Cavanaugh JD, Osa A, Kumanogqh A, Freeman GJ, Awad MM, Christiani DC, Bueno R, Hammerman PS, Dranoff G and Wong KK 2017, J. Thorac. Oncol, 12, 1268–1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Miura K, Ishioka M, Minami S, Horie Y, Ohshima S, Goto T and Ohnishi H 2016, J. Biol. Chem, 291, 11504–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kavanagh ME, Conroy MJ, Clarke NE, Gilmartin NT, O’Sullivan KE, Feighery R, MacCarthy F, O’Toole D, Ravi N, Reynolds JV, O’Sullivan J and Lysaght J 2016, Cancer Lett, 370, 117–24. [DOI] [PubMed] [Google Scholar]
- 51.Gorman S, Geldenhuys S, Weeden CE, Grimbaldeston MA and Hart PH 2018, Arch. Dermatol. Res, 310, 221–230. [DOI] [PubMed] [Google Scholar]
- 52.Mousa A, Naderpoor N, Teede H, Scragg R and de Courten B 2018, Nutr. Rev, 76, 380–394. [DOI] [PubMed] [Google Scholar]
- 53.Vahedpoor Z, Jamilian M, Bahmani F, Aghadavod E, Karamali M, Kashanian M and Asemi Z 2017, Horm. Cancer, 8, 58–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Crockett SD, Barry EL, Mott LA, Ahnen DJ, Robertson DJ, Anderson JC, Wallace K, Burke CA, Bresalier RS, Figueiredo JC, Snover DC and Baron JA 2018, Gut, Epub 2018/03/03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hardiman G, Savage SJ, Hazard ES, Wilson RC, Courtney SM, Smith MT, Hollis BW, Halbert CH and Gattoni-Celli S 2016, Pharmacogenomics, 17, 1129–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Marshall DT, Savage SJ, Garrett-Mayer E, Keane TE, Hollis BW, Horst RL, Ambrose LH, Kindy MS and Gattoni-Celli S 2012, J. Clin. Endocrinol. Metab, 97, 2315–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kulbersh JS, Day TA, Gillespie MB and Young MR 2009, Otolaryngol. Head Neck Surg, 140, 235–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Walsh JE, Clark AM, Day TA, Gillespie MB and Young MR 2010, Hum. Immunol, 71, 659–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Going CC, Alexandrova L, Lau K, Yeh CY, Feldman D and Pitteri SJ 2018, Breast Cancer Res. Treat, 167, 797–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hohaus S, Tisi MC, Bellesi S, Maiolo E, Alma E, Tartaglia G, Corrente F, Cuccaro A, D’Alo F, Basile U, Larocca LM and De Stefano V 2018, Cancer Med, 7,270–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Anand A, Singh S, Sonkar AA, Husain N, Singh KR, Singh S and Kushwaha JK 2017, Contemp. Oncol, 21, 145–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang L, Wang C, Wang J, Huang X and Cheng Y 2016, Sci. Rep, 6, 38962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Helde-Frankling M, Hoijer J, Bergqvist J and Bjorkhem-Bergman L 2017, PLoS One, 12, eO 184208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Antunac Golubic Z, Barsic I, Librenjak N and Plestina S 2018, Nutr. Cancer, 70, 413–417. [DOI] [PubMed] [Google Scholar]
- 65.Cadeau C, Fournier A, Mesrine S, Clavel-Chapelon F, Fagherazzi G and Boutron-Ruault MC 2016, Int. J. Cancer, 139, 2193–200. [DOI] [PubMed] [Google Scholar]
- 66.Rees JR, Mott LA, Barry EL, Baron JA, Bostick RM, Figueiredo JC, Bresalier RS, Robertson DJ and Peacock JL 2016, J. Nutr, 146, 2312–2324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Brenner H, Jansen L, Saum KU, Holleczek B and Schottker B 2017, J. Nutr, 147, 1325–1333. [DOI] [PubMed] [Google Scholar]
- 68.Kimball SM, Mirhosseini N and Holick MF 2017, Dermatoendocrinol, 9, el300213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Barry EL, Peacock JL, Rees JR, Bostick RM, Robertson DJ, Bresalier RS and Baron JA 2017, J.A.M.A. Oncol, 3, 628–635. [DOI] [PMC free article] [PubMed] [Google Scholar]