Abstract
HIV-positive rural individuals carry a 1.3 times greater risk of a depressive diagnosis than their urban counterparts. This randomized clinical trial tested whether telephone-administered interpersonal psychotherapy (tele-IPT) acutely relieved depressive symptoms in 132 HIV-infected rural persons from 28 states diagnosed with DSM-IV Major Depressive Disorder (MDD), partially remitted MDD, or Dysthymic Disorder. Patients were randomized to either 9 sessions of one-on-one tele-IPT (n=70) or standard care (SC; n=62). A series of intent-to-treat (ITT), therapy completer, and sensitivity analyses assessed changes in depressive symptoms, interpersonal problems, and social support from pre- through post-intervention. Across all analyses, tele-IPT patients reported significantly lower depressive symptoms and interpersonal problems than SC controls; 22% of tele-IPT patients were categorized as a priori “responders” who reported ≥50% reductions in depressive symptoms compared to only 4% of SC controls in ITT analyses. Brief tele-IPT acutely decreased depressive symptoms and interpersonal problems in depressed rural people living with HIV.
Keywords: HIV, rural, teletherapy, IPT, depression
INTRODUCTION
At the end of 2013, roughly 51,000 persons living with HIV (PLWH) lived in non-metropolitan areas of the United States (communities of 50,000 residents or fewer), accounting for 6% of all HIV/AIDS cases.1 HIV prevalence rates in rural areas will increase for two reasons. First, increasingly efficacious ART regimens will extend survival for many rural PLWH.2 Second, many rural PLWH (33 to 50%) engage in high HIV transmission risk behaviors that further spread HIV in rural areas.3,4
Several urban-rural differences complicate efforts to improve life quality in rural PLWH. Compared to their urban counterparts, rural PLWH confront a shortage of mental health care professionals experienced in providing HIV care, fewer social supports, reduced access to public and private transportation, and more HIV-related stigma from community members.5,6 Perhaps unsurprisingly, a greater mortality rate was reported over a 10-year period in rural (10.4%) than urban (6.0%) PLWH.7
Rural PLWH evince a higher rate of depression than urban PLWH. Sheth et al.8 compared depression prevalence rates between urban and rural PLWH presenting at the Dartmouth-Hitchcock HIV Program. Using a retrospective cohort design and Rural-Urban Commuting Area (RUCA) Scores,9 they categorized patients as living in small towns/rural (n=185), micropolitan (n=145), or metropolitan (n=316) areas. Depression rates were highest in rural areas (60%) followed by micropolitan (52%) and metropolitan areas (41%), with rural PLWH 1.3 times more likely to receive a depression diagnosis than their metropolitan counterparts.
High depression rates in rural PLWH are troubling because depression in PLWH is associated with poor antiretroviral therapy (ART) adherence, impaired daily functioning, poor engagement and retention in care, more comorbid health conditions, and the continued practice of risky sexual behaviors.10–14 That rural PLWH are less likely to have seen a mental health provider over the past year and make fewer visits to mental health professionals15 than urban PLWH makes high depression rates in rural PLWH all the more worrisome.
Despite the need for mental health treatments for rural PLWH, mental health treatment shortages and geographic barriers preclude many rural PLWH from accessing and receiving treatment. Ninety-six percent of all U.S. households have traditional landline and/or cellular telephones,16 which can provide practical treatment administration routes for depressed rural PLWH. Teletherapy overcomes geographic distances separating patients and practitioners, maximizes confidentiality (e.g., teletherapy spares the patient from publicly, physically entering a mental health venue), and provides emotional and informational supports to geographically-remote individuals.17 Teletherapy has considerable depression treatment efficacy. Mohr et al.’s18 meta-analysis found significant reductions in depressive symptoms across all assessment periods for patients enrolled in telephone-administered psychotherapy compared to standard care (SC) controls (d = .26); even greater reductions emerged when analyses were limited to changes from pre- to post-intervention (d = .82).
A few studies have examined the efficacy of teletherapy to treat rural PLWH, but their results are inconclusive. Heckman et al.19 treated 299 rural PLWH recruited in 13 states and found that neither 8 sessions of telephone-administered coping effectiveness group training nor 8 sessions of information-support group training reduced depressive symptoms. Ransom et al.20 pilot-tested whether brief tele-IPT reduced psychiatric distress in 79 rural PLWH. Patients received either SC (n=38) or six sessions of tele-IPT plus SC (n=41). Tele-IPT patients evinced significantly greater reductions in depressive symptoms and overall levels of psychiatric distress from pre- through post-intervention than SC controls; one-third of tele-IPT patients reported clinically-meaningful reductions in psychiatric distress.
Based on Ransom et al.’s promising pilot RCT,20 we conducted a more comprehensive RCT using a larger and more geographically-diverse sample to test tele-IPT’s efficacy to relieve depressive symptoms in rural PLWH diagnosed with unipolar depression. IPT is a time-limited, diagnosis-targeted psychotherapy that focuses on one’s feelings in an interpersonal context and enhancing interpersonal skills.21 IPT helps patients resolve their depressive symptoms by linking a current interpersonal crisis to the patient’s depressive episode. By helping patients to resolve that crisis, tele-IPT helps the patient gain a sense of mastery over an oppressive environment, relieve depressive symptoms, and improve his or her life.
This RCT evaluated the efficacy of tele-IPT to reduce depressive symptoms in 132 HIV-infected persons living in rural U.S. areas. Patients completed surveys at pre-intervention, post-intervention, and 4- and 8-month follow-up assessing depressive symptoms (primary outcome), interpersonal problems (secondary outcome), and social support (secondary outcome). Analyses in this report examined only acute changes (from pre- through post-intervention) in depressive symptoms, interpersonal problems, and social support, as follow-up data collection is ongoing. We hypothesized that (i) tele-IPT patients would report greater reductions in depressive symptoms and interpersonal problems and increases in social support than SC controls, and (ii) a significantly greater proportion of tele-IPT patients would respond favorably to treatment (i.e., depressive symptom relief ≥50%) than SC controls.
METHOD
Patients and Procedures
Between August 2010 and September 2014, AIDS service organizations (ASOs) in 28 states distributed recruitment brochures to their HIV-infected rural clients through face-to-face interactions, regular mail, and placement of study brochures in “high-traffic” areas of their facilities. The Rural Center for AIDS Prevention (RCAP) at Indiana University distributed study advertisements through its listserv and publicized the study on its website. Patients were from the states of Alabama, Arkansas, California, Colorado, Florida, Georgia, Illinois, Indiana, Kansas, Kentucky, Louisiana, Maine, Minnesota, Mississippi, Missouri, Montana, New Hampshire, New York, North Carolina, Ohio, Oklahoma, Oregon, Pennsylvania, South Carolina, Tennessee, Texas, Vermont and Virginia. The IRBs of all participating institutions approved the project’s protocol and all patients provided written informed consent. No adverse events were reported during the trial.
Potential participants contacted the research office via a toll-free telephone number or a project-specific e-mail address listed in recruitment materials. During this contact, research staff provided detailed information about the study, described the informed consent process, and gathered preliminary screening information, such as current age, county of residence, and contact information. County of residence was used to determine the individual’s U.S. Department of Agriculture’s Urban-Rural Continuum Code.9 If the individual satisfied the rurality inclusion criterion and expressed interest in the study, study personnel mailed (or e-mailed) an informed consent form to the individual to be signed and returned to the research office. After receiving the signed consent document, research staff contacted the individual and conducted an eligibility screening, which generally took less than 30 minutes to complete. Telephone-based eligibility interviews administered the Primary Care Evaluation of Mental Disorders (PRIME-MD)22 and the Modified Mini Mental State Examination (3MS).23
Inclusion and exclusion criteria.
Inclusion criteria were: (1) ≥18 years of age; (2) self-reported diagnosis of HIV infection or AIDS; (3) residing in a county with U.S. Department of Agriculture Rural-Urban Continuum Code of “4” through “9”; (4) diagnosis of DSM-IV Major Depressive Disorder (MDD), MDD in Partial Remission, or Dysthymic Disorder based on the Mood Module of the PRIME-MD; (5) the patient intended to stay in his or her current residence for ≥1 year; and (6) written informed consent. This study enrolled rural PLWH who received a unipolar mood disorder diagnosis (not self-reported elevated depressive symptoms) because: (1) IPT was developed specifically for individuals diagnosed with mood disorders; (2) HIV manifestation and medication side effects can mimic somatic symptoms of depression (interviews differentiated these symptoms); and (3) an actual depressive diagnosis had been an inclusion criterion in the pilot RCT.20
The sole exclusion criterion was serious cognitive or neuropsychiatric impairment based on the telephone-administered version of the 3MS (scores < 70). Individuals were not excluded on the basis of alcohol or substance use disorders, active bipolar disorder, psychotic symptoms, or current receipt of psychotherapy or pharmacotherapy in order to assemble a sample high in external validity.
Assessment
Patients were mailed a self-administered, pre-intervention assessment and self-addressed postage-paid envelope to return it. Patients completed the survey in the privacy of their home. Patients were compensated $40 for completing the pre-intervention assessment and an additional $40 for the post-intervention assessment, which tele-IPT patients self-administered immediately after their final intervention session. SC controls completed post assessments coincident with their time-matched tele-IPT counterparts. Measures used in intervention-outcome analyses are described below. All Cronbach alphas and test-retest reliability coefficients (rtt) are based on current study data. Test-retest coefficients were calculated using pre- and post-intervention data from SC controls who were expected to report few, if any, changes.
Beck Depression Inventory (BDI-II).24
For the study’s primary outcome, the 21-item BDI-II assessed cognitive, affective, and somatic symptoms of clinical depression during the past week. Self-report responses made along four severity levels (“0” to “3”) yielded a total score from 0 to 63. Outcome analyses focused on depressive symptoms because depression is the most common psychiatric condition in PLWH25 and PLWH who report more depressive symptoms also report greater fatigue, more rapid decreases in CD4 T-cells, more rapid increases in viral load, and higher mortality risk.13,26 The BDI demonstrated good internal consistency (α=.86) and test-retest reliability, rtt(61) = .82, p< .001.
Inventory of Interpersonal Problems (IIP).27
As a secondary outcome, the 64-item, self-administered IIP assessed severity levels of interpersonal problems. Its 5-point scale (0=“Not at all” to 4 “Extremely”) describes experiences with a range of interpersonal problems. Total IIP scores summate the 64 items. The IIP demonstrated excellent internal consistency (α=.93) and test-retest reliability, rtt(61)=.81, p< .001 and has shown responsiveness to change in previous IPT treatments.28
Provision of Social Relations Scale (PSRS).29
As a secondary outcome, the 15-item PSRS assessed perceived social support from family members and friends, with each item using a 5-point Likert scale. The PSRS demonstrated good internal consistency (α=.86) and test-retest reliability, rtt (62) = .77, p< .001.
Mental Health and Substance Use Services Utilization.
Patients indicated if, over the past month, they participated (yes/no) in self-help groups for problems related to mental health or alcohol/drug use (e.g., AIDS specific support groups or 12-step programs). Patients also specified if they sought help from any of the following practitioners in the past year for problems related to mental health or alcohol/drug use (yes/no) and how long ago they sought help: psychiatrist; psychologist; social worker; counselor; minister/priest/rabbi; or psychiatric nurse. Patients also indicated if they used a hotline (yes/no) for problems related to mental health or alcohol/drug use in the past month.
Demographic Characteristics.
Patients self-reported their age, gender, education, employment status, annual income, relationship status, sexual self-identity, HIV symptom severity, and HIV/AIDS status. The study did not collect data to assess patients’ immunologic functioning (e.g., CD4 cell count or HIV viral load).
Intervention Conditions
After completing pre-intervention surveys, patients were assigned to one of two conditions using a randomization module in Microsoft EXCEL. A priori power analyses, informed by data from our previous rural PLWH research,20 showed that 70 patients per study arm would yield power >.85 for clinically significant reductions in BDI-II depression scores, the study’s primary outcome.
Standard Care (SC) Control.
SC controls received no active study treatment but had access to community-based support services available to PLWH (e.g., AIDS-related support groups, 12-step programs, individual therapy, prescribed antidepressant medications). No limitations were imposed on patients’ use of psychosocial services outside of the RCT. Their use of these services was documented during the study.
Tele-Interpersonal Psychotherapy (tele-IPT) + SC.
Tele-IPT + SC patients received nine weekly, one-hour telephone IPT treatments (adapted from the “Manual for Interpersonal Therapy with Depressed HIV-Seropositive Patients”).30 Sessions 1 and 2 consisted of patient-therapist introductions and an overview of therapy protocol. Teletherapists and patients also explored patients’ depressive symptoms, discussed the nature of depression, reviewed current interpersonal relationships, and identified a problem relationship or circumstance that served as the therapeutic focus for the remainder of treatment. Therapists framed each patient’s primary interpersonal concern using one of four focal areas: interpersonal role dispute (e.g., conflict with partner); role transition (e.g., loss of employment, moving from an urban to a rural environment); grief (death of loved one); or interpersonal sensitivities (chronic difficulties forming or maintaining close relationships). Sessions 3 through 9 addressed the problematic relationship/issue identified in Sessions 1 and 2. Sessions 8 and 9 addressed issues of therapy termination and maintenance of treatment gains.
Tele-IPT patients used the following protocol during therapy: (1) a private, television- and computer-free location was preferred for therapy; (2) weekly therapy sessions scheduled at times when no interruptions were anticipated; (3) avoidance of call waiting, except in possible emergency situations; (4) avoiding teletherapy via cellphone while driving; (5) when possible, using traditional land-line telephones to reduce likelihood of “dropped” calls; (6) avoiding use of the speakerphone feature; and (7) if using a cell phone, ensuring a fully charged battery.
Therapist Training and Supervision
Prior to initiating the RCT, John Markowitz, M.D., an IPT clinical trials expert21 and architect of IPT for PLWH, conducted a two-day in-person training session with teletherapists, all of whom were PhD-level psychologists and many of whom had considerable teletherapy experience. This was the only formal training offered to teletherapists; no additional centralized or formal trainings were conducted after initiating the RCT, as would likely be the case when administered by clinical or community health professionals. Following the initial training, each teletherapist was e-mailed a tele-IPT intervention manual for review prior to conducting teletherapy. Similar to patients, teletherapists were located in various regions of the United States. This study purposely employed this minimal instruction approach because, in all likelihood, this is how many manualized teletherapies are (and will be) disseminated through practitioners in community settings. This approach also enhanced the external validity of the tele-IPT treatment and arguably made this study a hybrid efficacy-effectiveness trial.
Teletherapists participated in monthly telephone-based supervision conference calls. Monthly tele-supervision provided therapists with opportunities to discuss their administration of tele-IPT, any clinical concerns they had, and helped to verify and increase treatment fidelity. At the completion of each tele-IPT session, therapists completed a “Therapy Content Checklist” to enhance treatment fidelity. All teletherapy sessions were digitally audio recorded and reviewed by study team members to ensure fidelity to intervention protocol.
Patient Flow
Patients were recruited in waves of 2, 4, or 6 and randomly assigned to condition using an algorithm that ensured equal cell sizes. Teletherapists were blinded to patients’ pre-intervention data and the investigator who conducted the randomization was blinded to patients’ eligibility screening and pre-intervention data.
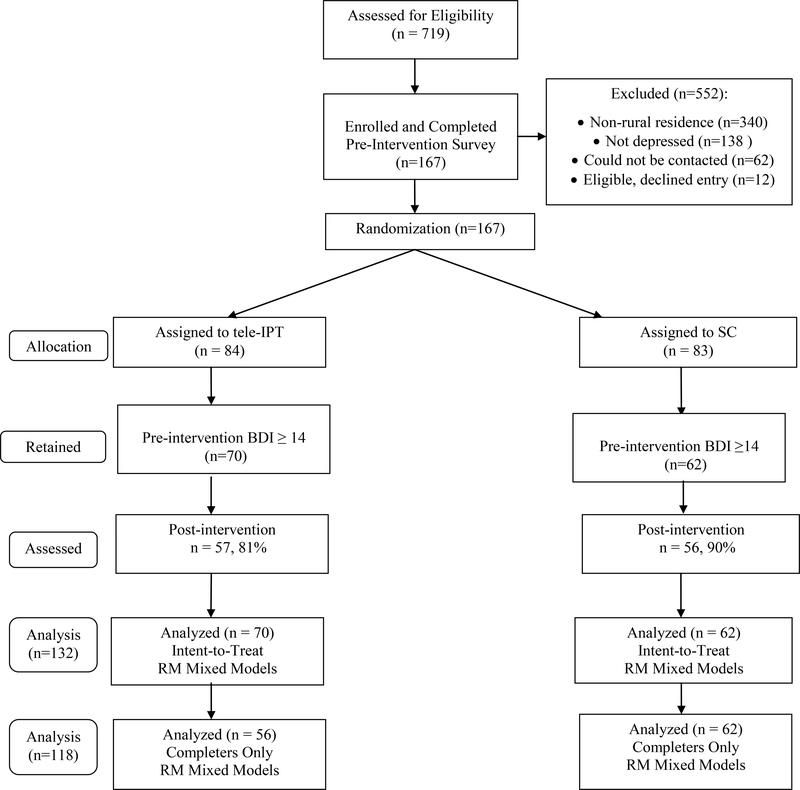
Figure 1 shows that 719 individuals made telephone or e-mail inquiries about the study. Of these, 379 satisfied the rural-residence criterion, 305 of whom returned completed informed consent forms. Of the 305 individuals who completed eligibility screenings, 138 did not satisfy the depression-related inclusion criteria. Ultimately, 167 individuals satisfied inclusion and exclusion criteria and were assigned to a study arm.
Figure 1.
Patient Flow Chart Following the Guidelines of the Consolidated Standards of Reporting Trials. SC = Standard Care;
While all patients were diagnosed with a PRIME-MD-based depressive disorder in eligibility screenings, 35 patients (14 tele-IPT and 21 SC controls) had pre-intervention BDI values <14, the threshold for mild depressive disorder.24 To minimize the possibility of a “floor effect” in intervention outcome analyses, and because assessing the efficacy of tele-IPT with non-depressed individuals has questionable utility, these patients were excluded from outcome analyses, yielding 132 intent-to treat and 118 therapy completer patients (i.e., patients who completed all nine teletherapy sessions). Eighty-six percent of patients (113/132) completed post-intervention assessments.
Data Analysis
Chi-squared tests of association and one-way ANOVA compared demographic, clinical, clinical services utilization, and BDI, IIP, and PSRS values between study arms at pre-intervention and compared patients who completed post-intervention assessments to those who did not. Regression analyses examined the relationship between number of teletherapy sessions attended and pre-intervention BDI values. ANOVA compared depressive symptoms and perceptions of social support by Rural Urban Continuum Code to determine if depression and social support varied by rurality and if rurality should be considered in intervention-outcome analyses.
Outcomes were assessed between the two conditions using intent-to-treat (N=132) and completer-only (N=118) approaches for patients with pre-intervention BDI values ≥14. Intent-to-treat analyses used data from all patients with pre-intervention BDI values ≥14, regardless of number of teletherapy sessions attended. Completer-only analyses used data from tele-IPT patients who attended all nine teletherapy sessions as well as all standard care controls. Linear mixed effect repeated measurement (MMRM) approaches with regression-based multiple imputation for missing data31 utilized all data available for outcome analyses of depressive symptoms, interpersonal difficulties, and social support. Sensitivity analyses were conducted using data from all 167 patients enrolled regardless of pre-intervention BDI values using an intent-to-treat approach and multiple imputation for missing data. Because the sample contained male and female patients, additional analyses tested if “Gender” moderated intervention outcomes. Inferential analyses used 2-tailed tests of significance at α=.05.
The clinical meaningfulness of depressive symptom reductions was assessed using Bengtson et al.’s methodology,32 which categorizes therapy response a priori as: (1) “Responder”: ≥50% reduction in depressive symptoms from pre- through post-intervention; (2) “Partial Responder”: 25–49% reduction; and (3) “Non-Responder”: <25% reduction. Chi-squared analyses assessed the association between study arm and treatment response category. Effect sizes (Cohen’s “d”) were calculated to complement statistical significance testing and used the traditional cutoffs, small=0.2, medium=0.5, and large=0.8.
RESULTS
Study Cohort
Patients (N=132) were, on average, 51.9 years of age, Caucasian (75%), diagnosed with AIDS (57%), and gay/bisexual self-identified (54%; see Table 1). The modal patient (36%) lived in a county with a population of 2,500 to 19,999 that was adjacent to a metropolitan area. The mean pre-intervention BDI value was 26.6 (SD = 9.4). No difference by treatment condition emerged on any pre-intervention variable.
Table 1.
Demographic, clinical, and psychiatric characteristics at pre-intervention by study arm (Mean ± SD or % [n]); Pre-Intervention BDI ≥ 14
|
Variable |
Overall Sample (N=132) |
tele-IPT (n=70) |
Standard Care (n=62) |
|---|---|---|---|
| Age | 51.9 ± 10.3 | 51.1 ± 9.4 | 52.9 ± 10.3 |
| Male | 63% (83) | 67% (47) | 57% (36) |
| Self-Identify Gay/Bisexual | 54% (71) | 59% (41) | 49% (30) |
| Caucasian | 75% (99) | 78% (55) | 74% (44) |
| Years of Education | 13.1 ± 2.1 | 13.1 ± 2.0 | 13.2 ± 2.1 |
| Annual Income ≤ $20,000 | 88% (116) | 89% (62) | 87% (54) |
| On Social Security/Disability | 68% (90) | 66% (46) | 71% (44) |
| Years Living with HIV | 17.7 ± 7.7 | 17.2 ± 7.6 | 18.3 ± 7.8 |
| Progressed to AIDS | 57% (75) | 58% (41) | 56% (34) |
| Bipolar Disorder Diagnosis | 27% (36) | 29% (20) | 25% (16) |
| Prescribed Anti-Depressant | 62% | 63% | 62% |
| Prescribe Anxiolytic | 41% | 44% | 37% |
| Sought Treatment from Practitioner (e.g., Psychiatrist), Past Year | 40% | 41% | 40% |
| Used Hotline for Assistance, Past Month | 7% (9) | 10% (7) | 3% (2) |
| Attended Self-Help Group, Past Month | 18% (24) | 23% (16) | 13% (8) |
| BDI Value at Baseline | 26.6 ± 9.4 | 26.3 ± 8.3 | 26.9 ± 10.5 |
| PSRS Value at Pre-Intervention | 40.8 ± 9.3 | 40.9 ± 8.8 | 40.7 ± 9.8 |
| IIP Value at Pre-Intervention | 100.9 ± 33.1 | 104.3 ± 33.9 | 97.1 ± 31.9 |
The vast majority of patients (81%) were diagnosed with Major Depressive Disorder, the remainder with either Partial Remission of MDD or Dysthymic Disorder. In addition to being diagnosed with depression, patients self-reported other psychiatric conditions with which they had been diagnosed at the time of study enrollment. Fifteen patients (9 IPT, 6 controls) self-reported the following comorbid psychiatric conditions: “post-traumatic stress disorder,” “dissociative disorder,” “borderline personality disorder,” “schizoaffective disorder,” “schizophrenia,” and “chronic depression with psychotic features.”
As shown in Table 1, patients’ use of psychotropic medications and supportive mental health services did not differ between conditions (all ps > .10). Comparable proportions of tele-IPT (63%) and controls (62%) reported taking prescribed anti-depressant medications and similar proportions of tele-IPT (44%) and controls (37%) reported taking prescribed anti-anxiety medications. Comparable proportions of tele-IPT (29%) and SC controls (25%) reported having received a diagnosis of bipolar disorder or taking medications for bipolar disorder. Comparable proportions of tele-IPT (41%) and SC controls (40%) had sought treatment from a practitioner for treatment of mental health or alcohol/drugs problems. Similar proportions of tele-IPT (10%) and SC controls (3%) had used hotlines in the past month for support related to drug, alcohol, or emotional problems. Finally, comparable proportions of tele-IPT (23%) and SC controls (13%) attended one or more self-help groups in the past month.
Depressive symptoms and perceptions of social support were comparable across the rurality continuum (see Table 2). Specifically, BDI values did not differ by rural- urban continuum codes, F (5,126) = 0.68, p= .64. Similarly, perceptions of social support did not differ by rural-urban continuum code, F (5,126) = 0.48, p=.79.
Table 2.
Depressive Symptoms and Social Support at Pre-Intervention (N=132) and Therapy Session Attendance by RUCA Code
|
Rural Urban Continuum Code/Country Description |
Baseline Social Support Value | Baseline BDI Value | Therapy Sessions Attended |
|---|---|---|---|
| 4: Urban population of 20,000 or more, adjacent to metropolitan area | 40.7 (7.6) (n=21) |
24.8 (10.2) (n=21) |
8.25 (2.6) (n=12) |
| 5: Urban population of 20,000 or more; not adjacent to metropolitan area | 39.1 (11.7) (n=20) |
26.5 (9.5) (n=20) |
8.42 (2.0) (n=12) |
| 6: Urban population of 2,500 to 19,999, adjacent to metropolitan area | 41.1 (8.3) (n=46) |
27.2 (9.7) (n=46) |
7.21 (3.2) (n=19) |
| 7: Urban population of 2,500 to 19,999, not adjacent to metropolitan area | 42.6 (8.7) (n=33) |
27.8 (8.6) (n=33) |
7.20 (3.6) (n=20) |
| 8: Completely rural or less than 2,500 urban population, adjacent to metropolitan area | 38.8 (12.6) (n=6) |
28.0 (10.7) (n=6) |
7.33 (2.8) (n=3) |
| 9: Completely rural or less than 2,500 urban population, not adjacent to metropolitan area | 37.5 (13.0) (n=6) |
21.3 (6.6) (n=6) |
9.00 (0.0) (n=4) |
Teletherapy Participation and Post-Intervention Assessment Completion
Tele-IPT patients attended an average of 7.7 teletherapy sessions; 80% attended all nine sessions (Mdn=9.0, Mode=9.0, Range=0–9). Number of teletherapy sessions attended was unrelated to pre-intervention BDI value, β = - 0.89, p= .46. Patients who had been living with HIV for more years attended a greater number of teletherapy sessions, β = .29, p= .016 and also reported higher pre-intervention BDI values, β = .29, p= .015. Table 2 shows that therapy session attendance did not differ by rural urban continuum code, F(5,78) = 0.56, p=.73.
Of the 132 patients, 19 (14%) did not complete post-intervention assessments. Assessment completers (n=113) did not differ significantly from assessment non-completers (n=19) on any pre-intervention demographic, clinical, or psychiatric outcome variable (all ps >.05).
Depressive Symptoms at Acute Outcome Assessment (Post-Intervention)
Patients and teletherapists initially identified an interpersonal focal point to frame subsequent tele-IPT sessions. The primary interpersonal focal problems identified were: Role Transition (54%); Interpersonal Sensitivity (16%); Interpersonal Role Disputes (15%); and Unresolved Grief/Bereavement (15%).
ITT analyses with multiple imputation.
MMRM ITT analyses with regression-based multiple imputation for missing data found a significant “Time x Study Arm” interaction for BDI, t = 2.52, p= .012, d = 0.45. Table 3 shows that tele-IPT patients reported significant BDI reductions from pre-intervention (M=26.3) through post-intervention (M=20.9), whereas BDI values in SC controls remained largely unchanged from pre-intervention (M=27.0) through post-intervention (M=25.4). A significant “Time x Study Arm” interaction was also found for IIP-64 scores, t = 2.78, p= .006, d = 0.46. Tele-IPT patients reported significant reductions in IIP-64 values from pre-intervention (M=104.4) through post-intervention (M=93.0) whereas SC controls reported slight increases from pre-intervention (M=97.1) through post-intervention (M=98.5).
Table 3.
Changes from Pre-Intervention through Post-Intervention in Depressive Symptoms, Interpersonal Problems, and Social Support by Study Arm, Mean (SD)
| Variable | No. | Pre-Intervention | Post-Intervention | Diff |
|---|---|---|---|---|
| BDI | ||||
| MMRM Imputation | ||||
| IPT | 70 | 26.3 (1.0) | 20.9 (1.3) | - 5.4 |
| Standard Care | 62 | 27.0 (1.3) | 25.4 (1.5) | - 1.6 |
| Completer-Only | ||||
| IPT | 56 | 26.0 (1.3) | 20.2 (1.4) | - 5.8 |
| Standard Care | 62 | 27.0 (1.2) | 25.6 (1.4) | - 1.4 |
| IIP-64 | ||||
| MMRM Imputation | ||||
| IPT | 70 | 104.4 (4.0) | 93.0 (4.8) | - 11.4 |
| Standard Care | 62 | 97.1 (4.1) | 98.5 (4.5) | + 1.4 |
| Completer-Only | ||||
| IPT | 56 | 104.8 (4.9) | 90.1 (5.3) | -14.7 |
| Standard Care | 62 | 97.5 (4.9) | 100.7 (5.2) | + 3.2 |
| PSRS | ||||
| MMRM Imputation | ||||
| IPT | 70 | 41.0 (1.1) | 40.1 (1.4) | - .90 |
| Standard Care | 62 | 40.7 (1.2) | 40.1 (1.3) | - .60 |
| Completer-Only | ||||
| IPT | 56 | 40.2 (1.2) | 39.4 (1.4) | - .80 |
| Standard Care | 62 | 40.7 (1.2) | 40.1 (1.4) | - .60 |
Social support was unchanged in both tele-IPT and SC controls from pre-intervention through post-intervention, t = 0.18, p= .860, d = 0.03.
Completer analyses.
Table 3 shows a significant “Time x Study Arm” interaction for BDI scores, t = 2.84, p= .005, d = 0.53. Tele-IPT patients reported significant BDI reductions from pre-intervention (M=26.0) through post-intervention (M=20.2) whereas SC controls reported no significant change in BDI values from pre- (M=27.0) through post-intervention (M=25.6). A significant “Time x Study Arm” interaction was also found for IIP-64 scores, t = 3.11, p= .002, d = 0.58. Tele-IPT patients reported significant reductions in interpersonal problems from pre- (M=104.8) through post-intervention (M=90.1) while SC controls’ IIP-64 scores were unchanged from pre- (M=97.5) through post-intervention (M=100.7). Social support was unchanged in both tele-IPT and SC controls, t = 0.12, p = .900, d =0.02.
Sensitivity analyses.
Additional analyses were conducted that included all 167 patients randomized to condition regardless of pre-intervention BDI values. ITT analysis with multiple imputation revealed significant “Time x Study Arm” interactions for BDI (d = .32, p = .034) and IIP-64 (d = .37, p < .006) but not for PSRS values (ES = .07, p = .640). As might be expected, the effect sizes for changes in the BDI and IIP from the larger sample (N=167) were smaller than those found in analyses that excluded patients with pre-intervention BDI values ≤14. Taken together, completer-only and ITT-MMRM analyses using data from all 167 patients did not differ from those with pre-intervention BDI values ≥14, further confirming the efficacy of tele-IPT for this population.
Gender as a potential moderator.
Because this sample included male and female patients, intervention outcome analyses were re-conducted using gender as a potential moderator variable, although no “Gender x Condition” interactions were hypothesized. Using an intent-to-treat approach and only patients who reported pre-intervention values ≥ 14, no “Gender x Condition” interaction was found for any outcome measure, depressive Symptoms, F (1,127) = 0.52, p= 0.47, interpersonal problems, F (1,115) = 0.20, p = 0.66, and social support, F (1,125) = 3.20, p = 0.08
Proportion of Patients Responding to Therapy
A reduction of ≥50% in depressive symptoms is used as a binary outcome variable to determine the proportion of patients who “responded” to therapy.33 As Table 4 shows, in ITT MMRM multiple imputation analyses, a chi-squared analysis found a significant association between study arm and treatment response category, X2(2)=12.8, p= .002, with a greater proportion of tele-IPT patients (22%) responding than SC controls (4%), z=2.94, p< .004. In completer-only analyses, a chi-squared analysis also found a significant association, X2(2)=17.2, p= .001, with more tele-IPT patients (23%) responding than SC controls (3%), z=3.63, p < .001.
Table 4.
Proportions of Responders, Partial Responders, and Non-Responders by Study Arm for, MMRM Multiple Imputation and Completer-Only Analyses
| BDI | Non-Responder | Partial Responder | Responder |
|---|---|---|---|
| MMRM Multiple Imputation | |||
| IPT (n=70) | 50% | 28% | 22% |
| Standard Care (n=62) | 78% | 18% | 4% |
| Completers-Only | |||
| IPT (n=56) | 48% | 28% | 23% |
| Standard Care (n=62) | 82% | 15% | 3% |
DISCUSSION
Easily accessible, contextualized, psychotherapeutic treatments for depression are urgently needed for the growing population of rural PLWHA. This is the first large-scale RCT to test tele-IPT’s efficacy to provide acute depressive symptom relief in rural PLWHA diagnosed with depression. Tele-IPT was a highly acceptable form of treatment for depressed rural PLWHA, with 80% of patients completing all nine treatment sessions. Across a series of intervention-outcome approaches, tele-IPT patients reported significantly fewer depressive symptoms and interpersonal problems at post-intervention than controls, with 23% of tele-IPT patients reporting reductions in depressive symptoms of 50% or greater and intervention effect sizes that were “medium” in magnitude in completer-only analyses. This proportion (23%) is identical to findings from Ransom et al.’s20 pilot RCT of tele-IPT for depressed rural PLWHA. Although a favorable response rate of 23% is relatively modest compared to those found in some previous IPT studies,34 this rate is compelling given the brevity of treatment (9 sessions), the minimal formal training provided to IPT teletherapists, and the large proportion of patients included in the sample with histories of other mental health and substance use disorders. Many individuals with these conditions are typically excluded from AIDS psychotherapy outcomes research.
More than half the patients linked their depression to a recent role transition. Common role transitions in rural PLWHA included sudden relationship changes (newly divorced), loss of job or change in employment status, new or unanticipated caregiving roles, moving from an urban to a rural area, or worsening health (e.g., diagnosed with a serious non-HIV-related health condition). In this study, tele-IPT focused on depressive symptom relief associated with role transitions by encouraging the patient to mourn the loss of the old role, acquire new skills to succeed in the new role, develop new attachments and supports made possible through the new role, and identifying positive aspects of the new role.35 Mental health practitioners and agencies who work with rural PLWHA should anticipate that many depressive episodes in this group are triggered by difficult role transitions.
Face-to-face IPT has demonstrated efficacy across many disorders, including nonpsychotic major depression,36 recurrent depression,37 bulimia nervosa,38 binge eating disorder,39 and PTSD,40 and is an indicated treatment in numerous treatment guidelines for mood and eating disorders. Several formative studies suggest that IPT can be administered successfully via telephone. Donnelly et al.41 used a single-arm pilot study to demonstrate tele-IPT’s feasibility for women with breast cancer. Miller and Weissman42 established feasibility and preliminary efficacy of tele-IPT for depressed women with a lifetime history of recurrent depression and low rates of previous treatment. Neugebauer et al.43 found that one to six sessions of telephone-administered interpersonal counseling (a briefer form of IPT) provided symptom relief in depressed women who had miscarried compared to standard of care. The current clinical trial is arguably the largest, most definitive, and most rigorous test of tele-IPT’s acute depression treatment efficacy and underscores IPT’s feasibility to be administered via traditional land-line and cellular telephones.
To date, no research has examined the relationship between rurality, depression, and social support in rural PLWHA. Conventional wisdom suggests that the highest levels of depression and isolation should occur in PLWHA in the most geographically-isolated communities. Interestingly, this research found that PLWHA in the most rural areas (continuum codes of 8 and 9) reported depressive symptoms and perceptions of social support comparable to PLWHA in more densely populated rural communities and rural communities adjacent to large metropolitan areas. Rurality was also unrelated to tele-IPT session attendance, suggesting IPT’s acceptability among all rural PLWHA.
While tele-IPT reduced patients’ depressive symptoms and interpersonal problems, no treatment-related changes were observed in social support. One explanation for this null finding is that very few, if any, social supports existed in patients’ immediate geographic vicinities that they could mobilize. It is also plausible that nine weeks of treatment was insufficient to improve social support networks for PLWHA in rural areas. Practitioners who offer tele-IPT for depressed rural PLWHA should consider how the lack of social supports in rural areas might affect the administration of an interpersonal treatment that relies heavily on developing, accessing, and benefiting from social support networks.
This clinical trial has several limitations. A more rigorous study design would have included an attention-equivalent control group. Some patients’ therapeutic gains may have resulted from enrollment in a clinical trial, interactions with supportive research staff, and weekly sessions with caring mental health professionals (i.e., common factors) independent of the psychotherapy. Thus this design precludes attributing gains specifically to IPT, as opposed to other psychotherapies. Approximately 20% of patients attended self-help groups in the past month and many had been working with practitioners from a variety of helping professions. Some gains reported by patients may be attributable to outside services unrelated to tele-IPT. All data were collected through self-report methodologies; no data were collected through chart reviews or electronic medical records (e.g., data to verify patients’ HIV-seropositive status). No data were collected to assess patients’ virologic responses to tele-IPT (e.g., reductions in HIV viral loads).
Tele-IPT therapists received relatively little structured training in tele-IPT and relied almost exclusively on manuals for teletherapy administration. This may have yielded an underestimate of the true potency of tele-IPT. A more rigorous and quantifiable assessment of fidelity to intervention protocol would have also strengthened the study. Finally, several rural urban continuum codes contained relatively few patients. Comparisons of depressive symptoms, social support, and therapy session attendance across these codes were likely under-powered.
Despite these limitations, this study had numerous strengths. These included considerable geographic diversity in the sample (patients enrolled from 28 states), a high rate of assessment follow-up at post-intervention (86%) in a group that is oftentimes difficult to track and retain, and the inclusion of many patients with comorbid psychiatric disorders and/or alcohol and substance use disorders, all of which increase the study’s external validity. Additionally, this study used multiple intervention-outcome data analytic approaches, with all findings converging on tele-IPT’s acute depression treatment efficacy for this group, reducing the likelihood that significant intervention effects were an artifact of a single data analytic approach.
CONCLUSIONS
Telephone-administered IPT provides clinically-meaningful acute reductions in depressive symptoms and interpersonal problems in rural PLWHA. Tele-IPT is also a highly acceptable form of treatment, with 4 out of 5 tele-IPT patients participating in all nine teletherapy sessions. Future analyses will assess the long-term efficacy of tele-IPT to reduce depressive symptoms in rural PLWHA and identify potential mediators and moderators of tele-IPT for depression treatment in this clinical population. Conclusions regarding the efficacy of tele-IPT for depressed HIV-infected rural persons should be reserved until findings from long-term intervention outcome analyses are available. If tele-IPT provides acute and long-term depressive symptom relief in rural PLWHA, this manualized treatment can be offered by community-based rural practitioners who treat large numbers of rural PLWHA.
Footnotes
ClinicalTrials.gov Identifier: NCT02299453.
Contributor Information
Timothy G. Heckman, University of Georgia.
Bernadette D. Heckman, University of Georgia.
Timothy Anderson, Ohio University.
Travis I. Lovejoy, Oregon Health and Science University.
John C. Markowitz, Columbia University College of Physicians & Surgeons.
Ye Shen, University of Georgia.
Mark Sutton, University of Georgia.
References
- 1.Centers for Disease Control and Prevention. HIV Surveillance Report, 2013; vol. 25. http://www.cdc.gov/hiv/library/reports/surveillance/. Published February 2015. Accessed [May 19, 2015].
- 2.Palella FJ, Baker RK, Moorman AC, et al. Mortality in the highly active antiretroviral therapy era: Changing causes of death and disease in the HIV outpatient study. J Acq Immun Def Synd. 2006; 43: 27–34. [DOI] [PubMed] [Google Scholar]
- 3.Beltrami JF, Fann SA, Toomey KE. Characteristics of persons with AIDS in rural and urban Georgia: Use of alcohol and other drugs, history of sexually transmitted diseases and tuberculosis, high-risk sexual behaviors, and problems obtaining social services. Journal of the Medical Association of Georgia. 2000; 89: 10–14. [PubMed] [Google Scholar]
- 4.Cosio D, Heckman TG, Anderson T, Heckman BD, Garske J, McCarthy J. Telephone-administered motivational interviewing to reduce risky sexual behavior in HIV-infected rural persons: A pilot randomized clinical trial. Sex Transm Dis. 2010; 37: 140–146. [DOI] [PubMed] [Google Scholar]
- 5.Heckman TG, Somlai AM, Kalichman SC, Franzoi S, Kelly JA. Psychosocial differences between urban and rural person living with HIV/AIDS. J Rural Health. 1998; 14: 138–146. [DOI] [PubMed] [Google Scholar]
- 6.Schur CL, Berk ML, Dunbar JR, Shapiro MF, Cohn SE, Bozzette SA. Where to seek care: An examination of people in rural areas with HIV/AIDS. J Rural Health. 2002; 18: 337–347. [DOI] [PubMed] [Google Scholar]
- 7.Lahey T, Lin M, Marsh B, Curtin J, Wood K, Eccles B, von Reyn CF. Increased mortality in rural patients with HIV in New England. AIDS Res Hum Retrov. 2007; 2: 693–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sheth SH, Jensen PT, Lahey T. Living in rural New England amplifies the risk of depression in patients with HIV. BMC Infectious Diseases. 2009: 9:25 also retrieved at http://www.biomedcentral.com/1471-2334/9/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.United States Department of Agriculture. Rural-Urban Continuum Codes. http://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx. Accessed [May 19, 2015].
- 10.Havlik RJ. “Health Status, Comorbidities, and Health-Related Quality of Life,” in Brennan Karpiak, et al. , Editors, Older Adults with HIV: An In-Depth Examination of an Emerging Population. 2009. New York: Nova Publishers, 19–37. [Google Scholar]
- 11.High KP, Brennan-Ing M, Clifford DB, Cohen MH, Currier J. et al. HIV and aging: State of knowledge and areas of critical need for research. A report to the NIH Office of AIDS Research by the HIV and Aging Working Group. J Acq Immun Def Synd. 2012; 60: Supp. 1, S1–S18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Negin J, Martiniuk A, Cumming RG, Naidoo N, Phaswana-Mafuya N, Madurai L, Williams S, Kowal P. Prevalence of HIV and chronic comorbidities among older adults. AIDS. 2012; 31: 26: Sup. 1, S55–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rabkin JG. HIV and depresson” 2008 review and update. Current HIV/AIDS Report. 2008; 5(40): 163–171. [DOI] [PubMed] [Google Scholar]
- 14.Cook SH, Valera P, Wilson PA, and the Adolescent Trials Network for HIV/AIDS Interventions. HIV status disclosure, depressive symptoms, and sexual risk behavor among HIV-positive men who have sex with men. J Behav Med. 2015; 38: 3, 507–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reif S, Whetten K, Ostermann J, Raper JL. Characteristics of HIV-infected adults in the Deep South and their utilization of mental health services: A rural vs. urban comparison. AIDS Care. 2006; 18: 10–17. [DOI] [PubMed] [Google Scholar]
- 16.Federal Communications Commission. (2003). Supplemental Telephone Penetration Report. Washington D.C.: FCC. [Google Scholar]
- 17.Rounds K AIDS in rural areas: Challenges to providing care. Social Work. 1988; 33: 257–261. [DOI] [PubMed] [Google Scholar]
- 18.Mohr D, Vella L, Hart SL, Heckman T, Simon GE. The effect of telephone-administered psychotherapy on symptoms of depression and attrition: A meta-analysis. Clin Psychol-Sci Pr. 2008; 15: 243–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heckman TG, Carlson B. A randomized clinical trial of two telephone-delivered, mental health interventions for HIV-infected persons in rural areas of the United States. AIDS Behav. 2007; 11: 5–14. [DOI] [PubMed] [Google Scholar]
- 20.Ransom D, Heckman TG, Anderson T, Garske J, Holroyd K, Basta T. Telephone-delivered, interpersonal psychotherapy for HIV-infected rural persons diagnosed with depression: A pilot randomized clinical trial. Psychiat Serv. 2008; 59: 871–877. [DOI] [PubMed] [Google Scholar]
- 21.Weissman MM, Markowitz JC, Klerman GL. Comprehensive Guide to Interpersonal Psychotherapy. 2000. Basic Books, New York, NY. [Google Scholar]
- 22.Spitzer RL, Williams JB, Kroenke K. et al. Utility of a new procedure for diagnosing mental disorders in primary care: the PRIME-MD 1000 study. J Amer Med Assoc. 1994; 272: 1749–1756. [PubMed] [Google Scholar]
- 23.Teng EL, Chui HC.The Modified Mini-Mental Status (3MS) examination. J Clin Psychiat. 1987; 48: 314–318. [PubMed] [Google Scholar]
- 24.Beck AT, Steer RA, & Brown GK. Manual for the Beck Depression Inventory-II”. 1996. San Antonio TX; Psychological Corporation. [Google Scholar]
- 25.Tate D, Paul RH, Flanigan TP, Tashima K, Nash J, Adair C., oland R, Cogen RA. The impact of apathy and depression on quality of life in patients infected with HIV. AIDS Pateint Care ST. 2003; 17: 115–120. [DOI] [PubMed] [Google Scholar]
- 26.Leserman J, Jackson ED, Petitto JM, Golden RN, Silva SG, Perkins DO, Cai J, Folds JD, Evans DL. Progression to AIDS: The effects of stress, depressive symptoms, and socal support. Psychosom Med. 1999; 61: 397–406. [DOI] [PubMed] [Google Scholar]
- 27.Alden LE, Wiggins JS, Pincus AL. Construction of circumplex scales for the Inventory of Interpersonal Problems. J Pers Assess. 1990; 55: 521–536, [DOI] [PubMed] [Google Scholar]
- 28.Ravitz P, Maunder R, McBride C. Attachment, contemporary interpersonal therapy and IPT: An integration of theoretical, clinical, and empirical perspectives. J Contemp Psychother. 2008; 38: 11–21. [Google Scholar]
- 29.Turner RJ, Frankel BG, Levi DM. Social suport: Conceptualization, measurement, and implications for mental health. Research in Community and Mental Health. 1983; 6: 67–111. [Google Scholar]
- 30.Markowitz J, Klerman G, Clougherty K, Josephs L. Manual for interpersonal therapy with depressed HIV-seropositive patients. 1993. Unpublished.
- 31.Siddiqui O, Hung J, O’Neill R. MMRM vs. LOCF: a comprehensive comparison based on simulation study and 25 NDA datasets. J Biopharm Stat. 2009; 19(2): 227–246. doi: 10.1080/10543400802609797 [DOI] [PubMed] [Google Scholar]
- 32.Bengtson AM, Pence BW, O’Donnell J, Thielman N, Heine A, Zinski A, Modi R. et al. Improvements in depression and changes in quality of life among HIV-infected adults. AIDS Care. 2015; 27: 47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Elkin I, Shea MT, Watkins JT, Imber SD, Sotsky SM, Collins JF, et al. National Institute of Mental Health treatment of depression collaborative research program: General effectiveness of treatments. Arch Gen Psychiat. 1989; 46: 971–982. [DOI] [PubMed] [Google Scholar]
- 34.Koszycki D, Bisserbe JC, Blier P, Bradwejn J, Markowitz J. Interpersonal psychotherapy versus brief supportive therapy for depressed infertile women: first pilot randomized controlled trial. Arch Womens Ment Health. 2012;15:193–201. [DOI] [PubMed] [Google Scholar]
- 35.Weissman Markowitz Klerman (2007). Clinician’s Q Interpersonal psychotherapy versus brief supportive therapy for depressed uick Guide to Interpersonal Psychotherapy. Oxford University Press. [Google Scholar]
- 36.Frank E, Kupfer DJ, Perel JM, Cornes C., et al. Three-year outcomes for maintenance therapies in recurrent depression. Arch Gen Psychiat. 1990; 47: 1093–1099. [DOI] [PubMed] [Google Scholar]
- 37.Agras WS, Walsh BT, Wilson GT, Fairburn CG. A multi-site comparison of cognitive behavior therapy (CBT) and interpersonal psychotherapy (IPT) in the treatment of bulimia nervosa. Presented at Eating Disorders, London, April 20–22, 1999. [Google Scholar]
- 38.Wilfey DE. Treatment of binge eating disorder: Research findings and clinical applications. In B.T. Walsh (Chair), Integrating Research and Clinical Practice. Plenary session presented at the meeting of the 4th International Conference on Eating Disorders, London 1999. [Google Scholar]
- 39.Markowitz JC, Petkova E, Neria Y, Van Meter P, Zhao Y, Hembree E, Lovell K, Biyanova T, Marshall RD: Is exposure necessary? A randomized clinical trial of interpersonal psychotherapy for PTSD. Am J Psychiat. 2015;172: 430–440 Feb 13 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Donnelly JM, Kornblith AB, Fleishman S, Zuckerman E, Raptis G, Hudis CA, Hamilton N, Payne D, Massie MJ, Norton L, Holland JC. (2000). A pilot study of interpersonal psychotherapy by telephone with cancer patients and their partners. Psycho-oncol. 2000; 9(1):44–56. [DOI] [PubMed] [Google Scholar]
- 41.Miller L, Weissman M. Interpersonal psychotherapy delivered over the telephone to recurrent depressives. A pilot study. Depress Anxiety, 2002; 16(3):114–7. [DOI] [PubMed] [Google Scholar]
- 42.Neugebauer R, Kline J, Bleiberg K, Baxi L, Markowitz JC, Rosing M, Levin B, Keith J. Preliminary open trial of interpersonal counseling for subsyndromal depression following miscarriage. Depress Anxiety. 2007; 24(3):219–22. [DOI] [PubMed] [Google Scholar]