Abstract
To compare the effects of a pedometer-based behavioral intervention (Fitness for Life [FFL] program) and a traditional high-intensity fitness (TRAD) program on physical activity (PA), Army Physical Fitness Test (APFT), and coronary heart disease risk factors in Army National Guard members who failed the APFT 2-mile run. From a pool of 261 Army National Guard, a total of 156 were randomized to TRAD or FFL for 24 weeks consisting of a 12-week progressive conditioning program followed by 12 weeks of maintenance. For both groups, the total APFT score and 2-mile run time/score improved from baseline to 12 weeks (FFL: ↓ 7.4%, p = 0.03; TRAD: ↓ 5%, p = 0.08) but at 24 weeks they had regressed toward baseline. PA improved modestly and coronary risk profile changed minimally in both groups. A pedometer-based exercise intervention had results similar to a high-intensity program for improving PA, APFT, and 2-mile run times/score. Neither group sustained the improved run times over the 12 weeks of maintenance.
INTRODUCTION
The wars in Afghanistan (Operation Enduring Freedom) and Iraq (Operation Iraqi Freedom) have seen an unprecedented use of the reserve component of the military,1 accounting for 40% of those deployed.2 With heavy war-time use, deployability is a concern since Reserve and National Guard forces who deploy are generally older and less fit than active duty forces.3 Although most Reserve and National Guard members can perform their military tasks without problems, the risk of a coronary heart disease (CHD) event is higher for members not physically fit.4
Maintaining physical fitness is viewed as an individual reservist’s responsibility. Yet, one of the difficulties that Army National Guard (ARNG) members encounter is meeting the requirements of the Army Physical Fitness Test (APFT), specifically the 2-mile run. Monthly physical training (PT) conducted during reserve duty is insufficient to ensure fitness, and the part-time nature of the ARNG service makes it difficult to adhere to an exercise program and sustain improvements once the program has ended. A common barrier to increasing physical activity (PA) is lack of time5; it is hard to incorporate work and family activities while trying to make time for aerobic exercise. This is even truer for the “citizen” soldier who has a full-time civilian job and works part-time in the ARNG. By comparison, the 2008 to 2009 national multiple jobholding rate for civilian workers is only 5.2%.6 Thus, a sizeable proportion of reserve component members, including ARNG members, fail the physical fitness test, threatening their readiness status.7
One approach that may be useful in integrating PA into daily life is the use of a pedometer to help accumulate steps throughout the day. Pedometer-driven programs have been shown to significantly increase the amount and intensity of PA8,9 and to decrease blood pressure (BP) and body mass index (BMI).10 Using a pedometer to accumulate moderate-to-high intensity PA in short bouts improves cardiorespiratory fitness (maximal oxygen consumption [VO2 max]).11-13 Key to this approach is setting step goals and tracking steps via a diary.10 Increased moderate-to-high intensity PA improves aerobic fitness14 and reduces CHD risk.15
This randomized controlled trial (RCT) compared the effects of a pedometer-based behavioral intervention and the traditional Army physical fitness (TRAD) program on PA, aerobic fitness, and CHD risk factors in healthy adult men and women in the ARNG who had failed the APFT. Baseline findings have been reported elsewhere.4
METHODS
Participants
Volunteer participants were recruited from the Maryland and Washington, DC, ARNG. All were part-time guard members who had failed the 2-mile run component of the APFT, that is, scoring ≤60 points on the run, where scoring is based on gender, age category, and run time. Those with 12 months or longer before re-enlistment or retirement were included in the study. ARNG members were excluded from the study if they had a history of CHD or stroke, were currently taking hypertensive or cholesterol lowering medications, had been pregnant within the previous 6 months, were post-menopausal or currently taking hormone replacement therapy, or had major musculoskeletal disorders. Post-menopausal women and women on hormone replacement therapy were excluded owing to their small numbers and potential confounding effect on serum lipids. From a pool of 261 ARNG soldiers who failed the run portion of the APFT, 156 met the criteria for inclusion in the study and were randomized into 2 groups. The study was conducted under a protocol approved by the Uniformed Services University of the Health Sciences (USUHS) Institutional Review Board, and each participant provided written informed consent.
Design
A randomized 2 (group) × 3 (time: baseline, 12 weeks, 24 weeks) design with 12 weeks of conditioning and 12 weeks of maintenance was used to compare the pedometer-based Fitness for Life (FFL) program to a TRAD program on the primary outcomes of PA and performance on the APFT at 12 and 24 weeks and on the secondary outcome of CHD risk factors.
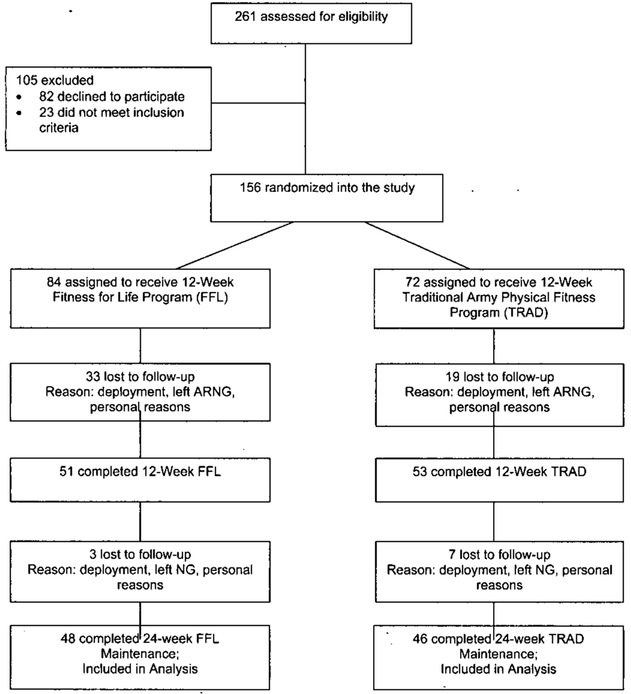
Participants were tested at baseline and were then randomly assigned to either the FFL or the TRAD program. They were tested again at the conclusion of the 12-week intensive intervention and following the 12 weeks of maintenance (Fig. 1).
FIGURE 1.
Flow diagram of the ARNG study.
Intervention Training Programs
ARNG FFL Program
The ARNG FFL program was designed specifically for the reserve components of ARNG and Reserve to teach soldiers working a full-time civilian job and a part-time military job to incorporate moderate intensity PA into their daily lives. The pedometer was the central focus used to motivate and monitor steps through setting step goals, maintaining a daily step log, and promoting activities to increase steps. The counseling sessions discussed various activities to increase their daily step count. At the beginning of the program, participants were instructed to wear a Digiwalker (Yamax SW 200; New Lifestyles, Lees Summit, MO) pedometer for self-monitoring of their daily steps. In weeks 1 to 4, the pedometer was used as a motivator to accumulate daily steps through short bouts of walking combined with behavioral-based PA counseling. During brief weekly telephone counseling (<5 minutes), pedometer logs were reviewed and feedbacks provided. Motivational postcards were mailed weekly to suggest various ways to increase steps. Monthly group meetings were held to provide support, emphasize relapse prevention, and encourage self-monitoring of steps.
Weeks 5 to 12 focused on increasing the intensity of soldiers’ activities. Soldiers were taught to rate their perceived exertion while performing moderate-to-high intensity daily activities in their target heart rate range, defined as 60 to 90% of predicted maximum heart rate, calculated as 220 – age. Using the Rating of Perceived Exertion scale,16 participants gauged the intensity of their activities by means of feedback from their target heart rate. The pedometer continued to be the central focus of behavioral strategies for setting step goals, monthly support meetings, weekly booster telephone calls, and bimonthly motivational mailings.
Weeks 13 to 24 focused on sustaining gains in the amount of steps and intensity of PA. Participants were expected to continue using the pedometer to monitor their PA. Monthly maintenance meetings were continued; telephone calls were tapered to every 2 weeks, then monthly to increase autonomy. Relapse prevention, self-monitoring, and reinforcement were continually emphasized during the maintenance phase.
TRAD Program
The comparator exercise intervention was the TRAD. This program follows Army Regulation 350-41, with recommendations detailed in the Army’s Field Manual 21-20. The program consists of 12 weeks of high-intensity conditioning, defined as 75 to 80% of maximum heart rate and 12 weeks of maintenance. In the current study, participants in the TRAD exercise program were instructed to perform vigorous physical fitness training 3 to 6 days per week, including three 30-minute sessions of aerobic training and three 30-minute strength training sessions, performed unsupervised separately or combined, during their normal work day or during leisure time. Oversight of the 12-week training program was provided by a Master Fitness Trainer, an ARNG soldier who had completed a 2-week reserve component training course. Participants received a 60 minute briefing with supplementary booklet on the TRAD. A brief reminder call was made before each monthly meeting. The TRAD group received pretest, posttest, and follow-up testing to match the testing of the FFL group.
Measurements
Physical Activity
The 7-day physical activity recall (PAR) interview was used to estimate energy expenditure as defined by multiples of resting metabolic energy expenditure (METS).17 The PAR was administered by a trained interviewer at baseline, 12 weeks, and 24 weeks. Participants were questioned about the amount of time spent asleep (1.0 MET) and in moderate (4 METS), hard (6 METS), and very hard (10 METS) intensity PAs for the previous weekdays and weekend. It was assumed that they spent the remaining time in “light” activities (1.5 METS). To estimate energy expenditure per week, the average number of minutes at each activity level was multiplied by the respective MET value for an estimate of light, moderate, hard, and very hard PAs in kcal/kg. Total PA was the sum of the 4 PA intensity levels.18 In addition, the sum of moderate, hard, and very hard activity (total PA) was calculated because both interventions were designed to increase these 3 activity levels, but not low-intensity activity. The 7-day PAR is moderately correlated with VO2 max, r = 0.61,19 the accepted standard for cardiorespiratory fitness.
The participants recorded their step count in a daily pedometer log. A Digiwalker pedometer was used to count the number of steps taken per day. The Digiwalker’s accuracy is within 1% of the actual step count on a 4.88-km sidewalk course.20
Physical Fitness
The APFT, a standardized measure of cardiorespiratory fitness and muscular endurance, was administered by Army fitness monitors according to standardized protocols detailed in Chapter 14 of the Army Field Manual 21-20.21 The APFT is a 3-event physical performance test consisting of push-ups, sit-ups, and a 2-mile run. Each participant is tested on (1) the number of standard Army push-ups performed in 2 minutes; (2) the number of standard Army sit-ups performed in 2 minutes; and (3) the time to complete a 2-mile run. The APFT scoring is a normative-based scale.22 Raw scores for each test are converted to points using standard age-adjusted and gender-adjusted scoring tables available in Army FM 21-20. Each event has a possible score range from 0 to 100. A total score of 180 or higher is needed to pass the APFT, with a minimum score of 60 in each event. Results of the 2-mile run have been correlated with VO2 max23; the push-ups and sit-ups indicate muscular endurance.24
CHD Risk Factors
Demographic and Physical Information
Self-reports on age, gender, and race were obtained from participants. Weight and height were measured using a digital scale, with participants in gym shorts and T-shirt without shoes. BMI was then calculated as weight (kg) divided by height (m2).
Blood Pressure
An automatic digital BP monitor (Model 6009; American Diagnostic, Tokyo, Japan) was used to measure seated BP and heart rate using the dominant arm at heart level. Three measurements were taken at 1 to 2-minute intervals, and the mean of the 2 closest readings was reported. Cuff sizes reflected the circumference of the participant’s arm. Extreme values were checked by trained personnel, who repeated the digital recording and then recorded BP manually.
Serum Lipids
Venipuncture from the anterior cubital fossa was used to draw fasting blood samples (>9 hours) while participants were in a seated position. The samples were allowed to clot at room temperature, then centrifuged at 3,000 rpm for 15 minutes, and the resulting serum was removed and stored at −80° until analysis. Total cholesterol (TC), triglycerides, low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C) were analyzed; very low-density lipoprotein cholesterol and TC:HDL-C ratio were calculated. The lipid panel was analyzed using the Cholestech LDX system analyzer (Cholestech, Hayward, CA), with a sensitivity of 0.8%. The intra-assay and interassay coefficients of variance are 2.03% and 4.10% for triglycerides, 3.60% and 5.23% for TC, 2.96% and 4.74% for HDL-C, 5.24% and 5.55% for LDL-C, and 1.58% and 4.46% for very low-density lipoprotein cholesterol, respectively. All assays were conducted at Johns Hopkins Bayview Campus in the General Clinical Research Center.25
Smoking Status
Smoking status was classified as current, former, or never. Former smokers were those who had quit smoking before their assessment. Nonsmokers reported never smoking.
Statistical Analyses
Statistical analyses were completed using PASW Statistics (SPSS) version 17.0. Descriptive statistics were calculated including frequencies, means, SDs, and percents, χ2 test or Fisher’s exact test was used to examine relationships between group assignment and categorical variables. Independent sample t test statistics were used to determine the differences between the groups at baseline on the primary outcome variables (APFT and PA) and secondary outcome variable (CHD risk). A repeated measures of analysis of variance was used to test for main effects of the intervention (FFL vs. TRAD) over time (baseline, 12-week, and 24-week follow-up) and for the intervention by time interaction. The Geisser-Greenhouse correction26 was applied if the statistical assumption of compound symmetry was not met. We used expectation-maximization for imputation estimates of missing data in the group of protocol completers, with SPSS Missing Value Analysis 16.0.27 The missing data for individual variables ranged between 1% and 19%. Missing data were determined to be missing at random, meeting expectation-maximization assumptions.28 A 2-tailed p value of ≤0.05 was set for statistical significance.
Based on the predicted effect of the intervention with projected 40% attrition, we estimated a total sample size of 156 ARNG soldiers to demonstrate a 10% improvement in APFT scores (effect size, d = 0.65) and PA (effect size d = 0.56) at an α of 0.05 and a power of 0.80.
RESULTS
Study Attrition
From the total of 156 participants who enrolled in the study, 104 completed the 12-week evaluation and 94 completed baseline, 12-week, and 24-week evaluations. Of the 62 individuals lost to follow-up, 36 were in the FFL group and 26 in the TRAD group; this was not significant. The reasons for noncompletion were personal reasons (n = 22), quitting the ARNG (n = 21), deployment (n = 15), injury not related to the study (n = 3), and completion of ARNG training requirement of passing the APFT (n = 1).
Neither demographics, PA, APFT variables, nor CHD risk factors differed significantly between dropouts and 24-week completers, but dropouts had a lower baseline high-density lipoprotein (HDL) (t = 2.6; p = 0.01) and a higher baseline TC:HDL ratio (t = −2.96; p = 0.01). Dropouts performed fewer sit-ups (t = −2.22; p = 0.30) at baseline and had significantly lower baseline scores on the push-ups (t = −1.99; p = 0.05) and on the total APFT score (t = −2.01; p = 0.05).
Characterization of Completers
Among those 94 soldiers who completed the 12- and 24-week evaluations, there were no differences at baseline between the FFL (n = 48) and TRAD (n = 46) groups on demographic variables (Table I). Baseline differences between the groups on PA, APFT, and CHD risk factors are shown in Table II. There were no significant differences in total PA, steps walked, APFT scores, 2-mile run time, push-up and sit-up repetitions, but there were differences in the levels of intensity of PA. Those in the TRAD group performed more moderate and very hard intensity PAs. HDL-C was slightly but significantly higher in the FFL group at baseline (Table II); all other CHD risk factors were comparable between the groups.
TABLE I.
Demographic Characteristics of the Participants Completing the Study
| FFL (N = 48) | TRAD (N = 46) | p Value | |
|---|---|---|---|
| Age (Years) | 32.7 (10.1) | 32.8 (8.3) | 0.66a |
| Sex (%) | |||
| Male | 33 (68.8) | 37 (80.4) | 0.24b |
| Female | 15 (31.3) | 9 (19.6) | |
| Height (cm) | 171 (8.5) | 173 (8.7) | 0.20a |
| Race (%) | |||
| Caucasian | 31 | 50 | 0.13c |
| African American | 50 | 39 | |
| Asian/Pacific Islander | 7 | 7 | |
| Other | 12 | 4 | |
| Marital Status (%) | |||
| Single | 62 | 56 | 0.58c |
| Married | 25 | 35 | |
| Divorced | 13 | 9 | |
| Education (%) | |||
| Some High School | 0 | 0 | 0.45c |
| High School Graduate | 27 | 31 | |
| Some College | 50 | 50 | |
| College Graduate | 7 | 2 | |
| Some Post-graduate | 8 | 15 | |
| Advanced Degree | 8 | 2 | |
| Employment Status (%) | |||
| Unemployed | 8 | 7 | 0.96c |
| Student | 13 | 13 | |
| Employed | 73 | 76 | |
| Student and Employed | 6 | 4 | |
| Income (%) | |||
| $0,000-$19,999 | 13 | 22 | 0.56c |
| $20,000-$39,999 | 21 | 32 | |
| $40,000-$59,999 | 21 | 21 | |
| $60,000-$79,999 | 17 | 7 | |
| $80,000 and Over | 11 | 11 | |
| Declined to Answer | 17 | 7 | |
| Rank (%) | |||
| Enlisted | 96 | 96 | 0.62c |
| Officer | 4 | 4 | |
| Smoker | |||
| Never | 61 | 63 | 0.25c |
| Quit <6 Months | 2 | 7 | |
| Quit >6 Months | 6 | 13 | |
| Yes | 31 | 17 | |
Values are mean ± SD except where indicated. Percentages may not add to 100% due to rounding.
Independent sample t test
Fisher’s exact test
Pearson χ2 test.
TABLE II.
Baseline Characteristics of Participants for PA, APFT, and CHD Risk Factors
| Variable | FFL (N = 48) | TRAD (N = 46) | p Value |
|---|---|---|---|
| PA | |||
| Total PA | 211.4 (46.6) | 223.8 (58.4) | 0.26 |
| Moderate Intensity PA | 21.9 (36.5) | 46.8 (60.0) | 0.02 |
| Hard Intensity PA | 19.2 (43.0) | 7.2 (13.9) | 0.07 |
| Very Hard Intensity PA | 2.4 (5.2) | 10.8 (27.4) | 0.05 |
| Steps Walked/Day | 6415.9 (2858.8) | 7300.6 (4064.9) | 0.22 |
| APFT Variables | |||
| 2-Mile Run (s) | 1405.6 (424.8) | 1332.3 (433.8) | 0.41 |
| Push-up (No.) | 38.5 (12.7) | 41.51 (13.6) | 0.27 |
| Sit-up (No.) | 45.1 (13.6) | 47.1 (12.01) | 0.47 |
| Total APFT Score (0–300) |
159.5 (40.5) | 158.5 (36.3) | 0.90 |
| 2-Mile Run Score (0–100) |
29.0 (24.6) | 31.5 (24.9) | 0.64 |
| Sit-up Score (0–100) |
58.7 (19.4) | 60.8 (16.7) | 0.72 |
| Push-up Score (0–100) | 69.3 (13.0) | 68.6 (11.8) | 0.58 |
| CHD Risk Factors | |||
| Systolic BP (mm Hg) |
120.2 (16.5) | 125.7 (15.3) | 0.10 |
| Diastolic BP (mm Hg) |
74.7 (11.9) | 77.5 (10.2) | 0.24 |
| BM1 (kg/m2) | 28.6 (5.1) | 29.8 (3.8) | 0.18 |
| TC (mg/dL) | 185.8 (39.1) | 183.4 (32.6) | 0.74 |
| HDL-C (mg/dL) | 54.1 (16.1) | 45.8 (10.0) | 0.01 |
| LDL-C (mg/dL) | 109.6 (38.0) | 111.7 (32.1) | 0.78 |
| TC/HDL Ratio | 3.8 (1.4) | 4.2 (1.1) | 0.12 |
Values are mean ± SD except where indicated. Independent sample t test. The p values are for comparing the FFL and TRAD groups. Total PA is the sum of moderate, hard, and very hard intensity PA.
Adherence and APFT Pass Rate
FFL group participants who attended the group meetings for a total of 67.5 minutes (50% of the total meeting time) or more were defined as adherers to the program. TRAD group members who attended their meetings for a total of 30 minutes (50% of the meeting time) or more were considered adherers. Only 6 (12.5%) participants in the FFL group and 5 (10.8%) participants in the TRAD group did not adhere to their program (χ2 = 0.05, p = 0.81). The percentage of soldiers who passed the 2-mile run at 3 and 6 months was 52% in the FFL and 45.7% in the TRAD (χ2 = 0.39; p = 0.53).
Physical Activity
Intensity of PA
For total PA, the main effect of group was significant (F(1,92) = 4.42, p = 0.04); neither the time-group interaction nor the main effect of time was significant (Table III). Both groups had a slight but nonsignificant increase in total PA during the intensive phase of the program and a decrease during maintenance. Moderate intensity PA showed a significant main effect of time (F(2,184) = 3.88, p = 0.02); the time-group interaction and the main effect of group were not significant. Moderate intensity PA increased 70% in the FFL group from baseline to 12 weeks (t = −1.99, p = 0.05) and decreased 35% from 12 to 24 weeks (t = 1.61, p = 0.11); the TRAD decreased 10% (t = 0.48, p = 0.63) to 12 weeks and 46% from 12 to 24 weeks (t = 2.11, p = 0.40). Hard intensity PA showed a significant time-group interaction (F(2,184) = 5.79, p = 0.01); the main effect of time and the main effect of group were not significant. The FFL group showed a decrease in hard intensity PA of 50% from baseline to 12 weeks (t = 1.39, p = 0.17), whereas the TRAD group increased 154% (t = −1.9, p = 0.06). For very hard intensity PA, there was a significant main effect of group (F(1,92) = 6.91, p = 0.01); the time-group interaction and main effect of time were not significant. Very hard intensity PA levels did not change significantly in either group throughout the 24 weeks.
TABLE III.
Influence of a Home-Based Pedometer Program and TRAD Program on PA
| FFL (N = 48) |
TRAD (N = 46) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline |
12 Weeks |
24 Weeks |
Baseline |
12 Weeks |
24 Weeks |
Time |
Group |
Group X Time |
||||
| Variable | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | F | p | F | p | F | p |
| PA | ||||||||||||
| Total PA* (kcal/kg/wk) |
43.6 (63.9) | 49.7 (59.7) | 34.3 (49.8) | 64.8 (74.1) | 75.4 (102.3) | 60.0 (87.8) | 1.52 | 0.22 | 4.42 | 0.04 | 0.42 | 0.94 |
| Moderate Intensity PA (kcal/kg/wk) |
21.9 (36.5) | 37.1 (57.4)‡ | 24.1 (46.6) | 46.8 (60.1) | 42.2 (55.5) | 22.7 (38.3) *,‡ | 3.88 | 0.02 | 1.54 | 0.22 | 2.66 | 0.07 |
| Hard Intensity PA (kcal/kg/wk) |
19.2 (43.0) | 9.6 (15.4) | 7.2 (10.6)‡ | 7.21 (13.9) | 18.3 (35.6) | 26.6 (53.7)‡ | 0.34 | 0.72 | 1.74 | 0.20 | 5.79 | 0.01 |
| Very Hard Intensity PA (kcal/kg/wk) |
2.5 (5.2) | 3.1 (5.7) | 3.0 (7.5) | 10.9 (27.4) | 14.9 (46.6) | 10.7 (36.3) | 0.26 | 0.61 | 6.91 | 0.01 | 0.08 | 0.78 |
| Steps Walked/Day (Pedometer) |
6,415 (2858) | 8,027 (1422) | 7,702 (2841) | 7,300 (4064) | 6,593 (2108) | 7,478 (2984) | 2.31 | 0.11 | 0.37 | 0.55 | 5.69 | 0.01 |
Values are mean ± SD. Statistics based on imputed data. Total PA is the sum of moderate, hard, and very hard intensity PA.
Significant within-group differences from baseline (p < 0.05);
Significant within-group differences 12 weeks to 24 weeks (p < 0.05).
Average Daily Steps
For average number of steps walked per day, there was a significant time-group interaction (F(1.60, 147.76) = 5.69, p = 0.01). From baseline to 12 weeks, the FFL group increased their average steps per day by 25% (1,612 steps) during the intensive 12-week intervention (t = −6.43, p = 0.001) and slightly decreased by 4% or 325 steps per day during maintenance (t = 0.81, p = 0.42). The TRAD group decreased their steps by 9.6% (707 steps per day) during the intensive phase (t = 1.50, p = 0.14) and increased by 13% (885 steps per day) during maintenance (t = −1.62, p = 0.11). The main effect of group and main effect of time were not significant.
APFT Variables
APFT Raw Scores
The 2-mile run (in seconds) showed a significant time effect (F(1.84, 169.14) = 18.99, p = 0.01); however, the main effect of group and the time-group interaction were not significant (Table IV). Both groups improved their 2-mile run time after the first 12 weeks of the intervention (FFL: t = −4.37, p = 0.01; TRAD: t = −5.55, p = 0.01). At 24 weeks, the FFL group was 7.4% faster (t −2.20, p = 0.03) and the TRAD trended 5% faster (t = −1.78, p = 0.08) than at baseline. For the push-up and sit-up repetitions, neither the time–group interaction, main effect of time, or main effect of group were significant. Thus, neither intervention improved the push-up and sit-up portion of the APFT.
TABLE IV.
Influence of a Home-Based Pedometer Program and TRAD Program on APFT
| FFL (N = 48) |
TRAD (N = 46) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline |
12 Weeks |
24 Weeks |
Baseline |
12 Weeks |
24 Weeks |
Time |
Group |
Group X Time |
||||
| Variable | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | F | p | F | p | F | p |
| APFT Variables | ||||||||||||
| Push-up (No. Repetitions) |
38.5 (12.7) | 36.2 (14.8) | 37.1 (11.4) | 41.5 (13.6) | 40.8 (13.1) | 41.0 (12.3) | 1.52 | 0.22 | 2.38 | 0.13 | 0.41 | 0.63 |
| Sit-up (No. Repetitions) |
45.1 (13.6) | 45.4 (11.3) | 47.1 (10.7) | 47.1 (12.0) | 45.4 (10.1) | 46.3 (10.3) | 1.33 | 0.27 | 0.03 | 0.87 | 1.59 | 0.21 |
| 2-Mile Run (s) | 1405 (424) | 1172 (201)* | 1300 (441)‡ | 1332 (433) | 1117 (191)* | 1265 (332)‡ | 18.99 | 0.01 | 0.99 | 0.32 | 0.14 | 0.85 |
| Total APFT Score (0–300) |
159.5 (40.5) | 176.8 (40.9)* | 167.7 (38.6)‡ | 158.5 (36.3) | 178.2 (32.2)* | 162.9 (38.1)‡ | 15.01 | 0.01 | 0.05 | 0.83 | 0.43 | 0.65 |
| Push-up Score (0–100) |
69.3 (13.0) | 66.3 (15.5) | 67.8 (11.6) | 68.6 (11.8) | 68.9 (9.7) | 67.9 (10.8) | 0.81 | 0.45 | 0.10 | 0.75 | 1.18 | 0.31 |
| Sit-up Score (0–100) |
58.7 (19.4) | 60.1 (14.9) | 61.5 (14.8) | 60.8 (16.7) | 60.1 (12.5) | 60.2 (14.9) | 0.30 | 0.74 | 0.01 | 0.93 | 0.76 | 0.44 |
| 2-Mile Run Score (0–100) |
31.5 (24.9) | 50.3 (27.3)* | 38.5 (26.8)*,‡ | 29.0 (24.6) | 49.2 (24.5)* | 34.9 (24.6)‡ | 26.03 | 0.01 | 0.33 | 0.57 | 0.09 | 0.89 |
Values are mean ± SD. Statistics based on imputed data.
Significant within-group differences from baseline (p < 0.05);
Significant within-group differences 12 weeks to 24 weeks (p < 0.05).
APFT Standardized Scores
For the total APFT score, there was a significant main effect of time (F(2, 184) = 15.01, p = 0.01); however, the main effect of group and the time–group interaction were not significant. Both groups improved their total APFT score from baseline to 12 weeks (FFL: t = −3.90, p = 0.01; TRAD: t = −4.29, p = 0.01). Changes in the 2-mile run scores and push-up and sit-up scores, as well as their statistical significance, paralleled those of the raw values.
CHD Risk Factors
For HDL-C, there was a significant main effect of time (F(2,184) = 4.17, p = 0.02) and a main effect of group (F( 1,92) = 9.0, p = 0.01); the time–group interaction was not significant (Table V). The TRAD group saw a 4.6% increase in HDL from baseline at 12 weeks (t = −2.27, p = 0.03) and 5.9% at 24 weeks (t = −2.71, p = 0.01).
TABLE V.
Influence of a Home-Based Pedometer Program and TRAD Program on CHD Risk Factors
| FFL (N = 48) |
TRAD (N = 46) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline |
12 Weeks |
24 Weeks |
Baseline |
12 Weeks |
24 Weeks |
Time |
Group |
Group X Time |
||||
| Variable | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | F | p | F | p | F | p |
| CHD Risk Factors Systolic BP (mm Hg) | 120.2 (16.5) | 120.3 (17.3) | 120.5 (14.9) | 125.7 (15.3) | 125.3 (15.3) | 124.5 (15.5) | 0.08 | 0.93 | 2.71 | 0.10 | 0.17 | 0.85 |
| Diastolic BP (mm Hg) | 74.7 (11.9) | 76.0 (12.1) | 76.6 (10.8) | 77.5 (10.3) | 80.2 (11.0) | 78.8 (11.6) | 1.96 | 0.14 | 2.37 | 0.13 | 0.45 | 0.64 |
| BMI (kg/m2) | 28.6 (5.2) | 28.5 (4.9) | 28.7 (5.0) | 29.9 (3.7) | 30.0 (3.9) | 29.8 (3.6) | 0.14 | 0.87 | 1.87 | 0.18 | 1.22 | 0.30 |
| Weight (kg) | 82.6 (18.0) | 82.4 (17.1) | 82.7 (17.3) | 91.1 (16.0) | 91.5 (16.1) | 90.9 (15.8) | 0.01 | 0.90 | 5.19 | 0.03 | 0.10 | 0.75 |
| TC (mg/dL) | 185.8 (39.1) | 186.6 (45.6) | 192.8 (40.7) | 183.4 (32.6) | 180.0 (32.7) | 186.1 (35.1) | 3.03 | 0.06 | 0.53 | 0.47 | 0.42 | 0.63 |
| HDL-C(mg/dL) | 54.1 (16.1) | 56.0 (14.8) | 56.0 (17.5) | 45.8 (10.0) | 47.9 (10.6)* | 48.5 (11.4)* | 4.17 | 0.02 | 9.00 | 0.01 | 0.11 | 0.89 |
| LDL-C (mg/dL) | 109.6 (38.0) | 109.1 (44.8) | 113.2 (44.3) | 111.7 (32.1) | 108.7 (34.1) | 112.6 (32.6) | 1.43 | 0.24 | 0.01 | 0.96 | 0.20 | 0.79 |
| TC:HDL Ratio | 3.76 (1.38) | 3.60 (1.43) | 3.85 (1.52)‡ | 4.15 (1.05) | 3.96 (1.09)* | 4.09 (1.21) | 4.42 | 0.01 | 1.70 | 0.19 | 0.73 | 0.48 |
BMI, Body mass index; BP, blood pressure; HDL, High-density lipoprotein; LDL, Low-density lipoprotein; VLDL, Very low-density lipoprotein. Values are mean ± SD. Statistics based on imputed data.
Significant within-group differences from baseline (p < 0.05);
Significant within-group differences 12 weeks to 24 weeks (p < 0.05).
For the TC:.HDL ratio, there was a significant main effect of time (F(2,184 = 4.42), = 0.01); the main effect of group and the time–group interaction were not significant. From baseline to 12 weeks, both the FFL and TRAD groups saw a reduction in their TC:HDL ratio (FFL: t = 1.70, p = 0.10; TRAD: t = 2.42, p = 0.02). From 12 to 24 weeks, the FFL group saw a 2.4% increase in the TC:HDL ratio (t = −2.06, p = 0.05); the TRAD group saw a 13% decrease in TC:HDL ratio (t = 2.42, p = 0.02). For weight, there was a significant main effect of group; the main effect of time and the time–group interaction were not significant. For systolic BP, diastolic BP, BMI, TC, and LDL-C, neither the main effect of time, the main effect of group, or the time–group interaction were significant.
DISCUSSION
This is the first RCT, to our knowledge, to prospectively examine approaches to improve APFT in low-fit ARNG Soldiers. This study found that both the FFL and the TRAD programs improved the 2-mile run time and total APFT score of ARNG personnel modestly after a 12-week intervention. As a result, pass rates of 52% in FFL and 46% in the TRAD were observed in these soldiers who previously had failed to pass the APFT. Both groups, however, saw a reversion in these variables from 12-weeks to 24-week follow-up. This latter finding suggests that neither approach provided an adequate motivational arm for sustained benefits in ARNG members.
APFT failure rates (10%) of the Army Reserve are 2 times that of active duty soldiers (5.5–6.2%).29 In the spring of 2000, the APFT failure rate of the Maryland ARNG was 11 % for women and 16% for men. The vast majority of failures on the APFT (97%) were due to failing the run component of the test; in the current study, all individuals had failed the run.
The tenets of using a pedometer to motivate individuals to accumulate steps throughout the day have been used in previous sedentary civilian populations. A meta-analysis of 26 studies (8 RCTs and 18 observational studies) evaluated the effectiveness of pedometer use on PA and health outcomes among adults in an outpatient setting.10 Pedometer usage was associated with increased steps of approximately 2,000 per day (RCT: 2,491 steps/day over control; observational studies: 2,183 steps/day over baseline) and reductions in BMI and BP. There were no improvements in serum lipids or glucose. Predictors of increased PA by meta-regression were step goals (p = 0.001) and programs located outside the workplace (p = 0.02). Workplace programs were cited as attracting already active individuals. We targeted unfit individuals and saw increased daily steps walked in both pedometer-monitored and nonpedometer groups.
The FFL was designed for the reserve component (ARNG and Reserve) who works at their full-time civilian job and part-time as a citizen soldier in the military. Only one earlier military study retrospectively examined a program of monthly PT and command emphasis on APFT scores in an ARNG unit over a 6-month period.30 Memorandums, counseling, and informal conversations emphasized the command’s physical fitness policy and off-duty exercise. Command emphasis and PT during drill time were determined to be ineffective for improving APFT scores of ARNG soldiers.30
We found that although neither group sustained their improved 2-mile run time/score or total APFT score at 24 weeks, neither group regressed back to baseline values. Project ACTIVE, a 24-month RCT of 235 sedentary health adults, compared a gym-based exercise program to a lifestyle intervention that used pedometers to motivate and track steps. Both interventions had significant 6-month, 1-, and 2-year maintenance of improvements in PA, CV risk profile, and physical fitness; however, project ACTIVE study had a vigorous follow-up period and the sample was older (mean age 46 years).31–34 In this study of working adults with limited time for structured exercise, participants received only infrequent phone calls during the 12-week maintenance follow-up period, which could explain the difference in findings.
Some strengths of the current trial should be noted. Randomized intervention studies of military ARNG soldiers are rare, making the current findings relevant considering the current deployment rate of the reserve component. Furthermore, relatively few training studies have used pedometers as a motivational tool and objective measure of PA.
The limitations of this trial should also be recognized. Because this study included only ARNG soldiers drilling in Maryland and Washington, DC, our sample may not have been representative of the entire ARNG population. Further, ARNG soldiers who dropped out of the training program had lower baseline. APFT scores, suggesting that less fit individuals require more motivation to complete such a program. An additional limitation was the use of a self-report PA questionnaire to capture the levels of activity intensity (eg, moderate, hard, and very hard); self-reports are likely to overestimate performance compared to objective measures. Additionally, self-report methods may not account for activities less than 10 minutes in duration.35 Slight differences between pedometer step counts and self-reported PA may be related to the activity performed. The pedometer was removed during any water sports such as swimming.
Despite these limitations, the study demonstrates that a 12-week pedometer-driven behavioral intervention is as effective as the TRAD program for improving 2-mile run and total APFT score in ARNG soldiers who have failed the 2-mile run. The active duty military is currently so overextended that the National Guard and Reserve are supplying a substantial share of troops for operations in Iraq and Afghanistan. In these latter individuals, physical fitness and combat readiness are dependent to a large extent on civilian lifestyle patterns. Because a soldier’s level of physical fitness has a direct impact on combat readiness, the current findings highlight the need to explore various motivational methods to achieve and maintain higher levels of PA in these individuals.
ACKNOWLEDGMENTS
We thank the ARNG Volunteers in the FFL Study. This research was sponsored by the TriService Nursing Research Program, USUHS; however, the information or content and conclusions do not necessarily represent the official positions or policies of, nor should any official endorsement be inferred by, the TriService Nursing Research Program, the USUHS, the Department of Defense, or the U.S. Government (Award no. MDA 905-02-1-TS07; Project no. N02-007). USUHS, 4301 Jones Bridge Rd., Bethesda, MD 20814-4799, is the awarding and administering office.
We also acknowledge the Johns Hopkins Bayview General Clinical Research Center (which is funded by Department of Health and Human Services, National Institutes of Health [NIH], National Center for Research Resources, no. 5 MOI RR0279) for providing core laboratory and data management support and equipment, and the Intramural Research Program of the NIH, National Institute on Aging. Funding for this project was provided by Triservice Nursing Research Program, Johns Hopkins Bayview General Clinical Research Center, the Intramural Research Program of NIH, National Institute on Aging.
Footnotes
The views expressed in this article are those of the authors and do not reflect the official policies or positions of the Triservice Nursing Research Program, Uniformed Services University of the Health Sciences, the Department of Defense, National Institutes of Health, or the United States Government.
REFERENCES
- 1.Klerman JA: Rethinking the Reserves. Santa Monica, CA, RAND Corporation, 2008. [Google Scholar]
- 2.Davis L, Polich JM: Army stretched thin: There’s no easy way out for the nation. RAND Review. Summer 2005; 29(2): 12–5. [Google Scholar]
- 3.Government Accountability Office: Report to Congressional Committees: Military Personnel: Top Management Attention is Needed to Address Long-Standing Problems with Determining Medical and Physical Fitness of the Reserve Force Document No GAO-06–105. Washington, DC, GAO, October 27, 2005. [Google Scholar]
- 4.Talbot L, Weinstein A, Fleg J: Army Physical Fitness Test scores predict coronary heart disease risk in Army National Guard soldiers. Mil Med 2009; 174(3): 245–52. [DOI] [PubMed] [Google Scholar]
- 5.Stutts W: Physical activity determinants in adults. Perceived benefits, barriers, and self efficacy. Am Assoc Occup Health Nurse 2002; 50(11): 499–507. [PubMed] [Google Scholar]
- 6.Campbell J: Regional Trends: Multiple jobholdings in U.S. States in 2009. Monthly Labor Review. 2010. July; 133(7): 33/34. [Google Scholar]
- 7.GAO. Military Personnel: Top Management Attention is Needed to Address Long-Standing Problems with Determining Medical and Physical Fitness of the Reserve Force Document No GAO-06–105. Washington, DC, GAO, 2005. [Google Scholar]
- 8.Tudor-Locke C, Sisson S, Collova T, Lee S, Swan P: Pedometer-determined step count guidelines for classifying walking intensity in a young ostensibly healthy population. Can J Appl Physiol 2005; 30(6): 666–76. [DOI] [PubMed] [Google Scholar]
- 9.Dishman R, DeJoy D, Wilson M, Vandenberg R: Move to improve: a randomized workplace trial to increase physical activity. Am J Prev Med 2009; 36(2): 133–41. [DOI] [PubMed] [Google Scholar]
- 10.Bravata D, Smith-Spangler C, Sundaram V, et al. : Using pedometers to increase physical activity and improve health: a systematic review. JAMA 2007: 298(19): 2296–304. [DOI] [PubMed] [Google Scholar]
- 11.DeBusk S, Stenestrand U, Sheehan M, Haskell W: Training effects of long versus short bouts of exercise in healthy subjects. Am J Cardiol 1990; 65: 1010–13. [DOI] [PubMed] [Google Scholar]
- 12.Jakicic J, Wing R, Butler B, Robertson R: Prescribing exercise in multiple short bouts versus one continuous bout: effects on adherence, cardiorespiratory fitness and weight low in overweight women. Int J Obes Relat Metab Disord 1995; 19(12): 893–901. [PubMed] [Google Scholar]
- 13.Murphy M, Hardman A: Training effects of short and long bouts of brisk walking in sedentary women. Med Sci Sports Exerc 1998; 30: 152–7. [DOI] [PubMed] [Google Scholar]
- 14.Talbot L, Metter E, Fleg J: Leisure-time physical activities and their relationship to cardiorespiratory fitness in healthy men and women 18–95 years old. Med Sci Sports Exerc 2000; 32(2): 417–25. [DOI] [PubMed] [Google Scholar]
- 15.Wannamethee S, Shaper A: Physical activity in the prevention of cardiovascular disease: an epidemiological perspective. Sports Med 2001; 31(2): 101–14. [DOI] [PubMed] [Google Scholar]
- 16.Borg G: Borg’s Perceived Exertion and Pain Scales. Champaign, 1L, Human Kinetics, 1998. [Google Scholar]
- 17.Sallis J, Haskell W, Wood P, et al. : Physical activity assessment methodology in the Five-City Project. Am J Epidemiol 1985; 121(1): 91–106. [DOI] [PubMed] [Google Scholar]
- 18.Blair SN: How to assess exercise habits and rphysical fitness In: Behavioral Health: A Handbook of Health Enhancement and Disease Prevention, pp 424–47. Edited by Matarazzo JD, Weiss SM, Herd JA, Miller NE, Weiss WM. New York, John Wiley, 1984. [Google Scholar]
- 19.Dishman RK, Steinhardt M: Reliability and concurrent validity for a 7-d re-call of physical activity in college students. Med Sci Sports Exerc 1988; 20(1): 14–25. [DOI] [PubMed] [Google Scholar]
- 20.Bassett DR Jr, Ainsworth BE, Legett SR, et al. : Accuracy of five electronic pedometers for measuring distance walked. Med Sci Sports Exerc 1996; 28(8): 1071–7. [DOI] [PubMed] [Google Scholar]
- 21.Headquarters Department of the Army: Army Physical Fitness Training Physical Fitness Training (FM 21–20), pp 14–1–14–27. Washington, DC, Department of the Army, 1998. [Google Scholar]
- 22.Knapik J, Banderet L, Bahrke M, O’Connor J, Jones B, Vogel J: Army Physical Fitness Test (APFT): Normative Data on 6022 Soldiers Technical Report T94–7. Natick, MA, US: Army Research Institute of Environmental Medicine, 1994. [Google Scholar]
- 23.Kokkinos P, Holland J, Newman R, Fiest-Fite B, Signorino CE: Physical activity, smoking, alcohol consumtpion, body mass index, and plasma lipid profiles of military reserve officers. Mil Med 1989; 154: 600–3. [PubMed] [Google Scholar]
- 24.Knapik J: The Army physical fitness test (APFT): a review of the literature. Mil Med 1989; 154(6): 326–9. [PubMed] [Google Scholar]
- 25.Fedarko N: Laboratory Core. Baltimore, MD, Johns Hopkins Bayview Clinical Research Unit, 2010. Available at http://jhbgcrc.jhu.edu/Laboratory.cfm; accessed February 2007. [Google Scholar]
- 26.Greenhouse S, Geisser S: On methods in the analysis of profile data. Psychometrika 1959; 24: 95–112. [Google Scholar]
- 27.SPSS: SPSS Missing Value Analysis, Version 16.0. Chicago, SPSS, 2007. [Google Scholar]
- 28.Allison P: Missing Data. Thousand Oaks, CA, Sage Publications, 2002. [Google Scholar]
- 29.McHugh J: Active vs. Reserves: Who’s More Fit to Fight? Army Times. May 6, 1996: 12–3. [Google Scholar]
- 30.Powell G, Dumitru D, Kennedy J: The effect of command emphasis and monthly physical training on Army Physical Fitness Scores in a National Guard Unit. Mil Med 1993; 158(5): 294–7. [PubMed] [Google Scholar]
- 31.Tudor-Locke C: Taking steps toward increased physical activity: using pedometers to measure and motivate In: President’s Council on Physical Fitness and Sports: Research Digest, pp 1–7. Edited by Corbin C, Pangrazi R. Washington, DC, PCPFS, 2002. [Google Scholar]
- 32.Dunn AL, Marcus BJ, Kampert JB, Garcia ME, Kohl HW, Blair SN: Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: a randomized trial. JAMA 1999; 281(4): 327–34. [DOI] [PubMed] [Google Scholar]
- 33.Dunn A, Marcus B, Kampert J, Garcia M, Kohl H, Blair S: Reduction in cardiovascular disease risk factors: 6-month results from project Active. Prev Med 1997; 26: 883–92. [DOI] [PubMed] [Google Scholar]
- 34.Dunn AL, Andersen RE, Jakicic JM: Lifestyle physical activity interventions: history, short- and long-term effects, and recommendations. Am J Prev Med 1998; 15(5): 398–412. [DOI] [PubMed] [Google Scholar]
- 35.Tudor-Locke C, Myers A: Challenges and opportunities for measuring physical activity in sedentary adults. Sports Med 2001; 31: 91–100. [DOI] [PubMed] [Google Scholar]