Abstract
Staphylococcus simulans is a coagulase-negative organism, mainly an animal pathogen. Reports of human infection have been infrequent, mainly in patients with repeated animal contact. We report the first case of pleural empyema in an elderly woman. S. simulans tends to cause more severe infection because of a biofilm layer which helps in adherence and colonization of smooth surfaces, especially prosthetic devices, shunts, and catheters. The challenging problem even after CoNS isolation and identification is the assessment of their clinical relevance. Major factors that inhibit the penetration of antibiotics is the large-sized effusions/empyema, thickness of pleura, and the nature of antibiotic itself. Source control for septic patients remains the cornerstone of treatment along with optimal antimicrobial coverage. Staphylococcus simulans, a coagulase-negative staphylococcus, is emerging as an important cause of virulent infections with high mortality in humans. Given its propensity for multidrug resistance, including vancomycin, there is an imperative for early and accurate identification of the isolate. Despite aggressive treatment, the patient succumbed to her illness.
1. Introduction
Staphylococcus simulans is a coagulase-negative staphylococcus. It is mainly an animal pathogen and has been found to cause bovine mastitis. It can occasionally colonize the human skin. Human infections with Staphylococcus simulans have rarely been reported, mainly in patients who have repeated contact with animals. We report the first case of pleural empyema caused by S. simulans.
1.1. Case Report
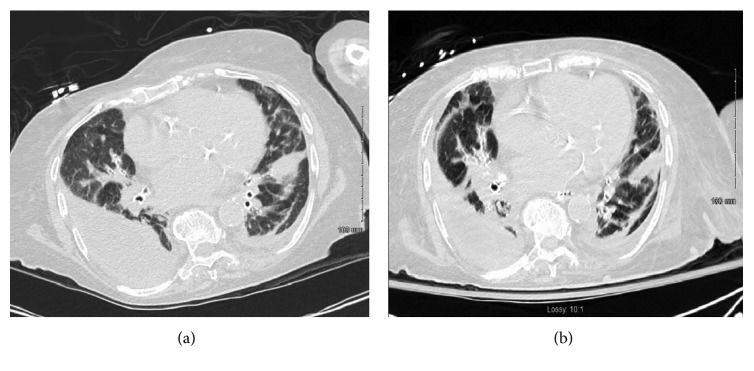
An 80-year-old woman was admitted to the hospital after a fall. Her prior history was notable for coronary artery disease status post percutaneous intervention, poorly controlled type 2 diabetes mellitus, congestive heart failure, hypothyroidism, and atrial fibrillation. She had had multiple mechanical falls in the past with cervical spine and right-sided rib fractures. She had no recent hospitalization in the last 90 days and has been living at home prior to presentation. There was no history of exposure to the farm animals. During this hospitalization, she developed progressive dyspnea and hypoxia. Computed tomography (CT) revealed a bilateral pleural effusion, right more than left, with diffuse interlobular septal thickening. Note was also made of a diffuse, mosaic-like attenuation of the lung parenchyma, likely related to air trapping or obstructive small airway disease. There was no pleural enhancement, septations, or air noted within the pleural space (Figure 1(a)). She was noted to have new fracture of right posterior seventh, eighth, and ninth ribs. Laboratory data at admission revealed a white blood cell (WBC) count of 9.7 × 1000/µL (with 83% neutrophils and 1% eosinophils). Her hemoglobin was 11.09 g/dL, hematocrit 40.6%, platelets 143 × 1000/µL, total protein 5.1 g/dL, blood urea nitrogen (BUN) 31 mg/dL, serum creatinine 1.51 mg/dL, serum sodium (Na) 145 mEq/L, chloride (Cl) 102 mEq/L, potassium (K) 3.6 mEq/L, aspartate aminotransferase (AST) 24 IU/L, and lactate dehydrogenase (LDH) 472 IU/L. Serum procalcitonin levels were elevated to 0.59 ng/mL (normal 0.00 – 0.08 ng/mL) and hemoglobin A1C (HbA1C) to 8.9%.
Figure 1.
(a) CT chest showing bilateral empyema (right more than left). (b) CT chest showing persistent bilateral empyema after attempted drainage through chest drains.
Blood cultures prior to initiation of antimicrobial therapy returned negative. Sputum culture was negative for bacteria, including acid-fast bacilli. Transthoracic echocardiography was unremarkable.
The patient was treated initially with levofloxacin and ampicillin/sulbactam for a pneumonia and parapneumonic pleural effusion. Despite antimicrobial therapy, her respiratory status continued to deteriorate and within 48 hours of hospitalization required endotracheal intubation and ventilatory support. A thoracentesis yielded 250 ml of pus (WBCs more than 50,000 with 95% neutrophils, elevated protein 3.6 g/dL (normal 0.0–2.4 g/dL), LDH 13461 IU/L, glucose 6 mg/dL, and pH 6.94). A right-sided thoracostomy was performed to facilitate evacuation of the empyema using a 32 French (F) thoracostomy tube. Postprocedure chest X-ray confirmed the optimal placement of the tube (Figure 2). Gram stains obtained from the pleural fluid collected under sterile conditions revealed gram-positive cocci, and her antibiotics were changed to vancomycin. The final isolate on culture and sensitivity was identified as S. simulans with heavy growth, susceptible to vancomycin and clindamycin only. A repeat CT scan of the chest revealed a persistent collection of right-sided empyema (Figure 1(b)). Ultrasound imaging of the pleural collections did not demonstrate any septations or loculated pockets on either side. Second attempt was made to evacuate the pleural collection with the use of intrapleural fibrinolytic tissue plasminogen activator (t-PA) with little success. The patient was considered a high-risk candidate for surgical intervention considering her frailty and other medical comorbidities. Her course was further complicated by circulatory shock requiring vasopressor supports and atrial fibrillation with rapid ventricular response requiring multiple rate-controlling drugs. After about 3 weeks of a tenuous course, her family elected to withdraw care and she passed away very shortly thereafter.
Figure 2.
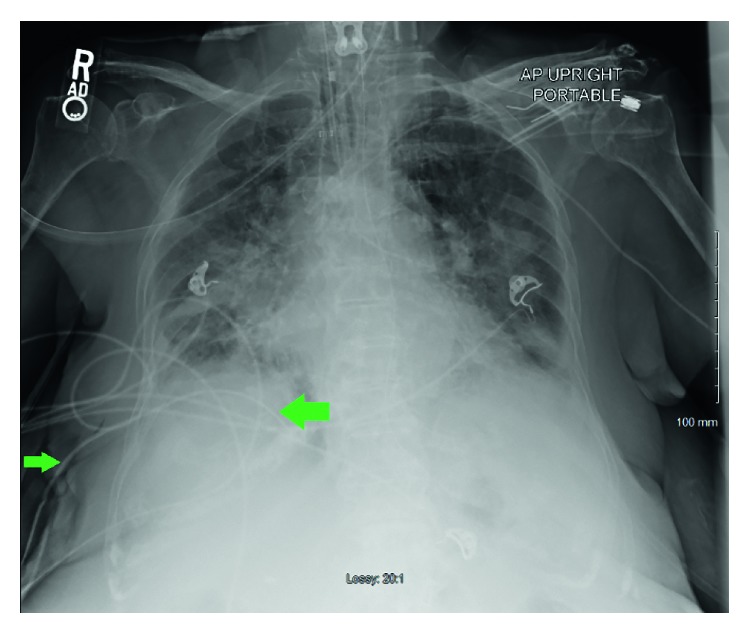
Chest X-ray showing the right-sided chest tube (green arrows), positioned in the most dependent area.
2. Discussion
Coagulase-negative staphylococcus (CoNS) has become an important cause of nosocomial infections. Common human isolates are Staphylococcus epidermidis, Staphylococcus capitis, Staphylococcus hominis, Staphylococcus haemolyticus, Staphylococcus warneri, Staphylococcus caprae, Staphylococcus saccharolyticus, Staphylococcus pasteuri, Staphylococcus saprophyticus, and Staphylococcus lugdunensis [1].
S. simulans commonly affects cows, sheep, goats, and horses. Human infections are rare, and the literature has commonly reported soft tissue infection, osteomyelitis, bacteremia, urinary tract infection, prosthetic joint infection, and native valve endocarditis [1–8] (Table 1). A case of pneumonia was reported by de Jesus et al. which revealed S. simulans in blood culture and CoNS in sputum culture [2]. de Jesus et al. also reported a case of acute respiratory failure, ARDS with blood culture growing S. simulans [2]. To the best of our knowledge, this is the first case of pleural empyema caused by S. simulans. In our patient, there was no history of contact with animals. Mode of acquisition of infection in our patient remained unclear.
Table 1.
| Author | Age/sex | Diagnosis | Tissue culture for S. simulans | Blood culture for S. simulans | Antibiotic resistance | Outcome | Animal exposure |
|---|---|---|---|---|---|---|---|
| Shields et al. [5] | 80/M | Right great toe cellulitis | Positive | Not specified | Tetracycline resistance | Resolution with TMP-SMX | Not specified |
| Tous Romero et al. [6] | 60/M | Pyoderma left hand | Positive | Not specified | Not specified | Resolution with azithromycin | Positive |
| Al Kline et al. [8] | 65/M | Abscess, osteomyelitis right foot | Positive bone culture | Positive | Ampicillin, ciprofloxacin, clindamycin, oxacillin, penicillin, ceftriaxone | Resolution with IV vancomycin | Positive |
| Vallianou et al. [3] | 46/M | Vertebral osteomyelitis, native valve, endocarditis | Not specified | Positive | Methicillin | Resolution with IV vancomycin, teicoplanin, oral clindamycin | Positive |
| Sturgess et al. [7] | 77/F | Right pubic osteomyelitis | Not specified | Positive | Pan-sensitive | Resolution with flucloxacillin, fusidic acid | Not specified |
| de Jesus et al. [2] | 84/M | Septicemia, colon cancer | Not specified | Positive | Methicillin-sensitive | Died | Not specified |
| de Jesus et al. [2] | 41/M | Acute respiratory failure, ARDS, H/O HIV, IV drug abuse | Not specified | Positive | Methicillin-sensitive | Died | Not specified |
| de Jesus et al. [2] | 63/M | Pneumonia | CN staph in sputum | Positive for S. simulans | Not specified | Resolved with erythromycin, cefuroxime | Not specified |
| de Jesus et al. [2] | 58/M | Colon cancer, septicemia | Not specified | Positive | Methicillin-resistant | Resolved with vancomycin | Not specified |
| Males et al. [1] | 39/M | Right ankle, osteomyelitis, septic, arthritis | Positive | Positive | Pan-sensitive | Penicillin | Not specified |
S. simulans tends to cause more severe infection because of a biofilm layer which helps in adherence and colonization of smooth surfaces, especially prosthetic devices, shunts, and catheters [8]. S. simulans has also been shown to share virulence factors with S. aureus in infectious animal isolates, including staphylococcal enterotoxins, tissue necrosis cytotoxin Panton–Valentine leukocidin, and the methicillin-resistance gene, mecA [5]. The encapsulated forms of S. simulans (i.e., slime layer or biofilm) have an antiphagocytic effect on human polymorphonuclear leucocytes as compared to unencapsulated forms of the pathogen [8]. Sequencing of the tuf gene has been shown to be the most accurate for the species identification of CoNS [9].
The critical event in the establishing the pathogenicity includes formation of multilayered biofilm, especially in foreign body-associated infections caused by CoNS. Members of the genus Staphylococcus produce various proteinaceous and nonproteinaceous adhesins, to mediate attachment to host surfaces, such as plasma extracellular and matrix proteins or even host cells [10, 11].
There are limited data available about how CoNS which are usually common pathogens in veterinary medicine are gaining pathogenicity in human hosts. There are some shared virulence factors with Staphylococcus aureus which are documented in Table 2 [5, 12–14]. Of note, mecA-positive CoNS are capable to horizontally transfer their genes inside the staphylococcal genus with the prospective to contribute increase in new methicillin-resistant strains [12].
Table 2.
| Staphylococcal species | Common virulence factors | Clinical manifestations |
|---|---|---|
| S. aureus and S. simulans | Staphylococcal enterotoxins (se) | Gastrointestinal manifestations of diarrhea, nausea, vomiting, and enterocolitis. |
| Tissue necrosis cytotoxin Panton–Valentine leukocidin (pvl) | Hospital-acquired pneumonia, infective endocarditis, and tissue necrosis | |
| Methicillin-resistance gene (mecA) | Major contributing factor for increase in new methicillin-resistant strains | |
| Exfoliative toxins (eta, etb) | Cutaneous manifestations of cellulitis | |
| Toxic shock syndrome toxin-1 (tst) | Septic shock and disseminated blood stream infections |
The challenging problem even after CoNS isolation and identification is the assessment of their clinical relevance. The major diagnostic question remains as to whether the CoNS isolate represents a contamination of the specimen, physiological colonization of the skin or mucus membranes, or a clinically significant infection. In our case, the absence of other microbiological data and the confidence in the sterile process of procuring the sample from pleural fluid warranted consideration of S. simulans in the pleural fluid as pathogenic. Important considerations include isolation of a strain in pure culture from the site of infection and repeated isolation of the same strain over the course of infection [11, 15].
While treating the pleural infections, clinicians need to be cognizant of the choice of antimicrobial therapy and relevant pharmacokinetics. Major factors that inhibit the penetration of antibiotics is the large-sized effusions/empyema, thickness of pleura, and the nature of antibiotic itself; acute inflammation is proven to be a supporting factor due to vasodilation [16, 17]. Teixeira et al. demonstrated that penicillin has the best penetration for the treatment of pleural pathologies, followed by metronidazole; gentamicin was found to have poor penetration and considered a poor choice for treatment of empyemas [16].
S. simulans is known to demonstrate resistance to multiple antibiotics including vancomycin [2]. In our case, the organism was resistant to ampicillin/sulbactam, cefazolin, ciprofloxacin, oxacillin, and tetracycline, but it was susceptible to vancomycin in vitro. The use of vancomycin in pleural infections has long been debated due to its suboptimal penetration; however, in our case, the multidrug-resistant nature of the isolate required its use. It is debatable in retrospect if continuation of a broader antimicrobial coverage would have changed the outcome for the patient, considering poor biochemical and clinical response with the chosen antibiotic regimen.
Source control for septic patients remains the cornerstone of treatment along with optimal antimicrobial coverage. The MIST-2 study reiterated the fact where use of t-PA and DNase combination therapy in patients with pleural infection improved drainage of pleural empyema, resulting in reduction in hospital stay and need for thoracic surgery intervention [18].
3. Conclusion
Staphylococcus simulans, a coagulase-negative staphylococcus, is emerging as an important cause of virulent infections with high mortality in humans. Given its propensity for multidrug resistance, including vancomycin, there is an imperative for early and accurate identification of the isolate.
Conflicts of Interest
All authors claim no conflicts of interest.
Authors' Contributions
AL conceived the study, drafted the manuscript, collected data, and reviewed and revised the study. JA collected the data, drafted the manuscript, and reviewed the study. AU collected the data, drafted the manuscript, and reviewed the study. GMA conceived the study, drafted the manuscript, and reviewed the study.
References
- 1.Males B. M., Bartholomew W. R., Amsterdam D. Staphylococcus simulans septicemia in a patient with chronic osteomyelitis and pyarthrosis. Journal of Clinical Microbiology. 1985;21(2):255–257. doi: 10.1128/jcm.21.2.255-257.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Jesus L., Caruso G., de Caprariis P., Ditchek A., Visconti E. Staphylococcus simulans septicemia. Infectious Diseases in Clinical Practice. 1993;2(5):351–352. doi: 10.1097/00019048-199309000-00008. [DOI] [Google Scholar]
- 3.Vallianou N., Evangelopoulos A., Makri P., et al. Vertebral osteomyelitis and native valve endocarditis due to Staphylococcus simulans: a case report. Journal of Medical Case Reports. 2008;2(1):p. 183. doi: 10.1186/1752-1947-2-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Razonable R. R., Lewallen D. G., Patel R., Osmon D. R. Vertebral osteomyelitis and prosthetic joint infection due to Staphylococcus simulans. Mayo Clinic Proceedings. 2001;76(10):1067–1070. doi: 10.4065/76.10.1067. [DOI] [PubMed] [Google Scholar]
- 5.Shields B. E., Tschetter A. J., Wanat K. A. Staphylococcus simulans: an emerging cutaneous pathogen. JAAD Case Reports. 2016;2(6):428–429. doi: 10.1016/j.jdcr.2016.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tous Romero F., Gutierrez Garcia-Rodrigo C., Velasco Tamariz V., Llamas Martin R. Acute infection by Staphylococcus simulans in the hand of a man. JAMA Dermatology. 2016;152(9):p. 1060. doi: 10.1001/jamadermatol.2016.0959. [DOI] [PubMed] [Google Scholar]
- 7.Sturgess I., Martin F. C., Eykyn S. Pubic osteomyelitis caused by Staphylococcus simulans. Postgraduate Medical Journal. 1993;69(818):927–929. doi: 10.1136/pgmj.69.818.927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al Kline D. Staphylococcus simulans osteomyelitis of the foot: a case report. Foot and Ankle Online Journal. 2010;3(1) [Google Scholar]
- 9.Carpaij N., Willems R. J., Bonten M. J., Fluit A. C. Comparison of the identification of coagulase-negative staphylococci by matrix-assisted laser desorption ionization time-of-flight mass spectrometry and tuf sequencing. European Journal of Clinical Microbiology and Infectious Diseases: Official Publication of the European Society of Clinical Microbiology. 2011;30(10):1169–1172. doi: 10.1007/s10096-011-1204-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heilmann C. Advances in Experimental Medicine and Biology. Basel, Switzerland: Springer Nature; 2011. Adhesion mechanisms of staphylococci; pp. 105–123. [DOI] [PubMed] [Google Scholar]
- 11.Becker K., von Eiff C. Manual of Clinical Microbiology. Washington, DC, USA: American Society of Microbiology; 2011. Staphylococcus, micrococcus, and other catalase-positive cocci; pp. 308–330. [Google Scholar]
- 12.Unal N., Cinar O. D. Detection of stapylococcal enterotoxin, methicillin-resistant and panton-valentine leukocidin genes in coagulase-negative staphylococci isolated from cows and ewes with subclinical mastitis. Tropical Animal Health and Production. 2012;44(2):369–375. doi: 10.1007/s11250-011-0032-x. [DOI] [PubMed] [Google Scholar]
- 13.Davis M. F., Cain C. L., Brazil A. M., Rankin S. C. Two coagulase-negative staphylococci emerging as potential zoonotic pathogens: wolves in sheep’s clothing? Frontiers in Microbiology. 2013;4:p. 123. doi: 10.3389/fmicb.2013.00123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lina G., Piemont Y., Godail-Gamot F., et al. Involvement of Panton-Valentine leukocidin-producing Staphylococcus aureus in primary skin infections and pneumonia. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 1999;29(5):1128–1132. doi: 10.1086/313461. [DOI] [PubMed] [Google Scholar]
- 15.Chatzika K., Manika K., Kontou P., et al. Moxifloxacin pharmacokinetics and pleural fluid penetration in patients with pleural effusion. Antimicrobial Agents and Chemotherapy. 2014;58(3):1315–1319. doi: 10.1128/aac.02291-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Teixeira L. R., Sasse S. A., Villarino M. A., Nguyen T., Mulligan M. E., Light R. W. Antibiotic levels in empyemic pleural fluid. Chest. 2000;117(6):1734–1739. doi: 10.1378/chest.117.6.1734. [DOI] [PubMed] [Google Scholar]
- 17.Valcke Y., Pauwels R., Van der Straeten M. Pharmacokinetics of antibiotics in the lungs. European Respiratory Journal. 1990;3(6):715–722. [PubMed] [Google Scholar]
- 18.Rahman N. M., Maskell N. A., West A., et al. Intrapleural use of tissue plasminogen activator and DNase in pleural infection. New England Journal of Medicine. 2011;365(6):518–526. doi: 10.1056/nejmoa1012740. [DOI] [PubMed] [Google Scholar]