Abstract
Background
Medicare's Hospital Readmissions Reduction Program assesses financial penalties to hospitals based on risk‐standardized readmission rates after specific episodes of care, including acute myocardial infarction. Detailed information about the type of patients included in the penalty is unknown.
Methods and Results
Starting with administrative data from Medicare, we conducted physician‐adjudicated chart reviews of all patients considered 30‐day readmissions after acute myocardial infarction from July 2012 to June 2015. Of 197 readmissions, 68 (34.5%) received percutaneous coronary intervention and 18 (9.1%) underwent coronary artery bypass grafting on index hospitalization. The remaining 111 patients did not receive any intervention. Of the 197 patients, 56 patients (28.4%) were considered too high risk for invasive management, 23 (11.7%) had nonobstructive coronary artery disease on diagnostic catheterization and therefore no indication for revascularization, 19 patients had a type II myocardial infarction (9.6%) for which noninvasive, outpatient workup was recommended, and 13 (6.6%) declined further care. The most common readmission diagnoses were cardiac causes and noncardiac chest discomfort, infection, and gastrointestinal bleeding.
Conclusions
Our results demonstrate that more than a quarter of the patients included in the penalty do not receive revascularization either because of provider assessment of risk or patient preference, and nearly one tenth have type II myocardial infarction. As such, administrative codes for prohibitive procedural risk, patient‐initiated “do not resuscitate” status, or type II myocardial infarction may improve the risk‐adjustment of the metric. Furthermore, provider organizations seeking to reduce readmission rates should focus resources on the needs of these patients, such as care coordination, hospice services when requested by patients, and treatment of noncardiac conditions.
Keywords: acute myocardial infarction, cardiovascular disease, medication therapy, readmission, revascularization
Subject Categories: Quality and Outcomes, Cardiovascular Disease, Percutaneous Coronary Intervention, Revascularization
Clinical Perspective
What Is New?
Of patients readmitted to acute care after acute myocardial infarction included in Medicare's readmission penalties, over one half do not receive revascularization during the index hospitalization.
More than a third of these patients either are deemed too high risk for invasive management or themselves articulate limited goals of care during the initial hospitalization.
About one tenth of these patients have type II myocardial infarction.
What Are the Clinical Implications?
Administrative codes for prohibitive procedural risk, patient initiated “do not resuscitate” status, and type II myocardial infarction may improve the risk‐adjustment of readmission metrics.
Patients who decline recommended revascularization should be counseled that they could have cardiac symptoms after hospital discharge, including angina and heart failure.
Provider organizations seeking to reduce readmission rates should focus resources on the needs of nonrevascularized patients, such as care coordination, hospice services when requested by patients, and treatment of noncardiac conditions.
Introduction
The Hospital Readmissions Reduction Program (HRRP) was created in attempt to reduce preventable 30‐day hospital readmissions. As part of the Affordable Care Act of 2010, HRRP applies financial penalties to hospitals based on risk‐standardized readmission rates following hospitalization for specific conditions.1 After a 3‐year performance period, hospitals are provided lists of specific patients readmitted that count towards the financial penalty. One of the first episodes of care identified for the penalty was all‐cause 30‐day readmission after acute myocardial infarction (AMI). Patients eligible for the penalty are those who have a principal billing diagnosis of AMI during an index hospitalization and who are in a fee‐for‐service Medicare insurance plan.
AMI was included in the HRRP because it is expensive,2 common, and associated with high and variable readmission rates; causes of readmission after AMI may also include several that might be addressed with novel follow‐up strategies. In 2013, the median hospital risk‐standardized payment for AMI readmission was $21 994 according to Medicare claims data.3 From 2011 to 2014, the median 30‐day readmission rate of patients with AMI was 17.7% with a large absolute difference of 7.5% across all hospitals, suggesting that quality differences between hospitals may influence readmission rates.3
After the passage of HRRP as part of health reform in 2010, large analyses of administrative data have shown that readmission rates after AMI decreased faster than they had been decreasing before the law.4, 5, 6 Because distinguishing these types of different patients with AMI is difficult from administrative data, it is not known what specific tactics have reduced readmissions or could further improve performance in the future. Therefore, more granular understanding of the clinical characteristics and chief complaint of patients included in the actual penalty is essential, both for provider organizations seeking to improve performance and for policymakers seeking to evaluate the utility of this quality metric. In the setting of these unanswered questions, we conducted chart reviews of patients who contributed to the penalty to better understand types of patients with AMI who count towards the actual penalty, as well as reasons for readmission for these patients.
Methods
Our study population included all patients who contributed to the HRRP penalty at our institution during the July 2012 to June 2015 penalty period. This 3‐year penalty period determined the hospital financial penalty for the fiscal year 2016.
Information provided by Centers for Medicare and Medicaid Services included medical record number, date of birth, sex, date of index hospitalization and date of readmission, and general medical comorbidities as determined from administrative data. In addition, chart reviews of patients were conducted by a physician (L.M.M.). From chart reviews, all patients with AMI were categorized as Type I non–ST‐segment–elevation myocardial infarction (NSTEMI), Type II NSTEMI, or STEMI. Demographic and clinical characteristics of patients in these categories were compared using χ2 tests or Fisher exact test for categorical variables and ANOVA for continuous variables. Furthermore, the chart reviewer also recorded whether patients received medical management, percutaneous coronary intervention (PCI), or coronary artery bypass grafting (CABG). The medical management category included (1) patients who were considered to be too high risk to undergo revascularization; (2) patients who received diagnostic catheterization that did not show obstructive coronary artery disease; (3) patients who had a type II NSTEMI for which noninvasive, outpatient cardiac workup was recommended; and (4) patients who declined catheterization.
For patients readmitted to the index hospital or a network affiliate within the shared electronic health record, cause of readmission and hospital of readmission were recorded. Specific causes of readmission were grouped into larger categories. Categories with <3 patients each were categorized as “other.”
Index diagnosis, index intervention, and readmission diagnosis were summarized using Pivot tables. We excluded patients who were not admitted to inpatient status, unable to be matched to a medical record number, and those who did not have AMI by the universal definition.7 We calculated the mean Charlson Comorbidity Index of our sample population using an online calculator excluding age as a variable (https://www.mdcalc.com/charlson-comorbidity-index-cci).
This project was approved by Partners Healthcare Institutional Review Board. Since this was a retrospective analysis of existing patient data, the requirement for informed consent was waived. The data, analytic methods, and study materials will not be made available to other researchers for purposes of reproducing the results.
Results
Of 200 patients, 3 were excluded (1.5%) as 1 was readmitted to the emergency department observation unit rather than inpatient care, 1 was unable to be matched to a medical record number, and 1 did not meet criteria for AMI during the index hospitalization. The 197 patients remaining were included in the analytic cohort. The average age was 77.7 years (±7.3), 40.6% (80/197) of the study population were female, and 90.4% (178/197) were white (Table). On average, patients had smoked 37 (±23) pack years, had an average low‐density lipoprotein cholesterol of 78.2 (±34.5) mg/dL, average creatinine of 1.30 (±0.62) mg/dL, and average hemoglobin A1C of 6.4% (±1.19). On index admission, 82.7% (163/197) had no restrictions on goals of care at beginning of index hospitalization (Table). Of all included patients, 148/197 (75.1%) had Type I NSTEMIs, 29/197 patients (14.7%) had STEMIs, and 20/197 (10.2%) had Type II NSTEMIs. The median length of stay for this population was 7.0 days on index hospitalization (interquartile range, 4–11 days) and the mean Charlson Comorbidity Index was 5.3±3.1. Demographic and clinical characteristics of these patients, divided by type of AMI, are described in Table.
Table 1.
Demographics and Clinical Characteristics of Patients Readmitted to Index Hospital Within 30 Days Post AMI
| Characteristics | All Patients (n=197) | Type I NSTEMI (n=148) | Type II NSTEMI (n=20) | STEMI (n=29) | P Value |
|---|---|---|---|---|---|
| Age, mean, SD | 77.7 (7.3) | 77.6 (7.3) | 78.3 (7.9) | 77.7 (7.1) | 0.94 |
| Women, % | 80 (41) | 63 (43) | 6 (30) | 11 (38) | 0.53 |
| Smoking, mean pack y, SD | 37 (23) | 36 (22) | 49 (29) | 30 (19) | 0.040 |
| LDL, mean, SD | 78.2 (34.5) | 78.0 (31.1) | 68.9 (26.9) | 85.9 (51.4) | 0.24 |
| Cr, mean, SD | 1.30 (0.62) | 1.36 (0.66) | 1.10 (0.41) | 1.11 (0.39) | 0.070 |
| HbA1C, mean, SD | 6.4 (1.19) | 6.47 (1.27) | 6.39 (1.04) | 6.03 (0.78) | 0.18 |
| Full code, % | 163 (82.7) | 128 (86.4) | 12 (60) | 23 (79.3) | 0.011 |
| Black | 1 (1) | 0 (0) | 1 (5) | 0 (0) | 0.10 |
| Hispanic | 4 (2) | 2 (1) | 2 (10) | 0 (0) | 0.082 |
| White | 178 (91) | 135 (91) | 16 (80) | 27 (93) | 0.22 |
| Asian | 3 (2) | 1 (1) | 1 (5) | 1 (3) | 0.15 |
| Other | 11 (6) | 10 (7) | 0 (0) | 1 (3) | 0.66 |
AMI indicates acute myocardial infarction; Cr, creatinine; HbA1C, hemoglobin A1C; LDL, low‐density lipoprotein; NSTEMI, non–ST‐segment–elevation myocardial infarction; STEMI, ST‐segment–elevation myocardial infarction.
Patients Receiving Revascularization During Index Hospitalization
Among all study patients, 86/197 (43.7%) underwent revascularization (Figure 1). Of these, the majority (68/86, 79.1%) were revascularized using PCI. Of the patients who received PCI, during index hospitalization, 50/68 (73.5%) had Type I NSTEMIs, 1/68 (1.5%) had a Type II NSTEMI, and 17/68 (25%) had STEMIs. All patients who underwent CABG had STEMIs (18/18, 100%).
Figure 1.
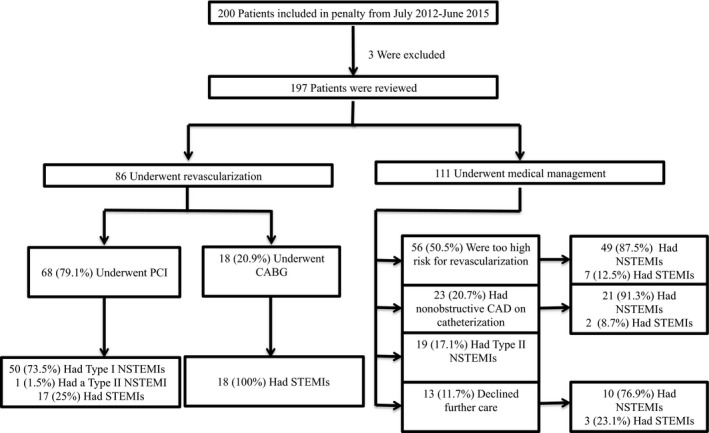
Eligibility, index intervention, and AMI diagnosis of our patient population. AMI indicates acute myocardial infarction; CABG, coronary artery bypass graft; CAD, coronary artery disease; NSTEMI, non–ST‐segment–elevation myocardial infarction; PCI, percutaneous coronary intervention.
Patients Receiving Medical Management Only During Index Hospitalization
Of all patients, 111/197 (56.3%) received medical management during index hospitalization. Among medically managed patients, 56/111 (50.5%) were deemed too high risk to undergo PCI/CABG. Revascularization was declined for the following reasons: (1) 37 had poor performance status because of dementia, metastatic cancer, gastrointestinal bleeding, stroke, or kidney disease; (2) 15 patients had multivessel disease but were considered to be nonsurgical patients; (3) 3 patients presented with a missed MI (3); and (4) 1 patient had an MI precipitated by cocaine use. Twenty‐three patients (20.7%) underwent catheterization but were managed medically because of nonobstructive coronary artery disease. The remaining 19 patients who were medically managed (19/111, 17.1%) were not revascularized because of Type II NSTEMI and 13 patients (11.7%) declined further care.
Causes of Readmission According to Index Hospitalization Clinical Management Categories
Of the 161 within‐network readmissions, the most common reasons for readmission were (1) concern for cardiac causes or noncardiac chest discomfort (68/161, 42.2%), (2) infection (36/161, 22.4%), and (3) gastrointestinal bleeding (15/161, 9.3%) (Figure 2). For CABG patients, the most common reason for readmission was infection (7/16, 43.8%, Figure 3), the second most common reason for readmission was cardiac (3/16, 18.8%), and the third most common reason for readmission was shortness of breath (2/16, 12.5%). For PCI patients, the most common reason for readmission was cardiac (25/57, 43.9%), the second most common reason for readmission was infection (10/57, 17.5%), and the third most common reason for readmission was gastrointestinal bleeding (6/57, 10.5%). For patients deemed too high risk for intervention on index stay, the most common reason for readmission was cardiac (21/45, 46.7%), the second most common reason for readmission was infection (10/45, 22.2%), and the third most common reason for readmission was gastrointestinal bleeding (5/45, 11.1%). For patients with nonobstructive coronary disease, the most common reason for readmission was cardiac (7/18, 38.9%), the second most common reason for readmission was infection (3/18, 16.7%), and the third most common reason for readmission was “other” (2/18, 11.1%). For patients with Type II NSTEMI, the most common reason for readmission was cardiac (5/15, 33.3%), the second most common reason for readmission was infection (4/15, 26.7%), and the third most common reason for readmission was gastrointestinal bleeding (2/15, 13.5%). For patients who declined intervention on index hospitalization, the most common reason for readmission was cardiac (7/10, 70.0%), the second most common reason for readmission was infection (2/10, 20.0%), and the third most common reason for readmission was stroke/transient ischemic attack (1/10, 10%).
Figure 2.
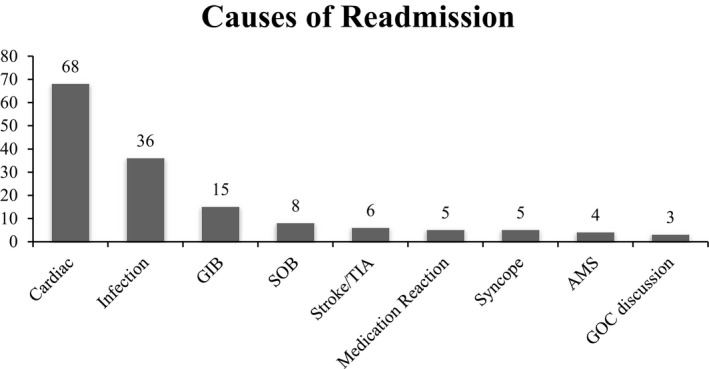
Causes of readmission within 30 days of readmitted AMI patients (N=161). Causes of readmission with n<3 were excluded (N=11). AMS indicates altered mental status; GIB, gastrointestinal bleeding; GOC, goals of care; SOB, shortness of breath; TIA, transient ischemic attack.
Figure 3.
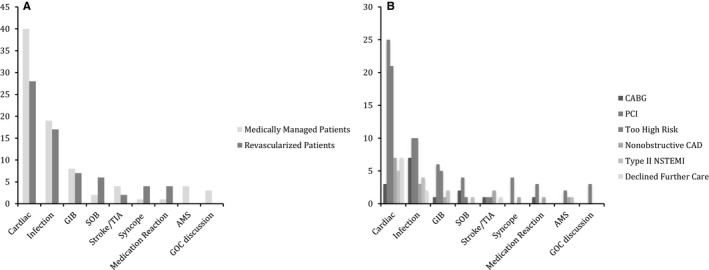
Causes of readmission grouped by management during index stay. A, Causes of readmission grouped by patients medically managed and revascularized during index stay. B, Shows causes of readmission grouped by specific index hospitalization clinical management categories. Causes of readmission with n<3 were excluded. AMS indicates altered mental status; CABG, coronary artery bypass graft; CAD, coronary artery disease; GIB, gastrointestinal bleeding; GOC, goals of care; NSTEMI, non–ST‐segment–elevation myocardial infarction; PCI, percutaneous coronary intervention; SOB, shortness of breath; TIA, transient ischemic attack.
Cardiac causes and noncardiac chest discomfort accounted for 68 of the 161 readmissions (42.2%). Of the 68 patients readmitted with concerns for all causes of cardiac or noncardiac chest discomfort, 32/68 (47.1%) presented with chest discomfort. Of these patients, 20/32 (62.5%) were medically managed on index stay. Among those medically managed patients, 10 (31.3%) were too high risk for revascularization, 5 (15.6%) declined further care, 3 (9.4%) had a Type II NSTEMI, and 2 (6.3%) had nonobstructive coronary artery disease. Among revascularized patients, 12 (37.5%) presenting with chest discomfort on readmission underwent PCI on index stay and no patients who underwent CABG on index stay represented with chest discomfort.
Other causes of cardiac‐related readmissions included congestive heart failure exacerbations (26/68, 38.2%), arrhythmias (8/68, 11.8%), and hypertension (2/68, 2.9%). Among patients readmitted for a congestive heart failure exacerbation, 16/26 (61.5%) were medically managed on index stay. Specifically, 9 (34.6%) were too high risk for revascularization, 5 (15.4%) had nonobstructive coronary artery disease, 2 (7.7%) had a Type II NSTEMI, and 1 (3.9%) declined further care on index stay. Among revascularized patients representing with a congestive heart failure exacerbation, 9 (34.6%) underwent PCI, and 1 (3.9%) underwent CABG on index stay.
Discussion
In this analysis of readmitted patients with AMI included in the HRRP, we demonstrate that the HRRP penalties affect large proportions of patients who do not receive revascularization during the index hospitalization. In particular, many patients are deemed too high risk for intervention by clinicians or they themselves decline intervention. Additionally, more than one tenth of the patients considered under the penalty had Type II MI, a diagnosis without defined treatment strategies and until recently lacking its own ICD10 code.
Our work confirms and extends previous knowledge about readmissions after AMI. Previous work has shown that chest pain, infection, and gastrointestinal bleeding are common causes of readmission after AMI,8, 9 which is consistent with our work. In addition, more medically managed patients were readmitted compared with patients who were revascularized.8, 10 Our results suggest that our sample population of patients readmitted after AMI have longer lengths of stay on index admission and higher Charlson Comorbidity Index when compared with the other AMI patient populations.11, 12 Both of these factors have previously been defined to be associated with increased readmission rates.13
Our results emphasize that patients with AMI with different index hospitalization clinical management have different reasons for readmission. For example, patients with AMI treated with CABG are most likely to be readmitted with infections, while other patients are more likely to be readmitted with cardiac complaints. Furthermore, patients who themselves decline revascularization during index AMI hospitalization have the highest proportion of readmissions related to cardiac complaints. As such, different strategies to reduce readmission may be efficacious for these different types of patients. In particular, patients who decline recommended revascularization should be counseled that they could have cardiac symptoms after hospital discharge, including angina and heart failure.
While previous work has identified that medically managed patients are likely to be readmitted,14 no work to date has provided a physician‐adjudicated chart review describing the clinical profile of these patients within the population of patients specifically relevant to the penalty. This work is important because it extends knowledge about both how to improve the risk‐adjustment of the penalty, potentially with novel administrative codes, as well as how to improve performance on the measure. In particular, patients with Type II MI have different demographics, clinical outcomes,15 and causes of readmission than patients with other types of MI.16 Since the optimal treatment for patients with Type II MI may vary based on coexistent acute illnesses, strategies meant to improve quality and reduce readmissions for patients with Type II MI may differ compared with Type I NSTEMI or STEMI patient populations.
Overall, our findings suggest that providers should focus on 2 distinct types of quality to improve HRRP metric performance. First are tactics that are likely to appropriately triage and evaluate patients with chest discomfort after PCI. We previously have shown that improved access to cardiology care in the emergency department can reduce unnecessary readmissions for low‐risk chest discomfort after PCI.6 Other strategies include reducing risk of infection and gastrointestinal bleeding. Second, for more complex patients who do not receive revascularization, case management and outpatient access interventions may be more effective along with patient‐centered ascertainment of preferences regarding goals of care. Such medically managed patients should know to expect angina in the outpatient setting and should be connected to palliative care colleagues if appropriate. Lastly, evaluating low‐risk chest discomfort patients in either an observational or outpatient setting may ultimately be more cost effective than admission. The implications of these types of quality improvement strategies, including monitoring for adverse events, should be tested prospectively. Ultimately, these findings emphasize that the HRRP algorithm includes patients who are not having traditional STEMI or Type I NSTEMI. Therefore, new administrative codes for physician ascertainment of excessive procedural risk, patient‐initiated “do not resuscitate” status, or Type II NSTEMI may improve risk standardization in the methodology used for the HRRP.
Our analysis should be interpreted in the setting of important limitations. First, since this was an analysis based on chart reviews, we only had access to medical information on readmissions for those patients readmitted within the index hospital network. Second, as an analysis of Medicare patients, the extent to which we can generalize our findings to patients of different age and insurance status is unclear. However, our analysis matches the HRRP penalty population, since the patient list was derived based on the penalty list. Finally, as a single‐center study, patterns of care at our hospital may differ from patterns of care at other hospitals.
In conclusion, we have demonstrated that over half of patients with AMI included in the HRRP are medically managed patients treated without revascularization, including those declined for PCI or CABG, those with limited goals of care, as well as a percentage with Type II MI. These findings suggest that administrative billing codes to reflect these factors may improve the discrimination of the risk‐adjustment methodology. Furthermore, these findings emphasize the heterogeneous tactics needed for quality improvement in the HRRP penalty population.
Sources of Funding
This work was funded in part by the National Institutes of Health and Harvard Catalyst (KL2 TR001100) as well as the American Heart Association (18CDA34110215), both awarded to Dr Wasfy.
Disclosures
Dr Januzzi is a consultant at Roche Diagnostics (Amount: >$10 000) and is involved in research at Siemens Diagnostics (Amount: >$10 000), Abbott Diagnostics (Amount: >$10 000), Prevencio (Amount: >$10 000), Singulex (Amount: >$10 000), and Novartis (Amount: >$10 000). Dr Singh is a consultant at St. Jude Medical (Amount: <$10 000), Boston Scientific (Amount: <$10 000), Biotronik (Amount: <$10 000), Medtronic (Amount: <$10 000), Liva Nova (Amount: <$10 000), Impulse Dynamics (Amount: <$10 000), Medscape (Amount: <$10 000), Respicardia Inc (Amount: <$10 000), American College of Cardiology (Amount: >$10 000), and is a Deputy Editor at Clinical Electrophysiology. Dr Wasfy reports grant support from the National Institutes of Health and Harvard Catalyst (Amount: >$10 000), the American Heart Association (Amount: >$10 000), as well as salary support as a medical director of the Massachusetts General Physicians Organization (Amount: >$10 000). The remaining authors have no disclosures to report.
(J Am Heart Assoc. 2018;7:e009339 DOI: 10.1161/JAHA.118.009339.)
References
- 1. McIlvennan CK, Eapen ZJ, Allen LA. Hospital readmissions reduction program. Circulation. 2012;131:1796–1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Andrews RM, Elixhauser A. STATISTICAL BRIEF # 42 The National Hospital Bill: Growth Trends and 2005 Update on the Most Expensive Conditions by Payer. Rockville, MD: Agency for Healthcare Research and Quality; 2007:1–13. [PubMed] [Google Scholar]
- 3. Strait K. Medicare Hospital Quality Chartbook. 2012. 47. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Downloads/MedicareHospitalQualityChartbook2012.pdf. Accessed December 10, 2017.
- 4. Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016;374:1543–1551. [DOI] [PubMed] [Google Scholar]
- 5. Desai NR, Ross JS, Kwon JY, Herrin J, Dharmarajan K, Bernheim SM, Krumholz HM, Horwitz LI. Association between hospital penalty status under the Hospital Readmission Reduction Program and readmission rates for target and nontarget conditions. JAMA. 2016;316:2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wasfy JH, Strom JB, O'Brien C, Zai AH, Luttrell J, Kennedy KF, Spertus JA, Zelevinsky K, Normand SLT, Mauri L, Yeh RW. Causes of short‐term readmission after percutaneous coronary intervention. Circ Cardiovasc Interv. 2014;7:97–103. [DOI] [PubMed] [Google Scholar]
- 7. Jaffe AS. Third universal definition of myocardial infarction. Clin Biochem. 2013;46:1–4. [DOI] [PubMed] [Google Scholar]
- 8. Kwok CS, Wong CW, Shufflebotham H, Brindley L, Fatima T, Shufflebotham A, Barker D, Pawala A, Heatlie G, Mamas MA. Early readmissions after acute myocardial infarction. Am J Cardiol. 2017;120:723–728. [DOI] [PubMed] [Google Scholar]
- 9. Cruz Rodriguez JB, Acharya P, Olson E, Cler L. Risk factors for 30‐day readmissions after acute myocardial infarction. Int Cardiovasc Forum J. 2015;4:30. [Google Scholar]
- 10. Sangu PV, Ranasinghe I, Aliprandi Costa B, Devlin G, Elliot J, Lefkovitz J, Brieger D. Trends and predictors of rehospitalisation following an acute coronary syndrome: report from the Australian and New Zealand population of the Global Registry of Acute Coronary Events (GRACE). Heart. 2012;98:1728–1731. [DOI] [PubMed] [Google Scholar]
- 11. Núñez JE, Núñez E, Fácila L, Bertomeu V, Llàcer A, Bodí V, Sanchis J, Sanjuán R, Blasco ML, Consuegra L, Martínez A. Chorro FJ Prognostic value of Charlson comorbidity index at 30 days and 1 year after acute myocardial infarction [in Spanish]. Rev Española Cardiol. 2004;57:842–849. [PubMed] [Google Scholar]
- 12. Rana S, Tran T, Luo W, Phung D, Kennedy RL, Venkatesh S. Predicting unplanned readmission after myocardial infarction from routinely collected administrative hospital data. Aust Heal Rev. 2014;38:377–382. [DOI] [PubMed] [Google Scholar]
- 13. Philbin EF, DiSalvo TG. Prediction of hospital readmission for heart failure: development of a simple risk score based on administrative data. J Am Coll Cardiol. 1999;33:1560–1566. [DOI] [PubMed] [Google Scholar]
- 14. Arnold SV, Smolderen KG, Kennedy KF, Li Y, Shore S, Stolker JM, Wang TY, Jones PG, Zhao Z, Spertus JA. Risk factors for rehospitalization for acute coronary syndromes and unplanned revascularization following acute myocardial infarction. J Am Heart Assoc. 2015;4:e001352 DOI: 10.1161/JAHA.114.001352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gaggin HK, Liu Y, Lyass A, van Kimmenade RRJ, Motiwala SR, Kelly NP, Mallick A, Gandhi PU, Ibrahim NE, Simon ML, Bhardwaj A, Belcher AM, Harisiades JE, Massaro JM, D'Agostino RB, Januzzi JL Jr. Incident type 2 myocardial infarction in a cohort arterial angiography. Circulation. 2017;135:116–127. [DOI] [PubMed] [Google Scholar]
- 16. Januzzi JL, Sandoval Y. The many faces of type 2 myocardial infarction. J Am Coll Cardiol. 2017;70:1569–1572. [DOI] [PubMed] [Google Scholar]


