Abstract
Background
There is growing evidence that sleep duration and quality may be associated with cardiovascular harm and mortality.
Methods and Results
We conducted a systematic review, meta‐analysis, and spline analysis of prospective cohort studies that evaluate the association between sleep duration and quality and cardiovascular outcomes. We searched MEDLINE and EMBASE for these studies and extracted data from identified studies. We utilized linear and nonlinear dose‐response meta‐analysis models and used DerSimonian–Laird random‐effects meta‐analysis models of risk ratios, with inverse variance weighting, and the I2 statistic to quantify heterogeneity. Seventy‐four studies including 3 340 684 participants with 242 240 deaths among 2 564 029 participants who reported death events were reviewed. Findings were broadly similar across both linear and nonlinear dose‐response models in 30 studies with >1 000 000 participants, and we report results from the linear model. Self‐reported duration of sleep >8 hours was associated with a moderate increased risk of all‐cause mortality, with risk ratio, 1.14 (1.05–1.25) for 9 hours, risk ratio, 1.30 (1.19–1.42) for 10 hours, and risk ratio, 1.47 (1.33–1.64) for 11 hours. No significant difference was identified for periods of self‐reported sleep <7 hours, whereas similar patterns were observed for stroke and cardiovascular disease mortality. Subjective poor sleep quality was associated with coronary heart disease (risk ratio, 1.44; 95% confidence interval, 1.09–1.90), but no difference in mortality and other outcomes.
Conclusions
Divergence from the recommended 7 to 8 hours of sleep is associated with a higher risk of mortality and cardiovascular events. Longer duration of sleep may be more associated with adverse outcomes compared with shorter sleep durations.
Keywords: cardiac risk factors, coronary artery disease, meta‐analysis, prevention
Subject Categories: Lifestyle
Clinical Perspective
What Is New?
In this meta‐analysis of 74 studies representing over 3 million participants, we found a J‐shaped relationship between sleep duration and mortality and incident cardiovascular disease.
Duration of sleep >8 hours of sleep was associated with increased risk of mortality.
No significant effect was identified for periods of sleep <7 hours. Similar patterns were observed for stroke and cardiovascular disease mortality.
Subjective poor sleep quality was associated with a significant increase in coronary heart disease, but not other outcomes.
What Are the Clinical Implications?
Our study suggests that abnormal sleep is a marker of elevated cardiovascular risk.
Future work should evaluate whether attention to optimizing the duration and quality of sleep may help reduce the burden of cardiovascular disease.
Introduction
Cardiovascular disease (CVD) causes over 787 000 deaths in the United States.1 Whereas sleep duration is generally not considered a traditional risk factor for cardiovascular disease (CVD), growing evidence supports its association with cardiovascular risk (CVR) factors2, 3, 4, 5, 6, 7 and disease,8, 9, 10, 11 and quality of sleep appears to contribute to CVR.10, 12 Yet, current guidelines for the risk reduction of CVD make limited recommendations about quality or duration of sleep.13, 14
The National Sleep Foundation recommends 7 to 9 hours of sleep for people aged 26 to 64 years and 7 to 8 hours of sleep for people aged ≥65 years,14 and the Centers for Disease Control and Prevention has similar recommendations for adults.15 Whether adults sleep the recommended hours is influenced by cultural, social, psychological, behavioral, pathophysiological, and environmental influences.16, 17 Sleep duration may be reduced because of irregular working and shift‐work patterns and round‐the‐clock availability of commodities of modern society.18 However, guidelines make no specific reference with regard to sleeping beyond the recommended limit. Long sleep duration may be associated with obstructive sleep apnea, heart disease, and failing health19 or may represent a symptom of early “latent” disease preceding a formal diagnosis.20
Although previous reviews have evaluated sleep duration and mortality and cardiovascular outcomes,10, 16 these reviews have not quantified the CVR associated with each hour deviation below or above the recommended sleep duration. In addition, none of the previous reviews assessed the influence of sleep quality.10, 16 Thus, we conducted a systematic review and meta‐analysis of the impact of sleep duration and quality on CVD and mortality.
Methods
Data, analytical methods, and study materials will not be made available to other researchers for purposes of reproducing the results or replicating the procedure.
The full methods, including detailed eligibility criteria, search strategy, data selection, extraction, and analysis, are reported in Data S1. The article was prepared according the guidance of the Meta‐analysis of Observational Studies in Epidemiology (MOOSE) statement (Data S2).
Eligibility Criteria
We selected prospective cohort studies that reported on participants who quantified their duration of sleep or quality of sleep, and their association with subsequent CVD and mortality. The primary outcome was all‐cause mortality, and secondary outcomes were CVD and mortality.
Search Strategy
We searched Medline and Embase using Ovid SP (from inception to the end of October 2015) using the search terms in Data S3.
Study Selection and Data Extraction
Two reviewers (C.S.K. and A.M.) checked all titles and abstracts for studies that could potentially meet the inclusion criteria. Data extraction and risk of bias assessment were performed independently by at least 2 reviewers (C.S.K., G.K., or M.G.). Publication bias was assessed using funnel plots.
Statistical Analysis
We used Stata software (version 14; StataCorpLP, College Station, TX) to perform regression analysis with random‐effects dose‐response meta‐analysis models to estimate the association between hours of sleep and adverse outcomes, using 7 hours of sleep as the reference category. The linear model represents the primary analysis, and the cubic model was included as a supplemental analysis.
Conventional random‐effects meta‐analysis was performed as a secondary analysis using RevMan 5.3 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). We decided to use random‐effects models because they are more conservative compared with fixed‐effect models, in the presence of any heterogeneity. Statistical heterogeneity was assessed using the I2 statistic. The details of the main and sensitivity analyses are described in Data S1. We also performed analysis of sleep quality (Data S4) in relation to mortality and cardiovascular outcomes.
Results
Description of Included Studies
A total of 74 studies met the inclusion criteria; the process of study selection is shown in Figure 1.8, 9, 11, 12, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90 Study design and participant characteristics are shown in Table 1. The included studies were dated 1970–2017, which represented 3 340 684 participants. Among studies that reported crude events, there were 242 240 all‐cause deaths in 2 564 029 participants from 44 studies (9.4%), 5435 coronary heart disease (CHD) deaths in 741 695 participants from 7 studies (0.7%), 6380 stroke deaths in 374 728 participants from 5 studies (1.7%), 32 988 cardiovascular deaths in 759 939 participants from 14 studies (4.3%), 32 084 CHD events in 540 538 participants from 14 studies (5.9%), 14 946 stroke events in 525 620 participants from 11 studies (2.8%), and 4160 CVD events in 97 832 participants from 6 studies (4.3%). Data S5 shows the prevalence of CVD and CVR factor profiles for each cohort.
Figure 1.
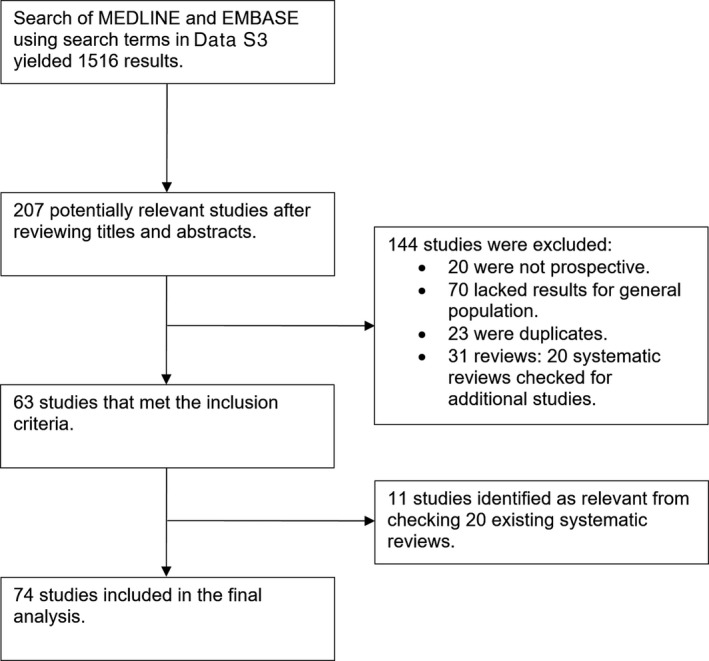
Flow diagram of study inclusion.
Table 1.
Study Design and Demographics Table
| Study ID | Design; Country; Year | No. of Participants | Mean Age, y | % Male | Participant Inclusion Criteria |
|---|---|---|---|---|---|
| Akersted, 201721 | Prospective cohort study; Sweden; 1997–2010 | 43 868 | 51 | 36 | Participants were aged >18 y in the Swedish National March study. |
| Amagai, 201022 | Prospective cohort study; Japan; April 1992 to July 1995 | 11 367 | 55 | 39 | Participants were adults of varying ages in 12 rural areas of Japan from the Jichi Medical School Cohort Study. |
| Aurora, 201623 | Prospective cohort study; USA; 1995–2011 | 5784 | 64 | 46 | Participants were aged 40 y and not treated for sleep‐disordered breathing in the Sleep Heart Health Study. |
| Ayas, 200324 | Prospective cohort study; USA; 1986–1996 | 71 617 | Unclear | 0 | Participants were US female health professionals aged 45 to 65 y who were enrolled in the Nurses’ Health Study. |
| Bellavia, 201425 | Prospective cohort study; Sweden; 1998–2012 | 70 973 | Unclear | 53 | Participants were Swedish males and aged 45 to 79 y and females aged 39 to 76 y from the population‐based Cohort of Swedish Men and the Swedish Mammography Cohort. |
| Burazeri, 200326 | Prospective cohort study; Israel; 1985 with up to 11 years’ follow‐up | 1842 | Unclear | 46 | Participants were aged >50 y in West Jerusalem in the Kiryat Yovel Community Health Study. |
| Cai, 201527 | Prospective cohort study; China; 1996–2010 | 113 138 | 54 | 41 | Participants were Chinese men and women in Shanghai, China in the Shanghai Women's Health Study and the Shanghai Men's Health Study. |
| Canivet, 201428 | Prospective cohort study; Sweden; 1991–2005 | 13 617 | Unclear | 43 | Participants were all people between the ages of 45 and 65 residing in Malmo, Sweden from the Malmo Diet and Cancer Study 1991. |
| Castro‐Costa, 201129 | Prospective cohort study; Brazil; 1997–2005 | 1512 | Median 69 | 38 | Participants were all residents of Bambui city, Brazil aged ≥60 years on January 1, 1997 and part of the Bambui Cohort Study. |
| Chandola, 201030 | Prospective cohort study; England; 1985–1988 | 10 308 | Unclear | 67 | Participants were adults aged 35 to 55 y from 20 London‐based civil service departments in the Whitehall II Cohort. |
| Chen, 200831 | Prospective cohort study; USA; 1994–1998 | 93 175 | Unclear | 0 | Participants were postmenopausal women aged 50 to 79 y from all over the United States in the Women's Health Initiative Observational study cohort. |
| Chen, 201332 | Prospective cohort study; Taiwan; 1999–2002 | 4064 | 73.8 | 56 | Participants were residents of the Shih‐Pai area of Taipei, Taiwan who were aged >65 y and part of the Shih‐Pai Sleep Study. |
| Chien, 201033 | Prospective cohort study; Taiwan; 1990–1991 | 3430 | 54.8 | 50 | Participants were adults aged >35 years in the Chin‐Shan Community Cardiovascular Cohort study and of Chinese ethnicity living in Chin‐Shan township, Taiwan. |
| Cohen‐Mansfeld, 201234 | Prospective cohort study; Israel; 1989–1992 | 1166 | 83 | 55 | Participants were older Jewish adults aged >75 y in the Cross‐Sectional and Longitudinal Aging Study. |
| Ensrud, 201235 | Prospective cohort study; USA; 2003–2005 | 2505 | 76 | 100 | Participants were nonfrail males aged ≥65 y, recruited by the prospective Osteoporotic Fractures in Men study. |
| Gangwisch, 200836 | Prospective cohort study; USA; 1982–1992 | 9789 | Unclear | 37 | Participants were men and women aged 25 to 74 y in the NHANES I epidemiological follow‐up study. |
| Garde, 201337 | Prospective cohort study; Denmark; 1970–2001 | 5249 | 49 | 100 | Participants were in the Copenhagen Male Study who were all men aged 40 to 59 y at 14 companies were invited. |
| Gianfagna, 201638 | Prospective cohort study; Italy; 1986–2008 | 2277 | 51 | 100 | Participants were men aged 35 to 74 y and CVD free in the MONICA‐Brianza and PAMELA population based cohorts. |
| Goto, 201339 | Prospective cohort study; Japan; 1987–1999 | 724 | Unclear | 65 | Participants were aged ≥65 y in Okinawa Japan. |
| Hale, 201340 | Prospective cohort study; USA; 1993–2009 | 3942 | 62 | 0 | Participants were in the Women's Health Initiative clinical trial and observational study who were postmenopausal women aged 50 to 79 y and did not have history of CHD. |
| Hall, 201541 | Prospective cohort study: USA; 1997 start follow‐up of 9 years | 3013 | 73.6 | 48.6 | Participants were adults in the Health, Aging and Body Composition Study. |
| Hamazaki, 201142 | Prospective cohort study; Japan; 1994–2008 | 2282 | 44 | 100 | Participants were men aged 35 to 54 y at a light metal factory (Japan) who did not have previous cardiovascular events or missing information at baseline survey. |
| Helbig, 201543 | Prospective cohort study; Germany; 1984–2001 | 17 604 | 48 | 50 | Participants were age 25 to 74 y in the Monitoring Trends and Determinants in Cardiovascular Disease/Cooperative Health Research in the Region of Augsburg study. |
| Heslop, 200244 | Prospective cohort study; Scotland; 1970–1995 | 3030 | Unclear | 85 | Participants were working Scottish men and women recruited between 1970 and 1973. |
| Hoevenaar‐Blom, 201112 | Prospective cohort study; Netherlands; 1993–2012 | 20 432 | 42 | 45 | Participants were aged 20 to 65 y in the MORGEN study. |
| Huang, 201345 | Prospective cohort study; Taiwan; 1999–2010 | 1901 | Unclear | 51 | Participants were aged ≥65 y in the Elderly Nutrition and Health Survey in Taiwan. |
| Hublin, 200746 | Prospective cohort study; Finland; 1975–2003 | 21 268 | 41 | 48 | Participants were in Finnish Twin Cohort who were all Finnish twin pairs of the same sex born before 1958 with both co‐twins alive in 1975. |
| Ikehara, 200947 | Prospective cohort study; Japan; 1988–2003 | 98 634 | Unclear | 42 | Participants were in the Japan Collaborative Cohort Study for Evaluation of Cancer Risk where were aged 40 to 79 y and living in Japan. |
| Jung, 201348 | Prospective cohort study; USA; 1984–2001 | 2001 | 74 | 44 | Participants were in the community‐dwelling adults aged 60 to 96 y in The Rancho Bernardo Study. |
| Kakizaki, 201349 | Prospective cohort study; Japan; 1994–2008 | 49 256 | 60 | 48 | Participants were aged 40 to 79 y in the Ohsaki Cohort Study. |
| Kawachi, 201650 | Prospective cohort study; Japan; 1992–2008 | 27 896 | 54 | 54 | Participants were men and women aged ≥35 y in the Takayama Cohort Study. |
| Kim, 201351 | Prospective cohort study; USA; 1993–2007 | 135 685 | Unclear | 46 | Participants were aged 45 to 75 y in the Multiethnic Cohort Study from Hawaii and Los Angeles. |
| Kojima, 200052 | Prospective cohort study; Japan; 1982–1996 | 5322 | 47 | 46 | Participants were aged 20 to 76 y from Shirakawa town, Japan. |
| Kripke, 200253 | Prospective cohort study; USA; 1982–1988 | 1 116 936 | 57 | 43 | Participants were aged 30 to 102 y in the Cancer Prevention Study II mainly friends/relatives of American Cancer Society volunteers. |
| Lan, 200754 | Prospective cohort study; Taiwan; 1993–2003 | 3079 | 71 | 55 | Participants were ≥64 y in the Survey of Health and Living Status of the Elderly in Taiwan. |
| Lee, 201455 | Prospective cohort study; Hong Kong; 2001–2010 | 3427 | 74 | 51 | Participants were men and women in Hong Kong aged ≥65 y. |
| Lee, 201756 | Prospective cohort study; Taiwan; 2006–2010 | 937 | 65 | 55 | Participants were Taiwanese aged ≥53 y in the Social Environment and Biomarkers of Aging Study. |
| Leng, 20159 | Prospective cohort study; United Kingdom; 1998–2009 | 9692 | 62 | 46 | Participants were adults aged 42 to 81 y in the European Prospective Investigation into Cancer‐Norfolk cohort. |
| Li, 201357 | Prospective cohort study; Japan; 1983–1990 | 12 489 | Unclear | 38 | Participants were residents aged 20 to 79 y in the Minami Saku area of Japan who were a part of the SAKUCESS project. |
| Liu, 201458 | Prospective cohort study; USA; 1971–2007 | 3381 | 45 | 48 | Participants were aged >30 y and were free from CHD in the Framingham Offspring Study. |
| Magee, 201159 | Prospective cohort study; Australia; 2006–2009 | 218 155 | 63 | 47 | Participants were Australian adults aged ≥45 y, residing in the state of New South Wales and part of the 45 and Up study. |
| Magee, 201360 | Prospective cohort study; Australia; 2006–2009 | 227 815 | Unclear | 46.3 | Participants were Australian adults aged ≥45 y, residing in the state of New South Wales and part of the 45 and Up study. |
| Mallon, 200261 | Prospective cohort study; Sweden; 1983–1995 | 1870 | 56 | 48 | Participants were a random adults aged 45 to 65 y in the population register of the County of Dalarna in Sweden. |
| Martin, 201162 | Prospective cohort study; USA; Unclear | 245 | 81 | 62 | Participants were adults aged ≥65 y admitted to postacute rehabilitation sites in the Los Angeles area in the USA. |
| Meisinger, 200763 | Prospective cohort study; Germany; 1984–1995 | 6896 | 58 | 50.9 | Participants were German adults aged 45 to 74 y who were part of the MONICA Augsburg project. |
| Mesas, 201064 | Prospective cohort study; Spain; 2001–2008 | 3820 | 71.8 | 44 | Participants were noninstitutionalized adults aged ≥60 y living in Spain. |
| Pan, 201465 | Prospective cohort study; Singapore; 1993–1998 | 63 257 | 57 | 44 | Participants were Chinese adults in Singapore aged 45 to 74, recruited from Hokkiens and Cantonese dialect groups residing in government housing estates. |
| Patel, 200466 | Prospective cohort study; USA; 1986–2000 | 82 969 | 53 | 0 | Participants were women aged 30 to 55 y and residing in 11 US states that were part of the Nurses’ Health Study. |
| Pollak, 199067 | Prospective cohort study; USA; 1984–1985 | 1855 | 75 | Unclear | Participants were elderly residents of an urban community aged 65 to 98 y. |
| Qiu, 201168 | Prospective cohort study; China; 2005–2008 | 12 671 | 86 | 57 | Participants were elderly Chinese adults from 22 provinces in China in the Chinese Longitudinal Healthy Longevity Survey. |
| Qureshi, 199769 | Prospective cohort study; USA; 1982–1992 | 7844 | Unclear | 36 | Participants were US civilian noninstitutionalized adults aged >31 y and in the NHANES I Epidemiologic Follow‐up Study (NHEFS). |
| Rhee, 201270 | Prospective cohort study; Korea; 1992–2008 | 14 533 | 51 | 100 | Participants were male subjects aged 40 to 59 y in the Seoul Male Cohort Study. |
| Rod, 201471 | Prospective cohort study; UK; 1985–2010 | 9098 | 45 | 67 | Participants were in the Whitehall II Cohort Study who were London‐based office staff aged 35 to 55 y working in 20 civil service departments in 1985. |
| Ruigomez, 199572 | Prospective cohort study; Spain; 1986–1991 | 1219 | Unclear | 39 | Participants were an elderly population in the 1986 Health Interview Survey of Barcelona. |
| Ruiter Petrov, 201473 | Prospective cohort study; USA; 2003–2010 | 5666 | 61 | 44 | Participants were aged ≥45 y in the Reasons for Geographic And Racial Differences in Stroke study. |
| Sands‐Lincoln, 201374 | Prospective cohort study; USA; 1993–2009 | 86 329 | 63 | 0 | Participants were in the Women's Health Initiative clinical trial and observational study who were postmenopausal women aged 50 to 79 y and did not have a history of CHD. |
| Shankar, 200875 | Prospective cohort study; Singapore; 1993–2006. | 58 044 | 56 | 44 | Participants were Chinese adults aged 45 to 75 y in the Singapore Chinese Health Study. |
| Song, 201676 | Prospective cohort study; China; 2006–2010 | 95 203 | 51 | 79 | Participants were aged 18 to 98 y in the Kailuan study. |
| Stone, 200977 | Prospective cohort study; USA; Unclear | 6107 | 80 | 50 | Participants were community‐dwelling older adults participating in the Study of Osteoporotic Fractures and the Outcomes of Sleep Disorders in Older Men Study. |
| Strand, 201678 | Prospective cohort study; Taiwan; 1998–2011 | 392 164 | 40 | 49 | Participants were Taiwanese adults aged 20 y who were participants in a health check‐up program run by MJ Health Management Institution. |
| Suzuki, 200911 | Prospective cohort study; Japan; 1999–2006 | 12 601 | 74 | 51 | Participants were elderly residents aged 65 to 85 y in the Shizuoka Study. |
| Tamakoshi, 200479 | Prospective cohort study; Japan; 1988–1999 | 104 010 | 58 | 42 | Participants were aged 40 to 79 y in the Japan Collaborative Cohort Study on Evaluation of Cancer Risk study. |
| Tsubono, 199380 | Prospective cohort study; Japan; 1988–1992 | 4318 | Unclear | 40 | Participants were aged ≥40 y in Japan who participated in the annual health examination program implemented by the Town Council. |
| Tu, 201281 | Prospective cohort study; China; 1997–2006 | 68 832 | 60 | 0 | Participants were women aged 40 to 70 y in the Shanghai Women's Health Study. |
| Twig, 201682 | Prospective cohort study; Israel; unclear | 23 690 | 30 | 100 | Participants were men aged >25 y in the Israeli Defense Forces who were in the MELANY cohort study. |
| Von Ruesten, 201283 | Prospective cohort study; Germany; 1994–2007 | 23 620 | 49 | 39 | Participants were in the European Prospective Investigation into Cancer and Nutrition (EPIC) study in Potsdam. |
| Wang, 201684 | Prospective cohort study; China; 2006–2010 | 95 903 | 51 | 80 | Participants were aged 18 to 98 y in the Kailuan study. |
| Werle, 201185 | Prospective cohort study; Brazil; 1994–2009 | 187 | 84 | 36 | Participants were aged >80 y in the city of Veranopolis, Brazil. |
| Westerlund, 20138 | Prospective cohort study; Sweden; 1997–2010 | 41 192 | Unclear | 35 | Participants were aged ≥18 y in the Swedish National March Cohort Study. |
| Wingard, 198386 | Prospective cohort study; USA; 1965–1974 | 6928 | Unclear | 47 | Participants were aged 30 to 69 y of age in 1965 in California. |
| Xiao, 201487 | Prospective cohort study; USA; 1995–2011 | 239 896 | 63 | 56 | Participants were aged 51 to 72 y in the NIH AARP Diet and Health Study. |
| Yeo, 201388 | Prospective cohort study; Korea; 1993–2010 | 13 164 | 55 | 41 | Participants were aged ≥20 y in the Korean Multi‐center Cancer Cohort study. |
| Zawisza, 201589 | Prospective cohort study; Poland; 1986–2008 | 2449 | 72 | 35 | Participants were aged ≥65 y from Krakow city centre in Poland. |
| Zuubier, 201590 | Prospective cohort study; Netherlands; 2004–2013 | 1734 | 62 | 47 | Participants were aged ≥45 y in the Rotterdam Study. |
CHD indicates coronary heart disease; CVD, cardiovascular disease; MELANY, Metabolic Lifestyle and Nutrition Assessment in Young Adults; MONICA‐Brianza, Monitoring of Cardiovascular Disease‐Brianza; MORGEN, Monitoring Project on Risk Factors and Chronic Diseases in the Netherlands; NHANES, National Health and Nutrition Examination Survey; PAMELA, Pressioni Arteriose Monitorate E Loro Associazioni; SAKUCESS, Saku Cancer Etiology Surveillance Study.
Quality Assessment of Included Studies
The quality assessment is shown in Data S6. Studies used questionnaires or direct questioning to ascertain information about sleep quality or sleep duration. Methods used to estimate outcomes included population registries, death certification, questionnaires, and review of medical records or patient through interview or telephone call. Most studies adjusted for potential confounders, but the factors adjusted for varied across studies. Loss to follow‐up was unclear in 30 studies, and 12 studies had 10% or more loss to follow‐up or missing data. The study reference group and studies included for each analysis are shown in Data S7.
Sleep Duration and All‐Cause Mortality
Numeric results of analyses are shown in Tables 2 and 3. For the spline analysis, a total of 30 studies* reported data that could be used for the all‐cause mortality analysis. When spline analysis was applied using a linear model, incremental deviation <7 hours of self‐reported sleep was not associated with increased risk of all‐cause mortality, but sleep durations >8 hours were associated with increased risk of all‐cause mortality (Figure 2). The cubic spline analysis model is shown in Data S8.
Table 2.
Study Cohort, Follow‐up and Results for Studies With Authors Akersted to Akersted
| Study ID | Follow‐up Duration | Outcomes and Crude Rate of Outcomes | Results |
|---|---|---|---|
| Akersted, 201721 | 13 y | All‐cause mortality: 3548/39 191 | Sleep duration and mortality: ≤5 h: aHR 1.12 (0.99–1.27), 6 h: aHR 0.98 (0.88–1.09), 7 h: aHR 1.00, ≥8 h: aHR 1.10 (1.00–1.20). |
| Amagai, 201022 | 10.7 y | CVD events: 481/11 367. MI: 80/11 367. Stroke: 411/11 367 |
Sleep duration and CVD in males: <5.9 h: aHR 2.14 (1.11–4.13), 6.0 to 6.9 h: aHR 1.04 (0.61–1.76), 7.0 to 7.9 h: aHR 1.00, 8.0 to 8.9 h: aHR 0.98 (0.69–1.40), ≥9.0 h: aHR 1.33 (0.93–1.92). Sleep duration and CVD in females: <5.9 h: aHR 1.46 (0.70–3.04), 6.0 to 6.9 h: aHR 0.64 (0.38–1.10), 7.0 to 7.9 h: aHR 1.00, 8.0 to 8.9 h: aHR 0.85 (0.60–1.20), ≥9.0 h: aHR 1.28 (0.88–1.87). Sleep duration and MI in men: <5.9 h: aHR 1.78 (0.50–6.28), 6.0 to 6.9 h: aHR 0.77 (0.25–2.33), 7.0 to 7.9 h: aHR 1.00, 8.0 to 8.9 h: aHR 0.69 (0.34–1.41), ≥9.0 h: aHR 0.99 (0.47–2.06). Sleep duration and MI in women: <5.9 h: aHR 4.93 (1.31–18.61), 6.0 to 6.9 h: aHR 0.59 (0.13–2.73), 7.0 to 7.9 h: aHR 1.00, 8.0 to 8.9 h: aHR 0.59 (0.21–1.66), ≥9.0 h: aHR 0.84 (0.27–2.62). Sleep duration and stroke in men: <5.9 h: aHR 2.00 (0.93–4.31), 6.0 to 6.9 h: aHR 1.13 (0.63–2.03), 7.0 to 7.9 h: aHR 1.00, 8.0 to 8.9 h: aHR 1.03 (0.69–1.53), ≥9.0 h: aHR 1.39 (0.92–2.10). Sleep duration and stroke in women: <5.9 h: aHR 0.97 (0.39–2.41), 6.0 to 6.9 h: aHR 0.68 (0.39–1.18), 7.0 to 7.9 h: aHR 1.00, 8.0 to 8.9 h: aHR 0.86 (0.60–1.23), ≥9.0 h: aHR 1.29 (0.86–1.91). |
| Aurora, 201623 | 10.8 y | All‐cause mortality: 1509/5784 | Sleep duration and mortality: <7 h: aHR 0.98 (0.87–1.10), 7 to 8 h: aHR 1.00, ≥9 h: aHR 1.25 (1.05–1.47). |
| Ayas, 200324 | 10 y | CHD: 934/71 617 | Sleep duration and CHD: ≤5 h: aOR 1.39 (1.05–1.84), 6 h: aOR 1.18 (0.98–1.43), 7 h: aOR 1.10 (0.92–1.31), 8 h: aOR 1.00, >9 h: aOR 1.37 (1.02–1.85). |
| Bellavia, 201425 | 15 y | All‐cause mortality 13 450/70 973. CVD mortality: 3981/70 973 |
Sleep duration and all‐cause mortality: <6 h: aHR 1.25 (1.13–1.37), 6 to 6.5 h: aHR 1.10 (1.04–1.17), 6.6 to 7.4 h: aHR 1.00 (reference), 7.5 to 8 h: aHR 1.03 (0.98–1.08), >8 h: aHR 1.14 (1.05–1.24). Sleep duration and CVD mortality: <6 h: aHR 1.44 (1.20 to 1.73), 6 to 6.5 h: aHR 1.23 (1.09–1.38), 6.6 to 7.4 h: aHR 1.00, 7.5 to 8 h: aHR 1.02 (0.92–1.12), >8 h: aHR 1.11 (0.95–1.31). |
| Burazeri, 200326 | 10 y | All‐cause mortality: 403/1842 |
Total sleep duration and all‐cause mortality in men: <6 h: aHR 1.00, 6 to 8 h: aHR 1.41 (0.83–2.39), >8 h: aHR 2.13 (1.23–3.71). Total sleep duration and all‐cause mortality in women: <6 h: aHR 1.00, 6 to 8 h: aHR 0.63 (0.42–0.97), >8 h: aHR 0.80 (0.51–1.24). Total sleep duration and CVD mortality in men: <6 h: aHR 1.00, 6 to 8 h: aHR 1.54 (0.75–3.15), >8 h: aHR 2.02 (1.01–4.03). Total sleep duration and CVD mortality in women: <6 h: aHR 1.00, 6 to 8 h: aHR 0.69 (0.37–1.29), >8 h: aHR 0.79 (0.42–1.48). |
| Cai, 201527 | Median 6 to 7 y | All‐cause mortality: 4277/113 138 |
Sleep duration and all‐cause mortality: 4 to 5 h: aHR 1.11 (1.00–1.23), 6 h: aHR 1.06 (0.97–1.16), 7 h: aHR 1.00, 8 h: aHR 1.15 (1.05–1.26), 9 h: aHR 1.34 (1.17–1.54), ≥10 h: 1.81 (1.59–2.06). Sleep duration and all‐cause mortality in men: 4 to 5 h: aHR 1.06 (0.90–1.25), 6 h: aHR 1.07 (0.94–1.23), 7 h: aHR 1.00, 8 h: aHR 1.13 (1.00–1.28), 9 h: aHR 1.34 (1.10–1.62), ≥10 h: aHR 1.55 (1.29–1.86). Sleep duration and all‐cause mortality in women: 4 to 5 h: aHR 1.15 (1.01–1.32), 6 h: aHR 1.06 (0.94–1.20), 7 h: aHR 1.00, 8 h: aHR 1.17 (1.04–1.32), 9 h: aHR 1.36 (1.13–1.64), ≥10 h: aHR 2.11 (1.77–2.52). Sleep duration and cardiovascular mortality: 4 to 5 h: aHR 1.05 (0.87–1.26), 6 h: aHR 1.10 (0.94–1.29), 7 h: aHR 1.00, 8 h: aHR 1.22 (1.05–1.43), 9 h: aHR 1.47 (1.17–1.85), ≥10 h: aHR 2.04 (1.65–2.53). Sleep duration and cardiovascular mortality in men: 4 to 5 h: aHR 1.09 (0.82–1.46), 6 h: aHR 1.06 (0.83–1.34), 7 h: aHR 1.00, 8 h: aHR 1.25 (1.00–1.56), 9 h: aHR 1.68 (1.23–2.30), ≥10 h: aHR 1.58 (1.14–2.18). Sleep duration and cardiovascular mortality in women: 4 to 5 h: aHR 1.02 (0.80–1.30), 6 h: aHR 1.12 (0.91–1.39), 7 h: aHR 1.00, 8 h: aHR 1.20 (0.96–1.50), 9 h: aHR 1.28 (0.91–1.82), ≥10 h: aHR 2.64 (1.99–3.52). Sleep duration and stroke mortality: 4 to 5 h: aHR 0.91 (0.70–1.18), 6 h: aHR 0.99 (0.79–1.23), 7 h: aHR 1.00, 8 h: aHR 1.28 (1.04–1.58), 9 h: aHR 1.31 (0.94–1.82), ≥10 h: aHR 2.35 (1.78–3.09). Sleep duration and stroke mortality in men: 4 to 5 h: aHR 0.93 (0.62–1.40), 6 h: aHR 0.78 (0.55–1.10), 7 h: aHR 1.00, 8 h: 1.20 (0.89–1.62), 9 h: aHR 1.62 (1.06–2.48), ≥10 h: aHR 1.73 (1.14–2.64). Sleep duration and stroke mortality in women: 4 to 5 h: aHR 0.92 (0.65–1.29), 6 h: aHR 1.14 (0.85–1.52), 7 h: aHR 1.00, 8 h: aHR 1.36 (1.01–1.82), 9 h: aHR 0.98 (0.58–1.66), ≥10 h: aHR 3.09 (2.14–4.47). |
| Canivet, 201428 | 14 y | Unclear |
Sleep duration and cardiovascular events in men: ≤6 h: aHR 1.1 (0.96–1.3), 7 to 8 h: aHR 1.0, ≥9 h:aHR 1.3 (1.01–1.7). Sleep duration and cardiovascular events in women: ≤6 h: aHR 1.3 (1.1–1.5), 7 to 8 h: aHR 1.0, ≥9 h: aHR 1.5 (1.1–2.1). |
| Castro‐Costa, 201129 | Unclear | All‐cause mortality: 440/1512 | Night‐time sleep duration and all‐cause mortality: <6 h: aHR 1.09 (0.78–1.53), 6 to 7 h: aHR 0.84 (0.60–1.17), 7 to 8 h: aHR 1.00 (reference), 8 to 9 h: aHR 1.31 (0.97–1.78), ≥9 h: aHR 1.53 (1.12–2.09). |
| Chandola, 201030 | 15 y | CHD mortality, MI, angina: 1205/8998 |
Sleep duration and CHD mortality, MI and angina: <5 h: aRR 1.05 (0.92–1.20), 6 h: aRR 0.98 (0.83–1.16), 7 h: aRR 1.00, >8: aRR 0.99 (0.77–1.27). Poor sleep quality (more than usual restless, disturbed nights) and CHD mortality, MI, and angina: aRR 1.36 (1.10–1.68). |
| Chen, 200831 | 7.5 y | Ischaemic stroke: 1166/93 175 | Sleep duration and ischemic stroke: <6 h: aHR 1.14 (0.97–1.33), 7 h: aHR 1.00, 8 h: aHR 1.24 (1.04–1.47), >9 h: aHR 1.70 (1.32–2.21). |
| Chen, 201332 | 9 y | All‐cause mortality: 1004/4064. CVD mortality: 259/4064 |
Sleep duration and all‐cause mortality: <4 h: aHR 1.00 (0.75–1.33), 5 h: aHR 0.92 (0.74–1.15), 6 h: aHR 0.88 (0.73–1.06), 7 h: aHR 1.00, 8 h: aHR 1.26 (1.04–1.53), >9 h: aHR 1.66 (1.28–2.17). Sleep duration and CVD mortality: <4 h: aHR 1.05 (0.61–1.79), 5 h: aHR 0.95 (0.62–1.48), 6 h:aHR 0.79 (0.54–1.16), 7 h: aHR 1.00, 8 h: aHR 1.36 (0.92–2.01), >9 h: aHR 2.36 (1.46–3.80). Poor sleep quality (subjective) and all‐cause mortality: aHR 0.81 (0.47–1.38). Poor sleep quality (subjective) and CVD mortality: aHR 0.60 (0.19–1.93). |
| Chien, 201033 | Median 15.9 y | All‐cause mortality: 901/3430. CVD events: 420/3430 |
Sleep duration and all‐cause mortality: <5 h: aRR 1.15 (0.9–1.46), 6 h: aRR 0.97 (0.79–1.21), 7 h: aRR 1, 8 h: aRR 1.04 (0.86–1.27), ≥9 h: aRR 1.34 (1.08–1.67). Sleep duration and CVD event: <5 h: aRR 0.94 (0.65–1.35), 6 h: aRR 0.91 (0.67–1.24), 7 h: aRR 1, 8 h: aRR 1.05 (0.80–1.39), >9 h: aRR 1.12 (0.81–1.55). |
| Cohen‐Mansfeld, 201234 | 20 y | All‐cause mortality: 1108/1166 | Sleep duration and mortality: <7 h: aHR 0.98 (0.84–1.13), 7 to 9 h: 1.00, >9 h: aHR 1.32 (1.09–1.58). |
| Ensrud, 201235 | 3.4 y | All‐cause mortality: 180/2505 |
Poor sleep quality (PSQI score >5) and all‐cause mortality: >5 81/1018 vs ≤5 99/1487, aOR 1.02 (0.73–1.42). Sleep duration and all‐cause mortality: ≤5 h: 21/269 vs 159/2236, aOR 1.08 (0.65–1.80). |
| Gangwisch, 200836 | Up to 10 y | All‐cause mortality: 1877/9789 | Sleep duration and all‐cause mortality: ≤5 h: aHR 1.17 (0.99–1.39), 6 h: aHR 0.95 (0.81–1.11), 7 h: aHR 1.00, 8 h: aHR 1.23 (1.08–1.39), ≥9 h: aHR 1.34 (1.15–1.56). |
| Garde, 201337 | 30 y | All‐cause mortality: 2643/5249. Ischaemic heart disease mortality: 587/5249 |
Sleep duration on all‐cause mortality in men: <6 h: aHR 1.06 (0.90–1.25). 6 to 7 h: aHR 1.00. ≥8 h: aHR 0.99 (0.84 to 1.09). Sleep duration and ischemic heart disease mortality in men: <6 h: aHR 1.46 (1.07–2.00). 6 to 7 h: aHR 1.00. ≥8 h: aHR 1.20 (0.97–1.49). |
| Gianfagna, 201638 | Median 17 y | CVD event: 293/2277. CHD event: 214/2277 |
Sleep duration and CVD event: ≤6 h: aHR 1.14 (0.84–1.53), 7 to 8 h: aHR 1.00, ≥9 h: aHR 1.55 (1.08–2.21). Sleep duration and CHD event: ≤6 h: aHR 1.14 (0.80–1.61), 7 to 8 h: aHR 1.00, ≥9 h: aHR 1.32 (0.85–2.07). Sleep disturbance on CVD event vs none/some: moderate aHR 1.14 (0.74–1.77), severe aHR 1.80 (1.07–3.03). Sleep disturbance on CHD event vs none/some: moderate aHR 1.35 (0.83–2.21), severe aHR 1.83 (0.98–3.41). |
| Goto, 201339 | 12 y | All‐cause mortality: 305/724 |
Sleep duration and all‐cause mortality in men: aHR <6 h: aHR 1.29 (0.50–3.34), 6 to 7 h: aHR 1.00, >7 h: aHR 1.54 (092–2.58). Sleep duration and all‐cause mortality in women: aHR <6 h: aHR 2.62 (1.36–5.07), 6 to 7 h: aHR 1.00, >7 h: aHR 1.40 (0.91–2.15). |
| Hale, 201340 | Up to 16 y | All‐cause mortality: 335/3942. CHD: 132/3942 |
Sleep duration and all‐cause mortality: ≤5 h: aOR 1.01 (0.68–1.51), 6 h: aOR 0.94 (0.71–1.24), 7 to 8 h: aOR 1.00, ≥9 h: aOR 1.55 (0.92–2.60). Sleep duration and CHD: ≤5 h: aOR 1.09 (0.63–1.89), 6 h: aOR 0.66 (0.42–1.04), 7 to 8 h: aOR 1.00, ≥9 h: aOR 1.88 (0.92–3.83). |
| Hall, 201541 | 9 y | All‐cause mortality: 953/3075 | Sleep duration and all‐cause mortality: <6 h: aHR 1.06 (0.83–1.34), 6 h: aHR 1.00 (0.82–1.22), 7 h: aHR 1.00, 8 h: aHR 1.10 (0.91–1.33), >8 h: aHR 1.23 (0.93–1.63). |
| Hamazaki, 201142 | 14 y | CVD events: 64/2282. Stroke: 30/2282. Coronary events: 27/2282 |
Sleep duration and CVD events: <6 h: aHR 3.49 (1.30–9.40), 6 to 6.9 h: aHR 1.11 (0.55–2.25), 7 to 7.9 h: aHR 1.00, ≥8 h: aHR 1.71 (0.90–3.24). Sleep duration and stroke: <6 h: aHR 1.84 (0.23–14.90), 6 to 6.9 h: aHR 0.96 (0.30–3.10), 7 to 7.9 h: aHR 1.00, ≥8 h: aHR 2.25 (0.91–5.57). Sleep duration and coronary events: <6 h: aHR 4.95 (1.31–18.73), 6 to 6.9 h: aHR 1.12 (0.40–3.13), 7 to 7.9 h: aHR 1.00 (reference), ≥8 h: aHR 1.78 (0.67–4.76). |
| Helbig, 201543 | 14 y | Stroke: 917/17 604 |
Sleep duration and strokes in men: ≤5 h: aHR 1.36 (0.95–1.94), 6 h: aHR 0.92 (0.70–1.22), 7 to 8 h: aHR 1.00, 9 h: aHR 1.05 (0.78–1.43), ≥10 h: aHR 1.38 (0.98–1.94). Sleep duration and strokes in women: ≤5 h: aHR 0.68 (0.40–1.18), 6 h: aHR 1.25 (0.91–1.70), 7 to 8 h: aHR 1.00, 9 h: aHR 1.09 (0.76–1.57), ≥10 h: aHR 0.91 (0.55–1.51). Poor sleep quality (difficulty staying asleep) and stroke in men: aHR 1.06 (0.87–1.30). Poor sleep quality (difficulty staying asleep) and stroke in women: aHR 0.87 (0.68–1.10). |
| Heslop, 200244 | 25 y | All‐cause mortality: 1062/7028. CVD mortality: 557/7028 |
Sleep duration and all‐cause mortality in men: <7 h: aHR 1.15 (0.93–1.42), 7 to 8 h: aHR 1.00, >8 h: aHR 0.91 (0.57–1.46). Sleep duration and all‐cause mortality in women: <7 h: aHR 1.73 (0.99–3.03), 7 to 8 h: 1.00, >8 h: aHR 0.58 (0.08–4.22). Sleep duration and CVD mortality in men: <7 h: aHR 1.19 (0.90–1.58), 7 to 8 h: aHR 1, >8 h: aHR 0.63 (0.30–1.34). Sleep duration and CVD mortality in women: <7 h: aHR 2.30 (0.94–5.60), 7 to 8 h: aHR 1, >8 h: aHR 1.53 (0.20–11.8). |
| Hoevenaar‐Blom, 201112 | 11.9 y | CVD events: 1486/20 432. CHD: 1148/20 432 |
Sleep duration on incident CVD: ≤6 h: aHR 1.11 (0.97–1.27), 7 h: aHR 1.00, 8 h: aHR 0.95 (0.84–1.08), ≥9 h: aHR 0.96 (0.77–1.18). Sleep duration and incident CHD: ≤6 h: aHR 1.19 (1.00–1.40), 7 h: aHR 1.00, 8 h: aHR 0.85 (0.73–1.00), ≥9 h: aHR 0.78 (0.58–1.04). Poor sleep quality and incident CVD: aHR 1.04 (0.87–1.26). Poor sleep quality and incident CHD: aHR 1.19 (0.96–1.50). |
| Huang, 201345 | 10 y | All‐cause mortality: 182/1865 |
Poor sleep quality (good vs poor) and all‐cause mortality in men: aHR 0.60 (0.42–0.87). Poor sleep quality (good vs poor) and all‐cause mortality in women: aHR 0.99 (0.68–1.45). |
| Hublin, 200746 | 22 y | All‐cause mortality: 3700/21 268 |
Sleep duration and all‐cause mortality in men: <7 h: aHR 1.26 (1.11–1.43), 7 to 8 h: aHR 1.00, >8 h: aHR 1.24 (1.09–1.41). Sleep duration and all‐cause mortality in women: <7 h: aHR 1.21 (1.05–1.40), 7 to 8 h: aHR 1.00, >8 h: aHR 1.17 (1.03–1.34). Poor sleep quality and all‐cause mortality in men: aHR 1.10 (0.87–1.39). Poor sleep quality and all‐cause mortality in women: aHR 0.99 (0.77–1.27). |
| Ikehara, 200947 | Median 14.3 y | All‐cause mortality 14 540/98 634. CVD mortality 4287/98 634. Stroke mortality: 1964/98 634. CHD mortality 881/98 634 |
Sleep duration and all‐cause mortality in men: ≤4 h: aHR 1.29 (1.02–1.64), 5 h: aHR 1.02 (0.90–1.16), 6 h: aHR 1.08 (1.00–1.16), 7 h: aHR 1.00, 8 h: aHR 1.06 (1.00–1.12), 9 h: aHR 1.13 (1.05–1.22), ≥10 h: aHR 1.41 (1.29–1.54). Sleep duration and all‐cause mortality in women: ≤4 h: aHR 1.28 (1.03–1.60), 5 h: aHR 1.11 (0.98–1.25), 6 h: aHR 1.05 (0.97–1.14), 7 h: aHR 1.00, 8 h: aHR 1.16 (1.08–1.24), 9 h: aHR 1.32 (1.20–1.45), ≥10 h: aHR 1.56 (1.40–1.75). Sleep duration and CVD mortality in men: ≤4 h: aHR 1.11 (0.67–1.83), 5 h: aHR 0.99 (0.77–1.27), 6 h: aHR 1.01 (0.87–1.18), 7 h: aHR 1.00, 8 h: aHR 1.11 (1.00–1.24), 9 h: aHR 1.14 (0.99–1.32), ≥10 h: aHR 1.56 (1.33–1.83). Sleep duration and CVD mortality in women: ≤4 h: aHR 1.28 (0.88–1.86), 5 h: aHR 1.22 (1.00–1.50), 6 h: aHR 1.00 (0.86–1.16), 7 h: aHR 1.00, 8 h: aHR 1.28 (1.14–1.44), 9 h: aHR 1.37 (1.17–1.62), ≥10 h: aHR 1.54 (1.28–1.86). Sleep duration and stroke mortality in men: ≤4 h: aHR 1.56 (0.82–2.94), 5 h: aHR 0.85 (0.58–1.26), 6 h: aHR 0.95 (0.76–1.20), 7 h: aHR 1.00, 8 h: aHR 1.11 (0.95–1.30), 9 h: aHR 1.14 (0.92–1.42), ≥10 h: aHR 1.66 (1.31–2.08). Sleep duration and stroke mortality in women: ≤4 h: aHR 1.07 (0.59–1.91), 5 h: aHR 0.99 (0.72–1.37), 6 h: aHR 0.93 (0.75–1.16), 7 h: aHR 1.00, 8 h: aHR 1.24 (1.05–1.47), 9 h: aHR 1.29 (1.01–1.64), ≥10 h: aHR 1.69 (1.29–2.20). Sleep duration and CHD mortality in men: ≤4 h: aHR 0.29 (0.04–2.05), 5 h: aHR 1.02 (0.62–1.70), 6 h: aHR 0.86 (0.63–1.19), 7 h: aHR 1.00, 8 h: aHR 1.02 (0.82–1.27), 9 h: aHR 0.96 (0.70–1.31), ≥10 h: aHR 1.12 (0.77–1.63). Sleep duration and CHD mortality in women: ≤4 h: aHR 2.32 (1.19–4.50), 5 h: aHR 1.64 (1.07–2.53), 6 h: aHR 1.23 (0.88–1.72), 7 h: aHR 1.00, 8 h: aHR 1.24 (0.94–1.64), 9 h: aHR 1.52 (1.05–2.19), ≥10 h: aHR 1.04 (0.63–1.72). |
| Jung, 201348 | Up to 19 y | All‐cause mortality: 1224/2001 |
Night‐time sleep duration and all‐cause mortality in men: <6 h: aHR 0.98 (0.673–1.43), 6.0 to 6.9 h: aHR 1.12 (0.85–1.48) 7.0–7.9 h: aHR 1.0, 8.0–8.9 h: aHR 0.98 (0.79–1.22), ≥9 h: aHR 1.09 (0.82–1.45). Night‐time sleep duration and all‐cause mortality in women: <6 h: aHR 1.11 (0.77–1.60), 6.0–6.9 h: aHR 1.17 (0.85–1.61) 7.0–7.9 h: aHR 1.0, 8.0–8.9 h: aHR 1.19 (0.90–1.57), ≥9 h: aHR 1.51 (1.05–2.18). |
| Kakizaki, 201349 | 13 y | All‐cause mortality 8447/49 256. CVD mortality 2549/49 256. Stroke mortality 1165/49 256. IHD mortality 561/49 256 |
Sleep duration and all‐cause mortality: ≤6 h: aHR 1.01 (0.93–1.09), 7 h: aHR 1.00, 8 h: aHR 1.07 (1.01–1.14), 9 h: aHR 1.14 (1.06–1.24), ≥10 h: aHR 1.37 (1.27–1.47). Sleep duration on CVD mortality: ≤6 h: aHR 1.10 (0.96–1.28), 7 h: aHR 1.00, 8 h: aHR 1.21 (1.08–1.36), 9 h: aHR 1.32 (1.15–1.52), ≥10 h: aHR 1.49 (1.30–1.71). Sleep duration and stroke mortality: ≤6 h: aHR 1.05 (0.84–1.30), 7 h: aHR 1.00, 8 h: aHR 1.17 (0.99–1.39), 9 h: aHR 1.30 (1.06–1.60), ≥10 h: aHR 1.51 (1.24–1.85). Sleep duration and IHD mortality: ≤6 h: aHR 1.38 (1.02–1.86), 7 h: aHR 1.00, 8 h: aHR 1.36 (1.06–1.73), 9 h: aHR 1.49 (1.10–2.02), ≥10 h: aHR 1.41 (1.04–1.92). |
| Kawachi 201650 | Up to 16 y | Stroke mortality: 611/27 896 |
Sleep duration and stroke mortality: ≤6 h: aHR 0.77 (0.59–1.01), 7 h: aHR 1.00, 8 h: aHR 1.13 (0.91–1.40), ≥9 h: aHR 1.51 (1.16–1.97). Sleep duration and stroke mortality in men: ≤6 h: aHR 0.51 (0.34–0.77), 7 h: aHR 1.00, 8 h: aHR 0.88 (0.66–1.17), ≥9 h: aHR 1.23 (0.90–1.69). Sleep duration and stroke mortality in women: ≤6 h: aHR 1.06 (0.75–1.50), 7 h: aHR 1.00, 8 h: aHR 1.50 (1.10–2.04), ≥9 h: aHR 1.93 (1.38–2.70). |
| Kim, 201351 | 13 y | All‐cause mortality: 19 335/135 685. CVD mortality 6610/135 685. Stroke mortality: 1259/135 685. MI mortality: 1188/135 685 |
Sleep duration and all‐cause mortality in men: aHR ≤5 h: 1.15 (1.06–1.23), 6 h: aHR 1.04 (0.99–1.10), 7 h: aHR 1.00, 8 h: 1.07 (1.01–1.12), ≥9 h: 1.19 (1.12–1.27). Sleep duration and all‐cause mortality in women: aHR ≤5 h: 1.14 (1.06–1.23), 6 h: aHR 1.05 (0.99–1.12), 7 h: aHR 1.00, 8 h: 1.02 (0.96–1.08), ≥9 h: 1.22 (1.13–1.31). Sleep duration and CVD mortality in men: aHR ≤5 h: 1.13 (1.00–1.28), 6 h: aHR 1.01 (0.92–1.11), 7 h: aHR 1.00, 8 h: 1.05 (0.96–1.14), ≥9 h: 1.22 (1.09–1.35). Sleep duration and CVD mortality in women: aHR ≤5 h: 1.20 (1.05–1.36), 6 h: aHR 1.06 (0.96–1.18), 7 h: aHR 1.00, 8 h: 1.08 (0.98–1.20), ≥9 h: 1.29 (1.13–1.47). Sleep duration and stroke mortality in men: aHR ≤5 h: 1.02 (0.74–1.40), 6 h: aHR 1.10 (0.88–1.37), 7 h: aHR 1.00, 8 h: 1.13 (0.91–1.39), ≥9 h: 1.35 (1.03–1.75). Sleep duration and stroke mortality in women: aHR ≤5 h: 1.16 (0.88–1.52), 6 h: aHR 0.99 (0.79–1.23), 7 h: aHR 1.00, 8 h: 1.07 (0.87–1.33), ≥9 h: 1.39 (1.06–1.83). Sleep duration and MI mortality in men: aHR ≤5 h: 1.24 (0.94–1.64), 6 h: aHR 0.92 (0.74–1.15), 7 h: aHR 1.00, 8 h: 0.98 (0.80–1.20), ≥9 h: 1.16 (0.89–1.50). Sleep duration and MI mortality in women: aHR ≤5 h: 1.18 (0.87–1.59), 6 h: aHR 1.23 (0.96–1.56), 7 h: aHR 1.00, 8 h: 1.10 (0.86–1.40), ≥9 h: 1.29 (0.95–1.75). |
| Kojima, 200052 | 12 y | All‐cause mortality: 256/5322 |
Sleep duration and all‐cause mortality in men: <7 h: aRR 1.93 (1.12–3.35), 7.0 to 8.9 h: aRR 1.00, 9.0 to 9.9 h: aRR 1.15 (0.74–1.77), ≥10.0 h: aRR 1.77 (0.88–3.54). Sleep duration and all‐cause mortality in women: <7 h: aRR 0.90 (0.50–1.61), 7.0 to 8.9 h: aRR 1.00, 9.0 to 9.9 h: aRR 1.07 (0.58–1.95), ≥10.0 h: aRR 0.40 (0.06–2.92). Poor sleep quality (waking up feeling bad) on all‐cause mortality (Male): aRR 1.13 (0.60–2.12). Poor sleep quality (waking up feeling bad) on all‐cause mortality (Female): aRR 2.03 (1.10–3.74). |
| Kripke, 200253 | Up for 6 y | All‐cause mortality: 77 640/1 116 936 |
Sleep duration and all‐cause mortality in men: 3 h: aHR 1.19 (0.96–1.47), 4 h: aHR 1.17 (1.06–1.28), 5 h: aHR 1.11 (1.05–1.18), 6 h: aHR 1.08 (1.04–1.11), 7 h: aHR 1.00 (ref), 8 h: aHR 1.12 (1.09–1.15), 9 h: aHR 1.34 (1.28–1.40), ≥10 h: 1.08 (1.01–1.16). Sleep duration and all‐cause mortality in women: 3 h: aHR 1.33 (1.08–1.64), 4 h: aHR 1.11 (1.01–1.22), 5 h: aHR 1.07 (1.01–1.13), 6 h: 1.07 (1.03–1.11), 7 h: aHR 1.00 (ref), 8 h: aHR 1.13 (1.09–1.16), 9 h: 1.23 (1.17–1.28), ≥10 aHR 1.41 (1.34–1.50). |
| Lan, 200754 | 8 y | All‐cause mortality: 1338/3079. CVD mortality: 379/3079 |
Sleep duration and all‐cause mortality in men: <7 h: aHR 0.98 (0.76–1.25), 7 h: aHR 1.00, 8 h: aHR 1.09 (0.89–1.33), 9 h: aHR 1.14 (0.91–1.42), ≥10 h: aHR 1.51 (1.19–1.92). Sleep duration and all‐cause mortality in women: <7 h: aHR 1.14 (0.77–1.67), 7 h: aHR 1.00, 8 h: aHR 1.36 (1.01–1.84), 9 h: aHR 1.86 (1.36–2.53), ≥10 h: aHR 2.06 (1.50–2.83). Sleep duration and CVD mortality in men: <7 h: aHR 0.91 (0.53–1.57), 7 h: aHR 1.00, 8 h: aHR 1.40 (0.93–2.10) 9 h: aHR 1.26 (0.80–1.98), ≥10 h: aHR 1.81 (1.13–2.89). Sleep duration and CVD mortality in women: <7 h: aHR 1.07 (0.54–2.15), 7 h: aHR 1.00, 8 h: aHR 1.77 (1.05–2.98), 9 h: aHR 1.75 (1.00–3.07), ≥10 h: aHR 1.85 (1.04–3.27). |
| Lee, 201455 | 61.7 months | All‐cause mortality: 297/3427 |
Night time sleep duration ≥10 h and mortality in men: aHR 1.75 (1.09–2.81). Night time sleep duration ≥10 h and mortality in women: aHR 2.88 (1.01–8.18). |
| Lee, 201756 | 4.7 y. | All‐cause mortality: 72/937. | Sleep duration and all‐cause mortality: <6 h: aHR 1.21 (0.67–2.17), 6 to 7 h: aHR 1.00, ≥8 h: aHR 2.11 (1.19–3.76). |
| Leng, 20159 | 9.5 y | Stroke 346/9692 |
Sleep duration and stroke: <6 h: aHR 1.18 (0.91–1.53), 6 to 8 h: aHR 1.00, >8 h: aHR 1.46 (1.08–1.98). Sleep duration and stroke in men: <6 h: aHR 1.08 (0.75–1.57), 6 to 8 h: aHR 1.00, >8 h: aHR: 1.21 (0.80–1.82). Sleep duration and stroke in women: <6 h: aHR 1.25 (10.86–1.83), 6 to 8 h: aHR 1.00, >8 h: aHR: 1.80 (1.13–2.85). |
| Li, 201357 | 7 y | All‐cause mortality: 312/12 489 |
Sleep duration and all‐cause mortality in men: <5 h: aHR 1.44 (0.65–3.19), 6 h: aHR 0.86 (0.50–1.48), 7 h: aHR1.00, 8 h: aHR 1.05 (0.72–1.53), >9 h: aHR 1.70 (1.07–2.70). Sleep duration and all‐cause mortality in women: <5 h: aHR 1.01 (0.42–2.39), 6 h: aHR 1.31 (0.78–2.21), 7 h: aHR 1.00, 8 h: aHR 1.01 (0.63–1.60), >9 h: aHR 1.85 (1.09–3.13). Sleep duration and CVD mortality in men: <5 h: aHR 1.57 (0.35–7.15), 6 h: aHR 0.60 (0.17–2.15), 7 h: aHR 1.00, 8 h: aHR 1.04 (0.49–2.21), >9 h: aHR 2.73 (1.22–6.11). Sleep duration and CVD mortality in women: <5 h: aHR 0.80 (0.18–3.47), 6 h: aHR 0.91 (0.38–2.23), 7 h: aHR 1.00, 8 h: aHR 1.13 (0.57–2.23), >9 h: aHR 1.72 (0.76–3.89). |
| Liu, 201458 | Over 20 y | CHD: 491/3381 | Sleep duration and CHD: ≤6 h: aHR 1.29 (1.03–1.61), 7 to 8 h: aHR 1.00, ≥9 h: aHR 1.13 (0.81–1.58). |
aHR indicates adjusted hazard ratio; aOR, adjusted odds ratio; aRR, adjusted risk ratio; CHD, coronary heart disease; CVD, cardiovascular disease; IHD, ischemic heart disease; MI, myocardial infarction; PSQI, Pittsburgh Sleep Quality Index.
Table 3.
Study Cohort, Follow‐up and Results for Studies With Authors Magee to Zuubier
| Study ID | Follow‐up Duration | Outcomes and Crude Rate of Outcomes | Results |
|---|---|---|---|
| Magee, 201159 | Unclear | Stroke 6541/218 155. Heart disease 25 669/218 155 |
Sleep duration and stroke: <6 h: aOR 1.54 (1.36–1.75), 6 h: aOR 1.25 (1.14–1.38), 7 h: aOR 1.00, 8 h: aOR 1.08 (1.01–1.17), ≥9 h: 1.50 (1.38–1.62). Sleep duration and heart disease: <6 h: aOR 1.23 (1.15–1.33), 6 h: aOR 1.11 (1.06–1.17), 7 h: aOR 1.00, 8 h: aOR 1.01 (0.97–1.05), ≥9 h: aOR 1.14 (1.09–1.19). |
| Magee, 201360 | 2.8 y | All‐cause mortality 8782/227 815 | Sleep duration and all‐cause mortality: <6 h: aHR 1.13 (1.01–1.25), 6 h: aHR 0.99 (0.91–1.06), 7 h: aHR 1.00, 8 h: aHR 1.02 (0.96–1.08), 9 h: aHR 1.04 (0.96–1.12), >10 h: aHR 1.26 (1.16–1.36). |
| Mallon, 200261 | 12 y | All‐cause mortality 266/2663. Coronary artery disease mortality: 91/2663. |
Sleep duration and all‐cause mortality in men: <6 h: aRR 1.1 (0.6–7.0), 7 to 8 h: aRR 1.00, >8 h: aRR 2.0 (1.2–3.2). Sleep duration and all‐cause mortality in women: <6 h: aRR 1.0 (0.6–1.8), 7 to 8 h: aRR 1.00, >8 h: aRR 1.3 (0.6–2.6). Sleep duration and coronary artery disease mortality in men: <6 h: aRR 0.7 (0.3–1.7), 7 to 8 h: aRR 1.00, >8 h: aRR 2.2 (1.0–4.4). Sleep duration and coronary artery disease mortality in women: <6 h: aRR 1.2 (0.4–4.2), 7 to 8 h: aRR 1.00, >8 h: aRR 0.7 (0.1–5.2). Poor sleep quality (difficulty maintaining sleep) and all‐cause mortality in men: aRR 1.4 (1.1–1.9). Poor sleep quality (difficulty maintaining sleep) and coronary artery disease mortality in men: aRR 1.2 (0.7–1.9). Poor sleep quality (difficulty maintaining sleep) and all‐cause mortality in women: aRR 1.1 (0.7–1.7). Poor sleep quality (difficulty maintaining sleep) and coronary artery disease mortality in women: aRR 1.1 (0.5–2.9). |
| Martin, 201162 | 1 y | All‐cause mortality: 57/245 | Sleep quality (high PQSI 7‐day score) and all‐cause mortality: aHR 1.12 (1.04–1.21). |
| Meisinger, 200763 | Unclear | Acute coronary event: 295/6896 |
Sleep duration and acute coronary event in men: ≤5 h: aHR 1.13 (0.66–1.92), 6 h: aHR 1.05 (0.71–1.55), 7 h: aHR 1.22 (0.92–1.61), 8 h: aHR 1.00 (reference), ≥9 h: aHR 1.07 (0.75–1.53). Sleep duration and acute coronary event in women: ≤5 h: aHR 2.98 (1.48–6.03), 6 h: aHR 1.05 (0.49–2.27), 7 h: aHR 1.34 (0.75–2.40), 8 h: aHR 1.00 (reference), ≥9 h: aHR 1.40 (0.74–2.64). Poor sleep quality (difficulty maintaining sleep) and acute coronary events in men: aHR 1.12 (0.84–1.48). Poor sleep qualtiy (difficulty maintaining sleep) and acute coronary events in women: aHR 1.53 (0.99–2.37). |
| Mesas, 201064 | 6.8 y | All‐cause mortality: 897/3820 | Sleep duration and all‐cause mortality: <5 h: aOR 1.42 (1.04–1.96), 6 h: aOR 1.23 (0.90–1.69), 7 h: aOR 1.00, 8 h: aOR 1.34 (1.02–1.76), 9 h: aOR 1.48 (1.12–1.96), 10 h: aOR 1.73 (1.30–2.29), >11 h: aOR 1.66 (1.23–2.24). |
| Pan, 201465 | Up to 8 y | Stroke mortality: 1381/63 257 |
Sleep duration and stroke deaths: <5 h: aHR 1.25 (1.05–1.50), 6 h: aHR 1.01 (0.87–1.18), 7 h: aHR 1.00, 8 h: aHR 1.09 (0.95–1.26), >9 h: aHR 1.54 (1.28–1.85). Sleep duration and ischaemic or unspecified stroke deaths: <5 h: aHR 1.37 (1.12–1.68), 6 h: aHR 1.04 (0.87–1.24), 7 h: aHR 1.00, 8 h: aHR 1.14 (0.96–1.34), >9 h: aHR 1.68 (1.36–2.06). Sleep duration and hemorrhagic stroke death: <5 h: aHR 0.92 (0.62–1.36), 6 h: aHR 0.91 (0.67–1.24), 7 h: aHR 1.00, 8 h: aHR 0.97 (0.73–1.29), >9 h: aHR 1.14 (0.76–1.72). |
| Patel 200466 | 14 y | All‐cause mortality: 5409/82 969. CVD mortality: 1084/82 969 | Sleep duration and all‐cause mortality: <5 h: aRR 1.08 (0.96–1.22), 6 h: aRR 0.99 (0.92–1.06), 7 h: aRR 1.00, 8 h: aRR 1.11 (1.03–1.19), >9 h: aRR 1.40 (1.25–1.55). Sleep duration and cardiovascular mortality: <5 h: aRR 1.04 (0.79–1.35), 6 h: aRR 1.06 (0.91–1.25), 7 h: aRR 1.00, 8 h: aRR 1.12 (0.95–1.31), >9 h: aRR 1.56 (1.25–1.96). |
| Pollak, 199067 | 3.5 y | All‐cause mortality: 309/1855 |
Incremental increase in h of sleep and all‐cause mortality in men: HR 0.96 (0.66–1.39). Incremental increase in h of sleep and all‐cause mortality in women: HR 1.11 (0.80–1.54). |
| Qiu, 201168 | 3 y | All‐cause mortality: 5199/12 671 |
Sleep duration and all‐cause mortality: <5 h: aHR 0.97 (0.88–1.08), 6 h: aHR 1.05 (0.95–1.16), 7 h: aHR 1.00 (0.90–1.11), 9 h: aHR 0.95 (0.83–1.07), >10 h: aHR 1.09 (1.00–1.18). Sleep duration and all‐cause mortality and men: <5 h: aHR 1.17 (1.01–1.38), 6 h: aHR 1.06 (0.91–1.25), 7 h: aHR 1.17 (0.99–1.37), 9 h: aHR 1.08 (0.89–1.31), >10 h: aHR 1.22 (1.08–1.38). Sleep duration and all‐cause mortality and women: <5 h: aHR 0.85 (0.75–0.98), 6 h: aHR 1.02 (0.90–1.15), 7 h: aHR 0.88 (0.76–1.01), 9 h: aHR 0.86 (0.72–1.02), >10 h: aHR 1.00 (0.90–1.11). Sleep quality (poor vs good) and all‐cause mortality: aHR 0.91 (0.83–1.00). Sleep quality (poor vs good) and all‐cause mortality in men: aHR 1.11 (0.95–1.30). Sleep quality (poor vs good) and all‐cause mortality in women: aHR 0.81 (0.71–0.91). |
| Qureshi, 199769 | 10 y | Stroke 322/7844. CHD: 474/7844 |
Sleep duration and risk for stroke: <6 h: aOR 1.0 (0.7–1.5), 6 to 8 h: aOR 1.0, >8 h: aOR 1.5 (1.1–2.0). Sleep duration and CHD: <6 h: aOR 1.3 (1.0–1.8), 6 to 8 h: aOR 1.0, >8 h: aOR 1.1 (0.8–1.5). |
| Rhee, 201270 | Up to 15 y | All‐cause mortality: 990/14 533 | Sleep duration and all‐cause mortality: ≤5 h: aHR 1.53 (1.11–2.12), 6 to 7 h: aHR 1.04 (0.88–1.22), ≥8 h: aHR 1.00. |
| Rod, 201471 | 22 y. | All‐cause mortality: 804/9098. CVD mortality: 221/9098 |
Sleep duration and all‐cause mortality in men: ≤5 h: aHR 1.11 (0.73–1.68), 6 h: aHR 1.23 (1.01–1.50), 7 h: aHR 1.00, 8 h: aHR 1.18 (0.92–1.50), >9 h: aHR 1.44 (0.59–3.50). Sleep duration and all‐cause mortality in women: ≤5 h: aHR 1.21 (0.76–1.91), 6 h: aHR 1.14 (0.86–1.52), 7 h: aHR 1.00, 8 h: aHR 0.91 (0.63–1.30), >9 h: aHR 1.48 (0.60–3.65). Sleep duration and CVD mortality: ≤6 h: aHR 1.18 (0.87–1.63), 7 to 8 h: aHR 1.00, >9 h: aHR 1.61 (0.40–6.59). Poor sleep quality (disturbed sleep) and all‐cause mortality in men: aHR 0.85 (0.62–1.16). Poor sleep quality (disturbed sleep) and all‐cause mortality in women: aHR 1.03 (0.70–1.52). Poor sleep quality (disturbed sleep) and CVD mortality: aHR 1.04 (0.72–1.49). |
| Ruigomez, 199572 | 55.7 months | All‐cause mortality 224/1219 |
Sleep duration and all‐cause mortality: <7 h: aRR 0.83 (0.56–1.23), 7 to 9 h: aRR 1.00, >9 h: aRR 1.37 (0.89–2.11). Sleep duration and all‐cause mortality in men: <7 h: aRR 1.06 (0.61–1.83), 7 to 9 h: aRR 1.00, >9 h: 1.30 (0.71–2.38). Sleep duration and all‐cause mortality in women: <7 h: aRR 0.66 (0.37–1.16), 7 to 9 h: aRR 1.00, >9 h: 1.46 (0.79–2.70). |
| Ruiter Petrov, 201473 | 2 y | Stroke (at least 1 symptom): 224/5666 | Sleep duration on stroke symptoms: <6 h: aHR 1.47 (0.89–2.45), 6 h: aHR 1.22 (0.82–1.81), 7 h: aHR 1.00, 8 h: aHR 1.30 (0.92–1.83), ≥9 h: aHR 1.42 (0.82–2.45). |
| Sands‐Lincoln, 201374 | 10.3 y | CVD events: 7257/86 329 |
Sleep duration and CVD: ≤5 h: aHR 1.06 (0.96–1.16), 6 h: aHR 1.00 (0.95–1.06), 7 to 8 h: aHR 1.00, 9 h: aHR 0.95 (0.83–1.08), ≥10 h: aHR 1.23 (0.89–1.70). Sleep duration and CHD: ≤5 h: aHR 1.08 (0.96–1.20), 6 h: aHR 1.00 (0.94–1.07), 7 to 8 h: aHR 1.00, 9 h: aHR 0.93 (0.80–1.08), ≥10 h: aHR 1.33 (0.94–1.88). |
| Shankar, 200875 | 13 y | CHD mortality: 1416/58 044 | Sleep duration and CHD mortality: ≤5 h: aRR 1.57 (1.32–1.88), 6 h: aRR 1.13 (0.98–1.31), 7 h: aRR 1.00, 8 h: aRR 1.12 (0.97–1.29), ≥9 h: aRR 1.79 (1.48–2.17). |
| Song, 201676 | 7.9 y | Stroke: 3135/95 023 |
Sleep duration and stroke: <6 h: aHR 0.92 (0.81–1.05), 6 to 8 h: aHR 1.00, >8 h: aHR 1.29 (1.01–1.64). Sleep duration and stroke in men: <6 h: aHR 0.90 (0.78–1.03), 6 to 8 h: aHR 1.00, >8 h: aHR 1.24 (0.96–1.60). Sleep duration and stroke in women: <6 h: aHR 1.09 (0.75–1.60), 6 to 8 h: aHR 1.00, >8 h: aHR 1.91 (0.98–3.74). |
| Stone, 200977 | Up to 4.1 y | All‐cause mortality: 793/6107 |
Sleep duration and all‐cause mortality in men: <5 h: RH 1.2 (0.8–1.8), 7 to 8 h: RH 1.00. Sleep duration and all‐cause mortality in women: <5 h: RH 1.8 (1.3–2.5), 7 to 8 h: RH 1.00. |
| Strand, 201678 | 9.7 y | CHD mortality: 711/392 164 |
Sleep duration and CHD mortality: <4 h: aHR 1.36 (0.88–2.10), 4 to 6 h: aHR 1.03 (0.85–1.24), 6 to 8 h: aHR 1.00, <8 h: aHR 1.28 (1.05–1.56). Sleep duration and CHD mortality in men: <4 h: aHR 1.03 (0.53–2.00), 4 to 6 h: aHR 1.06 (0.85–1.32), 6 to 8 h: aHR 1.00, <8 h: aHR 1.11 (0.88–1.41). Sleep duration and CHD mortality in women: <4 h: aHR 1.84 (1.03–3.29), 4 to 6 h: aHR 0.99 (0.72–1.37), 6 to 8 h: aHR 1.00, <8 h: aHR 1.81 (1.28–2.56). Difficulty getting to sleep and CHD mortality: aHR 1.01 (0.80–1.26). |
| Suzuki, 200911 | 6 y | All‐cause mortality: 1004/14 001. CVD mortality: 310/14 001 |
Sleep duration and all‐cause mortality: ≤5 h: aHR 0.92 (0.66–1.28), 6 h: aHR 1.06 (0.80–1.39), 7 h: aHR 1.00, 8 h: aHR1.36 (1.09–1.70), 9 h: aHR 1.41 (1.05–1.90), ≥10 h: aHR 1.96 (1.49–2.57). Sleep duration and all‐cause mortality in men: ≤5 h: aHR 1.08 (0.72–1.61), 6 h: aHR 1.05 (0.75–1.47), 7 h: aHR 1.00, 8 h: aHR 1.36 (1.04–1.78), 9 h: aHR 1.52 (1.08–2.15), ≥10 h: aHR 1.86 (1.34–2.56). Sleep duration and all‐cause mortality in women: ≤5 h: aHR 0.71 (0.39–1.29), 6 h: aHR 1.08 (0.67–1.74), 7 h: aHR 1.00, 8 h: aHR 1.39 (0.92–2.09), 9 h: aHR 1.15 (0.64–2.09), ≥10 h: aHR 2.27 (1.37–3.76). Sleep duration and CVD mortality: ≤5 h: aHR 1.10 (0.62–1.93), 6 h: aHR 0.85 (0.50–1.45), 7 h: aHR 1.00, 8 h: aHR 1.52 (1.01–2.29). 9 h: aHR 1.55 (0.91–2.63), ≥10 h: aHR 1.95 (1.18–3.21). Sleep duration and CVD mortality in men: ≤5 h: aHR 0.97 (0.46–2.05), 6 h: aHR 0.75 (0.38–1.48), 7 h: aHR 1.00, 8 h: aHR 1.05 (0.63–1.75). 9 h: aHR 1.26 (0.65–2.45), ≥10 h: aHR 1.71 (0.94–3.11). Sleep duration and CVD mortality in women: ≤5 h: aHR 1.48 (0.59–3.67), 6 h: aHR 1.08 (0.44–2.66), 7 h: aHR 1.00, 8 h: aHR 2.83 (1.39–5.76). 9 h: aHR 2.32 (0.93–5.77), ≥10 h: aHR 2.31 (0.91–5.82). Poor sleep quality (frequent awakening) and all‐cause mortality: aHR 0.99 (0.83–1.18). Poor sleep quality (frequent awakening) and all‐cause mortality in men: aHR 1.00 (0.81–1.24). Poor sleep quality (frequent awakening) and all‐cause mortality in women: aHR 0.96 (0.69–1.31). Poor sleep quality (frequent awakening) and CVD mortality: aHR 0.91 (0.66–1.26). Poor sleep quality (frequent awakening) and CVD mortality in men: aHR 0.97 (0.64–1.48). Poor sleep quality (frequent awakening) and CVD mortality in women: aHR 0.81 (0.49–1.35). |
| Tamakoshi, 200479 | 9.9 y | All‐cause mortality: 11 071/104 010 |
Sleep duration and all‐cause mortality in men: ≤4 h: aRR 0.88 (0.44–1.78), 5 h: aRR 1.07 (0.83–1.38), 6 h: aRR 1.11 (0.95–1.28), 7 h: aRR 1.00, 8 h: aRR 1.19 (1.07–1.32), 9 h: aRR 1.27 (1.08–1.48), ≥10 h: aRR 1.75 (1.46–2.09). Sleep duration and all‐cause mortality in women: ≤4 h: aRR 1.83 (1.20–2.81), 5 h: aRR 1.18 (0.90–1.53), 6 h: aRR 1.17 (0.99–1.39), 7 h: aRR 1.00, 8 h: aRR 1.35 (1.17–1.56), 9 h: aRR 1.57 (1.26–1.96), ≥10 h: aRR 2.12 (1.67–2.68). |
| Tsubono 199380 | 4 y | All‐cause mortality: 207/4318 | Sleep duration and all‐cause mortality: ≤6 h: aRR 1.26 (0.81–1.97), 7 to 8 h: aRR 1.00, ≥9 h: aRR 1.58 (1.16–2.15). |
| Tu, 201281 | 4 y | Unclear |
Sleep duration and CHD in women: ≤4 h: aOR 1.46 (1.26–1.70), 5 h: aOR 1.28 (1.15–1.43), 6 h: aOR 1.11 (1.02–1.21), 7 h: aOR 1.00, 8 h: aOR 0.95 (0.86–1.03), 9 h: aOR 1.07 (0.92–1.25), ≥10 h: aOR 1.41 (1.19–1.67). Sleep duration and stroke in women: ≤4 h: aOR 1.75 (1.49–2.07), 5 h: aOR 1.37 (1.21–1.55), 6 h: aOR 1.16 (1.05–1.29), 7 h: aOR 1.00, 8 h: aOR 1.05 (0.94–1.17), 9 h: aOR 1.07 (0.89–1.29), ≥10 h: aOR 1.88 (1.56–2.27). |
| Twig, 201682 | 6.4 y | Coronary artery disease 92/26 023 | Poor sleep quality (highest vs lowest quartile) and coronary artery disease: aHR 2.38 (1.37–4.11). |
| Von Ruesten, 201283 | 8 y | Stroke 169/23 620. MI 197/23 620 |
Sleep duration and MI: <6 h: aHR 1.44 (0.85–2.43) 6 h: aHR 0.80 (0.53–1.20), 7 h: aHR 1.00, 8 h: aHR 0.82 (0.56–1.19), ≥9 h: aHR 0.89 (0.54–1.49). Sleep duration and strokes: <6 h: aHR 2.06 (1.18–3.59), 6 h: aHR 1.13 (0.72–1.77), 7 h: aHR 1.00, 8 h: aHR 1.16 (0.77–1.73), ≥9 h: aHR 1.65 (1.00–2.73). |
| Wang, 201684 | 3.98 y | MI: 423/101 510. All‐cause mortality: 1793/101 510 |
Sleep duration and MI: ≤5 h: aHR 0.89 (0.60–1.30), 6 h: aHR 0.84 (0.61–1.16), 7 h: aHR 1.00, 8 h: aHR 0.86 (0.66–1.13), ≥9 h: aHR 1.12 (0.58–2.16). Sleep duration and all‐cause mortality: ≤5 h: aHR 1.23 (1.03–1.80), 6 h: aHR 1.95 (0.81–1.12), 7 h: aHR 1.00, 8 h: aHR 1.06 (0.92–1.20), ≥9 h: aHR 1.65 (1.22–2.22). |
| Werle, 201185 | 9 y | All‐cause mortality: 141/187. CV mortality: 56/187 |
Incremental increase in h of sleep and all‐cause mortality: aHR 0.95 (0.89–1.02). Incremental increase in h of sleep and cardiovascular mortality: aHR 0.83 (0.73–0.95). |
| Westerlund 20138 | 13 y | CVD mortality: 857/41 192. Stroke: 1685/41 192. MI: 1908/41 192 |
Sleep duration and CVD mortality: ≤5 h: aHR 1.11 (0.76–1.64), 6 h: aHR 1.17 (0.88–1.55), 7 h: aHR 1.00, ≥8 h: aHR 1.12 (0.85–1.47). Sleep duration and CVD: ≤5 h: aHR 1.05 (0.88–1.26), 6 h: aHR 0.97 (0.86–1.09), 7 h: aHR 1.00, ≥8 h: aHR 1.00 (0.89–1.13). Sleep duration and stroke: ≤5 h: aHR 1.05 (0.80–1.37), 6 h: aHR 0.95 (0.79–1.14), 7 h: aHR 1.00, ≥8 h: aHR 0.87 (0.72–1.04). Sleep duration and MI: ≤5 h: aHR 1.19 (0.92–1.55), 6 h: aHR 1.05 (0.88–1.25), 7 h: aHR 1.00, ≥8 h: aHR 1.19 (1.00–1.41). Poor sleep quality (difficulty maintaining sleep) and CVD mortality: mostly/always aHR 0.97 (0.77–1.20). |
| Wingard, 198386 | 9 y | All‐cause mortality: 369/6928 |
Sleep duration and all‐cause mortality in men: ≤6 h: 52/352, 7 to 8 h: 142/1735, ≥9 h: 15/132. Sleep duration and all‐cause mortality in women: ≤6 h: 35/386, 7 to 8 h: 107/1902, ≥9 h: 17/200. |
| Xiao, 201487 | 14 y | All‐cause mortality: 44 100/239 896. CVD mortality: 11 635/239 896 |
Sleep duration and all‐cause mortality: <5 h: aRR 1.16 (1.11–1.26), 5 to 6 h: aRR 1.04 (1.02–1.06), 7 to 8 h: aRR 1.00, ≥9 h: aRR 1.11 (1.06–1.19). Sleep duration and CVD mortality: <5 h: aRR 1.25 (1.13–1.38), 5 to 6 h: aRR 1.06 (1.02–1.10), 7 to 8 h: aRR 1.00, ≥9 h: aRR 1.07 (0.97–1.17). |
| Yeo, 201388 | 9 y | All‐cause mortality: 1580/13 164. CVD mortality: 363/13 164 |
Sleep duration and all‐cause mortality: ≤5 h: aHR 1.21 (1.03–1.41), 6 h: aHR 1.10 (0.95–1.27), 7 h: aHR 1.00, 8 h: aHR 1.03 (0.89–1.19), 9 h: aHR 1.36 (1.11–1.67), ≥10 h: aHR 1.36 (1.07–1.72). Sleep duration on CVD mortality: ≤5 h: aHR 1.40 (1.02–1.93), 6 h: aHR 1.25 (0.92–1.69), 7 h: aHR 1.00, 8 h: aHR 1.04 (0.76–1.42), 9 h: aHR 1.26 (0.81–1.96), ≥10 h: aHR 1.37 (0.82–2.29). |
| Zawisza, 201589 | 10.8 y | All‐cause mortality 2093/2449. | Incremental increase in h of sleep and all‐cause mortality: aHR 1.04 (1.003–1.075). |
| Zuubier, 201590 | 7.3 y | All‐cause mortality: 154/1734. | Sleep duration and all‐cause mortality: <6 h: aHR 1.12 (0.77–1.65), 6 to 7.5 h: aHR 1.00, ≥7.5 h: 1.18 (0.70–1.98). |
aHR indicates adjusted hazard ratio; aOR, adjusted odds ratio; aRR, adjusted risk ratio; CHD, coronary heart disease; CVD, cardiovascular disease; HR, hazard ratio; MI, myocardial infarction; PSQI, Pittsburgh Sleep Quality Index; RH, relative hazard.
Figure 2.
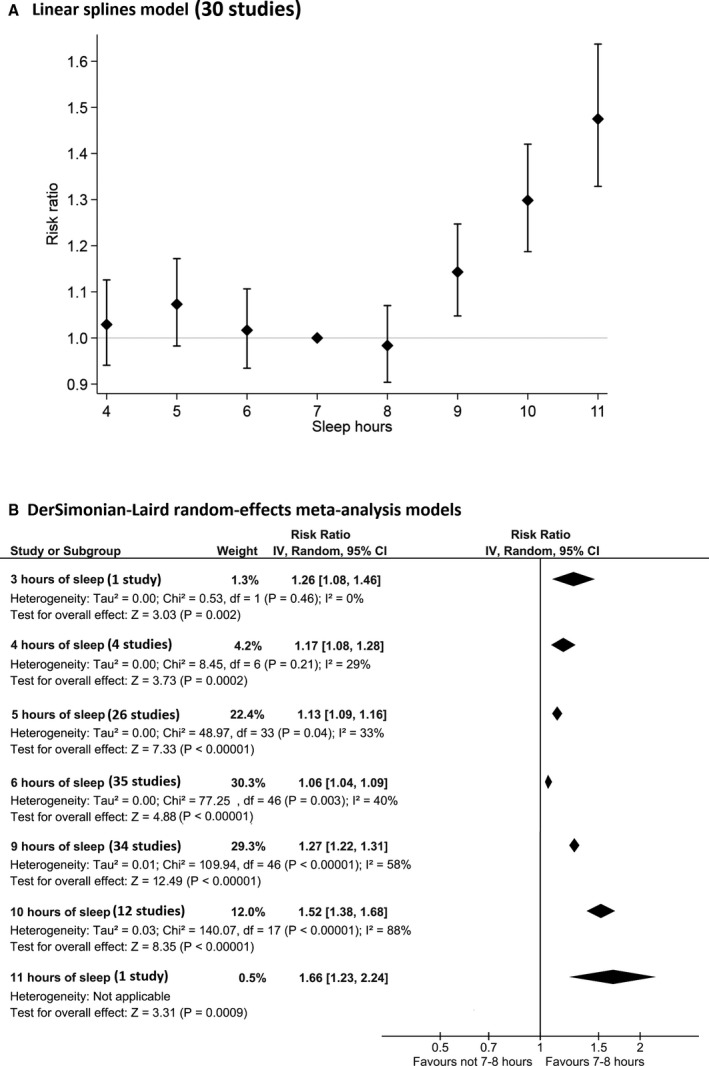
Sleep duration and risk of all‐cause mortality with linear and cubic splines. A, Linear splines model (30 studies). B, DerSimonian–Laird random‐effects meta‐analysis models. CI indicates confidence interval.
Pooled risk of all‐cause mortality for the entire cohort (Figure 2, Data S9) and the subgroup of men and women only are shown in Data S10. There were a total of 39 studies included in the analysis.** The funnel plot for sleep duration and mortality did not suggest that there was publication bias. Deviation from self‐reported sleep duration of 7 or 8 hours appeared to be associated with all‐cause mortality, where longer sleep durations are associated with greater mortality compared with small increases for shorter durations. The similar J‐shaped relationship was observed for the subgroup of men and women.
Sleep Duration and CHD Mortality and CHD
A total of 537, 47, 49, 75, 78 and 12*** studies were included in spline analysis for CHD mortality and CHD, respectively. Linear spline analysis failed to demonstrate any significant difference for both outcomes for self‐reported shorter and longer sleep durations (Figure 3, cubic model in Data S8).
Figure 3.
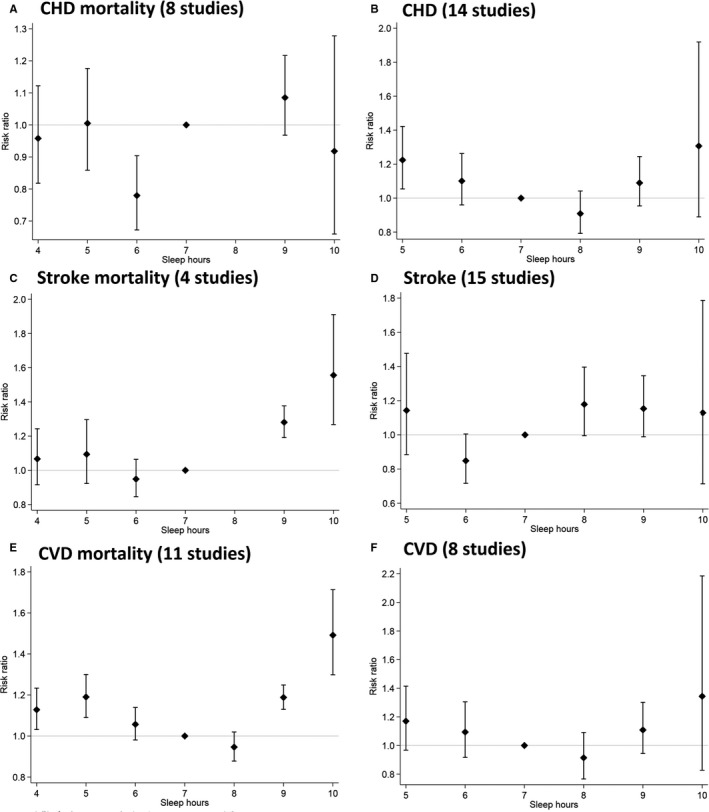
Linear models for adverse cardiovascular events. A, CHD mortality (8 studies). B, CHD (14 studies). C, Stroke mortality (4 studies). D, Stroke (15 studies). E, CVD mortality (11 studies). F, CVD (8 studies). CHD indicates coronary heart disease; CVD, cardiovascular disease.
For the meta‐analysis, there were 7 studies37, 47, 49, 51, 61, 75, 78 (Data S11) and 15 studies**** (Data S12) for CHD mortality and CHD, respectively. Although there were fewer studies, a similar J‐shaped pattern was observed where there was greater risk of CHD mortality and events with incremental deviation from the reference 7 to 8 hours of self‐reported sleep (a modest increase for 6 hours and greater increase for ≤5 hours; Data S10). The funnel plot for self‐reported sleep duration and CHD mortality suggested a possible publication bias whereas for CHD the plot did not suggest that there was a publication bias.
Sleep Duration and Stroke Mortality and Stroke
Linear spline analysis for stroke mortality and stroke included 347, 49, 65 and 98, 22, 31, 42, 43, 50, 69, 76, 83 studies, respectively. There was no difference in stroke events associated with self‐reported sleep duration shorter or longer than 7 hours, but a moderate increase in stroke mortality if sleep duration was >7 hours (Figure 3, Data S8).
Meta‐analysis of 5 studies27, 47, 49, 51, 65 were included in the analysis of stroke mortality (Data S10). For stroke events, there were 13 studies.† The funnel plot for sleep duration and stroke mortality did not suggest a publication bias. For stroke mortality, there appeared to be no difference in events with self‐reported sleep duration <7 hours, but significant and moderate increase in events with longer sleep duration >8 hours (Data S13). However, for stroke events, the increase in event rates are preserved for both sleep duration <7 hours (modest for 6 hours and a greater increase for ≤5 hours) and a moderate increase for >8 hours (Data S14). The funnel plot for sleep duration and stroke did not suggest a publication bias.
Sleep Duration and Cardiovascular Mortality and CVD
Spline analysis using linear models did not shown any difference in events with shorter duration than 7 hours for both cardiovascular mortality (8 studies)11, 25, 44, 47, 49, 71, 87, 88 and CVD (7 studies).8, 12, 22, 33, 38, 42, 74 However, longer self‐reported sleep duration >7 hours appeared to be associated with a moderate increase in greater stroke mortality (cubic model shown in Data S8).
There were 16 studies‡ (Data S15) that evaluated CVD mortality and 8 studies8, 12, 22, 28, 33, 38, 42, 74 (Data S16) that evaluated CVD events. The J‐shaped pattern was observed for self‐reported sleep duration and CVD mortality, but this was not the case for CVD events, but there were fewer studies in the event analysis. The funnel plot for sleep duration and CVD mortality and CVD did not suggest a publication bias. Incremental decrease in hours of sleep was associated with significant increase in mortality (Data S10).
Sleep Quality and Mortality and Adverse Cardiovascular Outcomes
A total of 17 studies§ were included in the analysis of subjective sleep quality and adverse outcomes (Data S10 and Data S17). For all‐cause mortality, there were 12 652 deaths among 73 702 participants from 10 studies, and the pooled results suggest that poor subjective quality of sleep was not associated with significant increase in mortality (risk ratio, 1.03; 95% confidence interval, 0.93–1.14). Poor sleep quality was associated with a significant and moderate increase in coronary heart disease (risk ratio, 1.44 95% confidence interval, 1.09–1.90) but not for any other outcomes. The funnel plot for sleep quality did not suggest publication bias.
Sensitivity Analysis Excluding Studies That Did Not Exclude Baseline CVD, Adjust for Cardiac Risk Factors, and Adjusted for Snoring or Obstructive Sleep Apnea
Sensitivity analysis was performed on the meta‐analysis data (Data S18). After exclusion of studies that included participants with baseline CVD, there was a significant increase in all‐cause mortality with longer and shorter self‐reported hours of sleep (small for 6 hours, modest for 5 and 9 hours, and moderate for 4 and 10 hours) and moderate increase in CVD mortality and stroke mortality with longer hours of sleep. Similar observations were found for studies that adjusted for CVR factors. For the analysis of CHD and stroke, there were significant and moderate increases in events when baseline CVD was excluded with 5‐hour duration of sleep. For the adjustments for obstructive sleep apnea analysis, some of the results were no longer statistically significant because there were fewer studies.
Discussion
In this meta‐analysis of 60 studies representing over 3 million participants, we observed that divergence from the recommended 7 to 8 hours of sleep was significantly associated with a moderate increase in mortality and incident CVD. We observed a J‐shaped relationship between sleep duration and mortality, and incident adverse cardiovascular events were observed. When spline analysis was applied to evaluate the incremental association of sleep duration and adverse events, our results suggest that longer than the recommended duration of 7 to 8 hours of sleep may be associated with a moderate degree of harm, compared with those who slept for durations shorter than that recommended.
Our study provides evidence that may contribute to important clinical and public health messages. First, we observed through spline analysis a more‐precise estimation of the risk gradient of CVD and mortality on the greater side of the recommended 7 to 8 hours of sleep compared to existing studies. Second, deviations in sleep duration and quality may be a nonspecific marker for increased CVR that might warrant determination of CVR. In particular, clinicians may need to be aware that the risk gradient appears to be steeper for long sleep duration compared with short duration, so individuals with excessive sleeping patterns may warrant further clinical assessment. Third, we provide updated evidence that supports the J‐shaped relationship where longer sleep is associated with significantly higher mortality and CVD and further the knowledge by highlighting that excess sleep is possibly associated with a greater likelihood of harm than less sleep with spline analysis. In addition, we found that sleep quality emerged as an important risk factor for CHD, so clinicians should consider nonrestorative sleep (or “waking up unrefreshed”) during patient assessment. Finally, our study highlights current evidence that sleep may be an important factor for individuals who wish to adopt a healthier lifestyle—our findings support public health campaigns promoting good sleep practices and behaviors and the importance of the clinician discussing sleep in primary care consultations.
St‐Onge et al recently published a scientific statement on behalf of the American Heart Association.91 Their review surveyed the literature and found that sleep duration, mostly short sleep, and sleep disorders are related to adverse cardiometabolic risk, such as obesity, hypertension, type 2 diabetes mellitus, and CVD. Unlike their review, we focused on mortality and CVD and quantitatively pooled the impact of individual hours of sleep duration and these events. We were able to show, with metaregression, that the association of short sleep duration and adverse events was lost, but the association of long sleep duration and adverse events still persists. It is possible that the adverse outcomes associated with short sleep duration may be manifested through the risk factors described by St‐Onge's review. Our findings support the clinical recommendations of the American Heart Association, in which sleep behaviors should be addressed to promote cardiac health, and public health campaigns addressing sleep behavior should include explicit guidelines for adequate sleep.
Our meta‐analysis results show a possible increase in mortality with both long and short duration of sleep relative to 7 or 8 hours, but after spline analysis, there is no difference in mortality for patients with shorter sleep duration. The spline regression is the gold standard for metaregression for nonlinear relationships to model exposures and outcomes. We further used this method to perform analysis on the subgroups studies that had more‐complete reporting that include crude event rates.
The exact mechanisms that underlie the association between sleep and CVD and mortality are not fully understood. Short sleep duration has been shown to increase levels of leptin and ghrelin,92, 93 which leads to increased appetite, caloric intake, reduce energy expenditure, and facilitates the development of obesity80 and impaired glycemic control.94 Cortisol also increases with reduced sleep, and altered growth hormone metabolism may increase CVR.95 Low‐grade inflammation occurs with reduced sleep, which may be associated with CVD and cancer. Long sleep duration may be associated with an increased risk of CVD because of an adverse CVR factor profile or prevalent comorbidities that lead to fatigue, such as chronic inflammatory disorders and anemia. Depressive symptoms, low socioeconomic status, unemployment, and low physical activity are also associated with long sleep duration, which may confound the association of long sleep with morbidity and mortality.20
An important consideration in the temporal relationship between sleep and adverse outcomes is the potential influence of CVR factors. For example, a Japanese study observed that sleep disturbances were associated with a higher risk of later‐onset of type 2 diabetes mellitus.96 In addition, it is unclear whether abnormal sleep is a marker of undiagnosed prevalent CVDs or of early/latent disease that subsequently manifests in adverse cardiovascular outcomes and death. Some studies have attempted to reduce the effect of baseline prevalent CVD by excluding patients with these conditions whereas other studies adjusted for these factors. Despite our sensitivity analysis considering exclusion and adjustments, there may still be residual confounding given that there may be undiagnosed or latent disease or risk factors because some of these population‐based studies do investigate patients at baseline for these variables and rely on self‐reporting. The other important consideration is whether the increased incident CVR is causally related to sleep directly or whether abnormal sleep patterns may contribute to adverse health behaviors that increase CVR thereby contributing to the increase in cardiovascular events.
Several studies have evaluated the mismatch between self‐reported sleep and more‐objective measures. An analysis of 669 participants in the CARDIA (Coronary Artery Risk Development in Young Adults) Sleep Study suggests a moderate correlation between self‐reported and objectively measured sleep duration with evidence of systematic errors in the mean and calibration.97 Another study of 2086 Hispanic Americans suggests a moderate correlation between self‐reported sleep and actigraphy results.98 A smaller study that compared self‐reported sleep and actigraphy in 56 participants reported a poor agreement between sleep duration and quality, as assessed by a questionnaire and objectively measured sleep.99 In addition, a different analysis of 63 patients who were overweight and obese individuals and who underwent actigraphy also reported a weak correlation between usual sleep time and actigraph estimates.100 With respect to CVR, studies suggest that self‐reported sleep duration is different from objectively assess sleep duration.101, 102 Although the exact reasons for discrepancies between subjective and objective measures are not clear, it appears that self‐reported sleep is only, at best, moderately correlated with objective measures of sleep and perhaps multiple measures of sleep duration should be recommended for future studies.
In the current analysis, the study by Kripke et al53 represented more than one third of the entire cohort, and this large study has implications to the interpretation of the results. This cohort was a diverse group of adults who were friends or relatives of American of Cancer Society volunteers who were aged between 30 and 102 years. The mean age in this study was 57 years and 43% of participants were female, which were both slightly lower than the average of 60 years of age and 52% female in all the included studies. In addition, the study took place in the 1980s, which may affect the applicability of its findings to the current population. Collectively, these findings may limit the generalizability of the current study.
Our study has a number of limitations. Although we used adjusted estimates where available, there are likely to be residual or unmeasured confounding and bias. For example, an underlying physical or mental health condition may be the driver behind extreme sleep patterns. A key limitation was that sleep duration was assessed by self‐reported questionnaires. It is unclear whether this is truly reflective of actual sleep patterns given that there are studies that clearly show that with respect to CVR, self‐reported sleep duration and objectively assessed sleep duration are significantly different.101, 102 Another limitation was the absence of individual patient‐level data, so we could not make assumptions about the CVR factor profiles of patients based on their sleep duration or quality. Some studies did report baseline risk factors for patients, but every study reported different risk factors, and the combinations of the risk‐factor profiles reported were too heterogeneous to make general assumptions. Although we demonstrated an association between sleep quality, duration, and outcomes, these relationships cannot infer causality and it is unclear whether sleep duration or quality is a marker of prevalent CVR, an adverse CVR factor profile, or adverse health behaviors that contribute to the adverse outcomes reported.
Conclusion
In conclusion, we found a significant association between deviations in sleep duration and both mortality and adverse cardiovascular outcomes. National guidelines should consider advocating this as the recommended sleep duration. We also found evidence that sleep duration above the recommended level of 7 to 8 hours was associated with a moderate degree of harm compared with sleeping less than the suggested duration. Furthermore, the greater the divergence from the recommended durations of sleep, the greater the association for cardiovascular harm and mortality. Our study suggests that abnormal sleep is a marker of elevated CVR—and greater consideration should be given in exploring during patient consultations in both the duration and quality of sleep.
Disclosures
None.
Supporting information
Data S1. Full Description of Methods and Data Analysis.
Data S2. MOOSE Reporting Checklist for Authors, Editors, and Reviewers of Meta‐Analyses of Observational Studies.9
Data S3. Inclusion Criteria and Search Strategy.
Data S4. Definition of Sleep Quality
Data S5. Cardiovascular Disease and Cardiovascular Risk Factors in Studies
Data S6. Risk of Bias Table
Data S7. Study Reference Groups and Analyses
Data S8. Cubic spline models for mortality and adverse cardiovascular events.
Data S9. Sleep duration and risk of all‐cause mortality and funnel plot.
Data S10. Summary of meta‐analysis results. A, Sleep duration and risk of all‐cause mortality. B, Sleep duration and cause specific mortality. C, Sleep duration and risk of adverse cardiovascular events. D, Sleep quality and risk of mortality and adverse cardiovascular events. E, Incremental decrease in sleep hour and adverse outcomes.
Data S11. Sleep duration and coronary heart disease mortality and funnel plot.
Data S12. Sleep duration and coronary heart disease and funnel plot.
Data S13. Sleep duration and stroke mortality and funnel plot.
Data S14. Sleep duration and stroke and funnel plot.
Data S15. Sleep duration and cardiovascular mortality and funnel plot.
Data S16. Sleep duration and cardiovascular disease and funnel plot.
Data S17. Sleep quality and adverse outcomes and funnel plot.
Data S18. Sensitivity analysis of meta‐analysis including studies that excluded patients with baseline cardiovascular disease, adjusted for cardiovascular risk factors, and adjusted for obstructive sleep apnea or snoring. A, Sleep duration and adverse outcomes among studies that excluded baseline cardiovascular disease. B, Sleep duration and adverse outcomes among studies that adjusted for cardiovascular risk factors. C, Sleep duration and adverse outcomes among studies that adjusted for obstructive sleep apnea or snoring.
Acknowledgments
We thank Francesco Cappuccio for his useful comments and suggestions.
(J Am Heart Assoc. 2018;7:e008552 DOI: 10.1161/JAHA.118.008552.)
Notes
* References 11, 21, 23, 25, 26, 29, 32, 33, 36, 41, 44, 47, 48, 49, 52, 55, 56, 57, 60, 64, 66, 68, 70, 71, 79, 80, 84, 86, 87, 88.
References
- 1. American Heart Association . 2015 Heart Disease and Stroke Statistics. Available at: https://www.heart.org/idc/groups/ahamah-public/@wcm/@sop/@smd/documents/downloadable/ucm_470704.pdf. Accessed June 27, 2018.
- 2. Meng L, Zheng Y, Hui R. The relationship of sleep duration and insomnia to risk of hypertension incidence: a meta‐analysis of prospective cohort studies. Hypertens Res. 2013;36:985–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Guo X, Zheng L, Wang J, Zhang X, Zhang X, Li J, Sun Y. Epidemiological evidence for the link between sleep duration and high blood pressure: a systematic review and meta‐analysis. Sleep Med. 2013;14:324–332. [DOI] [PubMed] [Google Scholar]
- 4. Holliday EG, Magee CA, Kritharides L, Banks E, Attia J. Short sleep duration is associated with risk of future disease but no cardiovascular disease: a prospective study and meta‐analysis. PLoS One. 2013;8:e82305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cappuccio FP, D'Elia L, Strazzull P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta‐analysis. Diabetes Care. 2010;33:414–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity. 2008;16:643–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, Miller MA. Meta‐analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Westerlund A, Belloccco R, Sundstrom J, Adami HO, Akerstedt T, Trolle Lagerros Y. Sleep characteristics and cardiovascular events in a large Swedish cohort. Eur J Epidemiol. 2013;28:463–473. [DOI] [PubMed] [Google Scholar]
- 9. Leng Y, Cappuccio FP, Wainwright NW, Surtees PG, Luben R, Brayne C, Khaw KT. Sleep duration and risk of fatal and nonfatal stroke: a prospective study and meta‐analysis. Neurology. 2015;84:1072–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta‐analysis of prospective studies. Eur Heart J. 2011;32:1482–1492. [DOI] [PubMed] [Google Scholar]
- 11. Suzuki E, Yorifuji T, Ueshima K, Takao S, Sugiyama M, Ohta T, Ishikaawa‐Takata K, Doi H. Sleep duration, sleep quality and cardiovascular disease mortality among the elderly: a population‐based cohort study. Prev Med. 2009;49:135–141. [DOI] [PubMed] [Google Scholar]
- 12. Hoevenaar‐BLom MP, Spijkerman AM, Kromhout D, van den Berg JF, Verschunren WM. Sleep duration and sleep quality in relation to 12‐year cardiovascular disease incidence: the MORGEN study. Sleep. 2011;34:1487–1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Perk J, de Backer G, Gohlke H, Graham I, Reiner Z, Vershuren M, Albus C, Benlian P, Boysen G, Cifkova R, Deaton C, Ebrahim S, Fisher M, Germano G, Hobbs R, Hoes A, Karadeniz S, Mezzani A, Prescott E, Ryden L, Scherer M, Syvänne M, Scholte op Reimer WJ, Vrints C, Wood D, Zamaorano JL, Zannad F; European Association for Cardiovascular Prevention & Rehabilitation (EACPR); ESC Committee for Practice Guidelines (CPG) . European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur Heart J. 2012;33:1635–1701. [DOI] [PubMed] [Google Scholar]
- 14. National Sleep Foundation . National Sleep Foundation Recommends New Sleep Times. Available at: http://sleepfoundation.org/press-release/national-sleep-foundation-recommends-new-sleep-times/page/0/1. Accessed June 27, 2018.
- 15. CDC . Are you getting enough sleep? Available at: http://www.cdc.gov/features/sleep/index.html. Accessed June 27, 2018.
- 16. Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Sleep duration and all‐cause mortality: a systematic review and meta‐analysis of prospective studies. Sleep. 2010;33:585–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. McBeth J, Wilkie R, Bedson J, Chew‐Graham CA, Lacey R. Sleep disturbance and chronic widespread pain. Curr Rheumatol Rep. 2015;17:1–10. [DOI] [PubMed] [Google Scholar]
- 18. Akerstedt T, Nilsson PM. Sleep as restitution: a introduction. J Inter Med. 2003;254:6–12. [DOI] [PubMed] [Google Scholar]
- 19. Grander MA, Drummond SPA. Who are the long sleepers? Towards an understanding of the mortality relationship. Sleep Med Rev. 2007;11:341–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Stranges S, Dorn JM, Shipley MJ, Kandala NB, Trevisan M, Miller MA, Donahue RP, Hovey KM, Ferrie JE, Marmot MG, Cappuccio FP. Correlates of short and long sleep duration: a cross‐cultural comparison between United Kingdom and the United States: the Whitehall II Study and the Western New York Health Study. Am J Epidemiol. 2008;168:1353–1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Akersted T, Ghilotti F, Grotta A, Bellavia A, Lagerros YT, Bellocco R. Sleep duration, mortality and the influence of age. Eur J Epidemiol. 2017;32:881–891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Amagai Y, Ishikawa S, Gotoh T, Kayaba K, Nakamura Y, Kajii E. Sleep duration and incidence of cardiovascular events in a Japanese population: the Jichi Medical School Cohort Study. J Epidemiol. 2010;20:106–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Aurora RN, Kim JS, Crainiceanu C, O'Hearn D, Punjabi NM. Habitual sleep duration and all‐cause mortality in a general community sample. Sleep. 2016;39:1903–1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ayas NT, White DP, Manson JE, Stampfer MJ, Speizer FE, Malhotra A, Hu FB. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163:205–209. [DOI] [PubMed] [Google Scholar]
- 25. Bellavia A, Akerstedt T, Bottai M, Wolk A, Orsini N. Sleep duration and survival percentiles across categories of physical activity. Am J Epidemiol. 2014;179:484–491. [DOI] [PubMed] [Google Scholar]
- 26. Burazeri G, Gofin J, Kark JD. Over 8 hours of sleep—marker of increased mortality in Mediterranean population: follow‐up population study. Croat Med J. 2003;44:193–198. [PubMed] [Google Scholar]
- 27. Cai H, Shu XO, Xiang YB, Yang G, Li H, Ji BT, Gao J, Gao YT, Zheng W. Sleep duration and mortality: a prospective study of 113,138 middle‐aged and elderly Chinese men and women. Sleep. 2015;38:529–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Canivet C, Nilsson PM, Lindeberg SI, Karasek R, Ostergren PO. Insomnia increases risk for cardiovascular events in women and in men with low socioeconomic status: a longitudinal, register‐based study. J Psychosom Res. 2014;76:292–299. [DOI] [PubMed] [Google Scholar]
- 29. Castro‐Costa E, Dewey ME, Ferri CP, Uchoa E, Firmo JO, Rocha FL, Prince M, Lima‐Costa MF, Stewart R. Association between sleep duration and all‐cause mortality in old age: 9‐year follow‐up of the Bambui Cohort Study, Brazil. J Sleep Res. 2011;20:303–310. [DOI] [PubMed] [Google Scholar]
- 30. Chandola T, Ferrie JE, Perski A, Akbaraly T, Marmot MG. The effect of short sleep duration on coronary heart disease risk is greatest among those with sleep disturbance: a prospective study from the Whitehall II cohort. Sleep. 2010;33:739–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Chen JC, Brunner RL, Ren H, Wassertheil‐Smoller S, Larson JC, Levine DW, Allison M, Naughton MJ, Stefanick ML. Sleep duration and risk of ischemic stroke in postmenopausal women. Stroke. 2008;39:3185–3192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chen HC, Su TP, Chou P. A nine‐year follow up study of sleep patterns and mortality in community dwelling older adults in Taiwan. Sleep. 2013;36:1187–1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chien KL, Chen PC, Hsu HC, Su TC, Sung FC, Chen MF, Lee YT. Habitual sleep duration and insomnia and the risk of cardiovascular events and all‐cause death: report from a community‐based cohort. Sleep. 2010;33:177–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Cohen‐Mansfeld J, Perach R. Sleep duration, nap habits, and mortality in older person. Sleep. 2012;35:1003–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ensrud KE, Blackwell TL, Ancoli‐Israel S, Redline S, Cawthon PM, Paudel ML, Dam TTL, Stone KL. Sleep disturbances and risk of frailty and mortality in older men. Sleep Med. 2012;13:1217–1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gangwisch JE, Heymsfield SB, Boden‐Albala B, Guijs RM, Kreier F, Opler MG, Pickering TG, Rundle AG, Zammit GK, Malaspina D. Sleep duration associated with mortality in elderly, but not middle‐aged, adults in a large US sample. Sleep. 2008;31:1087–1096. [PMC free article] [PubMed] [Google Scholar]
- 37. Garde AH, Hansen AM, Holtermann A, Gyntelberg F, Suadicani P. Sleep duration and ischemic heart disease and all‐cause mortality: prospective cohort study on effects of transquilizers/hypnotics and perceived stress. Scand J Work Environ Health. 2013;39:550–558. [DOI] [PubMed] [Google Scholar]
- 38. Gianfagna F, Veronesi G, Bertu L, Cesana G, Grassi G, Stranges S, Callegari C, Ferrario MM. Influence of sleep disturbances on age at onset and long‐term incidences of major cardiovascular events: the MONICA‐Brianza and PAMELA cohort studies. Sleep Med. 2016;21:126–132. [DOI] [PubMed] [Google Scholar]
- 39. Goto A, Yasumara S, Nishise Y, Sakihara S. Association of health behaviour and social role with total mortality among Japanese elders in Okinawa, Japan. Aging Clin Exp Res. 2003;15:443–450. [DOI] [PubMed] [Google Scholar]
- 40. Hale L, Parente V, Dowd JB, Sands M, Berger JS, Song Y, Martin LW, Allison MA. Fibrinogen may mediate the association between long sleep duration and coronary heart disease. J Sleep Res. 2013;22:305–314. [DOI] [PubMed] [Google Scholar]
- 41. Hall MHK, Smagula SF, Boudreau RM, Ayonayon HM, Goldman SE, Harris TB, Naydeck BL, Rubin SM, Samuelsson L, Satterfield S, Stone KL, Visser M, Newman AB. Association between sleep duration and mortality is mediated by markers of inflammation and health in older adults: the Health, Aging and Body Composition Study. Sleep. 2015;38:189–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hamazaki Y, Morikawa Y, Nakamura K, Sakurai M, Miura K, Ishizaki M, Kido T, Naruse Y, Suwazono Y, Nakagawa H. The effects of sleep duration on the incidence of cardiovascular events among middle‐aged male workers in Japan. Scand J Work Environ Health. 2011;37:411–417. [DOI] [PubMed] [Google Scholar]
- 43. Helbig AK, Stockl D, Heier M, Ladwig KH, Meisinger C. Symptoms of insomnia and sleep duration and their association with incident strokes: findings from the population‐based MONICA/KORA Augsburg Cohort study. PLoS One. 2015;10:e0134480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Heslop P, Smith GD, Metcalfe C, Macleod J, Hart C. Sleep duration and mortality: the effect of short or long sleep duration on cardiovascular and all‐cause mortality in working men and women. Sleep Med. 2002;3:305–314. [DOI] [PubMed] [Google Scholar]
- 45. Huang YC, Wahlqvist ML, Lee MS. Sleep quality and survival of elderly Taiwanese for dietary diversity and pyridoxine in men and women. J Am Coll Nutr. 2013;32:417–427. [DOI] [PubMed] [Google Scholar]
- 46. Hublin C, Partinen M, Koskenvuo M, Kaprio J. Sleep and mortality: a population‐based 22‐year follow‐up study. Sleep. 2007;30:1245–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ikehara S, Iso H, Date C, Kikuchi S, Watanabe Y, Wada Y, Inaba Y, Tamakoshi A. Association of sleep duration and mortality from cardiovascular disease and other causes for Japanese men and women: the JACC study. Sleep. 2009;32:259–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Jung KI, Song CH, Ancholi‐Israel S, Barrett‐Connor E. Gender differences in nighttime sleep and daytime napping as predictors of mortality in older adults: the Rancho Bernardo Study. Sleep Med. 2013;14:12–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Kakizaki M, Kuriyama S, Nakaya N, Sone T, Nagai M, Sugawara Y, Hozawa A, Fukudo S, Tsuji I. Long sleep duration and cause‐specific mortality according to physical function and self‐rated health: the Ohsaki cohort study. J Sleep Res. 2013;22:209–216. [DOI] [PubMed] [Google Scholar]
- 50. Kawachi T, Wada K, Nakamura K, Tsuji M, Tamura T, Konishi K, Nagata C. Sleep duration and the risk of mortality from stroke in Japan, The Takayama Cohort Study. J Epidemiol. 2016;26:123–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kim Y, Wilkens LR, Schembre SM, Henderson BE, Kolonel LN, Goodman MT. Insufficient and excessive amounts of sleep increase the risk of premature death from cardiovascular and other disease: the Multiethnic cohort study. Prev Med. 2013;57:377–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Kojima M, Wakai K, Kawamura T, Tamakoshi A, Aoki R, Lin Y, Nakayama T, Horibe H, Aoki N, Ohno Y. Sleep patterns and total mortality: a 12‐year follow‐up study in Japan. J Epidemiol. 1999;10:87–93. [DOI] [PubMed] [Google Scholar]
- 53. Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–136. [DOI] [PubMed] [Google Scholar]
- 54. Lan TY, Lan TH, Wen CP, Lin TH, Chuang YL. Nighttime sleep, Chinese afternoon nap and mortality in the elderly. Sleep. 2007;30:1105–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Lee JSW, Auyeung TW, Leung J, Chan D, Kwok T, Woo J, Wing YK. Long sleep duration is associated with higher mortality in older people independent of frailty: a 5‐year cohort study. J Am Med Dir Assoc. 2014;15:649–654. [DOI] [PubMed] [Google Scholar]
- 56. Lee WJ, Pen LN, Lian CK, Chiou ST, Chen LK. Long sleep duration, independent of frailty and chronic inflammation, was associated with higher mortality: a national population‐based study. Geriatr Gerontol Int. 2017;17:1481–1487. [DOI] [PubMed] [Google Scholar]
- 57. Li Y, Sato Y, Yamaguchi N. Potential biochemical pathways for the relationship between sleep duration and mortality. Sleep Med. 2013;14:98–104. [DOI] [PubMed] [Google Scholar]
- 58. Liu J, Yuen J, Kang S. Sleep duration, C‐reactive protein and risk of incident coronary heart disease—results from the Framingham offspring study. Nutr Metab Cardiovasc Dis. 2014;24:600–605. [DOI] [PubMed] [Google Scholar]
- 59. Magee CA, Kritharides L, Attias J, Mcelduff P, Banks E. Short and long sleep duration are associated with prevalent cardiovascular disease in Australian adults. J Sleep Res. 2011;21:441–447. [DOI] [PubMed] [Google Scholar]
- 60. Magee CA, Holliday EG, Attia J, Kritharides L, Banks E. Investigation of the relationship between sleep duration, all‐cause mortality, and pre‐existing disease. Sleep Med. 2013;14:591–596. [DOI] [PubMed] [Google Scholar]
- 61. Mallon L, Broman JE, Hetta J. Sleep complaints predict coronary artery disease mortality in males: a 12‐year follow‐up study of a middle‐aged Swedish population. J Intern Med. 2002;251:207–216. [DOI] [PubMed] [Google Scholar]
- 62. Martin JL, Fiorentino L, Jouldjian S, Mitchell M, Josephson KR, Alessi CA. Poor self‐reported sleep quality predicts mortality within one year of inpatients post‐acute rehabilitation among older adults. Sleep. 2011;34:1715–1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Meisinger C, Heier M, Lowel H, Schneider A, Doring A. Sleep duration and sleep complaints and risk of myocardial infarction in middle‐aged men and women from the general population: the MONICA/KORA Augsburg Cohort Study. Sleep. 2007;30:1121–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Mesas AE, Lopez‐Garcia E, Leong Munoz LM, Guallar‐Castillon P, Rodriguez‐Artalejo F. Sleep duration and mortality according to health status in older adults. J Am Geriatr Soc. 2010;58:1870–1877. [DOI] [PubMed] [Google Scholar]
- 65. Pan A, de Silva DA, Yuan JM, Koh WP. Sleep duration and risk of stroke mortality among Chinese adults. Stroke. 2014;45:1620–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE, Stampfer MJ, Hu FB. A prospective study of sleep duration and mortality risk in women. Sleep. 2004;27:440–444. [DOI] [PubMed] [Google Scholar]
- 67. Pollak CP, Perlick D, Linsner JP, Wenston J, Hsieh F. Sleep problems in the community elderly as predictors of death and nursing home placement. J Community Heatlh. 1990;15:123–135. [DOI] [PubMed] [Google Scholar]
- 68. Qui L, Sautter J, Liu Y, Gu D. Age and gender differences in linkages of sleep with subsequent mortality and health among very old Chinese. Sleep Med. 2011;1008–1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Qureshi AI, Giles WH, Croft JB, Bliwise DL. Habitual sleep patterns and risk for stroke and coronary heart disease: a 10‐year follow‐up from NHANES I. Neurology. 1997;48:904–911. [DOI] [PubMed] [Google Scholar]
- 70. Rhee CW, Kim JY, Park BJ, Li ZM, Ahn YO. Impact of individual and combined health behaviours on all causes of premature mortality among middle aged men in Korea: the Seoul Male Cohort Study. J Prev Med Public Health. 2012;45:14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Rod NH, Kumari M, Lange T, Kivimaki M, Shipley M, Ferrie J. The joint effect of sleep duration and disturbed sleep on cause‐specific mortality: results from the Whitehall II cohort study. PLoS One. 2014;9:e91965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Ruigomez A, Zlonso J, Anto JM. Relationship of health behaviours to five‐year mortality and adverse COPD outcomes. Sleep Med. 2012;13:476–483.22429651 [Google Scholar]
- 73. Ruiter Petrov ME, Letter AJ, Howard VJ, Kleindorfer D. Self‐reported sleep duration in relation to incident stroke symptoms: nuances by body mass and race from the REGARDS study. J Stroke Cerebrovasc Dis. 2014;23:e123–e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Sands‐Lincoln M, Loucks EB, Lu B, Carskadon MA, Sharkey K, Stefanick ML, Ockene J, Shah N, Hairston KG, Robinson JG, Limacher M, Hales L, Eaton CB. Sleep duration, insomnia, and coronary heart disease among postmenopausal women in the Women's Health Initiative. J Womens Health. 2013;22:477–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Shankar A, Koh WP, Yan JM, Lee HP, Yu MC. Sleep duration and coronary heart disease mortality among Chinese adults in Singapore: a population‐based cohort study. Am J Epidemiol. 2008;168:1367–1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Song Q, Liu X, Zhou W, Wang L, Zheng X, Wang X, Wu S. Long sleep duration and risk of ischemic stroke and hemorrhagic stroke: the Kailuan Prospective Study. Sci Rep. 2016;6:33664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Stone KL, Balckwell T, Ancoli‐Israel S, Cauley JA, Ensrud KE, Bauer DC, Barrett‐Connor E, Patel S, Hillier TA, Redline S. Actingraphic measures of sleep duration and risk of mortality in older men and women. Sleep. 2009;32:A114. [Google Scholar]
- 78. Strand LB, Tsai MK, Gunnell D, Janszky I, Wen CP, Chang SS. Self‐reported sleep duration and coronary heart disease mortality: a large cohort study of 400,000 Taiwanese adults. Int J Cardiol. 2016;207:246–251. [DOI] [PubMed] [Google Scholar]
- 79. Tamakoshi A, Ohno Y. Self‐reported sleep duration as a predictor of all‐cause mortality: result from the JACC study, Japan. Sleep. 2004;27:51–54. [PubMed] [Google Scholar]
- 80. Tusubono Y, Kukao A, Hisamichi S. Health practices and mortality in a rural Japanese population. Tohoku J Exp Med. 1993;171:339–348. [DOI] [PubMed] [Google Scholar]
- 81. Tu X, Cai H, Gao YT, Wu X, Ji BT, Yang G, Li H, Zheng W, Shu XO. Sleep duration and its correlates in middle‐aged and elderly Chinese women: the Shanghai Women's Health Study. Sleep Med. 2012;13:1138–1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Twig G, Shina A, Afex A, Derazne E, Tzur D, Cukierman‐Yaffe T, Schechter‐Amir D, Gerstein HC, Tirosh A. Sleep quality and risk of diabetes and coronary artery disease among young men. Acta Diabetol. 2016;53:261–270. [DOI] [PubMed] [Google Scholar]
- 83. Von Ruesten A, Weikert C, Fietze I, Boeing H. Association of sleep duration with chronic diseases in the European Prospective Investigation into Cancer and Nutrition (EPIC)‐Potsdam study. PLoS One. 2012;7:e30972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Wang X, Liu X, Song Q, Wu S. Sleep duration and risk of myocardial infarction all‐cause death in a Chinese population: the Kailuan study. Sleep Med. 2016;19:13–16. [DOI] [PubMed] [Google Scholar]
- 85. Werle MH, Moriguchi E, Fuchs SC, Bruscato NM, de Carli W, Danni F. Risk factors for cardiovascular disease in the very elderly: result from a cohort study in a city in southern Brazil. Eur J Cardiovasc Prev Rehabil. 2011;18:369–377. [DOI] [PubMed] [Google Scholar]
- 86. Wingard DL, Berkman LF. Mortality risk associated with sleeping patterns among adults. Sleep. 1983;6:102–107. [DOI] [PubMed] [Google Scholar]
- 87. Xiao Q, Keadle SK, Hollenbeck AR, Matthews CE. Sleep duration and total and cause‐specific mortality in a large US cohort: interrelationships with physical activity, sedentary behaviour, and body mass index. Am J Epidemiol. 2014;180:997–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Yeo Y, Ma SH, Park SK, Chang SH, Shin HR, Kang D, Yoo KY. A prospective cohort study on the relationship of sleep duration with all‐cause and disease‐specific mortality in the Korean multi‐center cancer cohort study. J Prev Med Public Health. 2013;46:271–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Zawisza K, Tobiasz‐Adamczyk B, Salas A, Brzyska M. Sleep duration and mortality among older adults in 22‐year follow up study: an analysis of possible effect modifiers. Eur J Ageing. 2015;12:119–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Zuubier LA, Liuk AI, Hofman A, Franco OH, van Someren EJWV, Tiemeier H. Fragmentation and stability of circadian activity rhythms predict mortality. Am J Epidemiol. 2015;181:54–63. [DOI] [PubMed] [Google Scholar]
- 91. St‐Onge MP, Grandner MA, Brown D, Conroy MB, Bhatt DL. Sleep duration and quality: impact on lifestyle behaviours and cardiometabolic health. Circulation. 2016;134:e367–e386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Spiegel K, Tasali E, Penev P, Van Cauter E. Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141:846–850. [DOI] [PubMed] [Google Scholar]
- 93. Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Spiegel K, Knutson K, Leproult R, Tasali E, Van Cauter E. Sleep loss: a novel risk factor for insulin resistance and type 2 diabetes. J Appl Physiol. 2005;99:2008–2019. [DOI] [PubMed] [Google Scholar]
- 95. Copinschi G. Metabolic and endocrine effects of sleep deprivation. Essent Psychopharmcol. 2005;6:341–347. [PubMed] [Google Scholar]
- 96. Kawakami N, Takatsuka N, Shimizu H. Sleep disturbance and onset of type 2 diabetes. Diabetes Care. 2004;27:282–283. [DOI] [PubMed] [Google Scholar]
- 97. Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Sleep duration: how well do self‐reports reflect objective measures? The CARDIA Sleep Study. Epidemiology. 2008;19:838–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Cespedes EM, Hu FB, Redline S, Rosner B, Alcantara C, Cai J, Hall MH, Loredo JS, Mossavar‐Rahmani Y, Ramos AR, Reid KJ, Shah NA, Sotres‐Alverez D, Zee PC, Wang R, Patel SR. Comparison of self‐reported sleep duration with actigraphy: results from Hispanic Community Health Study/Study of Latinos Sueno Ancillary Study. Am J Epidemiol. 2016;183:561–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Girschik J, Fritschi L, Heyworth J, Waters F. Validation of self‐reported sleep against actigraphy. J Epidemiol. 2012;22:462–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. O'Brien E, Hart C, Wing RR. Discrepancies between self‐reported usual sleep duration and objective measures of total sleep time in treatment seeking overweight and obese individuals. Behav Sleep Med. 2016;14:539–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. King CR, Knutson KL, Rathouz PJ, Sidney S, Liu K, Lauderdale DS. Short sleep duration and incident coronary artery calcification. JAMA. 2008;300:2859–2866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Reinhard W, Plappert N, Zeman F, Hengstenberg C, Riegger G, Novack V, Maimon N, Pfeifer M, Arzt M. Prognostic impact of sleep duration and sleep efficiency on mortality in patients with chronic heart failure. Sleep Med. 2013;14:502–509. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Full Description of Methods and Data Analysis.
Data S2. MOOSE Reporting Checklist for Authors, Editors, and Reviewers of Meta‐Analyses of Observational Studies.9
Data S3. Inclusion Criteria and Search Strategy.
Data S4. Definition of Sleep Quality
Data S5. Cardiovascular Disease and Cardiovascular Risk Factors in Studies
Data S6. Risk of Bias Table
Data S7. Study Reference Groups and Analyses
Data S8. Cubic spline models for mortality and adverse cardiovascular events.
Data S9. Sleep duration and risk of all‐cause mortality and funnel plot.
Data S10. Summary of meta‐analysis results. A, Sleep duration and risk of all‐cause mortality. B, Sleep duration and cause specific mortality. C, Sleep duration and risk of adverse cardiovascular events. D, Sleep quality and risk of mortality and adverse cardiovascular events. E, Incremental decrease in sleep hour and adverse outcomes.
Data S11. Sleep duration and coronary heart disease mortality and funnel plot.
Data S12. Sleep duration and coronary heart disease and funnel plot.
Data S13. Sleep duration and stroke mortality and funnel plot.
Data S14. Sleep duration and stroke and funnel plot.
Data S15. Sleep duration and cardiovascular mortality and funnel plot.
Data S16. Sleep duration and cardiovascular disease and funnel plot.
Data S17. Sleep quality and adverse outcomes and funnel plot.
Data S18. Sensitivity analysis of meta‐analysis including studies that excluded patients with baseline cardiovascular disease, adjusted for cardiovascular risk factors, and adjusted for obstructive sleep apnea or snoring. A, Sleep duration and adverse outcomes among studies that excluded baseline cardiovascular disease. B, Sleep duration and adverse outcomes among studies that adjusted for cardiovascular risk factors. C, Sleep duration and adverse outcomes among studies that adjusted for obstructive sleep apnea or snoring.


