Abstract
Background
Patients with impaired liver function (ILF) were excluded from clinical trials that investigated non–vitamin K antagonist oral anticoagulants (NOACs) for stroke prevention in patients with atrial fibrillation. The aim of this study was to evaluate the efficacy and safety of NOACs in atrial fibrillation patients with ILF.
Methods and Results
A cohort study based on electronic medical records was conducted from 2009 to 2016 at a multicenter healthcare provider in Taiwan and included 6451 anticoagulated atrial fibrillation patients (aged 76.7±7.0 years, 52.5% male). Patients were classified into 2 subgroups: patients with normal liver function (n=5818) and patients with ILF (n=633, 9.8%). Cox regression analysis was performed to investigate the risks of thromboembolism, bleeding, and death associated with use of NOACs and warfarin in patients with normal liver function and ILF, respectively. In patients with normal liver function, compared with warfarin therapy (n=2928), NOAC therapy (n=4048) was associated with significantly lower risks of stroke or systemic embolism (adjusted hazard ratio: 0.75; 95% confidence interval, 0.65–0.88; P<0.001) and death (adjusted hazard ratio: 0.69; 95% confidence interval, 0.60–0.80; P<0.001) with no difference in major bleeding or gastrointestinal bleeding. In patients with ILF, compared with warfarin therapy (n=394), NOAC therapy (n=342) was associated with significantly lower risk of death (adjusted hazard ratio: 0.64; 95% confidence interval, 0.49–0.83; P<0.001), but no difference in stroke or systemic embolism, major bleeding, or gastrointestinal bleeding.
Conclusions
In atrial fibrillation patients with ILF, NOAC therapy and warfarin therapy were associated with similar risks of stroke or systemic embolism, major bleeding, and gastrointestinal bleeding.
Keywords: anticoagulation, atrial fibrillation, impaired liver function, non–vitamin K antagonist oral anticoagulant, outcome
Subject Categories: Atrial Fibrillation, Cerebrovascular Disease/Stroke, Mortality/Survival
Clinical Perspective
What Is New?
Non–vitamin K antagonist oral anticoagulants, compared with warfarin, are associated with significantly lower risk of death but no difference in stroke or systemic embolism, major bleeding, or gastrointestinal bleeding in patients with atrial fibrillation and impaired liver function.
What Are the Clinical Implications?
Non–vitamin K antagonist oral anticoagulant use is a reasonable alternative to warfarin in atrial fibrillation patients aged ≥65 years with impaired liver function.
Introduction
Data on the safety and efficacy of anticoagulation therapy in atrial fibrillation (AF) patients with impaired liver function (ILF) are currently limited.1 ILF is associated with increased bleeding risk and has been included in a bleeding risk scoring system for assessing the 1‐year risk of major bleeding associated with warfarin therapy in patients with AF.2, 3, 4 In addition, hepatitis‐related chronic liver disease and cirrhosis are prevalent in Asia and are associated with higher risks of ischemic stroke, portal vein thrombosis, intracranial hemorrhage, and variceal bleeding.5, 6, 7, 8 Non–vitamin K antagonist oral anticoagulant (NOAC) represents a major advance in stroke prevention for AF patients, offering at least equivalent efficacy and less bleeding compared with warfarin.9, 10, 11, 12 Patients with ILF, however, were mostly excluded from major clinical trials of NOACs for stroke prevention in patients with nonvalvular AF.9, 10, 11, 12 Consequently, there is no recommended treatment strategy for patients with ILF according to current AF management guidelines.13, 14
At present, it is unclear whether the efficacy and safety of NOAC therapy is comparable to warfarin therapy in patients with ILF. In particular, these patients are also affected by coagulopathy, with which high bleeding and thrombotic risks are anticipated.3 A few recent studies reported comparable bleeding rates between NOAC and conventional anticoagulant therapies in patients with chronic liver disease or cirrhosis.15, 16, 17, 18 However, given the small sample sizes of these studies and the few studies evaluating efficacy and safety concurrently, more data are needed to establish the efficacy and safety of NOAC therapy in patients with ILF. The objective of this study was to compare the efficacy and safety of NOAC and warfarin therapies for stroke prevention in AF patients with ILF.
Methods
The data that support the findings of this study are available from the corresponding author on reasonable request.
In this retrospective cohort study, patient data were obtained from the Chang Gung Hospital System, which is currently the largest healthcare provider in Taiwan, comprising 3 major teaching hospitals and 4 tertiary care medical centers. The healthcare provider has >10 000 beds and admits 280 000 patients every year.19 The hospital identification number of each patient was encrypted and deidentified to protect privacy; therefore, informed consent was waived for this study. The diagnoses and laboratory data could be linked and continuously monitored using consistent data encryption. The institutional review board of Chang Gung Memorial Hospital approved the study protocol.
Study Cohort
From 2009 to 2016, 45 986 patients diagnosed with AF (International Classification of Diseases, 9th Revision [ICD‐9] code 427.31 or 10th Revision [ICD‐10] codes I48.0, I48.1, and I48.2) were identified. Among these patients, 20 673 had at least 1 prescription filled for oral anticoagulation therapy after AF diagnosis. Anticoagulation therapy was defined as using warfarin or NOACs (dabigatran, rivaroxaban, apixaban, or edoxaban).The index date was defined as the first date of prescribing NOAC or warfarin. Patients were allowed to use warfarin before initiating treatment with NOACs. We enrolled patients with AF aged ≥65 years because Taiwan's National Health Institute only reimburses payments for NOAC prescriptions for these patients. Patients were excluded if they had experienced a stroke within 2 weeks before the index date (n=3943); had deep vein thrombosis or pulmonary embolism within 6 months before the index date (n=760); received joint or heart valve replacement within 6 months before the index date (n=579); had end‐stage renal disease before the index date (n=1803); had in‐hospital bleeding, stroke, systemic embolism, or death within 7 days after the index date (n=568); were aged <65 years (n=4356), or did not have a serum AST (aspartate aminotransferase), ALT (alanine aminotransferase), or total bilirubin test within the year before the index date (n=2213). Finally, 6451 patients were eligible for this study and were divided into 2 subgroups: patients with normal liver function (n=5818) and those with ILF (n=633). ILF was defined as serum AST or ALT >2‐fold the upper limit of normal or total bilirubin >1.5‐fold the upper limit of normal.10, 11 The study design flowchart and patient enrollment are shown in Figure. The risks of stroke or systemic embolism (S/SE), major bleeding, gastrointestinal bleeding, and death were compared in patients receiving NOAC and warfarin therapies with normal liver function and ILF, respectively.
Figure 1.
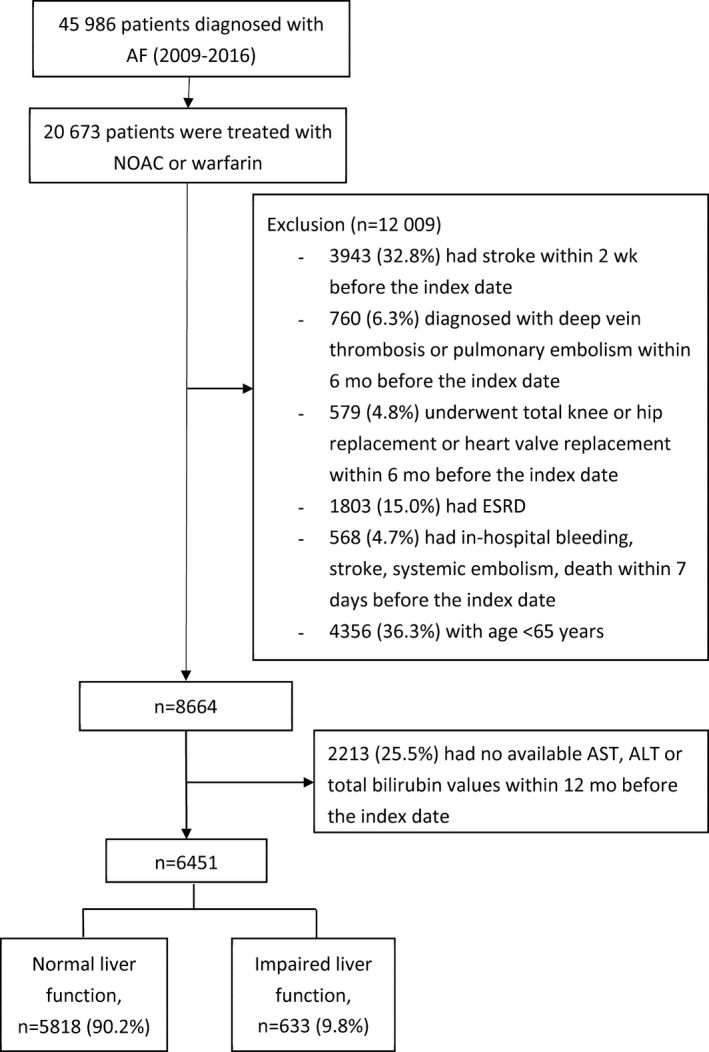
Enrollment of patients aged ≥65 years with nonvalvular atrial fibrillation (AF). From January 1, 2009, to December 31, 2016, this study evaluated 5818 patients with normal liver function vs 633 patients with impaired liver function. The index date was defined as the first date of prescribing non–vitamin K antagonist oral anticoagulant (NOAC) or warfarin. ALT indicates alanine aminotransferase; AST, aspartate aminotransferase; ESRD, end‐stage renal disease.
Assessment of Other Covariates
Baseline comorbidities of the study cohort include hypertension, diabetes mellitus, chronic kidney disease, and past history of heart failure, myocardial infarction, transient ischemic attack, S/SE, and bleeding. Laboratory data include serum hemoglobin, estimated glomerular filtration rate, and lipid profiles. Baseline medications were defined from medical records within 180 days of initiating oral anticoagulants, including antiplatelets, NSAIDs, statins, amiodarone, and anticonvulsants.
Outcome Measures
The efficacy end point was the occurrence of S/SE. The safety end point was the occurrence of major bleeding or gastrointestinal bleeding. Major bleeding was defined as hospitalization with a primary diagnosis of bleeding and blood transfusion during the period of drug use or within 14 days after the last day of drug use. Gastrointestinal bleeding was defined as hospitalization with a primary diagnosis of bleeding in any segment of the gastrointestinal tract, from the esophagus to the rectum during the drug‐use period or within 14 days after the last day of drug use. The follow‐up period was defined as being from the index date until the first occurrence of any study outcome or the end date of the study period (December 31, 2016), whichever came first. Patients who changed oral anticoagulants were censored 14 days following their switch in treatment. If an event or death occurred within 14 days following a switch, that event and time were ascribed to the initial therapy. The diagnostic codes used to identify the study outcomes and the baseline covariates are summarized in Table 1.
Table 1.
ICD‐9 and ICD‐10 Codes Used to Define Comorbidities and Outcomes
| ICD‐9 Codes | ICD‐10 Codes | Diagnosis Definition | |
|---|---|---|---|
| Heart failure | 428 | I50 | Discharge |
| Hypertension | 401, 402 | I10–I16 | Outpatient department ≥2 |
| Diabetes mellitus | 250 | E10 | Outpatient department ≥2 |
| Myocardial infarction | 410 | I21 | Discharge |
| Ischemic heart disease | 410, 411, 412, 413, 414 | I21, I22, I23, I24, I25 | Discharge |
| Peripheral vascular disease | 440 | I700, I702, I703, I704, I705, I706, I707, I708, I709 | Discharge |
| Transient ischemic attack | 435 | G45 | Discharge |
| S/SE | 433, 434, 435, 436, 437, 444 | I65, I66, I74, G458, G459 | Discharge |
| All bleeding | 430, 431, 531, 532, 533, 534, 578, 432.0, 432.1, 432.9, 852.0, 852.2, 852.4, 853.0, 530.7, 53.12, 531.4, 531.6, 532.2, 532.4, 532.6, 533.2, 533.4, 533.6, 534.2, 534.4, 534.6, 569.3, 336.1, 363.6, 719.1, 423.0, 772.5, 535.01, 535.11, 535.21, 353.1, 535.41, 535.51, 535.61, 535.71, 537.83, 537.84, 562.02, 562.03, 562.12, 562.13, 569.85, 372.72, 376.32, 377.42, 379.23, 593.81, 866.01, 866.02, 866.11, 866.12, 729.92 | I60, I62, N02, R04, R31, I690, I691, I692, J942, K250, K254, K260, K264, K270, K280, K920, K921, K922, S064, S065, S066 | Discharge |
| Gastrointestinal bleeding | 535.11, 535.21, 535.31, 535.41, 535.51, 535.61, 535.71, 537.83, 537.84, 562.12, 562.13, 569.85, 53.10, 53.20, 53.30, 53.40, 57.80, 530.7, 531.2, 531.4, 531.6, 532.2, 532.4, 532.6, 533.2, 533.4, 534.2, 534.4, 534.6, 569.3, 535.1, 562.2, 562.3 | K250, K254, K260, K264, K270, K280, K920, K921, K922 |
ICD‐9 indicates International Classification of Diseases, Ninth Revision; ICD‐10, International Classification of Diseases, Tenth Revision; S/SE, stroke or systemic embolism.
Statistical Analysis
Data were presented as mean and standard deviation or median and interquartile range for continuous variables and as proportions for categorical variables. Differences between continuous values were assessed using an unpaired 2‐tailed t test. Differences between nominal variables were compared by the χ2 test. We calculated crude incidence as the number of events divided by 100 person‐years. Cox proportional hazards regression with time‐dependent covariates was used to compare event rates between NOAC and warfarin therapies in patients with normal liver function and ILF, respectively. For comparing risks of S/SE, major bleeding, gastrointestinal bleeding, and death between NOAC and warfarin therapies, the analyses were adjusted for age, sex, hypertension, diabetes mellitus, chronic kidney disease, history of myocardial infarction, history of ischemic heart disease, history of systemic embolism, history of peripheral vascular disease, history of transient ischemic attack, history of stroke, history of heart failure, statins, amiodarone, anticonvulsants, NSAIDs, aspirin, clopidogrel, and ticagrelor. Because of the high mortality rate for AF patients with ILF, we reanalyzed the data using death as a competing risk factor for S/SE, major bleeding, and gastrointestinal bleeding. All analyses were conducted using SAS v9.4 (SAS Institute).
Results
Baseline Characteristics
Baseline characteristics of patients with or without ILF are shown in Table 2. A total of 5818 patients had normal liver function, with a mean age of 76.6±7.0 years, a mean CHA2DS2‐VASc score of 4.1±1.6, and a mean HAS‐BLED score was 2.7±0.9. In addition, 633 patients (9.8%) had ILF, with a mean age of 77.3±6.9 years, a mean CHA2DS2‐VASc score of 4.2±1.7, and a mean HAS‐BLED score of 3.2±1.1. Patients with ILF were significantly older (P=0.014), had higher HAS‐BLED scores (P<0.001), had a higher proportion of comorbidities, and had a higher proportion of amiodarone or antiplatelet use than patients with normal liver function; however, there was no significant difference in CHA2DS2‐VASc score between the 2 groups (P=0.456).
Table 2.
Baseline Characteristics of Anticoagulated AF Patients with Normal Liver Function and ILF
| All patients (n=6451) | Liver Function | P Value | ||
|---|---|---|---|---|
| Normal (n=5818) | ILF (n=633) | |||
| Age, y | 76.7±7.0 | 76.6±7.0 | 77.3±6.9 | 0.014 |
| Male, n (%) | 3389 (52.5) | 3066 (52.7) | 323 (51.0) | 0.424 |
| Past history | ||||
| Heart failure, n (%) | 2708 (42.0) | 2386 (41.0) | 322 (50.9) | <0.001 |
| Hypertension, n (%) | 4801 (74.4) | 4363 (75.0) | 438 (69.2) | 0.002 |
| Diabetes mellitus, n (%) | 2146 (33.3) | 1953 (33.4) | 193 (30.5) | 0.119 |
| Myocardial infarction, n (%) | 426 (6.6) | 357 (6.1) | 69 (10.9) | <0.001 |
| Ischemic heart disease, n (%) | 2820 (43.7) | 2546 (43.8) | 274 (43.3) | 0.819 |
| Systemic embolism, n (%) | 159 (2.5) | 144 (2.5) | 15 (2.4) | 0.871 |
| Peripheral vascular disease, n (%) | 65 (1.0) | 61 (1.1) | 4 (0.6) | 0.319 |
| Transient ischemic attack, n (%) | 215 (3.3) | 193 (3.3) | 22 (3.5) | 0.833 |
| Stroke, n (%) | 1607 (24.9) | 1455 (25.0) | 152 (24.0) | 0.582 |
| Bleeding, n (%) | 2698 (41.8) | 2443 (42.0) | 255 (40.3) | 0.409 |
| CHA2DS2‐VASc score | 4.1±1.6 | 4.1±1.6 | 4.2±1.7 | 0.456 |
| HAS‐BLED score | 2.7±0.9 | 2.7±0.9 | 3.2±1.1 | <0.001 |
| Laboratory data | ||||
| AST, U/L | 27 (22–37) | 26 (21–33) | 71 (36–110) | <0.001 |
| ALT, U/L | 20 (15–29) | 19 (14–27) | 64 (21–102) | <0.001 |
| Total bilirubin, mg/dL | 0.9 (0.6–1.2) | 0.8 (0.6–1.1) | 1.5 (0.9–2.5) | <0.001 |
| eGFR, mL/min/1.73 m2 | 64.9 (51.1–79.7) | 65.3 (51.8–79.8) | 59.9 (44.3–78.7) | <0.001 |
| Hemoglobin, g/dL | 12.6 (11.1–14.0) | 12.7 (11.2–14.1) | 11.7 (10.4–13.3) | <0.001 |
| Platelet, ×1000/μL | 187 (152–228) | 189 (155–229) | 171 (129–218) | <0.001 |
| LDL‐C, mg/dL | 94 (76–113) | 95 (77–114) | 86 (69–105) | <0.001 |
| HDL‐C, mg/dL | 46 (38–55) | 46 (38–55) | 41 (33–51) | <0.001 |
| Cholesterol, mg/dL | 163 (141–187) | 165 (142–188) | 152 (126–176) | <0.001 |
| Triglyceride, mg/dL | 95 (69–130) | 96 (70–131) | 87 (63–122) | <0.001 |
| Medication | ||||
| Statin, n (%) | 1868 (29.0) | 1714 (27.5) | 154 (24.3) | 0.007 |
| Amiodarone, n (%) | 780 (12.1) | 599 (10.3) | 181 (28.6) | <0.001 |
| Antiplatelet, n (%) | 3696 (57.3) | 3326 (57.2) | 370 (58.5) | 0.535 |
| Anticonvulsant, n (%) | 85 (1.3) | 70 (1.2) | 15 (2.4) | 0.015 |
| NSAID, n (%) | 1347 (20.9) | 1200 (20.6) | 147 (23.2) | 0.127 |
| Warfarin, n (%) | 3332 (51.7) | 2928 (50.3) | 394 (62.2) | <0.001 |
| NOAC, n (%) | 4390 (68.1) | 4048 (69.6) | 342 (54.0) | <0.001 |
| Dabigatran, n (%) | 1483 (23.0) | 1387 (23.8) | 96 (17.3) | |
| Rivaroxaban, n (%) | 2219 (34.4) | 2044 (35.1) | 175 (27.6) | |
| Apixaban, n (%) | 598 (9.3) | 534 (9.2) | 64 (10.1) | |
| Edoxaban, n (%) | 90 (1.4) | 83 (1.4) | 7 (1.1) | |
Values are mean±SD or median (interquartile range) except as noted. CHA2DS2‐VASc score awards 1 point each for congestive heart failure, hypertension, diabetes mellitus, vascular disease, age 65–74 y, and female sex (sex category) and 2 points each for age ≥75 y and previous stroke or transient ischemic attack. HAS‐BLED score awards 1 point each for hypertension, abnormal renal or liver function, stroke, bleeding history, labile international normalized ratio, age ≥65 y, and antiplatelet drug or alcohol use. AF indicates atrial fibrillation; ALT, alanine aminotransferase; AST, aspartate aminotransferase; eGFR, estimated glomerular filtration rate; HDL‐C, high‐density lipoprotein; ILF, impaired liver function; LDL‐C, low‐density lipoprotein; NOAC, non–vitamin K antagonist oral anticoagulant.
Patients With Normal Liver Function
Table 3 (upper panel) shows the event rate per 100 person‐years with 95% confidence intervals (CIs) for adverse outcomes associated with types of oral anticoagulants in patients with AF and normal liver function. In these patients, the respective event rates in the NOAC and warfarin groups were 5.52 and 8.08 per 100 person‐years for S/SE, 1.23 and 2.16 per 100 person‐years for major bleeding, 1.27 and 1.23 per 100 patient‐years for gastrointestinal bleeding, and 2.80 and 3.65 per 100 person‐years for death. In addition, adjusted hazard ratios (aHRs), 95% CIs, and P values were given for prescription of NOAC versus warfarin in these patients. As shown in the Table 3, compared with warfarin therapy (n=2928), NOAC therapy (n=4048) was associated with significantly lower risks of S/SE (aHR: 0.75; 95% CI, 0.65–0.88; P<0.001) and death (aHR: 0.69; 95% CI, 0.60–0.80; P<0.001) with no significant difference in major bleeding or gastrointestinal bleeding.
Table 3.
Event Rate and Risk of S/SE, Bleeding, and Death in Anticoagulated AF Patients
| Event Rate/100 Person‐Years (95% CI) | Crude | Adjusteda | Competing Risk | |||||
|---|---|---|---|---|---|---|---|---|
| NOAC | Warfarin | HR (95% CI) | P Value | HR (95% CI) | P Value | HR (95% CI) | P Value | |
| Normal liver function (n=5818) | ||||||||
| S/SE | 5.52 (4.99–6.11) | 8.08 (7.45–8.77) | 0.78 (0.68–0.91) | <0.001 | 0.75 (0.65–0.88) | <0.001 | 0.75 (0.64–0.88) | <0.001 |
| MB | 1.23 (1.01–1.50) | 2.16 (1.87–2.50) | 0.86 (0.65–1.14) | 0.292 | 0.83 (0.62–1.11) | 0.201 | 0.81 (0.61–1.09) | 0.162 |
| GIB | 1.27 (1.04–1.54) | 1.23 (1.02–1.49) | 1.39 (1.02–1.90) | 0.039 | 1.36 (0.99–1.88) | 0.059 | 1.33 (0.95–1.85) | 0.094 |
| Death | 2.80 (2.45–3.20) | 3.65 (3.26–4.08) | 0.70 (0.61–0.80) | <0.001 | 0.69 (0.60–0.80) | <0.001 | ||
| ILF (n=633) | ||||||||
| S/SE | 8.80 (6.50–11.90) | 6.92 (5.46–8.78) | 0.99 (0.65–1.52) | 0.976 | 0.77 (0.49–1.22) | 0.271 | 0.72 (0.46–1.15) | 0.169 |
| MB | 3.86 (2.52–5.92) | 3.83 (2.83–5.19) | 1.14 (063–2.08) | 0.658 | 1.31 (0.70–2.48) | 0.399 | 1.19 (0.60–2.35) | 0.622 |
| GIB | 3.64 (2.35–5.65) | 2.17 (1.47–3.22) | 1.49 (0.79–2.81) | 0.218 | 1.68 (0.86–3.29) | 0.132 | 1.44 (0.75–2.75) | 0.272 |
| Death | 9.80 (7.43–12.93) | 12.07 (10.02–14.53) | 0.68 (0.53–0.87) | 0.002 | 0.64 (0.49–0.83) | <0.001 | ||
AF indicates atrial fibrillation; CI, confidence interval; GIB, gastrointestinal bleeding; HR, hazard ratio; ILF, impaired liver function; MB, major bleeding; NOAC, non–vitamin K antagonist oral anticoagulant; S/SE, stroke or systemic embolism.
Adjusted for age, sex, hypertension, diabetes mellitus, chronic kidney disease, history of myocardial infarction, history of ischemic heart disease, history of systemic embolism, history of peripheral vascular disease, history of transient ischemic attack, history of stroke, history of heart failure, statins, amiodarone, anticonvulsants, NSAIDs, aspirin, clopidogrel, and ticagrelor.
Patients With ILF
Table 3 (lower panel) shows the event rate per 100 person‐years with 95% CI for adverse outcomes associated with types of oral anticoagulants in patients with AF and ILF. In these patients, the respective event rates in the NOAC and warfarin groups were 8.80 and 6.92 per 100 person‐years for S/SE, 3.86 and 3.83 per 100 person‐years for major bleeding, 3.64 and 2.17 per 100 person‐years for gastrointestinal bleeding, and 9.80 and 12.07 per 100 person‐years for death. In addition, aHRs, 95% CIs, and P values were also given for prescription of NOAC versus warfarin. As shown in the Table 3, compared with warfarin therapy (n=394), NOAC therapy (n=342) was associated with significantly lower risk of death (aHR: 0.64; 95% CI, 0.49–0.83; P<0.001), but no difference was noted in S/SE, major bleeding, or gastrointestinal bleeding. The results were similar when death was treated as a competing risk in the Cox model (Table 3). We reanalyzed the data using 7 days as a censoring window for drug switches. The results were similar to the findings with 14 days as a censoring window for drug switches (Table S1).
Discussion
The main findings of this study are as follows: First, in patients with AF and normal liver function, use of NOAC has the distinct advantage of significantly reduced S/SE and death without a difference in major bleeding and gastrointestinal bleeding compared with warfarin use. Second, in patients with AF and ILF, use of NOAC has the distinct advantage of only significantly reduced death without a difference in S/SE, major bleeding, and gastrointestinal bleeding compared with warfarin use.
ILF is considered a potentially modifiable bleeding risk factor in the 2016 European Society of Cardiology guidelines for the management of AF and is an important predictor of bleeding risk in HAS‐BLED and HEMORR2HAGES scores.4, 13, 20 The coagulation system in patients with ILF is perceived to be unstable compared with healthy individuals, who have both sufficient and properly functioning procoagulants and anticoagulants. Studies of coagulation factors in patients with cirrhosis have revealed decreased amounts and disturbed procoagulant and anticoagulant activity.21, 22 The relative deficiency of both procoagulants and anticoagulants may cause increased thrombosis or bleeding depending on the prevailing circumstantial conditions.23
Significant differences in NOAC efficacy and safety were observed between AF patients with normal liver function and those with ILF. Unlike renal impairment, there is no dose adjustment rule for NOACs in patients with ILF.13, 14 The usual coagulation laboratory tests do not allow for measuring anticoagulant intensity for NOAC dose adjustment. Despite NOACs having major pharmacologic properties with advantages over warfarin, physicians often are still conservative when considering a NOAC as an appropriate replacement for warfarin in patients with ILF.
Clinical data of NOACs in patients with ILF are scarce. Patients were largely excluded from randomized controlled trials of NOACs if baseline liver function was abnormal.9, 10, 11, 12, 24, 25, 26, 27 ROCKET AF (Rivaroxaban Once‐daily oral direct factor Xa inhibition Compared with vitamin K antagonism for prevention of stroke and Embolism Trial in Atrial Fibrillation) and EINSTEIN (Oral Direct Factor Xa Inhibitor Rivaroxaban in Patients With Acute Symptomatic Deep‐Vein Thrombosis or Pulmonary Embolism) trials excluded patients with ALT levels >3 times the upper limit of normal.9, 25 RE‐LY (Randomized Evaluation of Long Term Anticoagulant Therapy) and RE‐COVER (Efficacy and Safety of Dabigatran Compared to Warfarin for 6 Month Treatment of Acute Symptomatic Venous Thromboembolism) trials excluded patients with AST or ALT levels more than twice the upper limit of normal.12, 27 ARISTOTLE (Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation), AMPLIFY (Apixaban for the Initial Management of Pulmonary Embolism and Deep‐Vein Thrombosis as First‐Line Therapy), ENGAGE AF (Effective Anticoagulation with Factor Xa Next Generation in Atrial Fibrillation), and Hokusai‐VTE (Comparative Investigation of Low Molecular Weight Heparin/Edoxaban Tosylate Versus Low Molecular Weight Heparin/Warfarin in the Treatment of Symptomatic Deep‐Vein Blood Clots and/or Lung Blood Clots) trials excluded patients with AST or ALT levels greater than twice the upper limit of normal or total bilirubin levels >1.5‐fold the upper limit of normal,10, 11, 24, 26 which was used as the criteria for ILF in the present study. Because major trials of NOAC excluded patients with ILF, data comparing NOAC and warfarin therapies in patients with ILF are restricted to small cohort studies.16, 17, 18 Three retrospective cohort studies compared the bleeding risk between NOAC and traditional anticoagulant therapies for thrombosis and stroke prevention in AF patients with cirrhosis or chronic liver disease.16, 17, 18 No significant difference in all‐cause bleeding was observed between traditional anticoagulants and NOACs during 3‐year follow‐up.16, 17, 18 Decreased risk of major bleeding was found in the NOAC group in one of the studies.16 The reason for the discrepancy between this study and ours may be that the enrollment of our study consisted of much older patients (mean age of 77 years versus 57–60 years in the previous study). In addition, the numbers of patients in the previous studies were small (N=37, N=49, and N=233).16, 17, 18 In contrast, we reported the outcomes of oral anticoagulant therapy in a much larger cohort of patients with ILF (n=633). Our results supported the notion that patients at high risk of bleeding with traditional anticoagulants also have an increased risk of bleeding with NOACs.
Liver function tests are often neglected in NOAC users. In the present cohort, 25.5% of patients in whom oral anticoagulant treatment was initiated did not have liver function examined before therapy. This may cause patients to be in danger due to incomplete assessment of bleeding risk. To estimate the bleeding risk associated with anticoagulant therapy, it is necessary to evaluate serum hemoglobin, renal function, and liver function before initiation of anticoagulant therapy.13, 14 For patients with high bleeding risk, such as elderly patients or patients with impaired liver or renal function, modifiable bleeding risk factors should be identified and causes corrected. Medications predisposing patients to bleeding such as antiplatelet drugs or NSAIDs should be avoided or balanced with the benefits of anticoagulant therapy. Patients consuming excess alcohol (≥8 drinks/wk) should receive alcohol cessation treatment.13
In the present study, we confined our analysis to patients aged ≥65 years. Elderly patients often have more comorbidities and polypharmacy, which are associated with higher bleeding risk than those without.28, 29, 30, 31 Our study agreed with a meta‐analysis of 4 major clinical trials of NOAC with improved efficacy in S/SE (relative risk: 0.81; 95% CI, 0.73–0.91; P<0.0001) and all‐cause mortality (relative risk: 0.90; 95% CI, 0.85–0.95; P<0.0001) and increased gastrointestinal bleeding (relative risk: 1.25; 95% CI, 1.01–1.55; P=0.04) when NOAC prescription was compared with warfarin.32 Our studies showed similar findings in patients with AF and normal liver function with significantly reduced S/SE (aHR: 0.75; 95% CI, 0.65–0.88; P<0.001) and death (aHR: 0.69; 95% CI, 0.60–0.80; P<0.001), with no difference in major bleeding (aHR: 0.83; 95% CI, 0.62–1.11; P=0.201) or gastrointestinal bleeding (aHR: 1.36; 95% CI, 0.99–1.88; P=0.059). In our study of patients with ILF, the results showed no difference in S/SE (aHR: 0.77; 95% CI, 0.49–1.22; P=0.271), major bleeding (aHR: 1.31; 95% CI, 0.70–2.48; P=0.399), and gastrointestinal bleeding (aHR: 1.68; 95% CI, 0.86–3.29; P=0.132) but significantly lower risk of death (aHR: 0.64; 95% CI, 0.49–0.83; P<0.001). In summary, the results of our study suggested NOACs still had efficacy and safety profiles similar to warfarin but had the distinct advantage of reduced all‐cause mortality compared with warfarin in patients with AF and ILF.
Study Strengths
The strengths of our study include a well‐defined source for a large study population; available data on baseline hemoglobin, liver function, and renal function before the initiation of anticoagulant therapy; and direct comparison of NOAC and warfarin therapies between patients with normal and ILF. To our knowledge, this study is the largest to date to evaluate the use of NOACs versus warfarin in patients with ILF.
Study Limitations
This study had several limitations. First, miscoding and misclassification are potential biases in an established database that relies on physician‐reported diagnoses. However, such miscoding and misclassification are highly unlikely to be different between patients with normal liver function and those with ILF. The favorable efficacy and safety profiles of NOACs versus warfarin in patients with normal liver function were comparable to the results of meta‐analyses and real‐world data.32, 33, 34 Second, we did not analyze the quality of anticoagulation control as reflected by time in therapeutic range in the warfarin group, given the close relationship between the time in therapeutic range and thromboembolism or bleeding. Third, we did not evaluate the influence from degree of live function abnormality or prognostic scores for cirrhosis, such as the Child–Pugh score or the model for end‐stage liver disease score. Fourth, although we adjusted the baseline differences between groups in multivariate regression analysis, other unmeasured confounders may still exist that could confound the results and conclusion. Finally, this study enrolled only Taiwanese patients; therefore, whether the results can be extrapolated to other populations remains unknown.
Conclusions
In AF patients with ILF, NOAC therapy was associated with lower risk of death compared with warfarin therapy, but no difference was observed in S/SE, major bleeding, or gastrointestinal bleeding.
Sources of Funding
This work was funded by research grants from the Chang Gung Memorial Hospital, Linkou, Taiwan (CORPG3G0261, CORPG3G0271).
Disclosures
None.
Supporting information
Table S1. Using 7 Days as a Censoring Window for Drug Switches
Acknowledgments
We acknowledge the statistical assistance and the support of the Maintenance Project of the Center for Big Data Analytics and Statistics (grant no. CLRPG3D0044) at Chang Gung Memorial Hospital for study design, monitoring, data analysis, and interpretation. This study is based in part on data from the Chang Gung Research Database provided by Chang Gung Memorial Hospital. The interpretation and conclusions do not represent the position of Chang Gung Memorial Hospital.
(J Am Heart Assoc. 2018;7:e009263 DOI: 10.1161/JAHA.118.009263.)
References
- 1. Qamar A, Vaduganathan M, Greenberger NJ, Giugliano RP. Oral anticoagulation in patients with liver disease. J Am Coll Cardiol. 2018;71:2162–2175. [DOI] [PubMed] [Google Scholar]
- 2. Lip GY, Clementy N, Pericart L, Banerjee A, Fauchier L. Stroke and major bleeding risk in elderly patients aged ≥75 years with atrial fibrillation: the Loire Valley atrial fibrillation project. Stroke. 2015;46:143–150. [DOI] [PubMed] [Google Scholar]
- 3. Amitrano L, Guardascione MA, Brancaccio V, Balzano A. Coagulation disorders in liver disease. Semin Liver Dis. 2002;22:83–96. [DOI] [PubMed] [Google Scholar]
- 4. Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user‐friendly score (HAS‐BLED) to assess 1‐year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138:1093–1100. [DOI] [PubMed] [Google Scholar]
- 5. Kuo L, Chao TF, Liu CJ, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Liao JN, Chung FP, Chen TJ, Lip GYH, Chen SA. Liver cirrhosis in patients with atrial fibrillation: would oral anticoagulation have a net clinical benefit for stroke prevention? J Am Heart Assoc. 2017;6:e005307 DOI: 10.1161/JAHA.116.005307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Qi X, Su C, Ren W, Yang M, Jia J, Dai J, Xu W, Guo X. Association between portal vein thrombosis and risk of bleeding in liver cirrhosis: a systematic review of the literature. Clin Res Hepatol Gastroenterol. 2015;39:683–691. [DOI] [PubMed] [Google Scholar]
- 7. Rajani R, Bjornsson E, Bergquist A, Danielsson A, Gustavsson A, Grip O, Melin T, Sangfelt P, Wallerstedt S, Almer S. The epidemiology and clinical features of portal vein thrombosis: a multicentre study. Aliment Pharmacol Ther. 2010;32:1154–1162. [DOI] [PubMed] [Google Scholar]
- 8. North Italian Endoscopic Club for the study and treatment of esophageal varices . Prediction of the first variceal hemorrhage in patients with cirrhosis of the liver and esophageal varices. A prospective multicenter study. N Engl J Med. 1988;319:983–989. [DOI] [PubMed] [Google Scholar]
- 9. Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, Breithardt G, Halperin JL, Hankey GJ, Piccini JP, Becker RC, Nessel CC, Paolini JF, Berkowitz SD, Fox KA, Califf RM. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–891. [DOI] [PubMed] [Google Scholar]
- 10. Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, Al‐Khalidi HR, Ansell J, Atar D, Avezum A, Bahit MC, Diaz R, Easton JD, Ezekowitz JA, Flaker G, Garcia D, Geraldes M, Gersh BJ, Golitsyn S, Goto S, Hermosillo AG, Hohnloser SH, Horowitz J, Mohan P, Jansky P, Lewis BS, Lopez‐Sendon JL, Pais P, Parkhomenko A, Verheugt FW, Zhu J, Wallentin L. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981–992. [DOI] [PubMed] [Google Scholar]
- 11. Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, Waldo AL, Ezekowitz MD, Weitz JI, Spinar J, Ruzyllo W, Ruda M, Koretsune Y, Betcher J, Shi M, Grip LT, Patel SP, Patel I, Hanyok JJ, Mercuri M, Antman EM. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369:2093–2104. [DOI] [PubMed] [Google Scholar]
- 12. Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, Pogue J, Reilly PA, Themeles E, Varrone J, Wang S, Alings M, Xavier D, Zhu J, Diaz R, Lewis BS, Darius H, Diener HC, Joyner CD, Wallentin L. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–1151. [DOI] [PubMed] [Google Scholar]
- 13. Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, Castella M, Diener HC, Heidbuchel H, Hendriks J, Hindricks G, Manolis AS, Oldgren J, Popescu BA, Schotten U, Van Putte B, Vardas P, Agewall S, Camm J, Baron Esquivias G, Budts W, Carerj S, Casselman F, Coca A, De Caterina R, Deftereos S, Dobrev D, Ferro JM, Filippatos G, Fitzsimons D, Gorenek B, Guenoun M, Hohnloser SH, Kolh P, Lip GY, Manolis A, McMurray J, Ponikowski P, Rosenhek R, Ruschitzka F, Savelieva I, Sharma S, Suwalski P, Tamargo JL, Taylor CJ, Van Gelder IC, Voors AA, Windecker S, Zamorano JL, Zeppenfeld K. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37:2893–2962. [DOI] [PubMed] [Google Scholar]
- 14. January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, Murray KT, Sacco RL, Stevenson WG, Tchou PJ, Tracy CM, Yancy CW. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130:2071–2104. [DOI] [PubMed] [Google Scholar]
- 15. Hart RG, Benavente O, McBride R, Pearce LA. Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta‐analysis. Ann Intern Med. 1999;131:492–501. [DOI] [PubMed] [Google Scholar]
- 16. Intagliata NM, Henry ZH, Maitland H, Shah NL, Argo CK, Northup PG, Caldwell SH. Direct oral anticoagulants in cirrhosis patients pose similar risks of bleeding when compared to traditional anticoagulation. Dig Dis Sci. 2016;61:1721–1727. [DOI] [PubMed] [Google Scholar]
- 17. Hum J, Shatzel JJ, Jou JH, Deloughery TG. The efficacy and safety of direct oral anticoagulants vs traditional anticoagulants in cirrhosis. Eur J Haematol. 2017;98:393–397. [DOI] [PubMed] [Google Scholar]
- 18. Goriacko P, Veltri KT. Safety of direct oral anticoagulants versus warfarin in patients with chronic liver disease and atrial fibrillation. Eur J Haematol. 2018;100:488–493. [DOI] [PubMed] [Google Scholar]
- 19. Tsai MS, Lai CH, Lee CP, Yang YH, Chen PC, Kang CJ, Chang GH, Tsai YT, Lu CH, Chien CY, Young CK, Fang KH, Liu CJ, Yeh RA, Chen WC. Mortality in tongue cancer patients treated by curative surgery: a retrospective cohort study from CGRD. PeerJ. 2016;4:e2794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gage BF, Yan Y, Milligan PE, Waterman AD, Culverhouse R, Rich MW, Radford MJ. Clinical classification schemes for predicting hemorrhage: results from the national registry of atrial fibrillation (NRAF). Am Heart J. 2006;151:713–719. [DOI] [PubMed] [Google Scholar]
- 21. Tripodi A, Primignani M, Lemma L, Chantarangkul V, Dell'Era A, Iannuzzi F, Aghemo A, Mannucci PM. Detection of the imbalance of procoagulant versus anticoagulant factors in cirrhosis by a simple laboratory method. Hepatology. 2010;52:249–255. [DOI] [PubMed] [Google Scholar]
- 22. Tripodi A, Primignani M, Chantarangkul V, Dell'Era A, Clerici M, de Franchis R, Colombo M, Mannucci PM. An imbalance of pro‐ vs anti‐coagulation factors in plasma from patients with cirrhosis. Gastroenterology. 2009;137:2105–2111. [DOI] [PubMed] [Google Scholar]
- 23. Kujovich JL. Coagulopathy in liver disease: a balancing act. Hematology Am Soc Hematol Educ Program. 2015;2015:243–249. [DOI] [PubMed] [Google Scholar]
- 24. Agnelli G, Buller HR, Cohen A, Curto M, Gallus AS, Johnson M, Masiukiewicz U, Pak R, Thompson J, Raskob GE, Weitz JI. Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med. 2013;369:799–808. [DOI] [PubMed] [Google Scholar]
- 25. Bauersachs R, Berkowitz SD, Brenner B, Buller HR, Decousus H, Gallus AS, Lensing AW, Misselwitz F, Prins MH, Raskob GE, Segers A, Verhamme P, Wells P, Agnelli G, Bounameaux H, Cohen A, Davidson BL, Piovella F, Schellong S. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med. 2010;363:2499–2510. [DOI] [PubMed] [Google Scholar]
- 26. Buller HR, Decousus H, Grosso MA, Mercuri M, Middeldorp S, Prins MH, Raskob GE, Schellong SM, Schwocho L, Segers A, Shi M, Verhamme P, Wells P. Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. N Engl J Med. 2013;369:1406–1415. [DOI] [PubMed] [Google Scholar]
- 27. Schulman S, Kearon C, Kakkar AK, Mismetti P, Schellong S, Eriksson H, Baanstra D, Schnee J, Goldhaber SZ. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361:2342–2352. [DOI] [PubMed] [Google Scholar]
- 28. Fillenbaum GG, Pieper CF, Cohen HJ, Cornoni‐Huntley JC, Guralnik JM. Comorbidity of five chronic health conditions in elderly community residents: determinants and impact on mortality. J Gerontol A Biol Sci Med Sci. 2000;55:M84–M89. [DOI] [PubMed] [Google Scholar]
- 29. Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13:57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Crooks CJ, West J, Card TR. Comorbidities affect risk of nonvariceal upper gastrointestinal bleeding. Gastroenterology. 2013;144:1384–1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Leiss W, Mean M, Limacher A, Righini M, Jaeger K, Beer HJ, Osterwalder J, Frauchiger B, Matter CM, Kucher N, Angelillo‐Scherrer A, Cornuz J, Banyai M, Lammle B, Husmann M, Egloff M, Aschwanden M, Rodondi N, Aujesky D. Polypharmacy is associated with an increased risk of bleeding in elderly patients with venous thromboembolism. J Gen Intern Med. 2015;30:17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, Camm AJ, Weitz JI, Lewis BS, Parkhomenko A, Yamashita T, Antman EM. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta‐analysis of randomised trials. Lancet. 2014;383:955–962. [DOI] [PubMed] [Google Scholar]
- 33. Pan KL, Singer DE, Ovbiagele B, Wu YL, Ahmed MA, Lee M. Effects of non‐vitamin k antagonist oral anticoagulants versus warfarin in patients with atrial fibrillation and valvular heart disease: a systematic review and meta‐analysis. J Am Heart Assoc. 2017;6:e005835 DOI: 10.1161/JAHA.117.005835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Larsen TB, Skjoth F, Nielsen PB, Kjaeldgaard JN, Lip GY. Comparative effectiveness and safety of non‐vitamin K antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: propensity weighted nationwide cohort study. BMJ. 2016;353:i3189. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Using 7 Days as a Censoring Window for Drug Switches


