Abstract
Background
Rapid detection of sources and transmission routes by molecular methods provides key data for risk management of methicillin-resistant Staphylococcus aureus-induced infections acquired in both the community and hospitals. This study aimed to determine the clonal relationship of methicillin-resistant S. aureus strains isolated from our hospital by pulsed-field gel electrophoresis (PFGE) and Staphylococcal protein A (spa) typing methods and to identify the predominant clones in Cukurova Region, Turkey.
Results
All isolates analyzed by PFGE were distributed among 11 clusters. Clusters A (n = 19) and B (n = 27) were 84.1% similar and accounted for 61% of all samples. All isolates were distributed among 18 spa types, with the most common type being t030 with 31 isolates (41.3%), followed by t223 with nine isolates (12%) and t127 with seven isolates (9.3%).
Conclusions
We found that t030 was the most common spa type in the area where the study was conducted, as also previously shown in studies undertaken in Turkey. However, the rate of t030 in our study was below the rates reported in the literature. We also detected some rare or sporadic spa types like t127, which has not been previously defined in our country. We consider that the spa typing and PFGE methods are useful for research on clonal relations in monitoring the changing prevalent clones in specific regions.
Keywords: spa typing, PFGE, MRSA, Protein a, Epidemiology
Background
Staphylococcus aureus, which can be found as floral bacteria in the skin and mucous membranes of humans, have the ability to develop resistance in a short time to broad-spectrum antibiotics, such as the β-lactam group of antibiotics, aminoglycosides, and quinolones that are widely used for the treatment of severe infections in clinical practice [1]. Methicillin-resistant S. aureus, first reported in the UK in 1961, remains to be a serious problem for hospitals. Various hospital-acquired methicillin-resistant S. aureus clones have spread across the world, becoming a major cause of mortality and morbidity in hospitals. The community-acquired MRSA clones first appeared at the beginning of the 1990s; then, some successful clones spread to hospitals and became predominant in the USA and Europe [2].
In order to identify the epidemiologic characteristics of MRSA strains and more importantly to study the evolution and spreading of epidemic clones, there is a need to employ applicable and reproducibility molecular methods with sufficient discriminative power that are capable of monitoring changes in time. The methods mostly used for this purpose include pulsed-field gel electrophoresis (PFGE), Multilocus Sequence Typing (MLST), staphylococcal cassette chromosome mec (SCCmec) typing, and staphylococcal protein A (spa) typing [3]. It is agreed that the PFGE method is the gold standard particularly for the short-term surveillance of S. aureus typing [3, 4]. Despite the difficulties in reproducibility and interlaboratory reliability, many countries have established a nomenclature for their local pulsotypes through the standardization of PFGE protocols [5, 6]. Sequence-based methods, such as MLST and spa typing are highly reproducible among laboratories, can easily be standardized, and have common names worldwide, rendering these methods more advantageous compared to the PFGE method [6, 7]. Although MLST has a lower distinction power than spa typing, it is a superior method for monitoring clonal evolution. The spa typing method, on the other hand, not only provides an sufficient discriminative power but also has the advantage of being cost-effective as it targets a single locus [8]. Moreover, the analysis of spa types using the based upon repeat patterns (BURP) algorithm has been found highly comparable to MLST [9].
This study aimed to detected the clonal relationship of MRSA strains isolated from clinical samples in our hospital by pulsed-field gel electrophoresis (PFGE) and Staphylococcal protein A (spa) typing methods and to determinated the predominant clones in Cukurova Region, Turkey.
Methods
A total of 197 non-duplicate Staphylococcus aureus (S.aureus) in 311 Staphylocoocus spp. isolates from different patients were collected between November-2012 and December-2013 from the clinical samples sent to the Central Laboratory of Çukurova University, Balcali Hospital, Turkey (Tables 1 and 2).
Table 1.
Study Patients Characteristics and Epidemiologic Classification
| Characteristics | n = 75 | percent |
|---|---|---|
| Sex: F/M | 23/52 | 30.6/69.4 |
| Age Distribution: | ||
| Median/IQR | 34/0–85 | – |
| Inpatients/Outpatients | 64/11 | 85.3/14.7 |
| Samples | ||
| Wound IP/OP | 20/10 | 26.7/13.3 |
| Tracheal aspirate IP/OP | 31/− | 41.3/− |
| Blood IP/OP | 11/− | 14.7/− |
| Urine IP/OP | 2/1 | 2.7/1.3 |
F Female, M Male, IQR Interquartile range, IP Inpatients, OP Outpatients
Table 2.
Distribution of isolates to hospital units
| Unit | Isolates number (%) |
|---|---|
| Pediatric Intensive Care Unit | 10 (13%) |
| Reanimation Intensive Care Unit | 10 (13%) |
| Internal Medicine Intensive Care Unit | 5 (6.7%) |
| Chest Disease Unit | 4 (5.3%) |
| Infectious Disease Unit | 4 (5.3%) |
| Dermatology Unit | 4 (5.3%) |
| Burn Unit | 3 (4%) |
| Pediatric Oncology Unit | 2 (2.7%) |
| Pediatric Haematology Unit | 2 (2.7%) |
| Pediatric İnfectious Disease Unit | 2 (2.7%) |
| Pediatric 2 Unit | 2 (2.7%) |
| Nephrology Unit | 2 (2.7%) |
| Urology Unit | 2 (2.7%) |
| Neurology Intensive Care Unit | 2 (2.7%) |
| Endocrinology Unit | 2 (2.7%) |
| Plastic and Reconstructive Surgery Unit | 2 (2.7%) |
| Haematology Unit | 2 (2.7%) |
| Neonatal Intensive Care Unit | 1 (1.3%) |
| Pedatric Allergy and Immunology Unit | 1 (1.3%) |
| Neurosurgery Unit | 1 (1.3%) |
| Ortopedics and Traumatology Unit | 1 (1.3%) |
| Gynecology and obstetrics unit | 1 (1.3%) |
| General Surgery Unit | 1 (1.3%) |
| Pediatric İnfectious Disease Unit 2 | 1 (1.3%) |
| Oncology Unit | 1 (1.3%) |
| Ophtalmology Unit | 1 (1.3%) |
| Pediatric Gastroenterology Unit | 1 (1.3%) |
| Pediatric Surgery Unit | 1 (1.3%) |
| Neurology Unit | 1 (1.3%) |
| Urology Unit 2 | 1 (1.3%) |
| Neurosurgery Unit | 1 (1.3%) |
| Pediatrics Cardiovascular surgery Unit | 1 (1.3%) |
| Total | 75 |
The identification and antibiotic sensitivity tests of the strains were performed on the Vitek 2 automated system for oxacillin, gentamicin, ciprofloxacin, erythromycin, clindamycin, linezolid, teicoplanin, vancomycin, imipenem, tetracycline, tigecycline, fosfomycin, fusidic acid, rifampicin and trimethoprim/sulfamethoxazole. Confirmation of 75 isolates with methicillin resistance was confirmed by the Kirby-Bauer disc diffusion method for cefoxitin. Breakpoints were applied according to the 2016 European Committee on Antimicrobial Susceptibility Testing (EUCAST) guidelines [10].
The SmaI-PFGE was performed as described in a previous study [11]. The band profiles were analyzed using GelCompar II software (version 4.0; Applied Maths, Sint-Martens-Latem, Belgium).
Deoxyribonucleic acid (DNA) was extracted from isolates by mechanical lysis using a Mickle tissue disintegrator (Mickle Laboratory Engineering Co. Ltd.). Polymerase chain reaction (PCR) was applied to DNA extracts using the spa-1113f (5’TAA AGA CGA TCC TTC GGT GAG C3’) and spa-1514r (5’CAG CAG TAG TGC CGT TTG CTT3’) primers [12]. The PCR products were purified using SentroPure® DNA purification kit (Sentromer DNA Technologies LLC, Istanbul, Turkey) according to the kit protocol. Then, cycle sequencing was undertaken using BigDye® Terminator v3.1 cycle sequencing kit (Applied Biosystems, CA, USA). The products were purified with ZR DNA Sequencing Clean-up Kit™ (Zymo Research, CA, USA) as recommended in the protocol. The DNA sequence analysis of the spa gene region was performed using ABI Prism 310 DNA sequencer (Applied Biosystems, CA, USA).
The raw data was processed with Sequencing Analysis Software version 5.1, and the spa types were identified by Ridom StaphType TM (Ridom GmbH, Würzburg, Germany) software. Using the BURP algorithm in the software, spa types were grouped based on six or less repeat differences.
Results
In this study, we determined antibiotic resistance of 75 MRSA isolates by the Vitek 2 automated system routinely used in the laboratory (Table 3).
Table 3.
Antibiotic resistance of MRSA isolates
| Antibiotics | CIP | DA | E | FOS | FA | CN | LZD | MOX | RA | TEI | TE | TIG | SXT | VA |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Resistant strains number | 39 | 43 | 46 | 26 | 5 | 36 | – | 32 | 39 | – | 47 | – | 13 | – |
| % | 52 | 57.3 | 61.3 | 34.6 | 6.7 | 48 | 0 | 42.7 | 52 | 0 | 62.6 | 0 | 17.3 | 0 |
CIP Ciprofloxacin, DA Clindamycin, E Erythromycin, Fusidic acid, FOS Fosfomycin, CN Gentamycin, IPM Imipenem, OX Oxacillin, LZD Linezolid, RA Rifampin, TEI Teicoplanin TE Tetracycline, TIG Tigecycline, SXT Trimethoprim-sulfametaxazole, VA Vancomycin
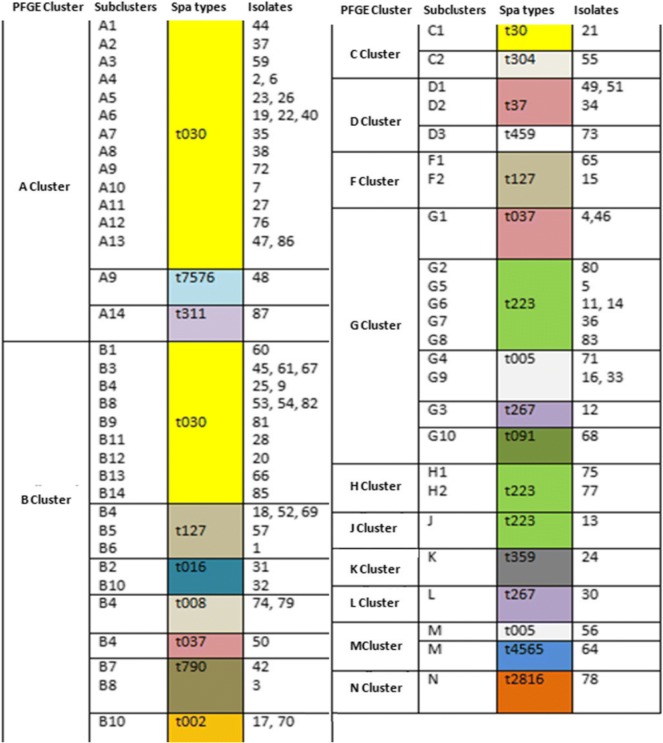
All of the isolates were evaluated with PFGE and spa typing to reveal their epidemiology in our region. When the similarity cut-off value was taken as 85%, 75 isolates were divided into 11 main clusters by the PFGE method. The largest cluster was cluster B with 27 members, followed by cluster A with 19 members. Clusters J, K, L and N had a single isolate. Clusters A and B constituted 61.3% of all isolates with a similarity of 84.1% according to PFGE.
The most common spa type was t30 with 31 isolates (41.3%), followed by t223 with nine isolates (12%) and t127 (9.3%) with seven isolates. Eight of the isolates were singletons (Table 4).
Table 4.
Distribution of test isolates by their spa types according to samples and spa types
| Spa types | PFGE types | Outpatients | Inpatients | Samples Number (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| TA | Wound | Blood | Urine | TA | Wound | Blood | Urine | |||
| t030 | A | – | – | – | – | 11 | 3 | 5 | 1 | 31 (41.3%) |
| B | – | – | – | 1 | 8 | 1 | – | – | ||
| C | – | – | – | 1 | ||||||
| t223 | G | – | – | – | – | 1 | 3 | 1 | 1 | 9 (12%) |
| H | – | – | – | – | – | – | 2 | – | ||
| J | – | – | – | – | 1 | – | – | – | ||
| t127 | B | – | 2 | – | – | 3 | – | – | – | 7 (9.3%) |
| F | – | – | – | – | 2 | – | – | – | ||
| t037 | B | – | – | – | – | – | 1 | – | – | 6 (8%) |
| D | – | – | – | – | – | 1 | 2 | – | ||
| G | – | – | – | – | – | 1 | 1 | – | ||
| t005 | G | – | 2 | – | – | – | 1 | – | – | 4 (5. 3%) |
| M | – | 1 | – | – | – | – | – | – | ||
| t002 | B | – | 1 | – | – | – | 1 | – | – | 2 (2.7%) |
| t267 | G | – | 1 | – | – | – | – | – | – | 2 (2.7%) |
| N | – | – | – | – | – | 1 | – | – | ||
| t008 | B | – | – | – | – | – | 2 | – | – | 2 (2.7%) |
| t016 | B | – | – | – | – | – | 2 | – | – | 2 (2.7%) |
| t790 | B | – | – | – | – | 1 | 1 | – | – | 2 (2.7%) |
| t304 | C | – | 1 | – | – | – | – | – | – | 1 (1.3%) |
| t459 | D | – | – | – | – | 1 | – | – | – | 1 (1.3%) |
| t359 | K | – | – | – | – | – | 1 | – | – | 1 (1.3%) |
| t311 | A | – | – | – | – | – | 1 | – | – | 1 (1.3%) |
| t091 | G | – | 1 | – | – | – | – | – | – | 1 (1.3%) |
| t7576 | A | – | – | – | – | 1 | – | – | – | 1 (1.3%) |
| t2816 | N | 1 | – | – | – | – | – | – | 1 (1.3%) | |
| t4565 | M | – | – | – | – | – | 1 | – | – | 1 (1.3%) |
| Total | 11 | 64 | 75 (100%) | |||||||
TA Tracheal aspirate
All the t030 isolates were in clusters A and B, except for one isolate in cluster C. Clusters A and B contained nine more spa types. The strains in cluster G, the third largest cluster, were distributed among five different spa types.t223 was the second most prevalent spa type and was distributed among clusters G, H and J, showing 80.1% similarity in SmaI-PFGE. The third common spa type, t127, was included in cluster B (Table 5).
Table 5.
Comparison of S.aureus strains with PFGE and spa typing
The spa types were divided into five clusters by the BURP analysis. Cluster 1 [Clonal Complex 005 (CC005)] consisted of t790, t223, t4565, t2816 and t016 originating from t005. Cluster 2 (CC459) contained t37, t30 and t7576 originating from t459 (Fig. 1).
Fig. 1.
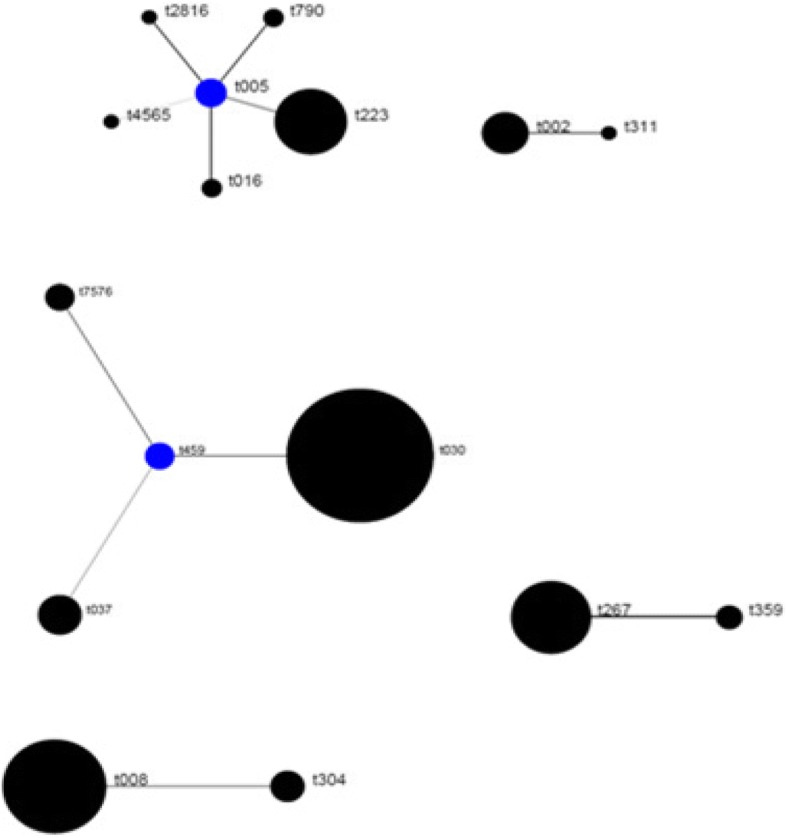
Distribution of spa clonal complexes (BURP analysis)
Discussion
Although many MRSA genotypes and clonal clusters have been identified in different biogeographic regions, it has been generally determined that certain gene clones are predominant. In the United States, community-associated ST8-spa t008 (USA300) and ST5-spa t002 clones are predominant, while ST22-spa t032, mostly associated with hospital, is more commonly seen [6, 13–15]. In France and Belgium, however, it is reported that the ST8-spa t008 clone, defined as the community origin similar to the USA, is widespread [14, 15]. In Bulgaria and the Balkan countries, such as Romania and Turkey, ST239-spa t030 is the predominant spa type [14]. It has been shown in studies conducted in Asia and Far East countries that ST239-spa t030, ST239-spa t037 and ST5-spa t002 are the most common types [16–18].
In the current study, 75 MRSA clinical isolates were examined. Twenty-eight isolates (37.3% of all isolates) were collected from intensive care units where MRSA infections were most prevalent [19]. Clonal relationship of MRSA strains were determined by pulsed-field gel electrophoresis (PFGE) and Staphylococcal protein A (spa) typing methods. In many studies similar to our study, MLST method was used together with spa typing and PFGE methods. However, MLST studies of these isolates has to be postpone due to funding reasons.
The isolates were distributed among 11 clusters with PFGE and 18 clusters with spa typing. Spa typing revealed that 31 isolates (41.3%) belonged to type t030. The other spa types detected were t223 (12%) with nine isolates, t127 (9.3%) with seven isolates, t037 (8%) with six isolates, and t005 (5.3%) with four isolates. This finding indicates that type t030 has high prevalence (41.3%) in Turkey, as in Asian and Balkan countries [14, 17].
t030 isolates were collected in clusters A and B, which were 80% similar to each other according to the PFGE band profiling. The second most frequent spa type, t223, was found in clusters G, H and J, which were 80.1% similar as revealed by PFGE. The third spa type, t127, was included in cluster B. Rare or sporadic spa types showed a heterogeneous distribution with PFGE. In a Finnish study, 90% of the most common spa types, t172 and t067, were clustered in FIN-4 and FIN-16 PFGE patterns, respectively. Similar to our study, rare spa types were associated with more than one PFGE cluster [20].
The ST239 clone containing spa t030 was first found to be widely distributed in a large number of patients in Brazil; therefore, this clone was called the Brazilian clone. Later spreading to the neighboring South American countries, such as Argentina, Chile, Uruguay, and European countries, including Portugal, Czech Republic, and Greece, the ST239 clone is now epidemically seen in most Asian countries [17, 21].
In a study conducted in China, it was reported that the predominant clone from 1994 to 2000 was ST239-spa t037 with 92.6% prevalence, but after 2000, this clone rapidly decreased and replaced by ST239-spa t030. In this study, spa types t30 and t37 were located in unrelated clusters by PFGE [17].
In Turkey, the first spa t030 isolates were identified from nine blood cultures in 2003–2004. Then, in a study conducted with 54 strains isolated from invasive infections (92% blood cultures) in eight university hospitals between 2005 and 2006, 89% of the strains were identified as spa t030. The rate of spa t030 in the current study was below the values given in these two studies. We consider that this difference may be due to the variances in the samples.
In another study, 48 MRSA isolates were divided into 14 PFGE clusters and the spa type of all isolates except two was spa t030 which collected in 3 months. As noted in the study, because the samples reflected a period of 3 months, genetic diversity may be limited [22–24].
However, our study, which shows that some community-based isolates are beginning to be seen in hospitals at increasing frequency, will be a guide for future studies.
In a 2008–2009 study conducted in 12 cities in Turkey, the most common PFGE pattern was found to be Pulsotype A (91.4%) and the most common spa type was t030 (85.1%) among the 397 MRSA isolates collected. This clone was called ‘TR09’. However, in the same study, it was determined that among the 91 isolates obtained in 2011, the rate of t30 decreased to 70.3% and the number of new sporadic types increased. The reduction in the rate of spa t030 in this study supported our work. This study showed that the most common community-associated MRSA clone was ST737-spa t005, which was named “TR10” [25]. We also found the prevalence of the t005 type as 5.3%. In addition, we also detected t790, t4565, t2816, and the second most common spa type t223 in our study, clustered in the same clonal complex with t005 by BURP analysis.
In our study, we identified t127 as the third most commonly defined spa type, which had not been previously defined in Turkey. Methicillin-sensitive and resistant t127 clones have been isolated from humans, food and animals in various studies and are considered community-associated [26–28].
Conclusion
In conclusion, among the MRSA strains, spa t030 was predominant in our region, as previously reported for other regions in Turkey. The most common spa types were closely clustered in PFGE. In the current study, spa t127, which is common among community-acquired isolates, was identified for the first time in Turkey. Therefore, it is considered that MRSA surveillance is absolutely required to constantly monitor clones across the world. Furthermore, it is beneficial to use the spa typing method and PFGE in the research of clonal relations to follow the changing clones that are prevalent in Turkey.
Acknowledgments
Funding
This study was financially supported by Cukurova University Scientific Research Projects (TF2012LTP40/TSA-2016-5577), Adana, Turkey.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- MRSA
Methicillin-Resistant Staphylococus aureus
- PFGE
Pulsed-Field Gel Electrophoresis
- spa
Staphylococcal protein A
Authors’ contributions
YK collected samples, cultured the isolates, and performed DNA extraction. YK and TGG performed the statistical analyses. FK and AY designed the study. FK and AY supervised the practical work and data management. YK, TGG and FK wrote the manuscript. All authors approved the final version of the manuscript.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Tülin Güven Gökmen, Email: yldzozdmr@hotmail.com.
Yıldız Kalayci, Phone: +90 5056139049, Email: tulinguven01@hotmail.com.
Akgün Yaman, Email: ayaman@cu.edu.tr.
Fatih Köksal, Email: fkoksal@cu.edu.tr.
References
- 1.Lowy FD. Staphylococus aureus infections. N Engl J Med. 1998;339:520–532. doi: 10.1056/NEJM199808203390806. [DOI] [PubMed] [Google Scholar]
- 2.Deurenberg RH, Vink C, Kalenic S, Friedrich AW, Bruggeman CA, Stobberingh EE. The molecular evolution of methicillin resistant Staphylococcus aureus. Clin Microbiol Infect. 2007;13:222–235. doi: 10.1111/j.1469-0691.2006.01573.x. [DOI] [PubMed] [Google Scholar]
- 3.Cookson BD, Robinson DA, Monk AB, Murchan S, Deplano A, de Ryck R, Struelens MJ, Scheel C, Fussing V, Salmenlinna S, Vuopio-Varkila J, Cuny C, Witte W, Tassios PT, Legakis NJ, van Leeuwen W, van Belkum A, Vindel A, Garaizar J, Haeggman S, Olsson-Liljequist B, Ransjo U, Muller-Premru M, Hryniewicz W, Rossney A, O’Connell B, Short BD, Thomas J, O’Hanlon S, Enright MC. Evaluation of molecular typing methods in characterizing a European collection of epidemic methicillin-resistant Staphylococcus aureus strains: the HARMONY collection. J Clin Microbiol. 2007;45:1830–1837. doi: 10.1128/JCM.02402-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chung M, De Lencastre H, Matthews P, Tomasz A, Adamsson I, De Sousa MA, Camou T, Cocuzza C, Corso A, Couto I, Dominguez A, Gniadkowski M, Goering R, Gomes A, Kikuchi K, Marchese A, Mato R, Melter O, Oliveira D, Palacio R, Sa-Leao R, Sanches IS, Song JH, Tassios PT, Villari P. Molecular typing of methicillin-resistant Staphylococcus aureus by pulsed-field gel electrophoresis: comparison of results obtained in a multilaboratory effort using identical protocols and MRSA strains. Microb Drug Resist. 2000;6:189–198. doi: 10.1089/mdr.2000.6.189. [DOI] [PubMed] [Google Scholar]
- 5.Murchan S, Kaufmann ME, Deplano A, de Ryck R, Struelens M, Zinn CE, Fussing V, Salmenlinna S, Vuopio-Varkila J, El Solh N, Cuny C, WitteW TPT, Legakis N, Van Leeuwen W, Van Belkum A, Vindel A, Laconcha I, Garaizar J, Haeggman S, Olsson-Liljequist N, Ransjo U, Coombes G, Cookson B. Harmonization of pulsed-field gel electro-phoresis protocols for epidemiological typing of strains of methicillin-resistant Staphylococcus aureus: a single approach developed by consensus in 10 European laboratories and its application for tracing the spread of related strains. J Clin Microbiol. 2003;41:1574–1585. doi: 10.1128/JCM.41.4.1574-1585.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stefani S, Chung DR, Lindsay JA, Friedrich AW, Kearns AM, Westh H, Mackenzie FM. Meticillin-resistant Staphylococcus aureus (MRSA): global epidemiology and harmonisation of typing methods. Int J Antimicrob Agents. 2012;39:273–282. doi: 10.1016/j.ijantimicag.2011.09.030. [DOI] [PubMed] [Google Scholar]
- 7.Enright MC, Day NP, Davies CE, Peacock SJ, Spratt BG. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus. J Clin Microbiol. 2000;38:1008–1015. doi: 10.1128/jcm.38.3.1008-1015.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shopsin B, Gomez M, Montgomery SO, Smith DH, Waddington M, Dodge DE, Bost DA, Riehman M, Naidich S, Kreiswirth BN. Evaluation of protein a gene polymorphic region DNA sequencing for typing of Staphylococcus aureus strains. J Clin Microbiol. 1999;37:3556–3563. doi: 10.1128/jcm.37.11.3556-3563.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Strommenger B, Kettlitz K, Weniger T, Harmsen D, Friedrich AW, Witte W. Assignment of Staphylococcus isolates to groups by spa typing, SmaI macrorestriction analysis, and multilocus sequence typing. J Clin Microbiol. 2006;44(7):2533–2540. doi: 10.1128/JCM.00420-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.EUAST: European Committee on antimicrobial susceptibility testing guide August 2016: 2016. Clinical breakpoint (http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/QC/v_8.0_EUCAST_QC_tables_routine_and_extended_QC.pdf). Accessed 12 May 2016.
- 11.Mulvey MR, Chui L, Ismail J, Louie L, Murphy C, Chang N, Alfa M. Development of a Canadian standardized protocol for subtyping methicillin-resistant Staphylococcus aureus using pulsed-field gel electrophoresis. J Clin Microbiol. 2001;39:3481–3485. doi: 10.1128/JCM.39.10.3481-3485.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harmsen D, Claus H, Witte W, Rothgänger J, Claus H, Turnwald D, Vogel U. Typing of methicillin-resistant Staphylococcus aureus in a university hospital setting by using novel software for spa repeat determination and database management. J Clin Microbiol. 2003;41:5442–5448. doi: 10.1128/JCM.41.12.5442-5448.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Otter JA, French GL. Community-associated meticillin-resistant Staphylococcus aureus strains as a cause of healthcare associated infection. J Hosp Infect. 2011;79(3):189–193. doi: 10.1016/j.jhin.2011.04.028. [DOI] [PubMed] [Google Scholar]
- 14.Grundmann H, Aanensen DM, van den Wijngaard CC, Spratt BG, Harmsen D, Friedrich AW. Geopraphic distribution of Staphylococcus aureus causing invasive infection in Europe: a molecular-epidemiological analysis. PLoS Med. 2010;7(1):e1000215. doi: 10.1371/journal.pmed.1000215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson AP. Methicillin-resistant Staphylococcus aureus: the European landscape. J Antimicrob Chemother. 2011;66(4):43–48. doi: 10.1093/jac/dkr076. [DOI] [PubMed] [Google Scholar]
- 16.Song JH, Hsueh PR, Chung DR, Ko KS, Cl K, Peck KR, Yeom JS, Kim SW, Chang HH, Kim YS, Jung SI, Son JS, So TM, Lalitha MK, Yang Y, Huang SG, Wang H, Lu Q, Carlos CC, Perera JA, Chiu CH, Liu JW, Chongthaleong A, Thamlikitkul V, Van PH. Spread of methicillin-resistant Staphylococcus aureus between the community and the hospitals in Asian countries: an ANSORP study. J Antimicrob Chemother. 2011;66:1061–1069. doi: 10.1093/jac/dkr024. [DOI] [PubMed] [Google Scholar]
- 17.Chen H, Liu Y, Jiang X, Chen M, Wang H. Rapid change of methicillin-resistant Staphylococcus aureus clones in a Chinese tertiary care hospital over a 15-year period. Antimicrob Agents Chemother. 2010;54(5):1842–1847. doi: 10.1128/AAC.01563-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ho CM, Ho MW, Lee CY, Tien N, Lu JJ. Clonal spreading of methicillin-resistant SCCmec Staphylococcus aureus with specific spa and dru types in Central Taiwan. Eur J Clin Microbiol Infect Dis. 2012;31(4):499–504. doi: 10.1007/s10096-011-1338-3. [DOI] [PubMed] [Google Scholar]
- 19.Dulon M, Haamann F, Peters C, Schablon A, Nienhaus A. MRSA prevalence in European healthcare settings: a review. BMC Infect Dis. 2011;11:138. doi: 10.1186/1471-2334-11-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vainio A, Koskela S, Virolainen A, Vuopio J, Salmenlinna S. Adapting typing for national laboratory-based surveillance of methicillin-resistant. Eur J Clin Microbiol Infect Dis. 2011;30(6):789–797. doi: 10.1007/s10096-011-1158-5. [DOI] [PubMed] [Google Scholar]
- 21.Teixeira LA, Resende CA, Ormonde LR, Rosenbaum R, Figueiredo AM, De Lencastre H, Tomasz A. Geographic spread of epidemic multiresistant Staphylococcus aureus clone in Brazil. J Clin Microbiol. 1995;33:2400–2404. doi: 10.1128/jcm.33.9.2400-2404.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ergon MC, Biçmen M, Gülay Z. Dokuz Eylül Üniversitesi Hastanesindeki dominant metisiline dirençli Staphylococcus aureus suşunun moleküler yöntemlerle tiplendirilmesi. ANKEM Derg. 2010;24(2):65–70. [Google Scholar]
- 23.Alp E, Klaassen CHW, Doğanay M, Altoparlak Ü, Aydin K, Engin A, Kuzucu Ç, Özakin C, Özinel MA, Turhan Ö, Voss A. MRSA genotypes in Turkey: persistence over 10 years of a single clone of ST239. J Inf Secur. 2009;58:433–438. doi: 10.1016/j.jinf.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 24.Yılmaz ŞK, Acuner İÇ, Strommenger B, Bek Y, Witte W. Türkiye’nin Orta Karadeniz bölgesinde metisiline dirençli Staphylococcus aureus kökenlerinin enfeksiyözite-rezistotip-genotip kümelenmesi. Mikrobiyol Bül. 2014;48(1):14–27. [PubMed] [Google Scholar]
- 25.Bozdoğan B, Yıldız Ö, Oryaşın E, Kırdar S, Gülcü B, Aktepe O, Arslan U, Bayramoğlu G, Çoban AY, Coşkuner SA, Güdücüoğlu H, Karabiber N, Öncü S, Tatman M, Özkütük N, Özyurt M, Şener AG. t030 is the most common spa type among methicillin-resistant Staphylococcus aureus strains isolated from Turkish hospital. Mikrobiyol Bul. 2013;47(4):571–581. doi: 10.5578/mb.5770. [DOI] [PubMed] [Google Scholar]
- 26.Fetscha A, Contzenb M, Harteltc K, Kleiserd A, Maassene S, Raub J, Kraushaara B, Layerg F, Strommenger B. Staphylococcus aureus food-poisoning outbreak associated with the consumption of ice-cream. Int J Food Microbiol. 2014;187:1–6. doi: 10.1016/j.ijfoodmicro.2014.06.017. [DOI] [PubMed] [Google Scholar]
- 27.Otter JA, French GL. The emergence of community-associated methicillin-resistant Staphylococcus aureus at a London teaching hospital, 2000–2006. Clin Microbiol Infect. 2008;14:670–676. doi: 10.1111/j.1469-0691.2008.02017.x. [DOI] [PubMed] [Google Scholar]
- 28.Franco A, Hasman H, Iurescia M, Lorenzetti R, Stegger M, Pantosti A, Feltrin F, Ianzano A, Porrero MC, Liapi M, Battisti A. Molecular characterization of spa type t127, sequence type 1 methicillin-resistant Staphylococcus aureus from pigs. J Antimicrob Chemother. 2011;66(6):1231–1235. doi: 10.1093/jac/dkr115. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.