Abstract
Context:
Since autism spectrum disorder (ASD) is a lifelong disease and because of its nature, the negative effects of the disease on the quality of life (QoL) of caregivers as well as patients are incontrovertible.
Aims:
It was aimed to evaluate the effect of the variables related to both parents and children on the QoL scores of the parents of the children with ASD.
Settings and Design:
This is a causality analysis study.
Subjects and Methods:
Questionnaire on sociodemographic/disease-related variables, QoL in Autism Questionnaire-Parent Version (QoLA-P), autism behavior checklist and Clinical Global Impression scale were assessed of 162 patients with ASD.
Statistical Analysis Used:
Unpaired t- test, Mann–Whitney U test, Kruskal–Wallis test, and one-way ANOVA test were used for comparing groups. The parameters found to be statistically significant for QoLA-P in different analyses were included as the independent variable in the logistic regression analysis. The backward (variable elimination) model was selected as the model in the analysis.
Results:
The causality has been established may be stated as the severity of autism, the presence of psychiatric disorder in the mother/father, attendance of the child at school, duration since the diagnosis of autism, and the child's medication use.
Conclusions:
Autism affects the QoL of caregivers. The intervention of treatment by considering the factors that affect the QoL positively or negatively may increase the QoL of caregivers.
Key words: Autism, caregivers, child, logistic regression, parenting, quality of life
INTRODUCTION
Neurodevelopmental disorders are developmental deficiencies that emerge during the developmental process, most frequently during the preschool period, and characterized by impairment in personal, social, academic, and occupational functionality. Autism spectrum disorder (ASD) falls into the category of neurodevelopmental disorders according to The Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5) diagnostic classification system and is described as a disease characterized by a chronic impairment in social communication and social interaction.[1] Although the severity is not the same in all patients with ASD, the clinical manifestation is characterized by impairments and deviations in social-emotional functionality, verbal, and nonverbal communication skills as well as limited-restricted interests and behaviors in general.[2] According to the World Health Organization (WHO), quality of life (QoL) is defined as “the individual's perception of their position in life in the context of the culture and value systems in which they live.”[3,4] Health-related QoL is a broad concept which includes many factors that are directly or indirectly related to health. Health-related QoL refers to the impact of health status on the individual's ability to function and the individual's perception of physical, mental, and social domains of life. According to the WHO, health is a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity. Almost all descriptions of the health-related QoL include these components.[5] Nowadays, as for the treatment, it is not only eliminating a disease but also the improvement of the individual's QoL. For this reason, measurability of well-being and QoL has become important. Since ASD is a lifelong disease and because of its nature, the negative effects of the disease on the QoL of caregivers as well as patients are incontrovertible. The QoL of patients with ASD as well as their caregivers is negatively affected. In their study published in 2007, Mugno et al. assessed the QoL of family members of children with ASD, cerebral palsy, and mental retardation and found that the QoL scores of the parents in the ASD group were significantly lower than the healthy group in many fields.[6] Furthermore, in some studies, it was demonstrated that parents, especially mothers, of children with ASD had a higher rate of depression and anxiety symptoms compared to healthy control groups and to families of children with Down syndrome.[7,8]
In this study, it was aimed to evaluate the effect of the variables related to both parents and children on the QoL scores of the parents of the children with ASD.
SUBJECTS AND METHODS
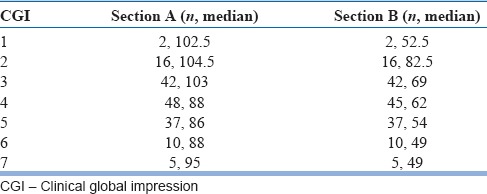
The study was in accordance with the Declaration of Helsinki for human subjects and has been approved by the Local Ethics Committee. The medical charts of 162 patients with ASD who admitted to the child and adolescent psychiatry outpatient clinic and had been included in the Turkish validity and reliability of QoL in Autism Questionnaire-Parent Version (QoLA-P) study.[9] were retrospectively reviewed. The diagnoses of the patients were made according to the DSM-IV-TR. The Section A and B scores in QoLA-P were used as the dependent variable to determine the factors affecting the QoL in autism. The parameters found to be statistically significant for Section A and/or B in different analyses were included as the independent variable in the logistic regression analysis. In the approach that we used to categorize the dependent variable in logistic regression analysis dichotomously, the disease severity assessment variable (Clinical Global Impression [CGI] scale) was categorized, and the cutoff values for Sections A and B were set as 103 and 82 points, respectively, as shown in Table 1.
Table 1.
Median scores of the quality of life in autism questionnaire-parent version according to the Clinical Global Impression-Severity
Data collection tools
The QoLA-P results of the participants were used to assess the QoL in autism objectively. The questionnaire on sociodemographic/disease-related variables was assessed to determine the independent variables, and the results of the Autism Behavior Checklist (ABC) and CGI scale were assessed for determining the severity of the disorder.
Questionnaire on sociodemographic/disease-related variables
A questionnaire containing the sociodemographic characteristics of the children with ASD and their families were used in the study. In addition, the query items included a five-point Likert-type question to query the time allocated by their mothers and fathers to the care of the children. The disease-related variables included the duration of diagnosis, the attendance at special education programs, the attendance at school, medication use, comorbid diseases, and the type of diagnosis.
The Quality of Life in Autism Questionnaire-Parent version
Developed by Eapen et al., this questionnaire consists of two subscales (Sections A and B).[10] Section A contains 28 questions in total that measure how parents perceive their own QoL. Section B assesses the perception of parents related to the extent to which the autism-specific difficulties encountered by their children constitute a problem for the parents. The score that can be obtained from the entire scale ranges from 48 to 240. However, it is recommended that each section is scored and used separately. The Turkish validity and reliability of the questionnaire were performed by Gürbüz Özgür et al.[9]
Autism behavior checklist
The ABC is a 57-item assessment tool which was developed by Krug et al. for assessment and screening of autism.[11] The scale consists of five subscales: sensory behavior, social relating, body and object use, language and communication skills, and social and adaptive skills. The Turkish validity and reliability of the scale were performed by Irmak et al.[12]
Clinical Global Impression scale
The CGI scale is a brief scale that allows the clinician to assess the overall functionality of the patient.[13] It contains a “severity” section that rates the severity of psychopathology on a scale from 1 to 7, and an “improvement” section that rates the change from the initiation of the treatment, also using a 7-point scale. In this study, the CGI-severity section was used to determine the disease severity.
Statistical analysis
The data of the participants were evaluated using the SPSS 17.0 software package for Windows (SPSS Inc., Chicago, IL, US). The descriptive data were expressed as a minimum, maximum, mean, median, standard deviation, number, and percentage. Conformance of the data to a normal distribution was evaluated using the Shapiro–Wilk test. For intergroup comparisons, the t-test was used as the parametric test for independent groups; and the Mann–Whitney U-test was used as the nonparametric test. For comparisons of more than two groups, the one-way ANOVA test was used as the parametric test, and the Kruskal–Wallis test was used as the nonparametric test. In cases that statistical significance was found in the one-way ANOVA test, the post hoc Tukey test was used to identify the group that caused the difference. A logistic regression analysis was performed using various variables to determine causality separately for the A and B indices of the QoLA-P. The backward (variable elimination) model was selected as the model in the analysis. P < 0.05 were considered statistically significant.
RESULTS
The results of descriptive analysis
Of the 162 participants in total, those who did not answer more than three questions for each section while completing the QoLA-P were excluded from the study. As a result, the numbers of participants eligible for the analysis were 160 and 157 for the Section A and B, respectively. The mean age of the mothers was 34.2 ± 6.7 years, and the mean age of the fathers was 38.5 ± 7.3 years. Nearly 10.5% of the mothers and 3.7% of the fathers had psychiatric disorders. 6.2% (n = 10) of the families had another dependent individual with a chronic disease at home. 77.2% (n = 125) of all participants included in the study were attending special education programs. The mean duration of attendance at special education programs was 2.5 ± 3.1 years. Nearly 64.2% (n = 104) of the participants were attending school. When the comorbid diseases except for mental retardation were considered, it was seen that 36.4% (n = 59) of the participants had at least one, 1.9% (n = 3) had at least two, and 0.6% (n = 1) had at least three comorbidities. The most common comorbidity was attention deficit hyperactivity disorder (ADHD) (21% [n = 34]). Nearly 10.5% (n = 17) of the participants had epilepsy and 5.6% (n = 9) had asthma. When they were evaluated according to their medication use, it was observed that 52.5% (n = 85) were receiving medications and 47.5% (n = 77) were not receiving any medication.
When the times allocated to the care of the children by the mothers were grouped, no statistically significant difference was found for the scores of Section A and B separately (P = 0.47, P = 0.84, Kruskal–Wallis test). However, it was found that the QoL scores of the mother improved for both sections with increasing time allocation by the father to the care of the child (P = 0.001 for the Section A, and P = 0.01 for the Section B, Kruskal–Wallis test) [Figure 1].
Figure 1.
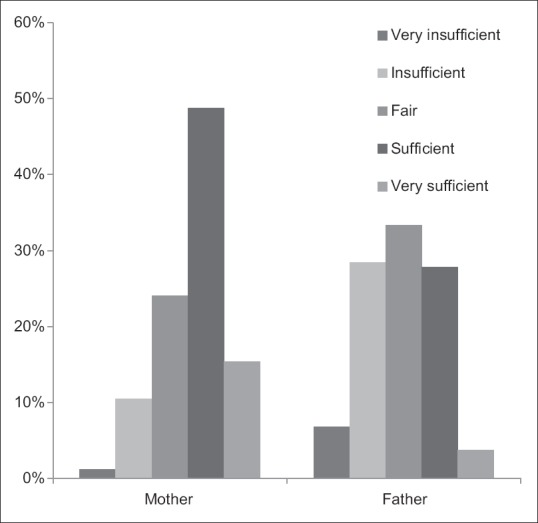
Perception of mothers for the time allocated to the care of children by mothers and fathers
The results of causality analysis
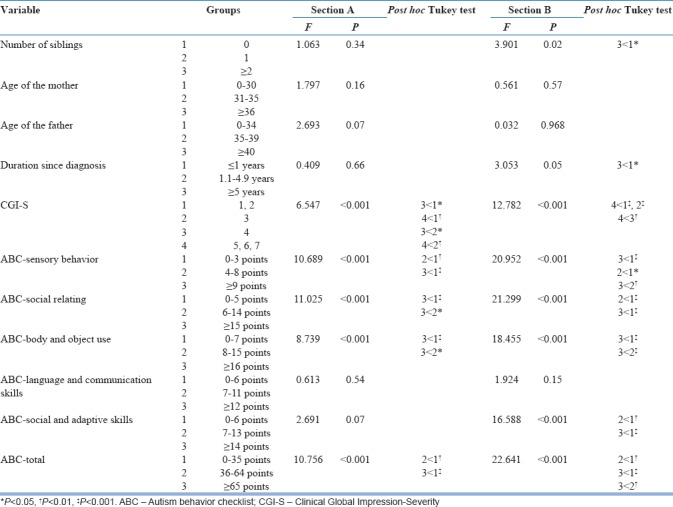
For the Section A, the QoL scores were low in cases of low educational level of the father (P = 0.007), presence of a psychiatric disorder in the mother/father (P = 0.04), low level of income (P < 0.001), nonattendance of the child at school (P = 0.02), unemployment of the mother (P = 0.02), and alcohol use of the father (P = 0.006) [Tables 2 and 3]. In the Section B, low educational level of the father (P = 0.05), diagnosis of the child with autistic disorder (P < 0.001), nonattendance of the child at school (P = 0.001), low level of income of the family (P = 0.01), medication use of the child (P = 0.05), alcohol use of the father (P = 0.002), having more than two siblings compared to being the only child (P = 0.02) and a longer than 5 years duration of autism diagnosis (P = 0.05) were associated with worsening QoL scores [Tables 2–4]. High disease severity was associated with low QoL scores for both the Sections A and B [Table 4].
Table 2.
Comparison of the quality of life in autism questionnaire-parent version Section A and Section B scores according to the variables in independent groups using the t-test
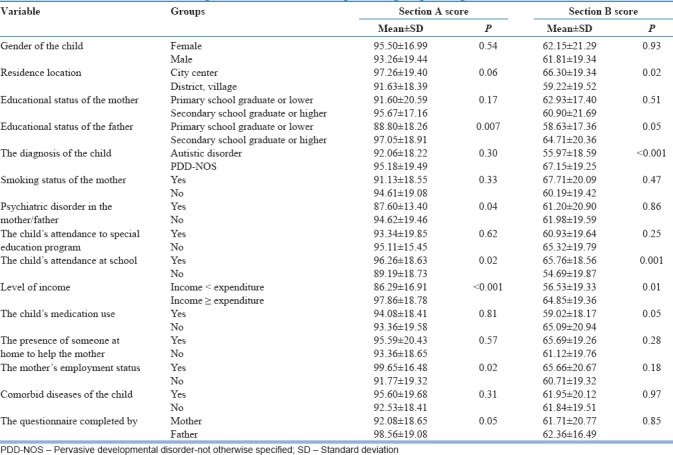
Table 3.
Comparison of the quality of life in autism questionnaire-parent version Section A and Section B scores according to the variables in independent groups using the Mann-Whitney U-test
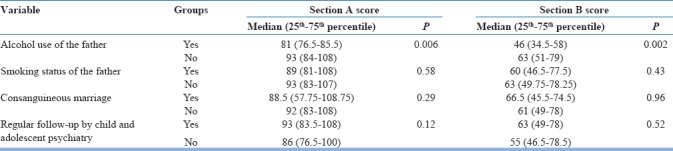
Table 4.
Comparison of the quality of life in autism questionnaire-parent version Section A and Section B scores according to the variables in independent groups using the one-way ANOVA test
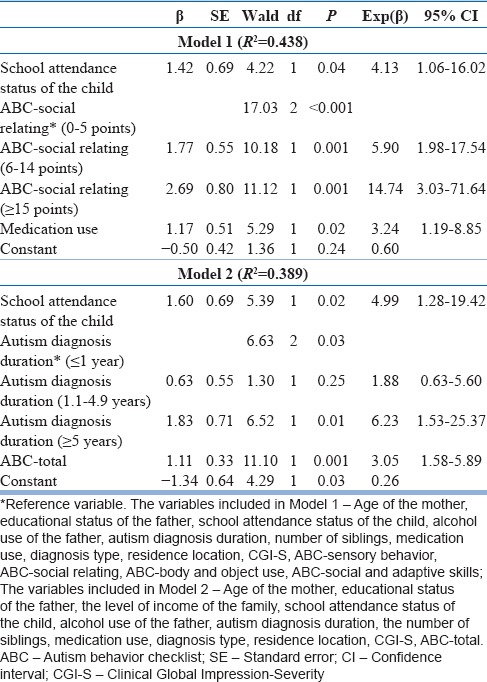
The results obtained by causality analysis using logistic regression analysis for the above-mentioned statistically significant variables for the Section A and Section B are presented in Tables 5 and 6. The sensory behavior subdimension of the ABC was included in the first model applied for the Section A. According to the results obtained, a one-unit increase in the score of the participants with 4–8 points in the ABC sensory behavior dimension increases the chances of obtaining a high score from the QoLA-P Section A by 3.20 times compared to the participants with 0–3 points; for the participants with ≥9 points, an increase of 5.97 times was observed [Table 5]. When a logistic regression model was created by categorizing the ABC-total scores for the Section A, it was seen that the QoL scores worsen with increasing ABC scores [Table 5]. On the other hand, for the Section B, it was seen that the QoL scores worsen with increasing ABC-social relating scores in the Model 1, and it was also seen that nonattendance of the child at school and medication use of the child increases the chances of worse scores from the questionnaire by 4.13 times and 3.24 times, respectively [Table 6]. When the ABC total score was included in the model and when the variables that were found to be associated with the Section B scores at the reduced final step were considered, nonattendance of the child at school, a longer than 5 years' duration of autism diagnosis, and the ABC-total score increased the chances of worse scores from the questionnaire by 4.99 times, 6.23 times, and 3.05 times, respectively [Table 6].
Table 5.
Reduced final models of logistic regression for the quality of life in autism questionnaire-parent version Section A
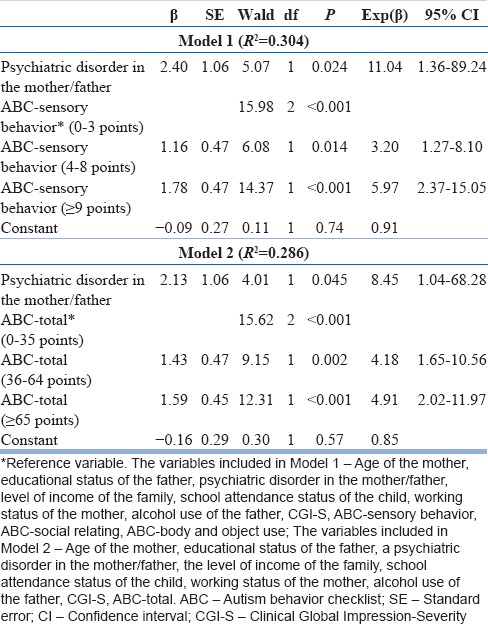
Table 6.
Reduced final models of logistic regression for the quality of life in autism questionnaire-parent version Section B
DISCUSSION
In this study, the QoL and the factors affecting the QoL of caregivers of children diagnosed with ASD were investigated. The QoL of the caregiver and the family is negatively affected related to the characteristics of the disorder. Lower state of well-being, more depressive symptoms, and higher anxiety levels were reported in the mothers of children diagnosed with highly functioning ASD when compared to the mothers of normally developing children.[14] A review article on the marital quality of families having children with developmental disorders including ASD reported that the divorce rates are higher for the families of children with ASD, and more depression, anxiety, and other mental health problems are seen in the parents.[15] Moreover, it was suggested that the marital quality of the parents affects the development and well-being of the child.[16] Mothers had a higher number of important support needs that are unmet than fathers, and the educational status of the parents, the age of the child with ASD, accompanying behavioral disorders, the presence of mental retardation, and the level of income are associated with the support needs of the mothers.[17]
ASD may be accompanied by various comorbidities.[18] ADHD is one of the most common comorbidities of ASD. In our sample, ADHD was found to be the most common comorbidity of ASD; 21% of the participants were diagnosed with ADHD. Since the modification in DSM-5 now allows a diagnosis of ADHD comorbid with ASD, it appears that the frequency of ADHD comorbid with ASD will increase in the new studies. The second most common comorbidity was epilepsy. In the literature, the prevalence of epilepsy in Turkish children is reported to be 0.8%.[19] Moreover, studies show that the frequency of epilepsy is higher in ASD than in the normal population.[20] The fact that 10.5% of our participants were diagnosed with epilepsy appears to be consistent with the literature. The third most common comorbidity was asthma with 5.6% of our participants. There is evidence suggesting that allergic diseases worsen the behavioral problems and ASD symptoms in children with ASD.[21]
Medications are commonly used for behavioral disorders associated with or comorbidities seen with ASD. In the study conducted by Dogan et al.,[22] it was reported that 56.3% of the children with ASD in their clinical sample were receiving psychotropic medications, and treatment was prescribed most commonly for hyperactivity. In another study, Gurkan et al.[23] found that the rate of medication use in children with ASD was 44% when antiepileptic medication use was considered in addition to the psychotropic medication use. Consistent with the literature, we found that 52.5% of our participants were receiving medications. The QoL scores were significantly worse in the group that was receiving medications. The possible cause of this finding may be that the frequency of comorbidities and the severity of ASD were higher in the group that was receiving medications.
In our study, it was found that the QoLA-P Section A and B scores of the mother decreased with decreasing time allocation by the father to the care of the child. In other words, the QoL of the mother worsens with decreasing time allocation by the father to the care of the child. In the literature, a study on the relationship of fathers with their children with ASD, the parenting stress scores of the fathers decrease with increasing frequency of playing games with their children with ASD.[24] In the light of this information, it may be suggested that increasing the role of the father in giving care to the child with ASD will have a direct positive effect on the QoL of the father as well as indirectly improving the QoL of the mother.
In the literature, a study that evaluated the effects of having a child with autism on the family functions found that both the mother and father have more psychopathology and less mutual agreement in their relationship compared to the parents having normally developing children. It was found that mothers of children with ASD show less marital satisfaction, endearment, family harmony, and cohesion compared to those having normally developing children. Moreover, it was stated that the mothers in this group showed more psychopathology and experienced more marital conflict compared to the fathers.[25] In our study, we found that, in the presence of a psychiatric diagnosis in the mother and/or father (21%), QoL is significantly negatively affected. This may possibly be caused by the increased burden and responsibility on the caregiving parent, and the decreased moral support from the parent with the psychiatric disorder.
In our study, the educational status of the mothers did not significantly affect their QoL scores. However, the low educational status of the father was associated with low scores in both the Section A and Section B. Schlebusch et al.[26] reported a positive correlation between the QoL and the educational status of the parents in families having a child with ASD. When we looked at the other studies conducted on the parental educational status and QoL, a study that investigated the factors affecting the QoL of the mothers of children with cerebral palsy using the SF-36 reported that lack of education of the mother together with cerebral palsy accompanied by mental retardation negatively affect the QoL of the mother.[27]
Tekinarslan[28] assessed the QoL and depression levels of the mothers of children with ASD, Down syndrome and cerebral palsy using the Beck Depression Scale and The WHOQOL-BREF scale; they found no difference between the groups regarding the depression levels of the mothers. However, the authors reported that while the QoL score (the WHOQOL-BREF environmental domain) of mothers of children with cerebral palsy was significantly lower than the Down syndrome group, the mothers of children with ASD obtained high scores using the WHOQOL-BREF social relationships domain.[28] Gürbüz Özgür et al.[9] reported a positive correlation among all dimensions of the WHOQOL-BREF and the Section A scores of the QoLA-P scale. Tekinarslan[28] found that the depression scores increased and the QoL scores worsened with increasing age of the mother and that there was a positive correlation with the educational status and the level of income. In our study, the age of the mother and the QoL scores were not correlated while there was a significant correlation with the level of income in both sections of the questionnaire. Higher QoL scores observed in working mothers is one of the important results of this study. The facts that the working mother shares the burden and responsibility contribute to the income of the family, and has a different occupation other than caring for the child may be the factors improving her QoL. A study conducted in South Africa reported that there is no association between the employment status of the mother and the QoL of the family in families having a child with ASD.[26]
When the participants with ASD were evaluated with respect to their attendance at educational institutions, it was seen that 64.2% were attending daycare, preschool, or organized educational institutions. Moreover, 77.2% were attending special education programs. The QoLA-P Section A and B scores of the parents of the children attending preschool or organized educational institutions were higher compared to the parents of the children who do not attend school. In other words, the QoL of the parents having children with ASD who attend school is better than those whose children do not attend school. This may possibly be caused by the better functionality of the children who attend school, the mother being able to set aside time for herself when the child is outside the home, and attendance at school increases the likelihood to benefit from support systems such as education and healthcare and provides a positive contribution to the child in developing his/her independence skills.
A statistical relationship was observed between the scores in the subsections assessed with the ABC and the QoL scores of the parents. The QoL scores of the parents worsened with increasing sensory behavior, body and object use, and social relating scores of the ABC and the total ABC scores. These results led us to conclude that the QoL of the parents of children who have more problems in certain domains is more negatively affected. In general, a statistically significant relationship was found between the disease severity assessed either by the CGI scale or the ABC scale and the QoL scores of the parents. This is consistent with the studies in the literature.[26,29,30,31] There are some limitations of the study. Since there are no cutoff values in the literature for this QoL scale, a receiver operating characteristic (ROC) analysis was performed to determine the cutoff point; however, no breakpoint could be obtained. In addition, since the sample consisted only of children diagnosed with autism, the disease severity with score leaps was used instead of performing a ROC.
CONCLUSIONS
In the light of the information obtained in this study, several factors that positively or negatively affect the QoL of the caregivers of patients with autism were determined. Among these factors, those for which the causality has been established may be stated as the severity of autism, the presence of psychiatric disorders in the mother/father, attendance of the child at school, duration since the diagnosis of autism, and the child's medication use. Conduction of further studies to evaluate other parameters that may affect causality may allow a more holistic approach to the issue by identifying different factors affecting the QoL of the caregivers in ASD.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.DSM-5 Task Force. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. Washington, D.C.: American Psychiatric Association; 2013. American Psychiatric Association; p. xliv.p. 947. [Google Scholar]
- 2.Volkmar FR, Lord C, Klin A, Schultz R, Cook E. Autism and the pervasive developmental disorders. In: Martin A, Volkmar FR, editors. Lewis's Child and Adolescent Psychiatry: A Comprehensive Textbook. 3rd ed. Philadelphia, PA, US: LWW; 2002. [Google Scholar]
- 3.What quality of life? The WHOQOL group. World Health Organization quality of life assessment. World Health Forum. 1996;17:354–6. [PubMed] [Google Scholar]
- 4.The WHOQOL Group. The development of the World Health Organization quality of life assessment instrument (the WHOQOL) In: Orley J, Kuyken W, editors. Quality of Life Assessment: International Perspectives. Heidelberg: Springer Verlag; 1994. pp. 41–57. [Google Scholar]
- 5.Testa MA, Simonson DC. Assessment of quality-of-life outcomes. N Engl J Med. 1996;334:835–40. doi: 10.1056/NEJM199603283341306. [DOI] [PubMed] [Google Scholar]
- 6.Mugno D, Ruta L, D'Arrigo VG, Mazzone L. Impairment of quality of life in parents of children and adolescents with pervasive developmental disorder. Health Qual Life Outcomes. 2007;5:22. doi: 10.1186/1477-7525-5-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cantwell DP, Baker L, Rutter M. Families of autistic and dysphasic children. I. Family life and interaction patterns. Arch Gen Psychiatry. 1979;36:682–7. doi: 10.1001/archpsyc.1979.01780060072008. [DOI] [PubMed] [Google Scholar]
- 8.McAdoo W, DeMyer M. Personality characteristics of parents. In: Rutter M, Schopler E, editors. Autism: A Reappraisal of Concepts and Treatment. New York: Plenum Press; 1978. pp. 251–67. [Google Scholar]
- 9.Gürbüz Özgür B, Aksu H, Eser E. Turkish validity and reliability of quality of life in autism questionnaire-parent version. Anadolu Psikiyatri Derg. 2017;18:344–52. [Google Scholar]
- 10.Eapen V, Crnčec R, Walter A, Tay KP. Conceptualisation and development of a quality of life measure for parents of children with autism spectrum disorder. Autism Res Treat 2014. 2014:160783. doi: 10.1155/2014/160783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krug D, Arick J, Almond P. Autism Screening İnstrument for Educational Planning. Austin, TX: PRO-ED; 1980. [Google Scholar]
- 12.Irmak T, Sütçü S, Aydın A, Sorias O. An Investigation of Validity And Reliabilty of Autism Behavior Checklist (ABC) Turk J Child Adolesc Ment Health. 2007;14:13–23. [Google Scholar]
- 13.Guy W. ECDEU Assessment Manual for Psychopharmacology. Rockville, MD: U.S. Department of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs; 1976. National Institute of Mental Health (U.S.) Psychopharmacology Research Branch, Early Clinical Drug Evaluation Program; p. 603. [Google Scholar]
- 14.Lee GK. Parents of children with high functioning autism: How well do they cope and adjust? J Dev Phys Disabil. 2009;21:93–114. [Google Scholar]
- 15.Hartley SL, Seltzer MM, Barker ET, Greenberg JS. Marital quality and families of children with developmental disabilities. Int Rev Res Dev Disabil. 2011;41:1–29. doi: 10.1016/B978-0-12-386495-6.00001-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cummings EM, Davies PT, Campbell SB. Developmental Psychopathology and Family Process: Theory, Research, and Clinical İmplications. New York: Guilford Press; 2000. [Google Scholar]
- 17.Hartley SL, Schultz HM. Support needs of fathers and mothers of children and adolescents with autism spectrum disorder. J Autism Dev Disord. 2015;45:1636–48. doi: 10.1007/s10803-014-2318-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Medical Comorbidities in Autism Spectrum Disorders. Treating Autism Publications; 2013. Treating Autism, Autism Treatment Trust. [Google Scholar]
- 19.Serdaroğlu A, Ozkan S, Aydin K, Gücüyener K, Tezcan S, Aycan S, et al. Prevalence of epilepsy in Turkish children between the ages of 0 and 16 years. J Child Neurol. 2004;19:271–4. doi: 10.1177/088307380401900406. [DOI] [PubMed] [Google Scholar]
- 20.Mouridsen SE, Rich B, Isager T. A longitudinal study of epilepsy and other central nervous system diseases in individuals with and without a history of infantile autism. Brain Dev. 2011;33:361–6. doi: 10.1016/j.braindev.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 21.Jyonouchi H. Autism spectrum disorders and allergy: Observation from a pediatric allergy/immunology clinic. Expert Rev Clin Immunol. 2010;6:397–411. doi: 10.1586/eci.10.18. [DOI] [PubMed] [Google Scholar]
- 22.Dogan BS, Cak HT, Cengel Kultur SE. The frequency of psychotropic medication use, distribution and associated variables ın children diagnosed with autistic spectrum disorder. Turk J Child Adolesc Ment Health. 2014;21:105–14. [Google Scholar]
- 23.Gurkan K, Soykan Aysev A, Akcakin M. Pharmacological management of pervasive developmental disorders. Bull Clin Psychopharmacol. 2005;15:53–9. [Google Scholar]
- 24.Bloom J. Fathers' Physical Play with their Children with Autism: Benefits for Fathers. Ontario: Windwor; 2015. [Google Scholar]
- 25.Gau SS, Chou MC, Chiang HL, Lee JC, Wong CC, Chou WJ, et al. Parental adjustment, marital relationship, and family function in families of children with autism. Res Autism Spectr Disord. 2012;6:263–70. [Google Scholar]
- 26.Schlebusch L, Dada S, Samuels AE. Family quality of life of south african families raising children with autism spectrum disorder. J Autism Dev Disord. 2017;47:1966–77. doi: 10.1007/s10803-017-3102-8. [DOI] [PubMed] [Google Scholar]
- 27.Ahmadizadeh Z, Rassafianib M, Khalilia MA, Mirmohammadkhani M. Factors associated with quality of life in mothers of children with cerebral palsy in Iran. Hong Kong J Occup Ther. 2015;25:15–22. [Google Scholar]
- 28.Tekinarslan IC. A comparison study of depression and quality of life in turkish mothers of children with down syndrome, cerebral palsy, and autism spectrum disorder. Psychol Rep. 2013;112:266–87. doi: 10.2466/21.02.15.PR0.112.1.266-287. [DOI] [PubMed] [Google Scholar]
- 29.Soltanifar A, Akbarzadeh F, Moharreri F, Soltanifar A, Ebrahimi A, Mokhber N, et al. Comparison of parental stress among mothers and fathers of children with autistic spectrum disorder in İran. Iran J Nurs Midwifery Res. 2015;20:93–8. [PMC free article] [PubMed] [Google Scholar]
- 30.Baker BL, Blacher J, Crnic KA, Edelbrock C. Behavior problems and parenting stress in families of three-year-old children with and without developmental delays. Am J Ment Retard. 2002;107:433–44. doi: 10.1352/0895-8017(2002)107<0433:BPAPSI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 31.Lecavalier L, Leone S, Wiltz J. The impact of behaviour problems on caregiver stress in young people with autism spectrum disorders. J Intellect Disabil Res. 2006;50:172–83. doi: 10.1111/j.1365-2788.2005.00732.x. [DOI] [PubMed] [Google Scholar]


