Abstract
The use of respiratory protection, an important component of personal protective equipment (PPE) in healthcare, is dependent on the hazard and environmental conditions in the workplace. This requires the employer and healthcare worker (HCW) to be knowledgeable about potential exposures and their respective protective measures. However, the use of respirators is inconsistent in healthcare settings, potentially putting HCWs at risk for illness or injury. To better understand respirator use, barriers, and influences, the National Institute for Occupational Safety and Health (NIOSH) Health and Safety Practices Survey of Healthcare Workers provided an opportunity to examine self-reported use of respirators and surgical masks for targeted hazards. The hazards of interest included aerosolized medications, antineoplastic drugs, chemical sterilants, high-level disinfectants, influenza-like illness (ILI), and surgical smoke. Of the 10,383 HCWs who reported respiratory protection behaviors, 1,904 (18%) reported wearing a respirator for at least one hazard. Hazard type, job duties, site characteristics, and organizational factors played a greater role in the likelihood of respirator use than individual factors. The proportion of respirator users was highest for aerosolized medications and lowest for chemical sterilants. Most respondents reported using a surgical mask for at least one of the hazards, with highest use for surgical smoke generated by electrosurgical techniques and ILI. The high proportion of respirator non-users who used surgical masks is concerning because HCWs may be using a surgical mask in situations that require a respirator, specifically for surgical smoke. Improved guidance on hazard recognition, risk evaluation, and appropriate respirator selection could potentially help HCWs better understand how to protect themselves at work.
Keywords: Healthcare worker safety, hospital chemical hazards, personal protective equipment (PPE), respirators and surgical masks, respiratory protection
Introduction
Health and safety precautions are essential to prevent exposures when working with or around health hazards—a daily occurrence in U.S. healthcare settings. Workplace safety is important as healthcare workers (HCWs) experience one of the highest numbers of nonfatal occupational injuries and illnesses compared to other service industries.[1] To prevent occupational exposures, the hierarchy of controls specify that unless the hazard can be eliminated or substituted with a less toxic substance, exposure controls should be systematically implemented in the following decreasing order of efficacy: engineering controls, administrative controls, work practice controls, and personal protective equipment (PPE).[2] PPE, such as gowns, gloves, and respirators, are often used in combination with other controls as a last defense to prevent potential highly toxic exposures. However, PPE use has been found to be inconsistent in health-care settings and is affected by factors such as guidelines, employer policies, availability, user adherence, and safety culture.[3–6]
Respirators are a specific type of PPE used to protect the wearer from inhaling harmful particulates, aerosols, and other airborne hazards.[7] The Occupational Safety and Health Administration (OSHA) provides respiratory protection standards, regulations, and guidance for respiratory protection programs including recommendations for hazard recognition, risk evaluation, and appropriate respirator selection and use.[8] Many studies, however, have found that a hurdle to correct respirator use in practice is understanding how to select the appropriate type of protection necessary for a given exposure.[4,6] This problem may be exacerbated in the healthcare industry, which has nearly five times the number of respirator-using employees than any other private sector service industry.[9] Respirator use can depend on an individual’s perceived likelihood of exposure, knowledge of risk, and awareness of appropriate respirator type.[3] Inconsistent use of respirators may also be influenced by a lack of awareness of the types of protection provided by surgical masks vs. respirators.[10] Surgical masks provide barrier protection against large-particle droplets, splashes, sprays, or splatter, but do not effectively filter small particles and are not considered respiratory protection.[11,12] Without adequate knowledge of respiratory protection, employers, supervisors, and HCWs may not be equipped to make evaluations correctly and may choose insufficient protection.[13]
Previously reported findings from the National Institute for Occupational Safety and Health (NIOSH) Health and Safety Practices Survey of Healthcare Workers found that PPE best practices are not always used.[14–16] Specifically, Silver and colleagues found predictive factors for PPE use with antineoplastic drugs to be familiarity with guidelines, training in safe handling practices, and perceived availability.[17] Safety climate plays a role in influencing adherence, which may vary in interpretation by the type of HCW, the HCW’s responsibilities at work, and the influence of management.[18,19] There is considerable interaction between individual behaviors, environmental factors, and organizational characteristics affecting PPE adherence prompting the need to better understand these influences to improve workplace health and safety.
Recognizing the unique PPE challenges faced in healthcare, the Institute of Medicine recommended the exploration of respirator designs specific to HCW needs.[20] Manufacturers, policy makers, and research initiatives are gathering data about respirator users to help design the next generation of respirators.[21,22] However, data on respirator use and users in health-care are limited. Investigating trends in respirator use when HCWs are potentially exposed to specific airborne hazards can help explain the nuances of HCW respiratory practices so that training and recommendations can address identified deficiencies. An analysis of the respirator data for specific hazards of interest from the NIOSH Health and Safety Practices Survey of Healthcare Workers allows further exploration of the use of respirators and surgical masks among HCWs. The primary objective of this cross-sectional analysis is to better understand respirator use for each of the targeted hazards and to describe barriers and influences to using respirators in the health-care setting.
Methods
Survey methodology
The NIOSH Health and Safety Practices Survey of Healthcare Workers, an anonymous, multi-module, web-based survey was conducted in 2011. The study population included members of 21 professional practice organizations representing HCWs who routinely use or come in to contact with selected chemical agents. Major occupational groups represented by these organizations included nurses, pharmacy practitioners, technologists/technicians, anesthesiologists and other anesthesia care providers, respiratory therapists, and dentists and other dental practitioners. Information on the methods used in the development and testing of the survey instrument, implementation, respondent characteristics, strengths, and limitations have been previously reported.[23]
Survey instrument
The survey included a screening module, core module, and seven hazard-specific modules. The screening module determined if respondents were eligible to complete the survey based on whether they had used or been in contact with any of the targeted chemical hazards in the 7 days prior to the survey, with the exception of the aerosolized medication pentamidine for which use or contact was up to 30 days prior to the survey. Those with potential exposures were eligible for the survey.
The core module collected information on respondent demographics, occupation, employer characteristics, and other topics relevant to HCWs. The core module also provided questions about potential exposure to seasonal influenza or patients with influenza-like illness (ILI) symptoms in the year prior to the survey and corresponding respiratory protection practices. This study examines respiratory protection practices for ten potential respiratory hazard scenarios based on data from six of the seven hazard modules:
compounding antineoplastic drugs;
administering antineoplastic drugs;
administering aerosolized ribavirin;
administering aerosolized antibiotics (tobramycin, amikacin, colistin);
administering aerosolized pentamidine;
handling chemical sterilants (ethylene oxide, hydrogen peroxide gas plasma);
handling high-level disinfectants (glutaraldehyde, orthophthaldehyde, peracetic acid, hydrogen peroxide);
proximity to surgical smoke generated by laser techniques;
proximity to surgical smoke generated by electrosurgical techniques; and
exposure to seasonal influenza or patients with ILI.
Photos depicting different types of respirators and surgical masks were used to minimize response error.
Data analysis
For each hazard that included questions on the use of respiratory protection, respondents were asked: Did you wear any of the following while working with [aforementioned hazard]? Response options were:
N95 respirator (including surgical N95 respirator)
Powered air-purifying respirator (PAPR) with particulate filter(s)
Half-facepiece air-purifying respirator with particulate filter(s)
Full-facepiece air-purifying respirator with particu-late filter(s)
Standard surgical mask (including laser mask for surgical smoke exposure)
I did not wear any respirators or masks
Other
I don’t know
Respondents were able to select as many responses as were applicable to their work. For this study, respondents were classified as respirator users if they wore an N95 respirator, PAPR, or half- or full-face-piece respirator for at least one of the hazards and respirator non-users if they only used surgical masks or responded I did not wear any respirators or masks. Less than 1% of the overall responses were other or I don’t know and were excluded from the classification as a respirator user or non-user. The highest level of protection was recorded if multiple answers were reported. For example, if a participant selected surgical mask and N95 respirator, they were classified as a respirator user. As participants were recruited only if they had contact with the chemical hazard of interest recently (7 days for most hazards), those who reported respirator use would likely be considered frequent users and were of most interest to this analysis. Those who reported they did not always use respirators, excluding exposure to ILI, were asked a follow-up question to ascertain why respiratory protection was not always used.
Perceived safety climate questions relating to PPE use were also considered in this analysis to capture organizational factors that may play a role in respirator use. Respondents were asked about safety training in the past 12 months related to each specific hazard, influenza vaccination status, and if they had experienced a work-related injury, illness, or exposure. Safety climate statements related to PPE use and training included the following: proper PPE is available, have received adequate training from employer to recognize health and safety hazards, usually have enough time to take safety precautions, and feel the organization has a positive safety culture. Responses using a Likert scale were dichotomized into yes (agree or strongly agree) or no (disagree or strongly disagree) categories. Respondents were also asked to report their level of stress at work (none, moderate, or a lot).
If participants completed more than one module, they were counted as one respondent but all responses were recorded. The number of respondents varied for each hazard and not all eligible participants answered all of the questions provided. Descriptive statistics with percentages are presented and only responses related to the question of interest were included for analysis. Bivariate comparisons using Pearson’s chi-squared test compared whether differences in the observed distribution between the respirator users and non-users were due to chance, a p-value of ≤0.01 was considered significant. Statistical analysis was conducted using SAS version 9.3 (Cary, NC).
The NIOSH Institutional Review Board (IRB) determined that the activities of this project constituted surveillance and did not meet the criteria of research according to 45 CFR 46.110(b)(2) and the Centers for Disease Control and Prevention (CDC) Guidelines for Defining Public Health Research and Public Health Non-Research. Although not required by the IRB, elements of a traditional informed consent document were included in the invitation letter, which included a hyperlink to the survey, and informed consent was implied in the anonymous web survey.
Results
A total of 10,383 HCWs reported their hazard-specific respiratory protection behaviors; 1,904 (18%) respondents were classified as respirator users and the remaining 8,479 were classified as non-users. The highest percentage of respirator users were nurses (52%), therapists (22%), physicians (10%), and technologists/technicians (10%) (Table 1). When detailed occupations were reported, the highest percentage of respirator users were: respiratory therapist (22%), nurse anesthetist (13%), and physician anesthesiologist (10%). Noteworthy was that nursing specialties (anesthetist, oncology, hematology/oncology, and gastroenterology/endoscopy) represented four of the top six occupational categories for respirator users. Respiratory therapists, who often deal with aerosolized medications, had the greatest difference in proportion of respirator users (22%) vs. non-users (4%) compared to the other occupations.
Table 1.
Distribution of characteristics that differed significantly in respirator users vs. non-users.
| Respirator users | Respirator non-users | |||||
|---|---|---|---|---|---|---|
| Characteristic | nA = 1904 | % | nA = 8479 | % | p-value | |
| Sex | Female | 1246 | 67.2 | 6096 | 74.2 | <0.01 |
| Male | 609 | 32.8 | 2116 | 25.8 | ||
| Facility type | Hospital | 1543 | 82.5 | 5599 | 67.3 | <0.01 |
| Ambulatory setting | 272 | 14.5 | 2514 | 30.2 | ||
| Residential/social care | 56 | 3.0 | 202 | 2.4 | ||
| Major occupational | Nurse | 969 | 51.5 | 4746 | 57.0 | <0.01 |
| group | Therapist | 419 | 22.3 | 306 | 3.7 | |
| Physician | 190 | 10.1 | 909 | 10.9 | ||
| Technologist/technician | 188 | 10.0 | 1194 | 14.3 | ||
| Dentist/dental practitioner | 53 | 2.8 | 816 | 9.8 | ||
| Pharmacist/pharmacy practitioner | 25 | 1.3 | 134 | 1.6 | ||
| Detailed occupation+ | Respiratory therapist | 418 | 22.3 | 303 | 3.6 | <0.01 |
| Nurse anesthetist | 239 | 12.7 | 1458 | 17.5 | ||
| Physician anesthesiologist | 186 | 9.9 | 905 | 10.9 | ||
| Oncology nurse | 155 | 8.3 | 671 | 8.0 | ||
| Hematology/oncology nurse | 131 | 7.0 | 510 | 6.1 | ||
| Gastroenterology/endoscopy nurse | 116 | 6.2 | 481 | 5.8 | ||
| Time spent in direct | 76–100% | 1213 | 64.6 | 5901 | 71.0 | <0.01 |
| patient care | 51–75% | 285 | 15.2 | 1053 | 12.7 | |
| 26–50% | 157 | 8.4 | 465 | 5.6 | ||
| 1–25% | 177 | 9.4 | 526 | 6.3 | ||
| 0 | 46 | 2.5 | 363 | 4.37 | ||
| Urban vs. rural work | Large city (≥50,000 people) | 1191 | 63.6 | 4693 | 56.6 | <0.01 |
| setting | Small city (<50,000 people) | 357 | 19.0 | 1781 | 21.5 | |
| Suburbs/rural | 326 | 17.4 | 1818 | 21.9 | ||
| Size of employer | >1000 workers | 819 | 43.8 | 2593 | 31.3 | <0.01 |
| 100–1000 workers | 652 | 34.8 | 2713 | 32.8 | ||
| 1–99 workers | 401 | 21.4 | 2979 | 36.0 | ||
The denominator for each percentage is the column total (i.e., group total of users or non-users) that answered each question minus any non-responses.
Number of respondents varied for individual items (i.e., those who elected not to answer).
Occupations that represented more than 5% of overall responses.
Respirator users were more likely to work in settings with more than 1,000 employees and in cities with 50,000 or more people (Table 1). The distribution of respirator users significantly (p < 0.01) differed from non-users for: sex, facility type, major occupational group, detailed occupation, time spent in direct patient care, urban vs. rural, and number of employees at site. Respirator users did not differ from non-users on age, job experience, or education.
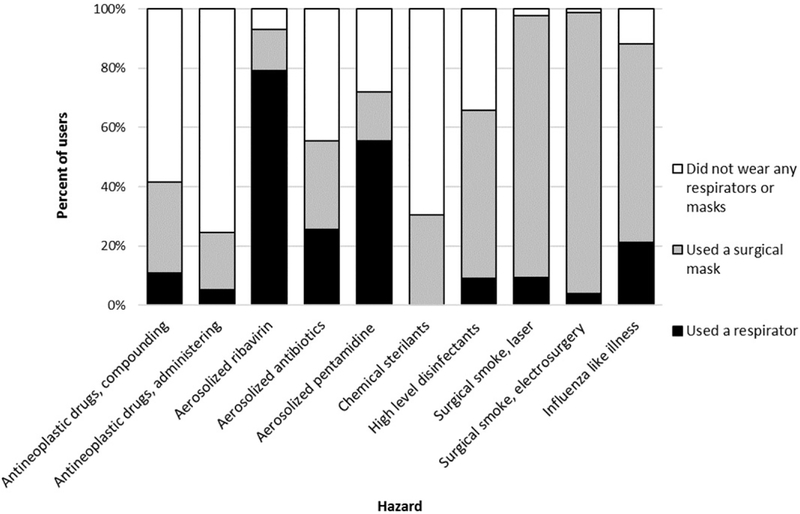
Use of an N95 respirator was reported the most often (93%) of the respirator types; very few respondents indicated the use of half- or full-facepiece respirators (3%) or PAPRs (4%). In Figure 1, the proportion of respirator users is compared to two sub-categories of respirator non-users: surgical mask users and those who reported they did not wear either a mask or a respirator, both of which constitute no respiratory protection. The proportion of respirator users was highest for aerosolized medications, including ribavirin (79%), pentamidine (56%), and antibiotics (26%), and lowest for chemical sterilants (0%). Those exposed to patients with ILI symptoms also had a relatively high proportion of respirator users (21%). All other hazard types had a low proportion of respirator users, less than 11%. If participants used a respirator, they were asked if they had been fit tested for the respirator they used, only 440 of the 1,767 respondents who answered the question reported that they had been fit tested for the respirator they used. Most respondents reported using a surgical mask (78%) for at least one of the hazards, ranging from 14–95% across the different hazards, with highest use for surgical smoke generated by electrosurgical techniques (95%) and ILI (73%).
Figure 1.
Healthcare worker use of respirators and surgical masks by hazard.
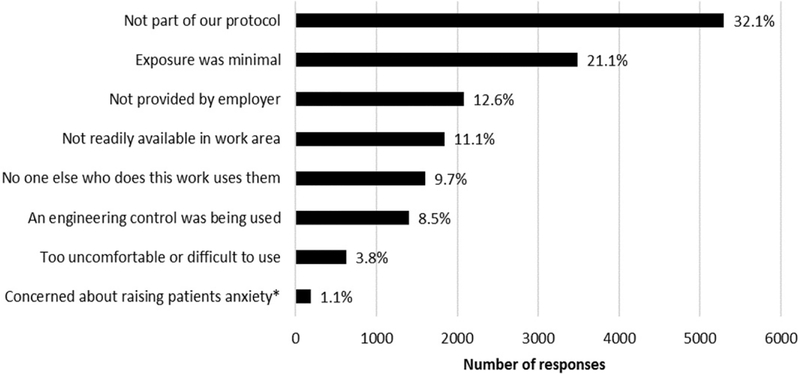
Respondents who did not use a respirator when potentially exposed to the hazards of interest were asked why they did not use a respirator (Figure 2). Multiple responses were permitted therefore associated counts represent the total number of responses (n = 16,522). The two most common responses were not part of our protocol (n = 5,289) and exposure was minimal (n = 3,483), followed by not provided by employer (n = 2,079), not readily available in work area (n = 1,840), no one else who does this work uses them (n = 1,606), and an engineering control was being used (n = 1,398). The two least common responses were too uncomfortable or difficult to use (n = 629) and concerned about raising patient’s anxiety (n = 189). The response concerned about raising patient’s anxiety was only asked about hazards where direct patient care was involved (e.g., aerosolized medications, antineoplastic drugs, and surgical smoke).
Figure 2.
Reasons for not always wearing a respirator while working with targeted hazards. Percentage denominator is the total number of responses as multiple answers were permitted. * Response provided only if direct patient care was involved.
Responses to perceived safety climate questions relating to PPE use are shown in Table 2. There were significant (p < 0.01) differences in distribution of characteristics between respirator users and non-users for respirators users having received an influenza vaccination, trained in the past 12 months, having adequate training, and PPE availability. There was not a significant difference between respirator users and non-users for experiencing a work-related injury or illness in the past year, having enough time to take safety precautions, having a positive safety culture, or having stress in the workplace.
Table 2.
Participant responses to perceived safety climate questions comparing respirator users and respirator non-users.
| Respirator users | Respirator non-users | |||||
|---|---|---|---|---|---|---|
| Question | Response^ | nA = 1904 | % | nA = 8479 | % | p-value |
| Have you received a seasonal influenza vaccine in the last 12 months? |
Yes | 1541 | 84.4 | 6198 | 77.1 | <0.01 |
| When was the last time you received training on procedures for the safe handling of [the hazard]? |
In past 12 months | 929 | 48.8 | 3335 | 39.3 | <0.01 |
| In the past 12 months, have you experienced a work-related injury, illness, or exposure? |
Yes | 263 | 14.2 | 1109 | 13.6 | 0.49 |
| I usually have enough time to take safety precautions while completing my duties. |
Yes | 1554 | 86.7 | 6881 | 87.1 | 0.62 |
| Proper personal protective equipment is available to me. |
Yes | 1684 | 94.5 | 7284 | 92.5 | <0.01 |
| I have received adequate training from my current employer to recognize health and safety hazards in my job. |
Yes | 1588 | 89.3 | 6642 | 85.0 | <0.01 |
| I feel my organization has a positive safety culture. |
Yes | 1579 | 88.5 | 6828 | 86.7 | 0.04 |
| How much stress would you say you experienced | None | 182 | 10.0 | 913 | 11.3 | 0.06 |
| at work in past 7 calendar days? | Moderate | 1123 | 61.5 | 5031 | 62.4 | |
| A lot | 521 | 28.6 | 2114 | 26.2 | ||
The denominator for each percentage is the column total (i.e., group total of users or non-users) that answered each question minus any non-responses.
Responses using a Likert scale were dichotomized into yes (agree or strongly agree) or no (disagree or strongly disagree) categories.
Number of respondents varied for individual items (i.e., those that elected not to answer).
Discussion
The goal of this study was to explore respirator use for prominent chemical hazards in healthcare settings and to describe influences and barriers to using respiratory protection. Comparing respiratory protection practices across several hazards of interest, reasons why respiratory protection was not used, and factors that vary between respirator users and non-users allows for a better understanding of prevailing occupational safety practices in healthcare. This analysis builds upon previously published analyses of the NIOSH Health and Safety Practices Survey of Healthcare Workers by analyzing behaviors across all hazards to capture respiratory-specific safety practices.
It is important to consider in this cross-sectional analysis that the hazards in the survey have different respiratory recommendations and guidelines. The type of hazard, employer policies, and guidelines would be the appropriate drivers in determining whether respirator use is warranted, including when environmental action levels are exceeded.[23] For example, a respirator is recommended during compounding or administering antineoplastic drugs when splashes, aerosols, or vaporization are likely—unlike aerosolized antibiotics, which have not been classified by NIOSH as hazardous drugs.[24] During administration as an aerosol, ribavirin, and pentamidine require at least an N95 respirator but only when appropriate engineering controls are not in place.[25,26] Engineering controls are often employed for chemical sterilants and high-level disinfectants, but if ineffective, a respirator would be recommended.[27] Current recommendations for surgical smoke include the removal of the smoke at the source using portable smoke evacuators or wall suction systems, but in the absence of these engineering controls, respiratory protection is recommended.[28,29] For ILI, a surgical mask is recommended for seasonal influenza, and a respirator is recommended for high-risk procedures or potentially pandemic strains.[7]
Each hazard had a different proportion of respirator users, surgical mask users, and neither mask nor respirator users. N95 respirators were the most commonly reported respirator type with only 175 responses across all the hazards indicating the use of PAPRs or half- or full-facepiece respirators, with these results being similar to those from another national survey.[30] Respirator use was highest among those who administered pentamidine and ribavirin, which are hazards with well-defined recommendations, followed by antibiotics, which lack authoritative safe handling guidelines and the perceived need for respiratory protection. Respirator use was lowest for chemical sterilants—a finding not unexpected as these chemicals are often used in enclosed processes with engineering controls, where the potential for worker exposure would be minimal under normal operating conditions.
There was a high proportion of respirator non-users who used surgical masks. Surgical masks only provide barrier protection against large-particle droplets and do not effectively filter small particles.[11,12] They are primarily used in healthcare settings to protect patients and HCWs from those who may have a respiratory infection or to protect sterilized or disinfected equipment. This high prevalence of surgical mask use is concerning because HCWs may be using a surgical mask in situations that require respiratory protection. Specifically, this study found a pattern of potential inappropriate or overuse of a surgical mask with regard to surgical smoke. Nearly all respondents reported wearing a surgical mask (which includes laser masks) when working in the vicinity of surgical smoke. However, surgical masks do not provide adequate protection against surgical smoke.[31] This is worrisome as engineering controls for surgical smoke are not always used or available.[15] Additionally, it is unacceptable to use surgical masks during compounding of or administration of highly toxic antineoplastic drugs.[24] Other studies have found that HCWs may not be knowledgeable about selection of a respirator nor know the specific type of respirator they use.[13,33] These results underscore the need for training and education of employers and HCWs about respirator types.
Although the reason respondents wore a surgical mask is unknown, further exploration of their inappropriate, widespread use to protect against anti-neoplastic drugs, aerosolized medications, surgical smoke, and other chemical hazards seems warranted. Information on the types of protection used indicate it is important to provide HCWs with current and accurate information on the hazards they may be working around. This should include the most recent best practices and guidelines for respiratory protection based on the risks associated with the hazards and the likelihood of exposure to the hazards.
In light of the previous findings, we post hoc explored associations between HCWs respiratory protection behaviors and if the employee was aware if the employer had a procedure for handling the hazard of interest. Knowing there was a procedure was only associated with those that wore only a surgical mask. Perhaps HCWs are correctly following procedures, but the high surgical mask use in situations where a surgical mask will not provide appropriate respiratory protection implies that procedures may not match the risks of the hazards. Other studies have found that HCWs respiratory protection recommendation knowledge may be less than ideal.[13,32] For these reasons, policy-level changes may be the best way to ensure that HCWs are protected, regardless of their personal knowledge about respiratory risks.
Reasons for respirator non-use can be divided into two categories: (1) legitimate non-use of a respirator (not part of the facility’s protocol, exposure was minimal, an engineering control was in use); and (2) potential under-protection due to deviation from protocols (not readily available in work area, no one else who does this work uses them, too uncomfortable or difficult to use, and concerned about raising patient’s anxiety). The majority of reasons why HCW did not use a respirator fall into the legitimate non-use of a respirator category (62%). However, 26% of respondents reported a reason that suggests potential under-protection. Targeting these barriers to respirator use could improve workplace protections for HCWs. The final reason for not using a respirator, not provided by an employer, is difficult to categorize as it could be a legitimate non-use, i.e., employer protocol deemed a respirator not necessary, or potential under-protection, i.e., employer not providing respirators to employees when needed. It should be pointed out that not being part of the protocol should be carefully interpreted, as protocols must be updated if exposure or hazard recommendations change and HCWs should be made aware of the revised protocols.
These responses can also be sorted into barrier categories: organizational, personal, and product. As shown in Figure 2, more than half of responses as to why HCWs did not wear a respirator aligned with the organizational level factors (not being part of the protocol, not being readily available, and not being provided by employer) and could be addressed with site-wide interventions. At the personal level, no one else who does this work uses them was the main reason for non-use of respirators. Training and education on the risks associated with exposure could help encourage use of respirators when needed. When the exposure is minimal or engineering controls are used, HCWs should be able to identify if, and when, there is a failure of the controls or when exposure is no longer minimal to ensure that adequate respiratory protection is used. Product barriers (too uncomfortable or difficult to use and concerned about raising the patient’s anxiety) were reported the least often as the reason HCWs did not use respiratory protection, indicating that the product itself did not necessarily hinder use as often.
Study findings indicate that individual factors, such as education, age, or experience, did not play a significant role in the decision to use a respirator or not, which is consistent with previous studies.[4,32] Instead, characteristics of the job (i.e., job type and percentage of time spent in direct patient care) as well as work-site characteristics (i.e., number of employees and facility type) were more predictive of respirator use. This may be due to an emphasis on job- or hazard-specific training and is encouraging to safety professionals.
As seen in Table 2, respirator users were more likely to have received a seasonal influenza vaccination and to have had training in the past 12 months than those who did not use respirators, potentially indicating a safety-focused individual or working environment. Respirator users were also more likely to have PPE available to them and to have received adequate training. There was no significant difference between respirator users and non-users related to having the time to take safety precautions, having positive safety climate, or work-related stress, reinforcing that individual factors have less of an impact on wearing a respirator than job or organizational safety practices. A study of nurses who administered liquid antineoplastic drugs from this survey found that use of PPE and engineering controls was better when perceived management commitment to safety—a key component of safety climate—was higher.[18]
Limitations of the survey instrument and implementation have been discussed elsewhere.[23] The exposures included are not an exhaustive list of possible risks that require respirator use in the healthcare setting; notably, respirator use for infectious diseases other than ILI, such as tuberculosis, was not captured.
This survey was unique in that it collected information on respiratory protection practices from HCWs who routinely use or were in contact with hazardous chemicals. It is important for respiratory protection program managers to obtain feedback from employees and provide guidance to improve compliance and mitigate barriers to using appropriate respiratory protection.
Conclusions
This study reports on respiratory protection practices across prominent healthcare hazards, reasons why respiratory protection was not used, and factors that vary between respirator users and non-users. N95 respirators were the most commonly used respirator type. The widespread use of surgical masks warrants further investigation, as they appear to be used in some situations where respiratory protection is recommended, such as around surgical smoke and antineo-plastic drugs. Guidance, tools, and training should be innovative to increase hazard recognition, risk evaluation, and appropriate respirator selection and use for HCWs. Additionally, as site-specific characteristics were the key drivers for respirator use, organizational-level interventions should be considered to ensure that protocols follow best practices, guidelines are updated regularly, and that appropriate respiratory protection is provided and available.
Acknowledgments
The authors are grateful to the professional practice organizations and their members who participated in the survey. Additionally, thanks to the internal and external subject matter experts who reviewed the manuscript prior to journal submission.
Footnotes
Publisher's Disclaimer: Disclaimer
Publisher's Disclaimer: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the National Institute for Occupational Safety and Health (NIOSH). Mention of company names or products does not constitute endorsement by NIOSH.
References
- [1]. Bureau of Labor Statistics: “Employer-Reported Workplace Injuries and Illnesses.” Available at https://www.bls.gov/iif/oshwc/osh/os/ostb4736.pdf (accessed May 1, 2017).
- [2]. NIOSH: “Hierarchy of Controls.” Available at https://www.cdc.gov/niosh/topics/hierarchy/ (accessed May 2017).
- [3]. Gralton J, Rawlinson W, and McLaws M: Health care workers’ perceptions predicts uptake of personal protective equipment. Am. J. Infect. Control 41:2–7 (2013). [DOI] [PubMed] [Google Scholar]
- [4]. Nichol K, McGeer A, Bigelow P, O’Brian-Pallas L, Scott J, and Holness D: Behind the mask: Determinants of nurse’s adherance to facial protective equipment. Am. J. Infect. Control 41(1):8–13 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5]. Candiotti K, Rodriguez Y, Shekhter I, et al. : A comparison of different types of hazardous material respirators available to anesthesiologists. Am. J. Disaster Med. 7(4):313–319 (2012). [DOI] [PubMed] [Google Scholar]
- [6]. Moore D, Gamage B, Bryce E, Copes R, and Yassi A: Protecting healthcare workers from SARS and other respiratory pathogens: Organizational and individual factors that affect adherence to infection control guidelines. Am. J. Infect. Control 33(2):88–96 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7]. NIOSH: “Hospital Respiratory Protection Program Toolkit.” Available at http://www.cdc.gov/niosh/docs/2015-117/pdfs/2015-117.pdf (accessed October 12, 2015).
- [8]. OSHA: “Regulations (Standards 29 CFR 1910.134).” Available at https://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=standards&p_id=12716 (accessed October 15, 2017).
- [9]. Doney B, Groce D, Cambell D, et al. : A survey of private sector respirator use in the United States: An overview of findings. J. Occup. Environ. Hyg 2(5):267–276 (2005). [DOI] [PubMed] [Google Scholar]
- [10]. Taormina D, and Burgel B: Development of a respiratory protection survey instrument for occupational health nurses: An educational project. Workplace Health Saf. 61(2):79–83 (2013). [DOI] [PubMed] [Google Scholar]
- [11]. Rengasamy S, Miller A, Eimer BC, and Shaffer R: Filtration performance of FDA-cleared surgical masks. J. Int. Soc. Resp. Prot 26(I–II):54–70 (2009). [PMC free article] [PubMed] [Google Scholar]
- [12]. FDA. “Masks and N95 Respirators.” Available at https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/GeneralHospitalDevicesandSupplies/PersonalProtectiveEquipment/ucm055977.htm (accessed March 19, 2018).
- [13]. Peterson K, Novak D, Stradtman L, Wilson D, and Couzens L: Hospital respiratory protection practices in 6 U.S. states: A public health evaluation study. Am. J. Infect. Control 43(1):63–71 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14]. Tsai R, Boiano JM, Steege AL, and Sweeney M: Precautionary practices of respiratory therapists and other healthcare practitioners who administer aerosolized medications. Respir. Care 60(10):1409–1416 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15]. Steege AL, Boiano JM, and Sweeney M: Secondhand smoke in the operating room? Precautionary practices lacking for surgical smoke. Am. J. Ind. Med 59:1020–1031 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Boiano JM, Steege AL, and Sweeney M: Adherence to safe handling guidelines by healthcare workers who administer antineoplastic drugs. J. Occup. Environ. Hyg 11(11):728–740 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Silver S, Steege AL, and Boiano JM: Predictors of adherence to safe handling practices for antineo-plastic drugs: A survey of hospital nurses. J. Occup. Environ. Hyg 13(3):203–221 (2016). [DOI] [PubMed] [Google Scholar]
- [18].Peterson K, Rogers B, Brousseau L, et al. : Difference is hospital managers’, unit managers’, and healthcare workers’ perceptions of the safety climate for respiratory protection. Workplace Health Saf. 64(7):326–336 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Dejoy D, Smith T, Woldu H, Dyal MA, Steege AL, and Boiano JM. Effect of organizational safety practices and percieved safety climate on PPE usage, engineering controls, and adverse events involving liquid antineoplastic drugs among nurses.J. Occup. Environ. Hyg 14(7):485–493 (2017). [DOI] [PubMed] [Google Scholar]
- [20].IOM: “Preparing for an Influenza Pandemic: Personal Protective Equipment for Healthcare Workers.” Available at https://www.nap.edu/catalog/11980/preparing-for-an-influenza-pandemic-personal-protective-equipment-for-healthcare (accessed April 6, 2016).
- [21].NIOSH: “NIOSH Personal Protective Technology Program Healthcare Stakeholder Meeting.” Available at https://www.cdc.gov/niosh/npptl/resources/certpgmspt/meetings/06182013/healthcareinvitationlttr06182013.html (accessed April 6, 2016).
- [22].Gosch M, Shaffer R, Eagan A, Roberge R, Davey V, and Radonovich L: B95: A new respirator for healthcare personnel. Am. J. Infect. Control 41(12):1124–1130 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Steege AL, Boiano JM, and Sweeney M: NIOSH health and safety practices survey of health-care workers: Training and awareness of employer safety procedures. Am. J. Ind. Med 57(6):640–652 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].NIOSH: NIOSH List of Antineoplastic and Other Hazardous Drugs in Healthcare Settings, 2016, by Connor TH, MacKenzie BA, DeBord DG, Trout DB, and O’Callaghan JP (Publication Number 2016–161). U.S. DHHS, CDC, 2016, [Google Scholar]
- [25].OSHA: “Regulations (Standards 29 CFR 1910.1200).” Available at https://www.osha.gov/pls/oshaweb/owadisp.show_document?p_=tablestandards&p_id=10099 (accessed March 24, 2018).
- [26].OSHA: “Controlling Occupational Exposure to Hazardous Drugs.” Available at https://www.osha.gov/SLTC/hazardousdrugs/controlling_occex_hazard-ousdrugs.html (accessed March 24, 2018).
- [27].OSHA: “Best Practices for the Safe Use of Gluteraldehyde in Health Care.” Available at https://www.osha.gov/Publications/3258-08N-2006-English.html (accessed March 24, 2018).
- [28].Recommended Practices for Laser Safety in Perioperative Practice Settings In Standards, Recommended Practices, and Guidelines, Connor R (ed). Association of Perioperative Registered Nurses Inc. Denver, CO: AORN, Inc., 2014. pp. 141–154. [Google Scholar]
- [29].Recommended Practices for Electrosurgery In Perioperative Standards and Recommended Practices,Connor R (ed.). Association of Perioperative Registered Nurses Inc. Denver, CO: AORN, Inc., 2014. pp. 123–139. [Google Scholar]
- [30].Wizner K, Stradtman L, Novak D, and Shaffer R: Prevalence of respiratory protective devices in U.S. healthcare facilities: Implications for emergency prepardness. Workplace Health Saf. 64:359–368 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Gao S, Koehler R, Yermakov M, and Grinshpun S: Performance of facepiece respirators and surgical masks against surgical smoke: Simulated workplace protection factor study. Ann. Occup. Hyg 60(5):608–618 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Hines L, Rees E, and Pavelchak N: Respiratory protection policies and practices among the healthcare workforce exposed to influenza in New York State: Evaluating emergency preparedness for the next pandemic. Am. J. Infect. Control 42(3):240–245 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Nichol K, Bigelow P, O’Brian-Pallas L, McGreer A, Manno M, and Holness D: The individual, environmental, and organizational factors that influence nurses’ use of facial protection to prevent occupational transmission of communicable respiratory illness in acute care hospitals. Am. J. Infect. Control 36(7):481–487 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]