Abstract
Oral squamous cell carcinoma (OSCC) is a major cancer type in the head and neck region. Recent studies have reported a marked rise in the incidence of OSCC. The present study was performed to better understand the roles that long non-coding RNAs (lncRNAs) serve in OSCC carcinogenesis. The levels of the lncRNA C5orf66 antisense RNA 1 (C5orf66-AS1) and of cytochrome c1 (CYC1) in OSCC tissues and cells were measured through reverse transcription-quantitative polymerase chain reaction. In addition, the levels of associated proteins were analyzed by western blotting, while MTT assay was used to detect the cell proliferation ability. Wound healing and transwell assays were also used to detect the migration and invasion abilities of OSCC cells in the experimental groups, while flow cytometry was applied to analyze cell apoptosis. The findings revealed that the expression of lncRNA C5orf66-AS1 in OSCC tissues and cells was significantly decreased. Overexpression of lncRNA C5orf66-AS1 significantly inhibited the proliferation, invasion and migration ability of OSCC cells, and promoted cell apop-tosis, while lncRNA C5orf66-AS1 downregulation presented the opposite effects. In addition, it was observed that CYC1 was upregulated in OSCC tissues and cells, and was negatively regulated by lncRNA C5orf66-AS1. Notably, CYC1 silencing markedly eliminated the effects of lncRNA C5orf66-AS1 downregulation on OSCC cells. Taken together, these findings indicated that lncRNA C5orf66-AS1 may prevent OSCC progression by inhibiting OSCC cell growth and metastasis via the regulation of CYC1 expression.
Keywords: oral squamous cell carcinoma, long non-coding RNA, C5orf66 antisense RNA 1, cell growth, metastasis
Introduction
Oral cavity and oropharyngeal squamous cell carcinoma is the eighth most common type of cancer among men and fourteenth most common among women in the U.S. according to recently reported data (1). Oral squamous cell carcinoma (OSCC) is the most common head and neck cancer worldwide, with a high morbidity and mortality, and is generally defined as squamous cell carcinoma originating in the lips, tongue, gums, cheeks, palate and mouth (2). Prognosis and treatment planning is typically assessed based on tumor staging according to the TNM classification and Union for International Cancer Control system (3-6). However, the biological heterogeneity of OSCC is not taken into consideration by these staging systems. Therefore, more specific bio-markers for OSCC are required.
The majority of OSCC cases are attributed to smoking, alcohol consumption, chewing betel nut and human papillomavirus infection (7). However, the precise mechanisms underlying OSCC development remain poorly understood. In recent decades, little improvement has been achieved to the overall prognosis for advanced-stage OSCC patients, with a heavy disease burden remaining for patients and their families (8). Thus, achieving a better understanding of the mechanisms underlying oral carcinogenesis continues to be urgent in order to aid the identification of effective therapeutic targets (9-11).
Long non-coding RNA (lncRNA) in the genome is a type of RNA that is >200 nt in length and lacks an open reading frame (12). The information contained in lncRNA is rich and serves a role in normal physiological processes, including cell growth, development, metabolism and apoptosis. In addition, a large number of abnormally expressed lncRNAs are involved in tumor metabolism, occurrence and development (13). Therefore, the study of lncRNAs associated with tumor formation, invasion and metastasis, as well as their underlying molecular mechanisms, serves an extremely important role in the prevention and treatment of cancer.
It has been estimated that >70% of DNA sequences in the human genome can be transcribed into RNA; however, only 2% of these transcripts are protein-coding, while the majority of transcripts are categorized as non-coding RNAs (ncRNAs) (14). With the exception of housekeeping ncRNAs, such as transfer RNAs and ribosomal RNAs, certain mRNA-like transcripts also exist that can be subdivided by length, including small ncRNAs (<200 nt) and long ncRNAs (lncRNA; >200 nt) (15). Small ncRNAs, such as microRNAs, have been extensively studied, and there is evidence to suggest that they may serve an important role in several types of cancer, including OSCC (16). However, the role of lncRNAs in cancer has only been investigated in the last decade (17,18). To date, a small amount of research has been conducted on the function of lncRNAs, indicating that they are involved in transcription and serve as post-transcriptional regulators. Furthermore, lncRNAs can reshape chromatin states (8,18-21), stabilize proteins and protein complexes (22), and compete with endogenous RNAs to regulate their function (23,24).
At present, the classification according to the tumor size and presence of distant metastasis of cancer cells in regional lymph nodes is not sufficient to accurately predict the prognosis of OSCC. Therefore, new prognostic parameters that are sufficiently specific and sensitive are urgently required to optimize patient stratification, treatment options and prognosis in clinical practice.
To better understand the role of lncRNAs in the carcinogenesis of OSCC and gain an insight into the identification of potential clinically relevant targets, the current study investigated the role and underlying mechanism of the lncRNA C5orf66 antisense RNA 1 (C5orf66-AS1) in OSCC tissues and cells.
Materials and methods
Clinical specimens
A total of 30 paired OSCC and adjacent normal tissues were collected from 30 OSCC patients (male, 21; female, 9; age, 35-67 years) at the Stomatological Hospital of Guizhou Medical University (Guiyang, China) between July 2016 and July 2017. None of the patients received radiotherapy, chemotherapy or other special treatment. All patients were diagnosed with oral squamous cell carcinoma by histological examination. All tissue samples were immediately flash-frozen in liquid nitrogen and stored at −80°C. The present study was approved by the Human Ethics Committee Review Board at the Stomatological Hospital of Guizhou Medical University. Informed consent was provided by each patient.
Cell culture and treatment
The OSCC cell line SCC9 and the primary normal human oral keratinocyte (HOK) cells were originally acquired from the American Type Culture Collection (Manassas, VA, USA) and cultured in our institute. OSCC cells were incubated in RPMI 1640 medium (Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA) containing 10% fetal bovine serum and 1% penicillin-streptomycin solution (Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) at 37°C with 5% CO2. Cells were passaged every 2-3 days.
Following two passages, SCC9 cells (3×104 cells/well) were seeded into 6-well plates and then transiently transfected with the negative control, lncRNA C5orf66-AS1-small interfering RNA (siRNA), lncRNA C5orf66-AS1-plasmid or lncRNA C5orf66-AS1-siRNA + cytochrome c1 (CYC1)-siRNA, respectively. For transfection, Lipofectamine 2000 (Invitrogen; Thermo Fisher Scientific, Inc.) was used, according to the manufacturer’s protocol.
MTT assay
In the present study, the cell proliferation ability was measured by performing an MTT assay (Sigma-Aldrich; Merck KGaA). Briefly, cells were seeded into 96-well plates (3×103 cells per well) and incubated for 0, 12, 24 or 48 h, after which 20 µl MTT was added to each well and then incubated for a further 4 h at 37°C. Cell viability was assessed by detecting the absorbance at 450 nm using a microplate reader. All tests were performed in quadruplicate.
Reverse transcription-quantitative polymerase chain reaction (RT-qPCR)
TRIzol reagent (Thermo Fisher Scientific, Inc.) was used to extract the total RNA from the cells. The total RNA concentration was detected by Nanodrop 2000 (Thermo Fisher Scientific, Inc.), and then stored at −80°C prior to use. Next, cDNA was generated using the PrimeScript™ RT reagent kit (Takara Bio, Inc.) in line with the manufacturer’s protocol. SYBR Premix Ex Taq (Takara Bio, Inc.) was then used to analyze the synthesized cDNAs according to the manufacturer’s instructions. Amplification conditions were as follows: 95°C for 10 min, followed by 40 cycles at 95°C for 15 sec, 72°C for 30 sec and 78°C for 1.5 min. Primer sequences used for qPCR were as follows: LncRNA C5orf66-AS1, forward 5′-GCTTCGCGTCAAGAGGGTAT-3′ and reverse 5′-GACCGACGTCTGCTGCTTTT-3′; CYC1, forward 5′-GAGGTGGAGGTTCAAGACGG-3′ and reverse 5′-TAGCTCGCACGATGTAGCTG-3′; B cell lymphoma 2 (Bcl-2), forward 5′-TTGGATCAGGGAGTTGGAAG-3′ and reverse 5′-TGTCCCTACCAACCAGAAGG-3′; Bcl-2-associated X protein (Bax), forward 5′-CGTCCACCAAGAAGCTGAGCG-3′ and reverse 5′-CGTCCACCAAGAAGCTGAGCG-3′; matrix metalloproteinase (MMP)-9, forward 5′-GAGGCGCTCATGTACCCTATGTAC-3′ and reverse 5′-GTTCAGGGCGAGGACCATAGA G-3′; Caspase-3, forward 5′-GGCTTGCCAGAAGATACCGGT-3′ and reverse 5′-GCATAAATTCTAGCTTGTGCGCGT-3′; Caspase-7, forward 5′-GATCAGCCTTGTGGGATGGCAGA-3′ and reverse 5′-GTACTGATATGTAGGCACTCG-3′; Caspase-9, forward 5′-CAGAATGCGCTCCTTTCACTTTG-3′ and reverse 5′-AAGTAGCTCACGATTCTCTCTAC-3′; and GAPDH, forward 5′-CTTTGGTATCGTGGAAGGACTC-3′ and reverse 5′-GTAGAGGCAGGGATGATGTTCT-3′. The 2−ΔΔCq method (25) was applied for the calculation of the relative expression of the genes. GAPDH was used as an internal control.
Cell migration and invasion assays
An in vitro invasion assay was performed using Transwell plates (BD Biosciences, Franklin Lakes, NJ, USA) with 8-µm pores. SCC9 cells (1×104 cells/ml) in RPMI 1640 medium were added to the upper chamber of the Transwell 24-well plates, while RPMI-1640 medium containing 20% fetal bovine serum as a chemoattractant was added to the lower chamber. After 48-h incubation, cells remaining in the upper chamber were removed using cotton wool, and the invading cells in the upper surface were fixed with methanol at room temperature for 30 min and stained with 0.5% crystal violet. Images were captured at ×200 magnification, and the cells were counted using a photomicroscope (Olympus Corporation, Tokyo, Japan).
For the wound healing assay, at 48 h after transfection, confluent monolayers of SCC9 cells cultured in 24-well plates (5×105 cells/ml) were mechanically wounded using a 10-µl pipette tip. The wells were washed to remove any cellular debris, and the cells were allowed to migrate for 24 h. Representative images were captured at ×100 magnification under an inverted microscope (Olympus Corporation, Tokyo, Japan). The experiments were repeated at least three times.
Cell apoptosis detection
Following treatment, OSCC cells were collected and washed with cold PBS for at least three times. OSCC cell apoptosis was then measured by a cell apoptosis assay. Briefly, OSCC cells (1×106 cells/well) in a 6-well plate from different groups were first resuspended in binding buffer, and then labeled with Annexin V-FITC and propidium iodide (BD Pharmingen, San Diego, CA, USA), in line with the manufacturer’s protocol. Flow cytometry (BD FACSAria; BD Biosciences, Franklin Lakes, NJ, USA) was applied to analyze the cell apoptosis. The experiment was repeated at least three times.
Western blot analysis
Following treatment, total cellular proteins from OSCC cells were extracted using radioim-munoprecipitation assay buffer (OriGene Technologies, Inc., Beijing, China). A BCA protein quantitative kit (Thermo Fisher Scientific, Inc.) was then used to measure the concentration of protein samples. Next, equal amounts of protein samples were resolved by 12% SDS-PAGE and then transferred onto polyvinylidene difluoride membranes. The membranes were blocked with 5% non-fat milk at room temperature for 1 h, followed by overnight incubation at 4°C with primary antibodies, including anti-CYC1 (ab224044; 1:1,000 dilution; Abcam, Cambridge, UK), anti-Bcl-2 (no. 4223; 1:1,000 dilution; Cell Signaling Technology, Inc., Danvers, MA, USA), anti-Bax (no. 5023; 1:1,000 dilution; Cell Signaling Technology, Inc.), anti-Caspase-3 (no. 9665; 1:1,000 dilution; Cell Signaling Technology, Inc.), anti-Caspase-7 (no. 9492; 1:1,000 dilution; Cell Signaling Technology; Inc.), anti-Caspase-9 (no. 9502; 1:1,000 dilution; Cell Signaling Technology, Inc.), anti-cleaved Caspase-3 (no. 9664; 1:1,000 dilution; Cell Signaling Technology, Inc.), anti-cleaved Caspase-7 (no. 9491; 1:1,000 dilution; Cell Signaling Technology, Inc.), anti-cleaved Caspase-9 (no. 9505; 1:1,000 dilution; Cell Signaling Technology, Inc.), and anti-MMP9 (no. 13667; 1:1,000 dilution; Cell Signaling Technology, Inc.). Subsequently, membranes were incubated with a horseradish peroxidase-conjugated anti-rabbit IgG secondary antibody (no. 7074; 1:5,000 dilution; Cell Signaling Technology, Inc.) at room temperature for 2 h. To visualize the protein blots, an ECL kit (Applygen Technologies, Inc., Beijing, China) was used according the manufacturer’s protocol. Results were quantified using Quantity One version 4.6 software (Bio-Rad Laboratories, Inc., Hercules, CA, USA).
Statistical analysis
All data are displayed as the mean ± standard deviation. SPSS statistical software (version 17.0; SPSS, Inc., Chicago, IL, United States) was performed for statistical analyses. Comparison between groups was performed by using Student’s t-test or analysis of variance. P<0.05 was considered to denote differences that were statistically significant.
Results
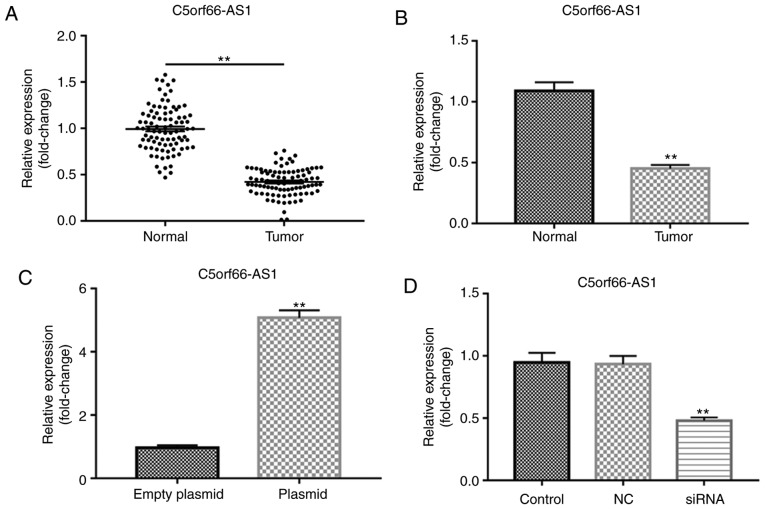
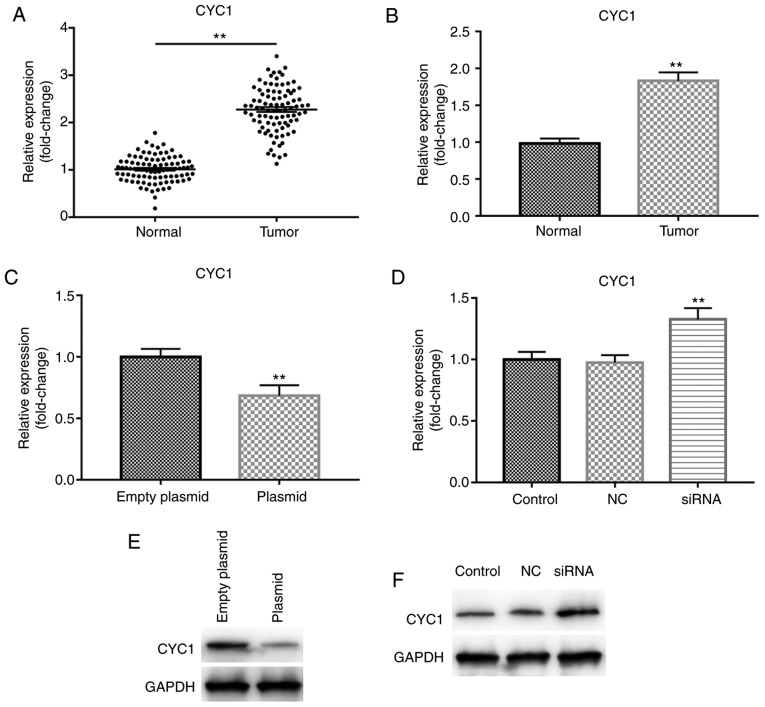
Expression of lncRNA C5orf66-AS1 in SCC9 cells
The present study first detected the level of the lncRNA C5orf66-AS1 in OSCC and adjacent normal tissues, as well as in the OSCC cell line SCC9 and primary normal HOK cells, using RT-qPCR. The results demonstrated that, compared with the adjacent normal tissues, lncRNA C5orf66-AS1 expression was significantly decreased in OSCC tissues (Fig. 1A). It was also observed that, compared with normal HOK cells, the expression of lncRNA C5orf66-AS1 was significantly reduced in SCC9 cells (Fig. 1B). Given the limited understanding of the role of lncRNA C5orf66-AS1 in SCC9 cells, the cells were then transiently transfected with lncRNA C5orf66-AS1-siRNA, the negative of lncRNA C5orf66-AS1-siRNA (NC) to further examine the effect of this lncRNA on SCC9 cells, and cells without any treatment were used as the control group. Besides, lncRNA C5orf66-AS1-plasmid was also transfected into SCC9 cells and empty plasmid as the control. The results indicated that the expression of lncRNA C5orf66-AS1 was significantly increased in the lncRNA C5orf66-AS1-plasmid-transfected cells, indicating successful overexpression by plasmid transfection (Fig. 1C). However, in the lncRNA C5orf66-AS1-siRNA group, the expression on lncRNA C5orf66-AS1 was significantly reduced, indicating successful silencing by siRNA transfection (Fig. 1D).
Figure 1.
lncRNA C5orf66-AS1 expression in OSCC tissues and cells was detected using RT-qPCR. Expression of lncRNA C5orf66-AS1 in (A) OSCC and adjacent normal tissues, and (B) OSCC cell line SCC9 and primary normal human oral keratinocyte cells. Next, SCC9 cells were transfected with (C) lncRNA C5orf66-AS1-plasmid (overexpression) or control plasmid, and with (D) lncRNA C5orf66-AS1-siRNA (knockdown) or NC-siRNA. Cells without any siRNA treatment were considered as the control group. After 48 h, lncRNA C5orf66-AS1 expression was detected using RT-qPCR. **P<0.01 vs. corresponding control groups. OSCC, oral squamous cell carcinoma; lncRNA, long non-coding RNAs; C5orf66-AS1, C5orf66 antisense RNA 1; siRNA, small interfering RNA; NC, negative control siRNA; RT-qPCR, reverse transcription-quantitative polymerase chain reaction.
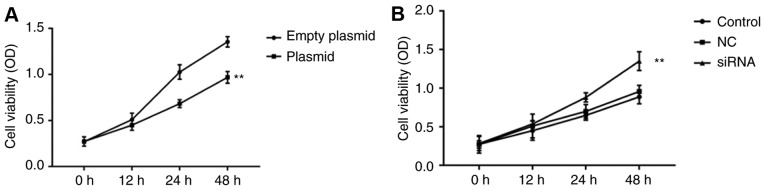
Effect of lncRNA C5orf66-AS1 on the proliferation of SCC9 cells
Cells were transiently transfected with the negative control, lncRNA C5orf66-AS1-siRNA, lncRNA C5orf66-AS1-plasmid and empty plasmid serving as the control. Next, the cell proliferation ability was detected using an MTT assay, and the results demonstrated that lncRNA C5orf66-AS1-plasmid significantly suppressed SCC9 cell proliferation (Fig. 2A), while lncRNA C5orf66-AS1-siRNA increased the proliferation ability of SCC9 cells (Fig. 2B).
Figure 2.
Effect of lncRNA C5orf66-AS1 on SCC9 cell proliferation. At 48 h after transfection with (A) lncRNA C5orf66-AS1-plasmid or (B) lncRNA C5orf66-AS1-siRNA, the cell proliferation ability was detected using an MTT assay. **P<0.01 vs. corresponding control groups. lncRNA, long non-coding RNAs; C5orf66-AS1, C5orf66 antisense RNA 1; siRNA, small interfering RNA; NC, negative control; OD, optical density.
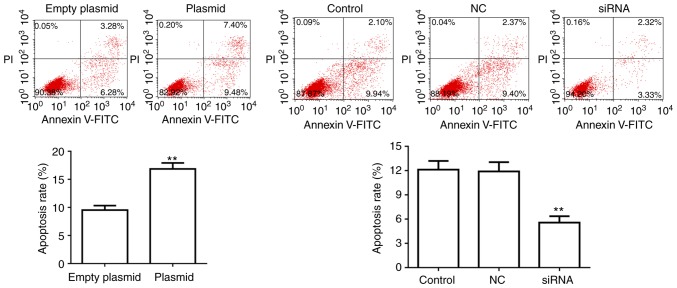
Effect of lncRNA C5orf66-AS1 on apoptosis of SCC9 cells
SCC9 cell apoptosis was also detected at 48 h after transfection. Flow cytometry analysis revealed that, compared with the control groups, the apoptosis of SCC9 cells was significantly upregulated in cells transfected with lncRNA C5orf66-AS1-plasmid. By contrast, the apoptosis rate was markedly decreased in lncRNA C5orf66-AS1-siRNA-transfected SCC9 cells compared with the control cells (Fig. 3).
Figure 3.
Effect of lncRNA C5orf66-AS1 on SCC9 cell apoptosis. At 48 h after transfection, cell apoptosis was detected using flow cytometry. **P<0.01 vs. control groups. lncRNA, long non-coding RNAs; C5orf66-AS1, C5orf66 antisense RNA 1; siRNA, small interfering RNA; NC, negative control.
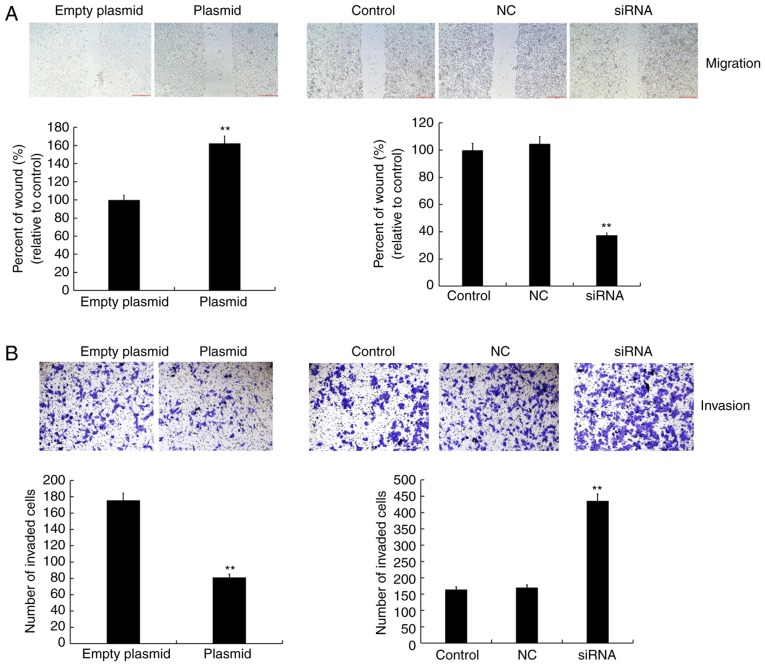
Effect of lncRNA C5orf66-AS1 on migration and invasion abilities of SCC9 cells
A wound healing assay was conducted to detect cell migration, while cell invasion was detected using a transwell assay. It was observed that the cell migration and invasion abilities were inhibited in the lncRNA C5orf66-AS1-plasmid transfection group as compared with the control group. By contrast, in the lncRNA C5orf66-AS1-siRNA transfection group, the cell migration and invasion abilities were increased and there was no statistically significant changes between the control group and the NC group (Fig. 4).
Figure 4.
Effect of lncRNA C5orf66-AS1 on SCC9 cell migration and invasion. At 48 h after transfection, the (A) migration and (B) invasion abilities of cells were detected using a wound healing assay and transwell assay, respectively. The cell migration into the wound was quantified, and the number of invasive cells was counted. Magnification, ×100 (migration) and ×200 (invasion). **P<0.01 vs. control groups. lncRNA, long non-coding RNAs; C5orf66-AS1, C5orf66 antisense RNA 1; siRNA, small interfering RNA; NC, negative control.
CYC1 is upregulated in OSCC tissues and cells, and is downregulated by lncRNA C5orf66-AS1 overexpression
The mRNA level of CYC1 in OSCC and adjacent normal tissues, and in the OSCC cell line SCC9 and primary normal HOK cells was detected using RT-qPCR. The results indicated that, compared with the adjacent normal tissues, CYC1 was significantly increased in OSCC tissues (Fig. 5A). It was also demonstrated that, compared with HOK cells, the expression of CYC1 was significantly increased in SCC9 cells (Fig. 5B). Subsequently, to explore the association between lncRNA C5orf66-AS1 and CYC1, SCC9 cells were trans-fected with the lncRNA C5orf66-AS1-plasmid or lncRNA C5orf66-AS1-siRNA for 48 h and the mRNA level of CYC1 was detected. The results revealed that overexpression of lncRNA C5orf66-AS1 significantly decreased the mRNA level of CYC1, while lncRNA C5orf66-AS1 silencing by siRNA transfection significantly enhanced the mRNA level of CYC1 (Fig. 5C and D). Furthermore, the protein level of CYC1 in SCC9 cells was detected following transfection with lncRNA C5orf66-AS1-plasmid or -siRNA. As expected, overexpression of lncRNA C5orf66-AS1 downregulated the protein level of CYC1 in SCC9 cells, while silencing of lncRNA C5orf66-AS1 significantly enhanced the protein level of CYC1, as compared with the corresponding control groups (Fig. 5E and F).
Figure 5.
CYC1 was negatively regulated by lncRNA C5orf66-AS1. CYC1 mRNA expression in (A) OSCC and adjacent normal tissues, and in (B) OSCC cell line SCC9 and normal human oral keratinocyte cells was detected using reverse transcription-quantitative polymerase chain reaction. CYC1 mRNA and protein levels were also detected in cells transfected with (C and E) lncRNA C5orf66-AS1-plasmid or (D and F) lncRNA C5orf66-AS1-siRNA. **P<0.01 vs. control groups. lncRNA, long non-coding RNAs; C5orf66-AS1, C5orf66 antisense RNA 1; siRNA, small interfering RNA; NC, negative control; CYC1, cytochrome c1.
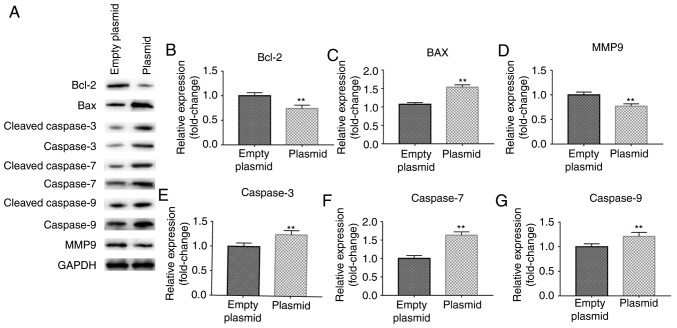
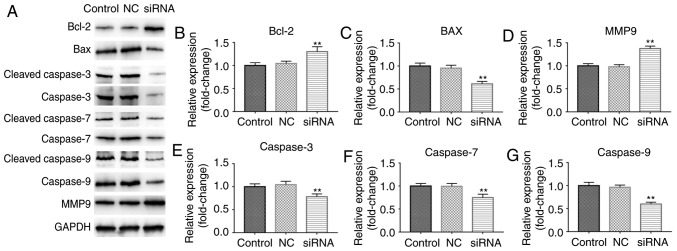
Effect of lncRNA C5orf66-AS1 on the expression levels of associated genes in SCC9 cells
Subsequently, the effects of lncRNA C5orf66-AS1 on the expression levels of genes associated with cell proliferation, apoptosis and metastasis, including Bcl-2, Bax, cleaved Caspase-3/7/9, Caspase-3/7/9 and MMP9, were investigated. The results demonstrated that lncRNA C5orf66-AS1-plasmid transfection significantly reduced the protein levels of Bcl-2 and MMP9, while the expression levels of Bax, cleaved Caspase-3/Caspase-3, cleaved Caspase-7/Caspase-7 and cleaved Caspase-9/Caspase-9 were significantly increased (Fig. 6A). The mRNA levels of Bcl-2 and MMP9 were also reduced by lncRNA C5orf66-AS1-plasmid transfection, while mRNA levels of Bax, Caspase-3, Caspase-7 and Caspase-9 were enhanced (Fig. 6B-G). However, lncRNA C5orf66-AS1-siRNA transfection significantly increased the protein levels of Bcl-2 and MMP9, while it markedly decreased the expression levels of Bax, cleaved Caspase-3/Caspase-3, cleaved Caspase-7/Caspase-7, and cleaved Caspase-9/Caspase-9 (Fig. 7). Taken together, these data indicated that lncRNA C5orf66-AS1 overexpression may induce SCC9 cell apoptosis through regulating the expression of apoptosis-associated proteins (Bcl-2 and Bax) and increasing the expression and activation of Caspase-3/7/9, while it may regulate SCC9 cell migration and invasion by regulating MMP9 expression.
Figure 6.
Effect of lncRNA C5orf66-AS1-plasmid on Bcl-2, Bax, MMP9, Caspase-3, Caspase-7 and Caspase-9 expression levels in SCC9 cells. (A) Western blot analysis was performed at 48 h after cell transfection to detect the protein levels. (B) Bcl-2, (C) Bax, (D) MMP9, (E) cleaved Caspase-3/Caspase-3, (F) cleaved Caspase-7/Caspase-7 and (G) cleaved Caspase-9/Caspase-9 in SCC9 cells were detected using reverse transcription-quantitative polymerase chain reaction. **P<0.01 vs. control groups. lncRNA, long non-coding RNAs; C5orf66-AS1, C5orf66 antisense RNA 1; Bcl-2, B-cell lymphoma 2; Bax, Bcl-2-associated X protein; MMP9, matrix metalloproteinase 9.
Figure 7.
Effect of lncRNA C5orf66-AS1-siRNA on Bcl-2, Bax, MMP9, Caspase-3, Caspase-7 and Caspase-9 expression levels in SCC9 cells. (A) Western blot analysis was performed at 48 h after cell transfection to detect the protein levels. (B) Bcl-2, (C) Bax, (D) MMP9, (E) cleaved Caspase-3/Caspase-3, (F) cleaved Caspase-7/Caspase-7 and (G) cleaved Caspase-9/Caspase-9 in SCC9 cells were detected using transcription-quantitative polymerase chain reaction. **P<0.01 vs. control groups. lncRNA, long non-coding RNAs; C5orf66-AS1, C5orf66 antisense RNA 1; siRNA, small interfering RNA; NC, negative control; Bcl-2, B-cell lymphoma 2; Bax, Bcl-2-associated X protein; MMP9, matrix metalloproteinase 9.
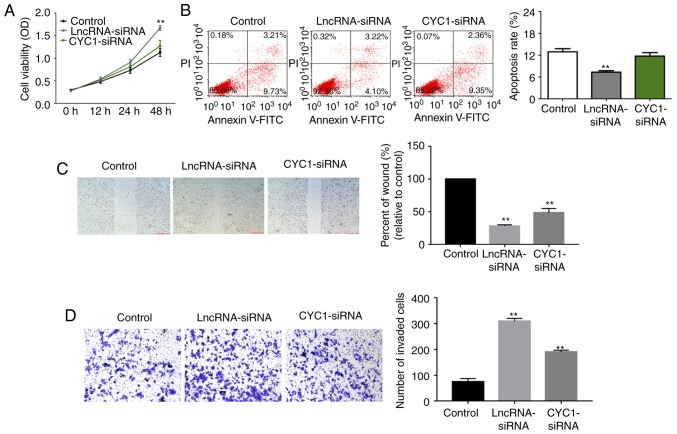
Low expression of CYC1 reverses the effect of lncRNA C5orf66-AS1-siRNA on the biological behavior of SCC9 cells
Next, to explore whether CYC1 was involved in the effect of lncRNA C5orf66-AS1 on SCC9 cells, the cells were transiently transfected with lncRNA C5orf66-AS1-siRNA or lncRNA C5orf66-AS1-siRNA + CYC1-siRNA. The findings suggested that lncRNA C5orf66-AS1-siRNA transfection significantly enhanced the proliferation, migration and invasion ability of SCC9 cells, and inhibited cell apoptosis. However, these changes were significantly reversed by CYC1-siRNA (Fig. 8).
Figure 8.
Effect of CYC1 on SCC9 cells. At 48 h after cell transfection with lncRNA C5orf66-AS1-siRNA or lncRNA C5orf66-AS1-siRNA + CYC1-siRNA, the (A) proliferation, (B) apoptosis, (C) migration and (D) invasion of SCC9 cells were determined using an MTT assay, flow cytometry, wound healing assay and transwell assay, respectively. Wound closure was quantified and the number of invasive cells was counted. **P<0.01 vs. control groups. Magnification, ×100 (migration) and ×200 (invasion). lncRNA, long non-coding RNAs; C5orf66-AS1, C5orf66 antisense RNA 1; siRNA, small interfering RNA; NC, negative control; CYC1, cytochrome c1.
Discussion
OSCC is a malignant tumor with poor prognosis that occurs in the head and neck region, and accounts for 90% of oral cancer cases (26). Despite the current advances in treatment strategies, the 5-year and 10-year survival rates of patients with OSCC have not significantly improved; therefore, OSCC severely impacts human health (27). Previous studies have demonstrated that dysregulation of oncogenes and tumor suppressor genes is an important factor in tumorigenesis and development (28-30). Previous studies have reported that lncRNAs have a complex biological function, are able to regulate the progression of a variety of diseases, and they are closely associated with tumor cell proliferation and metastasis (31). There are a large number of lncRNAs with an unknown function that have yet to be studied. While the genome-wide study of lncRNAs is a good approach to unveil more lncRNAs that may be involved in carcinogenesis or may represent potential therapeutic targets, performing direct comparisons of results from various studies remains challenging.
To the best of our knowledge, the present study is the first to evaluate the role of lncRNA C5orf66-AS1 in OSCC. First, the expression levels of lncRNA C5orf66-AS1 in OSCC and adjacent normal tissues, as well as in the OSCC cell line SCC9 and a normal oral cell line, were compared. The findings of the current study suggested that lncRNA C5orf66-AS1 was significantly downregulated in OSCC. Next, in order to assess the effect of lncRNA C5orf66-AS1 on OSCC cells, lncRNA C5orf66-AS1 was upregulated or downregulated in SCC9 cells through transfection with lncRNA C5orf66-AS1-plasmid or -siRNA, respectively. The results revealed that overexpression of lncRNA C5orf66-AS1 in OSCC significantly inhibited cell proliferation, invasion and migration, and promoted apoptosis, while lncRNA C5orf66-AS1 downregulation presented the opposite effects. These results suggested that lncRNA C5orf66-AS1 inhibits the malignant behavior of SCC9 cells, providing a basis for the treatment of OSCC.
CYC1 is an important subunit of mitochondrial complex III. It is well known that mitochondria are indispensable for energy metabolism. Approximately 90% of cellular adenosine triphosphate is generated in mitochondria through the oxidative phosphorylation pathway. Recent studies indicated that CYC1 serves a key role in the development of tumors, including breast cancer and osteosarcoma among others (32,33). To the best of our knowledge, the role of CYC1 in the progression of OSCC remains unclear. In the present study, it was observed that CYC1 was upregulated in OSCC tissues and cells. In addition, the data revealed that overexpression of lncRNA C5orf66-AS1 in OSCC cells inhibited the expression of CYC1, while knockdown of lncRNA C5orf66-AS1 in SCC9 cells promoted the expression of CYC1. This process may involve the mitochondrial pathway; however, the specific mechanism involved is not clear. Furthermore, it was observed that CYC1 silencing partially offset the promotion of lncRNA C5orf66-AS1 silencing on OSCC cells.
In conclusion, this is the first study to report that lncRNA C5orf66-AS1 was downregulated in OSCC, and overexpres-sion of lncRNA C5orf66-AS1 was able to prevent OSCC progression by inhibiting OSCC cell growth and metastasis via regulating CYC1 expression. Therefore, lncRNA C5orf66-AS1 may be a novel and promising target for OSCC treatment.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The analyzed data sets generated during the present study are available from the corresponding author on reasonable request.
Authors’ contributions
TL designed the study. TL and HL were responsible for data access and analysis. GY interpreted results. All authors collaborated to develop the manuscript.
Ethics approval and consent to participate
The present study was approved by the Human Ethics Committee Review Board at the Stomatological Hospital of Guizhou Medical University (Guiyang, China). Informed consent was provided by each patient.
Patient consent for publication
All patients provided consent for publication.
Competing interests
The authors declare no competing interests.
References
- 1.Ryerson AB, Eheman CR, Altekruse SF, Ward JW, Jemal A, Sherman RL, Henley SJ, Holtzman D, Lake A, Noone AM, et al. Annual report to the nation on the status of cancer, 1975–2012 featuring the increasing incidence of liver cancer. Cancer. 2016;122:1312–1337. doi: 10.1002/cncr.29936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 3.Gershenwald JE, Soong SJ, Balch CM, American Joint Committee on Cancer (AJCC) Melanoma Staging Committee TNM staging system for cutaneous melanoma…and beyond. Ann Surg Oncol. 2010;2010;17:1475–1477. doi: 10.1245/s10434-010-0986-3. [DOI] [PubMed] [Google Scholar]
- 4.Kreppel M, Drebber U, Rothamel D, Eich HT, Kübler A, Scheer M, Zöller JE. Prognostic impact of different TNM-based stage groupings for oral squamous cell carcinoma. Head Neck. 2011;33:1467–1475. doi: 10.1002/hed.21630. [DOI] [PubMed] [Google Scholar]
- 5.Kolk A, Jubitz N, Mengele K, Mantwill K, Bissinger O, Schmitt M, Kremer M, Holm PS. Expression of Y-box-binding protein YB-1 allows stratification into long- and short-term survivors of head and neck cancer patients. Br J Cancer. 2011;105:1864–1873. doi: 10.1038/bjc.2011.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Götz C, Drecoll E, Straub M, Bissinger O, Wolff KD, Kolk A. Impact of HPV infection on oral squamous cell carcinoma. Oncotarget. 2016;7:76704–76712. doi: 10.18632/oncotarget.12501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scully C, Bagan J. Oral squamous cell carcinoma overview. Oral Oncol. 2009;45:301–308. doi: 10.1016/j.oraloncology.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 8.Davidovich C, Cech TR. The recruitment of chromatin modifiers by long noncoding RNAs: Lessons from PRC2. RNA. 2015;21:2007–2022. doi: 10.1261/rna.053918.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rogers SN, Brown JS, Woolgar JA, Lowe D, Magennis P, Shaw RJ, Sutton D, Errington D, Vaughan D. Survival following primary surgery for oral cancer. Oral Oncol. 2009;45:201–211. doi: 10.1016/j.oraloncology.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 10.Nagtegaal ID, Quirke P, Schmoll HJ. Has the new TNM classification for colorectal cancer improved care. Nat Rev Clin Oncol. 2011;9:119–123. doi: 10.1038/nrclinonc.2011.157. [DOI] [PubMed] [Google Scholar]
- 11.Piazzolla D, Palla AR, Pantoja C, Cañamero M, de Castro IP, Ortega S, Gómez-López G, Dominguez O, Megías D, Roncador G, et al. Lineage-restricted function of the pluripotency factor NANOG in stratified epithelia. Nat Commun. 2014;5:4226. doi: 10.1038/ncomms5226. [DOI] [PubMed] [Google Scholar]
- 12.Balch C, Nephew KP. The role of chromatin, microRNAs, and tumor stem cells in ovarian cancer. Cancer Biomark. 8:203–221. 2010–2011. doi: 10.3233/CBM-2011-0214. [DOI] [PubMed] [Google Scholar]
- 13.Sun T. Long noncoding RNAs act as regulators of autophagy in cancer. Pharmacol Res. 2018;129:151–155. doi: 10.1016/j.phrs.2017.11.009. [DOI] [PubMed] [Google Scholar]
- 14.Carvalho AL, Nishimoto IN, Califano JA, Kowalski LP. Trends in incidence and prognosis for head and neck cancer in the United States: A site-specific analysis of the SEER database. Int J Cancer. 2005;114:806–816. doi: 10.1002/ijc.20740. [DOI] [PubMed] [Google Scholar]
- 15.Gutschner T, Diederichs S. The hallmarks of cancer: A long non-coding RNA point of view. RNA Biol. 2012;9:703–719. doi: 10.4161/rna.20481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Min A, Zhu C, Peng S, Rajthala S, Costea DE, Sapkota D. MicroRNAs as important players and biomarkers in oral carcinogenesis. Biomed Res Int. 2015;2015;186904 doi: 10.1155/2015/186904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Feng L, Houck JR, Lohavanichbutr P, Chen C. Transcriptome analysis reveals differentially expressed lncRNAs between oral squamous cellcarcinoma and healthy oral mucosa. Oncotarget. 2017;8:31521–31531. doi: 10.18632/oncotarget.16358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maruyama R, Suzuki H. Long noncoding RNA involvement in cancer. BMB Rep. 2012;45:604–611. doi: 10.5483/BMBRep.2012.45.11.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Quinn JJ, Chang HY. Unique features of long non-coding RNA biogenesis and function. Nat Rev Genet. 2016;17:47–62. doi: 10.1038/nrg.2015.10. [DOI] [PubMed] [Google Scholar]
- 20.Bartonicek N, Maag JL, Dinger ME. Long noncoding RNAs in cancer: Mechanisms of action and technological advancements. Mol Cancer. 2016;15:43. doi: 10.1186/s12943-016-0530-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang Q, Xu E, Dai J, Liu B, Han Z, Wu J, Zhang S, Peng B, Zhang Y, Jiang Y. A novel long noncoding RNA AK001796 acts as an oncogene and is involved in cell growth inhibition by resveratrol in lung cancer. Toxicol Appl Pharmacol. 2015;285:79–88. doi: 10.1016/j.taap.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 22.Clemson CM, Hutchinson JN, Sara SA, Ensminger AW, Fox AH, Chess A, Lawrence JB. An architectural role for a nuclear noncoding RNA: NEAT1 RNA is essential for the structure of paraspeckles. Mol Cell. 2009;33:717–726. doi: 10.1016/j.molcel.2009.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nie W, Ge HJ, Yang XQ, Sun X, Huang H, Tao X, Chen WS, Li B. LncRNA-UCA1 exerts oncogenic functions in non-small cell lung cancer by targeting miR-193a-3p. Cancer Lett. 2016;371:99–106. doi: 10.1016/j.canlet.2015.11.024. [DOI] [PubMed] [Google Scholar]
- 24.Peng W, Si S, Zhang Q, Li C, Zhao F, Wang F, Yu J, Ma R. Long non-coding RNA MEG3 functions as a competing endogenous RNA to regulate gastric cancer progression. J Exp Clin Cancer Res. 2015;34:79. doi: 10.1186/s13046-015-0197-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(−Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 26.SHahinas J, Hysi D. Methods and risk of bias in molecular marker prognosis studies in oral squamous cell carcinoma. Oral Dis. 2018;24:115–119. doi: 10.1111/odi.12753. [DOI] [PubMed] [Google Scholar]
- 27.Peurala E, Tuominen M, Löyttyniemi E, Syrjänen S, Rautava J. Eosinophilia is a favorable prognostic marker for oral cavity and lip squamous cell carcinoma. APMIS. 2018;126:201–207. doi: 10.1111/apm.12809. [DOI] [PubMed] [Google Scholar]
- 28.Lee EY, Muller WJ. Oncogenes and tumor suppressor genes. Cold Spring Harb Perspect Biol. 2010;2:a003236. doi: 10.1101/cshperspect.a003236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Iurlaro R, León-Annicchiarico CL, Muñoz-Pinedo C. Regulation of cancer metabolism by oncogenes and tumor suppressors. Methods Enzymol. 2014;542:59–80. doi: 10.1016/B978-0-12-416618-9.00003-0. [DOI] [PubMed] [Google Scholar]
- 30.Wang D, Qiu C, Zhang H, Wang J, Cui Q, Yin Y. Human microRNA oncogenes and tumor suppressors show significantly different biological patterns: From functions to targets. PLoS One. 2010;5:e13067. doi: 10.1371/journal.pone.0013067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Geisler S, Coller J. RNA in unexpected places: Long non-coding RNA functions in diverse cellular contexts. Nat Rev Mol Cell Biol. 2013;14:699–712. doi: 10.1038/nrm3679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Han Y, Sun S, Zhao M, Zhang Z, Gong S, Gao P, Liu J, Zhou J, Ma D, Gao Q, Wu P. CYC1 predicts poor prognosis in patients with breast cancer. Dis Markers. 2016;2016;3528064 doi: 10.1155/2016/3528064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li G, Fu D, Liang W, Fan L, Chen K, Shan L, Hu S, Ma X, Zhou K, Cheng B. CYC1 silencing sensitizes osteosarcoma cells to TRAIL-induced apoptosis. Cell Physiol Biochem. 2014;34:2070–2080. doi: 10.1159/000366402. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The analyzed data sets generated during the present study are available from the corresponding author on reasonable request.