Abstract
The Veterans Aging Cohort Study (VACS) Index is a composite marker of multisystem injury among HIV-infected persons. We aimed to examine its cross-sectional association with functional outcomes, after considering neurocognitive impairment (NCI) and other well-established correlates of everyday functioning among HIV-infected persons. Participants included 670 HIV-infected adults (ages 18–76; 88% male; 63% Non-Hispanic White; median current CD4=404 cells/mm3; 67% on antiretroviral therapy; AIDS=63%) enrolled in observational studies at the University of California San Diego HIV Neurobehavioral Research Program. Functional outcomes were assessed via self-report measures of declines in activities of daily living, perceived cognitive symptoms in daily life and employment status. NCI was assessed via a comprehensive neurocognitive test battery and defined based on established methods. Covariates examined included demographics, HIV-disease characteristics not included in the VACS Index, and psychiatric comorbidities. The VACS Index was computed via standard methods and categorized based on its distribution. Results from multivariable regression models showed that both higher VACS Index scores (indicative of worse health) and the presence of NCI were independently associated with declines in activities of daily living, increased cognitive symptoms in daily life, and unemployment. These independent effects remained after adjusting for significant covariates. In conclusion, the VACS Index may be a useful tool for identifying HIV-infected patients at high risk for everyday functioning problems. Considering factors such as NCI, historical HIV disease characteristics, and current mood, might be particularly important to enhance the predictive power of the VACS Index for functional status among HIV-infected persons.
Keywords: AIDS, biomarkers, comorbidity, employment status, activities of daily living, neurobehavioral manifestations
Introduction
The development of combination antiretroviral therapy (ART) has greatly improved life expectancy in individuals infected with human immunodeficiency virus (HIV), resulting in steady increases in the number of older adults living with HIV over recent years (Mahy et al. 2014). People living with HIV are now experiencing multiple age-related comorbidities (Deeks and Phillips 2009), and thus, composite biomarkers that incorporate both traditional HIV and non-HIV factors might better capture the complex nature of disease burden in HIV.
The Veterans Aging Cohort Study (VACS) Index was developed as a composite marker of multisystem injury among people living with HIV. It combines age, with HIV-biomarkers (i.e. plasma RNA and CD4+ T-cell counts) and non-HIV biomarkers (i.e. indicators of renal and liver function, anemia, and hepatitis C virus co-infection) (Justice et al. 2012; Justice et al. 2010) that are routinely collected and monitored by HIV-healthcare providers. It has been validated as a prognostic tool for mortality among HIV-infected persons (Justice et al. 2012; Justice et al. 2010; Justice et al. 2013; Tate et al. 2013), and has been linked to poor health outcomes, including increased risk for fragility fractures (Womack et al. 2013) and hospitalizations(Akgun et al. 2014). Additionally, in cross-sectional and longitudinal studies, it has been associated with neurocognitive impairment (NCI) and neurocognitive decline (Marquine, Montoya, et al. 2016; Marquine et al. 2014).
Neurocognitive impairment is highly prevalent in HIV. Approximately half of HIV-infected persons show NCI, and about half of HIV-infected persons with NCI also show deficits in everyday functioning, such as difficulties performing activities of daily living, cognitive symptoms in everyday life, unemployment, driving problems, and medication nonadherence (Heaton et al. 2004; Marcotte et al. 2004; Vance et al. 2014; Vance et al. 2013). Other important predictors of daily functioning problems among HIV-infected person include HIV disease burden, comorbid medical and psychiatric conditions, and certain demographics (e.g. older age, lower formal education) (Blaum et al. 2002; Morgan et al. 2012). Higher VACS Index scores (indicative of worse health) have been linked with dependence in instrumental activities of daily living (IADLs) and medication nonadherence (John et al. 2016). Yet, the limited prior research on the VACS Index and functional outcomes has not investigated its link to other important functional outcomes in HIV (e.g., cognitive symptoms in everyday life and unemployment) or considered the impact of other well-established determinants of functional status in HIV, such as neurocognitive impairment and psychiatric comorbidities, among others. As the use of the VACS Index as a marker of disease status in research continues to expand, examining its link to functional outcomes can aid in interpretation of findings from research on other important outcomes in HIV. Furthermore, given that the VACS Index is largely based on biomarkers commonly collected in clinic, understanding its association with functional outcomes may help clinicians better gauge whether HIV-infected patients might be at increased risk for everyday functioning problems.
There were two main aims to the current study. First, we were interested in extending prior findings showing a link between the VACS Index and some measures of functional status, (i.e., dependence in IADLs and ART adherence) (John et al. 2016), by examining the association of the VACS Index to other functional outcomes, i.e., cognitive symptoms in everyday life and employment status. We hypothesized that higher VACS Index scores (indicative of worse health status) would be associated with increased cognitive failures in everyday life and higher rates of unemployment. We were also interested in investigating whether the VACS Index might be independently associated with functional outcomes (i.e., unemployment, declines in activities of daily living and cognitive symptoms) after considering the impact of NCI and other established predictors of functional outcomes in HIV. We hypothesized that the VACS Index would independently contribute to functional status.
Methods
Participants
Six hundred and seventy HIV-infected adults enrolled in NIH-funded cohort studies at the University of California San Diego (UCSD) HIV Neurobehavioral Research Program from April 14th, 1999 to January 23rd, 2016, participated in the current study. The details of these studies have been reported previously (Heaton et al. 1995; Moore et al. 2017; Rippeth et al. 2004; Woods et al. 2004). Inclusion criteria for the present study were: (1) presence of HIV infection as determined by enzyme-linked immunosorbent assays (ELISA) with Western blot confirmatory test; (2) having laboratory data available to the calculate the VACS Index; (3) having valid data on measures used to assess functional outcomes measures, i.e., Patient’s Assessment of Own Functioning Inventory (PAOFI) and/or Activities of Daily Living Scale; (4) being primarily English speaking; and (5) being free of sensory and physical problems that would interfere with testing. For those participants who had data available on the VACS Index and functional outcome measures at more than one time point, data from the first date was used. Approximately a quarter of the sample (27%) had participated in at least one prior visit at our center. Data on the remaining of the sample (73%) was from the first visit at our center.
Materials and Procedures
All procedures were approved by the UCSD Human Research Protections Program Institutional Review Board. After providing written informed consent, participants completed extensive neuromedical, neurocognitive, psychiatric, and substance use evaluations, similar to prior research by our group on the VACS Index (Marquine et al. 2014). They also completed self-report measures of everyday functioning.
Neuromedical Evaluation
Participants underwent a standardized medical history interview, structured neurological and medical examinations, which included the collection of blood and urine samples. The medical history interviews were conducted by trained research staff and the examinations were performed by clinicians. Laboratory measurements included routine clinical chemistry panels, complete blood counts, rapid plasma reagin, HCV antibody, and CD4+ cells (flow cytometry) performed at Clinical Laboratory Improvement Amendments (CLIA)-certified, or CLIA equivalent, laboratory. Plasma HIV-1 RNA levels were measured by reverse transcriptase polymerase chain reaction (Roche Amplicor, v. 1.5; lower limit of quantitation, 50 copies per milliliter). Self-report data (verified by medical records when available) were collected on duration of HIV infection, nadir CD4+ T-cell count, and ART history. The VACS index was computed as described elsewhere(Justice et al. 2012; Justice et al. 2010), with higher scores representing worse disease status. Given the skewed distribution of VACS Index scores in the current sample, and based on prior findings on the association of the VACS Index and NCI(Marquine et al. 2014), we categorized VACS Index scores into three groups (low, medium, and high) based on the interquartile range (IQR) values in the current sample (VACS Index IQR=10–34). The low VACS Index group included participants with scores of 10 or lower in this index, the high VACS Index scores included those with scores of 34 or higher, and the medium VACS Index group, included those with scores that were within the IQR.
Functional Outcomes
Functional outcomes were ascertained via the Activities of Daily Living Scale (Lawton and Brody 1969), and the PAOFI (Chelune et al. 1986). The Activities of Daily Living Scale is a self-report measure that assesses current level of functioning in various daily activities, compared to when participants were functioning at their best (Lawton and Brody 1969). Participants rated their current and best (i.e., highest previous) ability levels on 11 IADLs (i.e., finances, grocery shopping, cooking, planning social activities, understanding reading material/TV, communication, transportation, shopping, managing medication, childcare, and work) and five basic activities of daily living (BADLs; i.e., housekeeping, home repairs, bathing, dressing, and laundry). For the present study, we used declines in IADLs scores, defined as the sum of the difference scores between the highest level of previous functioning and current functioning on the 11 items assessing IADLs.
The PAOFI is a self-report questionnaire used to measure participants’ perceived functional capacity in their everyday activities across memory, language and communication, higher level cognitive and intellectual functioning, motor, sensory-perceptual ability, and recreation (Chelune et al. 1986). Participants rated themselves using a 6-point Likert-type scale that is anchored at “Almost always” and “Almost never”. Items that obtain a rating of “Fairly often”, “Very often” or “Almost always” are assigned a point. The primary outcome was the number of everyday cognitive symptoms, as represented by the sum of all items, with a higher score indicating more cognitive problems. An additional single item concerning work functioning is included in the PAOFI, which was used to classify participants as either employed (i.e., full- or part-time) or unemployed.
Neurocognitive Impairment
Participants were administered a neuropsychological test battery designed to assess domains sensitive to HIV-associated NCI including verbal fluency, executive function, attention/working memory, episodic memory (learning and delayed recall), speed of information processing, and fine motor skills (Cysique et al. 2011). Raw scores from individual tests were converted to demographically adjusted T-scores, which were converted to global deficit scores, ranging from 0 (T score >39, no impairment) to 5 (T scores <20, severe impairment) (Carey et al. 2004). Global deficit scores greater than or equal to 0.5 were used to classify NCI (Carey et al. 2004).
Psychiatric and Substance Use Characteristics
In order to comprehensively consider the impact of psychiatric characteristics on everyday functioning, we obtained current (last 30 days) and lifetime (prior to the last 30 days) history of major depressive disorder (MDD) and substance use disorders in a subset of our sample (n=534) using structured interviews, which follow the criteria set by the Diagnostic and Statistical Manual of Mental Disorders–Fourth Edition (American Psychiatric Association 1994). Presence of a “substance use disorder” was defined as meeting criteria for either current (last 30 days) or lifetime abuse or dependence for any of the following substances: alcohol, cannabis, methamphetamine, opioids, cocaine, sedatives, and hallucinogens. Current mood was assessed with the original or second version of the Beck Depression Inventory (BDI), and we used appropriate cut points to quantify degree of depressed mood symptoms (Beck et al. 1961; Beck et al. 1996).
Statistical Analyses
Statistical analyses were conducted using a JMP software package (version 12.0.1). To examine the relationship between the VACS index and functional outcomes we initially ran a series of analyses of variances (ANOVAs) on IADL declines and PAOFI total scores, and a Chi-Square test on employment status by VACS Index group. Models that yielded significant VACS Index group differences were followed by pairwise comparisons with adjustments for multiple comparisons, using Tukey’s method. We then examined whether the VACS Index and NCI were independently associated with everyday functioning measures via a series of linear regression models on IADL declines and PAOFI total scores, and a logistic regression model on employment status, with VACS Index group and NCI as predictors. In order to investigate whether demographic (i.e., age, gender, education, race/ethnicity), HIV disease characteristics (i.e. nadir CD4+ count, ART status, months exposure to ART, AIDS status, and duration of infection) or psychiatric comorbidities (i.e. lifetime and current major depressive and substance use disorders, and current depressed mood symptoms) might account for the impact of the VACS Index and NCI on functional outcomes, we first examined the univariable association of each of these covariates with the functional outcomes via a series of independent sample t-tests, ANOVAs, Pearson correlation coefficients or Chi-Square tests, as appropriate. Variables which were associated with the functional outcomes at p<.10 in univariable analyses, were entered into a backward stepwise regression model, along with the VACS Index and NCI. Backward model reduction was done based on Akaike information criterion (AIC), which selects the best set of predictors for a given outcome. Variables selected via this method were included in the final models on IADL declines, PAOFI total scores and employment status.
Results
Demographic factors, HIV disease characteristics, and Psychiatric Conditions
Descriptive characteristics of the study cohort are listed in Table 1. The cohort consisted of a majority of Non-Hispanic White males who were between 18 and 76 years of age, and had between 6 and 20 years of education. Over half of the participants had AIDS and were on ART. Among those on ART, about half had detectable plasma HIV RNA. Approximately half of the sample reported a lifetime history of major depressive disorder, and nearly three quarters of the participants reported a lifetime history of substance use disorder.
Table 1.
Descriptive characteristics of the study cohort (n=670)
| Variable | Descriptive statistic |
|---|---|
| Demographics | |
| Age (years, M [SD]) | 42.7 (10.0) |
| Education (years, M [SD]) | 13.5 (2.5) |
| Sex (% male) | 88.36 |
| Ethnicity (%) | |
| Non-Hispanic White | 62.54 |
| Non-Hispanic Black | 18.36 |
| Hispanic | 13.73 |
| Other | 5.37 |
| HIV disease characteristics | |
| Current CD4+ T-cell count (Median, [IQR]) | 404 (190–605.3) |
| On ART (%) | 66.92 |
| Plasma HIV RNA (% detectable)a | 52.69 |
| Months of Exposure to ART (Median, [IQR]) | 25.4 (1.1–80.4) |
| Nadir CD4+ T-cell count (Median, [IQR]) | 148 (24.8–300) |
| AIDS (% Yes) | 62.88 |
| Duration of infection (years, Median [IQR])b | 9.4 (3.9–15.1) |
| Psychiatric Characteristics (% Yes) | |
| Lifetime Major Depressive Disorderc | 50.57 |
| Current Major Depressive Disorderd | 18.97 |
| Lifetime Substance Use Disorderc | 70.10 |
| Current Substance Use Disorderd | 13.65 |
| Current mood symptoms (%) | |
| Mild | 29.53 |
| Moderate | 17.97 |
| Severe | 7.12 |
| NCI (%) | 38.36 |
| VACS Index scores (Median, [IQR]) | 18 (10–34) |
| VACS Index group (%)e | |
| Low | 28.51 |
| Medium | 46.42 |
| High | 25.08 |
| Everyday functioning Outcomes | |
| IADL declines (Median, [IQR]) | 1 (0–3) |
| PAOFI total score (Median, [IQR]) | 3.5 (1–10) |
| Unemployment (%) | 71.60 |
Note.
Percent detectable among those on ART
n=607
n=534
n=520,
VACS Index group = VACS Index scores were grouped based on IQR; low<10, medium=10–34, high>34.
ART, antiretroviral therapy; IADL, instrumental activities of daily living; NCI, neurocognitive impairment; PAOFI, Patient Assessment of Own Functioning
Association of the VACS Index and NCI to Functional Outcomes
Figures 1a and 1b show means and standard errors on IADL declines and PAOFI total scores, respectively, by VACS Index group. Results from an ANOVA on IADL declines showed a significant effect of VACS Index group, F (2, 667) = 26.71, p< 0.0001. Follow-up pairwise comparisons with Tukey’s correction showed that the high VACS Index group reported significantly more IADL declines compared to both the low VACS Index group (Cohen’s d = 0.68; p< 0.0001) and the medium VACS Index group (Cohen’s d = 0.56; p< 0.0001), with no significant differences between the latter two groups (Cohen’s d = 0.15; p = 0.30).
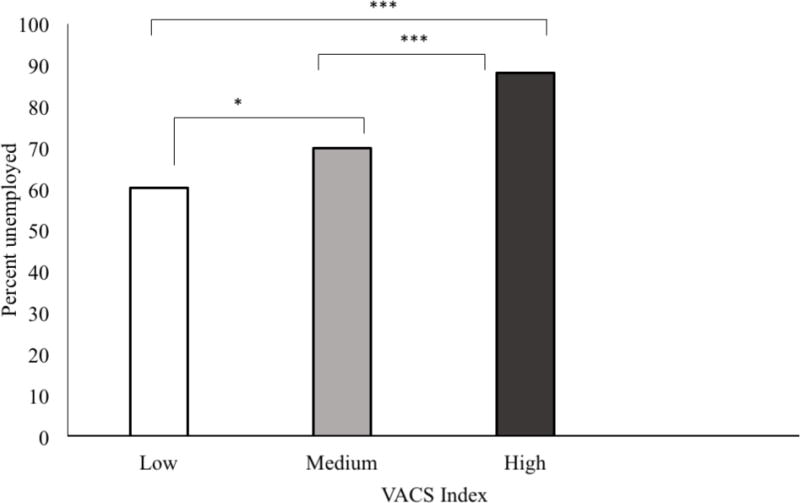
Figure 1.
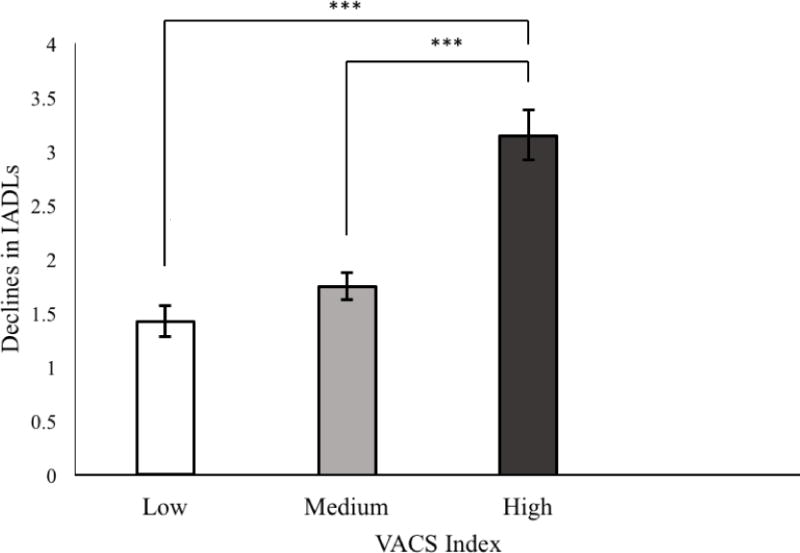
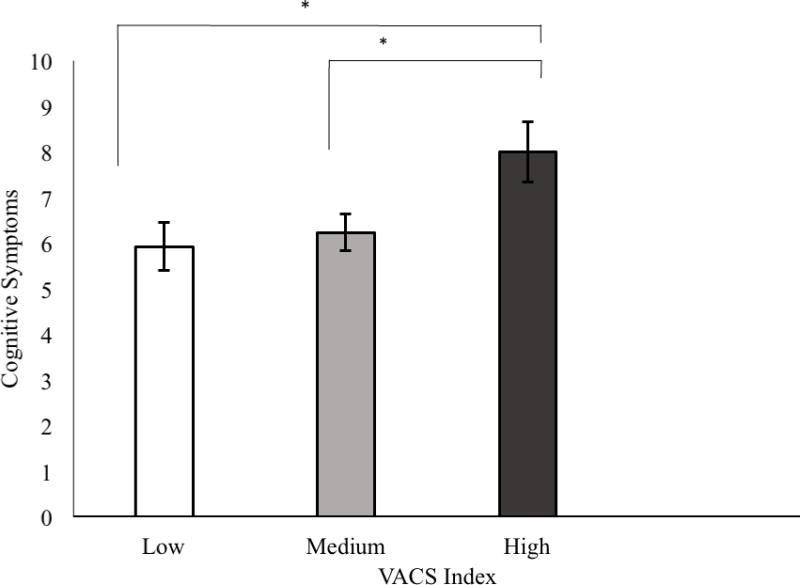
a: Means and standard errors of instrumental activities of daily living (IADL) declines
b: cognitive failures in everyday life
c: percent of unemployment
by Veterans Aging Cohort Study (VACS) Index group.
*p <.05; ** p<.01; *** p<.001
Results from an ANOVA on PAOFI total score showed a significant effect of the VACS Index, F(2, 667) = 4.24, p = 0.02. Follow-up pairwise comparisons with Tukey’s correction showed that the high VACS Index group reported significantly higher PAOFI total scores compared to both the low VACS Index group (Cohen’s d = 0.27; p = 0.02) and the medium VACS Index group (Cohen’s d = 0.23; p= 0.03), with no significant differences between the latter two groups (Cohen’s d = 0.04; p = 0.90).
Figure 1c shows percent of unemployed participants by VACS Index group. Results from Chi Square test showed significant group differences, χ2 = 38.09, df = 2, p< 0.0001. Follow-up analyses showed that there was a higher rate of unemployment in the high VACS Index group compared to the medium VACS Index group (OR = 3.18, CI =1.92 – 5.51, p< 0.0001), which in turn was higher than in the low VACS Index group (OR = 1.53, CI =1.04 – 2.23, p = 0.03). The High VACS Index group also had significantly higher rates of unemployment than the low VACS Index Group (OR = 4.86, CI =2.85 – 8.60, p< 0.0001)
Results from separate regression models on IADL declines, PAOFI total scores and unemployment, including the VACS Index and NCI as sole predictors, showed significant independent effects of VACS Index group and NCI (Table 2). The high VACS Index group reported significantly more IADL declines, perceived cognitive failures in daily life and unemployment than the low and medium VACS Index groups. The medium VACS Index group also showed higher unemployment than the low VACS Index group, with no significant group differences on other everyday functioning outcomes. The presence of NCI was significantly and independently associated with more IADL declines and cognitive failures in daily life, as well as higher unemployment.
Table 2.
Association of the VACS Index and NCI to functional outcomes (n=670)
| IADL declinesa | PAOFI total scoreb | Unemploymentc | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| Estimate (SE) | P | Estimate (SE) | p | OR (CI) | p | |
| Intercept | 2.78 (0.20) | — | 6.67 (0.63) | — | — | — |
| VACS Index [low]d | −1.62 (0.25) | <0.0001 | −1.70 (0.77) | 0.03 | 0.22 (0.12 – 0.38) | <0.0001 |
| VACS Index [medium]d | −1.30 (0.22) | <0.0001 | −1.42 (0.69) | 0.04 | 0.34 (0.19 – 0.56) | <0.0001 |
| NCI | 0.75 (0.19) | <0.0001 | 2.75 (0.58) | <0.0001 | 2.04 (1.40 – 3.00) | <0.001 |
Overall model: F (3, 669) = 23.44, p<.0001, Adj R2 = 0.09, pairwise comparisons; Low VACS Index group (compared to medium), Estimate = 0.32, SE = 0.23, p=.31
Overall model: F (3, 669) = 10.39, p<.0001, Adj R2 = 0.04,, pairwise comparisons; Low VACS Index group (compared to medium), Estimate = 0.28, SE = 0.67, p=.91
Overall model: X2(3)=52.22, p<.0001, pairwise comparisons; Low VACS Index group (compared to medium), OR=0.65(0.44–0.96), p=.03
Reference group = high VACS Index
We then examined whether covariates might account for the impact of the VACS Index and NCI on everyday functioning outcomes. Covariates associated with IADL declines in univariable analyses (at p< 0.10) included lower education, lower nadir CD4, AIDS status, increased current depressed mood symptoms, and history of lifetime and current major depressive disorder. These variables were entered into a stepwise regression on IADL declines, which selected all of the aforementioned covariates to be included in the final model, except for AIDS status and current major depressive disorder. Results from the final model (F [9, 430] = 19.19, p< 0.001, Adj R2 =.0 28) showed that both the VACS Index (p< 0.001) and NCI (p = 0.02) continued to be independently associated with IADL declines, as did most of the covariates (i.e., nadir CD4, current depressed mood symptoms, and lifetime history of major depression; ps < 0.01).
Covariates associated with PAOFI total scores in univariable analyses (at p< 0.10) were older age, lower education, lower nadir CD4, AIDS status, increased current depressed mood symptoms, and history of lifetime and current major depressive disorder and lifetime substance use disorder. These variables were included in a stepwise regression on PAOFI total scores, which selected all of these covariates except for AIDS status and current major depressive disorder. Results from the final model (F [11, 430]=24.24, p<0.001, Adj R2=.37) showed that NCI (p=0.02) continued to be independently associated with higher cognitive symptoms, and the medium VACS Index group reported significantly fewer cognitive symptoms than the high VACS Index group (p = 0.03), with no other significant VACS Index group differences. The covariates that were independently associated with cognitive failures in everyday life in this final analysis included age, education, and current mood symptoms (p<0.001).
Covariates associated with unemployment in univariable analyses (at p<0.10) included older age, lower education, lower nadir CD4, AIDS, ART status (on/off), duration of exposure to ART, worse current mood symptoms, lifetime and current major depressive disorder. Stepwise regression analyses assessing the association of the VACS Index and NCI to unemployment, selected age, education, AIDS status, duration of exposure to ART, and current mood symptoms to be included as covariates. Results from the final model (X2[10] = 82.27, p< 0.0001) showed that both the VACS Index (p< 0.01) and NCI (p = 0.02) continued to be independently associated with unemployment, as was lower education, AIDS status and worse current depressed mood symptoms (ps< 0.01).
Discussion
The VACS Index, a composite including age, HIV biomarkers, and biomarkers of multi-organ system dysfunction, has been previously linked to dependence in IADLs and ART nonadherence (John et al. 2016). Results from the present study extend these prior findings to other functional outcomes. Specifically, we found that higher VACS Index scores were associated with increased cognitive symptoms in everyday life and unemployment, in addition to more declines in IADLs. Present findings also show that the previously found link between the VACS Index and IADLs, remained after considering the impact of NCI, a well-established predictor of everyday functioning in HIV. Furthermore, both the VACS Index and NCI were independently associated with worse functional outcomes, even after adjusting for significant covariates, including demographics, HIV disease characteristics not included in the VACS Index and psychiatric comorbidities.
While higher VACS Index scores were associated with worse everyday functioning in all domains of functional status that were assessed (i.e., IADL declines, cognitive symptoms and unemployment), the most notable group differences were found between participants with high VACS Index scores compared to those with low and medium VACS Index scores. This suggests that participants with VACS Index scores in the uppermost quartile of our sample might be particularly vulnerable to everyday functioning problems. These results are consistent with prior findings by our group, showing that high VACS Index scores were the most predictive of concurrent NCI and neurocognitive decline (Marquine, Montoya, et al. 2016; Marquine et al. 2014). Additionally, effect sizes on the association of the VACS Index to IADL declines tended to be medium to large, and participants in the high VACS Index group were three to four times more likely to be unemployed than those in the low and medium VACS Index groups, respectively. In contrast, effect sizes on the association of the VACS Index to the perception of cognitive failures in everyday life, were small to medium, and tended to be less notable than for the other functional outcomes. These results indicate that the strength of the association between the VACS Index and functional outcomes might differ depending on the specific area of functioning assessed.
Both the VACS Index and NCI were independent predictors of everyday functioning for all outcomes, suggesting that the association between the VACS Index and everyday functioning cannot be fully explained by NCI. This is notable in light of prior findings based on separate studies that had found the VACS Index to be associated with NCI (Marquine, Montoya, et al. 2016; Marquine et al. 2014) and functional outcomes (John et al. 2016). These independent effects remained after adjusting for significant covariates, indicating that the combined effect of HIV disease burden and medical comorbidities, and NCI are all important factors driving everyday functioning problems in HIV.
In addition to the VACS Index and NCI, depressed mood was also an independent predictor for all functional outcomes. This is consistent with prior studies (Morgan et al. 2012; Rabkin 2008; Rourke et al. 1999), and highlights the important role that psychological factors might have on everyday functioning. Given the cross-sectional design of the present study, however, it might also be the case that increased difficulties in everyday functioning might lead a person to become increasingly depressed. Our cross-sectional data do not permit teasing apart the relative onset of depression symptoms versus declines in everyday functioning. Future research efforts to investigate the temporal relationship between everyday functioning outcomes and depression are warranted.
Historical HIV disease characteristics, such as nadir CD4 and AIDS, were also independent predictors for some of the outcomes (i.e., nadir CD4 for IADL declines, and AIDS for unemployment). This is also consistent with prior findings (Morgan et al. 2012), and underscores the importance of considering these historical HIV disease factors in addition to current health status, when assessing functional outcomes in HIV-infected persons.
The fact that NCI, and certain demographics, historical HIV disease characteristics and psychiatric comorbidities were independently associated with functional outcomes, after accounting for the VACS Index, suggests that these factors, which are not included in the VACS Index might improve its predictive utility for functional outcomes in HIV. Furthermore, while not investigated in the present study, the predictive accuracy of the VACS Index for functional outcomes might improve with the addition of biomarkers of inflammation. Several studies have found that fibrin degradation product, D-dimer, adds to the accuracy of the VACS Index for mortality(Justice et al. 2012; So-Armah et al. 2016). Perhaps the addition of other biomarkers of inflammation, monocyte activation, and coagulation that are usually associated with neurocognitive decline (e.g. blood levels of interleukin-6, soluble CD14) could add to the VACS Index’s predictive accuracy of neurocognitive and functional outcomes (So-Armah et al. 2016; Turchan et al. 2003).
Our study had several limitations. We had very few participants who were over the age of 65 or female. Also, prior findings showed that the association of the VACS Index to NCI was weaker among Hispanics (Marquine, Sakamoto, et al. 2016). Because of the relatively small percent of Hispanics in the present study, we were not able to investigate whether our findings differed by ethnic group, and caution is warranted when generalizing our findings to segments of the U.S. HIV-infected population that are not fully represented in the present study. As noted above, we cannot infer causality in the present study given its cross-sectional nature. An important next step would be to examine the predictive accuracy of the VACS index for functional outcomes via a longitudinal study design in a sample that includes a larger, older, and more diverse sample, which includes a sizeable number of women. It would also be important to assess everyday functioning via other type of measures that might augment participant’s self report, such as the utilization of informants’ report and of performance-based measures of everyday functioning.
Overall, we have extended initial evidence linking the VACS Index to everyday functioning, an important patient outcome in HIV. Given that the VACS Index uses regularly collected biomarkers, it can be a useful tool for clinicians to assess the degree to which HIV-infected patients might be at high risk for everyday functioning problems. Considering additional factors, such as NCI, historical HIV disease characteristics, and current mood, might be particularly helpful in determining functional status among HIV-infected persons.
Acknowledgments
This work was supported by the National Institutes of Health [grant numbers R01MH099987, P30MH062512, U01MH083506, R24MH59745, P01DA12065, K23MH105297, R25AG043364].
Footnotes
Conflicts of Interest
The authors declare that they have no conflict of interest.
References
- Akgun KM, Tate JP, Crothers K, Crystal S, Leaf DA, Womack J, Brown TT, Justice AC, Oursler KK. An adapted frailty-related phenotype and the VACS index as predictors of hospitalization and mortality in HIV-infected and uninfected individuals. J Acquir Immune Defic Syndr. 2014;67(4):397–404. doi: 10.1097/QAI.0000000000000341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th. Washington; DC: 1994. [Google Scholar]
- Beck AT, Erbaugh J, Ward CH, Mock J, Mendelsohn M. An inventory for measuring depression. Arch Gen Psychiat. 1961;4(6):561. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Ball R, Ranieri WF. Comparison of Beck Depression Inventories-IA and -II in psychiatric outpatients. Journal of Personality Assessment. 1996;67(3):588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Blaum CS, Ofstedal MB, Liang J. Low cognitive performance, comorbid disease, and task-specific disability: Findings from a nationally representative survey. J Gerontol a-Biol. 2002;57(8):M523–M531. doi: 10.1093/gerona/57.8.m523. [DOI] [PubMed] [Google Scholar]
- Carey CL, Woods SP, Gonzalez R, Conover E, Marcotte TD, Grant I, Heaton RK, the HNRC Group Predictive validity of global deficit scores in detecting neuropsychological impairment in HIV infection. Journal of Clinical and Experimental Neuropsychology. 2004;26(3):307–319. doi: 10.1080/13803390490510031. [DOI] [PubMed] [Google Scholar]
- Chelune GJ, Heaton RK, Lehman RA. Neuropsychological and personality correlates of patients complaints of disability. New York: Plenum Press; 1986. [Google Scholar]
- Cysique LA, Franklin D, Abramson I, Ellis RJ, Letendre S, Collier A, Clifford D, Gelman B, McArthur J, Morgello S, Simpson D, McCutchan JA, Grant I, Heaton RK, Grp C & Grp H Normative data and validation of a regression based summary score for assessing meaningful neuropsychological change. Journal of Clinical and Experimental Neuropsychology. 2011;33(5):505–522. doi: 10.1080/13803395.2010.535504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deeks SG, Phillips AN. HIV infection, antiretroviral treatment, ageing, and non-AIDS related morbidity. Brit Med J. 2009;338 doi: 10.1136/bmj.a3172. [DOI] [PubMed] [Google Scholar]
- Heaton RK, Grant I, Butters N, White DA, Kirson D, Atkinson JH, McCutchan JA, Taylor MJ, Kelly MD, Ellis RJ, Wolfson T, Velin R, Marcotte TD, Hesselink JR, Jernigan TL, Chandler J, Wallace M, Abramson I, the HNRC Group The HNRC 500–neuropsychology of HIV infection at different disease stages. HIV Neurobehavioral Research Center. Journal of the International Neuropsychological Society. 1995;1(3):231–251. doi: 10.1017/s1355617700000230. [DOI] [PubMed] [Google Scholar]
- Heaton RK, Marcotte TD, Mindt MR, Sadek J, Moore DJ, Bentley H, McCutchan JA, Reicks C, Grant I, the HNRC Group The impact of HIV-associated neuropsychological impairment on everyday functioning. Journal of the International Neuropsychological Society. 2004;10(3):317–331. doi: 10.1017/S1355617704102130. [DOI] [PubMed] [Google Scholar]
- John MD, Greene M, Hessol NA, Zepf R, Parrott AH, Foreman C, Bourgeois J, Gandhi M, Hare CB. Geriatric assessments and association with VACS Index among HIV-infected older adults in San Francisco. JAIDS. 2016;72(5):534–541. doi: 10.1097/QAI.0000000000001009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Justice AC, Freiberg MS, Tracy R, Kuller L, Tate JP, Goetz MB, Fiellin DA, Vanasse GJ, Butt AA, Rodriguez-Barradas MC, Gibert C, Oursler KA, Deeks SG, Bryant K, Team VP Does an index composed of clinical data reflect effects of inflammation, coagulation, and monocyte activation on mortality among those aging with HIV? Clin Infect Dis. 2012;54(7):984–994. doi: 10.1093/cid/cir989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Justice AC, McGinnis KA, Skanderson M, Chang CC, Gibert CL, Goetz MB, Rimland D, Rodriguez-Barradas MC, Oursler KK, Brown ST, Braithwaite RS, May M, Covinsky KE, Roberts MS, Fultz SL, Bryant KJ, Team VP Towards a combined prognostic index for survival in HIV infection: The role of ‘non-HIV’ biomarkers. Hiv Med. 2010;11(2):143–151. doi: 10.1111/j.1468-1293.2009.00757.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Justice AC, PM S, Tate JP, Althoff KN, Jacobson LP, Gebo KA, Kitahata MM, Horberg MA, Brooks JT, Buchacz K, Rourke SB, Rachlis A, Napravnik S, Eron J, Willig JH, Moore R, Kirk GD, Bosch R, Rodriguez B, Hogg RS, Thorne J, Goedert JJ, Klein M, Gill J, Deeks S, Sterling TR, Anastos K, Gange SJ. Predictive accuracy of the Veterans Aging Cohort Study Index for mortality with HIV infection: A North American cross cohort analysis. J Acquir Immune Defic Syndr. 2013;62(2):149–163. doi: 10.1097/QAI.0b013e31827df36c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–186. [PubMed] [Google Scholar]
- Mahy M, Autenrieth CS, Stanecki K, Wynd S. Increasing trends in HIV prevalence among people aged 50 years and older: Evidence from estimates and survey data. AIDS. 2014;28:S453–S459. doi: 10.1097/QAD.0000000000000479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcotte TD, Wolfson T, Rosenthal TJ, Heaton RK, Gonzalez R, Ellis RJ, Grant I, Grp HNRC A multimodal assessment of driving performance in HIV infection. Neurology. 2004;63(8):1417–1422. doi: 10.1212/01.wnl.0000141920.33580.5d. [DOI] [PubMed] [Google Scholar]
- Marquine MJ, Montoya JL, Umlauf A, Fazeli PL, Gouaux B, Heaton RK, Ellis RJ, Letendre SL, Grant I, Moore DJ, Group HIVNRP The Veterans Aging Cohort Study (VACS) Index and Neurocognitive Change: A Longitudinal Study. Clin Infect Dis. 2016;63(5):694–702. doi: 10.1093/cid/ciw328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquine MJ, Sakamoto M, Dufour C, Rooney A, Fazeli P, Umlauf A, Gouaux B, Franklin D, Ellis R, Letendre S, Cherner M, Heaton RK, Grant I, Moore DJ, Group H The impact of ethnicity/race on the association between the Veterans Aging Cohort Study (VACS) Index and neurocognitive function among HIV-infected persons. J Neurovirol. 2016;22(4):442–454. doi: 10.1007/s13365-015-0411-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquine MJ, Umlauf A, Rooney AS, Fazeli PL, Gouaux BD, Paul Woods S, Letendre SL, Ellis RJ, Grant I, Moore DJ, Group HIVNRP The Veterans Aging Cohort Study Index is associated with concurrent risk for neurocognitive impairment. J Acquir Immune Defic Syndr. 2014;65(2):190–197. doi: 10.1097/QAI.0000000000000008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore RC, Paolillo EW, Heaton A, Fazeli PL, Jeste DV, Moore DJ. Clinical utility of the UCSD Performance-Based Skills Assessment-Brief (UPSA-B) in adults living with HIV: Associations with neuropsychological impairment and patient-reported everyday functioning difficulties. Plos One. 2017;12(8):e0183614. doi: 10.1371/journal.pone.0183614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan EE, Iudicello JE, Weber E, Duarte NA, Riggs PK, Delano-Wood L, Ellis R, Grant I, Woods SP, HNRP Synergistic effects of HIV infection and older age on daily functioning. JAIDS. 2012;61(3):341–348. doi: 10.1097/QAI.0b013e31826bfc53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabkin JG. HIV and depression: 2008 review and update. Current HIV/AIDS reports. 2008;5(4):163–171. doi: 10.1007/s11904-008-0025-1. [DOI] [PubMed] [Google Scholar]
- Rippeth JD, Heaton RK, Carey CL, Marcotte TD, Moore DJ, Gonzalez R, Wolfson T, Grant I, the HNRC Group Methamphetamine dependence increases risk of neuropsychological impairment in HIV infected persons. Journal of the International Neuropsychological Society. 2004;10(1):1–14. doi: 10.1017/S1355617704101021. [DOI] [PubMed] [Google Scholar]
- Rourke SB, Halman MH, Bassel C. Neurocognitive complaints in HIV-infection and their relationship to depressive symptoms and neuropsychological functioning. Journal of Clinical and Experimental Neuropsychology. 1999;21(6):737–756. doi: 10.1076/jcen.21.6.737.863. [DOI] [PubMed] [Google Scholar]
- So-Armah KA, Tate JP, Chang CCH, Butt AA, Gerschenson M, Gibert CL, Leaf D, Rimland D, Rodriguez-Barradas MC, Budoff MJ, Samet JH, Kuller LH, Deeks SG, Crothers K, Tracy RP, Crane HM, Sajadi MM, Tindle HA, Justice AC, Freiberg MS, Team VP Do biomarkers of inflammation, monocyte activation, and altered coagulation explain excess mortality between HIV infected and uninfected people? JAIDS. 2016;72(2):206–213. doi: 10.1097/QAI.0000000000000954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tate JP, Justice AC, Hughes MD, Bonnet F, Reiss P, Mocroft A, Nattermann J, Lampe FC, Bucher HC, Sterling TR, Crane HM, Kitahata MM, May M, Sterne JA. An internationally generalizable risk index for mortality after one year of antiretroviral therapy. AIDS. 2013;27(4):563–572. doi: 10.1097/QAD.0b013e32835b8c7f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turchan J, Pocernich CB, Gairola C, Chauhan A, Schifitto G, Butterfield DA, Buch S, Narayan O, Sinai A, Geiger J, Berger JR, Elford H, Nath A. Oxidative stress in HIV demented patients and protection ex vivo with novel antioxidants. Neurology. 2003;60(2):307–314. doi: 10.1212/01.wnl.0000042048.85204.3d. [DOI] [PubMed] [Google Scholar]
- Vance DE, Fazeli PL, Ball DA, Slater LZ, Ross LA. Cognitive functioning and driving simulator performance in middle-aged and older adults with HIV. The Journal of the Association of Nurses in AIDS Care: JANAC. 2014;25(2):e11–26. doi: 10.1016/j.jana.2013.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vance DE, Fazeli PL, Gakumo CA. The impact of neuropsychological performance on everyday functioning between older and younger adults with and without HIV. The Journal of the Association of Nurses in AIDS Care: JANAC. 2013;24(2):112–125. doi: 10.1016/j.jana.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Womack JA, Goulet JL, Gibert C, Brandt CA, Skanderson M, Gulanski B, Rimland D, Rodriguez-Barradas MC, Tate J, Yin MT, Justice AC, Veterans Aging Cohort Study Project, T Physiologic frailty and fragility fracture in HIV-infected male veterans. Clin Infect Dis. 2013;56(10):1498–1504. doi: 10.1093/cid/cit056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods SP, Rippeth JD, Frol AB, Levy JK, Ryan E, Soukup VM, Hinkin CH, Lazzaretto D, Cherner M, Marcotte TD, Gelman BB, Morgello S, Singer EJ, Grant I, Heaton RK. Interrater reliability of clinical ratings and neurocognitive diagnoses in HIV. J Clin Exp Neuropsychol. 2004;26(6):759–778. doi: 10.1080/13803390490509565. [DOI] [PubMed] [Google Scholar]


