Abstract
BACKGROUND
Hospital readmission is a significant problem for patients with complex chronic illnesses such as liver cirrhosis.
PURPOSE
We aimed to describe the range of readmission risk in patients with cirrhosis and the impact of the model for end-stage liver disease (MELD) score.
DATA SOURCES
We conducted a systematic review of studies identified in Ovid MEDLINE, PubMed, EMBASE, CINAHL, the Cochrane Library, Scopus, Google Scholar, and ClinicalTrials.gov from 2000 to May 2017.
STUDY SELECTION
We examined studies that reported early readmissions (up to 90 days) in patients with cirrhosis. Studies were excluded if they did not examine the association between readmission and at least 1 variable or intervention.
DATA EXTRACTION
Two reviewers independently extracted data on study design, setting, population, interventions, comparisons, and detailed information on readmissions.
DATA SYNTHESIS
Of the 1363 records reviewed, 26 studies met the inclusion and exclusion criteria. Of these studies, 21 were retrospective, and there was significant variation in the inclusion and exclusion criteria. The pooled estimate of 30-day readmissions was 26%(95% confidence interval [CI], 22%–30%). Few studies examined readmission preventability or the relationship between readmissions and social determinants of health. Reasons for readmission were highly variable. An increased MELD score was associated with readmissions in most studies. Readmission was associated with increased mortality.
CONCLUSION
Hospital readmissions frequently occur in patients with cirrhosis and are associated with liver disease severity. The impact of functional and social factors on readmissions is unclear.
Cirrhosis is a morbid condition characterized by complications such as ascites, gastrointestinal bleeding, and hepatic encephalopathy. These complications frequently require hospitalization, which is a substantial burden to the healthcare system. In 2012, liver disease was responsible for nearly 250,000 admissions across the United States, costing $3 billion.1 Despite this substantial resource utilization, outcomes remain poor, with an inpatient mortality of 6%. For those that survive, many experience hospital readmission.
More generally, early readmission reflects poor quality of care in the US. In 2004, 30-day readmissions occurred in nearly 20% of Medicare beneficiaries and costed over $17 billion.2 In response to this problem, the Affordable Care Act established the Hospital Readmissions Reduction Program (HRRP), which reduces Centers for Medicare & Medicaid Services (CMS) payments to hospitals with excess 30-day readmissions for high-risk conditions, including pneumonia and heart failure.3 Heart failure, in particular, has been the subject of numerous studies detailing risk factors and interventions to predict and prevent readmission.4–6 Based on this extensive evidence, guidelines recommend disease management programs to reduce readmissions in this population.7 In contrast, readmission in the cirrhosis population has received limited attention.
We therefore conducted a systematic review aiming to examine the range of readmission risk noted in the literature, with a focus on the model for end-stage liver disease (MELD) score as a risk factor for readmission.
METHODS
Search Strategy
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines for conducting and reporting systematic reviews.8 A literature search was performed by a medical librarian using the following databases: Ovid MEDLINE, PubMed, EMBASE, CINAHL, the full Cochrane Library, Scopus, Google Scholar, and ClinicalTrials.gov. All the databases were searched from 2000 to May 2017. We did not include older reports because the review focused on contemporary care; earlier studies may not reflect current cirrhosis management. To ensure literature saturation, included articles’ reference lists were reviewed.
Search strategies were developed by combining database-specific subject headings and keywords for readmissions with those for cirrhosis or its complications (Supplementary Material). Google Scholar and ClinicalTrials.gov were searched using keywords only. All results were limited to the English language and those published in 2000 or later, but no other limits were applied.
Identified records were reviewed based on strict criteria. We excluded case reports, case series, reviews, editorials, letters, and meeting abstracts without final peer-reviewed publication. We also excluded studies of pediatric populations (age < 18 years), patients without cirrhosis, and patients with liver transplants. We excluded studies in which patients were not hospitalized at study onset and those where the index admission was for an elective procedure. Because our interest was to identify factors associated with early readmission, we excluded studies that did not report readmissions within 90 days or those with a mean or median follow-up of less than 30 days. We also excluded studies that did not examine the association between readmission and at least 1 independent variable or intervention. Duplicate reports of a common sample were excluded unless the duplicate provided additional information, and such reports were examined together in our synthesis.
Two authors identified potentially eligible records by independently screening titles and abstracts. At this stage, records that did not meet the eligibility criteria were excluded, and the reasons for exclusion were not recorded. Records with disagreement were retained for full-text review. After this initial exclusion of records, the remaining full-text records were reviewed independently. For this full-text review, we recorded exclusion reasons and disagreements were resolved through discussion.
Data Collection
Data were abstracted from each study by 2 authors independently and recorded in a REDCap database.9 Discrepancies were resolved through discussion. We recorded study characteristics, including study design, setting, population (including the inclusion/exclusion criteria, sample size, and patient and hospitalization characteristics), interventions, and comparisons. To facilitate comparisons across studies, we employed validated methods to approximate means and standard deviations (SD).10 We recorded detailed information on outcomes including readmissions, preventability, independent variables, and mortality. Studies that focused on a single independent factor or intervention were classified as “focused,” while those that examined multiple factors were classified as “broad.” We used the Newcastle–Ottawa Scale to assess the risk of bias in each study.11 This instrument uses a 9-point scale to gauge methodological quality based on selection, group comparability, and exposure/outcome assessment.
Statistical Analysis
Analyses were performed using Stata 13.1 (StataCorp LP, College Station, Texas). We determined the pooled proportion of patients with 30-day readmission using a random-effects model, with the Freeman–Tukey double-arcsine transformation for meta-analysis of proportions.12 We investigated the heterogeneity by stratifying analyses according to prespecified study characteristics, including “broad” versus “focused.” However, the readmission risk was not different in the stratified analysis; therefore, we chose to pool the findings. For point estimates, 95% confidence intervals (CIs) were calculated, and a P-value < .05 was considered statistically significant.
RESULTS
Search Results
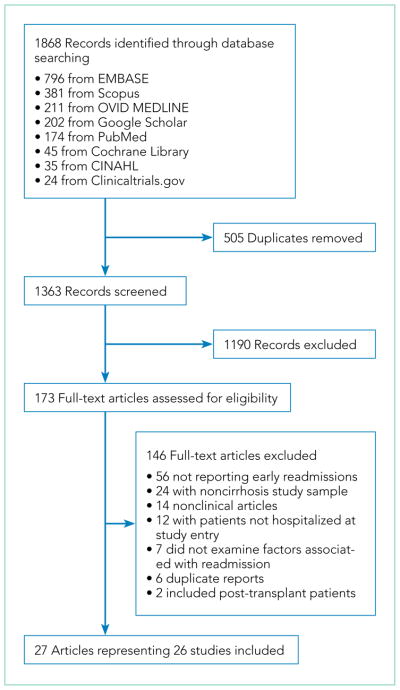
The initial search yielded 1363 records, of which 173 full-text articles were assessed for eligibility. Twenty-seven articles representing 26 studies of 180,049 patients were included (Figure 1).13–39
FIG 1.
Study flow.
Study Characteristics
Two studies were performed in Australia, 4 in Europe, and the remainder in North America. Twenty one of the 26 studies were retrospective cohort studies (Table 1). Twenty studies were single-center studies (of which half were performed at transplant centers), and 4 of the 6 multicenter studies were based on administrative data with large samples (173,254 patients). The inclusion/exclusion criteria varied widely (Supplementary Material). Some studies only included patients admitted for specific cirrhosis complications, while others included those admitted for any reason. Two studies excluded patients admitted in the prior 30 days, and 6 excluded patients discharged to hospice. The mean risk of bias score was 7.5 (SD 1.3) out of a possible 9 points, with most lacking an adequate description of follow-up and several lacking adjustment for confounders.
TABLE 1.
Study Characteristics
| Study | Study Design | Sample Size | Age (mean) | Males (%) | MELD (mean) | 30-day Readmissions, 95% CI (%) |
|---|---|---|---|---|---|---|
| Bini 200113 | Prospective cohort | 197 | 57 | 97 | NR | 20 (15–26) |
| Berman 201114 | Retrospective cohort | 554 | 54 | 57 | 19 | 20 (17–24) |
| Johnson 201115 | Quasi-experimental | 99 | 54 | 67 | NR | 27 (19–36) |
| Volk 201216 | Retrospective cohort | 402 | 54 | 57 | 19 | 37 (32–42) |
| Barsuk 201317 | Retrospective cohort | 502 | 57 | 60 | 23 | 44 (39–48) |
| Deitelzweig 201318 | Retrospective cohort | 21,864 | 55 | 64 | NR | 28 (27–29) |
| Morando 201319 | Quasi-experimental | 100 | 60 | 58 | 16 | 32 (23–41) |
| Singal 201320 | Retrospective cohort | 836 | 53 | 68 | 15 | 27 (24–30) |
| Desai 201421 | Quasi-experimental | 56 | 57 | 63 | 22 | 25 (16–38) |
| Fagan 201422 | Retrospective cohort | 41 | 54 | 78 | 17 | 42 (29–58) |
| Gaduputi 201423 | Retrospective cohort | 447 | 60 | 66 | 12 | 28 (24–32) |
| Ghaoui 2014/201524, 25 | Quasi-experimental | 303 | 54 | 60 | 16 | 36 (31–42) |
| Agrawal 201526 | Retrospective cohort | 111 | 59 | 98 | 14 | 27 (20–36) |
| Tapper 201527 | Retrospective cohort | 734 | 57 | 62 | 18 | 32 (29–36) |
| Atla 201628 | Retrospective cohort | 189 | 54 | 69 | 12 | 50 (43–57) |
| Bajaj 201629 | Prospective cohort | 1013 | 57 | 64 | 18 | NR |
| Courson 201630 | Retrospective cohort | 149 | 59 | 60 | 20 | 24 (17–31) |
| Graupera 201631 | Prospective cohort | 218 | 60 | 65 | 16 | NR |
| Kanwal 201632 | Retrospective cohort | 25,217 | 62 | 97 | NR | 14 (13–14) |
| Le 201633 | Retrospective cohort | 302 | 57 | 69 | 15 | 29 (24–34) |
| Moon 201634 | Retrospective cohort | 6451 | 61 | 97 | 12 | 22 (21–23) |
| Rassameehiran 201635 | Retrospective cohort | 140 | 56 | 62 | 18 | 10 (6–16) |
| Tapper 201636 | Retrospective cohort | 119,722 | 61 | 56 | NR | 13 (13–13) |
| Lyon 201737 | Retrospective cohort | 226 | 57 | 62 | 21 | 10 (6–14) |
| Morales 201738 | Retrospective cohort | 112 | 65 | 57 | 15 | 30 (22–39) |
| Strömdahl 201739 | Retrospective cohort | 64 | 58 | 74 | NR | 19 (11–30) |
Abbreviations: CI, confidence index; MELD, Model for End-Stage Liver Disease; NR, not reported.
The mean age of patients ranged from 53 to 65 years, and males comprised 56%–78% (except for 4 Veterans Affairs studies). The mean MELD score ranged from 12 to 23. Hepatitis C accounted for 14%–100% of cirrhosis, alcohol accounted for 25%–67%, and nonalcoholic fatty liver disease accounted for 0%–20%. Hepatocellular carcinoma was present in 6%–30% of the patients. Reasons for the index admission varied widely and were dependent on the inclusion/exclusion criteria.
Outcomes
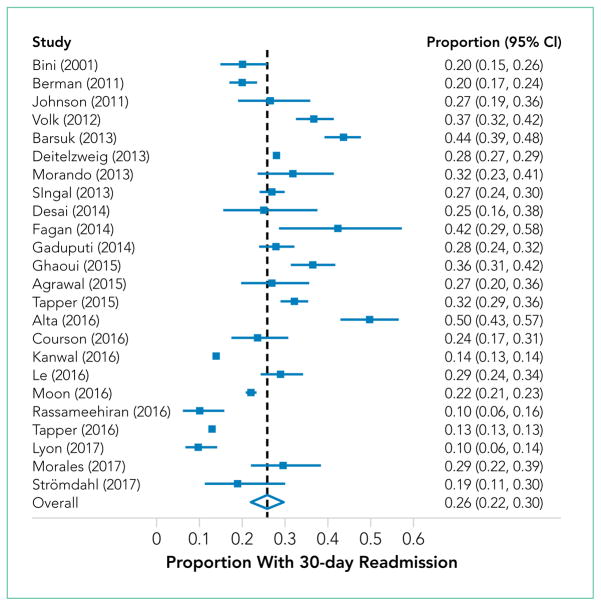
Thirty-day readmissions ranged from 10% to 50%, with a pooled estimate of 26% (95% CI, 22%–30%; Figure 2). Five studies reported 90-day readmissions, ranging from 21% to 71%.29,31,33,35,36 Only 4 of the 20 single-center studies captured readmissions at centers aside from the index admission hospital. Two studies assessed readmission preventability: 1 through independent chart review by 2 physicians (22% preventable), the other based on the judgement of 1 physician (37%).16,26 Reasons for readmission were reported in 12 studies and were highly variable: hepatic encephalopathy in 6%–100%, ascites/volume overload in 2%–38%, and decompensated liver disease (without further elaboration) in 25%–100%. The studies that focused on single risk factors or interventions reported a wide range of possible readmission risk factors, ranging from biomarkers to clinical processes of care. Although multiple putative risk factors were reported, few conclusions can be drawn due to the heterogeneity in the findings. In 5 studies, 90-day mortality was reported and ranged from 10.3% to 18.6%. The relationship between readmission and subsequent mortality was examined in 5 studies, and all were statistically significant.14,16,20,33,38
FIG 2.
Forest plot of the proportion of patients with cirrhosis with a 30-day hospital readmission.
Readmission and MELD
The MELD score was examined in numerous studies as a risk factor for readmissions and was found to be significantly associated with readmission in most studies (Table 2). Notably, even small differences in the MELD score are associated with a higher risk for readmission, though no cutoff point can be discerned. In addition, this association is seen regardless whether the MELD score is assessed at index admission or discharge. Several studies did not report the absolute differences in the MELD score listed in Table 2, but did find associations between increased MELD score and readmission in adjusted models.16,20,27,34 One study found that a higher MELD score was associated with decreased readmissions over 6 months, but this study did not account for the competing risk of death.37
TABLE 2.
Comparison of MELD Scores According to Readmission Status
| Index Admission MELD Score
|
Index Discharge MELD sScore
|
||||||
|---|---|---|---|---|---|---|---|
| Study | Outcome | Not Readmitted | Readmitted | P Value | Not Readmitted | Readmitted | P Value |
| Berman 201114 | 30-day readmission | NR | NR | 17.8 (6.4) | 20.4 (8.5) | .001 | |
|
| |||||||
| Fagan 201422 | 30-day readmission | 14.5 (6.0) | 18.9 (7.7) | .03 | NR | NR | |
|
| |||||||
| Agrawal 201526 | 30-day readmission | NR | NR | 13.4 (4.5) | 14.8 (4.6) | NS | |
|
| |||||||
| Atla 201628 | 30-day readmission | 9.8 (3.2) | 13.1 (6.7) | .001 | NR | NR | |
|
| |||||||
| Bajaj 201629 | 90-day readmission | 17.2 (6.6) | 19.0 (6.6) | .0001 | 16.3 (6.6) | 18.7 (6.5) | .0001 |
|
| |||||||
| Graupera 201631 | 90-day readmission | 15 (7) | 18 (7) | .003 | NR | NR | |
|
| |||||||
| Rassameehiran 201635 | 90-day readmission | 16.7 (7.0) | 17.8 (6.4) | .41 | NR | NR | |
|
| |||||||
| Morales 201738,a | 30-day readmission | NR | NR | 13.8 (4.6) | 16.9 (5.0) | .002 | |
The study by Morales et al. examined the discharge MELD-sodium score in relation to 30-day readmission.
NR; not reported.
DISCUSSION
Hospital readmission is a costly and common problem in the US.2 In addition to the negative impact that readmissions have on patients’ lives,40 readmissions are increasingly being used to measure quality. Unplanned 30-day readmissions are posted publicly, and excess readmissions for high-risk conditions are penalized through HRRP.3 Although HRRP does not currently include cirrhosis, the program has expanded to include several conditions that were not included in the initial iteration. Whether cirrhosis will be included in future iterations remains to be seen; however, increasing scrutiny is likely to continue. Of specific populations at risk, patients with cirrhosis are particularly vulnerable due to several features. Ascites management often requires hospitalization due to diuretic titration and poor access to paracentesis, and hepatic encephalopathy treatment requires complex lactulose titration.16 Other features of cirrhosis, such as gastrointestinal bleeding, infections, and renal failure, also place patients at risk of poor outcomes. The resulting readmission burden is high, with a pooled 30-day readmission rate of 26%. Other associated outcomes are also poor, with a consistent relationship between readmission and subsequent mortality.
We found striking heterogeneity in various aspects. First, the inclusion/exclusion criteria varied widely, both cirrhosis-specific (eg, spontaneous bacterial peritonitis) and more general (patients admitted within the prior 30 days). Some of these criteria may bias readmission estimates; the risk of readmission may be reduced in those on hospice, as patients forgo curative therapy. Additionally, an established risk factor for readmission is prior hospitalization41; excluding patients with prior admissions prohibits analysis of this variable. Another aspect is the capture of readmissions: readmissions outside of the index hospital were not included in most studies. In those that did include outside readmissions, the burden was sizeable: 17% in 1 single-center study and 23% in a multistate administrative database.16,36 These outside readmissions must be included in future studies; they are as important as same-center readmissions both to patients and CMS.3 Despite this heterogeneity, the studies scored relatively high on the Newcastle–Ottawa risk of bias scale, with the only common deficiency being an inadequate description of follow-up.
Building on the findings of this review, an important step will be the design of interventions to reduce readmissions. Such interventions require a full understanding of this population’s characteristics and needs. Critically, we found a lack of data on social determinants of health. Impairments in these factors are well-established contributors to readmission risk in other populations,4,40 and are highly prevalent in cirrhosis.42 Indeed, CMS has focused resources toward social determinants of health in the effort to reduce utilization and improve outcomes. This lack of data on social determinants of health, as well as other understudied factors, represents an important opportunity for future research efforts to better define the modifiable features that could be targeted in the future to prevent readmissions. Such research is urgently needed and will likely require prospective studies to gather these important factors. Notably, most studies in this systematic review were retrospective and therefore unable to examine many of these understudied factors. Another important aspect that has received little attention is readmission preventability: only 2 studies assessed preventability, both through unstructured chart review. Preventability assessments in noncirrhotic populations have used wide-ranging methodologies, yielding inconsistent results.43 This variability prompted recommendations that preventability should be assessed by multiple reviewers guided by explicit parameters.43 Such detailed attention to preventability is urgently needed to better inform interventions.
In contrast to the lack of data on social factors, we found that the MELD score was examined in most studies and was frequently associated with readmission. Despite this consistent association, differences in the MELD scores between studies limit inferences into specific cutoff values that could identify the highest risk patients. Because of its existing widespread clinical use, the MELD score may prove to be important in readmission risk stratification. Efforts to develop a useful model including the MELD score are needed to target interventions to the highest risk patients.
This review has several limitations. Although we used a broad search strategy to capture studies, some may not have been included due to our selection criteria. For instance, 1 retrospective paper described factors associated with high admission density during 1 year but did not specifically report the frequency of early readmissions.44 Similarly, a randomized trial of a disease management program did not specifically examine early readmissions.45 Another quasi-experimental study of a quality improvement initiative was not included because a large proportion of their subjects was post liver transplant.46 However, the inclusion of these papers is unlikely to change our conclusions; the retrospective study identified factors similar to those in the included studies, and the quasi-experimental study overlapped with the included study that assessed frailty.27 Another potential limitation is the exclusion of studies published in abstract form only. Such studies may be important, as the field of cirrhosis readmissions is relatively young. However, including only full-paper publications ensures the inclusion of only higher quality studies scrutinized during the peer-review process. Similarly, newer published studies may have been missed due to the abundant interest in this topic and ongoing research. Lastly, the significant heterogeneity of the studies limits conclusions that can be made regarding the pooled readmission rates.
In summary, we found that patients with cirrhosis experience a high incidence of hospital readmissions. Several processes of care may be associated with readmissions, suggesting room for improvement in caring for this population and reducing readmissions. However, we identified several gaps in the literature, which does not adequately describe social factors and is lacking details on readmission preventability assessment. Future studies should attempt to address these issues so that interventions can be targeted to the highest risk patients and designed to best meet the needs of patients with cirrhosis.
Supplementary Material
Acknowledgments
Funding Information: This work was supported, in part, by the National Institutes of Health, KL2 TR001106 and K23 DK109202.
Footnotes
Disclosures: Dr. Orman, Dr. Ghabril, and Dr. Emmett report no potential conflicts of interest. Dr. Chalasani reports personal fees from Lilly, personal fees from Abbvie, personal fees from Tobira/Allergan, personal fees from Ardelyx, personal fees from Amarin, personal fees from Shire, personal fees from Madrigal, personal fees from DS Biopharma (Afimmune), personal fees from Cempra, personal fees from NuSirt, grants from Galectin, grants from Gilead, grants from Intercept, grants from Cumberland, grants from Conatus, personal fees from Immuron, and personal fees from Axovant, outside the submitted work.
Additional Supporting Information may be found in the online version of this article.
References
- 1.Peery AF, Crockett SD, Barritt AS, et al. Burden of gastrointestinal, liver, and pancreatic diseases in the United States. Gastroenterology. 2015;149(7):1731–1741e3. doi: 10.1053/j.gastro.2015.08.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 3.Hospital Readmissions Reduction Program. [Accessed September 27, 2016]. https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html. Updated date November 30, 2017.
- 4.Calvillo-King L, Arnold D, Eubank KJ, et al. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J Gen Intern Med. 2013;28(2):269–282. doi: 10.1007/s11606-012-2235-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ross JS, Mulvey GK, Stauffer B, et al. Statistical models and patient predictors of readmission for heart failure: a systematic review. Arch Intern Med. 2008;168(13):1371–1386. doi: 10.1001/archinte.168.13.1371. [DOI] [PubMed] [Google Scholar]
- 6.Feltner C, Jones CD, Cené CW, et al. Transitional care interventions to prevent readmissions for persons with heart failure: a systematic review and meta-analysis. Ann Intern Med. 2014;160(11):774–784. doi: 10.7326/M14-0083. [DOI] [PubMed] [Google Scholar]
- 7.Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;128(16):e240–e327. doi: 10.1161/CIR.0b013e31829e8776. [DOI] [PubMed] [Google Scholar]
- 8.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9. W64. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 9.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. doi: 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. [Accessed October 12, 2015]. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp .
- 12.Freeman MF, Tukey JW. Transformations related to the angular and the square root. Ann Math Statist. 1950;21(4):607–611. doi: 10.1214/aoms/1177729756. [DOI] [Google Scholar]
- 13.Bini EJ, Weinshel EH, Generoso R, et al. Impact of gastroenterology consultation on the outcomes of patients admitted to the hospital with de-compensated cirrhosis. Hepatology. 2001;34(6):1089–1095. doi: 10.1053/jhep.2001.29204. [DOI] [PubMed] [Google Scholar]
- 14.Berman K, Tandra S, Forssell K, et al. Incidence and predictors of 30-day readmission among patients hospitalized for advanced liver disease. Clin Gastroenterol Hepatol. 2011;9(3):254–259. doi: 10.1016/j.cgh.2010.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson EA, Spier BJ, Leff JA, Lucey MR, Said A. Optimising the care of patients with cirrhosis and gastrointestinal haemorrhage: a quality improvement study. Aliment Pharmacol Ther. 2011;34(1):76–82. doi: 10.1111/j.1365-2036.2011.04692.x. [DOI] [PubMed] [Google Scholar]
- 16.Volk ML, Tocco RS, Bazick J, Rakoski MO, Lok AS. Hospital readmissions among patients with decompensated cirrhosis. Am J Gastroenterol. 2012;107(2):247–252. doi: 10.1038/ajg.2011.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barsuk JH, Cohen ER, Feinglass J, McGaghie WC, Wayne DB. Clinical outcomes after bedside and interventional radiology paracentesis procedures. Am J Med. 2013;126(4):349–356. doi: 10.1016/j.amjmed.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 18.Deitelzweig S, Amin A, Christian R, Friend K, Lin J, Lowe TJ. Hyponatremia-associated healthcare burden among US patients hospitalized for cirrhosis. Adv Ther. 2013;30(1):71–80. doi: 10.1007/s12325-012-0073-1. [DOI] [PubMed] [Google Scholar]
- 19.Morando F, Maresio G, Piano S, et al. How to improve care in outpatients with cirrhosis and ascites: a new model of care coordination by consultant hepatologists. J Hepatol. 2013;59(2):257–264. doi: 10.1016/j.jhep.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 20.Singal AG, Rahimi RS, Clark C, et al. An automated model using electronic medical record data identifies patients with cirrhosis at high risk for readmission. Clin Gastroenterol Hepatol. 2013;11(10):1335–1341e1. doi: 10.1016/j.cgh.2013.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Desai AP, Satoskar R, Appannagari A, et al. Co-management between hospitalist and hepatologist improves the quality of care of inpatients with chronic liver disease. J Clin Gastroenterol. 2014;48(4):e30–e36. doi: 10.1097/MCG.0b013e3182a87f70. [DOI] [PubMed] [Google Scholar]
- 22.Fagan KJ, Zhao EY, Horsfall LU, et al. Burden of decompensated cirrhosis and ascites on hospital services in a tertiary care facility: time for change? Intern Med J. 2014;44(9):865–872. doi: 10.1111/imj.12491. [DOI] [PubMed] [Google Scholar]
- 23.Gaduputi V, Chandrala C, Abbas N, Tariq H, Chilimuri S, Balar B. Prognostic significance of hypokalemia in hepatic encephalopathy. Hepatogastroenterology. 2014;61(133):1170–1174. [PubMed] [Google Scholar]
- 24.Ghaoui R, Friderici J, Visintainer P, Lindenauer PK, Lagu T, Desilets D. Measurement of the quality of care of patients admitted with decompensated cirrhosis. Liver Int. 2014;34(2):204–210. doi: 10.1111/liv.12225. [DOI] [PubMed] [Google Scholar]
- 25.Ghaoui R, Friderici J, Desilets DJ, et al. Outcomes associated with a mandatory gastroenterology consultation to improve the quality of care of patients hospitalized with decompensated cirrhosis. J Hosp Med. 2015;10(4):236–241. doi: 10.1002/jhm.2314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Agrawal K, Kumar P, Markert R, Agrawal S. Risk factors for 30-day readmissions of individuals with decompensated cirrhosis. South Med J. 2015;108(11):682–687. doi: 10.14423/SMJ.0000000000000371. [DOI] [PubMed] [Google Scholar]
- 27.Tapper EB, Finkelstein D, Mittleman MA, Piatkowski G, Lai M. Standard assessments of frailty are validated predictors of mortality in hospitalized patients with cirrhosis. Hepatology. 2015;62(2):584–590. doi: 10.1002/hep.27830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Atla PR, Sheikh MY, Gill F, Kundu R, Choudhury J. Predictors of hospital re-admissions among Hispanics with hepatitis C-related cirrhosis. Ann Gastroenterol. 2016;29(4):515–520. doi: 10.20524/aog.2016.0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bajaj JS, Reddy KR, Tandon P, et al. The 3-month readmission rate remains unacceptably high in a large North American cohort of patients with cirrhosis. Hepatology. 2016;64(1):200–208. doi: 10.1002/hep.28414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Courson A, Jones GM, Twilla JD. Treatment of acute hepatic encephalopathy: comparing the effects of adding rifaximin to lactulose on patient outcomes. J Pharm Pract. 2016;29(3):212–217. doi: 10.1177/0897190014566312. [DOI] [PubMed] [Google Scholar]
- 31.Graupera I, Solà E, Fabrellas N, et al. Urine monocyte chemoattractant protein-1 is an independent predictive factor of hospital readmission and survival in cirrhosis. PLOS ONE. 2016;11(6):e0157371. doi: 10.1371/journal.pone.0157371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kanwal F, Asch SM, Kramer JR, Cao Y, Asrani S, El-Serag HB. Early outpatient follow-up and 30-day outcomes in patients hospitalized with cirrhosis. Hepatology. 2016;64(2):569–581. doi: 10.1002/hep.28558. [DOI] [PubMed] [Google Scholar]
- 33.Le S, Spelman T, Chong CP, et al. Could adherence to quality of care indicators for hospitalized patients with cirrhosis-related ascites improve clinical outcomes? Am J Gastroenterol. 2016;111(1):87–92. doi: 10.1038/ajg.2015.402. [DOI] [PubMed] [Google Scholar]
- 34.Moon AM, Dominitz JA, Ioannou GN, Lowy E, Beste LA. Use of antibiotics among patients with cirrhosis and upper gastrointestinal bleeding is associated with reduced mortality. Clin Gastroenterol Hepatol. 2016;14(11):1629–1637e1. doi: 10.1016/j.cgh.2016.05.040. [DOI] [PubMed] [Google Scholar]
- 35.Rassameehiran S, Mankongpaisarnrung C, Sutamtewagul G, Klomjit S, Rakvit A. Predictor of 90-day readmission rate for hepatic encephalopathy. South Med J. 2016;109(6):365–369. doi: 10.14423/SMJ.0000000000000475. [DOI] [PubMed] [Google Scholar]
- 36.Tapper EB, Halbert B, Mellinger J. Rates of and reasons for hospital readmissions in patients with cirrhosis: a multistate population-based cohort study. Clin Gastroenterol Hepatol. 2016;14(8):1181–1188e2. doi: 10.1016/j.cgh.2016.04.009. [DOI] [PubMed] [Google Scholar]
- 37.Lyon KC, Likar E, Martello JL, Regier M. Retrospective cross-sectional pilot study of rifaximin dosing for the prevention of recurrent hepatic encephalopathy. J Gastroenterol Hepatol. 2017;32(9):1548–1552. doi: 10.1111/jgh.13759. [DOI] [PubMed] [Google Scholar]
- 38.Morales BP, Planas R, Bartoli R, et al. Early hospital readmission in decompensated cirrhosis: incidence, impact on mortality, and predictive factors. Dig Liver Dis. 2017;49(8):903–909. doi: 10.1016/j.dld.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 39.Strömdahl M, Helgeson J, Kalaitzakis E. Emergency readmission following acute upper gastrointestinal bleeding. Eur J Gastroenterol Hepatol. 2017;29(1):73–77. doi: 10.1097/MEG.0000000000000746. [DOI] [PubMed] [Google Scholar]
- 40.Rodríguez-Artalejo F, Guallar-Castillón P, Pascual CR, et al. Health-related quality of life as a predictor of hospital readmission and death among patients with heart failure. Arch Intern Med. 2005;165(11):1274–1279. doi: 10.1001/archinte.165.11.1274. [DOI] [PubMed] [Google Scholar]
- 41.van Walraven C, Dhalla IA, Bell C, et al. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. CMAJ. 2010;182(6):551–557. doi: 10.1503/cmaj.091117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bajaj JS, Wade JB, Gibson DP, et al. The multi-dimensional burden of cirrhosis and hepatic encephalopathy on patients and caregivers. Am J Gastroenterol. 2011;106(9):1646–1653. doi: 10.1038/ajg.2011.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.van Walraven C, Bennett C, Jennings A, Austin PC, Forster AJ. Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ. 2011;183(7):E391–E402. doi: 10.1503/cmaj.101860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ganesh S, Rogal SS, Yadav D, Humar A, Behari J. Risk factors for frequent readmissions and barriers to transplantation in patients with cirrhosis. PLOS ONE. 2013;8(1):e55140. doi: 10.1371/journal.pone.0055140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wigg AJ, McCormick R, Wundke R, Woodman RJ. Efficacy of a chronic disease management model for patients with chronic liver failure. Clin Gastroenterol Hepatol. 2013;11(7):850–8e1. doi: 10.1016/j.cgh.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 46.Tapper EB, Finkelstein D, Mittleman MA, Piatkowski G, Chang M, Lai M. A quality improvement initiative reduces 30-day rate of readmission for patients with cirrhosis. Clin Gastroenterol Hepatol. 2016;14(5):753–759. doi: 10.1016/j.cgh.2015.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.