Abstract
PURPOSE
Cement-retained implant prostheses can lack proper retrievability during repair, and residual cement can cause peri-implantitis. The purpose of this in vitro study was to evaluate the influence of abutment height and convergence angle on the retrievability of cement-retained implant prostheses with lingual slots, known as retrievable cement-type slots (RCS).
MATERIALS AND METHODS
We fabricated six types of titanium abutments (10 of each type) with two different heights (4 mm and 6 mm), three different convergence angles (8°, 10°, and 12°), a sloped shoulder margin (0.6 mm depth), a rectangular shape (6 mm × 6.5 mm) with rounded edges, and a rectangular ledge (2 mm × 1 mm) for the RCS. One monolithic zirconia crown was fabricated for each abutment using a dental computer-aided design/computer-aided manufacturing system. The abutments and crowns were permanently cemented together with dual-curing resin cement, followed by 24 hours in demineralized water at room temperature. Using a custom-made device with a slot driver and torque gauge, we recorded the torque (N·cm) required to remove the crowns. Statistical analysis was conducted using multiple regression analysis and Mann-Whitney U tests (α=.05).
RESULTS
Removal torques significantly decreased as convergence angles increased. Multiple regression analysis showed no significant interaction between the abutment height and the convergence angle (Durbin-Watson ratio: 2.186).
CONCLUSION
Within the limitations of this in vitro study, we suggest that the retrievability of cement-retained implant prostheses with RCS can be maintained by adjusting the abutment height and convergence angle, even when they are permanently cemented together.
Keywords: Lingual slot, Cement-retained implant prostheses, Abutment, Computer-aided design and computer-aided manufacturing (CAD/CAM), Retrievability
INTRODUCTION
Depending on the retention method, implant-fixed prostheses can be categorized into either screw-retained or cement-retained types. Screw-retained prostheses involve connecting the abutment and the final prosthesis to the fixture with a screw to obtain retention. The universal clearance-limited abutment is the typical example of a screw-retained prosthesis. For cement-retained prostheses, the abutment is connected to the implant fixture with a screw, and the final prosthesis is then cemented using dental cement. This is similar to existing fixed prostheses used for the restoration of natural teeth.1
Many studies have compared the advantages and disadvantages of screw-retained prostheses and cement-retained prostheses in order to select the best retention form for various circumstances.2,3,4 The biggest advantage of the screw-retained prosthesis is its convenience; it is easily retrieved when it requires repair. However, due to the need of a hole for the screw, its occlusal surface is esthetically unfavorable. In addition, when occlusal force is applied, the most desirable occlusal point is in the direction of the implant axis. This avoids the effect of hazardous lateral force on the implant fixture that would require restoration using composite resin.
Compared to screw-retained prostheses, cement-retained prostheses can be designed to apply occlusal force to the implant in a more vertical direction, since they lack the hole required for the screw. In addition, they can be fabricated with a more esthetic shape on the occlusal surface and at the same time offer simpler procedures in clinics and dental laboratories. However, if cement-retained implant prostheses need to be repaired, poor retrievability is a disadvantage.
To overcome these disadvantages for cement-retained implant prostheses, numerous studies have been performed and various clinical techniques were introduced. Ekfeldt et al.5 recommended avoiding permanent cement during the final application of cement-retained prostheses to ease retrieval, and Breeding et al.6 and Valbao et al.7 recommended using a temporary cement during the application of the crown to the abutment, in the cases with a long abutment height and an ideal slope. Other studies have suggested application of a small lingual screw to attach the crown to the abutment,8 use of a template fabricated by vacuum-formed thermosetting plastic that confirms the location of the screw with digital pictures,9,10 and recording the 3-dimensional location of the screw hole using a customized device11 in order to ease retrieval of cement-retained implant prostheses. Prestipino et al.12 and Schweitzer13 suggested forming a small slot on the interface between the abutment and the crown when the crown needs to be repaired. This method offers the advantage of easy crown removal with commonly used slot drivers, even if the cement-retained crowns are bonded using permanent cement. However, although many customized abutments are used in clinics, there are limited studies on manufacturing abutments with proper retrievability. In addition, studies on the design and manufacture of customized abutments in clinical settings are insufficient. Therefore, the purpose of this study was to evaluate the influence of abutment height and convergence angle on the retrievability of prostheses when fabricating customized abutments for cement-retained implant prostheses with lingual slots, known as retrievable cement-type slots (RCS). The null hypothesis was that there was no difference in the removal torques between different abutment heights and convergence angles of cement-retained implant prostheses with RCS.
MATERIALS AND METHODS
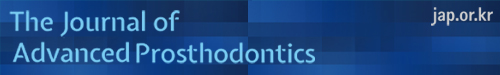
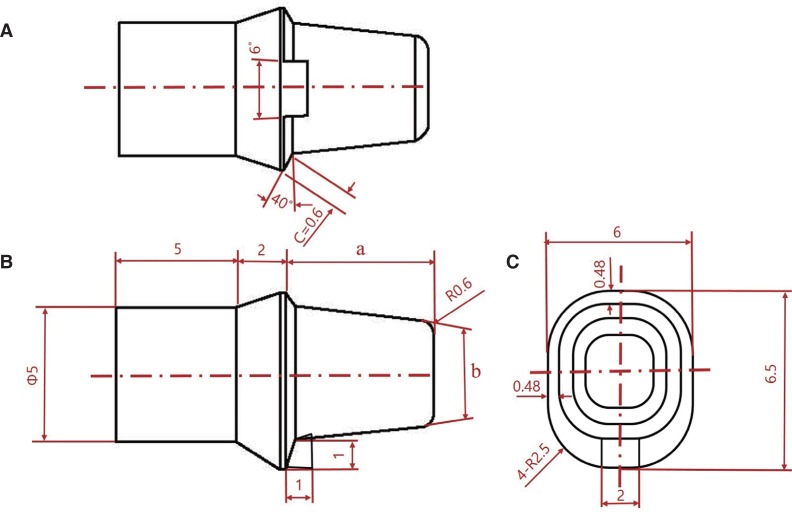
Fig. 1 shows the assembly drawing of the specimen used in this experiment, and Fig. 2 shows both the 3-dimensional design and the fabricated abutment (height: 6 mm; convergence angle: 8°). The fabricated abutment has a height of 6.5 mm, a sloped shoulder margin (width: 0.6 mm), a ledge shape for the RCS on one side (width: 2 mm; thickness: 1 mm), and a rectangular shape with a rounded edge. We fabricated six types of titanium abutments (10 of each), with two different heights (4 mm and 6 mm) and three different convergence angles (8°, 10°, and 12°), for a total of 60 abutments. The zirconia crowns were fabricated using a computer-aided design/computer-aided manufacturing (CAD/CAM) system from Ceramill (Amann Girrbach, Koblach, Austria), and the Ceramill Map400 was used for scanning. To prevent scan error caused by reflection of the metal, scan spray (Telescan, DIAMON, Riedenburg, Germany) was applied to the fabricated specimen. In the CAD program, the crowns were created in the shape of a maxillary first molar using a scanned image. Space for the cementing was set to 35 µm, which is similar to the value used in clinical settings. In addition, the distance on the marginal area without the cementation gap was set to 1 mm in the CAD program, in order to allow minimal retention from the margin during fitting. The thickness of the zirconia prostheses was set to greater than 1 mm in all areas, except the marginal area, in order to prevent fracture caused by focused stress of the removal torque on a thin area. The design of the completed prostheses was transferred to the Ceramill Motion 2, and fabricated into the crown prostheses using the Ceramill Zolid zirconia block through both a milling operation and a general sintering process.14
Fig. 1. Specimen diagram used in this experiment. (A) Lingual view; (B) Distal view; (C) Occlusal view; Ø: diameter; R: arc diameter; a: abutment height (4 mm and 6 mm); b: convergence angle (8°, 10°, and 12°).
Fig. 2. Three-dimensional design of abutment (A) and fabricated titanium abutment (B).
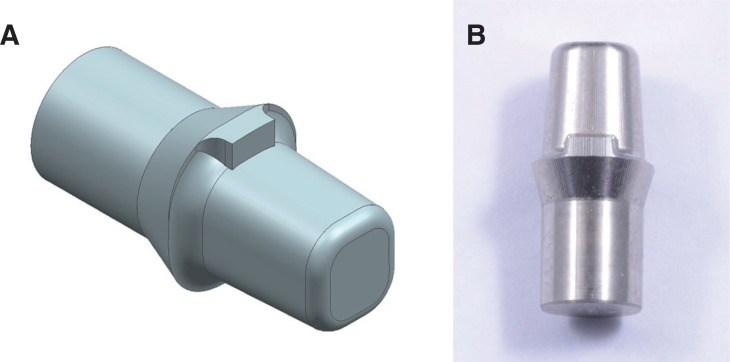
The RCS were created on the zirconia crown prostheses in order to provide an approach for a slot driver. On each crown, the contact area on the ledge part of the abutment was reduced, using a laboratory handpiece, to 2 mm in length and 1 mm in width. All work on the specimens was performed by a single, well-trained dental technician. Fig. 3 shows an abutment and crown before and after the creation of the RCS.
Fig. 3. Specimens before (A) and after (B) the fabrication of the retrievable cement-type slot (RCS).
For the permanent cementation of each abutment and zirconia crown, RelyX U200 (3M ESPE, St. Paul, MN, USA) double-curing resin cement was used. Following the manufacturer's instructions, mixed cement was applied on the inside of the prosthesis and cemented to the abutment. After cementation, excess cement around the margin and slot area was removed. A force of 50 N was then applied for 10 min, and the cement hardened without light-curing. After completion of cement hardening, the specimens were stored in distilled water at room temperature for 24 hours.
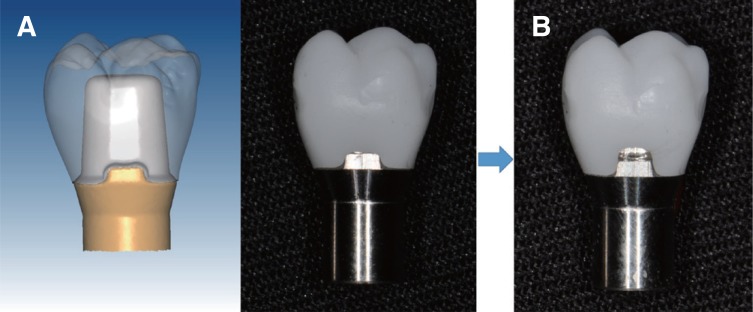
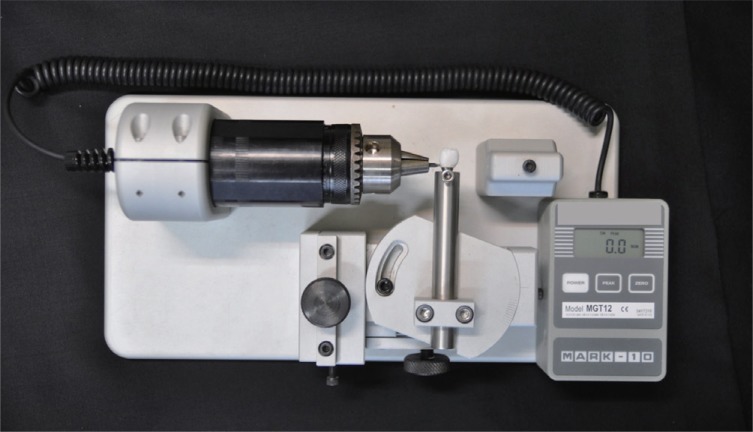
We used a custom-made device (Fig. 4) to record the removal torque. A basic torque gauge, MGT12 (Mark-10 Corp., Copiague, NY, USA), with a slot driver and a jig for specimen fixation was installed. During recording, the abutment was completely fixed; only the crown could be removed vertically, and the torque gauge could only be rotated at one place. Each specimen was fixed in the custom-made device. The slot driver was completely inserted into the RCS and then rotated to separate the abutment from the crown. The maximum torque value required to remove the crown from the abutment was measured using the torque gauge and recorded.
Fig. 4. The custom-made device used for measuring removal torque in this experiment.
A two-way analysis of variance (ANOVA) was used to analyze the difference depending on the height of abutment and the degree of the convergence angle. The Mann-Whitney U test was used for the post-hoc analysis. Multiple regression analysis was performed on the assumption that no correlation between height of the abutment and the convergence angle was present. The SPSS 20.0 for Windows (SPSS Inc., Chicago, IL, USA) was used for all statistical work (α = .05).
RESULTS
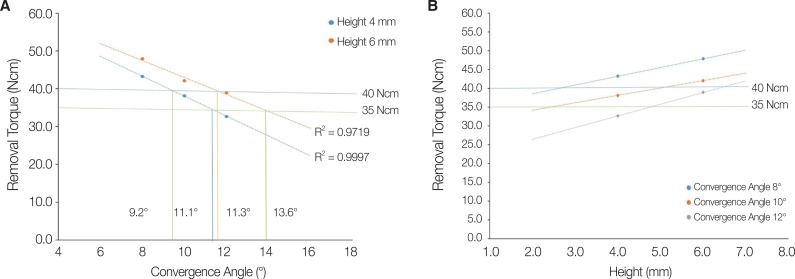
Table 1 shows the analysis of the removal torque values required. The results of the two-way ANOVA test indicated significant differences in removal torque depending on the height and the convergence angle (P < .05). However, a correlation effect was not found dependent on the height and the convergence angle. As the convergence angle increased from 8°, 10°, to 12°, removal torque value at 4 mm of height gradually decreased from 43.2 ± 1.2 N·cm, 38.1 ± 1.5 N·cm, to 32.7 ± 1.3 N·cm, respectively (P = .002). This decrease in removal torque was also present at the height of 6 mm (47.9 ± 2.6 N·cm, 42.1 ± 0.9 N·cm, and 38.9 ± 1.4 N·cm, respectively [P = .002]). As the height increased from 4 mm to 6 mm at a constant convergence angle, the removal torque increased with a statistically significant difference (P < .05). Fig. 5 depicts a graph demonstrating the results of the correlation analysis among variables using multiple regression analysis. There was a negative correlation between the convergence angle and the removal torque (unstandardized coefficient: B = −2.438) and a positive correlation between the height and the removal torque (standardized coefficient: β = 2.477). The Durbin-Watson value for the test of independence between the height and the convergence angle was 2.186 (R2 = 0.900). This result demonstrates the independence between the variables of height and convergence angle.
Table 1. Removal torque values (N·cm) according to abutment height and convergence angle.
| Abutment height (mm) | Convergence angle (°) | P value | ||
|---|---|---|---|---|
| 8 | 10 | 12 | ||
| 4 | 43.2 ± 1.2a,* | 38.1 ± 1.5b,* | 32.7 ± 1.3c,* | .002 |
| 6 | 47.9 ± 2.6A,† | 42.1 ± 0.9B,† | 38.9 ± 1.4C,† | .002 |
| P | .016 | .008 | .008 | |
Different superscripted characters within each row (a, b, c) and (A, B, C) and each column (*, †) indicate significant differences by Mann-Whitney U-test (α = .05).
Fig. 5. Graphs illustrating the variables obtained through multiple regression analysis. (A) Graph A demonstrates a negative correlation between convergence angle and removal torque (R2 = 0.9719), and (B) Graph B demonstrates a positive correlation between abutment height and removal torque (R2 = 0.9997).
DISCUSSION
This study was designed to evaluate the influence of abutment height and convergence angle on the ability to retrieve prostheses when fabricating customized abutments in RCS. We found that when the convergence angle increased while the height remained constant, there was a significant decrease in removal torque values. When the convergence angle remained constant, there was a significant increase in removal torque values when the height of abutment increased. These results coincide with those of previous studies15,16 that analyzed the differences in prosthesis retention depending on the height of the abutment and the changes in surface area. When fabricating customized abutments in clinical settings, controlling convergence angles is recommended to support prosthesis retention, as the height of the abutment is limited by the intermaxillary space. Generally, a 35 N·cm implant driver is used for removing screws between the implant fixture and the crown. Considering the decrease in retention due to occlusal forces, customized abutments should be fabricated by setting the proper height and convergence angle to facilitate removal using a 35 N·cm implant torque driver and slot driver (even if the abutment is permanently cemented). The convergence angle required for a retentive force (range: 35 – 40 N·cm) at a constant height was calculated based on the linear analysis and the interval forecast from our experimental results. In order to have a retentive force that ranged between 35 and 40 N·cm after resin cementation, the convergence angle should be set between 11.3° and 13.6° for the height of 6 mm and between 9.2° and 11.1° for the height of 4 mm (Fig. 5A).
These results show that a higher convergence angle is needed for retrieval of cement-retained implant prostheses, compared to the 6° standard value for the tooth preparation during full veneer crown fabrication on natural molars shown in previous studies.16,17,18,19 Additionally, it is essential to achieve retrievability while using resin cement in the cement-retained implant prostheses. These results provide a method for determining convergence angles, particularly when the height of the abutment is insufficient due to an intermaxillary space deficiency. When the height is 2 to 4 mm, the convergence angle should not be greater than 10° in order to prevent early failure due to decreased retention after prosthesis cementation (Fig. 5B). These findings support the results of a previous study15 that used resin cement to bond to abutments with heights of less than 2 mm.
This study is focused on the abutment height and convergence angle. It is very interesting to know the relationship between retentive force and surface area of abutment. Although the actual surface area of abutment is not measured in this study, it can be assumed that the surface area of abutment increases as the abutment height increases. The results of this study show that the retentive force increases as the abutment height increases, and it is predictable that the surface area of abutment may also be affected. Previous studies20,21 have suggested that abutment height has a significant effect on the resistance to removal. However, according to a follow-up study by Covey et al.,22 abutment height may be positively related to retention strength, but abutment's total surface area is not. Based on these studies, further research is needed to understand the relationship between actual surface area of abutment and retentive force.
Several studies have evaluated the retention force of the copings according to the conditions of the implant abutment. However, studies on the removal force of cement-retained implant prostheses with RCS are lacking. In a study by Abbo,20 the height of the implant abutment was estimated a relatively low removal force was observed at a 5.5 mm abutment (124.89 N) than the 6.5 mm titanium abutment (198.09 N). In a study by Safari,21 the height of the implant abutment was set at 4.5 mm and 5.5 mm, and the removal force decreased from 5.5 mm (460.44 N) to 4.5 mm (364.19 N). Similar to the results of various studies, this study also proved that the greater the abutment height, the greater the removal force. Our results also confirmed the reduction of the removal force with increasing convergence angle. Our results confirmed the general trends found in other literature.23 There are different methods for evaluating retention of general prostheses and for evaluating the removal stresses of cement-retained implant prostheses with RCS. The evaluation of retention of general prostheses is a method of measuring the pull force using a universal testing machine.20,21,22,23 However, in this study, cement-retained implant prostheses with RCS measured force removed through lingual slots. These differences should be considered.
We examined several studies to determine which cement to use for our cement-retained implant prostheses. Previous studies16,24 indicated that application of permanent cement without considering the retrievability is not recommended. Mehl et al.16 suggested using either zinc phosphate cement or glass ionomer cement as semi-permanent cementation to increase retrievability for cement-retained implant prostheses. However, resin cement is recommended only with abutments of less than 2 mm due to an intermaxillary space deficiency or when failure is expected due to the lack of prosthesis retention.24 In addition, many studies6,7,25 recommend the use of temporary cement to prevent damage to the abutment and the crown when the prosthesis requires repair. The results of these studies have led to the introduction of various implant cements to the market in order to provide both retention and retrievability.
Previous studies16,24 have shown that cement-retained implant prostheses with RCS are not recommended for use with permanent cements to improve retrievability. However, the resin cement of implant prostheses has been used because of the long-term durability.26 For this reason, we experimented without light-curing. In this study, the reason for resin cement hardening without light-curing was that the polymerization reaction was initiated without light exposure in a dual-cured cement and there was time for self-curing for 10 minutes while maintaining 50 N. Some studies27,28,29 have shown that the thickness of the zirconia crown does not allow light irradiation to pass, but it has a higher bond strength in the light-cured group than the self-cured group. However, there was no significant difference in bond strength between the self-cured group and the light-cured group after pretreatment of the dentin surface.29 Further studies measure the removal torque by considering the difference by light-curing, and a study is needed to determine if there is a difference by light-curing.
Compared to permanent cement, temporary cement can easily cause leakage on the marginal area due to its low strength properties. Peri-implantitis can also occur due to plaque deposits on the marginal gap.30,31 Furthermore, Lim et al.26 reported high fracture rates when resin cement was used on zirconia prostheses. Based on this report, application of resin cement is recommended for zirconia crown restoration, instead of using temporary cement or implant cement. In this study, we used RelyX U200 double-curing permanent resin cement for the cementation of the zirconia crowns and the abutments on the implant prostheses. We obtained retrievability by adjusting the height and convergence angle and providing RCS forms during the fabrication of the customized abutments. One of the limitations of this study is that we did not consider the variable that the prosthesis-repairing process takes place after a certain time period of using the prosthesis.32 Therefore, to replicate clinical conditions, further in vitro studies that examine either applied cyclic loading to reproduce occlusal force or thermocycling to reproduce temperature changes would be required.
CONCLUSION
Despite the experimental limitations of this study, our results showed the following. First, the retrievability of the final prostheses can be obtained by controlling the convergence angle of the abutment according to height and by providing RCS forms during the fabrication of customized abutments. Secondly, effective clinical treatment methods during the fabrication of cement-retained implant fixed prostheses should use customized abutments with properly controlled lingual slots, heights, and convergence angles for retrievability and retention, and permanent cement should be used for the final cementation of the crowns.
Footnotes
This work was supported by an Institute for Information & Communications Technology Promotion (IITP) grant funded by the Korean government (MSIP) (B0101-17-1081, Development of ICT based software platform and service technologies for medical 3D printing applications) and Industrial Strategic Technology Development Program (10062635, New hybrid milling machine with a resolution of less than 10 µm development, using open CAD/CAM S/W integrated platforms for one day prosthetic treatment of 3D smart medical care system) funded by the Ministry of Trade, Industry & Energy (MOTIE, Korea).
References
- 1.Misch CE. Contemporary implant dentistry. 2nd ed. St. Louis: Mosby Inc; 1999. pp. 549–593. [Google Scholar]
- 2.Misch CE. Screw-retained versus cement-retained implant supported prostheses. Pract Periodontics Aesthet Dent. 1995;7:15–18. [PubMed] [Google Scholar]
- 3.Hebel KS, Gajjar RC. Cement-retained versus screw-retained implant restorations: achieving optimal occlusion and esthetics in implant dentistry. J Prosthet Dent. 1997;77:28–35. doi: 10.1016/s0022-3913(97)70203-8. [DOI] [PubMed] [Google Scholar]
- 4.Chee W, Felton DA, Johnson PF, Sullivan DY. Cemented versus screw-retained implant prostheses: which is better? Int J Oral Maxillofac Implants. 1999;14:137–141. [PubMed] [Google Scholar]
- 5.Ekfeldt A, Carlsson GE, Börjesson G. Clinical evaluation of single-tooth restorations supported by osseointegrated implants: a retrospective study. Int J Oral Maxillofac Implants. 1994;9:179–183. [PubMed] [Google Scholar]
- 6.Breeding LC, Dixon DL, Bogacki MT, Tietge JD. Use of luting agents with an implant system: Part I. J Prosthet Dent. 1992;68:737–741. doi: 10.1016/0022-3913(92)90194-f. [DOI] [PubMed] [Google Scholar]
- 7.Valbao FP, Jr, Perez EG, Breda M. Alternative method for retention and removal of cement-retained implant prostheses. J Prosthet Dent. 2001;86:181–183. doi: 10.1067/mpr.2001.115687. [DOI] [PubMed] [Google Scholar]
- 8.Clausen GF. The lingual locking screw for implant-retained restorations--aesthetics and retrievability. Aust Prosthodont J. 1995;9:17–20. [PubMed] [Google Scholar]
- 9.Doerr J. Simplified technique for retrieving cemented implant restorations. J Prosthet Dent. 2002;88:352–353. doi: 10.1067/mpr.2002.128149. [DOI] [PubMed] [Google Scholar]
- 10.Daher T, Morgano SM. The use of digital photographs to locate implant abutment screws for implant-supported cement-retained restorations. J Prosthet Dent. 2008;100:238–239. doi: 10.1016/S0022-3913(08)60187-0. [DOI] [PubMed] [Google Scholar]
- 11.Wadhwani C, Chung KH. Simple device for locating the abutment screw position of a cement-retained implant restoration. J Prosthet Dent. 2013;109:272–274. doi: 10.1016/S0022-3913(13)60058-X. [DOI] [PubMed] [Google Scholar]
- 12.Prestipino V, Ingber A, Kravitz J, Whitehead GM. A practical approach for retrieving cement-retained, implant-supported restorations. Quintessence Dent Technol. 2001;24:182–187. [Google Scholar]
- 13.Schweitzer DM, Berg RW, Mancia GO. A technique for retrieval of cement-retained implant-supported prostheses. J Prosthet Dent. 2011;106:134–138. doi: 10.1016/S0022-3913(11)60110-8. [DOI] [PubMed] [Google Scholar]
- 14.Elshiyab SH, Nawafleh N, Öchsner A, George R. Fracture resistance of implant-supported monolithic crowns cemented to zirconia hybrid-abutments: zirconia-based crowns vs. lithium disilicate crowns. J Adv Prosthodont. 2018;10:65–72. doi: 10.4047/jap.2018.10.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rödiger M, Rinke S, Ehret-Kleinau F, Pohlmeyer F, Lange K, Bürgers R, Gersdorff N. Evaluation of removal forces of implant-supported zirconia copings depending on abutment geometry, luting agent and cleaning method during re-cementation. J Adv Prosthodont. 2014;6:233–240. doi: 10.4047/jap.2014.6.3.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mehl C, Harder S, Shahriari A, Steiner M, Kern M. Influence of abutment height and thermocycling on retrievability of cemented implant-supported crowns. Int J Oral Maxillofac Implants. 2012;27:1106–1115. [PubMed] [Google Scholar]
- 17.Mehl C, Harder S, Schwarz D, Steiner M, Vollrath O, Kern M. In vitro influence of ultrasonic stress, removal force preload and thermocycling on the retrievability of implant-retained crowns. Clin Oral Implants Res. 2012;23:930–937. doi: 10.1111/j.1600-0501.2011.02236.x. [DOI] [PubMed] [Google Scholar]
- 18.Pintinha M, Camarini ET, Sábio S, Pereira JR. Effect of mechanical loading on the removal torque of different types of tapered connection abutments for dental implants. J Prosthet Dent. 2013;110:383–388. doi: 10.1016/j.prosdent.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 19.Mehl C, Harder S, Steiner M, Vollrath O, Kern M. Influence of cement film thickness on the retention of implant-retained crowns. J Prosthodont. 2013;22:618–625. doi: 10.1111/jopr.12058. [DOI] [PubMed] [Google Scholar]
- 20.Abbo B, Razzoog ME, Vivas J, Sierraalta M. Resistance to dislodgement of zirconia copings cemented onto titanium abutments of different heights. J Prosthet Dent. 2008;99:25–29. doi: 10.1016/S0022-3913(08)60005-0. [DOI] [PubMed] [Google Scholar]
- 21.Safari S, Hosseini Ghavam F, Amini P, Yaghmaei K. Effects of abutment diameter, luting agent type, and re-cementation on the retention of implant-supported CAD/CAM metal copings over short abutments. J Adv Prosthodont. 2018;10:1–7. doi: 10.4047/jap.2018.10.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Covey DA, Kent DK, St Germain HA, Jr, Koka S. Effects of abutment size and luting cement type on the uniaxial retention force of implant-supported crowns. J Prosthet Dent. 2000;83:344–348. doi: 10.1016/s0022-3913(00)70138-7. [DOI] [PubMed] [Google Scholar]
- 23.Bresciano M, Schierano G, Manzella C, Screti A, Bignardi C, Preti G. Retention of luting agents on implant abutments of different height and taper. Clin Oral Implants Res. 2005;16:594–598. doi: 10.1111/j.1600-0501.2005.01159.x. [DOI] [PubMed] [Google Scholar]
- 24.Mehl C, Harder S, Wolfart M, Kern M, Wolfart S. Retrievability of implant-retained crowns following cementation. Clin Oral Implants Res. 2008;19:1304–1311. doi: 10.1111/j.1600-0501.2008.01587.x. [DOI] [PubMed] [Google Scholar]
- 25.Heinemann F, Mundt T, Biffar R. Retrospective evaluation of temporary cemented, tooth and implant supported fixed partial dentures. J Craniomaxillofac Surg. 2006;34:86–90. doi: 10.1016/S1010-5182(06)60019-X. [DOI] [PubMed] [Google Scholar]
- 26.Lim HP, Yoo JM, Park SW, Yang HS. Fracture load of implant-supported zirconia all-ceramic crowns luted with various cements. Int J Prosthodont. 2010;23:361–363. [PubMed] [Google Scholar]
- 27.Arrais CA, Giannini M, Rueggeberg FA, Pashley DH. Microtensile bond strength of dual-polymerizing cementing systems to dentin using different polymerizing modes. J Prosthet Dent. 2007;97:99–106. doi: 10.1016/j.prosdent.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 28.Lührs AK, De Munck J, Geurtsen W, Van Meerbeek B. Composite cements benefit from light-curing. Dent Mater. 2014;30:292–301. doi: 10.1016/j.dental.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 29.Youm SH, Jung KH, Son SA, Kwon YH, Park JK. Effect of dentin pretreatment and curing mode on the microtensile bond strength of self-adhesive resin cements. J Adv Prosthodont. 2015;7:317–322. doi: 10.4047/jap.2015.7.4.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pan YH, Lin CK. The effect of luting agents on the retention of dental implant-supported crowns. Chang Gung Med J. 2005;28:403–410. [PubMed] [Google Scholar]
- 31.Harder S, Dimaczek B, Açil Y, Terheyden H, Freitag-Wolf S, Kern M. Molecular leakage at implant-abutment connection--in vitro investigation of tightness of internal conical implant-abutment connections against endotoxin penetration. Clin Oral Investig. 2010;14:427–432. doi: 10.1007/s00784-009-0317-x. [DOI] [PubMed] [Google Scholar]
- 32.Chaar MS, Att W, Strub JR. Prosthetic outcome of cement-retained implant-supported fixed dental restorations: a systematic review. J Oral Rehabil. 2011;38:697–711. doi: 10.1111/j.1365-2842.2011.02209.x. [DOI] [PubMed] [Google Scholar]