Abstract
Introduction
Buried penis is a condition that causes the penis to become hidden beneath the skin. It has a significant impact on quality of life and can present in a variety of ways, with lower urinary tract symptoms and erectile dysfunction being common. Whilst there are several causes, obesity is the most common in adults. Due to the burden that obesity is increasingly presenting to healthcare, buried penis may become more common in the future.
The purpose of this article is to provide an overview of the causes, presentation and surgical management of this condition in adults.
Material and method
A literature review was conducted using urological and plastic surgery articles from PubMed, Embase and Medline. Eighteen studies, published between 1982 and 2016, were included.
Results
Original research trials discussed the treatment of buried penis in lymphoedema and balanitis xerotica obliterans (BXO), new techniques for fat removal, comparison of grafts and postoperative dressings. Several studies provided broad overviews, although focused on management rather than cause and presentation. Overall, studies suggest that, whilst some causes can only be treated with surgery, others can be modified by lifestyle changes and medical management.
Conclusions
Buried penis is a complex condition that may take years to treat. Several surgical techniques are available, with patients likely requiring a combination of techniques to treat this problem. This review aims to provide a comprehensive overview of the causes, presentation and surgical management of this condition, in order to further the understanding of clinicians who may be faced with this problem more commonly in the future.
Keywords: penis surgical intervention obesity diabetes
INTRODUCTION
Buried penis is a condition in which the penis is partially or completely hidden below the surface of the skin.
Anatomically it is described as when the penis is located beneath the abdomen, thigh or scrotum [1, 2]. It is important to note that the penis has a normal corporal length, but poor phallic exposure, and so is distinguishable from conditions such as micropenis [3]. In cases of buried penis, the penile shaft lies ‘below the prepubic skin’ and is no longer visible due to complete burying.
Whilst some use the term buried penis, others prefer the term concealed penis. Higuchi et al. [4] prefer the team ‘concealed’ as it allows for further sub-classification of the condition into trapped, buried and complex penis.
Higuchi et al. [4] described trapped penis as when the penile shaft becomes trapped within the scrotal skin, below a sub-coronal scar.
Complex buried penis is used for cases in which there are multiple causative factors resulting in burial of the penis – for example, patients suffering from both obesity and lymphoedema. Inevitably these patients prove very difficult to treat, often requiring multiple surgeries, delayed healing and a longer time to achieve satisfactory postoperative results [3].
Buried penis is becoming an increasingly common problem and has a variety of possible presenting complaints. With obesity becoming a progressively more common burden on society and healthcare, it is likely that buried penis will continue to present more frequently in the future.
Aetiology
Buried penis can be caused by congenital or acquired conditions.
For the purposes of this review, we will be discussing buried penis in adults.
Buried penis is most commonly due to (summarised in Table 1):
Table 1.
Table summarising the causes of buried penis
| Causes of buried penis |
|---|
|
(a) Obesity
Obesity is a growing epidemic. The central and suprapubic areas of the abdomen tend to be the preferential areas of adipose tissue deposition in men and can present a challenge to lose [5].
Whilst not every obese male will suffer from this condition, Higuchi et al. [4] reported that 87% of men that received surgical treatment for buried penis were obese.
Whilst there is no specific body mass index (BMI) that correlates with a certain percentage risk of developing buried penis, this may be something that is used in the future [4].
(b) Penoscrotal lymphodema
Penoscrotal lymphodema is an uncommon cause of buried penis. It causes a deformity of the shaft and scrotum, resulting in a buried penis. Facio et al. [6] discussed the need for combination treatment for the management of lymphoedema – including compression garments and mechanical drainage of lymph.
When attempting to treat buried penis in cases of penoscrotal lymphoedema, it is important to note that surrounding tissue can also be involved and can later result in recurrence or failure of grafts [6].
(c) Post-circumcision
During circumcision, a circumferential incision is made. The leftover foreskin is then removed and the proximal skin is sutured to mucosa. In some cases, too much foreskin is removed (also called radical circumcision) or the suture line constricts post-operatively and cause cicatricial scarring. This can trap the penis in the remaining foreskin or push the penis into the suprapubic area, leading to a buried penis.
(d) Persistent infection
Significant overlying abdominal fat creates an environment that encourages bacterial and fungal growth. This is often exacerbated by the fact that patients who are obese are more likely to develop type II diabetes mellitus. This may present difficulty in successfully and promptly managing the buried penis, as all infections should be treated completely before any surgical intervention. Recurrent infections can also lead to scar contracture, which causes prepubic skin to shift over the shaft and glans, thereby invaginating the skin of the shaft and leading to a buried penis.
(e) Balanitis xerotica obliterans
Balanitis xerotica obliterans (BXO) is a chronic inflammatory dermatological process that causes sclerosis of the glans, shaft, prepuce or urethra, which can result in a cicatrix of the distal penis, thereby trapping it. Treatment is usually with medical management.
(f) Dysgenic dartos
Higuchi et al. [4] described dysgenic dartos as dartos fascia that does not adequately attach the skin of the penis to the deep fascia surrounding the suspensory ligament. Alter et al. [7] state that the lack of dorsal support, alongside the hypermobility of the ventral skin and the dartos fascia, mean they do not attach adequately to the penis, thereby allowing it to ‘telescope’ into the scrotum – creating a ‘buried’ penis. Failure to identify this issue prior to surgery results in suboptimal results due to inappropriate reconstruction.
Presentation
The consequences of this condition can have a significant impact on the quality of life of patients. Patients may present in various ways (summarised in Table 2) including:
Table 2.
Table summarising the presenting symptoms of buried penis
| Presenting symptoms |
|---|
|
(a) Lower urinary tract symptoms
In their retrospective analysis of clinical outcomes following surgery, King et al. [8] described lower urinary tract symptoms as being the most common presenting complaint amongst those with buried penis. Patients may complain of the inability to control the passing of urine, particularly whilst standing, due to being unable to manipulate their penis to direct stream. This results in poor flow, hesitancy, post-void dribbling and incontinence.
(b) Erectile dysfunction and painful sex
Whilst patients may be able to develop erections, erections may be painful due to stretching of the overlying skin, which is immobile. Skin may then lacerate and bleed during sexual intercourse and penile sensation can become altered. Sexual intercourse may even be impossible if the penis is completely concealed.
(c) Soft tissue infections and urinary tract infections
The overhanging skin creates an environment that encourages bacterial and fungal growth. As per King et al. [8], patients who are obese and have diabetes are more vulnerable to infection. Recurrent infections then act to perpetuate the problem by causing skin contractures and scarring.
(d) Phimosis
Buried penis can cause secondary phimosis. Phimosis is the inability to retract the prepuce behind the glans in uncircumcised males. Phimosis can occur post-circumcision or with BXO, when scarring and inflammation causes tightening of the prepuce, resulting in consequential impedance of urinary flow [9].
(e) Low self-esteem and depression
Pestana et al. [11] discussed the inevitable low mood and self-esteem patients experience when suffering from buried penis. It is pertinent to treat these patients promptly and address any psychosocial issues they may be facing.
Treatment
There are various treatments available to patients with buried penis.
It is important to note that non-surgical interventions have a place in management. Such interventions include conservative attempts at weight loss, prompt and thorough treatment of soft tissue infections and counseling for psychological symptoms.
This review will focus on the surgical management.
Bariatric surgery
Should conservative attempts at weight loss be ineffective, patients are offered bariatric surgery. Patients should have a BMI of 40 or over, or a BMI of 35–40 and have a ‘serious health condition’ [e.g. diabetes mellitus (DM) or hypertension] associated with their obesity in order to be considered [10]. They must also have tried all appropriate lifestyle changes, be counseled on the consequences of surgery and be prepared to commit to lifelong follow-up.
Patients can be offered either a gastric band, gastric bypass or sleeve gastrectomy and this should be done prior to surgical management of the buried penis. However, bariatric surgery often leaves patients with excess skin that can present similar problems to excess fat, leaving patients with a buried penis despite bariatric surgery [11].
Surgical approach
Various surgical approaches have been suggested in literature.
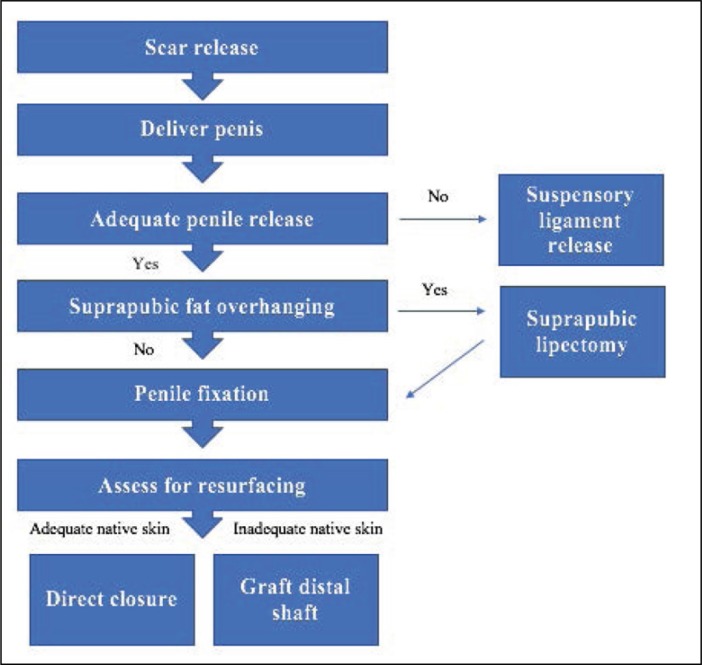
King et al. [8] developed a modified treatment algorithm employing a single surgical technique that incorporates aetiology and streamlines management (see Figure 1).
Figure 1.
Modified treatment algorithm by King et al. [8] (excluding children’s pathway).
Scar release
The primary step intra-operatively is scar release and mobilisation of the skin of the penis. It is important that the skin of the shaft is evaluated for viability both pre-operatively and intra-operatively. Mobility can be achieved in various ways, but usually involves releasing the dartos bands. In rare cases, where this is not possible, division of the suspensory ligament can be performed.
Fat removal
The next step, in those whom it is applicable, is usually fat removal. This is done to increase penile exposure. King et al. [8] suggest suprapubic lipectomy for overhanging fat. This is the technique most commonly used, however the following surgical techniques can also be employed (summarised in Table 3):
Table 3.
Table summarising the surgical techniques used for fat removal
| Surgical techniques |
|---|
| Panniculectomy |
| Suprapubic lipectomy |
| Abdominoplasty |
| Escutcheonectomy |
(a) panniculectomy – this involves removal of subcutaneous fat in the lower abdomen. A panniculectomy is indicated in patients who have excess skin that is a direct result of weight loss or bariatric surgery.
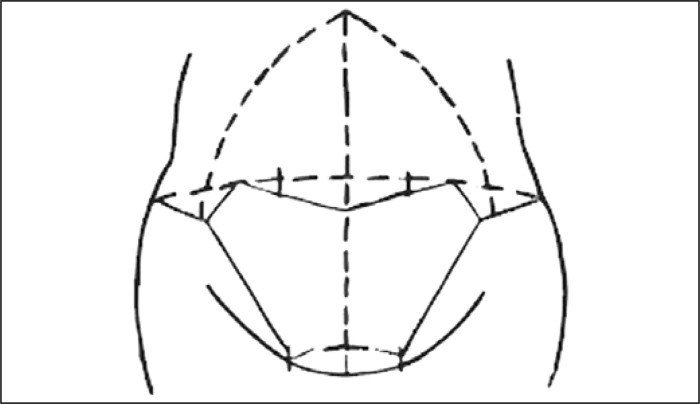
A V-shaped incision (see Figure 2) is made above the mons pubis and a Z-shaped incision made at the lateral margins in order to prevent overlapping of the abdominal flaps [12]. The incisions are then carried down to the rectus fascia and closed.
Figure 2.
Figure demonstrating the V-shaped incision above the mons pubis and lateral margin incisions made that are then carried down to the rectus fascia and closed.
Intraoperative blood loss is an important complication to be mindful of, as large panniculi can contain up to 700 ml of blood. Another complication that can be avoided is the formation of ‘dog ears’. It is important that patients are evaluated in both the standing and supine position prior to surgery in order to prevent ‘dog ears’ occurring at the anterior iliac spine.
Cooper et al. [12] found that higher BMI, hypertension and a large abdomen corresponded with higher rates of complication. However, in their nine-year study, there were high satisfaction rates post-panniculectomy, despite high complication rates.
(b) Suprapubic lipectomy – this involves resection of the suprapubic fat pad and tethering of the dartos bands to elongate the penis. It is indicated in patients in whom suprapubic fat remains despite several attempts at weight loss. However, contraindication to suprapubic lipectomy is morbid obesity, in which suprapubic lipectomy would be insufficient.
Preoperatively, the patient is marked for the procedure in the standing position as the landmarks of resection and particular amount of subcutaneous abdominal fat to be excised can be obstructed from view when the patient is lying down.
The suprapubic fat is then excised and the skin is secured to the rectus fascia. A W-shaped incision is made 2–3 cm from the base of the penis (see Figure 3), which allows for uncovering of the penile base position and can provide a suitable donor site for a skin graft [16].
Figure 3.
Figure demonstrating the excision of suprapubic fat and W-shaped incision made during suprapubic lipectomy.
The suprapubic area is then filled with large quantities of a tumescent solution (comprised of diluted local anaesthesia, saline and adrenaline) that encourages vascular congestion. Often following this, panniculectomy is performed, as suprapubic lipectomy alone is usually not effective enough.
The pubic skin and base of the penis is then sutured and secured to the rectus fascia. The site is then closed over a drain in a layered manner.
Complications include superficial wound infections, wound dehiscence, asymmetry of the abdomen and ‘dog-ears’, development of a seroma/haematoma and hypertrophic scarring.
(c) Abdominoplasty – this involves removal of excess fat and skin from the middle and lower part of the abdomen and tightening of the fascia and muscles of the abdominal wall (see Figure 4). Indications for abdominoplasty include excess skin and laxity of abdominal muscles following massive weight loss. However, like some of the other surgical techniques, a relative contraindication to abdominoplasty is morbid obesity.
Figure 4.
Figure demonstrating the prior markings and the initial inferior incision made in order to tighten the rectus abdominus during abdominoplasty (step 2).
Abdominoplasty and panniculectomy share some common features. Whilst both surgeries involve removal of excess skin, abdominoplasty also involves tightening of muscles and repositioning of the navel, leaving patients with a better cosmetic appearance. Abdominoplasty involves four key steps [13]:
Removal of excess fat and skin
Plication (or tightening) of the rectus abdominus, which is usually tightened from the xiphoid process, down to the pubic bone
Relocation of the umbilical stalk to provide a good aesthetic appearance
Closure of incisions
It should be noted that abdominoplasty can be combined with other cosmetic procedures to result in a better body contouring outcome.
Short-term complications from abdominoplasty include development of a haematoma or seroma, postoperative infection and wound dehiscence. Long-term complications tend to be surrounding scarring. Patients may also experience umbilical malpositioning.
Recovery usually takes between one and four weeks and compression hosiery or abdominal binders are often used to ensure contouring remains at its optimum.
(d) Escutcheonectomy [14, 15] – this involves the removal of the fat pad above the pubic area. Tang et al. [16] described the eschutcheon as the ‘tissue immediately above the penis, over which pubic hair is distributed’ that, in those with obesity, creates an overhanging area of tissue. This type of surgery is not commonly used. It can, however, be used in those who have complex concealed penis and require multiple surgical interventions. These cohorts of patients may require penile unburying, partial escutcheonectomy, de-fattening of the suprapubic fat pad and split-thickness grafting [17].
Surgery begins with a transverse incision that is curved in shape and forms a flap over the fat pad (see Figure 5) . This flap is then trimmed and defattened. The bottom part of the flap is then fixed to the suspensory ligament of the penis with sutures and the initial incision is closed.
Figure 5.
Figure demonstrating the transverse incision made and the trimming and defattening of the fat pads bilaterally.
Complications of this procedure include blood loss (which Tang et al. [16] found varied between 100 ml to 1.5 L), wound dehiscence and wound infection – with penile and scrotal infections occurring more often than abdominal infection.
It should be noted that escutcheonectomy is often performed alongside abdominoplasty in order to allow for better exposure of the penis, particularly when the patient is in the standing position. This is demonstrated in a study by Voznesensky et al. [18], in which ten out of twelve patients who underwent escutcheonectomy required abdominoplasty alongside to enable better aesthetic outcomes.
Penile fixation
Following fat removal, tacking sutures can be used from the tunica albuginea to the ventral subdermal dartos to prevent retraction of the penis into the fat.
Assess for resurfacing
Correction and reconstruction of skin defects is the final stage of management. If no abnormal shaft skin was removed, then primary closure is satisfactory. However, patients commonly require either z-plasty or skin grafting due to removal of diseased shaft skin intra-operatively.
Reconstruction of skin defects
Once diseased skin has been removed, various techniques can be employed to reconstruct defects.
Z-plasty
Z-plasty is a technique that can be used to improve the aesthetic outcome of scars(see Figure 6). A Z-shaped incision is made, with the interconnecting line being made along the greatest line of tension. The resulting two triangular flaps are then raised and transposed, thereby closing the skin. In this scenario, it can be used if a pensoscrotal web remains despite attempts at reconstruction and can increase ventral penile length when performed.
Figure 6.
Figure demonstrating the 90° Z-shaped incisions made at the penoscrotal junction for Z-plasty in penoscrotal web.
Skin autografting
In the case of z-plasty or primary closure not being possible, patients can undergo skin autografting. Grafts are harvested from the abdomen (if panniculectomy is performed) or the lateral thigh.
Most of the literature on the use of skin grafting to restore penile skin is regarding split-thickness grafts. However, thick split-thickness grafts and full split-thickness grafts have also been used. Deciding on which type of graft to use is imperative to the long-term success of the graft. Thakar and Dugi state that the decision on which graft to use depends on ‘anatomic and functional factors, disease process, ability of the penis to change size and normal graft healing and adherence’ [19].
When comparing grafts, data on split-thickness grafts show good adherence to site, whereas full split-thickness grafts show longevity. Split-thickness grafts are used more often in genital reconstruction because graft survival rates are good, they lack hair follicles and there is no need for a local flap or subsequent grafting [20]. Furthermore, penile skin is thin and has very little subcutaneous fat; therefore split-thickness grafting provides a good aesthetic match [2].
In comparison, thick grafts tend to provide the best durability and show reduced rates of graft-penile shrinkage, secondary contraction and fissure occurrence.
Following grafting, sutures are used to ensure adherence of the graft to the penis. This should include the superficial fascia tissue to encourage stabilisation.
Post-operatively
Many types of dressings have been suggested post-operatively. Pestana et al. [11] described the use of oiled cotton bolsters, penile splints and petroleum gauze. Most recently, negative-pressure dressings with vacuum-assisted closure have been used. This is the technique of using sub-atmospheric pressure, via controlled application to the wound, to promote healing. Importantly, the insertion of a urethral catheter can still be used in this type of closure and free urinary drainage is maintained.
Patients are kept on bed rest for two days and are then allowed to walk with the negative pressure wound vacuum therapy (NPWT) clamped. The dressing is kept on for a few days and is removed before the patient is sent home. At this point, the dressing can be changed to a more traditional petroleum gauze dressing.
Postoperatively, patients must be advised to abstain from sexual intercourse and heavy lifting. However, patients should be told that erections should not be avoided. In fact, the inability of the graft to expand during erection is indicative of early graft failure. This tends to occur most commonly with thicker grafts and can result in postoperative erectile dysfunction (which patients should be counseled about). In these instances, vacuum devices to assist erection can prove very effective.
Patients should also be informed that they may experience altered sensation over the split-thickness grafts, but should be able to experience satisfactory deep sensation to the phallus during sexual intercourse.
Postoperative follow-up data indicates that patients are now able to void whilst standing, have fewer soft tissue and urinary infections, do not suffer from any new lower urinary tract symptoms and have good aesthetic outcomes [21, 3, 22].
CONCLUSIONS
Buried penis is a condition that can be due to several causes. With obesity becoming more prevalent, we may see an increase in patients presenting in the future and clinicians may find themselves dealing with more complex, multifactorial cases of buried penis. This review aims to provide a comprehensive overview of the surgical management options for patients with buried penis.
Clinicians should be aware that this is likely to be a process that takes years to achieve success. Therefore, optimum planning prior to operating, educating patients on lifestyle measures and the postoperative process is important in effectively managing this condition.
Whilst it can be difficult to treat, the variety of treatment options available pose good outcomes and so management can be tailored to each individual’s needs.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Donatucci CF, Ritter EF. Management of the buried penis in adults. J Urol. 1998;159:420–424. doi: 10.1016/s0022-5347(01)63939-9. [DOI] [PubMed] [Google Scholar]
- 2.Gillett MD. Split-thickness skin graft for the management of concealed penis. J Urol. 2005;173:579–582. doi: 10.1097/01.ju.0000149606.27158.fa. [DOI] [PubMed] [Google Scholar]
- 3.Boonjindasup A, Pinsky M, Stewart C, et al. Management of adult concealed penis using a meshed, split-thickness skin graft. Canadian Urol Ass J. 2016;10:E407–E411. doi: 10.5489/cuaj.3787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Higuchi TT, Yagamuchi Y, Wood HM, Angermeier KW. Evaluation and treatment of adult concealed penis. Curr Urol Rep. 2012;13:277–284. doi: 10.1007/s11934-012-0255-z. [DOI] [PubMed] [Google Scholar]
- 5.Malloy TR, Wein AJ, Gross P. Scrotal and penile lymphedema: Surgical considerations and management. J Urol. 1983;130:263–265. doi: 10.1016/s0022-5347(17)51097-6. [DOI] [PubMed] [Google Scholar]
- 6.Facio M, Spessoto L, Gatti M, et al. Clinical treatment of penile fibrosis after penoscrotal lymphoedema. Urol Case Rep. 2017;11:14–18. doi: 10.1016/j.eucr.2016.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alter GJ, Ehrlich RM. A new technique for correction of the hidden penis in children and adults. J Urol. 1999;161:455.. [PubMed] [Google Scholar]
- 8.King IC, Tahir A, Ramanathan C, Siddiqui H. ISRN Urol. 2013. Buried penis: evaluation of outcomes in children and adults, modification of a unified treatment algorithm, and review of the literature; p. 109349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan IH, Wong KK. Common urological problems in children: prepuce, phimosis and buried penis. Hong Kong Med J. 2016;22:263–269. doi: 10.12809/hkmj154645. [DOI] [PubMed] [Google Scholar]
- 10.NICE guidelines . Obesity: identification, assessment and management. book. Available at: https://www.nice.org.uk/guidance/cg189/chapter/1-recommendations#surgical-interventions Accessed on [22.03.2017]. [Google Scholar]
- 11.Pestana IA, Greenfield JM, Walsh M, Donatucci CF, Erdmann D. Management of ‘buried’ penis in adulthood: an overview. Plast Reconstr Surg. 2009;124:1186–1195. doi: 10.1097/PRS.0b013e3181b5a37f. [DOI] [PubMed] [Google Scholar]
- 12.Cooper JM, Paige KT, Beshilan JM, Downey DL, Thirlby RC. Abdominal panniculectomies: high patient satisfaction despite significant complication rates. Ann Plast Surg. 2008;61:188–196. doi: 10.1097/SAP.0b013e318158a7b2. [DOI] [PubMed] [Google Scholar]
- 13.Abdominoplasty vs Panniculectomy: what is the difference? Available at http://drbrennerarticles.com/blog/abdominoplasty-vs-panniculectomywhat-is-the-difference/ Accessed on [08.06.2017]
- 14.Cavayero C, Cooper M, Harlin S. Adult-acquired hidden penis in obese patients: a critical survey of the literature. J Am Osteopath Ass. 2015;115:150–156. doi: 10.7556/jaoa.2015.028. [DOI] [PubMed] [Google Scholar]
- 15.Stokes TH, Follmar KE, Silverstein AD, et al. Use of negative-pressure dressings and split-thickness skin grafts following penile shaft reduction and reduction scrotoplasty in the management of penoscrotal elephantiasis. Ann Plast Surg. 2006;56:649–653. doi: 10.1097/01.sap.0000202826.61782.c9. [DOI] [PubMed] [Google Scholar]
- 16.Tang SH, Kamat D, Santucci RA. Modern management of adult-acquired buried penis. Urology. 2008;72:124–127. doi: 10.1016/j.urology.2008.01.059. [DOI] [PubMed] [Google Scholar]
- 17.Zucchi A, Perovic S, Lazzeri M, et al. Iatrogenic trapped penis in adults: new, simple 2-stage repair. J Urol. 2010;183:1060–1063. doi: 10.1016/j.juro.2009.11.030. [DOI] [PubMed] [Google Scholar]
- 18.Voznesensky MA, Lawrence WT, Keith JN, Erickson BA. Patient-reported social, psychological and urologic outcomes after adult buried penis repair. Urology. 2016;103:240–244. doi: 10.1016/j.urology.2016.12.043. [DOI] [PubMed] [Google Scholar]
- 19.Thakar HJ, Dugi DD., 3rd Skin grafting of the penis. Urol Clin North Am. 2013;40:439–448. doi: 10.1016/j.ucl.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 20.Weinfeld AB, Kelley P, Yuksel E, et al. Circumferential negative-pressure dressing (VAC) to bolster skin grafts in the reconstruction of the penile shaft and scrotunm. Ann Plast Surg. 2005;54:178–183. doi: 10.1097/01.sap.0000143606.39693.3f. [DOI] [PubMed] [Google Scholar]
- 21.Anderson KA, McAninch JW. Penile dressing splint. Urology. 1982;20:188. doi: 10.1016/0090-4295(82)90360-0. [DOI] [PubMed] [Google Scholar]
- 22.Warren AG, Peled ZM, Borud LJ. Surgical correction of a buried penis focusing on the mons as an anatomic unit. J Plast Reconstr Aesthet Surg. 2009;62:388–392. doi: 10.1016/j.bjps.2007.06.017. [DOI] [PubMed] [Google Scholar]