Abstract
Background:
Pneumonia is one of the most common hospital-acquired infections among bedridden patients in Intensive Care Units (ICUs). Colonization of mouth and pharynx by pathogenic bacteria and their aspiration into the lower respiratory tract is an important step in pathogenesis of hospital-acquired pneumonia. The purpose of this study was to compare the effects of chlorhexidine and potassium permanganate mouthwashes in preventing incidence of hospital-acquired pneumonia in hospitalized patients in the ICU.
Methods:
This study is a clinical trial, conducted on 150 patients on ventilator in ICU. Patients were divided into three groups: Chlorhexidine group, potassium permanganate group, and control group. Mouthwashing three times a day, each time 5 min for 1 week by sterile gas with 10 cc solution of chlorhexidine, potassium permanganate, or placebo, was performed. Finally, pneumonia incidence was recorded, according to the Center for Disease Control and Prevention criteria. The data were analyzed by SPSS software version 20.
Results:
In the present study, 28 cases of pneumonia among 150 patients on ventilator were investigated. There were 15 (30%), 6 (12%), and 7 (14%) incidences of pneumonia in control, chlorhexidine, and permanganate group, respectively. Pneumonia incidence in these groups differed significantly (P = 0.041).
Conclusions:
The use of common mouthwashes, especially chlorhexidine solution, for washing oropharynx of ICU patients, can decrease pneumonia incidence, especially in patients under ventilation. Thus, washing and sterilizing mouth of patients with mouthwashes is recommended due to the high risk of hospital-acquired pneumonia in these patients.
Keywords: Chlorhexidine, pneumonia ventilator associated, potassium permanganate
Introduction
Nowadays, hospital-acquired infections are one of the important causes of mortality and morbidity. According to the data, about 10% of bedridden cases in developed countries and 25% in developing countries lead to hospital-acquired infections. According to report of the World Health Organization, cost of hospital-acquired infections has been more than 20 billion US dollars.[1,2] Nosocomial infections are common in the Intensive Care Unit (ICU) patients.[3] Incidence of ICU-associated infections is 5 to 10 times more than acquired infections in general wards.[4,5] Hospital-acquired pneumonia, especially ventilator-associated pneumonia, is the leading cause of death in ICU, with mortality rate from 24% to 76%.[6]
ICU-associated infections increase morbidity, mortality, and hospitalization costs and duration. Preventing these infections by limiting their incidence and spread in hospitals can help to improve the patient's outcomes.[3]
Hospital-acquired pneumonia is appearance of infection in the lung, 48 h after hospitalization time, and generally, infectious agent enters the respiratory tract from nose, pharynx, and digestion tract.[7]
Criteria for clinical diagnosis of pneumonia include progressing infiltration in lung, fevers over 38.3°c, hypothermia below 36°c, leukocytosis over 12,000, or leukopenia below 4000 or purulent sputum. According to Center for Disease Control and Prevention (CDC) criteria, pneumonia is mooted in patients who possess radiologic documents, signs, and proved tests.[3] Colonization of oropharynx and stomach by Gram-negative pathogens will extend in unable patients immediately after hospitalization.[3]
Since bacterial colonization in mouth and pharynx is a threat for vigorless patients in ICU, several strategies have been used to prevent colonization, such as nonabsorbable antibiotics. Nevertheless, long application of prophylactic antibiotics can lead to increase in resistant organisms and thus is not recommended.[4]
Another intervention is the use of antiseptics for oral hygiene. Chlorhexidine and potassium permanganate are products that have been studied up to now.[4]
Chlorhexidine is an antimicrobial agent which is less effective against Gram-negative bacilli; however, it has an extended spectrum against Gram-positive cocci such as oxacillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci. In all studies, this product is devoid of side effects and completely tolerable. Chlorhexidine is absorbed by tissues and its effect will remain until 5 h after application.[4] Chlorhexidine is a poly cationic bisbiguanide that tends to the mouth mucosal membrane, salivary gland proteins, bacterium, and mouth biofilm. It damages the bacteria cell wall and clots cytoplasmic proteins. Because of oxidative effect on bacteria cell wall, potassium permanganate has a feeble antiseptic function. Aseptic effect of chlorhexidine is 100 times more than potassium permanganate.[6]
The purpose of this study was to compare the effects of chlorhexidine and potassium permanganate mouthwashes in preventing incidence of ventilator-associated pneumonia in patients hospitalized in the ICUs.
Methods
This study is a clinical trial that has been done in the ICU of AL-Zahra Clinical and Training Center of Isfahan from 2011 to 2012. In the present study, hospitalized patients who were on ventilation in ICU were investigated.
Inclusion criteria for the study were:
ICU-admitted patients on ventilator for more than 48 h
Age over 18 years
No fever at the time of entering the ICU
No pneumonia and no allergy to the utilized drugs.
In case of patient's death or release from hospital before due date or appearance of drug complications, they were excluded from the study. They were also excluded if they had pneumonia before 48 h of hospitalization or ventilation.
A hundred and fifty patients were selected among those who had been admitted to the ICU of AL-Zahra Hospital during 1 year and had been on ventilator. These patients were divided into three groups randomly, including group A (chlorhexidine 0.2%), Group B (potassium permanganate 0.01%), and Group C (control group), each comprising 50 patients.
Mouth and pharynx washing of selected patients was done by the trained nurses, three times a day, each time 5 min, for 1 week by abslung and sterile gas with 10 cc solution.[6] Criteria for clinical diagnosis of pneumonia include fever over 38.3°c or hypothermia below 36°c, leukocytosis over 12,000, or leucopenia <4000 or purulent sputum. According to the CDC criteria, pneumonia is mooted in patients who possess radiologic documents, signs, and proved tests (including complete blood count [CBC] and chest X-ray [CXR]). The final diagnosis was done by radiologist and infectious disease medical doctors. Data collection was done by clinicians who fill the questionnaire and evaluation of CBC and CXR. Collected information was analyzed with SPSS version 20 for Windows (SPSS Inc, Chicago, IL, USA). Statistical tests used for the data analysis were data analysis, t-test, and Chi-square test.
Results
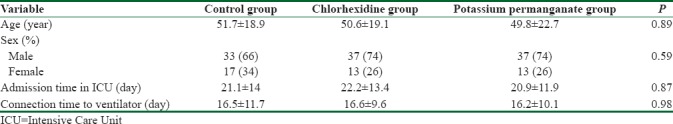
In this study, 150 patients hospitalized in the ICU were investigated from 2010 to 2011. The average age of all patients under study was 50.7 ± 20.2 years old. According to variance test, there was no significant difference between case and control groups in terms of age (P = 0.89) and sexual distribution (P = 0.59). The patients' average admission time in ICU and ventilator-connection period was 21.4 ± 13 and 16.4 ± 10.4 days, respectively. There was no significant difference between chlorhexidine, potassium permanganate, and control group in terms of duration of ICU admission (P = 0.87) and time on ventilator (P = 0.98) [Table 1].
Table 1.
Distribution of age, sex, Intensive Care Unit admission time, and duration on ventilator
During the study, 28 (18.7%) individuals were diagnosed with pneumonia out of 150 patients. The incidence of pneumonia was 15 cases in control group (30%), 6 cases in chlorhexidine group (12%), and 7 cases in permanganate group (14%). Chi-square test revealed that there is a significant difference in the incidence of pneumonia in the three groups (P = 0.041) [Table 2].
Table 2.
Incidence of pneumonia and mortality in cases and control groups
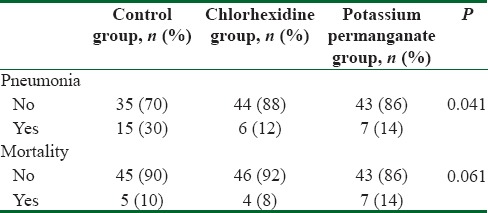
There were 16 patients who died during the study, including 5 patients from the control group, 4 patients from chlorhexidine group, and 7 patients from permanganate group [Table 3]. According to Chi-square test, the incidence of mortality revealed no significant difference between the three groups (P = 0.61).
Table 3.
Characteristic of patients among affected and not affected with pneumonia
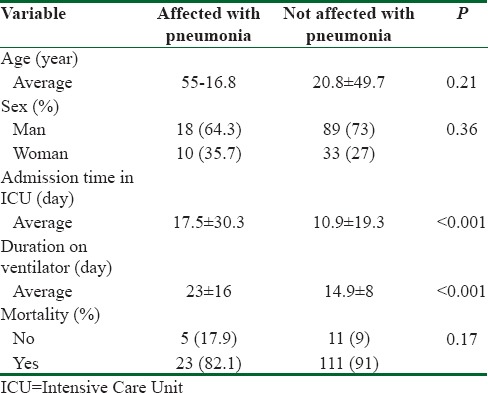
The average age of patients affected and nonaffected by pneumonia was 55 ± 16.8 and 49.7 ± 20.8 years old, respectively, and t-test showed no significant difference between the two groups.
There were 89 (73%) and 18 (64.3%) males in affected and nonaffected group, respectively. According to Chi-square test, the incidence of pneumonia did not have a significant difference between the two sexes (P = 0.36).
The average time of ICU admission was 30.3 ± 17.5 and 19.3 ± 10.9 days for patients affected and nonaffected by pneumonia, respectively, and according to t-test, the average residing time differed significantly between the two groups (P < 0.001).
The average age of control, chlorhexidine, and permanganate group was 51.7 ± 18.9, 50.6 ± 19.1, and 49.8 ± 22.7 years old, respectively, and according to variance analysis test, there was no significant difference between these three groups. Therefore, age has not had any effect on the outcome of study and groups have been comparable in terms of age. Similarly, the groups have been comparable in terms of sex since 66% of control group, 74% of chlorhexidine group, and 74% of permanganate group were men, and there was no significant difference between them.
Discussion
The main goal of this study was to determine the relative frequency of hospitalized pneumonia patients who have been underventilation and have been receiving 0.2% chlorhexidine oropharyngeal wash solution and 0.01% potassium permanganate compared to the control group at ICU of AL-Zahra Hospital (2010-2011).
The average age of patients hospitalized in ICU was 50.7 ± 20.2 years old which is similar to average age of patients who have been hospitalized in ICU due to other reasons.
Patients who have been hospitalized in ICU, in general, are more susceptible to hospital-associated infections compared to other patients. First of all, patients in ICU are typically older and their immune system is weaker compared to young individuals. Second, the elderly usually have bone and joint problems and do not have enough movement. Thus, they are more susceptible to infections, especially in their respiratory tract.
Moreover, other illnesses such as diabetes increase hospital-associated infections in these patients.
In the present study, the incidence of pneumonia in patients who had received mouthwash was less than patients who had not receive it (30% in control group, 12% chlorhexidine group, and 14% permanganate group). Furthermore, the incidence of pneumonia in chlorhexidine group was less than permanganate group, and there was a significant difference between the groups.
Bellissimo-Rodrigues et al. accomplished that chlorhexidine 0.12% cannot prevent the incidence of respiratory tract infection in patients hospitalized in ICU.[8] Furthermore, scan apiece et al. (2009) found that the use of chlorhexidine 0.12% does not have any role in deduction of oropharyngeal colonization, mortality, incidence of pneumonia with ventilator, and duration of hospitalization.[9]
In a study that was executed by Panchabhai and et al. in 2009, it was revealed that the use of chlorhexidine 0.2% does not decrease the incidence of pneumonia in hospitalized patients in ICU, but the use of mouthwash can decrease incidence of pneumonia, a part from ingredients of that mouthwash.[6] In this study, the incidence of pneumonia was compared between chlorhexidine and permanganate group.
Furthermore, according to the results of a study that was conducted by Beraldo and Andrade in 2008, the use of chlorhexidine decreases ventilator-associated pneumonia, whereas this method is harmless, tolerable and does not have side effects.[4]
A study that was conducted by Sebastian et al. on 63 patient who needed intubation in 2012 has shown that the use of chlorhexidine for disinfecting mouth does not prevent ventilator-associated pneumonia in 3-month to 15-year-old children.[10] However, a study that was done by Scannapieco and Binkley in 2012 has shown that the use of chlorhexidine decreases the incidence of ventilator-associated pneumonia.[11]
One research showed that application of a preintubation dose of chlorhexidine did not provide benefit over the postintubation chlorhexidine to reduce the risk of early-onset VAP.[12]
A recent study from Brazil has shown that oral hygiene through toothbrushing plus chlorhexidine in gel at 0.12% reduces the incidence of ventilator-associated pneumonia, the duration of mechanical ventilation, the length of hospital stay, and the mortality rate in ICUs, when compared to oral hygiene only with chlorhexidine, although the difference was not statistically significant (P = 0.084).[13]
Our data demonstrate that the use of mouthwash in patients hospitalized in ICU decreases colonization of bacteria in oropharynx which, in turn, decreases pneumonia incidence. Therefore, application of chlorhexidine 0.2% as mouthwash can ensconce in guarding guideline of patients hospitalized in ICU.
Other effective parameter in the incidence of pneumonia was duration of hospitalization in ICU and duration of connection to the ventilator. Patients with longer ICU admission suffered from unfavorable conditions, in addition to more prevalence of pneumonia.
Longer ICU admission or longer connection to ventilator are reasons discussed in this study that cause accumulation of infectious agents. In other words, longer connection of patients to the ventilator, which is an infection source, causes transmission of infectious agents from ventilator to the lung.
One of the actions that have been done in developed countries is oral cares by an independent team. Since oral care is an unfavorable task, nurses do not tend to do it and may be neglected in standard cares of ICU patients. Thus, this task should be considered as an important item in nursing training program and continuing education.
Conclusions
According to the results of the present study, the use of common mouthwashes, especially chlorhexidine for cleaning oropharynx of hospitalized patients in ICU, can decrease the incidence of pneumonia in patients on ventilation remarkably. Thus, due to high risk of incidence of acquired pneumonia in patients under ventilation, the use of mouthwash solutions for disinfecting mouth of patients is recommended.
Financial support and sponsorship
This project was fully sponsored by Research Council of Isfahan University of Medical Sciences, Isfahan, Iran.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Emmerson AM, Enstone JE, Griffin M, Kelsey MC, Smyth ET. The second national prevalence survey of infection in hospitals – Overview of the results. J Hosp Infect. 1996;32:175–90. doi: 10.1016/s0195-6701(96)90144-9. [DOI] [PubMed] [Google Scholar]
- 2.Weinstein RA. Nosocomial infection update. Emerg Infect Dis. 1998;4:416–20. doi: 10.3201/eid0403.980320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barsanti MC, Woeltje KF. Infection prevention in the Intensive Care Unit. Infect Dis Clin North Am. 2009;23:703–25. doi: 10.1016/j.idc.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 4.Beraldo CC, Andrade DD. Oral hygiene with chlorhexidine in preventing pneumonia associated with mechanical ventilation. J Bras Pneumol. 2008;34:707–14. doi: 10.1590/s1806-37132008000900012. [DOI] [PubMed] [Google Scholar]
- 5.Aly NY, Al-Mousa HH, Al Asar el SM. Nosocomial infections in a medical-surgical Intensive Care Unit. Med Princ Pract. 2008;17:373–7. doi: 10.1159/000141500. [DOI] [PubMed] [Google Scholar]
- 6.Panchabhai TS, Dangayach NS, Krishnan A, Kothari VM, Karnad DR. Oropharyngeal cleansing with 0.2% chlorhexidine for prevention of nosocomial pneumonia in critically ill patients: An open-label randomized trial with 0.01% potassium permanganate as control. Chest. 2009;135:1150–6. doi: 10.1378/chest.08-1321. [DOI] [PubMed] [Google Scholar]
- 7.Donowitz LG, Wenzel RP, Hoyt JW. High risk of hospital-acquired infection in the ICU patient. Crit Care Med. 1982;10:355–7. doi: 10.1097/00003246-198206000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Bellissimo-Rodrigues F, Bellissimo-Rodrigues WT, Viana JM, Teixeira GC, Nicolini E, Auxiliadora-Martins M, et al. Effectiveness of oral rinse with chlorhexidine in preventing nosocomial respiratory tract infections among Intensive Care Unit patients. Infect Control Hosp Epidemiol. 2009;30:952–8. doi: 10.1086/605722. [DOI] [PubMed] [Google Scholar]
- 9.Scannapieco FA, Yu J, Raghavendran K, Vacanti A, Owens SI, Wood K, et al. A randomized trial of chlorhexidine gluconate on oral bacterial pathogens in mechanically ventilated patients. Crit Care. 2009;13:R117. doi: 10.1186/cc7967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sebastian MR, Lodha R, Kapil A, Kabra SK. Oral mucosal decontamination with chlorhexidine for the prevention of ventilator-associated pneumonia in children – A randomized, controlled trial. Pediatr Crit Care Med. 2012;13:e305–10. doi: 10.1097/PCC.0b013e31824ea119. [DOI] [PubMed] [Google Scholar]
- 11.Scannapieco FA, Binkley CJ. Modest reduction in risk for ventilator-associated pneumonia in critically ill patients receiving mechanical ventilation following topical oral chlorhexidine. J Evid Based Dent Pract. 2012;12:103–6. doi: 10.1016/j.jebdp.2012.03.010. [DOI] [PubMed] [Google Scholar]
- 12.Munro CL, Grap MJ, Sessler CN, Elswick RK, Jr, Mangar D, Karlnoski-Everall R, et al. Preintubation application of oral chlorhexidine does not provide additional benefit in prevention of early-onset ventilator-associated pneumonia. Chest. 2015;147:328–34. doi: 10.1378/chest.14-0692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.de Lacerda Vidal CF, Vidal AK, Monteiro JG, Jr, Cavalcanti A, Henriques AP, Oliveira M, et al. Impact of oral hygiene involving toothbrushing versus chlorhexidine in the prevention of ventilator-associated pneumonia: A randomized study. BMC Infect Dis. 2017;17:112. doi: 10.1186/s12879-017-2188-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


