Abstract
Patient: Male, 61
Final Diagnosis: SVC syndrome
Symptoms: Dyspnea
Medication: —
Clinical Procedure: —
Specialty: Oncology
Objective:
Unusual clinical course
Background:
Superior vena cava (SVC) syndrome can result from external compression or invasion of the vessel from structural pathology within the mediastinum. Here we present a case of a patient that had no airway compromise, but who had hemodynamic instability due to pulmonary vasculature compression requiring urgent intervention.
Case Report:
A 61-year-old male who presented with severe dyspnea was found to have newly diagnosed small cell carcinoma of the right lung. The carcinoma compressed the SVC as well as the right pulmonary artery (PA) as seen on computed tomography scanning. He became critically hypoxic and was emergently intubated. Due to the lack of airway compromise, this instance of SVC syndrome was not emergently treated with radiation or chemotherapy. However, he received appropriate treatment while on mechanical ventilatory support and eventually recovered.
Conclusions:
SVC syndrome is considered an emergent condition in the setting of airway compromise. With the addition of PA compression, a case’s acuity should be reconsidered. Our case highlights the fact that SVC syndrome can be associated with compression of the right PA, due to its close proximity to the SVC. This can lead to rapid hemodynamic deterioration, thereby increasing the acuity when evaluating a patient with SVC syndrome. We recommend emergent intervention to be taken when a patient develops this combination of SVC syndrome and PA compromise.
MeSH Keywords: Lung Neoplasms, Small Cell Lung Carcinoma, Superior Vena Cava Syndrome
Background
Superior vena cava (SVC) syndrome can result from external compression or invasion of the vessel from structural pathology within the mediastinum or from thrombosis. Rapid evaluation and management are necessary for malignancy-related SVC syndrome particularly if due to rapidly progressing tumors. In general, SVC syndrome is not considered life-threatening when there is no compromise to the airway. Here we present a case of a patient that had no airway compromise, but who presented with hemodynamic instability due to pulmonary vasculature compression, requiring urgent intervention.
Case Report
A 61-year-old Caucasian male with a history of heavy tobacco use for many decades presented to the Emergency Department because of significant dyspnea at rest associated with swelling in both of his lower extremities. His examination revealed congested neck veins, normal breath sounds, and a regular pulse. He required 3 L of oxygen via nasal cannula to maintain an oxygen saturation of 97%. An x-ray of his chest showed a large mediastinal mass, and follow-up computed tomography (CT) of the chest showed SVC syndrome as well as significant compression of the right pulmonary artery (PA) due to the same mass (Figures 1, 2). His echocardiogram showed right ventricular failure with severe pulmonary hypertension indicated by a right ventricular systolic pressure (RVSP) above 70 mmHg. A bronchoscopy with a biopsy was done, which revealed small cell carcinoma; he remained on telemetry monitoring while awaiting the biopsy results. One week after admission, he was noted to be in acute respiratory distress. This was compounded by atrial fibrillation which increased his heart rate into the 150s. He was subsequently intubated and transferred to the medical intensive care unit where he was difficult to ventilate. Given his SVC syndrome in conjunction with right PA compression and hemodynamic instability, emergency chemotherapy with cisplatin was initiated by the Oncology Team. Radiation Oncology was also consulted, but due to his critical illness, he was unable to receive radiation therapy at our facility. With chemotherapy, the patient gradually improved and was eventually extubated and discharged home on oxygen via nasal cannula.
Figure 1.
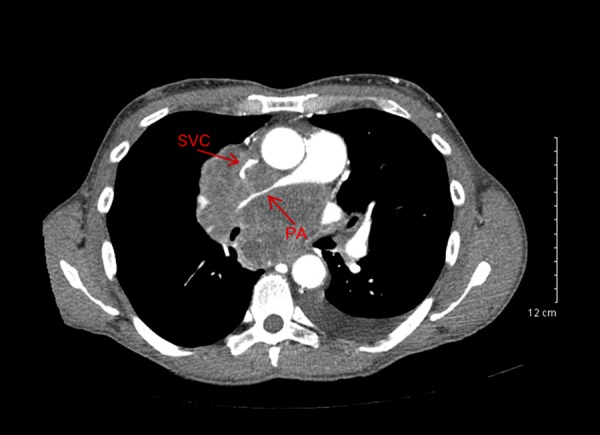
Transverse view of the thorax showing significant compression of the right pulmonary artery (PA). Superior vena cava (SVC) and pulmonary artery are indicated with arrows.
Figure 2.

Coronal view of the thorax demonstrating compression of the superior vena cava (SVC).
Discussion
Superior vena cava (SVC) syndrome results from any condition that leads to obstruction of blood flow through the SVC. Obstruction can be caused by thrombosis of blood within the SVC, or from invasion or external compression of SVC by a pathological process involving adjacent structures like the right lung, lymph nodes, or ascending aorta [1]. An intrathoracic malignancy accounts for 60–85% of all SVC syndromes. Non-small cell lung cancer is responsible for 50% of all cases followed by small-cell lung cancer and non-Hodgkin lymphoma [1]. Intrathoracic malignancies rarely cause compression of the main PA or one of its branches, but which can result in severe right ventricular hypertension and right ventricular failure. External compression of the PA is a rare but life-threatening entity due to decreased oxygenation and severe ventilation perfusion mismatch [2].
In the setting of new radiographic findings of a mediastinal mass, the possibility of SVC syndrome should always be a differential diagnosis. Treatment of SVC syndrome is aimed at symptomatic relief and treating the underlying cause [3]. Based on the current guidelines, urgent intervention in SVC syndrome should only be undertaken in the setting of laryngeal edema leading to airway compromise or with cerebral edema and underlying confusion [4]. There were no such signs in our patient. In fact, based on a published grading system, he would have fallen into the mild category which is grade 1 out of 5 [5]. On the other hand, in our patient’s case, the patient had hemodynamic instability due to extrinsic compression of the right PA coupled with SVC obstruction. His SVC obstruction led to significant preload reduction which was accentuated by atrial fibrillation. The concomitant severe stricture of the right PA essentially caused a functional pneumonectomy, as seen on CT scan (Figure 3), with right ventricular dysfunction due to a significant rise in pulmonary pressures acutely. Our case highlights the importance of urgent intervention when SVC syndrome is associated with significant PA compression. This combined “SVC-PA syndrome” can lead to rapid hemodynamic deterioration and should be addressed promptly upon recognition. In situations where significant obstruction persists despite chemotherapy, PA and SVC stenting can be considered. After a review of the literature, the current guidelines for SVC syndrome do not indicate aggressive intervention to be taken in this clinical scenario. However, evidence suggests that in the presence of compression of the PA, causing significant hemodynamic compromise, percutaneous stenting of the PA should be considered [2].
Figure 3.
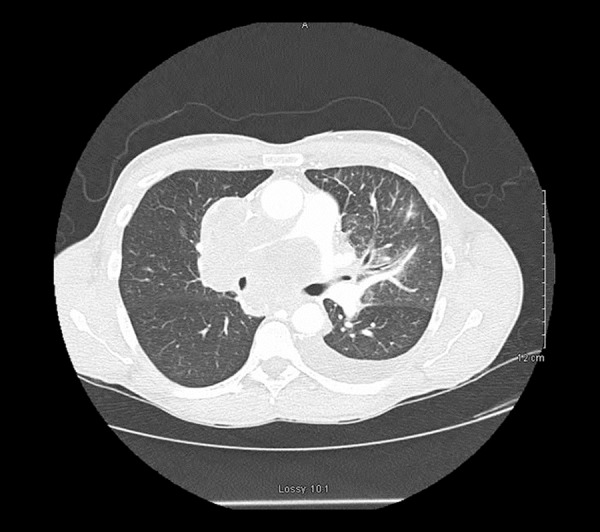
Transverse view of the thorax with the lung window representing significant decrease in lung markings in the right lung field.
Endovascular stenting is the current mainstay of treatment for life-threatening SVC syndrome. This provides the patient with significant relief and has been found to improve symptoms more rapidly than radiation therapy [6,7]. Although strong evidence on long-term results of endovascular stent placement is lacking [8], this intervention might result in a higher proportion of clinical relief of symptoms than chemotherapy and radiation treatment. Radiation therapy has less effect in the short-term and might lead to more significant complications, including edema [7]. Endovascular stenting is a relatively safe procedure to allow lung cancer patients to receive full doses of chemotherapy and radiation treatments without the fear of decompensation [9]. Extrinsic PA stenosis is treated with percutaneous PA stenting that results in relief of pulmonary hypertension and right heart failure. In this case, the patient might have benefitted from endovascular stenting of the SVC, as well as PA stenting versus more rapidly administered chemotherapy. As per the indications of PA stenting (Table 1) [10] an elevated RVSP would qualify for symptomatic response to stent placement. Our patient had a significantly elevated RVSP above 70 mmHg as seen on echocardiogram. In this case, perhaps earlier intervention with PA stenting would have prevented the rapid decompensation of our patient. With the additional tachycardia that he experienced, his cardiac output was likely severely diminished and was exacerbated by the lack of oxygen exchange via the right pulmonary vasculature.
Table 1.
Indications for pulmonary artery stenting.
| 1) Right ventricular peak systolic pressure (RVSP) equal to or greater than 50% of the aortic systolic pressure |
| 2) Quantitative pulmonary perfusion scans showing ipsilateral lung perfusion <35% than predicted in unilateral stenosis |
Conclusions
SVC syndrome is currently considered an emergent condition in the setting of airway compromise. With the addition of PA occlusion, the acuity of the case should be reconsidered. Our case highlights the fact that SVC syndrome can be associated with compression of other great vessels, especially the right PA due to its close proximity to SVC. This can lead to rapid hemodynamic deterioration and should be considered as a higher severity and a more emergent condition when evaluating a patient with SVC syndrome. We recommend more emergent intervention to be taken when patients develop this combination of SVC syndrome and PA compromise. Likewise, in our patient, hemodynamic instability and subsequent intubation could have been avoided with PA stenting early in his hospital treatment course.
Footnotes
Conflict of interest
None.
References:
- 1.Monaco R, Garcia, Bertoni H, et al. Use of self-expanding vascular endoprostheses in superior vena cava syndrome. Eur J Cardiothorac Surg. 2003;24(2):208–11. doi: 10.1016/s1010-7940(03)00293-8. [DOI] [PubMed] [Google Scholar]
- 2.Fierro-Renoy C, Velasquez H, Zambrano JP, et al. Cutaneous stenting of bilateral pulmonary artery stenosis caused by malignant extrinsic compression. Chest. 2002;122:1478–80. doi: 10.1378/chest.122.4.1478. [DOI] [PubMed] [Google Scholar]
- 3.Nickloes TA, Kallab AM, Dunlap AB. Superior vena cava syndrome treatment & management. Medscape. 2017. Available from: URL: https://emedicine.medscape.com/article/460865-treatment.
- 4.Straka C, Ying J, Kong FM, et al. Review of evolving etiologies, implications and treatment strategies for the superior vena cava syndrome. SpringerPlus. 2016;5:229. doi: 10.1186/s40064-016-1900-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.James YB, Wilson LD, Detterbeck FC. Superior vena cava syndrome a proposed classification system and algorithm for management. J Thorac Oncol. 2008;3:811–14. doi: 10.1097/JTO.0b013e3181804791. [DOI] [PubMed] [Google Scholar]
- 6.Anthony NA, Ettles DF, Arnold A, et al. Treatment of malignant superior vena cava obstruction: Metal stents or radiation therapy. J Vasc Interv Radiol. 1997;8(5):781–88. doi: 10.1016/s1051-0443(97)70660-2. [DOI] [PubMed] [Google Scholar]
- 7.Rowell NP, Gleeson FV. Steroids, radiotherapy, chemotherapy and stents for superior vena caval obstruction in carcinoma of the bronchus: A systematic review. Clin Oncol. 2002;14(5):338–51. doi: 10.1053/clon.2002.0095. [DOI] [PubMed] [Google Scholar]
- 8.Schindler N, Vogelzang RL. Superior vena cava syndrome. Surg Clin North Am. 1999;79(3):683–94. doi: 10.1016/s0039-6109(05)70032-3. [DOI] [PubMed] [Google Scholar]
- 9.Urruticoechea A, Mesia R, Dominguez J, et al. Treatment of malignant superior vena cava syndrome by endovascular stent insertion. Experience on 52 patients with lung cancer. Lung Cancer. 2004;43(2):209–14. doi: 10.1016/s0169-5002(03)00361-1. [DOI] [PubMed] [Google Scholar]
- 10.Mercieca V, Grech V, DeGiovanni JV. Use of stents for correction of pulmonary artery branch stenosis. Images Paediatr Cardiol. 2004;6(3):1–10. [PMC free article] [PubMed] [Google Scholar]


