Abstract
The trigeminocardiac reflex (TCR) is defined as a sudden onset of parasympathetic dysrhythmias during stimulation of the trigeminal nerve. We describe a peripheral variation of TCR during manipulation of the nasal mucosa. A 42-year-old patient suffering from severe obstructive sleep apnoea was scheduled for surgical treatment. After inducted anaesthesia, the surgeon infiltrated the nasal mucosa with a local anaesthetic. The patient immediately showed an asystole and was treated with ephedrine and five chest compressions, despite spontaneous sinus rhythm return after ceasing of manipulation. Treatment with atropine established this TCR episode and ensured an event-free surgery.
The authors present here, for the first time, a prolonged asystole caused by the TCR, triggered by minimal manipulation of the nasal mucosa. This severe manifestation of peripheral TCR demonstrates its importance in daily clinical business. This case was treated according to a modified treatment algorithm for all subtypes of TCR which is presented here.
Keywords: anaesthesia; cardiovascular medicine; arrhythmias; ear, nose and throat/otolaryngology; cranial nerves
Background
The trigeminocardiac reflex (TCR) is a generally accepted complication during surgery in areas that are innervated by the trigeminal nerve.1 2 It is triggered by either physical or chemical stimulation of the cranial nerve V (CN V) and clinically manifests as abrupt changes in haemodynamic parameters such as drop in blood pressure (BP) and/or heart rate (HR), apnoea and gastric hypermotility. Due to the acute onset and potentially fatal consequences (bradycardia up to a flat line in ECG), the central TCR gained increasing interest during its first clinical evaluation 1999.3 The TCR is well studied when triggered intracranially (eg, during surgery in the cerebellopontine angle), known as central TCR1 4 5 and extensively studied when triggered around the orbita, known as the oculocardiac reflex (OCR).6 7 Anyhow, next to the OCR, there are more peripheral variants of the TCR with a trigger point around the course of CN V before entering the petrous bone,8 and one possible trigger point is the facial skin and nasal mucosa. This case report presents a sinus arrest (absence of electrical impulses to stimulate myocardial fibres) with prolonged asystole (absence of ventricular contractions) caused by a puncture of the nasal mucosa.
Asystole in peripheral TCR is extremely rare and rarely described in the literature. The authors here describe, for the first time, an abrupt and prolonged asystole during minimal stimulation of nasal mucosa and discuss these findings in the context of the existing literature on the TCR.
Case presentation
A 42-year-old Caucasian male patient was scheduled for functional nasal septum plastic, bilateral endoscopic submucosal turbinoplastic, tonsillectomy, Fairbanks incision of the palatopharyngeal pillar and radiofrequency ablation of the soft palate to treat his mild obstructive sleep apnoea (OSA). The patient was preoperatively checked by the anaesthetist and had a normal body mass index (BMI) of 24.9 kg/m2 (79 kg, 178 cm). There was no regular medication intake. The patient was classified as ASA II (American Society of Anesthesiologists) due to nicotine consumption (20 cigarettes per day, 20 pack years), Gilbert’s syndrome and a previous allergic reaction (exanthema) to morphine. In polysomnography, the patient showed an apnoea–hypopnoea index (AHI) of 7/h. The Epworth sleepiness scale was 4/24 points. Rhinoscopy demonstrated obstructive synechiae after bilateral tamponade for epistaxis treatment in 2015 and a deviation of the nasal septum to the right side.
Physical examination presented no pathological findings, perioperative vital sign presented as BP 145/94 mm Hg, HR showed a normal sinus rhythm of 78 beats/min (bpm) and 98% oxygen saturation in room air. Preoperative laboratory examination and 12-channel ECG was not performed due to the young age and the good health condition of the patient.
The patient did not seem anxious and did not receive any premedication. Before induction of anaesthesia, standard monitoring was attached, including non-invasive BP, 5-channel ECG, oxygen saturation and train of four (TOF) monitoring. After 2 min of preoxygenation, anaesthesia was intravenously induced by target-controlled infusion of propofol 9 µg/mL, remifentanil 0.5 ng/mL, a bolus of fentanyl 0.25 mg and atracurium 40 mg. After complete relaxation in TOF monitoring, endotracheal intubation with a no. 3 Macintosh blade and an 8 mm RAE Tube was performed without any difficulty and no changes in sinus rhythm. Bispectral Index (BIS) monitoring was attached after induction and anaesthesia was maintained with propofol 3–5 µg/mL, remifentanil 4–8 ng/mL and fentanyl bolus if inadequate analgesia with remifentanil. Fifteen minutes after tracheal intubation, the surgeon started to infiltrate the mucosa of the lateral nasal wall and the septum with 0.5 mL of a lidocaine/epinephrine 1:1000 mixture. At the moment of nasal mucosal puncture, the patient developed a sudden asystole.
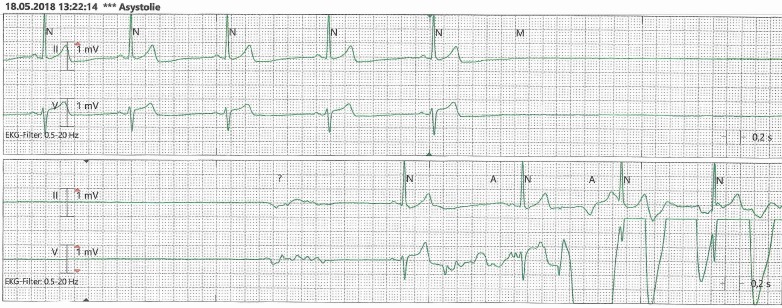
As demonstrated in figure 1, the five-lead ECG showed a stable sinus bradycardia during steady-state of anaesthesia. With the nasal puncture, a sudden sinus arrest with a flat line in ECG occurred. There was no presence of an escape rhythm, neither junctional nor ventricular. The surgeon was informed and the infiltration was interrupted. The sinus arrest persisted for 10 s when sinus bradycardia reappeared and five chest compressions were performed (visible as artefacts in rhythm, best seen in ECG lead V at the end of the timeline) while 9 mg ephedrine was established. The patient’s sinus rhythm returned with a HR baseline of 54 bpm. One minute later, the surgeon punctured the nasal mucosa again and the patient showed a sudden sinus bradycardia of 30 bpm. Injection of local anaesthetic (LA) was ceased again and atropine 0.5 mg was administrated. After a significant reaction to atropine (raise of HR from 54 to 78 bpm) another puncture and injection of 1 mL lidocaine/epinephrine showed no effect on the HR. BP was measured every minute and maintained at baseline during the episode of asystole and bradycardia while BIS monitoring showed a constant value between 38 and 42.
Figure 1.
Monitored ECG during puncture of nasal mucosa.
Outcome and follow-up
There was no other episode of bradycardia during the remaining surgery. At the end, the patient was successfully extubated and transferred to postanaesthesia care unit for further observation. A postoperative ECG showed regular sinus rhythm with early repolarisation and postoperative high-sensitive troponin T showed no elevation 4 hours after asystole. A cardiological consultation recommended no further evaluation of persistent heart disease.
Discussion
The present case demonstrates a sinus arrest with prolonged asystole induced by peripheral TCR. It shows also a unique pattern that we discuss in the following. Relevant literature was obtained for a further review.
This case describes a clinically significant drop in HR and asystole due to TCR triggered by physical and/or chemical stimulation of the nasal mucosa during injection of LA. These two episodes of bradycardia and asystole, respectively, present the typical diagnostic criteria of the TCR, earlier elaborated for a proper clinical definition by part of the authors.9 These events fulfil the two major criteria (plausibility and reversibility) and the two minor criteria (repetition and prevention). In contrast to the majority of recent studies on TCR, the presented case highlights the importance of these minor criteria. This temporal relationship underlines the reflexive character (vasovagal) of this event of sudden asystole. However, for clinical evaluation and definition of the TCR, a verification through the minor criteria is not practicable, from an ethical and medical point of view, in (any) clinical setting.
The classic classification9 divides the TCR into three subgroups according to the localisation of a stimulus: a central (proximal) TCR, a peripheral (distal) TCR and a Gasserian ganglion TCR. In this case, the stimulus is located at the anterior portion of the nose; mucosa of the anterior nasal septum and the lateral nasal wall, both innervated by the anterior ethmoidal nerve. This nerve derives from a direct continuation of the nasociliary nerve, coming from the ophthalmic nerve (V1), one of the three branches of the trigeminal nerve. The present case is, therefore, a good example of a ‘parasympathetic generalisation,9 that is not yet reported for the TCR. According to the clinical surrogate definition of the TCR, a peripheral TCR manifests as a drop in HR of ≥20% with prior stable values in BP or even hypertension.10 In this context, the present case underlines the recently adapted definition of the TCR.10
TCR is observed in a selection of patients with the same (surgical) procedure. Depending on the type of surgery and the involvement of the TCR central/peripheral subtype, the various prevalence ranges between 11% for surgery in the cerebellopontine angle3 up to 90% in strabismus surgery.11 It is also estimated that there is a higher prevalence in children than adults, based on their different, age-related reactivity of the autonomous nerve system. Various general risk factors for the occurrence of the TCR were discussed in the literature, some with stronger evidence (eg, type of surgery and technique,12 light plane anaesthesia13 and fast-acting opioids14) and others without clear evidence (eg, patients cardiac condition and beta-blocking agents). In the case presented h the only possible risk factor was the use of fast-acting opioids such as remifentanil. The combination of the nasal mucosa that is very prone to the TCR and the use of fast-acting opioids may have led to this severe event as described in an often performed intervention. Additionally, patients-related risk factors seems to be relevant; reports accumulate that suggest genetic polymorphisms and/or mutations of specific genes that make certain patients prone for the occurrence of the TCR.15 However, a multiple risk model seems therefore to be a valuable explanation for the occurrence of the TCR.
Research of relevant literature shows only one case of a cardiac arrest after similar stimulation of the CN V. In 1999, Bailey described an acute onset of bradycardia after nasal insertion of a temperature probe with an immediate recurrence of normal HR after removal.16 Repetitive insertion caused 3 s of reoccurring sinus arrest. In contrast to our case, manipulation of nasal mucosa first caused bradycardia—asystole only occurred gradually after repeated stimulation and was of shorter duration. Further, the TCR occurred immediately after administration of multiple drugs with cardiac depressive effects (such as alfentanil, thiopenthal, droperidol and vecuronium) for induction of anaesthesia. In our case, the patient showed asystole 15 min after induction with a steady state in haemodynamic parameters while BIS monitoring proved the adequate depth of narcosis. Therefore, this is the first time that an abrupt sinus arrest with prolonged asystole after minimal stimulation of the nasal mucosa is presented.
Further reported cases observed asystole during less similar settings, such as during surgery with major manipulation of the nasal skin and deeper structures, for example, dissection of the right frontal recess,17 after surgery possibly caused by nasal packing18 or ventricular fibrillation caused by local administration of minimal doses of epinephrine in the nasal mucosa.19 Different to those cases, we observed a manifestation of TCR as asystole during minimal manipulation in a surgery setting and there they are not comparable.
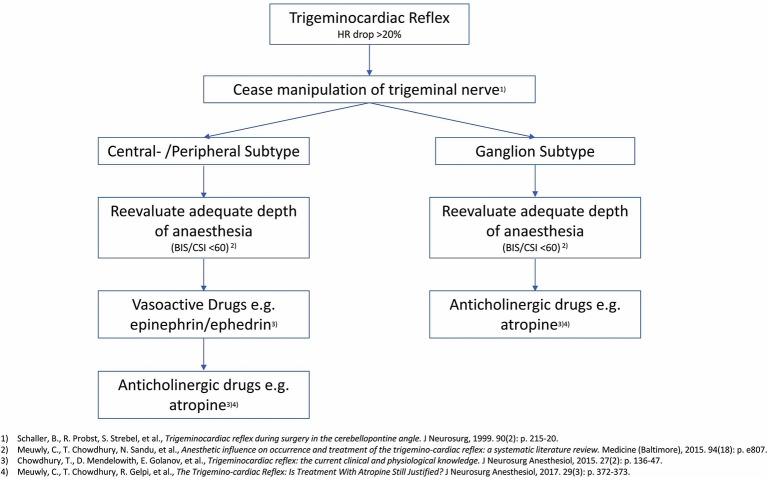
In this case of peripheral TCR, the state-of-the-art treating algorithms for the central TCR were followed.20 21 According to the actual scientific consensus, treatment of TCR should consider cessation of all possible stimuli first. This may represent the most successful treatment and is often sufficient to restore normal baseline values of haemodynamic parameters. The second step is the survey of the adequate depth of anaesthesia,13 the third step is the administration of vasoactive drugs (with positive inotrope and chronotropic effect) such as epinephrine or ephedrine. The use of vasoactive drugs is recommended in the central and peripheral subtype. In the ganglion subtype, the TCR can manifest in multifaceted changes in haemodynamic parameters (including hypertension)9 22 and therefore the cessation of the stimulus is the best option. Only if this treating cascade is not successful or the TCR reoccurs, administration of atropine is considered.20 It is essential to have an adequate depth of anaesthesia (BIS 40–60) as it has been shown that a BIS >60 is related to a higher incidence of TCR. Chowdhury et al even showed a case where the recurrent manifestation of TCR was successfully treated with a bolus of propofol.23 Administration of atropine should be considered only as second-line therapy due to its various side effects and proarrhythmic potential. Atropine can be helpful, as shown in this case report, to provide a safe setting for surgery in cases with recurrent TCR.
The presented case describes a peripheral variation of TCR. As there are no evaluated treatment algorithms for this subtype, the already established treatment protocol for the central subtype, as described above, was applied. Further, an appropriate depth of anaesthesia with a BIS around 40 was ensured. The presented manifestation of TCR demonstrates that sinus arrest can occur, despite an adequate depth of anaesthesia. Cease of manipulation often suffices for initiation of sinus rhythm, as seen in our case. After the spontaneous return of HR, chest compressions and medical intervention (such as ephedrine) were performed but not necessary. Administration of atropine, as postulated nearly 20 years ago,3 can be necessary to ensure a safe surgery in repetitive episodes of TCR. In our case, it guaranteed a successful continuation of surgery. The modified treatment algorithm, considering the three TCR subtypes, is presented in figure 2.
Figure 2.
Modified treatment algorithm for TCR. BIS, Bispectral Index; CSI, cerebral state index; TCR, trigeminocardiac reflex.
Learning points.
The trigeminocardiac reflex can cause sudden, clinically highly relevant arrhythmias until cardiac arrest during manipulation of the trigeminal nerve.
Treatment of peripheral trigeminocardiac reflex (TCR) is considered similar to central TCR.
Treatment includes cease of manipulation, survey of the adequate depth of anaesthesia and vasoactive drugs. Anticholinergic drugs should be considered as a second-line treatment due to its proarrhythmic potential.
Acknowledgments
The authors thank Professor Tschopp, Head of ENT clinics at Cantonal Hospital Baselland for his participation in this case report. He provided essential details about the patient.
Footnotes
Contributors: CM: contributed planning, conception, data analysis and a proof of the manuscript. GL: contributed main input in discussion and interpretation of data. TR: helped interpreting the case report. BS: supervised the working process and supported the first author in planning and conception; finalised the discussion.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Koerbel A, Gharabaghi A, Samii A, et al. Trigeminocardiac reflex during skull base surgery: mechanism and management. Acta Neurochir 2005;147:727–33. 10.1007/s00701-005-0535-1 [DOI] [PubMed] [Google Scholar]
- 2.Schaller BJ. Trigeminocardiac reflex. J Neurosurg 2007;107:243 10.3171/JNS-07/07/0243 [DOI] [PubMed] [Google Scholar]
- 3.Schaller B, Probst R, Strebel S, et al. Trigeminocardiac reflex during surgery in the cerebellopontine angle. J Neurosurg 1999;90:215–20. 10.3171/jns.1999.90.2.0215 [DOI] [PubMed] [Google Scholar]
- 4.Acioly MA, Carvalho CH, Koerbel A, et al. Intraoperative brainstem auditory evoked potential observations after trigeminocardiac reflex during cerebellopontine angle surgery. J Neurosurg Anesthesiol 2010;22:347–53. 10.1097/ANA.0b013e3181eac551 [DOI] [PubMed] [Google Scholar]
- 5.Lv X, Jiang C, Li Y, et al. Results and complications of transarterial embolization of intracranial dural arteriovenous fistulas using Onyx-18. J Neurosurg 2008;109:1083–90. 10.3171/JNS.2008.109.12.1083 [DOI] [PubMed] [Google Scholar]
- 6.Aschner B. Über einen bisher nicht beschriebenen Reflex vom Auge auf Kreislauf und Atmung: Verschwinden des radialis Pulses bei Druck auf das Auge. Wien 1908;21:1529. [Google Scholar]
- 7.Griffis CA. The effect of intraoperative retrobulbar block on anesthetic management of enucleation under general anesthesia. Nurse Anesth 1991;2:28–32. [PubMed] [Google Scholar]
- 8.Meuwly C, Chowdhury T, Sandu N, et al. Meta-areas of the trigeminocardiac reflex within the skull base: a neuroanatomic "thinking" model. J Neurosurg Anesthesiol 2016;28:437–8. 10.1097/ANA.0000000000000240 [DOI] [PubMed] [Google Scholar]
- 9.Meuwly C, Golanov E, Chowdhury T, et al. Trigeminal cardiac reflex: new thinking model about the definition based on a literature review. Medicine 2015;94:e484 10.1097/MD.0000000000000484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meuwly C, Chowdhury T, Gelpi R, et al. The clinical surrogate definition of the trigeminocardiac reflex: Development of an optimized model according to a PRISMA-compliant systematic review. Medicine 2017;96:e9033 10.1097/MD.0000000000009033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hahnenkamp K, Hönemann CW, Fischer LG, et al. Effect of different anaesthetic regimes on the oculocardiac reflex during paediatric strabismus surgery. Paediatr Anaesth 2000;10:601–8. 10.1111/j.1460-9592.2000.00588.x [DOI] [PubMed] [Google Scholar]
- 12.Lübbers HT, Zweifel D, Grätz KW, et al. Classification of potential risk factors for trigeminocardiac reflex in craniomaxillofacial surgery. J Oral Maxillofac Surg 2010;68:1317–21. 10.1016/j.joms.2009.12.039 [DOI] [PubMed] [Google Scholar]
- 13.Meuwly C, Chowdhury T, Sandu N, et al. Anesthetic influence on occurrence and treatment of the trigemino-cardiac reflex: a systematic literature review. Medicine 2015;94:e807 10.1097/MD.0000000000000807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arnold RW, Jensen PA, Kovtoun TA, et al. The profound augmentation of the oculocardiac reflex by fast acting opioids. Binocul Vis Strabismus Q 2004;19:215–22. [PubMed] [Google Scholar]
- 15.Filonzi L, Magnani C, Lavezzi AM, et al. Detoxification genes polymorphisms in SIDS exposed to tobacco smoke. Gene 2018;648:1–4. 10.1016/j.gene.2018.01.034 [DOI] [PubMed] [Google Scholar]
- 16.Bailey PL. Sinus arrest induced by trivial nasal stimulation during alfentanil-nitrous oxide anaesthesia. Br J Anaesth 1990;65:718–20. 10.1093/bja/65.5.718 [DOI] [PubMed] [Google Scholar]
- 17.Hughes N, Bewick J, Van Der Most R, et al. A previously unreported serious adverse event during balloon sinuplasty. BMJ Case Rep 2013;2013:bcr2012007879 10.1136/bcr-2012-007879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ruhl DS, Ramsey MJ, Ruffin DM. A profound case of neurally mediated syncope with asystole after septoplasty. J Clin Anesth 2012;24:310–4. 10.1016/j.jclinane.2011.10.006 [DOI] [PubMed] [Google Scholar]
- 19.Yang JJ, Shen JC, Xu JG. Cardiac asystole after nasal infiltration of lidocaine with epinephrine in a transsphenoidal hypophysectomy patient with hypertrophic cardiomyopathy. J Neurosurg Anesthesiol 2010;22:81–2. 10.1097/ANA.0b013e3181b8ada9 [DOI] [PubMed] [Google Scholar]
- 20.Meuwly C, Chowdhury T, Gelpi R, et al. The trigemino-cardiac reflex: is treatment with atropine still justified? J Neurosurg Anesthesiol 2017;29:372–3. 10.1097/ANA.0000000000000324 [DOI] [PubMed] [Google Scholar]
- 21.Chowdhury T, Mendelowith D, Golanov E, et al. Trigeminocardiac reflex: the current clinical and physiological knowledge. J Neurosurg Anesthesiol 2015;27:136–47. 10.1097/ANA.0000000000000065 [DOI] [PubMed] [Google Scholar]
- 22.Wang CM, Guan ZY, Zhang J, et al. Comparative study of trigeminocardiac reflex after trigeminal ganglion compression during total intravenous anesthesia. J Neurosurg Anesthesiol 2015;27:16–20. 10.1097/ANA.0000000000000076 [DOI] [PubMed] [Google Scholar]
- 23.Chowdhury T, Ahuja N, Schaller B. Severe bradycardia during neurosurgical procedure: depth of anesthesia matters and leads to a new surrogate model of the trigeminocardiac reflex: a case report. Medicine 2015;94:e2118 10.1097/MD.0000000000002118 [DOI] [PMC free article] [PubMed] [Google Scholar]