Abstract
Current trends in health care delivery and management such as predictive and personalized health care incorporating information and communication technologies, home-based care, health prevention and promotion through patients’ empowerment, care coordination, community health networks and governance represent exciting possibilities to dramatically improve health care. However, as a whole, current health care trends involve a fragmented and scattered array of practices and uncoordinated pilot projects. The present paper describes an innovative and integrated model incorporating and “assembling” best practices and projects of new innovations into an overarching health care system that can effectively address the multidimensional health care challenges related to aging patient especially with chronic health issues. The main goal of the proposed model is to address the emerging health care challenges of an aging population and stimulate improved cost-efficiency, effectiveness, and patients’ well-being. The proposed home-based and community-centered Integrated Healthcare Management System may facilitate reaching the persons in their natural context, improving early detection, and preventing illnesses. The system allows simplifying the health care institutional structures through interorganizational coordination, increasing inclusiveness and extensiveness of health care delivery. As a consequence of such coordination and integration, future merging efforts of current health care approaches may provide feasible solutions that result in improved cost-efficiency of health care services and simultaneously increase the quality of life, in particular, by switching the center of gravity of health delivery to a close relationship of individuals in their communities, making best use of their personal and social resources, especially effective in health delivery for aging persons with complex chronic illnesses.
Keywords: health management, e-health, patient-centered health care, home-based care, health governance, community health
Video abstract
Introduction
In recent years, health care delivery has witnessed a vertiginous revolution. Information and communication technologies (ICT) are bringing a new reality, allowing for powerful means of processing a variety of data about many individuals in different environments. This is facilitating the development of fresh and more effective approaches to prevention and treatment not possible just a few years ago. This rapid development of ICT brings new advantages but new challenges as well. On the positive side, ICT tools are allowing more autonomy and quality of life for patients and improving cost-efficiency of health centers, promoting a new culture of interagency collaboration and public participation. This may especially benefit patients with complex, multidimensional problems and comorbidities, as often occurs in many cases of older people with chronic diseases (CD).1 On the negative side, home-based ICT may pose new challenges for both the patient and the health care service. For the patient, such challenges can include increased dependence on their health center, false expectations of protection, difficulties managing the technology, increased isolation, excessive feelings of responsibility and blame, and false alarms created by disease predictions. For the health care services, challenges can include difficulties in data protection, an overwhelming flow of data, and the need for new human resources, training, and organizational structures.2–8 New ICT will not be maximally effective by just adapting the traditional health care systems to incorporate such tools. Such an introduction of a new ICT may represent more problems than advantages. We need to move forward toward novel health care approaches that are capable of making the best use of the potentials of new ICT along with the development of current trends. Current trends, approaches, and paradigms such as those pointed below are implemented in a myriad of scattered practices that need to be analyzed, incorporating the emerging tools and methods into solid systems.
The aim of the present work was to suggest feasible ways of incorporating these practices into a general model of advancement and innovation in health care delivery and management.
Challenges and opportunities in current health care trends of chronic diseases
The rising prevalence of chronic diseases
As people live longer, CD (such as chronic cardiovascular diseases, arthritis, osteoporosis, diabetes, hypertension, neurodegenerative disorders, severe psychiatric illnesses, chronic respiratory disorders, severe chronic pain problems, and dementia) are increasing in their relative prevalence when compared with other types of illnesses and are currently the leading causes of deaths in many countries, especially striking the aging population (eg, 75% of the population may die from CD in developed countries in the near future9–12).11 The multidimensionality of CD in the elderly is of particular importance, with different aggravating factors appearing together with general deterioration of physical and cognitive abilities, such as increased risk of falls, fractures, and disabilities; comorbid neurological and cerebrovascular disorders; nutritional deterioration; abuse of polypharmacy and self-medication; severe confusion syndrome; losses in basic life activities; emotional stress; difficulties associated with acceptance and compliance of treatment; deprivation of social support; reduced income; increased stigma and discrimination; reduced access to health and social services; physical and psychological abuse and neglect.11–16 There is a bi-directionality in the relationship between chronic disorders and many of these dependency-related problems thus increase the occurrence of possible comorbidities.16,17 This implies higher need for dependency-related complex care. Unsurprisingly, CD are currently the main cause of dependency of the aging population in developed countries. The data on CD clearly points out the need to improve early detection of CD and preventive care using multilevel approaches.
Current trends in health care innovation for the aging CD patient
Traditional illness-centered health care models fall short when facing the CD challenges in our increasing aging population. As the World Health Organization already challenged the traditional view in its definition of health in 1948, nowadays health care trends try to go further. Some authors18 propose to define health as “the ability to adapt and to self-manage”, reflecting the current reality of older chronic patients. Current trends try to make health services more effective by being personalized and tailored to the patients’ needs, resources, and characteristics, based on early detection of risks and preventive treatment in the person’s environment. New ICT tools for ambulatory care are strongly contributing to the feasibility of home-based health care even in serious cases which just some years ago were restricted to intensive care units in hospitals.19,20 But the application of these insights is hampered by the fragmentation of services in most health systems.21–23 The latest health care approaches are stressing the need to advance new frameworks for collaboration among social and health services in order to address the complex nature of CD progression in the older person, including biological, physiological, psychological, social, and contextual factors (eg, de Bruin et al and Burns et al24,25). Current health care trends do recognize such challenges and are progressing towards attaining the desired integration of health elements and services. A bibliographic review of evaluative research on innovative practices in the field allowed us to group them in the following current trends:
Early diagnosis and prevention,25,26 facilitated by new ICT tools.27–33 Multidimensional systems include noninvasive monitoring tools, gathering relevant patient’s biopsychosocial information within predictive applications to be used by the patients and health centers. E-health systems incorporate and process large amounts of real-time, multidimensional information from/to the patients’ home and natural settings, and from/to different areas and agencies in shared, interoperable, and synched big databases using cloud computing technology.5,19,20,33 Information recording and processing applications for smart wearable technologies (SWT), depth cameras, and knowledge management (KM) tools are more and more used in smartphones, tablets, and computers, including real-time information gathering and sharing tools, and patients and corporate portals for information interfaces and community participation. An ICT-supported KM approach may include collective intelligence processes, information-shared analysis, planning problem–solving, and actions to promote health and well-being, follow-up, and accountability.31–33 SWT, a noninvasive technology for remote, unobtrusive, and real-time recording of physiological data (heart rate, blood pressure, skin conductance, respiratory rate and volume, movement, and blood glucose) virtually without discomfort, allows a person to carry out their habitual daily activities while being monitored and guarded in their natural context.33 This technology opens tremendous possibilities for early detection and prevention of disease progression, relapses, and crises through the development of predictive tools including all the related biopsychosocial indices.
Home-based, outreach health care. This approach works in the natural context where the problems and solutions are most present to preserve the well-being and autonomy of the patient. Cost-effectiveness studies19 comparing inpatient care vs home care revealed that patients in their own environment could manage their own autonomy and health longer and with higher satisfaction. More sustainable health autonomy and improved quality of life together with a reduction of costs by having the patient at home appear to provide a more cost-efficient approach than in-patient centralized care.19,20 Providing home-based services appears to improve symptoms; saves costs to health services; reduces hospitalization; preserves patients’ preferences, autonomy, and medication adherence; increases practitioners’ satisfaction; and makes better use of psychosocial support.1,34,35 Good examples are the home-based reablement (intense rehabilitation) practices, successfully expanded in different countries.36
Psychosocial health promotion, centered on the patients’ personal and social resources. The World Health Organization16 points out the need to include community health promotion strategies in health care systems. Searching for increased cost-efficiency and effectiveness, health care should enhance psychosocial resources of the patient and their communities. Community health managers (those agents in charge of the general health in a local community) represent a fundamental avenue for reaching all patients in a local area, promoting health communities (groups of patients with similar illness organizing themselves in mutual-support communities) intertwined with the local community, and enhancing personal and social resources on health and well-being to increase self-competence, cognitive and social skills, physical autonomy, illness acceptance, treatment compliance, and proactive involvement of the patient, that is, empowering the patient.1 Current examples in this direction are the home and community care managers, and even nonhealth professionals after a training program, significantly contributing to reduce dependency and improve quality of life in older patients.37
Genetic, psychosocial and real-time physiological predictive tools and algorithms regarding the patients’ health. Such tools and algorithms can be used for early detection, screening, and overarching preventive diagnosis, and can incorporate mathematical and statistical models.17,27–33,38–43
- Integrated health care. This entails a set of procedures to merge services from different agencies and formal and informal resources in the relationship with the individual, family, and community. This approach is intended to tackle all main factors affecting a disease in a systemic and overarching manner,19–24,33 centered on improving the coordination among services and resources and the engagement of all stakeholders (including the patients and their communities) in decision-making, treatment, prevention, and health promotion.22,44 Aging persons with CD are perhaps the best example of cases with multifaceted and multilayered problems needing such a multidimensional approach to their care.24 Current integrated approaches include the following types of practices:
- Health care e-governance. The deployment of an organized health umbrella allows gathering and optimizing all formal services and informal resources (such as social capital), seeking mutual support and collaboration, and avoiding the fragmentation of service provision, overlaps among services, and social pockets of underserved groups in dire need.23 In particular, CD patients, who are more vulnerable to psychosocial stressors, may show a poor ability to use health resources due to well-known processes such as the Inverse Care Law (the higher the need for health or social services the less available they will be), the Matthew effect (people with more resources will have higher probability to access to health or social services), learned helplessness, and poor self-efficacy.45–47 This represents a challenge that requires the coordinating effort of all different agencies. Health information technology poses opportunities and challenges to improve not only horizontal but also vertical health governance (between patients’, managers’, and political levels of care coordination) as the greater information flow among levels may need a further effort in information management.48 However, health institutions still find it difficult to acquire the needed coordination with other agencies and services (such as education, social services, economy, housing, and environmental services) at local and national levels.21 In some cases, care coordination has not exhibited clear benefits in terms of cost-efficiency, while bringing more complexity and requiring greater effort in human resources.48 This could be due to a poor culture of interagency team work but also could be due to a lack of experience in or ability to change and adapt within each organization. Deploying health care governance models does not have much meaning if they do not bring along a structural simplification of each participant organization in health care delivery and management. Besides, even though, currently there is a general agreement that informal resources and social capital are fundamental for patients’ empowerment, their actual integration with formal health care management is still limited in most countries.21–23 There is a need to stress proactive health care management to engage and integrate all members of the community in the health system, to improve cost-efficiency, effectiveness, and quality of services.23
- Patient-centered, home- and community-based management models. Intraorganizational simplification in structures and processes, decentralization of services, participatory health value chains, and interorganizational development are achieved by centering services in the relationship with the patients in their home and community12,19,20,49–52 with the support of interoperable ITC/KM systems.33
- Self-management health models. These are aimed at strengthening individual and community empowerment in health self-care and increasing the perception of self-efficacy and control over personal health. The experience based on these approaches3,6 applied to CD will provide the basis from which to move forward from the dependency-ridden traditional health care models to a more balanced comanagement of health, which is especially important in CD cases due to the special need of these patients to preserve their autonomy and to prevent helplessness.
- Palliative care. Preserving the quality of life and well-being of the patient is currently regarded as a need and a right of advanced CD patients, allowing both quality of life and ability to face death with dignity. Whereas palliative care has undergone an exponential growth in the last decades, still only a small percentage of patients with advanced CD receives it. This is mainly due to organizational and budget difficulties of public health services in organizing the multi-agency and home-based services that palliative care requires.12,19–21
- Shared health care models. A collaborative work of health practitioners and patients is frequently carried out through a one-stop service directly related to the patients. Shared management is commonly personalized and very effective, as it is relatively easier and simpler to implement.20,33,44,51,52
Current research exhibits the effectiveness of patient-centered, home- and community-based integrated management models that are based on e-health governance and prevention/promotion approaches, tackling all main factors affecting a disease in a systematic approach compared with traditional inpatient and specialized treatments (eg, Labson et al, Luckett et al, Lehtinen et al19,20,53). This is being facilitated by current ICT/KM tools allowing mathematical and statistical methods to process large amounts of data on the patients’ organic systems and their relationship with the individual’s psychological and social environmental context to predict general health dynamics, embedded in a work philosophy of stakeholders’ proactive collaboration.
Despite the exciting perspectives opened by these trends, most innovative practices are represented by pilot experiences, excessively fragmented, partially scattered, not linked to a broader context, and not easily transferable or scalable.21,22 This chaotic variety of experiences results in poor agreement among public health institutions and systems on what methodologies are best to follow.23 A fundamental challenge of current health care approaches is the need for developing unified care management and delivery frameworks.22,23,44,54 Current directions in health care are aimed at finding greater agreement regarding the best combination of health care promotion, prevention and treatment strategies and tools. Furthermore, real tailored, community-and person-centered health care systems should be capable of adapting to any type of cultural, social, and institutional conditions. Social diversity is universal, so the experiences of adapting the health systems to a diverse society should render more agreement in the methods. The ability of health systems to have flexible methods adaptable to any social condition is especially needed when facing the multifaceted nature of most CDs.
Following these aims, a proposal for an integrated health care management system (IHMS) to apply to CD in the older population is outlined here, based on an effort to combine the most successful current trends. This system articulates the collaboration among institutions, practitioners, experts, and users, to provide a feasible and effective transdisciplinary health care delivery and management for the CD patient, including risk detection, prevention, and treatment to improve cost-effectiveness of services and quality of life in the aging CD population.
Proposed methodology: incorporating current trends into an innovative system centered on the aging patient with chronic disease
Target groups
The proposed IHMS outlined in this section focuses on the most frequent types of CD developing into serious dependency in the aging population, as they imply the highest challenges in health care services:1,9–14,16 oncologic illness, pulmonary chronic illness, cardiac chronic illness, neurologic diseases, diabetes, severe hepatic illness, and dementia/psychiatric disorders. Health managers and practitioners and those of other participant agencies (social services, education, housing, economy, etc.), informal caregivers, and community members are also viewed as participants in the overall health care system, contributing in all the stages of the system deployment process (system design and deployment, training, monitoring, evaluation, and dissemination).
System design procedure
Health care delivery to the aging CD patient should encompass a large set of interrelated social, environmental, psychological, genetic, and physiological features, tackling all these different factors with holistic, systemic approaches. The system here presented was designed by taking into account evidence-based successful innovative practices from different countries. The designed system proposed here has been developed by incorporating different disciplines (medical specialties, psychology, sociology, public management, policy-making, computer scientists, and engineering).
An effective IHMS approach applied to the aging CD patient is centered in the diverse society, using latest technology for personalized health, optimizing the balance between cost-efficiency, effectiveness, and patients’ well-being. Such an IHMS is intended to be adaptable to any social and geographical context. The key components of the IHMS are grouped into four basic areas: 1) home-based and community-centered health care delivery, 2) health care governance, and 3) latest ICT/KM tools on home-based monitoring and prediction, and 4) Y-relational health care management.
Home-based and community-centered health care
Person-centered health care implies pinpointing all the uniqueness and differential characteristics of each patient and their context in order to personalize health diagnosis, treatment, prevention, and health promotion. Person-centered health care entails distinguishing the entwined system of positive and negative elements around patients and integrating all the resources in the direct relationship with them. Shared health care sends the message to the patient that we are “counting on you”. “Full” patient involvement in the cocreation and comanagement of health care brings the possibility of a joint, deliberate, thoughtful, advised, informed, discussed, and mutually agreed upon type of health care that is desired and needed, especially useful on aging chronic patients.
In order to tailor the health system to the diverse society that we live in, the two most significant contexts of the patients, their home and community, should be the focus of health care. Home and community do not only refer to physical places but represent a unique biopsychosocial ecosystem constituting the person’s habitat. Reaching the person in their context means deeply understanding, caring, and using the patients’ resources as a powerful strategy for effective and cost-efficient health care. It facilitates tackling the negative contextual factors affecting the patient and enhancing the positive factors for individual and community empowerment, proactive health promotion, and wellness. This is especially true when facing CD, with frequent etiologies, risks, and vulnerabilities in their environments and with solutions within the formal and informal resources in their communities. Home- and community-centered health care also brings a better relational management approach, fundamental when care is aimed at following the evolution of the disease for an optimal quality of life in a supporting and close relationship with the patients, caregivers, and their communities. Health care methods adapted to a diverse society further enables transferability to other territories, as it should be free of social, cultural, and institutional biases. An approach based on a diverse society entails universal values that bring an opportunity to exchange experiences and to establish local and international collaborations based on the common goal of reaching all persons in need of services to guarantee social inclusion in the health system.
Health care e-governance
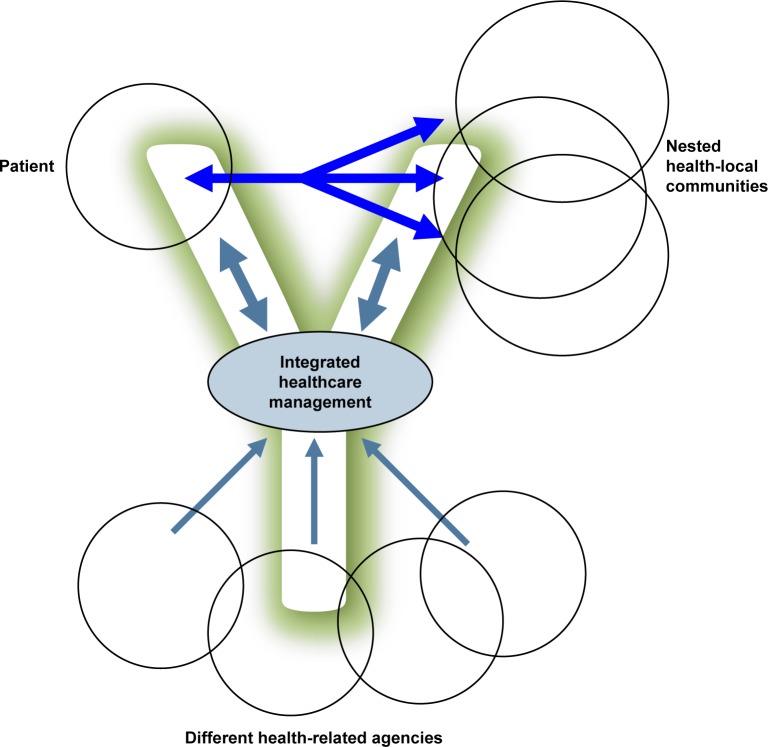
A good health care governance model should be able to coordinate, systematize, and standardize procedures and protocols of information exchanging, sharing, processing, decision-making, planning, and intervention in order to adapt them to different contexts in a joint work among local, national, and international agencies. The horizontal and proactive joint work among health departments, social services, education, housing, environmental services, NGOs, along with the (local and health) communities and patients will enable tackling more effectively different factors affecting health, with better inclusiveness (reaching those most excluded from the health system) and extensiveness (reaching all the people with CD or with risk of CD). Overarching health care based on an integrated analysis of biopsychosocial risk as well as protective factors will allow for implementation of collective intelligence and KM processes in health management, contributing to more accurate diagnoses of health-related problems, defining proper and desired care strategies, redesigning treatment programs, and monitoring them in order to prevent and treat CD. We also need to seize the opportunity to work toward new “intercommunity” systems supported by interoperable ICT/KM tools, while addressing the challenge of maintaining data protection and confidentiality in each location. The intercommunity approach may foster “nested” health communities promoting the integration between health and “overlapping” local communities, by sharing social capital and networks into health promotion and care (Figure 1).
Figure 1.
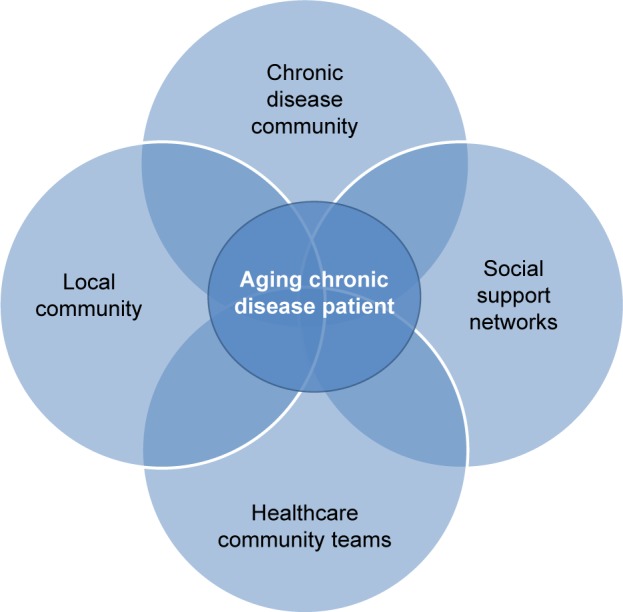
Nested communities in personalized, relational health care management centered on the patient.
Note: The health management system is aimed at enhancing mutual support among the patients’ social support, the chronic disease group (promoted as health community), the local community (neighborhood), and the health care teams.
ICT/KM systems
Health e-governance within integrated health care approaches are intended to make the best use of all knowledge resources available and to share them among stakeholders, patients, and communities, using social capital for an effective planning to solve problems. New ICTs/KM tools address these goals as they make it possible to monitor individuals in their natural context, processing interdimensional information and developing analytics to be included in software applications in order to better understand and predict CD progress and relapses. Thus, the result improves patient care, patient autonomy, and operational efficiency.33
The most common e-health recording devices monitor discrete physiological indices (heart rate, blood pressure, and respiratory measures) at specific regular moments which do not allow for synchronization and the analysis of the dynamic relationship among indices across time. Continuous (second by second) analyses of the relationship among indices provide more complete information of physiological patterns reacting to the persons’ stimuli, behavior, context, activities, and situations. Such an analysis allows for real-time comparisons with previously processed information from the patient (on crises and relapses) as well as comparison with analog patterns from different groups with similar or even different illnesses, facilitating the predictive accuracy of early detection and rapid response to health crises or relapses. Algorithms integrating physiological, behavioral, and postural information from depth cameras may also be included to provide a more complete overview for monitoring patient status and service delivery.
Patients’ biopsychosocial predicting profiles may include genetic, physical, and physiological indices, behavioral habits and activities, emotional changes, social and economic features, subjective well-being, quality of life indices, and disability scales. Many of these indices may be self-recorded by the patient in a mobile device, with indicators of well-being based on standard scales such as Satisfaction With Life Scale (SWLS), General Self-Efficacy Scale (GSES), Short Form Health Survey (SF-36), and World Health Organization Disability Assessment Schedule (WHODAS) 2.0 as additional procedures for the effectiveness evaluation. Easy-to-use features will allow the patient to have access to the information at any time with explanations and recommendations. Automatic integration of collected between- and within-subject data in databases can provide the medical and research communities with an opportunity to assess effectiveness, enabling insights into illness evolution, the effects of drug therapy, treatment compliance, and rehabilitation process. Acceptance by the patient is reinforced by developing friendly and useful applications. Furthermore, specific acceptance strategies of the e-health system may be developed through cocreation with the end user. In addition, the system may be integrated with microelectromechanical systems for the automatic delivery of drugs, making it compatible with regular Android and Apple smartphones, mobile and electronic companies, and with new protocols and services of data transmission, processing, storing, and protection (eg, HL7 Personal Health Monitoring Standard), thereby ensuring easy adaptability to most ambulatory recording devices already available in the health services where the system is deployed.
Training should be provided to formal and informal health care givers regarding assisting the patient in learning how to best use the system. The multidimensional data recording and processing capability will also allow for a continuous evaluation of the system performance in terms of cost-efficiency and effectiveness regarding reduction in patient hospitalizations, preservation of autonomy and cognitive functions, quality of life, functional capacity, self-monitoring ability, safety, comfort, cost-efficiency, treatment compliance, technical usability, and acceptance. Integrating genetic, physiological, psychological, and social information of the patient will allow for a more accurate, comprehensive, and interdisciplinary diagnosis, monitoring, and prevention. To do so, predictive software applications are included in the system based on a combination of mathematical and statistical approaches:
Mathematical approach: This quantifies the observation that the characteristics of biological processes that regulate physiological responsiveness and maintenance of stability are based on the patients’ genetic, physiological, psychological, and social background.34 Physiological resilience and adaptation may be represented in terms of chaos theory as two attractors for the dynamics of physiological regulation. Resilience mechanisms are suggested to help to protect an organism from short-term system perturbations and long-term overadaptation and to balance biological, psychological, and social arousing effects in interaction with adaptation mechanisms. Algorithms are defined based on noninvasive physiological recording to study and predict changes in the balance between resilience and adaptation.
Statistical approach: Based on interdisciplinary ontologies, cross-fertilization of methods and processes with other disciplines (eg, meteorology) may lead to new approaches for medical diagnosis and prediction. For instance, weather forecast provides a useful analogy for the dynamics of human physiology. Earth’s weather also represents a unit governed by a system of interrelated forces. Some ecological approaches understand the Earth’s surface as a “living system”. Mathematical (linear and nonlinear) dynamical models are not as useful in weather forecasting as statistical methods using multivariate tools, with increasing accuracy (eg, see Bellone et al, Enke and Spekat, Gardner and Dorling, and Cofiño et al55–58). These methods use past data from several indices across time and space to predict future “analog” weather conditions. Meteorologists have taken advantage of the speedy evolution of computer power to include more and more data from more variables, combining “machine-learning” methods with dynamic models, intending to get the “whole picture” (eg, “Bayesian Networks”58). The potential cross-fertilization may be useful when addressing how to predict the influence of multiple (genetic, physiological, and psychosocial) factors in physiological activity.41
ICT will also allow deeper decentralization and deconcentration of information analysis and decision-making, which can enhance strategies of data protection and confidentially. It is more difficult for a hacker to attack a “neural network” than a server where all information is centralized. “Big data” distributed systems may allow us to imitate our brain (as a knowledge network) as a sound strategy for data protection and effective management.
Information processing and management. Data stored in the local IHMS Data Banks can be connected together to form an international IHMS Data Bank. Data can then be stored on the servers and computers of the participant institutions and individuals gathering that information, connected via cloud computing technology. Methods and processes can be developed to exploit multivariate statistical analyses (including profile and trend analyses), bootstrap, mixed models, optimal scaling (multiset canonical correlation), and cluster analyses. All these aspects can be used to integrate, cross-classify, and organize information and study predictive relationships (eg, regressions), differences across systems (eg, multivariate analyses of variance), and patterns among variables and indicators (eg, cluster and analog analyses), combined with qualitative information (based on interviews and group dynamics on analyses of problems, definitions of solutions, and decision-making on actions to be taken). Patients’ biopsychosocial patterns will be compared with analog patterns of patients with different diseases in order to set probabilities of diseases and crisis.
Relational management approach
A relational management approach is used to integrate resources and services in the relationship with the person in the community. The desire for a real overarching, multimodal, and integrated management system centered on the person is shared by most practitioners from health and education agencies, social, employment, and environmental services, and general public managers. The IHMS uses participatory methods to gather and process sufficient and meaningful information from all stakeholders, for the cocreation of new knowledge reflecting their needs and problems and solutions. This way, health organizations may be able to implement integrated and interagency plans, with horizontal and vertical interoperable coordination procedures among services. This will facilitate further simplification of organizational structures and processes. A Y-relational management model is included here, with features such as integrated interagency services centered on the patient, collaborative leaderships, intercommunity nested social networks, health self-management tools, shared capital resources, new computer applications for information recording and processing in ambulatory care, and integrated management processes (Figure 2).
Figure 2.
Y-relational health care management.
Note: The management system integrates all (formal and informal) resources and services in the relationship with and between the patient, the disease groups (being promoted as health communities), and the local community.
The system should include different data collection methods: surveys, qualitative and quantitative techniques, and participatory-action research with home visits, and patients’ and community portals with smartphone apps coordinating the work of health practitioners and those from other different agencies participating within the community. This system will enable agencies and patients to share different fields of information with other agencies and users for KM, but without sharing fields that such other agencies, patients, and outside users do not need. This requires management of confidentiality with access filters applied to different fields depending on the services, agencies, and users. A main strategy is based on the “neural” distribution of information fields in each database in the servers of the different agencies who own that information, integrating it not by physical centers but in the peripheral devices of the users.
System structure and processes
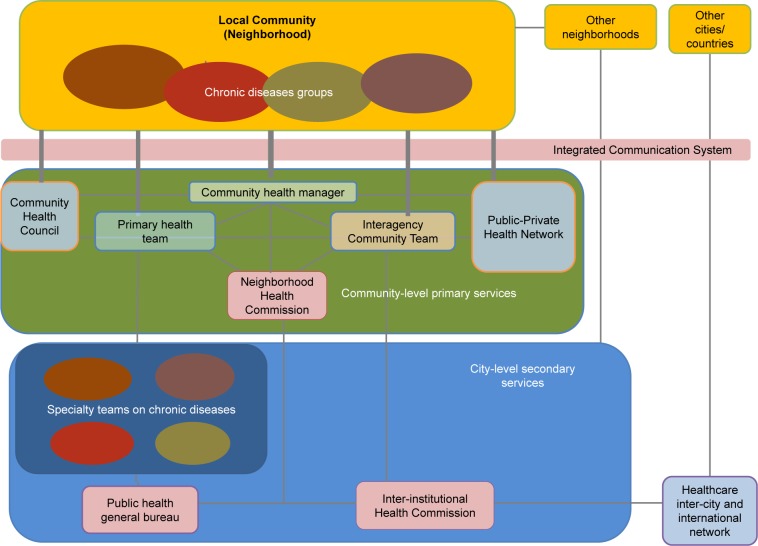
The four areas described above set up the framework of the IHMS structure and processes. The structure implies a turnaround of the traditional organizational charts of health care services, placing the “nested” local-health communities at the top of the chart. The services are centered on the territory where the needs and resources are most found. The general structure keeps the community-level primary and city-level secondary in-service provision (Figure 3).
Figure 3.
Structure of services of the Integrated Healthcare Management System.
Notes: A neighborhood level of primary health management includes six connected bodies: a Community Health Council (composed by neighbors), a Primary Health Team (health practitioners), an Interagency Community Team (including a general community manager and community agents from different social and health agencies), a Public– Private Health Network (all public and private entities that may contribute to promote community health and well-being), a Neighborhood Health Commission (with three or four representatives of major health and social agencies, to coordinate with the city-level authorities to follow general health plans), and a Community Health Manager in charge of facilitating the coordination of all bodies for patient-centered and community-based integration of (formal and informal) health resources and services.
Formal and informal resources are integrated in the relationship between a community health care manager (CHM) and the patients. This proposed CHM (similar to the above-mentioned home and community care managers37) will be the person from the public health system in charge of the general health in the community, providing community health services with tasks such as general community health analyses (including the relationship among causal, symptomatic, consequential, and mediating factors related to health and illness), detection of individuals and groups with risks and vulnerabilities, referrals to the community health center, mapping of formal and informal resources, as well as planning of actions with all stakeholders in the community.
The CHM will horizontally coordinate (using collaborative leadership approaches) an interagency community team (health, social, educational, environmental, housing, and socioeconomic). Other fundamental system components in the proposed IHMS will be the Health Community Council (including all community members), a Health Community Network of public and private entities, the current primary health teams, and the current health teams specialized in each disease, who will work the cases as a secondary city level of service provision. All these elements will also work directly with the patient, so the first contact of the system with a CD patient or a person with risk of chronic disease will not necessarily be done by the CHM. The CHM does not replace the role of the primary or general physician, who will keep the same functions, but with a closer relationship with the CHM. The CHM will neither carry out any medical diagnoses, nor refer a new case to a medical specialist (which will be done by the primary medical practitioner).
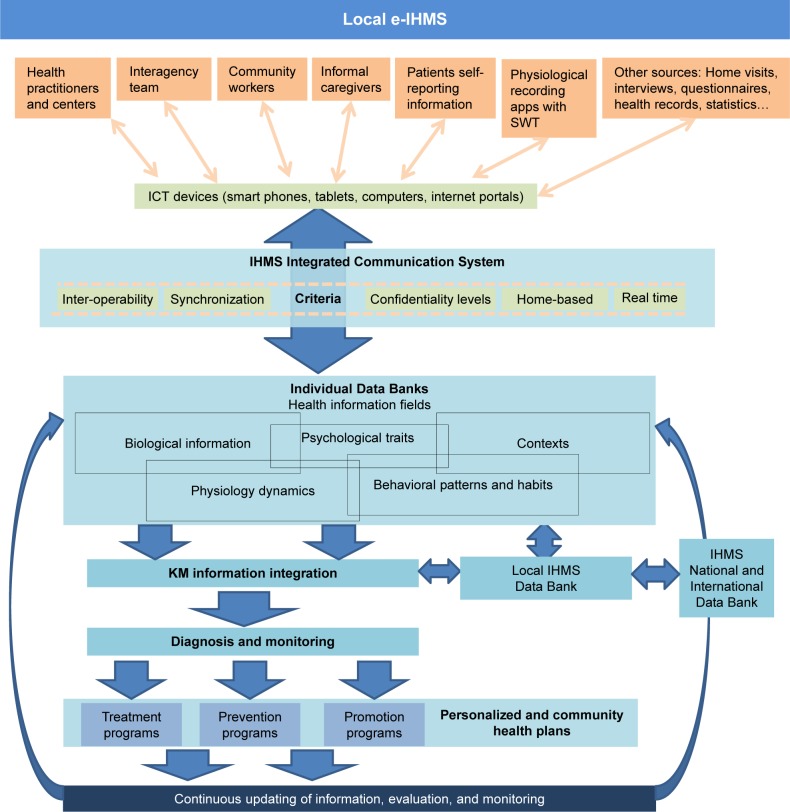
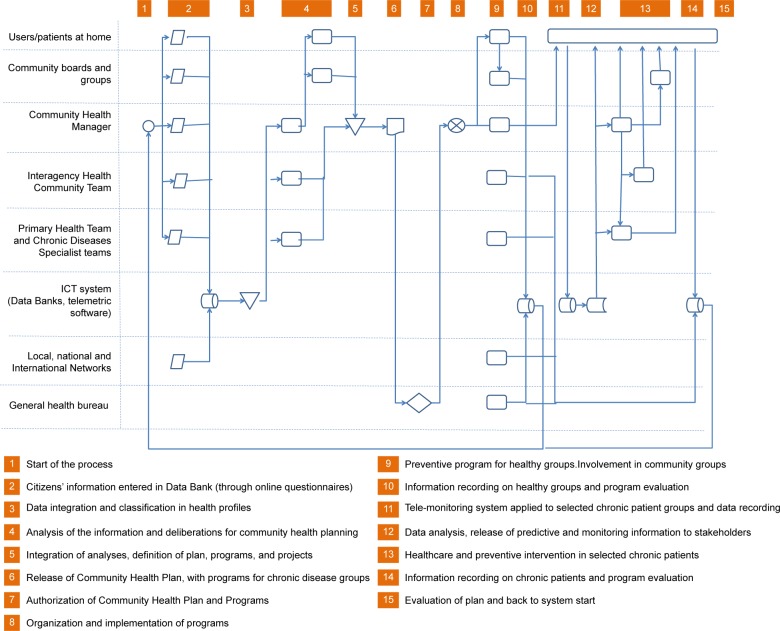
The incorporation of ICT is a fundamental element of the system. Figure 4 outlines the communication system and Figure 5 makes concrete the system organizational process and pathways.
Figure 4.
Schematic representation of the communication structure in each local IHMS.
Notes: All stakeholders and patients have available interfaces (“Personal Health Portals”) in ICT devices (smartphones, tablets, and computers) to provide and receive relevant information for monitoring and early detection of increased risks of disorder outbreaks or relapses. That information can be stored and real-time updated in local data banks to provide information for symptoms detection (and urgent intervention if needed), in combination with the information from an international IHMS Data Bank for knowledge management.
Abbreviations: ICT, Information and communication technologies; IHMS, Integrated Healthcare Management System.
Figure 5.
Integrated Healthcare Management System itinerary and pathways.
Abbreviation: ICT, Information and communication technologies.
System evaluation
The system is assessed using a scientific approach reflecting 1) the effectiveness and cost-efficiency of the health care management provided by a particular system; 2) the predictive effectiveness of the incorporated early detection tools, and 3) the efficiency and accuracy of methodology used to evaluate and monitor the degree of impact of system performance and its consequences regarding a disease treatment and the improvement in the patients’ well-being. The evaluation methodology may use the same multidimensional and interdisciplinary approach that is currently used in the disease diagnosis, monitoring, and follow-up.
Conclusion and challenges
Current trends in health care pave the way for overarching community- and home-based health management systems. They aim at exploiting the effectiveness and cost-efficiency of ICT-supported management and governance approaches to improve health care delivery as well as to enhance prevention of CD in geriatric settings. Future developments will certainly strengthen the collaboration between health institutions, researchers, companies, practitioners, community members, and patients regarding the sharing of effective approaches to tackle the multicausal factors affecting CD, identifying the best uses of the latest ICT to address these factors.
This paper highlights the great potential that can be realized by merging these trends and incorporating the best evidence-based tools and practices into an integrated health care system focused on prediction, prevention, and promotion of health within the patients’ ecosystem. Innovative e-health governance approaches will bring new revolutions in furthering prevention, care, and quality of life, especially in geriatric patients with CD. With new advances, new ethical dilemmas need to be addressed; for example, how to use different predictive probabilities in the best way for adequate prevention, or how to guarantee data protection and confidentiality. In this paper we described a feasible system that may overcome current limitations in e-health, for example, by guaranteeing that each stakeholder has access only to the information needed by their tasks. In addition, the potential misuse of predicting devices (for instance, raising alarms in the patient) could be reduced by the closer face-to-face relationship of that health community managers and teams with the patient. Another concern typically facing new healthcare structures is whether the proposed system is going to incur more costs and complexity for the health administration. However, the governance approach used here allows territory-based, overarching health care planning, allowing best use and synergies among formal and informal resources, simplifying the structure of services and bringing a more cost-efficient and effective health care value chain with the participation of all stakeholders, patients, and communities. To do so, horizontal and vertical collaborative protocols should be clearly defined.
Acknowledgments
We thank Dr Jerry Joseph Batzel, Institute of Physiology, Medical University of Graz, Austria, for his constructive comments and his insights during the preparation of the manuscript.
Footnotes
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Cummings E, Ellis L, Turner P. Health Literacy: Breakthroughs in Research and Practice. Hershey: IGI Global; 2017. Information Resources Management Association The past, the present, and the future: examining the role of the “Social” in transforming personal healthcare management of chronic disease; pp. 287–304. [Google Scholar]
- 2.Dahl S, Eagle L. Empowering or misleading? Online health information provision challenges. Market Intell Plan. 2016;34(7):1000–1020. [Google Scholar]
- 3.Fairbrother P, Ure J, Hanley J, et al. Telemonitoring for chronic heart failure: the views of patients and healthcare professionals – a qualitative study. J Clin Nurs. 2014;23(1–2):132–144. doi: 10.1111/jocn.12137. [DOI] [PubMed] [Google Scholar]
- 4.Gibert SH, Degrazia D, Danis M. Ethics of patient activation: exploring its relation to personal responsibility, autonomy and health disparities. J Med Ethics. 2017;43(10):670–675. doi: 10.1136/medethics-2017-104260. [DOI] [PubMed] [Google Scholar]
- 5.Haluza D, Jungwirth D. ICT and the future of healthcare: aspects of pervasive health monitoring. Inform Health Soc Care. 2018;43(1):1–11. doi: 10.1080/17538157.2016.1255215. [DOI] [PubMed] [Google Scholar]
- 6.Vaismoradi M, Jordan S, Kangasniemi M. Patient participation in patient safety and nursing input – a systematic review. J Clin Nurs. 2015;24(5–6):627–639. doi: 10.1111/jocn.12664. [DOI] [PubMed] [Google Scholar]
- 7.Haluza D, Jungwirth D. ICT and the future of health care: aspects of health promotion. Int J Med Inform. 2015;84(1):48–57. doi: 10.1016/j.ijmedinf.2014.09.005. [DOI] [PubMed] [Google Scholar]
- 8.Dang S. Telemedicine applications in geriatrics. In: Fillit H, Rockwood K, Young JB, editors. Brocklehurst’s Textbook of Geriatric Medicine and Gerontology. New York: Elsevier Ltd; 2010. pp. 1064–1069. [Google Scholar]
- 9.Murtagh FE, Bausewein C, Verne J, Groeneveld EI, Kaloki YE, Higginson IJ. How many people need palliative care? A study developing and comparing methods for population-based estimates. Palliat Med. 2014;28(1):49–58. doi: 10.1177/0269216313489367. [DOI] [PubMed] [Google Scholar]
- 10.Vega T, Arrieta E, Lozano JE, et al. Atención sanitaria paliativa y de soporte de los equipos de atención primaria en el domicilio [Palliative health care and support services of primary home care] Gaceta Sanitaria. 2011;25(3):205–210. doi: 10.1016/j.gaceta.2011.02.005. Spanish. [DOI] [PubMed] [Google Scholar]
- 11.Gómez-Batiste X, Martínez-Muñoz M, Blay C, Ambls J, Vila L, Costa X. Identificación de personas con enfermedades crónicas avanza-das y necesidad de atención paliativa en servicios sanitarios y sociales: elaboración del instrumento NECPAL CCOMS-ICO© [Detection of advanced chronic diseases and need of palliative social and health services: Elaboration of the NECPAL CCOMS-ICO instrument©] Medicina Clínica. 2013;140(6):241–245. doi: 10.1016/j.medcli.2012.06.027. Spanish. [DOI] [PubMed] [Google Scholar]
- 12.Beernaert K, Deliens L, de Vleminck A, et al. Early identification of palliative care needs by family physicians: a qualitative study of barriers and facilitators from the perspective of family physicians, community nurses, and patients. Palliat Med. 2014;28(6):480–490. doi: 10.1177/0269216314522318. [DOI] [PubMed] [Google Scholar]
- 13.Reynolds CF, Alexopoulos GS, Katz IR, Lebowitz BD. Chronic depression in the elderly. Drugs Aging. 2001;18(7):507–514. doi: 10.2165/00002512-200118070-00004. [DOI] [PubMed] [Google Scholar]
- 14.Charney DS, Reynolds CF, Lewis L, et al. Depression and Bipolar Support Alliance consensus statement on the unmet needs in diagnosis and treatment of mood disorders in late life. Arch Gen Psychiatry. 2003;60(7):664. doi: 10.1001/archpsyc.60.7.664. [DOI] [PubMed] [Google Scholar]
- 15.Kemp AH, Arias JA, Fisher Z. Social ties, health and wellbeing: a literature review and model. In: Ibanez A, Sedeno L, Garcia AM, editors. Neuroscience and Social Science. New York: Springer; 2017. pp. 397–427. [Google Scholar]
- 16.WHO . World Report on Ageing and Health. Geneva, Switzerland: World Health Organization; 2015. [Google Scholar]
- 17.Brown EG, Gallagher S, Creaven AM. Loneliness and acute stress reactivity: a systematic review of psychophysiological studies. Psychophysiology. 2018;55(5):e13031. doi: 10.1111/psyp.13031. [DOI] [PubMed] [Google Scholar]
- 18.Huber M, Knottnerus JA, Green L, et al. How should we define health? Br Med J. 2011;343(Jul 26 2):d4163. doi: 10.1136/bmj.d4163. [DOI] [PubMed] [Google Scholar]
- 19.Labson MC, Sacco MM, Weissman DE, Gornet B, Stuart B. Innovative models of home-based palliative care. Cleve Clin J Med. 2013;80(Electronic Suppl 1):eS30–eS35. doi: 10.3949/ccjm.80.e-s1.07. [DOI] [PubMed] [Google Scholar]
- 20.Luckett T, Phillips J, Agar M, Virdun C, Green A, Davidson PM. Elements of effective palliative care models: a rapid review. BMC Health Serv Res. 2014;14(1):136. doi: 10.1186/1472-6963-14-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Auschra C. Barriers to the integration of care in inter-organisational settings: a literature review. Int J Integr Care. 2018;18(1):5. doi: 10.5334/ijic.3068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grooten L, Borgermans L, Vrijhoef HJ. An instrument to measure maturity of integrated care: a first validation study. Int J Integr Care. 2018;18(1):10. doi: 10.5334/ijic.3063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nicholson C, Hepworth J, Burridge L, Marley J, Jackson C. Translating the elements of health governance for integrated care from theory to practice: a case study approach. Int J Integr Care. 2018;18(1):11. doi: 10.5334/ijic.3106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Bruin SR, Stoop A, Billings J, et al. The SUSTAIN Project: a European study on improving integrated care for older people living at home. Int J Integr Care. 2018;18(1):1–12. doi: 10.5334/ijic.3090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burns A, Dening T, Baldwin R. Mental health problems. Br Med J. 2001;322(7289):789–791. doi: 10.1136/bmj.322.7289.789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shapiro A, Taylor M. Effects of a community-based early intervention program on the subjective well-being, institutionalization, and mortality of low-income elders. Gerontologist. 2002;42(3):334–341. doi: 10.1093/geront/42.3.334. [DOI] [PubMed] [Google Scholar]
- 27.Salem A-BM, Revett K, El-Dahshan E-SA. Machine learning in electrocardiogram diagnosis; 2009 International Multiconference on Computer Science and Information Technology; October 12–14, 2009; Mrągowo, Poland. [Google Scholar]
- 28.Gong W, Wang S. Support vector machine for assistant clinical diagnosis of cardiac disease; 2009 WRI Global Congress on Intelligent Systems; May 19–21, 2009; Xiamen, China. [Google Scholar]
- 29.Huang S, Shen Q, Duong TQ. Artificial neural network prediction of ischemic tissue fate in acute stroke imaging. J Cereb Blood Flow Metab. 2010;30(9):1661–1670. doi: 10.1038/jcbfm.2010.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen Z, Purdon PL, Brown EN, Barbieri R. A unified point process probabilistic framework to assess heartbeat dynamics and autonomic cardiovascular control. Front Physiol. 2012;3:4. doi: 10.3389/fphys.2012.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Seliger A, Hansen LB. Characterization and Discrimination of Pathological Electrocardiograms Using Advanced Machine Learning Methods. Kongens, Lyngby: DTU; 2013. [Google Scholar]
- 32.Øvretveit J. Digital technologies supporting person-centered integrated care – a perspective. Int J Integrated Care. 2017;17(4):6. doi: 10.5334/ijic.3051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhu X, Cahan A. Wearable technologies and telehealth in care management for chronic illness. In: Weaver CA, Ball MJ, Kim GR, Kiel JM, editors. Healthcare Information Management Systems. New York: Springer; 2016. pp. 375–398. [Google Scholar]
- 34.Tralongo P, Ferraù F, Borsellino N, et al. Cancer patient-centered home care: a new model for health care in oncology. Ther Clin Risk Manag. 2011;7:387–392. doi: 10.2147/TCRM.S22119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mihic MM, Todorovic Mlj, Obradovic Vlj, Mitrovic ZM. Can we do better? Economic analysis of human resource investment to improve home care service for the elderly in Serbia. Clin Interv Aging. 2016;11:85. doi: 10.2147/CIA.S96778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tuntland H, Kjeken I, Langeland E, et al. Predictors of outcomes following reablement in community-dwelling older adults. Clin Interv Aging. 2017;12:55–63. doi: 10.2147/CIA.S125762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lewin G, Concanen K, Youens D. The Home Independence Program with non-health professionals as care managers: an evaluation. Clin Interv Aging. 2016;11:807. doi: 10.2147/CIA.S106180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee EM, Hughes BM. Trait dominance is associated with vascular cardiovascular responses, and attenuated habituation, to social stress. Int J Psychophysiol. 2014;92(2):79–84. doi: 10.1016/j.ijpsycho.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 39.Davydov DM, Zhdanov RI, Dvoenosov VG, Kravtsova OA, Voronina EN, Filipenko ML. Resilience to orthostasis and haemorrhage: a pilot study of common genetic and conditioning mechanisms. Sci Rep. 2015;5(1):10703. doi: 10.1038/srep10703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Decaro JA. Beyond catecholamines: measuring autonomic responses to psychosocial context. Am J Hum Biol. 2016;28(3):309–317. doi: 10.1002/ajhb.22815. [DOI] [PubMed] [Google Scholar]
- 41.Gandarillas MA. Psychosocial correlates of peripheral vegetative activity and coordination. Aletheia. 2011:35–36. 211–230. [Google Scholar]
- 42.Gandarillas MA, Câmara SG, Scarparo H. Estressores Sociais da hipertensão em comunidades carentes [Social stressors of high blood pressure in deprived communities] Psicologia: Reflexão e Crítica. 2005;18(1):62–71. Portugese. [Google Scholar]
- 43.Ottaviani C, Brosschot JF, Lonigro A, Medea B, van Diest I, Thayer JF. Hemodynamic profiles of functional and dysfunctional forms of repetitive thinking. Ann Behav Med. 2017;51(2):261–271. doi: 10.1007/s12160-016-9851-3. [DOI] [PubMed] [Google Scholar]
- 44.Suter E, Oelke ND, da Silva Lima MAD, et al. Indicators and measurement tools for health systems integration: a knowledge synthesis. Int J Integr Care. 2017;17(6):4. doi: 10.5334/ijic.3931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mercer SW, Guthrie B, Furler J, Watt GC, Hart JT. Multimorbidity and the inverse care law in primary care. Br Med J. 2012;344:e4152. doi: 10.1136/bmj.e4152. [DOI] [PubMed] [Google Scholar]
- 46.Callebaut L, Molyneux P, Alexander T. The relationship between self-blame for the onset of a chronic physical health condition and emotional distress: a systematic literature review. Clin Psychol Psychother. 2017;24(4):965–986. doi: 10.1002/cpp.2061. [DOI] [PubMed] [Google Scholar]
- 47.Cybulski M, Cybulski L, Krajewska-Kulak E, Cwalina U. The level of emotion control, anxiety, and self-efficacy in the elderly in Bialystok, Poland. Clin Interv Aging. 2017;12:305–314. doi: 10.2147/CIA.S128717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kuziemsky CE. HIT implementation and coordinated care delivery from the perspective of multisided markets. In: Vimarlund V, editor. E-Health Two-Sided Markets. Cambridge, MA: Academic Press; 2017. pp. 143–150. [Google Scholar]
- 49.Cooper TL, Bryer TA, Meek JW. Citizen-centered collaborative public management. Public Adm Rev. 2006;66(s1):76–88. [Google Scholar]
- 50.Habitat UN. Directrices Internacionales sobre descentralización y acceso a los servicios básicos para todos [International guidelines on decentralization and access to basic services for all] Nairobi: United Nations Human Settlements Programme; 2009. Available from: http://www.redalyc.org/pdf/1150/115025560018.pdf, Spanish. [Google Scholar]
- 51.Pollitt C. Decentralization: a central concept in contemporary public management. In: Ferlie E, Lynn L, Pollitt C, editors. The Oxford Handbook of Public Management. Oxford: Oxford University Press; 2005. [Google Scholar]
- 52.Ortendahl M. Shared decision-making based on different features of risk in the context of diabetes mellitus and rheumatoid arthritis. Ther Clin Risk Manag. 2007;3(6):1175–1180. [PMC free article] [PubMed] [Google Scholar]
- 53.Lehtinen V, Katschnig H, Kovess-Masféty H, Goldberg D. Developments in the treatment of mental disorders. In: Knapp D, McDaid D, Mossialos E, editors. Mental Health Policy and Practice Across Europe Glasgow. McGraw-Hill: Education; 2007. pp. 126–144. [Google Scholar]
- 54.Borgermans L, Marchal Y, Busetto L, et al. How to improve integrated care for people with chronic conditions: key findings from EU FP-7 Project INTEGRATE and Beyond. Int J Integr Care. 2017;17(4):1–12. doi: 10.5334/ijic.3096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bellone E, Hughes JP, Guttorp P. A hidden Markov model for downscaling synoptic atmospheric patterns to precipitation amounts. Clim Res. 2000;15:1–12. [Google Scholar]
- 56.Enke W, Spekat A. Downscaling climate model outputs into local and regional weather elements by classification and regression. Clim Res. 1997;8:195–207. [Google Scholar]
- 57.Gardner MW, Dorling SR. Artificial neural networks (the multilayer perceptron) – a review of applications in the atmospheric sciences. Atmos Environ. 1998;32(14–15):2627–2636. [Google Scholar]
- 58.Cofiño A, Cano R, Sordo C, Gutierrez J.Bayesian networks for probabilistic weather prediction. ECAI’02 Proceedings of the 15th European Conference on Artificial Intelligence Amsterdam: Frank van Harmelen Vrije Universiteit Amsterdam; 2002695–699. [Google Scholar]