Abstract
Background
Toxic anterior segment syndrome (TASS) can be a rare complication of anterior segment surgery. Here we reviewed the most recent advances in the understanding of TASS.
Methods
English articles related to TASS were retrieved from “PubMed” using the following keywords; “toxic anterior segment syndrome” or “TASS”. The authors of this paper reviewed all the retrieved literature and critical findings were summarized.
Results
The onset of TASS can vary from hours to months. The clinical manifestations are also variable. The causes of TASS are broad and continue to expand and could not be elucidated in over half of the reported cases. Prompt and thorough investigation to explore the causes of TASS is critical. Surgeons should be fully aware and updated regarding possible etiologies and make ceaseless efforts to prevent TASS. This effort begins with establishing TASS prevention protocols and regularly training surgical staff. Proper cleaning of surgical instruments is critical and should follow the guidelines set by The American Society of Cataract and Refractive Surgery TASS Task Force. When TASS occurs, sharing information with other ophthalmologists and reporting new causes is crucial for the prevention of outbreaks.
Conclusions
Anterior segment surgeons should be reminded that TASS is mostly preventable by the establishment of TASS prevention protocols, regular surgical staff training and thorough adherence to recommendations for cleaning and sterilizing intraocular surgical instruments.
Keywords: Cataract, Toxic, TASS, Anterior chamber, Inflammation
Background
Toxic anterior segment syndrome (TASS) is characterized by sterile postoperative inflammation of anterior segment after intraocular surgery [1, 2]. Although TASS most often occurs after cataract surgery, it has also been reported after keratoplasty and posterior segment surgeries [3–5]. The inflammation can be mild with a minimal cellular reaction or severe enough to cause marked cornea edema and hypopyon. The onset can be acute (within days) or delayed (after several months) [1, 6]. The overall incidence of TASS was found to be 0.22% in a large case series [7]. Additionally, a significant number of reported cases have occurred as clusters of outbreaks [7–11]. In cases of severe TASS, prompt control of inflammation is essential to prevent any permanent damage to delicate ocular structures such as the corneal endothelium, trabecular meshwork and macula. TASS frequently resembles the symptoms and signs of early postoperative bacterial endophthalmitis and therefore, makes accurate diagnosis challenging [1, 12]. While prompt initiation of oral and fortified topical antibiotics is key to the treatment of bacterial endophthalmitis, TASS usually does not respond to antibiotics and instead requires strong topical or systemic steroids for resolution. However, considering the potential detrimental and irreversible ophthalmic sequelae of bacterial endophthalmitis, most cases of unusual postoperative inflammation after cataract surgery are regarded as infectious endophthalmitis until proven otherwise.
When TASS is suspected, it is important to perform a thorough investigation to determine the causative agent. This investigation should include surgical instruments and disposable medical devices, e.g. ophthalmic viscoelastic agents, medications, surgical drapes, and sterilization systems. However, even thorough clinical and laboratory investigations sometimes fail to find the causative agent in many cases of TASS [9].
By heightening professionals’ awareness and understanding of TASS, new causes of TASS are reported every year. This updated information should be shared amongst ophthalmic surgeons for effective prevention of TASS. With this report, we attempt to review recent advances in the understanding of TASS. Using the PubMed search engine, the keywords “toxic anterior segment” initially retrieved 125 articles. We excluded 5 articles published before the year 2000 and then screened the title and abstract of the remaining 120 articles. A further 35 articles were excluded from this review due to being irrelevant to our topic, and 13 non-English articles were excluded. Finally, 72 articles were included in this review (see Fig. 1).
Fig. 1.
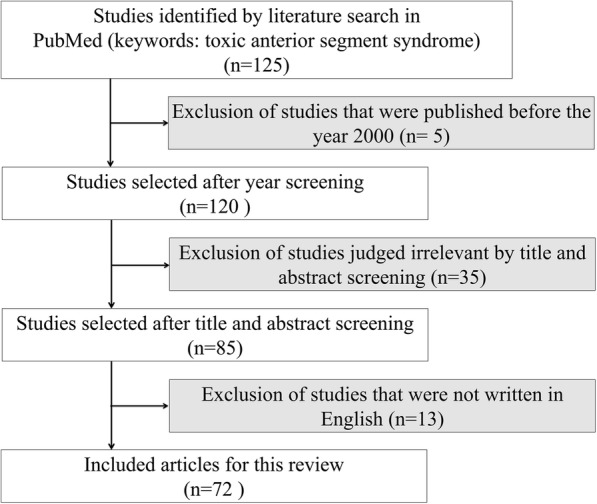
Flow chart to show the studies included in this review
Clinical manifestations
TASS is typically characterized by unusual anterior chamber inflammation in the early postoperative period. Depending on the severity of inflammation, other symptoms may be present, such as pain, conjunctival injection or chemosis, hypopyon, corneal edema, keratic precipitates, anterior vitreous opacities, macular edema and visual deterioration [1, 6, 7, 13]. Most reported cases of TASS have been anecdotal, and therefore the clinical manifestations vary widely as shown in Table 1 [9, 10, 14–17]. However, in 2015 and 2017, two large case-series studies (n = 251 and n = 147) were conducted in Japan [8, 18]. The large sample sizes enabled the estimation of the occurrence rate of key clinical signs related to TASS (see Table 2). Anterior chamber reactions such as cell, flare and fibrin were the most common signs of TASS in these case series. Hypopyon, keratic precipitates and vitreous opacities were found in less than a quarter of cases.
Table 1.
Summary of 15 recent case reports of toxic anterior segment syndrome
| First Author (ref. no.) | Number of cases | Onset (days after the surgery) | Inciting agents | Clinical presentations | Managements (n) | Visual outcomes (n) |
|---|---|---|---|---|---|---|
| Miyake et al. [19] | 6 | 42–167 | IOL (ISert model 251, Hoya) | Chemosis, Ciliary injection, Decreased BCVA, Corneal edema, Anterior chamber reaction, hypopyon |
Vitretomy and IOL removal (1), Capsule irrigation (2), Medical treatment only (5) |
BCVA 20/100 (1), BCVA ≥20/30 (5) |
| Suzuki et al. [18] | 251 | 38.44 ± 32.29 Range:0–161 | IOL (ISert model 251 and 255, Hoya) | Anterior chamber reaction (99.2%), conjunctival injection (41.4%) Hypopyon (22.7%) Corneal edema (19.1%) Keratic precipitates (27.9%) |
Medical treatment only (142), Surgical intervention: vitrectomy (49), IOL removal (22), chamber irrigation (51) |
BCVA 0.036 ± 0.242 logMAR |
| Sorenson et al. [10] | 10 | 1–7 | Bacterial biofilm contamination of autoclave reservoir | Anterior chamber reaction (10), Hypopyon (3), Corneal edema (1), Anterior vitreous reaction (4) |
Medical treatment only (3), Vitreous tap and intravitreal injection (7) |
No light perception (1), BCVA≥20/30 (9) |
| Ohika et al. [8] | 147 | 13.1 ± 16.4 Range: 1–88 | IOL (Acrysof, Alcon) | Anterior chamber reaction (97.2%), Conjunctival injection (39.8%), Fibrinous inflammation (43.1%) Hypopyon (22.7%) Corneal edema (15.6%) Keratic precipitates (21.6%), Ocular pain (9.5%) |
Medical treatment only (104), Surgical intervention: vitrectomy (21), IOL removal (10), chamber irrigation (33) |
BCVA> 20/40 (143), BCVA≤20/40 (4) |
| Moyle et al. [9] | 11 | 1 | unknown | Corneal edema (11), anterior chamber reaction (10), Inflammatory plaque on IOL (5), hypopyon (3), fibrin reaction (6), mild pain (2) |
Medical treatment only (11) | BCVA = 20/20 (11) |
| Sengupta et al. [7] | 60 | 1 | Balanced salt solution with a low pH of 6.0 (12), OVD (17), unknown (31) | Severe iridocyclitis with varying degree of corneal edema (60) | Medical treatment only (56), Vitreous tap (4) |
BCVA: 0.11 ± 0.1 logMAR, range: 0–0.3 logMAR |
| Matsou et al. [36] | 5 | 1 | Generic trypan blue | Painless blurry vision, corneal edema, anterior chamber reaction, hypopyon and fibrin reaction | Medical treatment only (5) | BCVA: 0.82 ± 0.18 (Snellen acuity) |
| Bielory et al. [14] | 2 | 1 | intracameral lidocaine HCl 1% and phenylephrine 2.5% inadvertently preserved with 10% benzalkonium chloride. | Acute corneal decompensation (3) | Medical treatment only (1), Corneal transplantation for decompensated cornea (2) |
BCVA = 20/20 (1), NA (1) |
| Althomali [38] | 15 | 1–2 | OVD | Corneal edema (15), hypopyon (8) |
Medical treatment only | BCVA: count finger (2) (other retina pathology), BCVA: 20/70 (2), BCVA≥20/50 (11) |
| Koban et al. [16] | 1 | 1 | Inadvertent overdose of intracameral gentamicin | Hyphema, corneal edema, chemosis, hemorrhagic fibrinous reaction, Corneal decompensation |
Penetrating keratoplasty after medical treatment | BCVA: 20/60 |
| Cetinkaya et al. [54] | 5 | 1 | unknown | corneal edema (5), anterior chamber reaction (5), fibrin (3), hypopyon (3), increased intraocular pressure (3) | Penetrating keratoplasty (2) | BCVA: 20/100 (1), BCVA: 20/40 (1), BCVA≥20/30 (3) |
| Ari et al. [27] | 19 (pediatric patients) | 1–2 | Ethylene oxide gas sterilization | Corneal edema, anterior chamber reaction, | Medical treatment only (18), Penetrating keratoplasty (1) |
NA |
| Buzard et al. [15] | 2 | 1 | Generic trypan blue | Cornea edema, anterior chamber reaction, hypopyon | Penetrating keratoplasty (2) | NA |
| Maier et al. [5] | 24 | 1–2 | Contamination of corneal trephine | Graft infiltration, corneal stromal edema | Medical treatment only (24) | NA |
| Choi et al. [28] | 15 | NA | Ethylene oxide gas sterilization | Corneal edema, anterior chamber reaction, conjunctival injection, pupil irregularity, fibrin reaction | Penetrating keratoplasty (5) | BCVA≥20/200 (14), Light perception (1), |
IOL intraocular lens, BCVA best corrected visual acuity, NA not available, n case number
Table 2.
Clinical manifestation of toxic anterior segment syndrome in large-scale outbreak studies
| Clinical manifestation | Suzuki et al. [18] (n:251) | Oshika et al. [8] (n:147) | Endophthalmitis vitrectomy study [12] (n:420) |
|---|---|---|---|
| Onset after surgery (day) | 38.44 ± 32.29 days Range:0–161 |
13.1 ± 16.4 days Range: 1–88 |
6 days Range: 1–63 |
| Pain | NA | 9.5% | 74.3% |
| Blurred vision | NA | NA | 94.3% |
| Lid swelling | NA | NA | 34.5% |
| Injection and/or chemosis | 41.4% | 39.8% | 82.1% |
| Corneal edema | 19.1% | 15.6% | NA |
| Anterior chamber fibrin reaction or membrane formation | 26.7% | 43.1% | NA |
| Anterior chamber cell and/or flare | 99.2% | Cells (97.2%), flare (63.0) | NA |
| Hypopyon | 22.7% | 10.6% | 85.7% |
| Keratic precipitates | 27.9% | 21.6% | NA |
| Anterior vitreous opacities | 21.5% | 23.8% | NA |
| Media opacity | NA | NA | 99.5% |
| Red reflex present | NA | NA | 32.0% |
| Macular edema or other retinal abnormalities | NA | 3.8% | NA |
NA not available
The last column refers clinical manifestation of endophthalmitis for the comparative purpose
Although the onset of symptoms and involvement of vitreous was suggested as differentiating points between TASS and infectious endophthalmitis in some studies, the time before the onset of TASS is now known to vary widely [1, 8, 18]. TASS typically starts earlier (within 24 h after surgery) than infectious endophthalmitis (4–7 days after surgery). However, later onset cases are not rare. Miyake et al. reported 6 cases of late-onset TASS occurring 42 to 137 days after surgery [19]. In cases of TASS related to intraocular lens (IOL) contamination, the mean onset time from surgery to TASS was approximately 38 days [18].
Even after successful treatment, eyes with TASS can suffer significant sequelae. Avisar et al. investigated the endothelial morphology of eyes after TASS and found lower cell density, higher cell area and lower percentage of hexagonal cells [20].
Clinicians should be aware that the typical signs of TASS can be masked by strong topical steroids during the early postoperative period. Thus in some cases, TASS can manifest after discontinuation of topical steroids [21].
Etiology
Investigating the causative agent of TASS is difficult and sometimes unsuccessful. In many cases, the exact cause of TASS remains unknown even after a thorough investigation [7, 9]. Sengupta et al. reported that the etiology was not found even after a careful search in approximately 51.7% of TASS cases in their large case series (60 cases after uneventful cataract surgery) [7]. To date, the major causes implicated in TASS include inadequate cleaning of surgical instruments, contamination of surgical instrument or IOLs, and adverse drug reactions [1, 22, 23].
Surgical instrument contamination
The American Society of Cataract and Refractive Surgery (ASCRS) TASS Task Force suggested that improper cleaning of surgical instruments is the most common cause of TASS [2, 22, 24]. Inadequate flushing of hand pieces, the use of enzymatic detergents and the use of ultrasound baths were the most common factors involved in TASS, especially enzymatic detergents for cleaning instrument containing endotoxins, which are not deactivated by autoclave sterilization [1, 23, 24]. It is noteworthy that enzyme remnants still exist at the tip of surgical instruments even after vigorous flushing and rinsing [25]. These enzymes are not inactivated by heat of less than 140 °C and most Statim™ (SciCan, Canonsburg, PA) autoclaves reach temperatures of only 138 °C [26]. The dose-dependent toxicity of enzymatic detergents in corneal endothelium has previously been verified in animal models [26]. Therefore, the ASCRS Task Force on Ophthalmic Instrument Cleaning and Sterilization recommended avoiding the use of enzymatic detergents for ophthalmic instrument cleaning [24]. Additionally, ethylene oxide gas sterilization of surgical tubing lines resulted in severe TASS in 13 and 15 patients, respectively [27, 28]. Moreover, bacterial biofilm contamination of autoclave reservoirs can produce heat stable bacterial toxins continuously and contaminate surgical instruments during autoclaving [10].
Intracameral injection
Corneal endothelial toxicity and TASS are potential concerns following the intracameral injection of any pharmacologic agents. Drug components, inadvertent dilution with causative agents, preservatives, abnormal pH, or increased osmolality are all possible causes of TASS [29]. In addition, Lockington et al. found free radicals present in 19 commonly used intracameral drug preparations including phenylephrine, cefuroxime, lidocaine and bevacizumab [30]. These free radicals can induce a dose dependent cellular damage. Previously, the inadvertent use of a balanced salt solution with a low pH of 6.0 resulted in 12 cases of TASS in an outbreak [7]. Recently, Bielory et al. reported that the inadvertent intracameral injection of lidocaine HCl 1% and phenylephrine 2.5% preserved with 10% benzalkonium chloride resulted in severe TASS with irreversible corneal decompensation [14]. Koban et al. reported that inadvertent intracameral injection of a high dose (20 mg/0.5 ml) of gentamicin, prepared for subconjunctival injection, induced severe TASS and bullous keratopathy [16]. It is also possible that small amounts of gentamicin can access the anterior chamber through surgical incisions after subconjunctival placement [17]. Although it is debated, TASS after intracameral injection of cefuroxime has also been reported [31, 32]. Balanced salt solution (BSS) contamination can be another risk factor for TASS. Andonegui et al. reported five cases of TASS after using BSS prepared in a hospital pharmacy [33]. Inadvertent seeping of ophthalmic ointment into the anterior chamber has also been implicated in causing TASS [34].
Indocyanine green dye and trypan blue for lens capsule staining
Anterior lens capsule staining with dyes such as indocyanine green or trypan blue has generally been accepted as a safe and effective method to improve the visualization during capsulorhexis [35]. However, dye agents used for anterior capsule staining can become contaminated during the manufacturing process. Matsou et al. reported five cases of TASS and Buzard et al. reported two cases after using a generic trypan blue for capsule staining [15, 36]. Tandogan et al. investigated the toxic effect of indocyanin green in the anterior chamber of a rabbit [37]. Higher concentrations and longer exposure times have been thought to result in severe inflammation mimicking TASS.
Ophthalmic viscosurgical devices
Contamination or denaturation of ophthalmic viscosurgical devices (OVDs) can be a potential cause of TASS. Suspicious batches of OVDs evoked 17 and 15 cases of TASS in separate studies [7, 38]. Contamination by endotoxin during manufacturing was suspected in cases where the OVDs were derived from bacterial fermentation. Thus the need for guidelines for endotoxin limits in ophthalmic preparations has been proposed [38, 39].
.Traces of OVD residue attached to surgical instruments are sometimes not removed completely during cleaning and can denature to become toxic material. OVD denaturation can occur due to inappropriate handling during shipping and storage. Recently, another large outbreak (34 cases in 2 weeks) of TASS, possibly related to OVD, was reported [40]. In this case series, utilization of new OVDs prevented further occurrence of TASS.
Intraocular lens contamination
Recently heavy metal, such as aluminum, contamination during manufacturing of IOLs was proposed as a possible cause of massive (147 cases) outbreak of subacute TASS in Japan [8]. In another report, 251 cases of late onset TASS were related to a particular type of IOL [18]. Other anecdotal cases of TASS related to IOLs have also been reported [19, 41].
Patient’s clinical characteristics
Patients’ factors can also contribute to TASS development. Yazqan et al. investigated the systemic disease profile in TASS patients compared to controls. They found that type 2 diabetes mellitus, systemic hypertension, hyperlipidemia, chronic ischemic heart disease, and chronic renal failure were significantly more common in TASS patients [42].
Evaluation for etiology
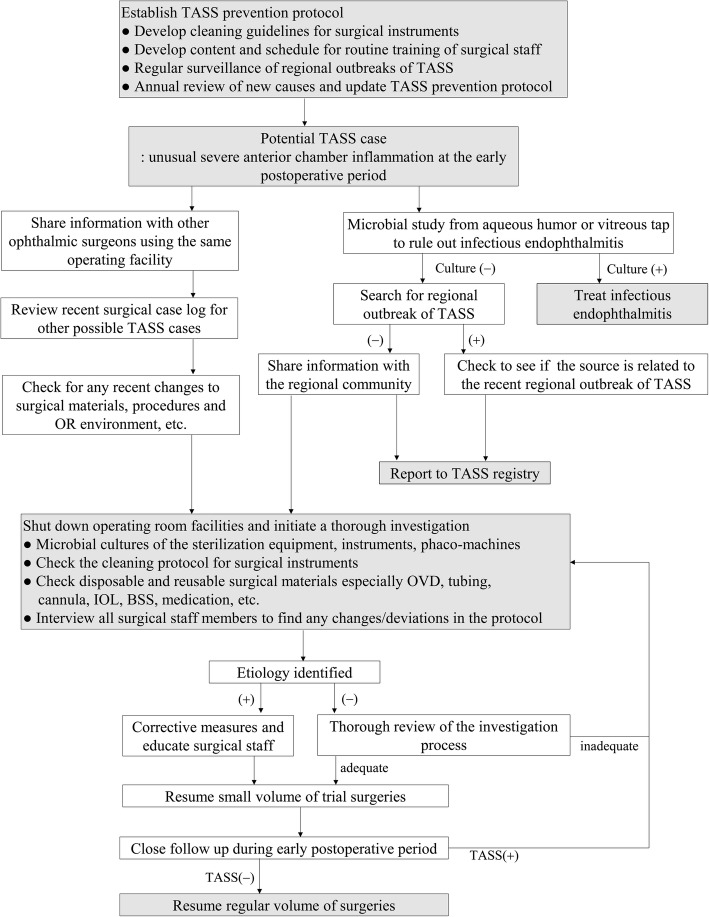
In cases of a TASS outbreak in a single institution, it is recommended that the surgical facility halts operations and immediately initiate a thorough investigation. It is important to share suspected TASS cases with other ophthalmic surgeons using the same surgical facility. By doing this, the incidence can be contained. It is also recommended that outbreaks be announced to outside surgeons in the same or different regions to share information and find any possible clues to explain regional outbreaks originating from IOLs or OVDs. All surgical staff members should be interviewed and any purposeful or inadvertent changes to their protocol should be investigated as shown in Fig. 2 [9].
Fig. 2.
Sample algorithm for the prevention and investigation of TASS
For laboratory evaluation, aqueous tapping for microbial studies is recommended. Especially in severe cases of TASS, differentiating between bacterial endophthalmitis and TASS is a critical step in the treatment algorithm. Vitreous involvement is more common in bacterial endophthalmitis and, in this case, vitreous tapping is also necessary. However, Gram stain and culture are often negative in some infectious endophthalmitis [43]. While waiting for microbial culture and sensitivity results, any recent changes in the surgical setup such IOLs, OVDs, solutions, surgical drapes, latex gloves, moving to a new operating room, using a new sterilization system or new phacoemulsification platform should be investigated as possible sources of contamination. Consulting infection prevention teams inside the hospital can be helpful. Bacterial culture screening of operating rooms, operating tables and surgical microscopes can provide important additional information after positive microbial test results. Obtaining cultures from sterilization systems is also essential for ruling out any contamination by heat stable bacterial toxins.
Suspected TASS cases should be reported to the TASS Registry (www.ascrs.org/tass-registry) run by the ASCRS. The website provides useful information such as TASS guidelines, a free link to the “Instrument Re-Processing and Product Questionnaire” (www.tassregistry.org/tass-combined-survey.cfm) developed by the ASCRS, and the quick link for the voluntary reporting of TASS to the Food and Drug Administration (FDA).
Prevention
The most important step for preventing TASS is raising awareness. It is very helpful to establish TASS prevention protocols and regularly train surgical staff. In the event of a TASS outbreak, this established protocol can be a valuable guideline to determine possible etiologies.
The use of preservative-free medications is important as well. The instillation of ophthalmic ointment after cataract surgery has largely been abandoned due to the risk of TASS by inadvertent entry into the anterior chamber.
Adequate cleaning and sterilization of ophthalmic surgical instruments are crucial to prevent TASS. The ASCRS, American Academy of Ophthalmology and American Society of Ophthalmic Registered Nurses participated in the joint TASS Task Force and published guidelines on how to clean and sterilize intraocular surgical instruments to prevent TASS [44]. (Table 3) Switching to single-use disposable instruments is also an effective way to prevent contaminating instruments during cleaning and sterilization.
Table 3.
Recommendations for cleaning and sterilizing intraocular surgical instruments modified from the guideline proposed by ASCRS, AAO and ASORN [44]
| Ensure adequate time for thorough cleaning and sterilization of instrument | |
| •Rigorous adherence to recommended procedures for cleaning and sterilization •Sufficient inventory of instruments to meet surgical volume and to provide adequate time for cleaning and sterilization | |
| Follow manufacturer’s directions for use for cleaning and sterilization | |
| Ophthalmic viscosurgical device solutions should not be allowed to dry on instruments | |
| •Instruments should be rinsed with sterile water immediately following the use | |
| Used instruments should be transported from the operating room in a closed container to the decontamination area | |
| Whenever possible, use disposable instruments and/or tubing and then discard after each use. | |
| •Do not reuse devices labeled for single use only. | |
| Clean intraocular instruments separately from non-intraocular surgical instruments. | |
| Avoid using enzymatic detergents for the cleaning of intraocular instruments. | |
| •When the use of enzymatic detergents is necessary, instruments should be thoroughly rinsed with copious volumes of water to remove all detergent. | |
| Ultrasonic cleaners should be emptied, cleaned, disinfected, rinsed and dried at least daily and preferably after each use. | |
| Do not reuse manual cleaning tools unless designed for reuse. | |
| •If brushes are reused, they should be designed for reuse and cleaned and treated with high-level disinfection or sterilization, preferably after each use, or at least once daily. | |
| Rinsing should provide flow of water through or over instruments and agitation in a basin of water should not be used. | |
| •Following thorough rinsing, instruments with lumens should be dried with forced or compressed air. | |
| If reusable woven materials are used for draping or wrapping trays or instruments, they should be laundered thoroughly between each use to eliminate surgical compounds, debris, and cleaning agents. | |
| Cleanliness and integrity of instruments should be verified. | |
| Sterilization | |
| •Glutaraldehyde is not recommended because of the toxicity of glutaraldehyde residues. •Low temperature methods of sterilization should not be used unless validated by the instrument manufacturer. •Regular autoclave sterilizers are preferred over Statim™ sterilizers because higher temperatures up to 190 °C can be reached. •Verification of sterilizer function should be completed at least weekly, preferably daily. | |
| Have a written policy in place for protocols for what happens to the instruments prior to and after each case in accordance with the manufacturer’s instructions. |
Treatment of TASS
Topical steroids are the mainstay treatment of TASS. In mild cases of TASS, frequent instillation (4 to 8 times per day) of a potent steroid, particularly 1% prednisolone acetate or alternatively dexamethasone 0.1% can be the initial choice of treatment [5, 9, 27, 36, 38]. Subconjunctival dexamethasone injection can be used when the effect of topical steroid is limited. In cases of severe TASS with dense fibrin and hypopyon, oral prednisolone up to 40 mg per day can be necessary to control the inflammation [19]. A topical NSAID can be added for pain control. Microbial culture can be negative in up to 30% of bacterial endophthalmitis [45]. Therefore, the combined use of broad spectrum antibiotics such as moxifloxacin is recommended, especially when the severe inflammation hinders the discrimination between TASS and bacterial endophthalmitis. In patients with severe fibrin reaction which is refractory to conventional steroid treatment, intracameral injection of recombinant tissue type plasminogen activator (25 μg/0.1 ml) can be effective [46]. Close follow up of the patient is critical to ensure that the inflammation responds to treatment. In cases where inflammation worsens with treatment, a repeat culture is recommended to rule out missed infectious endophthalmitis. Surgical interventions such as anterior chamber washout, vitrectomy or IOL removal can be performed according to the surgeon’s discretion, especially if the inflammation persist despite adequate medical treatment [8]. Ohika et al. and Suzuki et al. reported 29.3% and 43.4% of TASS cases, respectively, required surgical intervention such as anterior chamber irrigation, anterior vitrectomy, vitrectomy and IOL removal in their large case series [8, 18].
Mild cases of TASS usually resolve without any complications. However, irreversible corneal endothelial damage and decompensation by uncontrolled severe TASS may require corneal transplantation. Endothelial keratoplasty is an effective way to replace decompensated corneal endothelium after severe TASS [47, 48]. Kaur et al. reported that the time interval between TASS and endothelial keratoplasty is critical for successful surgical outcomes [49]. In their report, a time interval of less than 3 months (3cases) resulted in high rate of graft failure, while 12 cases with time intervals greater than 3 months resulted in 100% successful outcomes. Therefore, the surgeon should be prudent in deciding the timing of endothelial keratoplasty. In cases of secondary glaucoma following TASS, anti-glaucoma medications and, sometimes, glaucoma surgery is needed [28, 34]. Cystoid macular edema can occur due to TASS and this may require intraocular steroids or anti-VEGF injection treatment [13].
Visual outcome
As expected, prompt diagnosis and initiation of appropriate treatment determine the visual prognosis of TASS. By quickly resolving the diagnosis and treatment, irreversible damage to the corneal endothelium, trabecular meshwork and macula can be minimized. Visual outcomes of TASS seem to be relatively good with appropriate treatment [7, 8, 18]. Sengupta et al. reported that 58 out of 60 TASS eyes achieved a best corrected visual acuity of 6/9 or better on 1 month after treatment; however, significant numbers of eyes were complicated by atrophic iris (24%), posterior capsule opacification (16%), severe anterior capsular phimosis (12.5%) and cystoid macular edema (4%) 6 months after treatment [7]. Suzuki et al. reported the visual prognosis of all patients with IOL- related TASS was good with no single case of severe visual deterioration [18]. Oshika et al. reported only 2 out of 201 TASS cases resulted in best corrected visual acuity deterioration to 20/50 and 20/100, respectively, and those were due to macular edema after TASS treatment [8].
However, it is likely that the visual outcome after TASS treatment is dependent on the etiology. TASS caused by inadvertent intracameral drug injection may result in irreversible corneal damage and poor visual prognosis. TASS related to the exposure of an intraocular instrument to glutaraldehyde (2%) resulted in irreversible corneal decompensation in 100% of affected eyes [50]. Accidental use of methylene blue for capsule staining and accidental intracameral entry of gentamicin also resulted in irreversible corneal decompensation [16, 51, 52]. Bielory et al. reported 2 out of 3 TASS cases related to the inadvertent injection of 10% benzalkonium chloride containing medication needed corneal transplantation [14]. Werner et al. reported 3 out of 8 TASS cases caused by inadvertent seeping of antibiotic-steroid ointment into the anterior chamber resulted in corneal decompensation [34].
Some TASS cases caused by gas sterilization also showed poor visual outcomes. Choi et al. and Smith et al. reported 5 out of 15 TASS cases related to ethylene oxide gas sterilization and 6 out of 10 related to plasma gas sterilization required penetrating keratoplasty due to corneal decompensation, respectively [28, 53].
Conclusions
Albeit rare, TASS can perplex ophthalmic surgeons and result in unfortunate outcomes. Whenever TASS is suspected, a thorough investigation of possible etiologies is critical, as is sharing the information with colleagues. TASS can occur anytime and unexpectedly. However, anterior segment surgeons should be aware that TASS is mostly preventable by the establishment of TASS prevention protocols, regular training, and thorough adherence to recommendations for cleaning and sterilizing intraocular surgical instruments.
Acknowledgements
Publication of this article was supported in by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (Grant number: HI-15C1653).
Funding
This work was supported in part by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (Grant number: HI-15C1653).
Availability of data and materials
All data are available upon request to the corresponding author at rchuck@montefiore.org
Abbreviations
- BSS
Balanced salt solution
- IOL
Intraocular lens
- OVD
Ophthalmic viscoelastic device
- TASS
Toxic anterior segment syndrome
Authors’ contributions
CYP, JKL and RSC were responsible for the conception and design of this review. CYP and JKL acquired the data. CYP, JKL and RSC analyzed and interpreted the data. CYP and JKL wrote the draft. RSC and JKL revised the manuscript critically. All authors have read and approved the final manuscript.
Ethics approval and consent to participate
Not available.
Consent for publication
Not available.
Competing interests
Choul Yong Park and Roy S. Chuck are section editors of BMC Ophthalmology and Jimmy K Lee is the associate editor of the journal. The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Choul Yong Park, Email: oph0112@gmail.com.
Jimmy K. Lee, Email: jimmylee@montefiore.org
Roy S. Chuck, Phone: 1-718-920-6665, Email: rchuck@montefiore.org
References
- 1.Bodnar Z, Clouser S, Mamalis N. Toxic anterior segment syndrome: update on the most common causes. J Cataract Refract Surg. 2012;38(11):1902–1910. doi: 10.1016/j.jcrs.2012.06.053. [DOI] [PubMed] [Google Scholar]
- 2.Mamalis N. Toxic anterior segment syndrome update. J Cataract Refract Surg. 2010;36(7):1067–1068. doi: 10.1016/j.jcrs.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 3.Sevimli N, Karadag R, Cakici O, Bayramlar H, Okumus S, Sari U. Toxic anterior segment syndrome following deep anterior lamellar keratoplasty. Arq Bras Oftalmol. 2016;79(5):330–332. doi: 10.5935/0004-2749.20160094. [DOI] [PubMed] [Google Scholar]
- 4.Moisseiev E, Barak A. Toxic anterior segment syndrome outbreak after vitrectomy and silicone oil injection. Eur J Ophthalmol. 2012;22(5):803–807. doi: 10.5301/ejo.5000116. [DOI] [PubMed] [Google Scholar]
- 5.Maier P, Birnbaum F, Bohringer D, Reinhard T. Toxic anterior segment syndrome following penetrating keratoplasty. Arch Ophthalmol. 2008;126(12):1677–1681. doi: 10.1001/archopht.126.12.1677. [DOI] [PubMed] [Google Scholar]
- 6.Mamalis N, Edelhauser HF, Dawson DG, Chew J, LeBoyer RM, Werner L. Toxic anterior segment syndrome. J Cataract Refract Surg. 2006;32(2):324–333. doi: 10.1016/j.jcrs.2006.01.065. [DOI] [PubMed] [Google Scholar]
- 7.Sengupta S, Chang DF, Gandhi R, Kenia H, Venkatesh R. Incidence and long-term outcomes of toxic anterior segment syndrome at Aravind eye hospital. J Cataract Refract Surg. 2011;37(9):1673–1678. doi: 10.1016/j.jcrs.2011.03.053. [DOI] [PubMed] [Google Scholar]
- 8.Oshika T, Eguchi S, Goto H, Ohashi Y. Outbreak of subacute-onset toxic anterior segment syndrome associated with single-piece acrylic intraocular lenses. Ophthalmology. 2017;124:519–523. doi: 10.1016/j.ophtha.2016.12.010. [DOI] [PubMed] [Google Scholar]
- 9.Moyle W, Yee RD, Burns JK, Biggins T. Two consecutive clusters of toxic anterior segment syndrome. Optom Vis Sci. 2013;90(1):e11–e23. doi: 10.1097/OPX.0b013e318279e991. [DOI] [PubMed] [Google Scholar]
- 10.Sorenson AL, Sorenson RL, Evans DJ. Toxic anterior segment syndrome caused by autoclave reservoir wall biofilms and their residual toxins. J Cataract Refract Surg. 2016;42(11):1602–1614. doi: 10.1016/j.jcrs.2016.08.030. [DOI] [PubMed] [Google Scholar]
- 11.Kutty PK, Forster TS, Wood-Koob C, Thayer N, Nelson RB, Berke SJ, Pontacolone L, Beardsley TL, Edelhauser HF, Arduino MJ, et al. Multistate outbreak of toxic anterior segment syndrome, 2005. J Cataract Refract Surg. 2008;34(4):585–590. doi: 10.1016/j.jcrs.2007.11.037. [DOI] [PubMed] [Google Scholar]
- 12.Results of the Endophthalmitis Vitrectomy Study. A randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Endophthalmitis Vitrectomy study group. Arch Ophthalmol. 1995;113(12):1479–96. [PubMed]
- 13.Ugurbas SC, Akova YA. Toxic anterior segment syndrome presenting as isolated cystoid macular edema after removal of entrapped ophthalmic ointment. Cutan Ocul Toxicol. 2010;29(3):221–223. doi: 10.3109/15569527.2010.485285. [DOI] [PubMed] [Google Scholar]
- 14.Bielory BP, Shariff A, Hussain RM, Bermudez-Magner JA, Dubovy SR, Donaldson KE. Toxic anterior segment syndrome: inadvertent Administration of Intracameral Lidocaine 1% and phenylephrine 2.5% preserved with 10% Benzalkonium chloride during cataract surgery. Cornea. 2017;36:621–624. doi: 10.1097/ICO.0000000000001145. [DOI] [PubMed] [Google Scholar]
- 15.Buzard K, Zhang JR, Thumann G, Stripecke R, Sunalp M. Two cases of toxic anterior segment syndrome from generic trypan blue. J Cataract Refract Surg. 2010;36(12):2195–2199. doi: 10.1016/j.jcrs.2010.09.017. [DOI] [PubMed] [Google Scholar]
- 16.Koban Y, Genc S, Bilgin G, Cagatay HH, Ekinci M, Gecer M, Yazar Z. Toxic anterior segment syndrome following phacoemulsification secondary to overdose of Intracameral gentamicin. Case Rep Med. 2014;2014:143564. doi: 10.1155/2014/143564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Litwin AS, Pimenides D. Toxic anterior segment syndrome after cataract surgery secondary to subconjunctival gentamicin. J Cataract Refract Surg. 2012;38(12):2196–2197. doi: 10.1016/j.jcrs.2012.10.018. [DOI] [PubMed] [Google Scholar]
- 18.Suzuki T, Ohashi Y, Oshika T, Goto H, Hirakata A, Fukushita K, Miyata K, Japanese ophthalmological society HIL-REIC Outbreak of late-onset toxic anterior segment syndrome after implantation of one-piece intraocular lenses. Am J Ophthalmol. 2015;159(5):934–939 e932. doi: 10.1016/j.ajo.2015.01.023. [DOI] [PubMed] [Google Scholar]
- 19.Miyake G, Ota I, Miyake K, Zako M, Iwaki M, Shibuya A. Late-onset toxic anterior segment syndrome. J Cataract Refract Surg. 2015;41(3):666–669. doi: 10.1016/j.jcrs.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 20.Avisar R, Weinberger D. Corneal endothelial morphologic features in toxic anterior segment syndrome. Cornea. 2010;29(3):251–253. doi: 10.1097/ICO.0b013e3181b11568. [DOI] [PubMed] [Google Scholar]
- 21.Lee SN. Mild toxic anterior segment syndrome mimicking delayed onset toxic anterior segment syndrome after cataract surgery. Indian J Ophthalmol. 2014;62(8):890–892. doi: 10.4103/0301-4738.141067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mamalis N. Toxic anterior segment syndrome. J Cataract Refract Surg. 2006;32(2):181–182. doi: 10.1016/j.jcrs.2006.01.036. [DOI] [PubMed] [Google Scholar]
- 23.Cutler Peck CM, Brubaker J, Clouser S, Danford C, Edelhauser HE, Mamalis N. Toxic anterior segment syndrome: common causes. J Cataract Refract Surg. 2010;36(7):1073–1080. doi: 10.1016/j.jcrs.2010.01.030. [DOI] [PubMed] [Google Scholar]
- 24.Mamalis N. Toxic anterior segment syndrome: role of enzymatic detergents used in the cleaning of intraocular surgical instruments. J Cataract Refract Surg. 2016;42(9):1249–1250. doi: 10.1016/j.jcrs.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 25.Tsaousis KT, Werner L, Reiter N, Perez JP, Li HJ, Guan JJ, Mamalis N. Comparison of different types of phacoemulsification tips. II. Morphologic alterations induced by multiple steam sterilization cycles with and without use of enzyme detergents. J Cataract Refract Surg. 2016;42(9):1353–1360. doi: 10.1016/j.jcrs.2016.02.053. [DOI] [PubMed] [Google Scholar]
- 26.Parikh C, Sippy BD, Martin DF, Edelhauser HF. Effects of enzymatic sterilization detergents on the corneal endothelium. Arch Ophthalmol. 2002;120(2):165–172. doi: 10.1001/archopht.120.2.165. [DOI] [PubMed] [Google Scholar]
- 27.Ari S, Caca I, Sahin A, Cingu AK. Toxic anterior segment syndrome subsequent to pediatric cataract surgery. Cutan Ocul Toxicol. 2012;31(1):53–57. doi: 10.3109/15569527.2011.613426. [DOI] [PubMed] [Google Scholar]
- 28.Choi JS, Shyn KH. Development of toxic anterior segment syndrome immediately after uneventful phaco surgery. Korean J Ophthalmol. 2008;22(4):220–227. doi: 10.3341/kjo.2008.22.4.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Braga-Mele R, Chang DF, Henderson BA, Mamalis N, Talley-Rostov A, Vasavada A, Committee ACC. Intracameral antibiotics: safety, efficacy, and preparation. J Cataract Refract Surg. 2014;40(12):2134–2142. doi: 10.1016/j.jcrs.2014.10.010. [DOI] [PubMed] [Google Scholar]
- 30.Lockington D, Macdonald EC, Young D, Stewart P, Caslake M, Ramaesh K. Presence of free radicals in intracameral agents commonly used during cataract surgery. Br J Ophthalmol. 2010;94(12):1674–1677. doi: 10.1136/bjo.2009.171009. [DOI] [PubMed] [Google Scholar]
- 31.Cakir B, Celik E, Aksoy NO, Bursali O, Ucak T, Bozkurt E, Alagoz G. Toxic anterior segment syndrome after uncomplicated cataract surgery possibly associated with intracamaral use of cefuroxime. Clin Ophthalmol. 2015;9:493–497. doi: 10.2147/OPTH.S74249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gardner S, Barry P, Cordoves L. Toxic anterior segment syndrome and intracameral injection of cefuroxime axetil. Clin Ophthalmol. 2015;9:1865–1867. doi: 10.2147/OPTH.S91943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Andonegui J, Jimenez-Lasanta L, Aliseda D, Lameiro F. Outbreak of toxic anterior segment syndrome after vitreous surgery. Arch Soc Esp Oftalmol. 2009;84(8):403–405. doi: 10.4321/S0365-66912009000800007. [DOI] [PubMed] [Google Scholar]
- 34.Werner L, Sher JH, Taylor JR, Mamalis N, Nash WA, Csordas JE, Green G, Maziarz EP, Liu XM. Toxic anterior segment syndrome and possible association with ointment in the anterior chamber following cataract surgery. J Cataract Refract Surg. 2006;32(2):227–235. doi: 10.1016/j.jcrs.2005.12.093. [DOI] [PubMed] [Google Scholar]
- 35.Jacobs DS, Cox TA, Wagoner MD, Ariyasu RG, Karp CL, American Academy of O, ophthalmic technology assessment committee anterior segment P Capsule staining as an adjunct to cataract surgery: a report from the American Academy of ophthalmology. Ophthalmology. 2006;113(4):707–713. doi: 10.1016/j.ophtha.2006.01.024. [DOI] [PubMed] [Google Scholar]
- 36.Matsou A, Tzamalis A, Chalvatzis N, Mataftsi A, Tsinopoulos I, Brazitikos P. Generic trypan blue as possible cause of a cluster of toxic anterior segment syndrome cases after uneventful cataract surgery. J Cataract Refract Surg. 2017;43(6):848–852. doi: 10.1016/j.jcrs.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 37.Tandogan T, Khoramnia R, Uwe Auffarth G, Janusz Koss M, Young Choi C. Impact of Indocyanine green concentration, exposure time, and degree of dissolution in creating toxic anterior segment syndrome: evaluation in a rabbit model. J Ophthalmol. 2016;2016:3827050. doi: 10.1155/2016/3827050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Althomali TA. Viscoelastic substance in prefilled syringe as an etiology of toxic anterior segment syndrome. Cutan Ocul Toxicol. 2016;35(3):237–241. doi: 10.3109/15569527.2015.1082579. [DOI] [PubMed] [Google Scholar]
- 39.Kremer I, Levinger E, Levinger S. Toxic anterior segment syndrome following iris-supported phakic IOL implantation with viscoelastic Multivisc BD. Eur J Ophthalmol. 2010;20(2):451–453. doi: 10.1177/112067211002000229. [DOI] [PubMed] [Google Scholar]
- 40.Altintas AK, Ciritoglu MY, Beyazyildi ZO, Can CU, Polat S. Toxic anterior segment syndrome outbreak after cataract surgery triggered by viscoelastic substance. Middle East Afr J Ophthalmol. 2017;24(1):43–47. doi: 10.4103/meajo.MEAJO_226_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kumaran N, Larkin G, Hollick EJ. Sterile postoperative endophthalmitis following HOYA IOL insertion. Eye. 2014;28(11):1382. doi: 10.1038/eye.2014.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yazgan S, Celik U, Ayar O, Ugurbas SH, Celik B, Akdemir MO, Ugurbas SC, Alpay A. The role of patient's systemic characteristics and plateletcrit in developing toxic anterior segment syndrome after uneventful phaco surgery: a case-control study. Int Ophthalmol. 2018;38(1):43–52. [DOI] [PubMed]
- 43.Rahmani S, Eliott D. Postoperative Endophthalmitis: a review of risk factors, prophylaxis, incidence, microbiology, treatment, and outcomes. Semin Ophthalmol. 2018;33(1):95–101. doi: 10.1080/08820538.2017.1353826. [DOI] [PubMed] [Google Scholar]
- 44.American Society of C, Refractive S, American Society of Ophthalmic Registered N. Hellinger WC, Bacalis LP, Edelhauser HF, Mamalis N, Milstein B, Masket S, Cleaning AAHTFo et al. Recommended practices for cleaning and sterilizing intraocular surgical instruments. J Cataract Refract Surg. 2007;33(6):1095–1100. doi: 10.1016/j.jcrs.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 45.Durand ML. Endophthalmitis. Clin Microbiol Infect. 2013;19(3):227–234. doi: 10.1111/1469-0691.12118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dotan A, Kaiserman I, Kremer I, Ehrlich R, Bahar I. Intracameral recombinant tissue plasminogen activator (r-tPA) for refractory toxic anterior segment syndrome. Br J Ophthalmol. 2014;98(2):252–255. doi: 10.1136/bjophthalmol-2013-304294. [DOI] [PubMed] [Google Scholar]
- 47.Pineda R, 2nd, Jain V, Gupta P, Jakobiec FA. Descemet's stripping endothelial keratoplasty: an effective treatment for toxic anterior segment syndrome with histopathologic findings. Cornea. 2010;29(6):694–697. doi: 10.1097/ICO.0b013e3181bd473c. [DOI] [PubMed] [Google Scholar]
- 48.Arslan OS, Unal M, Arici C, Gorgun E, Yenerel M, Cicik E. Descemet-stripping automated endothelial keratoplasty in eyes with toxic anterior segment syndrome after cataract surgery. J Cataract Refract Surg. 2010;36(6):965–969. doi: 10.1016/j.jcrs.2009.12.037. [DOI] [PubMed] [Google Scholar]
- 49.Kaur M, Titiyal JS, Falera R, Arora T, Sharma N. Outcomes of Descemet stripping automated endothelial Keratoplasty in toxic anterior segment syndrome after phacoemulsification. Cornea. 2017;36(1):17–20. doi: 10.1097/ICO.0000000000001067. [DOI] [PubMed] [Google Scholar]
- 50.Unal M, Yucel I, Akar Y, Oner A, Altin M. Outbreak of toxic anterior segment syndrome associated with glutaraldehyde after cataract surgery. J Cataract Refract Surg. 2006;32(10):1696–1701. doi: 10.1016/j.jcrs.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 51.Lim AK, Ulagantheran VV, Siow YC, Lim KS. Methylene blue related sterile endophthalmitis. Med J Malaysia. 2008;63(3):249–250. [PubMed] [Google Scholar]
- 52.Brouzas D, Droutsas D, Charakidas A, Malias I, Georgiadou E, Apostolopoulos M, Moschos M. Severe toxic effect of methylene blue 1% on iris epithelium and corneal endothelium. Cornea. 2006;25(4):470–471. doi: 10.1097/01.ico.0000183488.78012.33. [DOI] [PubMed] [Google Scholar]
- 53.Smith CA, Khoury JM, Shields SM, Roper GJ, Duffy RE, Edelhauser HF, Lubniewski AJ. Unexpected corneal endothelial cell decompensation after intraocular surgery with instruments sterilized by plasma gas. Ophthalmology. 2000;107(8):1561–1566. doi: 10.1016/S0161-6420(00)00174-3. [DOI] [PubMed] [Google Scholar]
- 54.Cetinkaya S, Dadaci Z, Aksoy H, Acir NO, Yener HI, Kadioglu E. Toxic anterior-segment syndrome (TASS) Clin Ophthalmol. 2014;8:2065–2069. doi: 10.2147/OPTH.S71541. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are available upon request to the corresponding author at rchuck@montefiore.org