Abstract
Background
Jaundice is a common symptom of inherited or acquired liver diseases or a manifestation of diseases involving red blood cell metabolism. Recent progress has elucidated the molecular mechanisms of bile metabolism, hepatocellular transport, bile ductular development, intestinal bile salt reabsorption, and the regulation of bile acids homeostasis.
Main body
The major genetic diseases causing jaundice involve disturbances of bile flow. The insufficiency of bile salts in the intestines leads to fat malabsorption and fat-soluble vitamin deficiencies. Accumulation of excessive bile acids and aberrant metabolites results in hepatocellular injury and biliary cirrhosis. Progressive familial intrahepatic cholestasis (PFIC) is the prototype of genetic liver diseases manifesting jaundice in early childhood, progressive liver fibrosis/cirrhosis, and failure to thrive. The first three types of PFICs identified (PFIC1, PFIC2, and PFIC3) represent defects in FIC1 (ATP8B1), BSEP (ABCB11), or MDR3 (ABCB4). In the last 5 years, new genetic disorders, such as TJP2, FXR, and MYO5B defects, have been demonstrated to cause a similar PFIC phenotype. Inborn errors of bile acid metabolism also cause progressive cholestatic liver injuries. Prompt differential diagnosis is important because oral primary bile acid replacement may effectively reverse liver failure and restore liver functions. DCDC2 is a newly identified genetic disorder causing neonatal sclerosing cholangitis. Other cholestatic genetic disorders may have extra-hepatic manifestations, such as developmental disorders causing ductal plate malformation (Alagille syndrome, polycystic liver/kidney diseases), mitochondrial hepatopathy, and endocrine or chromosomal disorders. The diagnosis of genetic liver diseases has evolved from direct sequencing of a single gene to panel-based next generation sequencing. Whole exome sequencing and whole genome sequencing have been actively investigated in research and clinical studies. Current treatment modalities include medical treatment (ursodeoxycholic acid, cholic acid or chenodeoxycholic acid), surgery (partial biliary diversion and liver transplantation), symptomatic treatment for pruritus, and nutritional therapy. New drug development based on gene-specific treatments, such as apical sodium-dependent bile acid transporter (ASBT) inhibitor, for BSEP defects are underway.
Short conclusion
Understanding the complex pathways of jaundice and cholestasis not only enhance insights into liver pathophysiology but also elucidate many causes of genetic liver diseases and promote the development of novel treatments.
Keywords: Cholestasis, Genetic liver disease, Pediatric, Progressive familial intrahepatic cholestasis, Next generation sequencing, Bile acids
Background
Jaundice is a common symptom of inherited or acquired liver diseases of various causes. The underlying biochemical disturbance of jaundice is defined by direct or indirect hyperbilirubinemia. These two categories may represent different mechanisms causing jaundice. Indirect hyperbilirubinemia typically results from increased red blood cell turnover, increased bilirubin loading, or disturbances in hepatocellular update and bilirubin conjugation. Direct hyperbilirubinemia, typically defined as a direct/total bilirubin ratio of more than 15–20%, or a direct bilirubin level above 1.0 mg/dL, is collectively defined as cholestasis.
Recent progress in the past two decades has largely elucidated the molecular mechanisms underlying bile metabolism (including bilirubin, bile acids, cholesterol, phospholipid, and xenobiotics metabolism), hepatocellular transport (including uptake from sinusoidal blood and export to the canaliculus and bile ducts), bile ductular development, the intestinal reabsorption of bile salts, and the regulation of bile acids and cholesterol homeostasis. The understanding of these complex pathways not only provides insights into liver physiology but also elucidates many causes of genetic liver disease and facilitates the development of novel treatments. This review will focus mainly at hepatobiliary causes of jaundice and inherited cholestasis.
Main text
The composition and function of bile
The hepatobiliary system comprises the liver, bile duct and gall bladder. Bile is synthesized and secreted by polarized hepatocytes into bile-canaliculi, flows through bile ducts, stored in the gall bladder and is finally drained into the duodenum. The main physiological function of bile is to emulsify the lipid content of food, and this lipid emulsion facilitates lipid digestion and the absorption of lipid-soluble substances. Additionally, bile secretion is an important route to regulate cholesterol homeostasis, hemoglobin catabolism, and the elimination of drugs or drug metabolites [1].
Bile is a yellow-to-greenish amalgam of water, bile acids, ions, phospholipids (phosphatidylcholine), cholesterol, bilirubin, proteins (such as glutathione and peptides) and the other xenobiotics [1]. The yellow-to-greenish color of bile is caused by bilirubin and its derivative, which are also the origin of stool color. Bilirubin is the end catabolite of hemoglobin and other heme-containing proteins, such as myoglobin. The heme molecule is oxidized to biliverdin in hepatocytes and then reduced to unconjugated bilirubin. Unconjugated bilirubin is conjugated with one to two molecules of glucuronic acid via Uridine 5'-diphospho-glucuronosyltransferase 1A1 (UGT1A1). Bilirubin conjugation increases water solubility and reduces cytotoxicity of bilirubin. Hepatic and intestinal UGT1A1 are functionally reduced in neonatal stages, and hence, unconjugated hyperbilirubinemia is commonly found in human neonates [2]. Conjugated bilirubin, or direct bilirubin, is the major form of bilirubin in bile and is eliminated in stool. Jaundice, a yellowish pigmentation of the skin and sclera, is caused by the disrupted excretion of bilirubin and biliverdin. Interestingly, some studies involving neonates or adults have shown that hyperbilirubinemia is protective against diseases, including metabolic syndrome and asthma, [2, 3] suggesting that bilirubin may play a role as an antioxidant [4].
Bile acids are colorless and are the most abundant organic components of bile. Bile acids, a group of detergent-like molecules, are synthesized from cholesterol and are typically associated with sodium or potassium ions in the form of bile salts. Bile salts mediate lipid emulsion and act as signaling molecules to regulate gene expression [5–7]. Phospholipids and cholesterol, the second and third most abundant organic components of bile, protect against injury of the biliary epithelium from bile acids [1].
Biosynthesis and enterohepatic circulation of bile acids
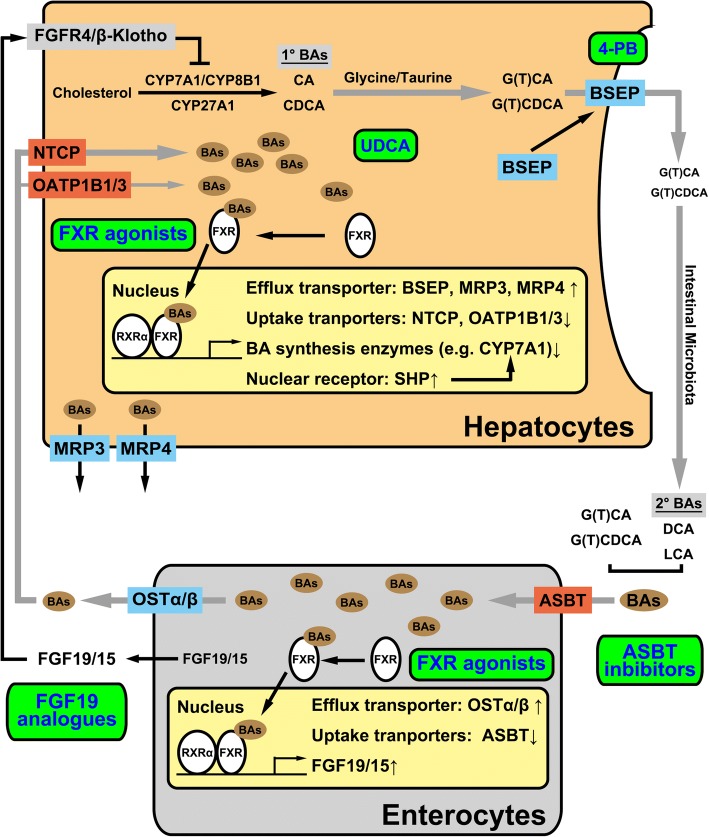
Bile acids can be synthesized from cholesterol via two pathways in hepatocytes to generate two primary bile acids, cholic acid (CA) and chenodeoxycholic acid (CDCA), through cytochrome P450 (CYP) enzymes, including CYP7A1, CYP8B1, and CYP27A1. Primary bile acids are conjugated with glycine or taurine (glyco- or tauro-conjugated CA and CDCA), with increased solubility and reduced cytotoxicity. In the intestines, gut-resident microbiota deconjugate bile salts to generate the secondary bile acids, deoxycholic acid (DCA) and lithocholic acid (LCA) [8, 9]. In human livers, de novo synthesized bile salts are 500–600 mg daily [10]. More than 90% of bile acids are reabsorbed at the distal ileum and transported back to the liver through circulation systems for the next cycle, called the enterohepatic circulation. Bile salts cycle 6- to 10-times daily. The total amount of bile salt in the body is called bile acid pool, which is approximately 2–3 g. In contrast to bile acids, only trace amounts of conjugated bilirubin will enter the enterohepatic circulation. The blockage of enterohepatic circulation to enhance bile salt elimination has been applied in surgical and medical treatments for cholestasis (Fig. 1).
Fig. 1.
The enterohepatic circulation, homeostasis of bile acids and treatment targets for cholestasis. The grey arrows indicate the route of enterohepatic circulation of bile acids. Bile acids are synthesized from cholesterol in hepatocytes to generate the primary bile acids CA and CDCA. After conjugation with glycine or taurine, bile acids (BAs) are transported from hepatocytes into the bile canaliculi via BSEP. Intestinal microbiota converts primary bile acids into the secondary bile acids DCA and LCA. Most of BAs reabsorbed by the enterocytes through ASBT in the apical membrane and then delivered into the portal circulation system via BA efflux transporter OSTα/β in the basolateral membrane. BAs are re-absorbed into hepatocytes. Hepatocytes secrete these BAs along with the de novo synthesized bile acids enter the next cycle. Bile acids also play roles in signaling to regulate the homeostasis of bile acids. The nuclear receptor FXR is the bile acid receptor to regulate bile acid homeostasis at the synthesis and the elimination levels, acting in the hepatocytes and enterocytes. The figure also shows different therapeutic targets at hepatocellular transport or enterohepatic circulations. 1°BAs, primary bile acids; 2°BAs, secondary bile acids; 4-PB, 4-phenylbutyrate; ASBT, apical sodium dependent bile acid transporter; BAs, bile acids; BSEP, bile salt export pump; CA, cholic acid; CDCD, chenodeoxy cholic acid; DCA, deoxycholic acid; FGFR4, fibroblast growth factor receptor 4; FXR, farnesoid X receptor; G(T)CA, glyco- or tauro-cholic acid; G(T)CDCA, glyco- or tauro-chenodeoxy cholic acid; LCA, lithocholic acid; MRP3, multidrug resistance-associated protein 3; MRP4, multidrug resistance-associated protein 4; NTCP, sodium/taurocholate co-transporting polypeptide; OATP1B1/3, organic-anion-transporting polypeptide 1B1 and 1B3; OSTα/β, organic solute transporter-α/β; RXRα, retinoid X receptor α; SHP, small heterodimer partner; UDCA, ursodeoxycholic acid
In human fetuses after 22 and 26 weeks of gestation, taurine-conjugated di-hydroxyl bile acids can be detected in the gallbladder. After 28 weeks, small amounts of glycine conjugates are synthesized. In postnatal stages, the ratio of CA to CDCA declines from 2.5 to 1.2 [11]. Infant livers are under development, have a small bile acid pool, and have a limited capacity for bile excretion and reabsorption. Therefore, neonates and infants, particularly premature infants, are prone to cholestasis caused by various insults, such as ischemia, drugs, infection, or parenteral nutrition.
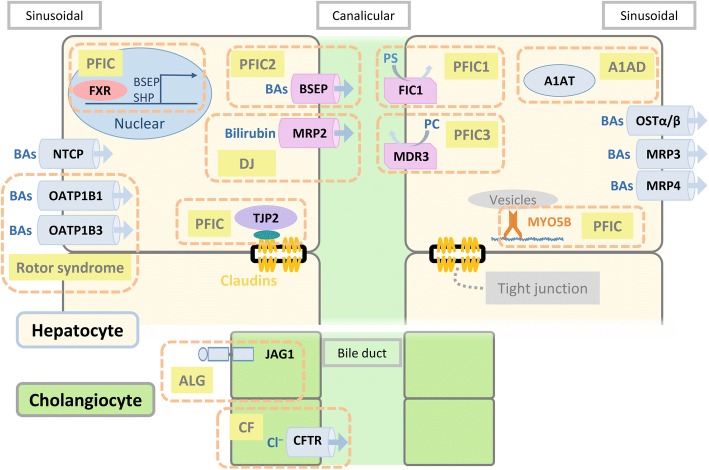
Hepatocellular transporters mediating bile flow (Fig. 2)
Fig. 2.
Hepatocellular transporters, enzymes, and regulators involving in bile transport, metabolism, and secretion. A1AD, alpha-1 antitrypsin deficiency; A1AT, alpha-1 antitrypsin; ALG, Alagille syndrome; BAs, bile acids; BSEP, bile salt export pump; Canalicular, canalicular membrane; CF, cystic fibrosis; CFTR, cystic fibrosis transmembrane conductance regulator; DJ, Dubin-Johnson syndrome; FIC1, familial intrahepatic cholestasis 1; FXR, farnesoid X receptor; JAG1, jagged 1; MDR3, multidrug resistance protein 3; MRP2, multidrug resistance-associated protein 2; MRP3, multidrug resistance-associated protein 3; MRP4, multidrug resistance-associated protein 4; MYO5B, myosin VB; NTCP, sodium/taurocholate co-transporting polypeptide; OATP1B1, organic-anion-transporting polypeptide 1B1; OATP1B3, organic-anion-transporting polypeptide 1B3; OSTα/β, organic solute transporter-α/β; PC, phosphatidylcholine; PFIC, progressive familial intrahepatic cholestasis; PS, phosphatidylserine; Sinusoidal, sinusoidal membrane; SHP, small heterodimer partner; TJP2, tight junction protein 2
Bile flow is generated by osmotic forces associated with the amount of bile salts secreted into bile canaliculi. Bile secretion from hepatocytes is mediated by a group of transport proteins, particularly ATP-binding cassette (ABC) containing proteins. The bile salt export pump (BSEP encoded by ABCB11) is the pivotal transporter mediating bile acid transport into bile canaliculi. BSEP is exclusively expressed in the apical/canalicular membrane of hepatocytes. After secreted into the small intestine, bile salts are absorbed into intestinal cells via the apical sodium-dependent bile acid transporter (ASBT encoded by SLC10A2) and then secreted into the circulation system through the basolateral heterodimeric transporter OSTα-OSTβ (encoded by OSTA and OSTB, respectively) [12–14].
The basolateral/sinusoidal membrane of hepatocytes contains several bile acid transporters to absorb bile acids from sinusoidal blood, including Na+-taurocholate co-transporting polypeptide NTCP (encoded by SLC10A1), OATP1B1 and OATP1B3 (encoded by SLCO1B1 and SLCO1B3, respectively) [12, 15]. OATP1B1 and OATP1B3 also function in the uptake of bilirubin into hepatocytes [16]. Conjugated bilirubin and organic anions are transported via canalicular multidrug resistance-associated protein 2 MRP2 (encoded by ABCC2) and, to a lesser extent, via ABCG2 into bile. Under physiological or cholestatic conditions, conjugated bilirubin may be excreted via MRP3 (encoded by ABCC3) across sinusoidal membranes into blood, to a lesser extent, and reabsorbed by OATP1B1 and OATP1B3 [3, 16].
Lipids are also important components of bile. The heterodimeric transporter ABCG5/8 mediates cholesterol across canalicular membranes. Phosphatidylcholine (PC) is flopped by the floppase multidrug resistance P-glycoprotein 3 (MDR3, encoded by ABCB4) to the outer lipid leaflet and then extracted by bile salts into bile to form micelles. The combination of cholesterol and sphingomyelin makes membranes highly detergent resistant [17, 18]. The flippase FIC1(ATP8B1) is required to flip phosphatidylserine (PS) back from the outer lipid leaflet to the inner lipid leaflet of the canalicular membrane to stabilize the integrity of the canalicular membrane [19]. Additionally, FIC1 is required for the functional expression of MDR3 [20]. Thus, hepatocytes and biliary epithelium are protected from bile acid toxicity through the efflux of bile acids mediated by BSEP and the functions of MDR3 and FIC1.
Homeostasis of bile acid pools
The homeostasis of bile acids is tightly controlled by the de novo synthesis of bile acids and the expression of transporters that affect hepatocellular bile acid levels. The key regulating molecules are farnesoid X receptor (FXR, NR1H4) and membrane-bound Takeda G protein-coupled receptor (TGR5) [6]. FXR is a nuclear receptor that is highly expressed in hepatocytes and enterocytes in the distal small intestine and colon. TGR5 is expressed in enteroendocrine cells, gallbladder cells and cholangiocytes. FXR forms heterodimers with other nuclear receptors to mediate its transcriptional activity [21–24]. Upon binding with bile acids as its natural ligands, FXR downregulates the expression of bile acid synthesis enzymes (mainly CYP7A1) and the sinusoidal uptake transporter of NTCP but upregulates the expression of the bile acid efflux transporter BSEP to reduce intracellular bile acid concentrations [25–29]. When bile acids are accumulated in hepatocytes, activated hepatic FXR increases sinusoidal bile acid efflux via MRP4 and heterodimeric OSTα/β [30, 31]. FXR also inhibits the expression of the ileal bile acid transporter ASBT to reduce the enterohepatic circulation of bile acids [32, 33]. Activation of FXR induces enterocytes to release FGF19. Through enterohepatic circulation via the portal vein, FGF19 translocates to the liver and inhibits the expression of CYP7A1 in the hepatocytes [34]. Through FXR, bile is controlled via a negative feedback loop at the transcriptional level via transporters and bile acid synthesis systems.
Cholestasis
Cholestasis is defined as disturbances in bile flow caused by diseases either in the hepatocytes, intrahepatic bile ducts or extrahepatic biliary system. Cholestatic liver disease is one of the most common forms of liver disorders resulting from inherited or acquired liver diseases. Inadequate bile flow of any causes results in accumulation of bile contents, including bilirubin, bile acids, and lipids in the liver, and consequently cause elevated levels of bilirubin and bile salts in the liver and blood, as well as dysregulated lipid metabolisms. Clinically, patients usually manifest jaundice as a result of hyperbilirubinemia. Other symptoms include clay stool, pruritus, or infrequently, bleeding episodes such as intracranial hemorrhage. Chronic cholestatic liver disease may progress to liver cirrhosis and liver failure and is the leading cause of pediatric liver transplantation. According to the anatomical location of its occurrence, cholestasis is divided into extrahepatic and intrahepatic cholestasis. Extrahepatic cholestasis is caused by structural abnormalities of the biliary tract including the obstruction of bile ducts and the gallbladder. Surgical treatments are typically applied to restore the physiological function. However, intrahepatic cholestasis is more complicated and typically requires sophisticated investigations. The common causes of extrahepatic and intrahepatic cholestasis are shown in Fig. 3.
Fig. 3.
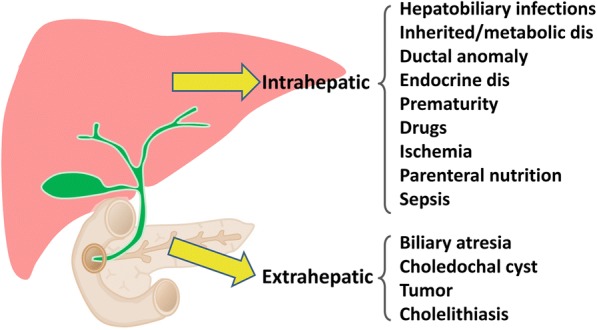
Etiologies of intrahepatic and extrahepatic cholestasis of inherited or secondary causes. dis: disorders
Etiologies of inherited bilirubin metabolism disorders causing indirect hyperbilirubinemia
Disturbances in the bilirubin metabolisms result in accumulation of bilirubin in the liver and blood, and consequently cause hyperbilirubinemia detected by routine serum biochemistry test, or called jaundice clinically. Gilbert syndrome is a benign clinical condition usually present mild intermittent jaundice in children or adult. TA repeat polymorphism (UGT1A1*28) in the promoter of UGT1A1 gene is the most commonly affected region. Gilbert syndrome can be identified in the general population, and many are identified by blood test of a health exam [35].
Crigler-Najjar syndrome is also cause by mutations in the UGT1A1 gene. Type I is a rare autosomal recessive disorder with complete loss of enzymatic function that cause extremely high bilirubin levels (above 20 mg/dL) and may lead to encephalopathy due to kernicterus. Treatments include phototherapy, exchange transfusion, or liver transplantation. Crigler-Najjar syndrome Type II manifests medium levels of hyperbilirubinemia (around 5–20 mg/dL), with retention of some enzymatic activity. Phenobarbital can be used intermittently to reduce bilirubin levels below 10-15 mg/dL.
Genetic variations in the UGT1A1 gene, especially 211 G to A (G71R in exon 1) mutation, as well as variations in the glucose-6-phosphate dehydrogenase (G6PD) and OATP2 genes, also contribute to the occurrence of neonatal jaundice and breast-feeding jaundice [36–38]. Homozygous 211 G to A mutation has been reported to be associated with severe neonatal jaundice.
Etiologies of inherited cholestasis causing direct hyperbilirubinemia
Inherited cholestatic liver diseases may manifest early in life. The presenting age ranges from infancy to young adulthood. In the last 20 years, there has been tremendous progress in understanding the genetic background of cholestatic liver disease [39–43]. Table 1 lists the categories and genes involved in inherited genetic disorders. Up to now, more than 100 inherited diseases are identified to cause cholestatic liver diseases with the initial presentation of jaundice. Some disorders may be associated with congenital anomalies or with multiple organ involvement. We have previously investigated the genetic background of pediatric patients in Taiwan with BSEP, FIC1, MDR3 defects [44–47]. We have also reported adaptive changes of hepatocyte transporters associated with obstructive cholestasis in biliary atresia, an important extrahepatic cholestatic liver disease with common symptom of prolonged neonatal jaundice [48, 49]. The distribution of disease types in Taiwanese infants with intrahepatic cholestatic liver diseases is shown in Fig. 4.
Table 1.
Differential diagnosis of jaundice caused by primary or secondary intrahepatic liver diseases
| Diseases/phenotype | Gene (Alias) |
|---|---|
| Indirect hyperbilirubinemia | |
| Crigler-Najjar syndrome | UGT1A1 |
| Gilbert syndrome | UGT1A1 |
| Direct hyperbilirubinemia | |
| Progressive familial intrahepatic cholestasis | |
| PFIC1 | ATP8B1 (FIC1) |
| PFIC2 | ABCB11 (BSEP) |
| PFIC3 | ABCB4 (MDR3) |
| Others | |
| TJP2 (ZO2) | |
| NR1H4 (FXR) | |
| Myosin 5B (MYO5B) | |
| Bilirubin Transport Defects | |
| Rotor syndrome | SLCO1B1 (OATP1B1)/ SLCO1B3 (OATP1B3) |
| Dubin-Johnson syndrome | ABCC2 (MRP2) |
| Syndromic cholestasis | |
| Alagille syndrome (paucity of interlobular bile ducts) | JAG1 |
| NOTCH2 | |
| Arthrogryposis-renal dysfunction-cholestasis syndrome. | VPS33B |
| VIPAR | |
| Inborn errors of bile acid metabolisms | |
| Bile acid synthetic defects | HSD3B7 |
| AKR1D1 (SRD5B1) | |
| CYP7B1 | |
| Bile acid conjugation defects | BAAT |
| Cerebrotendinous Xanthomatosis | CYP27A1 |
| Metabolic liver disease | |
| Wilson disease | ATP7B |
| Alpha-1-antitrypsin deficiency | SERPINA1 |
| Cystic fibrosis | CFTR |
| Neonatal cholestasis caused by citrin deficiency (type 2 citrullinemia) | SLC25A13 (CITRIN) |
| Niemann-Pick disease type C (NPC) | NPC1 |
| NPC2 | |
| Wolman disease | LIPA |
| Hepatic mitochondriopathy | |
| TWNK (C10orf2), DGUOK, MPV17, POLG, BCS1L, RRM2B, SCO1, SUCLG1 | |
| Neonatal sclerosing cholangitis | |
| CLDN1 | |
| Polycystic diseases (polycystic kidney disease; polycystic liver diseases; ductal plate malformation) | |
| PKD1, PKD2, PRKCSH, SEC63, PKHD1 | |
| Diseases with multi-organ involvement | |
| Down syndrome | |
| Endocrine disorders | |
| Hypopituitarism | |
| Hypothyroidism | |
| Hemophagocytic lymphohistiocytosis (HLH) | |
| Infections | |
| Viral infections (cytomegalovirus, enterovirus, EB virus, HIV, etc.) | |
| Bacteria infection, sepsis | |
| Toxoplasma | |
| Ischemia | |
| Shock, heart failure, cardiovascular surgery | |
| Parenteral nutrition-associated cholestasis | |
| Drugs | |
| Toxins | |
Fig. 4.
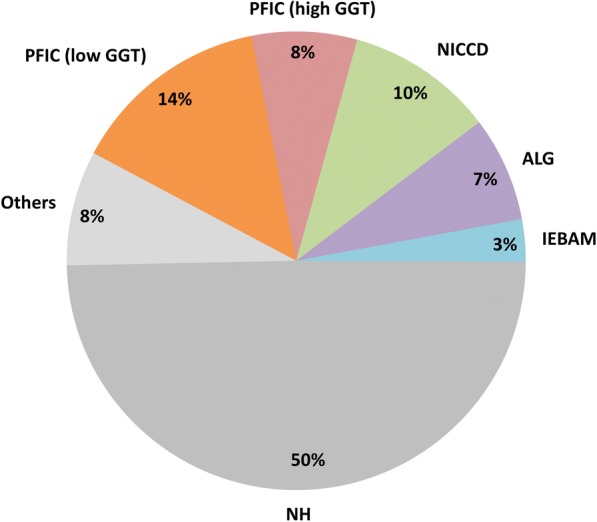
Distributions of final diagnosis of intrahepatic cholestasis in infancy in 135 Taiwanese infants 2000–2012. (Adapted from Lu FT et al., J Pediatr Gastroenterol Nutr 2014;59: 695–701). ALG, Alagille syndrome; GGT, gamma-glutamyl transpeptidase; IEBAM, inborn error of bile acid metabolism; NH, neonatal hepatitis; NICCD, neonatal intrahepatic cholestasis caused by citrin deficiency; PFIC, progressive familial intrahepatic cholestasis
Progressive familial intrahepatic cholestasis (PFIC) is a clinical syndrome with features of chronic intrahepatic cholestasis that typically begin in infancy and progress to biliary cirrhosis and hepatic failure by the first or second decade of life [40, 46, 50]. The first three types of genetic defects identified are commonly referred to as PFIC1, PFIC2, and PFIC3. PFIC1 and PFIC2 are characterized by low serum γ-glutamyltransferase (GGT) levels. PFIC1 (Byler’s disease) patients have FIC1 gene mutations, and PFIC2 patients have mutated BSEP gene. PFIC3 is characterized by high serum GGT levels and is caused by genetic mutations in the MDR3 gene [51, 52]. BSEP plays a pivotal role in bile physiology as it mediates canalicular bile salt export and is the main driving force of bile flow [53].
With the advances in genetic technologies in recent years, novel disease-causing genes for PFIC have been reported. FXR, the key regulator of bile acid metabolism, have been implicated in a novel form of infant cholestasis with liver failure in two European families [54]. We also identified a fatal case of infant cholestasis with liver failure occurring before 3 months of age [55]. Additionally, TJP2 and MYO5B have been found to cause PFIC. TJP2 is an important component of tight junctions, and a deficiency of TJP2 disrupts the tight-junction structure in the liver [56]. MYO5B is associated with low GGT infant cholestasis. MYO5B is an actin-based motor protein and an effector of Rab11a/b. MYO5B mutations result in the dysregulation of Rab proteins and further disrupt the trafficking of BSEP [57, 58]. Doublecortin domain containing 2 (DCDC2), a tubulin-binding protein, is associated with renal-hepatic ciliopathy and neonatal sclerosing cholangitis [59–61]. The mitochondrial transcription factor TFAM is associated with mitochondrial DNA depletion syndrome [62]. Recently, a homozygous single nucleotide deletion in organic solute transporter-β (OSTβ/SLC51B) was demonstrated to cause congenital diarrhea and cholestasis [63].
Dubin-Johnson and Rotor syndrome are two inherited disorders manifesting direct hyperbilirubinemia but with normal or minimally elevated alanine transaminase (ALT) levels, clinically manifesting as jaundice. Dubin-Johnson syndrome is caused by disruption of MRP2 and characterized by grossly black livers and pigment deposition in hepatocytes. Neonatal cholestasis caused by Dubin-Johnson syndrome has been reported in Taiwan and Japan [64, 65]. Our group has identified patients recovered from neonatal cholestasis had re-emergence of jaundice in young adulthood after long-term follow-up [64]. Rotor syndrome has recently been identified to be caused by genetic disruption of both SLCO1B1 and SLCO1B3 genes [66, 67]. These two disorders are benign and do not require specific treatment.
Genetic cholestasis not only causes pediatric liver disease but may also be present in adult liver disease. Additionally, adult liver diseases may result from genetic liver diseases. In general, protein functional disturbances are less detrimental and are typically caused by missense genetic mutations or multifactorial disorders. Cholestasis in pregnancy has been associated with genetic variants/mutations in ABCB4, ABCB11, ATP8B1, ABCC2 and TJP2 [68]. Adult benign recurrent intrahepatic cholestasis (BRIC) is also associated with PFIC-related genes and may have mutations that are less damaging [69–72]. Acquired forms of cholestasis, such as drug-induced liver disease, have also been associated with genetic variants [73, 74].
Diseases related to ductal plate malformation are an important group of developmental disorders that lead to a paucity or malformation of intrahepatic or interlobular bile ducts. Alagille syndrome, first described by Alagille et al., is based on clinical diagnostic criteria including a characteristic face; a paucity of interlobular bile ducts in liver pathology; and cardiac, eye, and vertebral anomalies [75]. The JAG1 mutation accounts for > 90% of cases of Alagille syndrome, and mutations in NOTCH2 have been described in a minority of patients [76]. Other syndromic disorders and polycystic liver/kidney diseases may also present with infant cholestasis as the first symptom.
Cholestasis is a common manifestation of hepatic metabolic disorders, including carbohydrate, amino acid, and fat metabolism, as well as mitochondrial and endocrine anomalies. Most of these diseases are rare disorders, and the disease incidence largely depends on ethnic background. For example, neonatal cholestasis caused by citrin deficiency (NICCD) is an important cause of cholestasis in East Asian children [77, 78]. We have previously identified facial features and biochemical characteristics for the phenotypic diagnosis of NICCD [79, 80]. Alpha 1-antitrypsin (A1AT/SERPINA1) deficiency and cystic fibrosis are important causes in western countries but how lower incidences in Asian populations.
Inborn errors of bile acid metabolism constitute a group of important metabolic disorders causing infant cholestasis. Notably, oral primary bile acid supplementation is effective and can avoid patient deterioration and the need for liver transplantation upon timely treatment [81, 82].
Neonatal hemochromatosis is an important cause of neonatal liver failure that manifests as early onset cholestasis. However, recent studies have elucidated this condition as a disorder of gestational alloimmune liver diseases instead of hereditary hemochromatosis [83]. Treatment involves exchange blood transfusion and intravenous immunoglobulin applied as early as when the neonate is born.
Other congenital anomalies, such as chromosomal anomalies, endocrine disorders, and developmental disorders may also cause cholestasis. Liver disease is typically a multi-organ manifestation of congenital anomalies.
Diagnosis
Clinical history
A careful clinical history is important to investigate common secondary causes of jaundice and cholestasis, including hemolytic anemia, G6PD deficiency, hereditary spherocytosis and other red cell membrane disorders, prematurity, sepsis, drug-induced liver injury, parenteral nutrition-associated liver diseases, ischemia, and pregnancy. Ethnic background and parental consanguinity are clues for certain types of inherited liver disorders.
Phenotypic diagnosis
The traditional phenotypic diagnosis includes low GGT as a signature of PFIC1 (FIC1 defect) and PFIC2 (BSEP defect). GGT levels, Byler’s bile in electron microscopy, and duodenal biliary bile content can be used as clinical markers to indicate further genetic confirmation [84, 85]. Syndromic cholestasis, including Alagille syndrome, can be diagnosed by phenotypic criteria [75]. Patients with NICCD have phenotypic features, and we have developed a clinical scoring system to aid in diagnosis [79, 86]. Importantly, investigating the involvement of extrahepatic organs is important for differential diagnosis.
Biochemical diagnosis
For patients suspecting jaundice or cholestasis, routine liver biochemistry tests include total and direct bilirubin levels, aspartate transferase levels, ALT levels, GGT and alkaline phosphatase (ALP) levels. Low serum GGT level disproportionate to severity of cholestasis is a clinical clue for inherited cholestasis such as PFIC and inborn errors of bile acid synthesis. Some disorders with metabolic signatures can be diagnosed with biochemical analysis. Diseases, such as inborn error of bile acid metabolism (IEBAM), [87] and metabolic disorders, such as NICCD, [86] require analysis by mass spectrometry.
Genetic diagnosis
Genetic diagnosis is a definitive diagnosis for inherited genetic liver diseases, as many of these diseases lack adequate biomarkers. Genetic tests have largely evolved in the past two decades due to the tremendous progress of genetic analysis technologies. Conventional genetic diagnosis uses direct sequencing for selected genes based on the phenotype of the patient. High-throughput methods have subsequently been developed, such as a resequencing chip that detects 5 genes for genetic cholestasis (SERPINA1, JAG1, ATP8B1, ABCB11, and ABCB4) in 2007 [88]. Denaturing high-performance liquid chromatography and high-resolution melting analysis have been used to detect single-gene variants in large numbers of patients [46, 79]. Recent next generation sequencing (NGS) panels in liver diseases have incorporated a limited number of genes, particularly PFIC [65, 89]. Expanded panel-based NGS involving more than 50 genes has been used in clinical patients with promising results [55, 90]. Whole exome sequencing has been applied to identify novel disease-causing genes [57, 63].
Treatment
Nutritional support
Bile mediates the intestinal absorption of fat and fat-soluble vitamins. In cholestatic liver diseases, the defective absorption of fat and fat-soluble vitamins (vitamins A, D, E, and K) is commonly observed but clinically obscure. Fat malabsorption results in calorie insufficiency and failure to thrive, especially in early childhood. Patients are advised to use formulas containing medium-chain triglycerides or add oils containing medium-chain triglycerides to their food. Deficiency in fat-soluble vitamins may result in multiple organ dysfunctions, including rickets, coagulopathy, and defective neurological, immunological and visual functions. Without supplementation, symptoms of deficiency, such as coagulopathy, osteoporosis, fracture, growth failure and life-threatening hemorrhage, may occur in patients. In addition, deficiencies in fat-soluble vitamins may also cause inadequate anti-oxidation, which is frequently overlooked in clinical patients.
Medical treatment
Although jaundice is the common manifestation of the highly variable etiologies, treatment does not target only to jaundice improvement (to reduce serum bilirubin level), but to target the underlying disorders that may cause hepatobiliary injury and progressive fibrosis and cirrhosis, which is usually associated with elevated bile acid levels or abnormal metabolites. Additional treatment goals are to improve nutritional status, pruritus and life quality, to prevent or to treat cirrhosis related complications.
PFICs, Alagille syndrome, and inborn errors of bile acid synthesis are the most devastating disorders that cause cirrhosis and may need liver transplantation. Effective treatment options for PFICs and Alagille syndrome are limited. Several drugs are under investigation and clinical trial. Here we will discuss about the standard treatment and several newly developed therapeutic strategies for these disorders.
Ursodeoxycholic acid (UDCA) has widely been used to treat cholestatic liver disease and is effective to improve biochemical parameters and pruritus [91]. However, UDCA is not an ideal therapeutic option for PFIC2 patients with BSEP defects. In animal models, UDCA may aggravate liver injury due to the inability of BSEP to export UDCA from hepatocytes [92]. There is a need to develop new drugs targeting BSEP defects. Missense mutations in BSEP/ABCB11 impair protein translation or intracellular trafficking, which reduce canalicular expression of BSEP and eventually cause cholestasis. Recent studies have indicated that 4-phenylbutyrate (4-PB, Buphenyl), a clinically approved pharmacological chaperone, can be used to restore the canalicular expression of BSEP. By using MDCK II cells and SD rats, Hayashi et al. reported that 4-PB significantly relocalizes and enhances the cell surface expression of both wild-type and mutated rat Bsep [93]. Besides its effect on Bsep expression, 4-PB treatment significantly increased hepatic MRP2 and decreased serum bilirubin level in patient with ornithine transcarbamylase deficiency (OTCD) [94]. Moreover, Gonzales et al. applied 4-PBA to PFIC2 patients and successfully restored the hepatic secretion of bile acids and decreased total serum bilirubin via the re-localization of mutated BSEP to canalicular membranes [95]. In addition to 4-PB, steroids are a therapeutic option to enhance BSEP expression. Cell culture experiments have suggested that dexamethasone upregulates Bsep and Mrp2 at the mRNA level in rat primary hepatocytes [96, 97], and treatment with glucocorticoids induces the expression of Bsep, Mrp2, and cytochrome P450 oxidase in rat livers [98]. Additional animal experiments and clinical tests have shown that steroid treatment improved bile homeostasis. For example, dogs receiving a high dosage of hydrocortisone (5 mg/kg) showed a significant increase in bile flow [99]. Engelmann et al. reported that steroids effectively ameliorated cholestatic itches and reduced the serum level of bile salts and bilirubin in two PFIC2 patients carrying missense mutations in BSEP [100].
Blocking enterohepatic circulation has been recently shown as a promising strategy to reduce the hepatic accumulation of bile acids in PFIC2 patients. After secretion from the gallbladder into the intestine, a majority of bile acid is absorbed by enterocytes via ASBT and recycled to liver via enterohepatic circulation. Two independent animal studies have shown that small molecule ASBT inhibitors, SC-425 and A4250, effectively reduced the enteric uptake of bile acid, decreased serum total bilirubin levels, and improved liver fibrosis and inflammation in Mdr2 knockout mice, an animal model of PFIC3 [101]. Moreover, on March 2018, A4250 successfully passed clinical phase II trials (ClinicalTrials.gov Identifier: NCT02630875).
The recently developed FXR agonist (Obeticholic acid) has been demonstrated to improve the ALP level in primary biliary cirrhosis [102], and has also been investigated for the treatment of nonalcoholic steatohepatitis (NASH) [103–105].
Certain types of the inborn errors of bile acid metabolism are treatable [81]. Oral cholic acid therapy is indicated for 3β-Hydroxy-Δ(5)-C27-steroid oxidoreductase (HSD3B7) deficiency, Δ (4)-3-oxosteroid 5β-reductase (SRD5B1, AKR1D1) deficiency, and Zellweger spectrum disorders [106]. CDCA has also been reported to be effective for oxysterol 7α-hydroxylase (CYP7B1) deficiency, cerebrotendinous xanthomatosis, and other forms of bile acid synthetic defects [107]. After treatment, patients may recover from liver dysfunction, free of jaundice, and avoid liver transplantation. Life-long therapy is indicated for the oral supplementation. Early diagnosis and treatment is important to improve outcome.
Many patients with cholestatic liver disease suffer from pruritus, except patients with inborn errors of bile acid synthesis. Alagille syndrome, PFIC1 and 2 commonly cause disturbing pruritus, which affects daily life quality. Antihistamines, rifampin, and cholestyramine have been used to partially improve the symptoms of this condition. UV-B phototherapy is an alternative therapy to treat pruritus.
Biliary diversion and nasogastric drainage
Palliative treatment with biliary diversion surgery by the disruption of enterohepatic circulation may relieve pruritus and improve liver biochemical profiles. Several strategies have been used, including external biliary diversion or ileal exclusion [108–110].
Liver transplantation
Liver transplantation is considered a curative treatment for various liver diseases [111]. However, for PFIC2 patients, the recurrence of the BSEP defect has been reported due to circulating BSEP antibodies [112, 113]. Anti-CD20 antibody and plasmapheresis have been reported to treat recurrent BSEP deficiency [114]. The outcomes in BSEP defects of common European mutations, such as D482G, are better than those of other mutation types [85]. In addition, patients with multi-organ manifestations, such as diarrhea and pancreatic insufficiency in PFIC1, cannot be treated by liver transplantation.
Liver tumor surveillance
The disruption of bile acid transport not only causes PFIC but has also been associated with hepatocellular carcinoma and cholangiocarcinoma [115, 116]. Patients with BSEP deficiency and tyrosinemia are of greater risk of developing hepatocellular carcinoma (HCC). It is mandatory that patients with PFIC be screened for liver tumors on a regular basis. Alpha-fetoprotein is not typically elevated. Some patients were found to have HCC in the explanted liver. Thirty-eight out of 175 pediatric HCC patients receiving liver transplantation were diagnosed with inherited liver diseases [117].
Hepatocyte transplantation and gene therapy
Liver transplantation is often an ultimate option for patients with severe cholestasis, but the rarity of organ sources is an important issue. Hepatocyte transplantation might be an alternative therapy to use efficiently donor tissue in a less invasive manner. Cell therapy has been investigated in animal models with various extents of hepatocyte repopulation, including models of PFIC3 (Mdr2 knockout mice), PFIC2 (Abcb11 knockout mice) and hereditary tyrosinemia [118–120]. In previous studies, we found that UDCA can provide a selective growth advantage to donor hepatocytes in Abcb11 knockout mice and enhance the repopulation of donor hepatocytes and partially correct the bile acid profile [92]. However, insufficient long-term substitution ratio of donor hepatocyte in the livers of recipients, and the lack of donor cell sources limits the wide application of UDCA to treat clinical patients. For the past two decades, more than 20 patients with inherited liver-based metabolic disorders have received hepatocyte transplantation. Most of these patients showed only partial and transient improvements in metabolic function for several months and finally underwent liver transplantation [121–123]. Among these individuals, two patients with PFIC2 showed no obvious benefits after hepatocyte transplantation, as the existing fibrosis impaired the engraftment of the transplanted hepatocytes [122]. Recently, glyceryl trinitrate have been shown to enhance the efficacy of the transplanted hepatocyte repopulation in Mdr2 knockout mice [124]. With additional treatment to boost donor cell repopulation, hepatocyte transplantation might be refined and benefit patients with cholestasis.
Few studies on experimental gene therapy for cholestatic liver diseases have been reported. The adenoviral transfer of the aquaporin-1 gene has been shown to improve bile flow in rats with estrogen-induced cholestasis, but the effect in inherited cholestatic disease has not been validated [125].
Conclusions
With the revolutionary development of genetic analysis technologies, we have largely elucidated the molecular mechanisms of jaundice, bile flow and bile metabolism and identified new causes of genetic liver diseases that cause cholestasis. The understanding of “bile biology” not only provides insights into the mechanisms of liver pathophysiology but also facilitates the diagnosis of genetic liver diseases and the development of novel treatments.
Acknowledgments
Funding
The authors’ work is supported by grants from Ministry of Science and Technology, Taiwan (MOST105–2314-B-002-132-MY3).
Abbreviations
- 4-PB
4-phenylbutyrate
- A1AT
Alpha 1-antitrypsin
- ABC
ATP-binding cassette
- AFP
Alpha-fetoprotein
- ASBT
Apical sodium dependent bile acid transporter
- BAs
Bile acids
- BSEP
Bile salt export pump
- CA
Cholic acid
- CDCD
Chenodeoxycholic acid
- CYP
Cytochrome P450
- DCA
Deoxycholic acid
- DCDC2
Doublecortin domain containing 2
- FGFR4
fibroblast growth factor receptor 4
- FXR
farnesoid X receptor
- G(T)CA
Glyco- or tauro-cholic acid
- G(T)CDCA
Glyco- or tauro-chenodeoxy cholic acid
- GGT
Gamma glutamyl transpeptidase
- HCC
Hepatocellular carcinoma
- IEBAM
Inborn error of bile acid metabolism
- LCA
Lithocholic acid
- MDR2/3
Multidrug resistance protein 2/3
- MRP2/3/4
Multidrug resistance-associated protein 2/3/4
- MYO5B
Myosin VB
- NASH
Nonalcoholic steatohepatitis
- NH
Neonatal hepatitis
- NICCD
Neonatal cholestasis caused by citrin deficiency
- NTCP
Sodium/taurocholate co-transporting polypeptide
- OATP1B1/3
Organic-anion-transporting polypeptide 1B1 and 1B3
- OSTα/β
Organic solute transporter-α/β
- PC
Phosphatidylcholine
- PFIC
Progressive familial intrahepatic cholestasis
- PS
Phosphatidylserine
- RXRα
Retinoid X receptor α
- SERPINA1
Serpin family A member 1
- SHP
Small heterodimer partner
- TFAM
Mitochondrial transcription factor A
- TGR5
Takeda G protein-coupled receptor 5 (G protein-coupled bile acid receptor 1 , GPBAR1)
- TJP2
Tight junction protein 2
- UDCA
Ursodeoxycholic acid
- UGT1A1
UDP-glucuronosyltransferase 1A1
Authors’ contributions
H-LC conceived the study and drafted the manuscript. S-HW drafted the manuscript. S-HH drafted the manuscript. B-YL drafted the manuscript. H-LC critically revised the manuscript. M-HC critically revised the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable (the manuscript does not content patient information).
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Huey-Ling Chen, Email: hueyling@ntu.edu.tw.
Shang-Hsin Wu, Email: shanghsinwu@ntu.edu.tw.
Shu-Hao Hsu, Email: hsush1@ntu.edu.tw.
Bang-Yu Liou, Email: byliou@ntu.edu.tw.
Hui-Ling Chen, Email: hlchen9@ntu.edu.tw.
Mei-Hwei Chang, Email: changmh@ntu.edu.tw.
References
- 1.Esteller A. Physiology of bile secretion. World J Gastroenterol. 2008;14:5641–5649. doi: 10.3748/wjg.14.5641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fujiwara R, Haag M, Schaeffeler E, Nies AT, Zanger UM, Schwab M. Systemic regulation of bilirubin homeostasis: potential benefits of hyperbilirubinemia. Hepatology. 2018;67:1609–1619. doi: 10.1002/hep.29599. [DOI] [PubMed] [Google Scholar]
- 3.Sticova E, Jirsa M. New insights in bilirubin metabolism and their clinical implications. World J Gastroenterol. 2013;19:6398–6407. doi: 10.3748/wjg.v19.i38.6398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sedlak TW, Saleh M, Higginson DS, Paul BD, Juluri KR, Snyder SH. Bilirubin and glutathione have complementary antioxidant and cytoprotective roles. Proc Natl Acad Sci U S A. 2009;106:5171–5176. doi: 10.1073/pnas.0813132106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chiang JY. Bile acid regulation of gene expression: roles of nuclear hormone receptors. Endocr Rev. 2002;23:443–463. doi: 10.1210/er.2000-0035. [DOI] [PubMed] [Google Scholar]
- 6.Molinaro A, Wahlstrom A, Marschall HU. Role of bile acids in metabolic control. Trends Endocrinol Metab. 2018;29:31–41. doi: 10.1016/j.tem.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Martinot E, Sedes L, Baptissart M, Lobaccaro JM, Caira F, Beaudoin C, Volle DH. Bile acids and their receptors. Mol Asp Med. 2017;56:2–9. doi: 10.1016/j.mam.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 8.Reshetnyak VI. Physiological and molecular biochemical mechanisms of bile formation. World J Gastroenterol. 2013;19:7341–7360. doi: 10.3748/wjg.v19.i42.7341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Russell DW. The enzymes, regulation, and genetics of bile acid synthesis. Annu Rev Biochem. 2003;72:137–174. doi: 10.1146/annurev.biochem.72.121801.161712. [DOI] [PubMed] [Google Scholar]
- 10.Chan J, Vandeberg JL. Hepatobiliary transport in health and disease. Clin Lipidol. 2012;7:189–202. doi: 10.2217/clp.12.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murphy GM, Signer E. Bile acid metabolism in infants and children. Gut. 1974;15:151–163. doi: 10.1136/gut.15.2.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Claro da Silva T, Polli JE, Swaan PW. The solute carrier family 10 (SLC10): beyond bile acid transport. Mol Asp Med. 2013;34:252–269. doi: 10.1016/j.mam.2012.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ballatori N, Christian WV, Wheeler SG, Hammond CL. The heteromeric organic solute transporter, OSTalpha-OSTbeta/SLC51: a transporter for steroid-derived molecules. Mol Asp Med. 2013;34:683–692. doi: 10.1016/j.mam.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dawson PA, Hubbert ML, Rao A. Getting the mOST from OST: role of organic solute transporter, OSTalpha-OSTbeta, in bile acid and steroid metabolism. Biochim Biophys Acta. 2010;1801:994–1004. doi: 10.1016/j.bbalip.2010.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Suga T, Yamaguchi H, Sato T, Maekawa M, Goto J, Mano N. Preference of conjugated bile acids over unconjugated bile acids as substrates for OATP1B1 and OATP1B3. PLoS One. 2017;12:e0169719. doi: 10.1371/journal.pone.0169719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keppler D. The roles of MRP2, MRP3, OATP1B1, and OATP1B3 in conjugated hyperbilirubinemia. Drug Metab Dispos. 2014;42:561–565. doi: 10.1124/dmd.113.055772. [DOI] [PubMed] [Google Scholar]
- 17.Schroeder RJ, Ahmed SN, Zhu Y, London E, Brown DA. Cholesterol and sphingolipid enhance the triton X-100 insolubility of glycosylphosphatidylinositol-anchored proteins by promoting the formation of detergent-insoluble ordered membrane domains. J Biol Chem. 1998;273:1150–1157. doi: 10.1074/jbc.273.2.1150. [DOI] [PubMed] [Google Scholar]
- 18.Guyot C, Stieger B. Interaction of bile salts with rat canalicular membrane vesicles: evidence for bile salt resistant microdomains. J Hepatol. 2011;55:1368–1376. doi: 10.1016/j.jhep.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 19.Linton KJ. Lipid flopping in the liver. Biochem Soc Trans. 2015;43:1003–1010. doi: 10.1042/BST20150132. [DOI] [PubMed] [Google Scholar]
- 20.Groen Annemiek, Romero Marta Rodriguez, Kunne Cindy, Hoosdally Sarah J., Dixon Peter H., Wooding Carol, Williamson Catherine, Seppen Jurgen, van den Oever Karin, Mok Kam S., Paulusma Coen C., Linton Kenneth J., Oude Elferink Ronald P.J. Complementary Functions of the Flippase ATP8B1 and the Floppase ABCB4 in Maintaining Canalicular Membrane Integrity. Gastroenterology. 2011;141(5):1927-1937.e4. doi: 10.1053/j.gastro.2011.07.042. [DOI] [PubMed] [Google Scholar]
- 21.Wang H, Chen J, Hollister K, Sowers LC, Forman BM. Endogenous bile acids are ligands for the nuclear receptor FXR/BAR. Mol Cell. 1999;3:543–553. doi: 10.1016/S1097-2765(00)80348-2. [DOI] [PubMed] [Google Scholar]
- 22.Parks DJ, Blanchard SG, Bledsoe RK, Chandra G, Consler TG, Kliewer SA, Stimmel JB, et al. Bile acids: natural ligands for an orphan nuclear receptor. Science. 1999;284:1365–1368. doi: 10.1126/science.284.5418.1365. [DOI] [PubMed] [Google Scholar]
- 23.Makishima M, Okamoto AY, Repa JJ, Tu H, Learned RM, Luk A, Hull MV, et al. Identification of a nuclear receptor for bile acids. Science. 1999;284:1362–1365. doi: 10.1126/science.284.5418.1362. [DOI] [PubMed] [Google Scholar]
- 24.Modica S, Gadaleta RM, Moschetta A. Deciphering the nuclear bile acid receptor FXR paradigm. Nucl Recept Signal. 2010;8:e005. doi: 10.1621/nrs.08005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goodwin B, Jones SA, Price RR, Watson MA, McKee DD, Moore LB, Galardi C, et al. A regulatory cascade of the nuclear receptors FXR, SHP-1, and LRH-1 represses bile acid biosynthesis. Mol Cell. 2000;6:517–526. doi: 10.1016/S1097-2765(00)00051-4. [DOI] [PubMed] [Google Scholar]
- 26.Xu G, Li H, Pan LX, Shang Q, Honda A, Ananthanarayanan M, Erickson SK, et al. FXR-mediated down-regulation of CYP7A1 dominates LXRalpha in long-term cholesterol-fed NZW rabbits. J Lipid Res. 2003;44:1956–1962. doi: 10.1194/jlr.M300182-JLR200. [DOI] [PubMed] [Google Scholar]
- 27.Balasubramaniyan N, Luo Y, Sun AQ, Suchy FJ. SUMOylation of the farnesoid X receptor (FXR) regulates the expression of FXR target genes. J Biol Chem. 2013;288:13850–13862. doi: 10.1074/jbc.M112.443937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wagner M, Fickert P, Zollner G, Fuchsbichler A, Silbert D, Tsybrovskyy O, Zatloukal K, et al. Role of farnesoid X receptor in determining hepatic ABC transporter expression and liver injury in bile duct-ligated mice. Gastroenterology. 2003;125:825–838. doi: 10.1016/S0016-5085(03)01068-0. [DOI] [PubMed] [Google Scholar]
- 29.Boyer JL, Trauner M, Mennone A, Soroka CJ, Cai SY, Moustafa T, Zollner G, et al. Upregulation of a basolateral FXR-dependent bile acid efflux transporter OSTalpha-OSTbeta in cholestasis in humans and rodents. Am J Physiol Gastrointest Liver Physiol. 2006;290:G1124–G1130. doi: 10.1152/ajpgi.00539.2005. [DOI] [PubMed] [Google Scholar]
- 30.Kullak-Ublick GA, Stieger B, Meier PJ. Enterohepatic bile salt transporters in normal physiology and liver disease. Gastroenterology. 2004;126:322–342. doi: 10.1053/j.gastro.2003.06.005. [DOI] [PubMed] [Google Scholar]
- 31.Geier A, Wagner M, Dietrich CG, Trauner M. Principles of hepatic organic anion transporter regulation during cholestasis, inflammation and liver regeneration. Biochim Biophys Acta. 2007;1773:283–308. doi: 10.1016/j.bbamcr.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 32.Li H, Chen F, Shang Q, Pan L, Shneider BL, Chiang JY, Forman BM, et al. FXR-activating ligands inhibit rabbit ASBT expression via FXR-SHP-FTF cascade. Am J Physiol Gastrointest Liver Physiol. 2005;288:G60–G66. doi: 10.1152/ajpgi.00170.2004. [DOI] [PubMed] [Google Scholar]
- 33.Neimark E, Chen F, Li X, Shneider BL. Bile acid-induced negative feedback regulation of the human ileal bile acid transporter. Hepatology. 2004;40:149–156. doi: 10.1002/hep.20295. [DOI] [PubMed] [Google Scholar]
- 34.Inagaki T, Moschetta A, Lee YK, Peng L, Zhao G, Downes M, Yu RT, et al. Regulation of antibacterial defense in the small intestine by the nuclear bile acid receptor. Proc Natl Acad Sci U S A. 2006;103:3920–3925. doi: 10.1073/pnas.0509592103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang CS. Molecular genetics of unconjugated hyperbilirubinemia in Taiwanese. J Biomed Sci. 2005;12:445–450. doi: 10.1007/s11373-005-3863-5. [DOI] [PubMed] [Google Scholar]
- 36.Memon N, Weinberger BI, Hegyi T, Aleksunes LM. Inherited disorders of bilirubin clearance. Pediatr Res. 2016;79:378–386. doi: 10.1038/pr.2015.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chou HC, Chen MH, Yang HI, Su YN, Hsieh WS, Chen CY, Chen HL, et al. 211 G to a variation of UDP-glucuronosyl transferase 1A1 gene and neonatal breastfeeding jaundice. Pediatr Res. 2011;69:170–174. doi: 10.1203/PDR.0b013e31820263d2. [DOI] [PubMed] [Google Scholar]
- 38.Chang PF, Lin YC, Liu K, Yeh SJ, Ni YH. Risk of hyperbilirubinemia in breast-fed infants. J Pediatr. 2011;159:561–565. doi: 10.1016/j.jpeds.2011.03.042. [DOI] [PubMed] [Google Scholar]
- 39.Jansen PL, Sturm E. Genetic cholestasis, causes and consequences for hepatobiliary transport. Liver Int. 2003;23:315–322. doi: 10.1034/j.1478-3231.2003.00856.x. [DOI] [PubMed] [Google Scholar]
- 40.Santos JL, Choquette M, Bezerra JA. Cholestatic liver disease in children. Curr Gastroenterol Rep. 2010;12:30–39. doi: 10.1007/s11894-009-0081-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.A W. Medical management of chronic cholestasis. In: Walker’s Pediatric Gastrointestinal Diseases. BC Decker Inc: Hamilton. 2008:797–799.
- 42.Loomes KM, Emerick KM. Pediatric cholestatic liver disease. In: Wyllie R, Hyams JS, Kay M ed. Pediatric gastrointestinal and liver disease. 5th edition. Elsevier (Philadelphia, PA) 2016:851–869.
- 43.Kelly Deirdre A., editor. Diseases of the Liver and Biliary System in Children. Chichester, UK: John Wiley & Sons, Ltd; 2017. [Google Scholar]
- 44.Chen HL, Chang PS, Hsu HC, Lee JH, Ni YH, Hsu HY, Jeng YM, et al. Progressive familial intrahepatic cholestasis with high gamma-glutamyltranspeptidase levels in Taiwanese infants: role of MDR3 gene defect? Pediatr Res. 2001;50:50–55. doi: 10.1203/00006450-200107000-00011. [DOI] [PubMed] [Google Scholar]
- 45.Chen HL, Chang PS, Hsu HC, Ni YH, Hsu HY, Lee JH, Jeng YM, et al. FIC1 and BSEP defects in Taiwanese patients with chronic intrahepatic cholestasis with low gamma-glutamyltranspeptidase levels. J Pediatr. 2002;140:119–124. doi: 10.1067/mpd.2002.119993. [DOI] [PubMed] [Google Scholar]
- 46.Chen HL, Liu YJ, Su YN, Wang NY, Wu SH, Ni YH, Hsu HY, et al. Diagnosis of BSEP/ABCB11 mutations in Asian patients with cholestasis using denaturing high performance liquid chromatography. J Pediatr. 2008;153:825–832. doi: 10.1016/j.jpeds.2008.06.034. [DOI] [PubMed] [Google Scholar]
- 47.Hsu YC, Chen HL, Wu MZ, Liu YJ, Lee PH, Sheu JC, Chen CH. Adult progressive intrahepatic cholestasis associated with genetic variations in ATP8B1 and ABCB11. Hepatol Res. 2009;39:625–631. doi: 10.1111/j.1872-034X.2009.00499.x. [DOI] [PubMed] [Google Scholar]
- 48.Lien TH, Chang MH, Wu JF, Chen HL, Lee HC, Chen AC, Tiao MM, et al. Effects of the infant stool color card screening program on 5-year outcome of biliary atresia in Taiwan. Hepatology. 2011;53:202–208. doi: 10.1002/hep.24023. [DOI] [PubMed] [Google Scholar]
- 49.Chen HL, Liu YJ, Chen HL, Wu SH, Ni YH, Ho MC, Lai HS, et al. Expression of hepatocyte transporters and nuclear receptors in children with early and late-stage biliary atresia. Pediatr Res. 2008;63:667–673. doi: 10.1203/PDR.0b013e318170a6b5. [DOI] [PubMed] [Google Scholar]
- 50.Strautnieks SS, Bull LN, Knisely AS, Kocoshis SA, Dahl N, Arnell H, Sokal E, et al. A gene encoding a liver-specific ABC transporter is mutated in progressive familial intrahepatic cholestasis. Nat Genet. 1998;20:233–238. doi: 10.1038/3034. [DOI] [PubMed] [Google Scholar]
- 51.Bull LN, van Eijk MJ, Pawlikowska L, DeYoung JA, Juijn JA, Liao M, Klomp LW, et al. A gene encoding a P-type ATPase mutated in two forms of hereditary cholestasis. Nat Genet. 1998;18:219–224. doi: 10.1038/ng0398-219. [DOI] [PubMed] [Google Scholar]
- 52.de Vree JM, Jacquemin E, Sturm E, Cresteil D, Bosma PJ, Aten J, Deleuze JF, et al. Mutations in the MDR3 gene cause progressive familial intrahepatic cholestasis. Proc Natl Acad Sci U S A. 1998;95:282–287. doi: 10.1073/pnas.95.1.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Thompson R, Strautnieks S. BSEP: function and role in progressive familial intrahepatic cholestasis. Semin Liver Dis. 2001;21:545–550. doi: 10.1055/s-2001-19038. [DOI] [PubMed] [Google Scholar]
- 54.Gomez-Ospina N, Potter CJ, Xiao R, Manickam K, Kim MS, Kim KH, Shneider BL, et al. Mutations in the nuclear bile acid receptor FXR cause progressive familial intrahepatic cholestasis. Nat Commun. 2016;7:10713. doi: 10.1038/ncomms10713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chen HL LH, Wu JF, Wu SH, Chen HL, Yang YH, Hsu YH, Liou BY, Chang MH, Ni YH. Panel-based Next-Generation Sequencing for the Diagnosis of Cholestatic Genetic Liver Diseases: Clinical Utility and Challenges. J Pediatr. 2018;(in press). [DOI] [PubMed]
- 56.Sambrotta M, Strautnieks S, Papouli E, Rushton P, Clark BE, Parry DA, Logan CV, et al. Mutations in TJP2 cause progressive cholestatic liver disease. Nat Genet. 2014;46:326–328. doi: 10.1038/ng.2918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Qiu YL, Gong JY, Feng JY, Wang RX, Han J, Liu T, Lu Y, et al. Defects in myosin VB are associated with a spectrum of previously undiagnosed low gamma-glutamyltransferase cholestasis. Hepatology. 2017;65:1655–1669. doi: 10.1002/hep.29020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gonzales E, Taylor SA, Davit-Spraul A, Thebaut A, Thomassin N, Guettier C, Whitington PF, et al. MYO5B mutations cause cholestasis with normal serum gamma-glutamyl transferase activity in children without microvillous inclusion disease. Hepatology. 2017;65:164–173. doi: 10.1002/hep.28779. [DOI] [PubMed] [Google Scholar]
- 59.Schueler M, Braun DA, Chandrasekar G, Gee HY, Klasson TD, Halbritter J, Bieder A, et al. DCDC2 mutations cause a renal-hepatic ciliopathy by disrupting Wnt signaling. Am J Hum Genet. 2015;96:81–92. doi: 10.1016/j.ajhg.2014.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Grammatikopoulos T, Sambrotta M, Strautnieks S, Foskett P, Knisely AS, Wagner B, Deheragoda M, et al. Mutations in DCDC2 (doublecortin domain containing protein 2) in neonatal sclerosing cholangitis. J Hepatol. 2016;65:1179–1187. doi: 10.1016/j.jhep.2016.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Girard M, Bizet AA, Lachaux A, Gonzales E, Filhol E, Collardeau-Frachon S, Jeanpierre C, et al. DCDC2 mutations cause neonatal Sclerosing cholangitis. Hum Mutat. 2016;37:1025–1029. doi: 10.1002/humu.23031. [DOI] [PubMed] [Google Scholar]
- 62.Stiles AR, Simon MT, Stover A, Eftekharian S, Khanlou N, Wang HL, Magaki S, et al. Mutations in TFAM, encoding mitochondrial transcription factor a, cause neonatal liver failure associated with mtDNA depletion. Mol Genet Metab. 2016;119:91–99. doi: 10.1016/j.ymgme.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 63.Sultan Mutaz, Rao Anuradha, Elpeleg Orly, Vaz Frédéric M., Abu-Libdeh Bassam, Karpen Saul J., Dawson Paul A. Organic solute transporter-β (SLC51B ) deficiency in two brothers with congenital diarrhea and features of cholestasis. Hepatology. 2018;68(2):590–598. doi: 10.1002/hep.29516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lee JH, Chen HL, Chen HL, Ni YH, Hsu HY, Chang MH. Neonatal Dubin-Johnson syndrome: long-term follow-up and MRP2 mutations study. Pediatr Res. 2006;59:584–589. doi: 10.1203/01.pdr.0000203093.10908.bb. [DOI] [PubMed] [Google Scholar]
- 65.Togawa Takao, Sugiura Tokio, Ito Koichi, Endo Takeshi, Aoyama Kohei, Ohashi Kei, Negishi Yutaka, Kudo Toyoichiro, Ito Reiko, Kikuchi Atsuo, Arai-Ichinoi Natsuko, Kure Shigeo, Saitoh Shinji. Molecular Genetic Dissection and Neonatal/Infantile Intrahepatic Cholestasis Using Targeted Next-Generation Sequencing. The Journal of Pediatrics. 2016;171:171-177.e4. doi: 10.1016/j.jpeds.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 66.van de Steeg E, Stranecky V, Hartmannova H, Noskova L, Hrebicek M, Wagenaar E, van Esch A, et al. Complete OATP1B1 and OATP1B3 deficiency causes human rotor syndrome by interrupting conjugated bilirubin reuptake into the liver. J Clin Invest. 2012;122:519–528. doi: 10.1172/JCI59526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kagawa T, Oka A, Kobayashi Y, Hiasa Y, Kitamura T, Sakugawa H, Adachi Y, et al. Recessive inheritance of population-specific intronic LINE-1 insertion causes a rotor syndrome phenotype. Hum Mutat. 2015;36:327–332. doi: 10.1002/humu.22745. [DOI] [PubMed] [Google Scholar]
- 68.Dixon PH, Sambrotta M, Chambers J, Taylor-Harris P, Syngelaki A, Nicolaides K, Knisely AS, et al. An expanded role for heterozygous mutations of ABCB4, ABCB11, ATP8B1, ABCC2 and TJP2 in intrahepatic cholestasis of pregnancy. Sci Rep. 2017;7:11823. doi: 10.1038/s41598-017-11626-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.van Mil SW, van der Woerd WL, van der Brugge G, Sturm E, Jansen PL, Bull LN, van den Berg IE, et al. Benign recurrent intrahepatic cholestasis type 2 is caused by mutations in ABCB11. Gastroenterology. 2004;127:379–384. doi: 10.1053/j.gastro.2004.04.065. [DOI] [PubMed] [Google Scholar]
- 70.Mullenbach R, Bennett A, Tetlow N, Patel N, Hamilton G, Cheng F, Chambers J, et al. ATP8B1 mutations in British cases with intrahepatic cholestasis of pregnancy. Gut. 2005;54:829–834. doi: 10.1136/gut.2004.058115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kagawa T, Watanabe N, Mochizuki K, Numari A, Ikeno Y, Itoh J, Tanaka H, et al. Phenotypic differences in PFIC2 and BRIC2 correlate with protein stability of mutant Bsep and impaired taurocholate secretion in MDCK II cells. Am J Physiol Gastrointest Liver Physiol. 2008;294:G58–G67. doi: 10.1152/ajpgi.00367.2007. [DOI] [PubMed] [Google Scholar]
- 72.Stapelbroek JM, van Erpecum KJ, Klomp LW, Venneman NG, Schwartz TP, van Berge Henegouwen GP, Devlin J, et al. Nasobiliary drainage induces long-lasting remission in benign recurrent intrahepatic cholestasis. Hepatology. 2006;43:51–53. doi: 10.1002/hep.20998. [DOI] [PubMed] [Google Scholar]
- 73.Ulzurrun E, Stephens C, Crespo E, Ruiz-Cabello F, Ruiz-Nunez J, Saenz-Lopez P, Moreno-Herrera I, et al. Role of chemical structures and the 1331T>C bile salt export pump polymorphism in idiosyncratic drug-induced liver injury. Liver Int. 2013;33:1378–1385. doi: 10.1111/liv.12193. [DOI] [PubMed] [Google Scholar]
- 74.Kubitz R, Droge C, Stindt J, Weissenberger K, Haussinger D. The bile salt export pump (BSEP) in health and disease. Clin Res Hepatol Gastroenterol. 2012;36:536–553. doi: 10.1016/j.clinre.2012.06.006. [DOI] [PubMed] [Google Scholar]
- 75.Alagille D, Odievre M, Gautier M, Dommergues JP. Hepatic ductular hypoplasia associated with characteristic facies, vertebral malformations, retarded physical, mental, and sexual development, and cardiac murmur. J Pediatr. 1975;86:63–71. doi: 10.1016/S0022-3476(75)80706-2. [DOI] [PubMed] [Google Scholar]
- 76.Grochowski CM, Loomes KM, Spinner NB. Jagged1 (JAG1): structure, expression, and disease associations. Gene. 2016;576:381–384. doi: 10.1016/j.gene.2015.10.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kobayashi K, Bang Lu Y, Xian Li M, Nishi I, Hsiao KJ, Choeh K, Yang Y, et al. Screening of nine SLC25A13 mutations: their frequency in patients with citrin deficiency and high carrier rates in Asian populations. Mol Genet Metab. 2003;80:356–359. doi: 10.1016/S1096-7192(03)00140-9. [DOI] [PubMed] [Google Scholar]
- 78.Ohura T, Kobayashi K, Tazawa Y, Abukawa D, Sakamoto O, Tsuchiya S, Saheki T. Clinical pictures of 75 patients with neonatal intrahepatic cholestasis caused by citrin deficiency (NICCD) J Inherit Metab Dis. 2007;30:139–144. doi: 10.1007/s10545-007-0506-1. [DOI] [PubMed] [Google Scholar]
- 79.Chen ST, Su YN, Ni YH, Hwu WL, Lee NC, Chien YH, Chang CC, et al. Diagnosis of neonatal intrahepatic cholestasis caused by citrin deficiency using high-resolution melting analysis and a clinical scoring system. J Pediatr. 2012;161:626–631.e622. doi: 10.1016/j.jpeds.2012.03.038. [DOI] [PubMed] [Google Scholar]
- 80.Chen HW, Chen HL, Ni YH, Lee NC, Chien YH, Hwu WL, Huang YT, et al. Chubby face and the biochemical parameters for the early diagnosis of neonatal intrahepatic cholestasis caused by citrin deficiency. J Pediatr Gastroenterol Nutr. 2008;47:187–192. doi: 10.1097/MPG.0b013e318162d96d. [DOI] [PubMed] [Google Scholar]
- 81.Clayton PT. Disorders of bile acid synthesis. J Inherit Metab Dis. 2011;34:593–604. doi: 10.1007/s10545-010-9259-3. [DOI] [PubMed] [Google Scholar]
- 82.Heubi JE, Setchell KD, Jha P, Buckley D, Zhang W, Rosenthal P, Potter C, et al. Treatment of bile acid amidation defects with glycocholic acid. Hepatology. 2015;61:268–274. doi: 10.1002/hep.27401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Taylor Sarah A., Kelly Susan, Alonso Estella M., Whitington Peter F. The Effects of Gestational Alloimmune Liver Disease on Fetal and Infant Morbidity and Mortality. The Journal of Pediatrics. 2018;196:123-128.e1. doi: 10.1016/j.jpeds.2017.12.054. [DOI] [PubMed] [Google Scholar]
- 84.Lu FT, Wu JF, Hsu HY, Ni YH, Chang MH, Chao CI, Chen HL. Gamma-Glutamyl transpeptidase level as a screening marker among diverse etiologies of infantile intrahepatic cholestasis. J Pediatr Gastroenterol Nutr. 2014;59:695–701. doi: 10.1097/MPG.0000000000000538. [DOI] [PubMed] [Google Scholar]
- 85.Pawlikowska L, Strautnieks S, Jankowska I, Czubkowski P, Emerick K, Antoniou A, Wanty C, et al. Differences in presentation and progression between severe FIC1 and BSEP deficiencies. J Hepatol. 2010;53:170–178. doi: 10.1016/j.jhep.2010.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Saheki T, Kobayashi K. Mitochondrial aspartate glutamate carrier (citrin) deficiency as the cause of adult-onset type II citrullinemia (CTLN2) and idiopathic neonatal hepatitis (NICCD) J Hum Genet. 2002;47:333–341. doi: 10.1007/s100380200046. [DOI] [PubMed] [Google Scholar]
- 87.Heubi JE, Setchell KD, Bove KE. Inborn errors of bile acid metabolism. Semin Liver Dis. 2007;27:282–294. doi: 10.1055/s-2007-985073. [DOI] [PubMed] [Google Scholar]
- 88.Liu C, Aronow BJ, Jegga AG, Wang N, Miethke A, Mourya R, Bezerra JA. Novel resequencing chip customized to diagnose mutations in patients with inherited syndromes of intrahepatic cholestasis. Gastroenterology. 2007;132:119–126. doi: 10.1053/j.gastro.2006.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Vitale G, Pirillo M, Mantovani V, Marasco E, Aquilano A, Gamal N, Francalanci P, et al. Bile salt export pump deficiency disease: two novel, late onset, ABCB11 mutations identified by next generation sequencing. Ann Hepatol. 2016;15:795–800. doi: 10.5604/16652681.1212618. [DOI] [PubMed] [Google Scholar]
- 90.Karpen SJ, Kamath BM, Alexander II, Ichetovkin I, Rosenthal P, Soliman W, ea. Use of a comprehensive 66 gene panel to diagnosis the cause of cholestasis in > 700 individuals. Hepatology 2017; 66(suppl 1):655A. [AASLD abstract].
- 91.Paumgartner G, Beuers U. Ursodeoxycholic acid in cholestatic liver disease: mechanisms of action and therapeutic use revisited. Hepatology. 2002;36:525–531. doi: 10.1053/jhep.2002.36088. [DOI] [PubMed] [Google Scholar]
- 92.Chen HL, Chen HL, Yuan RH, Wu SH, Chen YH, Chien CS, Chou SP, et al. Hepatocyte transplantation in bile salt export pump-deficient mice: selective growth advantage of donor hepatocytes under bile acid stress. J Cell Mol Med. 2012;16:2679–2689. doi: 10.1111/j.1582-4934.2012.01586.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hayashi H, Sugiyama Y. 4-phenylbutyrate enhances the cell surface expression and the transport capacity of wild-type and mutated bile salt export pumps. Hepatology. 2007;45:1506–1516. doi: 10.1002/hep.21630. [DOI] [PubMed] [Google Scholar]
- 94.Hayashi H, Mizuno T, Horikawa R, Nagasaka H, Yabuki T, Takikawa H, Sugiyama Y. 4-Phenylbutyrate modulates ubiquitination of hepatocanalicular MRP2 and reduces serum total bilirubin concentration. J Hepatol. 2012;56:1136–1144. doi: 10.1016/j.jhep.2011.11.021. [DOI] [PubMed] [Google Scholar]
- 95.Gonzales E, Grosse B, Cassio D, Davit-Spraul A, Fabre M, Jacquemin E. Successful mutation-specific chaperone therapy with 4-phenylbutyrate in a child with progressive familial intrahepatic cholestasis type 2. J Hepatol. 2012;57:695–698. doi: 10.1016/j.jhep.2012.04.017. [DOI] [PubMed] [Google Scholar]
- 96.Kubitz R, Warskulat U, Schmitt M, Haussinger D. Dexamethasone- and osmolarity-dependent expression of the multidrug-resistance protein 2 in cultured rat hepatocytes. Biochem J. 1999;340(Pt 3):585–591. doi: 10.1042/bj3400585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Warskulat U, Kubitz R, Wettstein M, Stieger B, Meier PJ, Haussinger D. Regulation of bile salt export pump mRNA levels by dexamethasone and osmolarity in cultured rat hepatocytes. Biol Chem. 1999;380:1273–1279. doi: 10.1515/BC.1999.162. [DOI] [PubMed] [Google Scholar]
- 98.Fardel O, Payen L, Courtois A, Vernhet L, Lecureur V. Regulation of biliary drug efflux pump expression by hormones and xenobiotics. Toxicology. 2001;167:37–46. doi: 10.1016/S0300-483X(01)00456-5. [DOI] [PubMed] [Google Scholar]
- 99.Brems JJ, Reese J, Kane R, 3rd, Kaminski DL. Effect of cyclosporine and steroids on canine bile flow. Hepatology. 1991;14:523–527. doi: 10.1002/hep.1840140319. [DOI] [PubMed] [Google Scholar]
- 100.Engelmann G, Wenning D, Herebian D, Sander O, Droge C, Kluge S, Kubitz R. Two case reports of successful treatment of cholestasis with steroids in patients with PFIC-2. Pediatrics. 2015;135:e1326–e1332. doi: 10.1542/peds.2014-2376. [DOI] [PubMed] [Google Scholar]
- 101.Miethke AG, Zhang W, Simmons J, Taylor AE, Shi T, Shanmukhappa SK, Karns R, et al. Pharmacological inhibition of apical sodium-dependent bile acid transporter changes bile composition and blocks progression of sclerosing cholangitis in multidrug resistance 2 knockout mice. Hepatology. 2016;63:512–523. doi: 10.1002/hep.27973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hirschfield GM, Mason A, Luketic V, Lindor K, Gordon SC, Mayo M, Kowdley KV, et al. Efficacy of obeticholic acid in patients with primary biliary cirrhosis and inadequate response to ursodeoxycholic acid. Gastroenterology. 2015;148:751–761.e758. doi: 10.1053/j.gastro.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 103.Mudaliar S, Henry RR, Sanyal AJ, Morrow L, Marschall HU, Kipnes M, Adorini L, et al. Efficacy and safety of the farnesoid X receptor agonist obeticholic acid in patients with type 2 diabetes and nonalcoholic fatty liver disease. Gastroenterology. 2013;145:574–582.e571. doi: 10.1053/j.gastro.2013.05.042. [DOI] [PubMed] [Google Scholar]
- 104.Neuschwander-Tetri BA, Loomba R, Sanyal AJ, Lavine JE, Van Natta ML, Abdelmalek MF, Chalasani N, et al. Farnesoid X nuclear receptor ligand obeticholic acid for non-cirrhotic, non-alcoholic steatohepatitis (FLINT): a multicentre, randomised, placebo-controlled trial. Lancet. 2015;385:956–965. doi: 10.1016/S0140-6736(14)61933-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Beuers U, Trauner M, Jansen P, Poupon R. New paradigms in the treatment of hepatic cholestasis: from UDCA to FXR, PXR and beyond. J Hepatol. 2015;62:S25–S37. doi: 10.1016/j.jhep.2015.02.023. [DOI] [PubMed] [Google Scholar]
- 106.Heubi JE, Bove KE, Setchell KDR. Oral Cholic acid is efficacious and well tolerated in patients with bile acid synthesis and Zellweger Spectrum disorders. J Pediatr Gastroenterol Nutr. 2017;65:321–326. doi: 10.1097/MPG.0000000000001657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Dai D, Mills PB, Footitt E, Gissen P, McClean P, Stahlschmidt J, Coupry I, et al. Liver disease in infancy caused by oxysterol 7 alpha-hydroxylase deficiency: successful treatment with chenodeoxycholic acid. J Inherit Metab Dis. 2014;37:851–861. doi: 10.1007/s10545-014-9695-6. [DOI] [PubMed] [Google Scholar]
- 108.Jericho HS, Kaurs E, Boverhof R, Knisely A, Shneider BL, Verkade HJ, Whitington PF. Bile acid pool dynamics in progressive familial intrahepatic cholestasis with partial external bile diversion. J Pediatr Gastroenterol Nutr. 2015;60:368–374. doi: 10.1097/MPG.0000000000000630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Emerick KM, Elias MS, Melin-Aldana H, Strautnieks S, Thompson RJ, Bull LN, Knisely A, et al. Bile composition in Alagille syndrome and PFIC patients having partial external biliary diversion. BMC Gastroenterol. 2008;8:47. doi: 10.1186/1471-230X-8-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Jankowska I, Czubkowski P, Kalicinski P, Ismail H, Kowalski A, Ryzko J, Pawlowska J. Ileal exclusion in children with progressive familial intrahepatic cholestasis. J Pediatr Gastroenterol Nutr. 2014;58:92–95. doi: 10.1097/MPG.0b013e3182a9097c. [DOI] [PubMed] [Google Scholar]
- 111.Oishi K, Arnon R, Wasserstein MP, Diaz GA. Liver transplantation for pediatric inherited metabolic disorders: considerations for indications, complications, and perioperative management. Pediatr Transplant. 2016;20:756–769. doi: 10.1111/petr.12741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Jara P, Hierro L, Martinez-Fernandez P, Alvarez-Doforno R, Yanez F, Diaz MC, Camarena C, et al. Recurrence of bile salt export pump deficiency after liver transplantation. N Engl J Med. 2009;361:1359–1367. doi: 10.1056/NEJMoa0901075. [DOI] [PubMed] [Google Scholar]
- 113.Stindt J, Kluge S, Droge C, Keitel V, Stross C, Baumann U, Brinkert F, et al. Bile salt export pump-reactive antibodies form a polyclonal, multi-inhibitory response in antibody-induced bile salt export pump deficiency. Hepatology. 2016;63:524–537. doi: 10.1002/hep.28311. [DOI] [PubMed] [Google Scholar]
- 114.Lin HC, Alvarez L, Laroche G, Melin-Aldana H, Pfeifer K, Schwarz K, Whitington PF, et al. Rituximab as therapy for the recurrence of bile salt export pump deficiency after liver transplantation. Liver Transpl. 2013;19:1403–1410. doi: 10.1002/lt.23754. [DOI] [PubMed] [Google Scholar]
- 115.Knisely AS, Strautnieks SS, Meier Y, Stieger B, Byrne JA, Portmann BC, Bull LN, et al. Hepatocellular carcinoma in ten children under five years of age with bile salt export pump deficiency. Hepatology. 2006;44:478–486. doi: 10.1002/hep.21287. [DOI] [PubMed] [Google Scholar]
- 116.Scheimann AO, Strautnieks SS, Knisely AS, Byrne JA, Thompson RJ, Finegold MJ. Mutations in bile salt export pump (ABCB11) in two children with progressive familial intrahepatic cholestasis and cholangiocarcinoma. J Pediatr. 2007;150:556–559. doi: 10.1016/j.jpeds.2007.02.030. [DOI] [PubMed] [Google Scholar]
- 117.Baumann U, Adam R, Duvoux C, Mikolajczyk R, Karam V, D'Antiga L, Chardot C, et al. Survival of children after liver transplantation for hepatocellular carcinoma. Liver Transpl. 2018;24:246–255. doi: 10.1002/lt.24994. [DOI] [PubMed] [Google Scholar]
- 118.Chen HL, Wang R, Chen HL, Hwu WL, Jeng YM, Chang MH, Ling V. Bone marrow transplantation results in donor-derived hepatocytes in an animal model of inherited cholestatic liver disease. J Biomed Sci. 2008;15:615–622. doi: 10.1007/s11373-008-9255-x. [DOI] [PubMed] [Google Scholar]
- 119.Smith AJ, de Vree JM, Ottenhoff R, Oude Elferink RP, Schinkel AH, Borst P. Hepatocyte-specific expression of the human MDR3 P-glycoprotein gene restores the biliary phosphatidylcholine excretion absent in Mdr2 (−/−) mice. Hepatology. 1998;28:530–536. doi: 10.1002/hep.510280234. [DOI] [PubMed] [Google Scholar]
- 120.Overturf K, Al-Dhalimy M, Tanguay R, Brantly M, Ou CN, Finegold M, Grompe M. Hepatocytes corrected by gene therapy are selected in vivo in a murine model of hereditary tyrosinaemia type I. Nat Genet. 1996;12:266–273. doi: 10.1038/ng0396-266. [DOI] [PubMed] [Google Scholar]
- 121.Sokal EM, Smets F, Bourgois A, Van Maldergem L, Buts JP, Reding R, Bernard Otte J, et al. Hepatocyte transplantation in a 4-year-old girl with peroxisomal biogenesis disease: technique, safety, and metabolic follow-up. Transplantation. 2003;76:735–738. doi: 10.1097/01.TP.0000077420.81365.53. [DOI] [PubMed] [Google Scholar]
- 122.Quaglia A, Lehec SC, Hughes RD, Mitry RR, Knisely AS, Devereaux S, Richards J, et al. Liver after hepatocyte transplantation for liver-based metabolic disorders in children. Cell Transplant. 2008;17:1403–1414. doi: 10.3727/096368908787648083. [DOI] [PubMed] [Google Scholar]
- 123.Heath RD, Ertem F, Romana BS, Ibdah JA, Tahan V. Hepatocyte transplantation: consider infusion before incision. World J Transplant. 2017;7:317–323. doi: 10.5500/wjt.v7.i6.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Boudechiche L, Tranchart H, Branchereau S, Davit-Spraul A, Lainas P, Groyer-Picard MT, Weber A, et al. Improvement of hepatocyte transplantation efficiency in the mdr2−/− mouse model by glyceryl trinitrate. Transplantation. 2015;99:36–40. doi: 10.1097/TP.0000000000000463. [DOI] [PubMed] [Google Scholar]
- 125.Marrone J, Lehmann GL, Soria LR, Pellegrino JM, Molinas S, Marinelli RA. Adenoviral transfer of human aquaporin-1 gene to rat liver improves bile flow in estrogen-induced cholestasis. Gene Ther. 2014;21:1058–1064. doi: 10.1038/gt.2014.78. [DOI] [PubMed] [Google Scholar]