Abstract
The hamstring autograft is one of the most popular grafts for anterior cruciate ligament (ACL) reconstruction. Although many techniques for arthroscopic ACL reconstruction using hamstring autografts have been invented, hamstring harvest techniques have not been focused. Hamstrings are harvested using an open technique that requires a 2- to 5-cm skin incision. In this Technical Note, we describe an endoscopic harvest technique of autogenous gracilis and semitendinosus tendon. This technique needs only a 1- to 1.5-cm skin incision and provides surgeons a sufficient view to safely harvest the hamstrings.
The hamstring autograft is one of the most popular grafts for anterior cruciate ligament (ACL) reconstruction because it is easily shaped according to surgeon preference. There are many kinds of ACL reconstruction procedures using hamstring autografts, including single bundle reconstruction,1, 2 bi-socket reconstruction,3 double-bundle reconstruction,4 and allograft augmentation of hamstring autografts.5 Moreover, combined ACL and anterolateral ligament reconstruction techniques using hamstring autografts were recently developed.6, 7, 8
Despite the invention of such techniques, the development of a hamstring harvest technique has not occurred and not much has changed over several decades. Hamstring harvests are performed using an open technique that requires a 2- to 5-cm skin incision.1, 4, 9 Here we evaluated an endoscopic technique for harvesting hamstring autografts. The present endoscopy technique not only results in a small skin incision length for hamstring harvest, it also provides surgeons a good view to safely dissect the fascial bands and accessory bands of the tendons and harvest the hamstrings. A summary of key steps is provided in Table 1, whereas a summary of the technique is provided in Video 1.
Table 1.
Key Steps for Endoscopic Harvest of Autogenous Gracilis and Semitendinosus Tendon
| Identify anatomic landmarks. |
| Tibial tubercle |
| Medial joint line |
| Gracilis tendon |
| Longitudinal skin incision: approximately 1 to 1.5 cm |
| 3 cm medial to the tibial tubercle |
| On the proximal edge of the gracilis tendon |
| Bluntly dissect the subcutaneous tissue. |
| Transversely cut the sartorial fascia approximately 1 to 2 cm. |
| Lift the sartorial fascia using a small retractor. |
| Introduce a 30° 4-mm diameter arthroscope. |
| Identify and hook the gracilis and semitendinosus tendons using curved forceps. |
| Pull the tendons laterally to detach them from the tibial attachment. |
| Separate the gracilis and semitendinosus tendons. |
| Whipstitch the gracilis and semitendinosus tendons. |
| Pull the semitendinosus tendon and dissect the accessory tendinous band. |
| Insert arthroscope and dissect the dense fascia, adherent soft tissue, and accessory bands. |
| Harvest the semitendinosus tendon using the tendon stripper. |
| Pull the gracilis tendon and dissect the accessory tendinous band. |
| Insert arthroscope and dissect the dense fascia, adherent soft tissue, and accessory bands. |
| Harvest the gracilis tendon using the tendon stripper. |
| When the tendon stripper stops, reintroduce the arthroscope and reassess other fascial and accessory bands. |
| Prepare the graft. |
Technique
Patient Positioning
The present surgical technique is performed under general anesthesia with the patient in the supine position. A padded tourniquet is placed on the proximal thigh of the operative leg, which is positioned with a leg holder to keep the thigh horizontal; in the meantime, the contralateral leg is held by a well-leg holder with the hip flexed and abducted to provide a wide working space around the operative knee. The bed is lowered to allow the surgeon to harvest the graft while in a seated position. Alternatively, the leg can be kept on the operating table and placed into a figure four position. The operative knee is prepared and draped in a standard fashion. The necessary tools include a small retractor, forceps, curved pean, curved Kelly forceps, Metzenbaum scissors, mosquito curved pean, and a closed tendon stripper (Smith & Nephew Endoscopy, Andover, MA) (Fig 1). No special device is necessary.
Fig 1.

Tools. A, small retractor; B, forceps; C, curved pean; D, curved Kelly forceps; E, Metzenbaum scissors; F, curved mosquito forceps, G, closed tendon stripper.
Endoscopic Graft Harvest
Patella, patellar tendon, and tibial tubercle are marked to ensure accurate incision positioning. The pes anserinus is palpated and drawn along the proximal edge of the gracilis tendon and the distal edge of the semitendinosus tendon. The skin is incised with a No. 15 scalpel. An approximately 1-cm-long longitudinal incision is made on the proximal edge of the gracilis tendon approximately 3 cm medial to the tibial tubercle (Fig 2). The subcutaneous tissue is bluntly dissected to the level of the sartorial fascia with the gauze grasped by the curved mosquito forceps.
Fig 2.
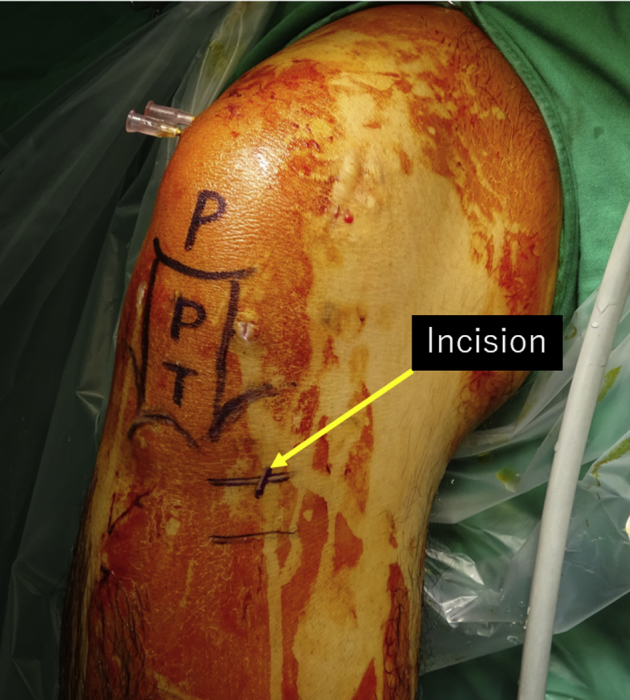
Intraoperative photograph (right knee) showing the location and size of the skin incision used for the endoscopic harvest of the gracilis and semitendinosus tendons. The patient is in the supine position. The operative leg is positioned with a leg holder to keep the thigh horizontal.
The bump of sartorial fascia due to the underlying gracilis and semitendinosus tendons can be palpated using forceps. The gracilis tendon is located proximal relative to the semitendinosus tendon. An approximately 1- to 2-cm-long transverse cut of the sartorial fascia is gradually made using Metzenbaum scissors in line with the proximal border of the gracilis tendon. The sartorial fascia is lifted together with the underlying hamstring using a small retractor introduced through the sartorial fascia incision.
A 30° 4-mm diameter arthroscope is then introduced into the space between the superficial medial collateral ligament and the hamstring tendons through the same sartorial incision. No joint irrigation liquid is used during the tendon harvest. The subcutaneous fat tissue around the skin incision is spread and cut using scissors to obtain a clear arthroscopy view. Hamstring tendons can be observed at the back side of the sartorial fascia (Fig 3). Using a curved pean or curved Kelly forceps, the gracilis and semitendinosus tendons are dissected free from the sartorial fascia and then hooked and pulled back together outside the skin incision. The tendons are laterally pulled to detach them from the tibial attachment. Because the skin incision is approximately 3 cm medial to the tibial tubercle, the ends of the detached tendons come out of the skin. If the tendons are retracted to inside the skin, the distal ends of the tendons are found arthroscopically and pulled back outside the skin using forceps.
Fig 3.
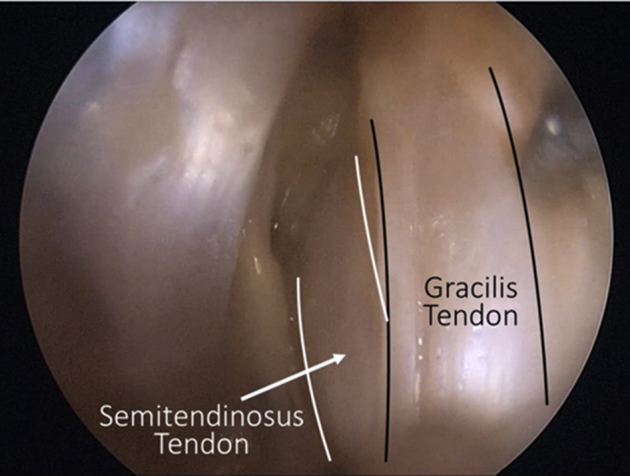
A 30° 4-mm diameter arthroscope is then introduced into the space between the superficial medial collateral ligament and the hamstring tendons through the incision. No joint irrigation liquid is used. The subcutaneous fat tissue is spread and cut using scissors to obtain a clear arthroscopy view. Hamstring tendons are visible at the back side of the sartorial fascia. Using a curved pean or a curved Kelly forceps, the gracilis and semitendinosus tendons are dissected free from the sartorial fascia. This figure shows anteromedial side of the right knee in the flexed position. Superficial medial collateral ligament is seen on the left side. Proximal of the knee is on the upper side.
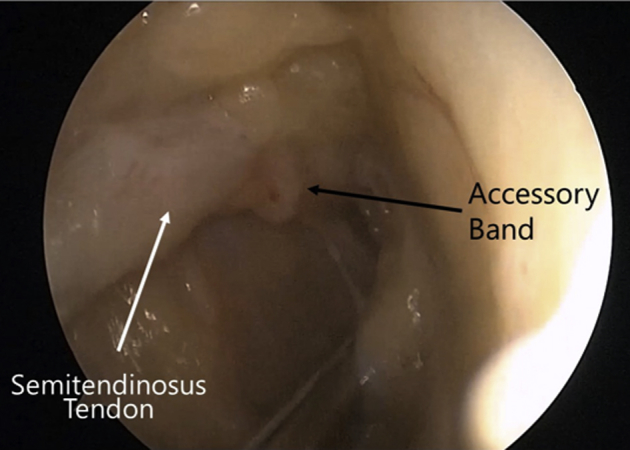
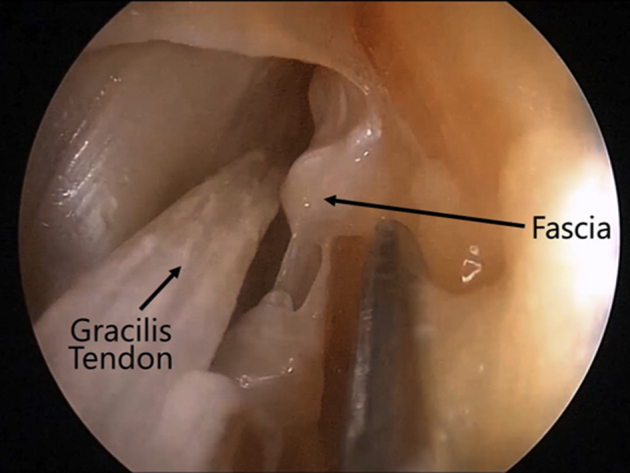
The gracilis and semitendinosus tendons are carefully separated by cutting the intertendinous bands with the scissors. Each end of the tendon is whipstitched with a No. 2 nonabsorbable suture (Ethicon, Somerville, NJ). The semitendinosus tendon is pulled by the suture, after which point the first accessory tendinous band or fascial band of the semitendinosus tendon can be usually seen outside the skin and cut using scissors (Fig 4). Then, by looking with the arthroscope through the same skin incision, the dense fascia ensheathing the tendon that adheres to the soft tissue and other accessory bands that may impede tendon stripping is gently dissected using Metzenbaum scissors (Fig 5). After confirmation that both tendons can move smoothly, the tendons are harvested using a closed tendon stripper. Stable traction on the end of the tendon and stable pushing of the tendon stripper are important to smooth tendon release. Although our group usually harvests the semitendinosus tendon first, the gracilis tendon can be harvested first as well. When the tendon stripper stops, other dense fascia, fascial bands, and accessory bands should be reassessed and dissected arthroscopically (Fig 6). Surgeons can then reattempt to harvest the tendon (Fig 7).
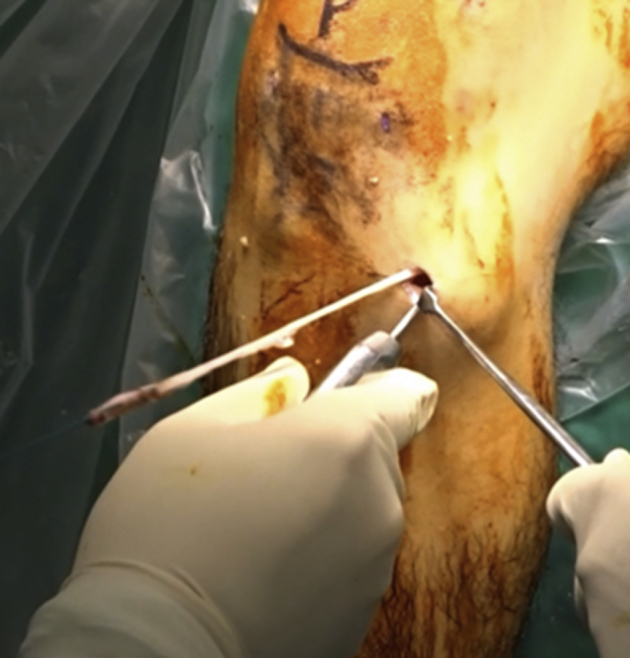
Fig 4.

The gracilis and semitendinosus tendons are hooked and pulled back together outside the skin incision. The tendons are laterally pulled to detach them from the tibial attachment. The gracilis and semitendinosus tendons are carefully separated by cutting the intertendinous bands with the scissors. Each end of the tendon is whipstitched with a No. 2 nonabsorbable suture (Ethicon). The semitendinosus tendon is pulled by the suture, after which point the first accessory tendinous band of the semitendinosus tendon is visible outside the skin and cut using scissors. This figure shows anteromedial side of the right knee in flexed position.
Fig 5.
The dense fascia ensheathing the tendon that adheres to the soft tissue and other accessory bands that may impede tendon stripping are arthroscopically dissected using Metzenbaum scissors. This figure shows anteromedial side of the right knee in the flexed position. Proximal of the knee is on the right upper side.
Fig 6.
After confirmation that both tendons can move smoothly, the tendons are harvested using a closed tendon stripper (Smith & Nephew Endoscopy). When the tendon stripper stops, other dense fascia, fascial bands, and accessory bands should be reassessed and dissected arthroscopically. This figure shows anteromedial side of the right knee in the flexed position. Proximal of the knee is on the right upper side.
Fig 7.
The gracilis tendon is harvested using the closed tendon stripper. This figure shows anteromedial side of the right knee in the flexed position.
The harvested hamstring graft can be prepared for the ACL reconstruction based on the surgeon's preference. We create the tibial tunnel from the same skin incision and perform single-bundle ACL reconstruction with a 4-stranded tendon graft. We then preserve the remnant whenever possible and affix the graft using absorbable interference screws (30-mm-long BIOSURE HA screw; Smith & Nephew Endoscopy) at the femoral and tibial tunnels.
Wound Closure
The wound is closed using conventional skin sutures. The final wound for the hamstring harvest is approximately 1 to 1.5 cm long (Fig 8).
Fig 8.

The right knee is extended on the table. The wound is closed using conventional skin sutures. The final wound for the hamstring harvest measures approximately 1 to 1.5 cm. Proximal of the knee is on the right side of the picture.
Discussion
In this Technical Note, we described endoscopic autogenous hamstring harvest for ACL reconstruction using the gracilis and semitendinosus tendons. Because the hamstring autograft has a reduced incidence of patellofemoral crepitance, kneeling pain, and extension loss,10, 11 it is among the most common grafts for ACL reconstruction. The hamstrings can also be used in other ligament reconstruction procedures, including the elbow12 and the ankle13, 14, 15 ligaments.
Recent evidence indicates that larger hamstring graft diameters are associated with increased tensile strength and a reduced risk of graft failure,16, 17 and secure harvest of the hamstrings is a critical issue. A clear understanding of the anatomy of the hamstring tendons and saphenous nerve course is obviously necessary.
The gracilis and semitendinosus tendons contact each other via the intertendinous bands at an average of 3.18 to 3.6 cm from the tibial crest18, 19 and become distinct at a more medial point.20 Introducing the arthroscope 3 cm medial to the tibial crest is a reasonable approach to easily identifying the 2 tendons. Too medial an incision will make it difficult to create the appropriate tibial tunnel for the transtibial femoral tunnel creation of the ACL reconstruction and make it dangerous to destroy the medial tibial plateau due to the shallow angle of the tibial drilling course.
Saphenous nerve injury may cause hypoesthesia, dysesthesia, painful neuroma and reflex sympathetic dystrophy, anterior knee pain, and kneeling pain.21 The saphenous nerve exits from the adductor canal and divides almost immediately into its sartorial and infrapatellar branches.22 The sartorial terminal branch travels vertically toward the medial knee behind the sartorius. It pierces the fascia between the sartorius and gracilis tendons and travels distally. The infrapatellar branch of the saphenous nerve (IPBSN) travels to the anterior side of the knee.23, 24 Sanders et al.24 reported sartorial terminal branch isolated injuries at a rate of 23%. Iatrogenic damage to the sartorial terminal branch is thought to be related to the passage of the stripper during the gracilis tendon harvest. Assessment of the proximal part with the arthroscope might reduce its incidence. The IPBSN has been more frequently injured, ranging from 12% to 88%.21, 25, 26 This evidence indicates that it is very difficult to completely avoid IPBSN injury. Therefore, the smaller skin incision is a good alternative to reduce the incidence and area of IPBSN injuries.
Tuncay et al.27 reported a high incidence of the fascial band between the semitendinosus and gastrocnemius. The mean distance from the insertion of the semitendinosus to the fascial band was 7 cm. Candal-Couto and Deehan19 found that accessory bands have high variability and were seen between tendons, connecting to the popliteal fascia, sartorius, gastrocnemius, and pretibial and superficial fascia. Moreover, accessory bands usually originated more than 10 cm proximal to the insertion site of the semitendinosus and gracilis tendon. Because the arthroscope is thinner and longer than fingers, it is easy to insert it more proximally and identify those accessory bands.
This report has several limitations. First, the present skin incision is so small that it is not suitable for double-bundle ACL reconstruction.4 Second, this procedure is technically demanding. However, surgeons can expand the incision and convert to conventional open procedure anytime when difficulty is encountered. Third, although this technique theoretically has possible advantages that reduce nerve injury, premature hamstring amputation, postoperative scar tissue, anterior knee pain, and the incidence of skin infections, no evidence has so far been reported from a comparative study; thus, future studies are necessary to prove our hypothesis. A summary of pearls and pitfalls is provided in Table 2.
Table 2.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| A longitudinal skin incision is made approximately 3 cm to the tibial tubercle to avoid the intertendinous bands and enable the easy identification of the gracilis and semitendinosus tendons. | The skin incision is so small that it may be very difficult to create 2 tibial tunnels for double-bundle anterior cruciate ligament reconstruction. |
| The use of a small skin incision and blunt dissection of the subcutaneous soft tissue prevent damage to small nerves. | This technique is relatively difficult and has a steep learning curve. However, surgeons can expand the skin incision and convert to a conventional open harvest procedure when necessary. |
| No joint irrigation liquid is used during the tendon harvest. | |
| A clear understanding of the anatomy of the hamstring tendons and course of the saphenous nerve is necessary to ensuring a safe hamstring harvest. | |
| The arthroscope can be inserted deeply to allow the surgeon to identify the more proximal fascial and accessory bands. | |
| When the tendon stripper stops, the surgeon should use it to reassess other fascial and accessory bands. |
This endoscopic harvest technique of the autogenous gracilis and semitendinosus tendons provides surgeons a smaller incision, higher safety, and greater reproducibility.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Surgical technique for endoscopic harvest of autogenous gracilis and semitendinosus tendons of the right knee, including remnant preserved single-bundle anterior cruciate ligament (ACL) reconstruction. This technique is performed under general anesthesia with the patient in the supine position. A padded tourniquet is placed on the proximal thigh of the operative leg, which is positioned with a leg holder to keep the thigh horizontal; in the meantime, the contralateral leg is held by a well-leg holder with the hip flexed and abducted to provide a wide working space around the operative knee. The bed is lowered to allow the surgeon to harvest the graft while in a seated position. Alternatively, the leg can be kept on the operating table and placed into a figure 4 position. The operative knee is prepared and draped in a standard fashion. The necessary tools include a small retractor, forceps, curved pean, curved Kelly forceps, Metzenbaum scissors, mosquito curved pean, and a closed tendon stripper (Smith & Nephew Endoscopy). Patella, patellar tendon, and tibial tubercle are drawn. The pes anserinus is palpated and marked along the proximal edge of the gracilis tendon and the distal edge of the semitendinosus tendon. A 1-cm-long incision is made on the proximal edge of the gracilis tendon. The subcutaneous tissue is bluntly dissected. A transverse cut of the sartorial fascia is made in line with the proximal border of the gracilis tendon. The sartorial fascia is lifted. A 30° 4-mm diameter arthroscope is then introduced into the space between the superficial medial collateral ligament and the hamstring. The subcutaneous fat tissue is spread. Hamstring tendons can be observed at the back side of the sartorial fascia. Adherent soft tissue is gently dissected to obtain a clear view of the hamstring tendons. Using a curved pean, the gracilis and semitendinosus tendons are dissected free from the sartorial fascia and then hooked and pulled back together outside the skin. The tendons are pulled to detach them from the tibial attachment. The gracilis and semitendinosus tendons are separated. Each end of the tendon is whipstitched with a No. 2 nonabsorbable suture (Ethicon). The semitendinosus tendon is pulled by the suture, after which point the first accessory tendinous band of the semitendinosus tendon can be usually seen outside the skin and cut using scissors. The dense fascia ensheathing the tendon that adheres to the soft tissue is gently dissected using Metzenbaum scissors. The accessory band is also carefully dissected. After confirmation that both tendons can move smoothly, the tendons are harvested using a closed tendon stripper. If the tendon stripper stops, another dense fascia should be reassessed and dissected. Surgeons then retry to harvest the tendon. The harvested hamstring graft can be prepared for the ACL reconstruction based on the surgeon’s preference. We create the single tibial tunnel from the same small skin incision. We then preserve the remnant whenever possible and create the femoral tunnel via the trans-tibial technique. We perform single-bundle ACL reconstruction with a 4-stranded tendon graft and fix the graft using absorbable interference screws (30-mm-long BIOSURE HA screw; Smith & Nephew Endoscopy) at the femoral and tibial tunnels. The final wound for the hamstring harvest is approximately 1 to 1.5 cm long.
References
- 1.Maeda A., Shino K., Horibe S., Nakata K., Buccafusca G. Anterior cruciate ligament reconstruction with multistranded autogenous semitendinosus tendon. Am J Sports Med. 1996;24:504–509. doi: 10.1177/036354659602400416. [DOI] [PubMed] [Google Scholar]
- 2.Sonnery-Cottet B., Freychet B., Murphy C.G., Pupim B.H., Thaunat M. Anterior cruciate ligament reconstruction and preservation: The single-anteromedial bundle biological augmentation (SAMBBA) technique. Arthrosc Tech. 2014;3:e689–e693. doi: 10.1016/j.eats.2014.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hamada M., Shino K., Horibe S. Single- versus bi-socket anterior cruciate ligament reconstruction using autogenous multiple-stranded hamstring tendons with endoButton femoral fixation: A prospective study. Arthroscopy. 2001;17:801–807. doi: 10.1016/s0749-8063(01)90002-7. [DOI] [PubMed] [Google Scholar]
- 4.Yasuda K., Kondo E., Ichiyama H. Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Arthroscopy. 2004;20:1015–1025. doi: 10.1016/j.arthro.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 5.Jacobs C.A., Burnham J.M., Makhni E., Malempati C.S., Swart E., Johnson D.L. Allograft augmentation of hamstring autograft for younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45:892–899. doi: 10.1177/0363546516676079. [DOI] [PubMed] [Google Scholar]
- 6.Sonnery-Cottet B., Thaunat M., Freychet B., Pupim B.H., Murphy C.G., Claes S. Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-year follow-up. Am J Sports Med. 2015;43:1598–1605. doi: 10.1177/0363546515571571. [DOI] [PubMed] [Google Scholar]
- 7.Helito C.P., Bonadio M.B., Gobbi R.G. Combined intra- and extra-articular reconstruction of the anterior cruciate ligament: The reconstruction of the knee anterolateral ligament. Arthrosc Tech. 2015;4:e239–e244. doi: 10.1016/j.eats.2015.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thaunat M., Clowez G., Saithna A. Reoperation rates after combined anterior cruciate ligament and anterolateral ligament reconstruction: A series of 548 patients from the SANTI study group with a minimum follow-up of 2 years. Am J Sports Med. 2017;45:2569–2577. doi: 10.1177/0363546517708982. [DOI] [PubMed] [Google Scholar]
- 9.Frank R.M., Hamamoto J.T., Bernardoni E. ACL reconstruction basics: Quadruple (4-strand) hamstring autograft harvest. Arthrosc Tech. 2017;6:e1309–e1313. doi: 10.1016/j.eats.2017.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chee M.Y., Chen Y., Pearce C.J. Outcome of patellar tendon versus 4-strand hamstring tendon autografts for anterior cruciate ligament reconstruction: A systematic review and meta-analysis of prospective randomized trials. Arthroscopy. 2017;33:450–463. doi: 10.1016/j.arthro.2016.09.020. [DOI] [PubMed] [Google Scholar]
- 11.Maletis G.B., Cameron S.L., Tengan J.J., Burchette R.J. A prospective randomized study of anterior cruciate ligament reconstruction: A comparison of patellar tendon and quadruple-strand semitendinosus/gracilis tendons fixed with bioabsorbable interference screws. Am J Sports Med. 2007;35:384–394. doi: 10.1177/0363546506294361. [DOI] [PubMed] [Google Scholar]
- 12.Hagemeijer N.C., Claessen F., de Haan R., Riedijk R., Eygendaal D.E., van den Bekerom M.P. Graft site morbidity in elbow ligament reconstruction procedures: A systematic review. Am J Sports Med. 2017;45:3382–3387. doi: 10.1177/0363546517693836. [DOI] [PubMed] [Google Scholar]
- 13.Paterson R., Cohen B., Taylor D., Bourne A., Black J. Reconstruction of the lateral ligaments of the ankle using semi-tendinosis graft. Foot Ankle Int. 2000;21:413–419. doi: 10.1177/107110070002100510. [DOI] [PubMed] [Google Scholar]
- 14.Coughlin M.J., Matt V., Schenck R.C., Jr. Augmented lateral ankle reconstruction using a free gracilis graft. Orthopedics. 2002;25:31–35. doi: 10.3928/0147-7447-20020101-13. [DOI] [PubMed] [Google Scholar]
- 15.Guillo S., Archbold P., Perera A., Bauer T., Sonnery-Cottet B. Arthroscopic anatomic reconstruction of the lateral ligaments of the ankle with gracilis autograft. Arthrosc Tech. 2014;3:e593–598. doi: 10.1016/j.eats.2014.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Conte E.J., Hyatt A.E., Gatt C.J., Jr., Dhawan A. Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy. 2014;30:882–890. doi: 10.1016/j.arthro.2014.03.028. [DOI] [PubMed] [Google Scholar]
- 17.Spragg L., Chen J., Mirzayan R., Love R., Maletis G. The effect of autologous hamstring graft diameter on the likelihood for revision of anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44:1475–1481. doi: 10.1177/0363546516634011. [DOI] [PubMed] [Google Scholar]
- 18.Ivey M., Prud'homme J. Anatomic variations of the pes anserinus: A cadaver study. Orthopedics. 1993;16:601–606. doi: 10.3928/0147-7447-19930501-14. [DOI] [PubMed] [Google Scholar]
- 19.Candal-Couto J.J., Deehan D.J. The accessory bands of gracilis and semitendinosus: An anatomical study. Knee. 2003;10:325–328. doi: 10.1016/s0968-0160(02)00154-0. [DOI] [PubMed] [Google Scholar]
- 20.Pagnani M.J., Warner J.J., O'Brien S.J., Warren R.F. Anatomic considerations in harvesting the semitendinosus and gracilis tendons and a technique of harvest. Am J Sports Med. 1993;21:565–571. doi: 10.1177/036354659302100414. [DOI] [PubMed] [Google Scholar]
- 21.Ruffilli A., De Fine M., Traina F., Pilla F., Fenga D., Faldini C. Saphenous nerve injury during hamstring tendons harvest: Does the incision matter? A systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25:3140–3145. doi: 10.1007/s00167-016-4217-8. [DOI] [PubMed] [Google Scholar]
- 22.Arthornthurasook A., Gaew-Im K. The sartorial nerve: Its relationship to the medial aspect of the knee. Am J Sports Med. 1990;18:41–42. doi: 10.1177/036354659001800107. [DOI] [PubMed] [Google Scholar]
- 23.Hunter L.Y., Louis D.S., Ricciardi J.R., O'Connor G.A. The saphenous nerve: Its course and importance in medial arthrotomy. Am J Sports Med. 1979;7:227–230. doi: 10.1177/036354657900700403. [DOI] [PubMed] [Google Scholar]
- 24.Sanders B., Rolf R., McClelland W., Xerogeanes J. Prevalence of saphenous nerve injury after autogenous hamstring harvest: An anatomic and clinical study of sartorial branch injury. Arthroscopy. 2007;23:956–963. doi: 10.1016/j.arthro.2007.03.099. [DOI] [PubMed] [Google Scholar]
- 25.Jameson S., Emmerson K. Altered sensation over the lower leg following hamstring graft anterior cruciate ligament reconstruction with transverse femoral fixation. Knee. 2007;14:314–320. doi: 10.1016/j.knee.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 26.Kjaergaard J., Fauno L.Z., Fauno P. Sensibility loss after ACL reconstruction with hamstring graft. Inter J Sports Med. 2008;29:507–511. doi: 10.1055/s-2008-1038338. [DOI] [PubMed] [Google Scholar]
- 27.Tuncay I., Kucuker H., Uzun I., Karalezli N. The fascial band from semitendinosus to gastrocnemius: The critical point of hamstring harvesting: An anatomical study of 23 cadavers. Acta Orthop. 2007;78:361–363. doi: 10.1080/17453670710013933. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique for endoscopic harvest of autogenous gracilis and semitendinosus tendons of the right knee, including remnant preserved single-bundle anterior cruciate ligament (ACL) reconstruction. This technique is performed under general anesthesia with the patient in the supine position. A padded tourniquet is placed on the proximal thigh of the operative leg, which is positioned with a leg holder to keep the thigh horizontal; in the meantime, the contralateral leg is held by a well-leg holder with the hip flexed and abducted to provide a wide working space around the operative knee. The bed is lowered to allow the surgeon to harvest the graft while in a seated position. Alternatively, the leg can be kept on the operating table and placed into a figure 4 position. The operative knee is prepared and draped in a standard fashion. The necessary tools include a small retractor, forceps, curved pean, curved Kelly forceps, Metzenbaum scissors, mosquito curved pean, and a closed tendon stripper (Smith & Nephew Endoscopy). Patella, patellar tendon, and tibial tubercle are drawn. The pes anserinus is palpated and marked along the proximal edge of the gracilis tendon and the distal edge of the semitendinosus tendon. A 1-cm-long incision is made on the proximal edge of the gracilis tendon. The subcutaneous tissue is bluntly dissected. A transverse cut of the sartorial fascia is made in line with the proximal border of the gracilis tendon. The sartorial fascia is lifted. A 30° 4-mm diameter arthroscope is then introduced into the space between the superficial medial collateral ligament and the hamstring. The subcutaneous fat tissue is spread. Hamstring tendons can be observed at the back side of the sartorial fascia. Adherent soft tissue is gently dissected to obtain a clear view of the hamstring tendons. Using a curved pean, the gracilis and semitendinosus tendons are dissected free from the sartorial fascia and then hooked and pulled back together outside the skin. The tendons are pulled to detach them from the tibial attachment. The gracilis and semitendinosus tendons are separated. Each end of the tendon is whipstitched with a No. 2 nonabsorbable suture (Ethicon). The semitendinosus tendon is pulled by the suture, after which point the first accessory tendinous band of the semitendinosus tendon can be usually seen outside the skin and cut using scissors. The dense fascia ensheathing the tendon that adheres to the soft tissue is gently dissected using Metzenbaum scissors. The accessory band is also carefully dissected. After confirmation that both tendons can move smoothly, the tendons are harvested using a closed tendon stripper. If the tendon stripper stops, another dense fascia should be reassessed and dissected. Surgeons then retry to harvest the tendon. The harvested hamstring graft can be prepared for the ACL reconstruction based on the surgeon’s preference. We create the single tibial tunnel from the same small skin incision. We then preserve the remnant whenever possible and create the femoral tunnel via the trans-tibial technique. We perform single-bundle ACL reconstruction with a 4-stranded tendon graft and fix the graft using absorbable interference screws (30-mm-long BIOSURE HA screw; Smith & Nephew Endoscopy) at the femoral and tibial tunnels. The final wound for the hamstring harvest is approximately 1 to 1.5 cm long.


