Abstract
Purpose
We examined how total volume of physical activity and reallocation of time spent at various objectively measured intensities of physical activity (PA) were associated with overall and abdominal fat distribution in a population-based study of adult Inuit in Greenland.
Methods
Data were collected as part of a countrywide cross-sectional health survey in Greenland. A combined accelerometer and heart rate monitor (ACC + HR) measured total physical activity energy expenditure (PAEE) and intensities of PA (N=1536). Visceral- and subcutaneous adipose tissue (VAT, SAT) was assessed by ultrasonography. Isotemporal substitution modeling was used to analyse the association between substitution of 1-hour of sedentary time to light or moderate intensity PA and 1-hour light intensity PA to moderate or vigorous intensity PA in relation to BMI, waist circumference (WC), SAT and VAT.
Results
A negative linear association was found for total PAEE and BMI, WC, VAT and SAT. Exchanging 1-hour of sedentary time with light intensity PA was associated with lower WC (-0.6 cm., p=0.01), SAT (-0.08 cm., p<0.001) and VAT (-0.04 cm., p=0.359). Exchanging light intensity PA with vigorous intensity PA resulted in -6.1 cm. lower WC (p<0.001), -0.7 cm. lower VAT (p=0.018) and -0.7 cm. lower SAT (p<0.001). When further adjusting for BMI the associations were attenuated; however, most of them remained significant, and the directions were mostly unchanged. Both 1,5, and 10 minutes bouts of MVPA were negatively associated with overall and abdominal fat distribution.
Conclusion
Increasing total physical activity energy expenditure is associated with lower BMI, WC and abdominal fat accumulation among Inuit in Greenland. The importance of promoting an upward shift of the whole PA intensity distribution and to spur even short bouts of MVPA to limit excessive accumulation of SAT and VAT is highlighted and can be used in the prevention of type 2 diabetes.
Keywords: isotemporal substitution, physical activity intensity, abdominal fat, physical activity bouts
Introduction
Inuit populations throughout the Arctic are facing a high and growing prevalence of overall and abdominal obesity (1;3). Accumulation of visceral fat is a serious public health problem due to its association with metabolic disturbances such as type 2 diabetes (35). Worldwide, growing evidence supports a negative association between total PA and abdominal fat, particularly visceral fat, independent of overall obesity (10;11;36). Some studies have shown that higher intensity PA reduces abdominal fat accumulation more effectively than low intensity PA (7;16;22;34). In Greenland total energy expenditure from physical activity has recently been found to be associated with the early development of type 2 diabetes in Greenland. Abdominal obesity was suggested as a potential mediator of this association (7).
Ethnic differences in abdominal fat distribution are well-known (18). A study among Inuit in Greenland showed a relatively greater amount of subcutaneous fat than visceral fat compared with western populations. Subcutaneous fat is suggested to contribute relatively more to waist circumference levels in Greenland and is suggested as a potential explanation for a lower metabolic risk for a given level of obesity compared with western populations (17).
A limited number of studies have examined how reallocating time spent on different intensities of PA and sedentary behavior is associated with abdominal fat distribution and studies differentiate widely in study sample and measurement methods. In addition most population-based studies are based on self-reported PA and proxy measures for abdominal fat distribution such as waist circumference, which do not allow differentiation between visceral and subcutaneous fat distribution (13;20;26;31;34;37).
The overall aim of this study was first, to examine how objectively measured PA energy expenditure was related to BMI, waist circumference, visceral fat (VAT) and subcutaneous abdominal adipose tissue (SAT).
Secondly, to examine how reallocating time spent at various intensities and bout patterns of PA was associated with abdominal fat distribution in a population-based study of adult Inuit in Greenland.
Methods
Study population
Data are from the Inuit Health in Transition study from 2005–2010 (2). In brief, data were collected as part of a countrywide cross-sectional health survey in Greenland. The total population of Greenland is 57,000 of whom 90% are ethnic Greenlanders (Inuit). Genetically, Greenlanders are Inuit with a mixture of European, mainly Danish genes (21). They are genetically and culturally related to the Inuit in Canada and Alaska and the Yupiit of Alaska and Siberia. Greenland’s 80 communities are all located on the coast and are divided into towns (between 469 and 15,469 inhabitants) and villages (up to about 550 inhabitants). Participants were selected as a stratified random sample. Greenland was divided into strata based on geography (South-West coast, Central-West coast, North-West coast, East Greenland, North Greenland) and community size (towns with ≥2000 inhabitants; towns with <2000 inhabitants; and villages). From each of these strata one or more towns and at least two villages were selected for the study as representative of the stratum with regard to living conditions. A random sample was drawn from the population register to obtain around 300 participants from each town. Villages were chosen at random in the strata and all adults in selected villages were invited to participate. Information on adults aged 18 years and older, born in Greenland or Denmark, in 9 towns and 13 villages. Ethnicity as Greenlander or Dane was determined at enrolment based on the primary language of the participant and self-identification. The current study focuses on Greenlanders only. The study was approved by the ethical review committee for Greenland. Written informed consent was obtained from all participants. A detailed description of the methods is available elsewhere (2).
Procedures of health examination
Data were collected by questionnaires and a clinical examination. Information on lifestyle was collected by interview.
Anthropometric measurements
Height was measured without shoes to the nearest millimetre and weight was measured to the nearest 0.1 kg with the participants wearing light indoor clothing. BMI was calculated as weight/height2. The waist Circumference of the standing participant was measured midway between the iliac crest and the costal margin. A Pie Medical ultrasound system with a 3C-RS curved transducer was applied to determine visceral and subcutaneous fat according to a validated protocol (25;33). Visceral fat was defined as the distance in centimeters from the peritoneum to the lumbar spine, and subcutaneous abdominal fat was defined as the distance in centimeters from the skin to the linea alba. Both measurements were obtained from where the xiphoid line and the WC met. A minimal pressure was applied to ensure no displacement of the abdominal cavity, and measurements were made at the end of expiration. Coefficients of variation for intra- and and interobserver variation were in the range 1.9-5.6%
Combined accelerometry and heart rate monitoring
A combined accelerometer and heart rate monitor (ACC + HR) (Actiheart, CamNtech Ltd, Papworth, UK) (4), was provided to a subgroup of the participants (n = 2055) and attached to the participant’s chest by two standard ECG electrodes (MXC55 MediMax, UK). Acceleration and heart rate was measured in 30-s intervals. The participants were asked to wear the monitor 24 h a day for up to 5 days. However, not all was able to wear it for this period of time and not all participants were given a monitor due to study logistics such as limited time available at each study location and a limited stock of monitors. The first 135 study participants also performed an individual calibration test (8-min step test) used to define a population-specific calibration equation of the heart rate–activity energy expenditure relationship. Baseline characteristics were not different between the subgroup and the total study population. Heart rate was pre-processed using Gaussian Process regression (32). Caloric intensity of PA was estimated by combining the acceleration-based estimate of intensity (6) with the heart rate-based estimate from the population- specific equation in a branched equation modelling framework (5). Resulting time-series of activity intensity (in J/min/kg) were summarized into total physical activity energy expenditure (PAEE) in kJ/kg/day and time spent at different intensity levels, whilst minimizing diurnal bias from potentially unbalanced data accumulated over hours of the day. The intensity levels were defined as sedentary activity (SED): 1 – 1.5METs (hours/day), light intensity PA (LPA): 1.5 – 3 METs (hours/day), moderate intensity PA (MPA): 3 METs – 6 METs (hours/day) and vigorous PA (VPA): >6 METs (hours /day), using a standard definition of 1MET. Minutes spent on 1, 5 and 10 minutes bouts of moderate to vigorous intensity PA (MVPA), corresponding to an intensity level of above 3METs, was calculated by the estimated fraction of time spent on different bouts of MVPA.
Data on PA were obtained from 2055 participants (n=2045 Inuit) as a part of the Inuit Health in Transition study 2005-10 in Greenland. After excluding recordings with invalid PA data e.g. incomplete data on either heart rate or accelerometry, data from 1497 participants with complete data from ACC + HR monitoring for 48 hours or more were available for analysis.
Statistical methods
Descriptive characteristics of the study sample are presented as means with range or medians with inter-quartile range due to skewed distributed variables.
The association between PAEE and overall and abdominal fat distribution was examined by multivariable linear regression models. Model 1 was adjusted for sex, age, smoking and fraction of weekend wear time. Model 2 was further adjusted for BMI. A test for non-linearity was applied by adding a squared term for PAEE and left out if non-significant. The beta coefficients from the multivariate analysis of PAEE should be interpreted as the difference in the outcome measure for every 10kJ/kg/day difference in PAEE.
To examine the theoretical effect of reallocating time spent in one intensity category with the same amount of time spent in another intensity category and the association with overall adiposity (BMI) and abdominal fat distribution, we used isotemporal substitution analyses in a linear regression model constrained to total observed physical activity.
Coefficients for the isotemporal substitution models represent the estimated effects of substituting one PA intensity category for the intensity of the single excluded intensity category while holding total physical activity time constant leaving out sleep time. We examined the replacement of 1-hour of sedentary time with 1-hour of light intensity PA and moderate intensity, 1-hour of light intensity PA with moderate and vigorous intensity PA. Replacement of sedentary time with vigorous activity was not considered realistic from a public health perspective. We examined the significance of the cross-product between sex, menopausal status and PA measures in the analyses to test for sex interactions. While no interaction was observed, analyses were performed for the total study population. Moreover obesity measures were standardized to a mean of 0 and SD of 1 to facilitate comparisons.
The associations of 1, 5 and 10 minutes bouts of MVPA with overall obesity and abdominal fat distribution was investigated by linear regression analyses adjusting for sex, age, smoking and fraction of weekend wear time.
Sensitivity analyses were performed including only participants with ACC+HR monitoring of ≥72 hrs. Gaussian Process regression of heart rate was performed in JAVA using a MySQL database, and all other analyses were carried out in STATA version 14.
Results
Participant characteristics are presented in table I. Mean age was 43.9 (range 18-84) years and 43.6% were men. Women had higher levels of BMI, WC and subcutaneous fat than men, but lower median visceral fat: 6.5cm (IQR 5.2-8.3) vs 5.4cm (IQR 4.3-7.0) for men vs. women. Median PAEE was 56.4(IQR 23.6-96.7) kJ/kg/day for men and 45.7 (IQR 34.2-60.7) kJ/kg/day for women. Median time spent in light intensity PA made up the greatest part of total daily PA time: 6.9 (IQR 5.2-8.2) hours/day for men and 6.5 (IQR 5.1-8.0) hours/day for women. Total daily time spent on vigorous intensity PA was: 6.1 (0.9-18.6) minutes and 3.0 (0.3-9.9) minutes per day for men and women (median (IQR).
Table I.
Characteristics of the study population, Greenland health survey 2005-2010, n=1497.
| Men (n=652) |
Women (n=845) |
|
|---|---|---|
| Age (years) | 44.9 (18-84) | 43.1 (18-83) |
| Physical Activity Energy Expenditure (KJ/kg/day) | 55.8 (40.2-74.8) | 45.5 (33.6-60.4) |
| Anthropometric measures | ||
| BMI (kg/m2) | 24.8 (22.3-28.6) | 25.8 (22.5-29.9) |
| Waist circumference (cm) | 91.0 (82.5-101.5) | 90.0 (80.5-100.4) |
| Fat percentage (%) | 21.0 (15.6-27.6) | 34.0 (27.1-40.1) |
| Visceral fat (cm) | 6.5 (5.2-8.3) | 5.4 (4.3-7.0) |
| Subcutaneous fat (cm) | 2.1 (1.3-3.0) | 3.7 (2.5-4.7) |
| Physical activity subcomponents (daily) | ||
| Light PA (hours) | 6.9 (5.2-8.2) | 6.5 (5.1-8.0) |
| Moderate PA (hours) | 1.4 (0.8-2.2) | 0.9 (0.5-1.5) |
| Vigorous PA (hours) | 0.1 (0.01-0.3) | 0.03 (0.0-0.1) |
| Sedentary time (hours) | 4.9 (3.6 - 6.5) | 6.1 (4.5-7.6) |
| Minutes spent on at least 1 minutes bouts of MVPA | 86.0 (48.9-142.0) | 53.7 (29.7-91.6) |
| Minutes spent on at least 5 minutes bouts of MVPA | 54.1 (27.8-104.0) | 31.6 (14.7-61.9) |
| Minutes spent on at least 10 minutes bouts of MVPA | 30.6 (11.1-65.6) | 13.0 (3.2 -34.5) |
| Wear time (hours)* | 75.3±17.7 | 75.2±18.0 |
Values are range (age) or median (IQR). Greenland Health Survey 2005-10.
estimated from participants with a wear time of 48 hours or more.
MVPA≈ moderate and vigorous intensity PA >3METs
Multivariable analyses of total PAEE and BMI, WC, subcutaneous fat and visceral fat showed statistically significant negative associations with lower levels of overall and abdominal fat with higher PAEE (table II). The directions of the associations were mostly unchanged when further adjusting for BMI although not statistically significant for all outcome measures. Adding a quadratic term did not provide evidence against the linearity between PAEE and abdominal fat.
Table II.
Regression coefficients (95% confidence intervals) for waist circumference (WC), visceral fat (VAT) and sub-cutaneous fat (SAT) according to energy expenditure from total physical activity (PAEE). Greenland health survey 2005-2010, n=1489.
| BMI (kg/m2)≠ β |
P-value | Waist Circumference (cm)≠ β |
P-value | Visceral fat (cm)≠ β |
P-value | Sub-cutaneous fat (cm)≠ β |
P-value | |
|---|---|---|---|---|---|---|---|---|
| PAEE | ||||||||
| Multivariablea | -0.28 (-0.40 to -0.02) | <0.001 | -0.88 (-1.19 to -0.57) | <0.001 | -0.12 (-0.17 to -0.06) | <0.001 | -0.08 (-0.11 to -0.05) | <0.001 |
| Multivariableb | -0.19 (-0.3 to -0.08) | 0.001 | -0.03 (-0.08 to 0.007) | 0.106 | -0.02 (-0.04 to 0.001) | 0.063 | ||
Analyses adjusted for sex, age, smoking and fraction of weekend wear time
Analyses further adjusted for BMI
Per 10 kJ/kg/day
Results from the isotemporal analyses showed that replacing 1-hour of sedentary time with light or moderate intensity PA was associated with lower BMI, WC, VAT and SAT, although associations were no longer statistically significant after adjusting for BMI (table III). The same pattern was found for reallocating light intensity PA with moderate intensity PA. Replacing 1-hour of light intensity PA with vigorous intensity PA was found to be most strongly associated with lower abdominal fat with -6.1 cm (CI:-9.20, -2.30) lower WC corresponding to a 6.4% reduction, -0.7 cm. lower visceral fat (CI:-1.21, -0.11) corresponding to af 7.8% reduction and -0.7 cm. lower sub-cutaneous fat (-1.01, -0.34) corresponding to a 35.7% reduction. When further adjusting for BMI the directions of the associations were unchanged; however, no longer statistically significant for visceral fat.
Table III.
Results from isotemporal substitution analyses. Coefficients represent change in outcome (BMI and abdominal fat distribution) by replacing 1-hour of sedentary and light intensity PA with light to vigorous intensity PA. Greenland Health Survey 2005-10, n=1484.
| Sedentary to light | P-value | Sedentary to moderate | P-value | Light to moderate | P-value | Light to vigorous | P-value | |
|---|---|---|---|---|---|---|---|---|
| Model 1 | ||||||||
| BMI (kg/m2) | -0.21 (-0.37,- 0.04) | 0.015 | -0.47 (-0.81, -0.14) | 0.006 | -0.27 (-0.67, 0.14) | 0.200 | -1.68 (-2.89, -0.46) | 0.007 |
| Waist Circumference (cm) | -0.57 (-1.00, -1.13) | 0.011 | -1.13 (-2.01, -0.26) | 0.011 | -0.56(-1.63, 0.50) | 0.299 | -6.05 (-9.20, -2.30) | <0.001 |
| Visceral fat (cm) | -0.04 (-0.11,0.04) | 0.359 | -0.23 (-0.39, -0.08) | 0.002 | -0.20 (-0.38, -0.02) | 0.034 | -0.66 (-1.21, -0.11) | 0.018 |
| Sub-cutaneous fat (cm) | -0.08 (-0.12,- 0.03) | 0.001 | -0.05 (-0.15, 0.04) | 0.256 | 0.02 (-0.09, 0.14) | 0.692 | -0.67 (-1.01, -0.34) | <0.001 |
| Model 2 | ||||||||
| Waist Circumference (cm) | -0.007 (-0.16, 0.14) | 0.921 | -0.01 (-0.32, 0.30) | 0.951 | -0.002(-0.37, 0.37) | 0.992 | -1.9(-3.0, -0.80) | 0.001 |
| Visceral fat (cm) | 0.03 (-0.02, 0.09) | 0.251 | -0.10 (-0.21, 0.02) | 0.092 | -0.13 (-0.27, 0.007) | 0.063 | -0.17(-0.58,0.25) | 0.427 |
| Sub-cutaneous fat (cm) | -0.03 (-0.06, 0.005) | 0.096 | 0.04 (-0.02, 0.10) | 0.203 | 0.07 (-0.01, 0.15) | 0.082 | -0.33(-0.56,-0.10) | 0.0052 |
SAT: subcutaneous adipose tissue, VAT: visceral adipose tissue, WC: waist circumference (cm). SED: sedentary behavior not including sleep, 1.00-1.5 METs, LPA: light physical activity >1.5-3.0 METs, MPA: moderate physical activity >3.0-6.0 METs, VPA: vigorous physical activity <6.0 METs.
Model 1: Analyses adjusted for age, sex, smoking and fraction of weekend wear time, total hours spent on PA >1 METs
Model 2: Analyses further adjusted for BMI
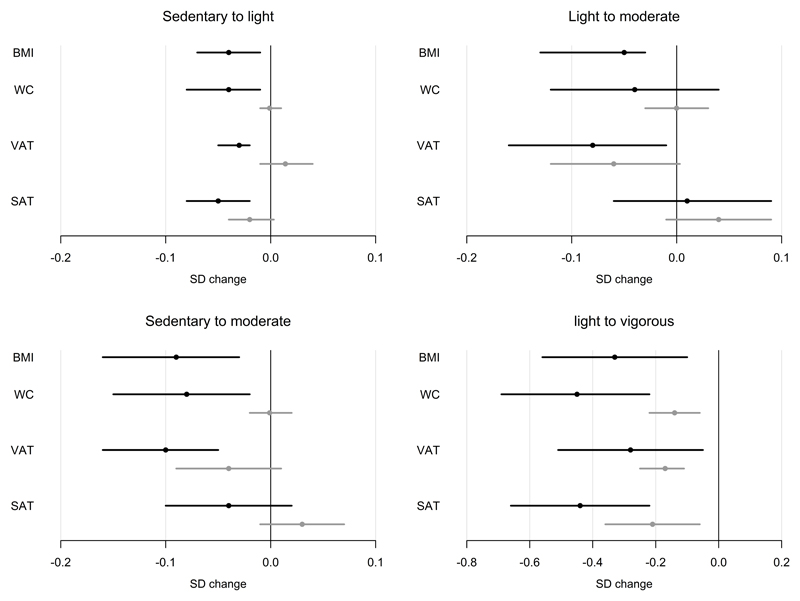
Similar patterns were found for reallocating time spent on moderate intensity PA with vigorous intensity PA (data not shown). The multiple adjusted β-coefficients interpret the size of the association between isotemporal replacements in PA on standard deviation change in obesity measures (figure I). Overall, the magnitude of the association was similar for BMI, WC, VAT and SAT.
Figure 1.
Regression coefficients from isotemporal substitution analyses: Standardised change in outcome (SD for BMI and abdominal fat distribution) by replacing 1-hour of sedentary and light intensity PA with light to vigorous intensity PA. Black lines: Analyses adjusted for age, smoking and fraction of weekend wear time, total hours spent on PA >1 METs. Grey lines: Analyses further adjusted for BMI
SAT: subcutaneous adipose tissue, VAT: visceral adipose tissue, WC: waist circumference (cm). SED: sedentary behavior, 1.00-1.5 METs, LPA: light physical activity >1.5-3.0 METs, MPA: moderate physical activity >3.0-6.0 METs, VPA: vigorous physical activity <6.0 METs.
Analyses of time spent on 1, 5 and 10 minutes bouts of MVPA showed that men compared to women spent more time on 10 minutes bouts of PA with a median of 31 minutes for men, and a median of 13 minutes/day for women (table I). The results of the regression analyses in table IV showed a negative association between both 1, 5 and 10 minutes bouts of PA and overall and abdominal fat distribution (p<0.001). The beta coefficients indicated a trend for lower WC, BMI, SAT and VAT by increasing length of activity bouts from 1 to 5 minutes bouts of MVPA but no difference between 5 and 10 minute bouts of MVPA, however the confidence intervals were overlapping.
Table IV.
Regression coefficients (95% confidence intervals) for waist circumference (WC), visceral fat (VAT) and sub-cutaneous fat (SAT) according to time spent on 1, 5 and 10 minutes bouts of moderate and vigorous intensity physical activity (MVPA). Greenland health survey 2005-2010, n=1458.
| Waist Circumference (cm)≠ β |
P-value | Visceral fat (cm)≠ β |
P-value | Sub-cutaneous fat (cm)≠ β |
P-value | |
|---|---|---|---|---|---|---|
| 1 minutes bouts of MVPA* | -0.0363301 (-0.05 to -0.03) | <0.001 | -0.0050204 (-0.007 to -0.003) | <0.001 | -0.0029539 (-0.004 to -0.002) | <0.001 |
| 5 minutes bouts of MVPA* | -0.0425909 (-0.06 to -0.03) | <0.001 | -0.0056932 (-0.008 to -0.004) | <0.001 | -0.0035231 (-0.005 to -0.002) | <0.001 |
| 10 minutes bouts of MVPA* | -0.045649 (-0.06 to -0.03) | <0.001 | -0.0056367 (-0.008 to -0.003) | <0.001 | -0.0037373 (-0.005 to -0.002) | <0.001 |
Analyses adjusted for age=43, sex, smoking and fraction of weekend wear time. * (>3 METs)
Discussion
We found that physical activity measured as total energy expenditure was negatively related to BMI, waist circumference, visceral fat and subcutaneous fat for men and women independently of BMI among Greenland Inuit. This finding is in accordance with other studies. A 10 kJ/kg/day increase in PAEE corresponded to a 0.9 cm lower waist circumference and a 1mm lower accumulation of visceral and sub-cutaneous fat. This difference could be achieved with an extra hour of gentle walking each day. Our analyses indicated a linear association between PAEE, which are found in a number of other studies (24).
Increasing physical activity intensity resulted in overall favorable results on abdominal fat distribution.
Replacing time spent in lower to higher intensities of PA revealed a negative association with accumulation of both subcutaneous and visceral fat and waist circumference, especially for more time being vigorously physically active. When further adjusting for BMI the associations were overall attenuated; however the directions of the associations were unchanged and associations remained statistically significant except for visceral fat.
Overall our findings correspond to those found in a study of Philipsen and colleagues using both objective measures of physical activity and ultrasonography (26). The effect of high intensity PA on visceral fat accumulation has been supported by other studies. Vissers and colleagues presented in a systematic review and meta-analysis that aerobic exercise of moderate or high intensity had the highest potential to reduce visceral adipose tissue in overweight males and females (34). Subcutaneous fat is found to be less metabolic active compared to visceral fat and in the literature it has been suggested that visceral fat might be especially sensitive to the adrenal driven adipocyte lipolysis that occurs with vigorous exercise (23). However both VAT and SAT has been found to be associated with cardiovascular risk independently of overall obesity indicating a clinical relevance of the lower SAT found in the present study (29).
We found no difference in the associations with PA intensity across components of abdominal fat distribution suggesting that health benefits from physical activity relate to an overall reduction in adipose tissue rather than a reduction in ectopic fat distribution. This may appear surprising as reduction in visceral adipose tissue has been hypothesized as one of the mechanisms underlying long term effects of physical activity on e.g. glucose metabolism (26).
When replacing sedentary time with light or moderate intensity PA and adjusting for BMI the association with abdominal fat distribution measures were no longer statistically significant. This may appear surprising. However, the measurement of PA with Actiheart did not allow a clear distinction between sleep time and sedentary time. Thus, some of the observed associations may reflect less time spent sleeping which in turn is known to increase risk of obesity. Moreover, it is possible that moving from sedentary to light intensity PA is of less importance for abdominal fat accumulation, given the very high level of PA in this population. Studies on sedentary behavior and abdominal fat distribution are still limited (14;15) and the results somewhat conflicting. Results from a 6-year follow-up study showed that changes in sedentary behavior were not associated with changes in visceral adiposity in adults (28).
It has been suggested that changes in sedentary behavior could be related to other parts of the regional fat distribution than visceral fat and subcutaneous fat. A study of Larsen and colleagues (2014) found that greater PA was associated with less visceral fat while greater sedentary time was associated with pericardial fat and concluded that sitting and PA had different associations with regional fat depositions in older adults (19). In line with the rapid changes in lifestyle among Inuit and the large proportion of the day spent sedentary and on light intensity PA, the potential effect of reallocating sedentary behavior – even to light intensity PA on regional fat distribution should be further investigated in a prospective design.
Wientzek and colleagues(37) investigated the effect of cardio-respiratory fitness (CRF), PA, MVPA and sedentary time on anthropometric markers in men and women. Interestingly CRF appeared to attenuate associations between PA, MVPA and sedentary time with abdominal adiposity indicating a possibly important role of CRF for abdominal obesity.
International guidelines have stated that physical activity should be performed in bouts of at least 10 minutes to achieve health benefits and most questionnaires are asking for activities of at least 10 minutes to be included in the response of the participants. An increasing amount of exercise intervention studies have compared longer bouts of exercise with accumulated shorter exercise bouts on different health outcomes. A study of Eriksen at al compared the effects on glycaemic control of two different exercise protocols in elderly men with type 2 diabetes mellitus and found that moderate to high-intensity training performed at 3×10 min/day was preferable to 1×30 min/day with regard to effects on glycaemic control (12). However, it has been stated that further research is required to determine health effects of even shorter bouts of accumulated exercise (<10 minutes). In the present study we were able to differentiate between minutes spent on 1, 5 and 10 minutes bouts of MVPA. In simple regression analyses we demonstrated negative associations between 1, 5 and 10 minutes bouts of MVPA and abdominal fat distribution. Moreover the results indicated a health benefit of increasing bouts of activity from 1 to 5 minutes, but no further benefits for 10 minutes bouts. However sample size might be a potential limitation for studying these differences. Promoting shorter bouts compared with longer bouts of MVPA may be of potential high relevance among those with the lowest activity level and the health effects should be investigated further.
Strengths and limitations
To our knowledge this is the first study to report on associations between objectively measured PA and abdominal fat distribution in a non-western population. A major strength is the large numbers of participants with objective measures of PA allowing for the investigation of intensities of PA. Issues of recall bias are avoided by the use of body-worn monitor-based measures of PA. All though not all participants were objectively monitored for 48 h or more this subsample still represents the largest study conducted to date in this population. Furthermore, participants included in the subsample differed only very little in age, sex and residence compared to participants without ACC + HR data, which implies a fairly representative sample meaning that results will apply to the adult population of Greenland (7). Lastly, we conducted sensitivity analyses to ascertain the impact of restricting our analyses to participants providing at least 72 h of valid PA data. The results are not presented since they were not materially different in relation to the size of the beta-coefficients.
A number of studies have shown that relying only on measures of BMI and Waist circumference may result in a misclassification of individuals in terms of visceral fat and metabolic risk (17;27). We used abdominal fat distribution measured by ultrasound. The gold standard for measuring abdominal fat distribution is commuted tomography (CT) and magnetic resonance imaging (MRI) (30). However, using these methods in a population based study is not feasible due to costs, accessibility and logistics. Ultrasound measurements to measure abdominal fat distribution has shown to be a validated method compared to CT and MRI and is feasible to use for epidemiological purpose (8;9;33).
One limitation in our study is the cross-sectional design, and reverse causality cannot be excluded. In a follow-up study of objectively measured PA and abdominal fat it was found that the association between body fat and MVPA was stronger than the reciprocal association (13). The isotemporal replacement analyses are modeled examples, and although we made adjustment for relevant confounders there is a risk of residual confounding.
Lastly, arbitrary cut-points for PA intensity introduce a risk of misclassification of the intensity level and the fact that increasing the intensity level will result in a higher PAEE independently of total time introduces a possible overestimation of the size of the association.
Conclusion
Along with the rapid social, economic and cultural transition among indigenous people in the Arctic, a more sedentary lifestyle is expected. In conclusion this study confirms that increasing total physical activity energy expenditure matters in relation to abdominal fat distribution among Inuit in Greenland. Especially being more vigorously physically active was related to a lower accumulation of both subcutaneous and visceral fat. However, also reallocating sedentary time to moderate intensity PA might be of great relevance for decreasing abdominal obesity on a population level. Moreover, this study indicates that even bouts of 1 minute of moderate to vigorous PA have a potential effect on abdominal fat distribution. The results of this study can be used in the specification of recommendations for physical activity and contribute to the prevention of the increasing burden of abdominal obesity and type 2 diabetes in Greenland.
Acknowledgments
This study was funded by the Karen Elise Jensen Foundation, Denmark. The authors are grateful to the participants and the participating communities. The authors would also like to thank Kate Westgate and Stefanie Mayle at the MRC Epidemiology Unit, Cambridge, United Kingdom, for assistance in data processing. The authors declare that there are no conflicts of interest.
The results of the present study do not constitute endorsement by the American College of Sports Medicine. The authors declare that the results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
References
- (1).Andersen S, Mulvad G, Pedersen HS, Laurberg P. Gender diversity in developing overweight over 35 years of Westernization in an Inuit hunter cohort and ethno-specific body mass index for evaluation of body-weight abnormalities. Eur J Endocrinol. 2004;151(6):735–40. doi: 10.1530/eje.0.1510735. [DOI] [PubMed] [Google Scholar]
- (2).Bjerregaard P. National Institute of Public Health. 2009. [cited December 2016]. Inuit Health in Transition. Greenland survey 2005-2009. Population sample and survey methods; pp. 1–13. Available from http://www.si-folkesundhed.dk/upload/inuit_health_in_transition_greenland_methods_5_002.pdf. [Google Scholar]
- (3).Bjerregaard P, Jørgensen ME. Prevalence of obesity among Inuit in Greenland and temporal trend by social position. Am J Hum Biol. 2013;25(3):335–40. doi: 10.1002/ajhb.22372. [DOI] [PubMed] [Google Scholar]
- (4).Brage S, Brage N, Franks PW, Ekelund U, Wareham NJ. Reliability and validity of the combined heart rate and movement sensor Actiheart. Eur J Clin Nutr. 2005;59(4):561–70. doi: 10.1038/sj.ejcn.1602118. [DOI] [PubMed] [Google Scholar]
- (5).Brage S, Brage N, Franks PW, et al. Branched equation modeling of simultaneous accelerometry and heart rate monitoring improves estimate of directly measured physical activity energy expenditure. J Appl Physiol. 2004;96(1):343–51. doi: 10.1152/japplphysiol.00703.2003. [DOI] [PubMed] [Google Scholar]
- (6).Brage S, Ekelund U, Brage N, et al. Hierarchy of individual calibration levels for heart rate and accelerometry to measure physical activity. J Appl Physiol. 2007;103(2):682–92. doi: 10.1152/japplphysiol.00092.2006. [DOI] [PubMed] [Google Scholar]
- (7).Dahl-Petersen IK, Bjerregaard P, Brage S, Jorgensen ME. Physical activity energy expenditure is associated with 2-h insulin independently of obesity among Inuit in Greenland. Diabetes Res Clin Pract. 2013;102(3):242–9. doi: 10.1016/j.diabres.2013.10.004. [DOI] [PubMed] [Google Scholar]
- (8).De Lucia RE, Norris SA, Sleigh A, et al. Validation of ultrasound estimates of visceral fat in black South African adolescents. Obesity (Silver Spring) 2011;19(9):1892–7. doi: 10.1038/oby.2011.213. [DOI] [PubMed] [Google Scholar]
- (9).De Lucia RE, Sleigh A, Finucane FM, et al. Ultrasound measurements of visceral and subcutaneous abdominal thickness to predict abdominal adiposity among older men and women. Obesity (Silver Spring) 2010;18(3):625–31. doi: 10.1038/oby.2009.309. [DOI] [PubMed] [Google Scholar]
- (10).Ekelund U, Besson H, Luan J, et al. Physical activity and gain in abdominal adiposity and body weight: prospective cohort study in 288,498 men and women. Am J Clin Nutr. 2011;93(4):826–35. doi: 10.3945/ajcn.110.006593. [DOI] [PubMed] [Google Scholar]
- (11).Ekelund U, Brage S, Franks PW, et al. Physical activity energy expenditure predicts changes in body composition in middle-aged healthy whites: effect modification by age. Am J Clin Nutr. 2005;81(5):964–9. doi: 10.1093/ajcn/81.5.964. [DOI] [PubMed] [Google Scholar]
- (12).Eriksen L, Dahl-Petersen I, Haugaard SB, Dela F. Comparison of the effect of multiple short-duration with single long-duration exercise sessions on glucose homeostasis in type 2 diabetes mellitus. Diabetologia. 2007;50(11):2245–53. doi: 10.1007/s00125-007-0783-0. [DOI] [PubMed] [Google Scholar]
- (13).Golubic R, Wijndaele K, Sharp SJ, et al. Physical activity, sedentary time and gain in overall and central body fat: 7-year follow-up of the ProActive trial cohort. Int J Obes (Lond) 2015;39(1):142–8. doi: 10.1038/ijo.2014.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (14).Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003-06. Eur Heart J. 2011;32(5):590–7. doi: 10.1093/eurheartj/ehq451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (15).Healy GN, Wijndaele K, Dunstan DW, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Diabetes Care. 2008;31(2):369–71. doi: 10.2337/dc07-1795. [DOI] [PubMed] [Google Scholar]
- (16).Irving BA, Davis CK, Brock DW, et al. Effect of exercise training intensity on abdominal visceral fat and body composition. Med Sci Sports Exerc. 2008;40(11):1863–72. doi: 10.1249/MSS.0b013e3181801d40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (17).Jørgensen ME, Borch-Johnsen K, Stolk R, Bjerregaard P. Fat distribution and glucose intolerance among Greenland Inuit. Diabetes Care. 2013;36(10):2988–94. doi: 10.2337/dc12-2703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (18).Kohli S, Sniderman AD, Tchernof A, Lear SA. Ethnic-specific differences in abdominal subcutaneous adipose tissue compartments. Obesity (Silver Spring) 2010;18(11):2177–83. doi: 10.1038/oby.2010.94. [DOI] [PubMed] [Google Scholar]
- (19).Larsen BA, Allison MA, Kang E, et al. Associations of physical activity and sedentary behavior with regional fat deposition. Med Sci Sports Exerc. 2014;46(3):520–8. doi: 10.1249/MSS.0b013e3182a77220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (20).McGuire KA, Ross R. Incidental physical activity and sedentary behavior are not associated with abdominal adipose tissue in inactive adults. Obesity (Silver Spring) 2012;20(3):576–82. doi: 10.1038/oby.2011.278. [DOI] [PubMed] [Google Scholar]
- (21).Moltke I, Fumagalli M, Korneliussen TS, et al. Uncovering the genetic history of the present-day Greenlandic population. Am J Hum Genet. 2015;96(1):54–69. doi: 10.1016/j.ajhg.2014.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (22).Murabito JM, Pedley A, Massaro JM, et al. Moderate-to-vigorous physical activity with accelerometry is associated with visceral adipose tissue in adults. J Am Heart Assoc. 2015;4(3):e001379. doi: 10.1161/JAHA.114.001379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (23).Murphy JC, McDaniel JL, Mora K, Villareal DT, Fontana L, Weiss EP. Preferential reductions in intermuscular and visceral adipose tissue with exercise-induced weight loss compared with calorie restriction. J Appl Physiol (1985) 2012;112(1):79–85. doi: 10.1152/japplphysiol.00355.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (24).Ohkawara K, Tanaka S, Miyachi M, Ishikawa-Takata K, Tabata I. A dose-response relation between aerobic exercise and visceral fat reduction: systematic review of clinical trials. Int J Obes (Lond) 2007;31(12):1786–97. doi: 10.1038/sj.ijo.0803683. [DOI] [PubMed] [Google Scholar]
- (25).Philipsen A, Carstensen B, Sandbaek A, et al. Reproducibility of ultrasonography for assessing abdominal fat distribution in a population at high risk of diabetes. Nutr Diabetes. 2013;3:e82. doi: 10.1038/nutd.2013.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (26).Philipsen A, Hansen AL, Jørgensen ME, et al. Associations of Objectively Measured Physical Activity and Abdominal Fat Distribution. Med Sci Sports Exerc. 2015;47(5):983–9. doi: 10.1249/MSS.0000000000000504. [DOI] [PubMed] [Google Scholar]
- (27).Pou KM, Massaro JM, Hoffmann U, et al. Patterns of abdominal fat distribution: the Framingham Heart Study. Diabetes Care. 2009;32(3):481–5. doi: 10.2337/dc08-1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (28).Saunders TJ, Tremblay MS, Despres JP, Bouchard C, Tremblay A, Chaput JP. Sedentary behaviour, visceral fat accumulation and cardiometabolic risk in adults: a 6-year longitudinal study from the Quebec Family Study. PLoS One. 2013;8(1):e54225. doi: 10.1371/journal.pone.0054225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (29).Scheuer SH, Faerch K, Philipsen A, et al. Abdominal Fat Distribution and Cardiovascular Risk in Men and Women With Different Levels of Glucose Tolerance. J Clin Endocrinol Metab. 2015;100(9):3340–7. doi: 10.1210/JC.2014-4479. [DOI] [PubMed] [Google Scholar]
- (30).Seidell JC, Bakker CJ, van der Kooy K. Imaging techniques for measuring adipose-tissue distribution--a comparison between computed tomography and 1.5-T magnetic resonance. Am J Clin Nutr. 1990;51(6):953–7. doi: 10.1093/ajcn/51.6.953. [DOI] [PubMed] [Google Scholar]
- (31).Smith HA, Storti KL, Arena VC, et al. Associations between accelerometer-derived physical activity and regional adiposity in young men and women. Obesity (Silver Spring) 2013;21(6):1299–305. doi: 10.1002/oby.20308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (32).Stegle O, Fallert SV, Mackay DJC, Brage S. Gaussian process robust regression for noisy heart rate data. Ieee Transactions on Biomedical Engineering. 2008;55(9):2143–51. doi: 10.1109/TBME.2008.923118. [DOI] [PubMed] [Google Scholar]
- (33).Stolk RP, Wink O, Zelissen PM, Meijer R, van Gils AP, Grobbee DE. Validity and reproducibility of ultrasonography for the measurement of intra-abdominal adipose tissue. Int J Obes Relat Metab Disord. 2001;25(9):1346–51. doi: 10.1038/sj.ijo.0801734. [DOI] [PubMed] [Google Scholar]
- (34).Vissers D, Hens W, Taeymans J, Baeyens JP, Poortmans J, Van GL. The effect of exercise on visceral adipose tissue in overweight adults: a systematic review and meta-analysis. PLoS One. 2013;8(2):e56415. doi: 10.1371/journal.pone.0056415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (35).Wander PL, Boyko EJ, Leonetti DL, McNeely MJ, Kahn SE, Fujimoto WY. Change in visceral adiposity independently predicts a greater risk of developing type 2 diabetes over 10 years in Japanese Americans. Diabetes Care. 2013;36(2):289–93. doi: 10.2337/dc12-0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (36).Wareham NJ, van Sluijs EM, Ekelund U. Physical activity and obesity prevention: a review of the current evidence. Proc Nutr Soc. 2005;64(2):229–47. doi: 10.1079/pns2005423. [DOI] [PubMed] [Google Scholar]
- (37).Wientzek A, Tormo Diaz MJ, Castano JM, et al. Cross-sectional associations of objectively measured physical activity, cardiorespiratory fitness and anthropometry in European adults. Obesity (Silver Spring) 2014;22(5):E127–E134. doi: 10.1002/oby.20530. [DOI] [PubMed] [Google Scholar]