Abstract
Background
Modifications to lifestyle risk factors for stroke may help prevent stroke events. This systematic review aimed to identify and summarise the evidence of acupuncture interventions for those people with lifestyle risk factors for stroke, including alcohol-dependence, smoking-dependence, hypertension, and obesity.
Methods
MEDLINE, CINAHL/EBSCO, SCOPUS, and Cochrane Database were searched from January 1996 to December 2016. Only randomised controlled trials (RCTs) with empirical research findings were included. PRISMA guidelines were followed and risk of bias was assessed via the Cochrane Collaboration risk of bias assessment tool. The systematic review reported in this paper has been registered on the PROSPERO (#CRD42017060490).
Results
A total of 59 RCTs (5,650 participants) examining the use of acupuncture in treating lifestyle risk factors for stroke met the inclusion criteria. The seven RCTs focusing on alcohol-dependence showed substantial heterogeneity regarding intervention details. No evidence from meta-analysis has been found regarding post-intervention or long-term effect on blood pressure control for acupuncture compared to sham intervention. Relative to sham acupuncture, individuals receiving auricular acupressure for smoking-dependence reported lower numbers of consumed cigarettes per day (two RCTs, mean difference (MD) = -2.75 cigarettes/day; 95% confidence interval (CI) = -5.33, -0.17; p = 0.04). Compared to sham acupuncture those receiving acupuncture for obesity reported lower waist circumference (five RCTs, MD = -2.79 cm; 95% CI: -4.13, -1.46; p<0.001). Overall, only few trials were considered of low risk of bias for smoking-dependence and obesity, and as such none of the significant effects in favour of acupuncture interventions were robust against potential selection, performance, and detection bias.
Conclusions
This review found no convincing evidence for effects of acupuncture interventions for improving lifestyle risk factors for stroke.
Introduction
Stroke is a major health issue with a significant burden upon quality of life and disability [1]. The control of stroke risk factors plays a vital role in reducing the risk of new or subsequent strokes of all types [2]. Three types of risk factors have been identified for stroke, including non-modifiable risk factors, medical risk factors, and lifestyle risk factors [2,3]. Lifestyle risk factors for stroke—hypertension, high cholesterol, smoking-dependence, alcohol-dependence, obesity, poor diet/physical inactivity—approximately accounted for 80% of the global risk of stroke [3]. Therefore, lifestyle risk factors for stroke are an ideal target for stroke prevention in comparison with other risk factors [4]. A growing stroke burden throughout the world suggests contemporary stroke prevention strategies for modifiable lifestyle risk factors may be insufficient and new effective approaches are needed [5]. However, the evidence for modification of lifestyle risk factors which are recommended by clinical guidelines for stroke management are not satisfactory [5,6].
Acupuncture is a traditional Chinese therapeutic intervention characterised by the insertion of fine metallic needles through the skin at specific sites (acupoints), with body and ears being the most common locations of acupoints [7]. Needles may be stimulated manually or by applying electric current [8]. There are various types of acupuncture treatments, such as needle acupuncture, electroacupuncture, acupressure, laser therapy, and transcutaneous electric acupoint stimulation (TEAS) [9]. Acupuncture has long been used for chronic diseases including musculoskeletal pain and hypertension [7]. The biological effects of acupuncture treatments, such as local inflammatory responses, anti-analgesia effects, and increase of opioid peptides, play an important role in the therapeutic effects of such therapy [10]. Nevertheless, the challenges inherent in designing and implementing rigorous acupuncture research may limit the understanding of the effectiveness of acupuncture, such as those relating to acupuncturists’ use of distinct syndrome classifications identified among people with the same condition and use of different skills when selecting and manipulating acupoints [11].
Using acupuncture to manage each lifestyle risk factor for stroke has attracted substantial and growing research interest over many decades. Previous reviews reported promising results of acupuncture use in controlling hypertension-associated symptoms [12], attaining weight loss [13], and reducing nicotine withdrawal symptoms [9]. In addition, WHO has indicated the effect of acupuncture for alcohol-dependence, in particular auricular acupuncture [14]. Nonetheless, a comprehensive systematic review assessing the effect of all forms of acupuncture for all identified lifestyle risk factors for stroke has not been conducted. As such, the aim of this paper is to identify and summarise the contemporary evidence of acupuncture interventions for lifestyle risk factors for stroke.
Methods
The systematic review reported in this paper has been registered with PROSPERO (International prospective register of systematic reviews, #CRD42017060490).
Search strategy
In accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guideline, a systematic search of the literature was conducted using the MEDLINE, CINAHL/EBSCO, Scopus, and Cochrane Database of Systematic Reviews databases for studies published from January 1996 to December 2016. The lifestyle risk factors for stroke included in this systematic review are high blood pressure (hypertension & prehypertension), high cholesterol, obesity (overweight/obesity), smoking-dependence, alcohol-dependence, and physical inactivity. The literature search employed keyword and MeSH searches for terms relevant to ‘acupuncture’ and each lifestyle risk factor for stroke. Search terms used for each database are available in Table 1. Relevant randomised controlled trials (RCT) listed as references of published systematic review papers on selected lifestyle risk factors for stroke were also searched via Google Scholar by title, in order to include all relevant RCTs in this field.
Table 1. Search terms for the systematic review.
| Acupuncture treatments | Acupuncture [MeSH Term & Keyword] OR Electroacupuncture [MeSH Term & Keyword] OR Electric stimulation [MeSH Term & Keyword] OR Acupressure [MeSH Term & Keyword] OR Laser acupuncture [MeSH Term & Keyword] OR *acupunctur*[Title/Abstract] | |
| AND | ||
| Lifestyle stroke risk factors | High blood pressure | Hypertension [MeSH Term & Keyword] OR Blood pressure [MeSH Terms & Keyword] OR Hypertens* [Title/Abstract] OR Prehypertens* [Title/Abstract] OR Systolic [Title/Abstract] OR Diastolic [Title/Abstract] OR |
| High cholesterol | Cholesterol [MeSH Term & Keyword] OR Triglycerides [MeSH Term & Keyword] OR Dyslipidemia [MeSH Term & Keyword] OR Epicholesterol [Title/Abstract] OR HDL [Title/Abstract] OR LDL [Title/Abstract] OR Triglyceride* [Title/Abstract] OR Hyperlipidem* [Title/Abstract] OR Lipidem* [Title/Abstract] OR | |
| Obesity | Obesity [MeSH Terms & Keyword] OR Overweight [MeSH Terms & Keyword] OR Metabolic syndrome [MeSH Terms & Keyword] OR Obes* [Title/Abstract] OR Adiposity [Title/Abstract] OR Adipos* [Title/Abstract] | |
| Alcohol-dependence/abuse | Alcohol [MeSH Terms & Keyword] OR Alcohol* [Title/Abstract] | |
| Smoking-dependence/abuse | Smoking [MeSH Terms & Keyword] OR Smok* [Title/Abstract] | |
| Physical inactivity | Exercise [MeSH Terms & Keyword] OR Exercis* [Title/Abstract] | |
* truncation symbol for literature search.
Selection criteria
Types of studies
Studies were eligible for inclusion if they met the following criteria: (1) RCTs focusing on the efficacy and safety of acupuncture for lifestyle risk factors for stroke; (2) conducted in humans; (3) published in a peer-reviewed English language journal with abstracts; (4) reported primary data findings. Exclusion criteria were (1) RCT protocols or observation of a RCT of this research area; (2) quasi-/pseudo-RCTs and cross-over RCTs (3) studies focusing on the efficacy and safety of acupuncture treatment(s) for stroke or post-stroke symptoms; (4) studies focusing on the efficacy and safety of acupuncture treatment(s) for the complications of stroke risk factors; and (5) conference abstracts.
Types of interventions
There was no limitation on the forms of (traditional) acupuncture and the frequency and duration of the intervention. However, contemporary acupuncture such as trigger points and dry needling was not eligible for inclusion in this review.
Types of outcome measures
Only anthropometric parameters and the widely used indicators of each lifestyle risk factor for stroke were included. The primary outcomes were a change in systolic blood pressure (SBP) and/or diastolic blood pressure (DBP) for hypertension-focused RCTs; triglycerides, LDL/HDL cholesterol for hyperlipidemia/dyslipidemia-focused RCTs; body weight (BW), body mass index (BMI), waist circumference (WC) for obesity-focused RCTs; alcohol craving, completion rate of treatment, withdrawal symptoms for RCTs focusing on alcohol-dependence; withdrawal symptoms, daily cigarette consumption, abstinence rate for RCTs focusing on smoking-dependence; physical activity minutes/day and cardiorespiratory fitness for physical inactivity-focused RCTs.
Data extraction
Title and abstracts of all citations identified in the search were imported to Endnote (Version X8) and duplicates removed. These citations were independently reviewed for eligibility by two authors (WP and RL) and the full texts of ambiguous articles were retrieved if consensus was not reached. Any disagreements were assessed by a third author. We contacted authors regarding raw data of their RCTs where necessary for meta-analysis. Where we failed to obtain such raw data, the RCT had to be excluded in the meta-analysis. According to the RCT description in the articles included, raw data were extracted from post-intervention effect and/or follow-up (long-term) effect.
Data were extracted into a pre-determined table (Table 2) and checked for coverage and accuracy by two authors independently. Table 2 includes detailed information on sample size, inclusion criteria, participants’ characteristics, intervention groups, add-on strategy, results of outcome measures, and side-effects. Both statistically significant within-group and/or between-group effect of acupuncture interventions for each lifestyle risk factor for stroke were recorded if reported.
Table 2. Summary of the included studies.
| Sample | Treatment intervention | Control intervention | Add-on strategya | Results | Side-effects | |
|---|---|---|---|---|---|---|
| Alcohol-dependence | ||||||
| Rampes et al. 1997 UK[21] | 59 randomized and 27, 26 completed at Wks 8, 24. | 1. Specific auricular electroacupuncture group Acupoints: Lung, Shenmen, Sympathetic; 2. Nonspecific auricular electroacupuncture group Acupoints: Elbow, Internal secretion; Manipulation: 100Hz frequency, 30 min/session, Weekly, 24 Wks | Individual alcohol counsellor/group therapy, 6 Wks | Conventional treatment | Alcohol craving: Significant within-group effect—TG1 & TG2 (8Wk) | Drowsiness; transient bleeding on needle removal; pain |
| TG1: n = 23, 4 F, age 38y; TG2: n = 20, 3 F, age 40y; CG: n = 16, 6 F, age 42y; | ||||||
| Inclusion: alcohol withdrawal (DSM-III-R); 18–65 years; no previous acupuncture use | ||||||
| Sapir-Weise et al. 1999 Sweden[20] | 72 randomized and 72, 59, 51 completed at Wk 10, Mos 3, 6. | Auricular acupuncture group Acupoints: Lung, Shenmen, Sympathetic; Manipulation: nurses administered. 45 mins/session, Weekly (2-Wk), 3 times/Wk (4-Wk), twice/Wk (4-Wk) | Non-specific acupuncture group Acupoints: 3-5mm from the real acupoints; Same manipulation | Conventional treatment | Drinking days/alcohol craving: NS | N/A |
| TG: n = 36, 11 F, age 47y; CG: n = 36, 10 F, age 45y; | ||||||
| Inclusion: alcohol withdrawal (DSM-III-R); no previous drug use | ||||||
| Bullock et al. 2002 USA[22] | 503 randomized and 356, 289, 247, 220 completed at Wk 3, Mos 3, 6, 12. | 1. Specific auricular acupuncture group Acupoints: Liver, Lung, Shenmen, Sympathetic; 2. Nonspecific auricular acupuncture group Acupoints: 5mm from the specific acupoints; 3. Symptom-based auricular acupuncture group Acupoints changed daily; Manipulation: acupuncturists administered. No manipulation. 40 mins/session, Weekly, 3 Wks | Conventional treatment group Detoxification, inpatient treatment, etc., 3 Wks | Conventional treatment | Alcohol withdrawal symptoms: Significant between-group effect—TG3>TG1 (12-Mo F/U) | N/A |
| TG1: n = 132, 65 F, age 39y; TG2: n = 133, 66 F, age 38y; TG3: n = 104, 52 F, age 38y; CG: n = 134, 67 F, age 38 y; | ||||||
| Inclusion: alcohol≥3 days/Wk; 18–66 years; on-site≥14 days; blood platelet>22,000; no medications for alcohol abuse | ||||||
| Karst et al. 2002 Germany[19] | 34 completed. | Auricular-body acupuncture group Auricular acupoints: Kidney, Liver, Lung, Shenmen, Sympathetic; Body acupoints: DU20, Extra1, LI4; Manipulation: 30 mins/session, daily, 10 sessions | Sham group Same acupoints/manipulation; Needles without tips | Carbamazepine | Alcohol withdrawal symptoms: Significant within-group effect—TG | N/A |
| TG: n = 17, 2 F, age 46y; CG: n = 17, 2 F, age 41y; | ||||||
| Inclusion: alcohol withdrawal (ICD-10); >18 years; no previous acupuncture use; no addiction to drugs | ||||||
| Trumpler et al. 2003 Switzerland[18] | 48 randomized and completed. | 1. Laser auricular acupuncture group 2. Needle auricular acupuncture group Acupoints: prescribed individually; Manipulation: acupuncturists administered, daily, 6 days. 830nm infrared laser stimulation, 1 min per acupoint; no manipulation of the needle acupuncture, <40 mins/session | Sham laser group Same acupoints; No activated laser beam | Clomethiazole; benzodiazepines if necessary; maintain other drugs before study | Alcohol withdrawal symptoms: NS | Convulsion (TG) |
| TG1: n = 17, 7 F, age 43y; TG2: n = 15, 5 F, age 45y; CG: n = 16, 8 F, age 49y; | ||||||
| Inclusion: alcohol withdrawal (DSM-IV); 18–65 years; no addiction to other drugs | ||||||
| Kunz et al. 2007 Germany[17] | 109 randomized and 74 completed. | Auricular acupuncture group Acupoints: Kidney, Liver, Lung, Shenmen, Sympathetic; Manipulation: psychiatrists/nurses administered. Needle stimulation, 45 mins/session, daily at 12:15PM, 5 days | Aromatherapy group 45 mins/session, daily at 12:15PM, 5 days | Carbamazepine or oxcarbazepine; benzodiazepines | Alcohol withdrawal symptoms/alcohol craving: NS | Pain, mild bleeding (TG); agitation, sneezing, sore throat (CG) |
| TG: n = 55, 10 F, age 48y; CG: n = 54, 10 F, age 44y; | ||||||
| Inclusion: alcohol withdrawal (ICD-10); alcohol≥10 days; 18–65 years; no addiction to other drugs | ||||||
| Lee et al. 2015 Korea[16] | 20 randomized and completed. | Body acupuncture group Acupoint: KI9; Manipulation: oriental medical doctors administered. 15 mins/session, twice/Wk, 4 Wks | Sham group Same acupoints/manipulation; Needles without tips | N/A | Alcohol craving: NS | N/A |
| TG: n = 10, age 43y; CG: n = 10, age 45y; | ||||||
| Inclusion: alcohol withdrawal (DSM-IV); male; no addiction to other drugs | ||||||
| Smoking-dependence | ||||||
| He et al. 1997 Norway[23,24] | 46 randomized (age 39y) and 44, 38, 33 completed at Wk 3, Mo 8, Year 5. | ① Body electroacupuncture, ② auricular acupuncture, ③ auricular acupressure group Acupoints: ① LU6, LU7; ② Lung, Mouth, Shenmen; ③ Endocrine, Hunger, Lung, Mouth, Shenmen, Trachea; Manipulation: acupuncturists administered, 3 Wks. ① 3Hz frequency, 20 mins, twice/Wk; ② needle stimulation, 20 mins, twice/Wk; ③ Vaccariae seeds acupressure 100 repeats/time, 4 times/day | Non-specific acupuncture group Acupoints: ① LI10, SJ8; ② Knees, Lumbar vertebra, Neck; ③ Buttock, Knees, Lumbar vertebra, Neck, Shoulder, Shoulder joint; Same manipulation | N/A | Daily cigarette consumption, desire to smoke: Significant within-group effect—TG (8-Mo/5-year F/U), CG (8-Mo F/U); Significant between-group effect—TG>CG (8-Mo F/U); | N/A |
| TG: n = 26, 18 F, age 38y; CG: n = 20, 10 F, age 40y; | Cotinine concentrations: Significant within-group effect—TG; | |||||
| Inclusion: smoking≥5 years and 10–30 cigarettes/day last year; heathy; no co-intervention for smoking | Smoking cessation rate: Significant between-group effect—TG>CG | |||||
| Waite & Clough 1998 UK[25] | 79 randomized and 78 completed at Wk 2, Mos 2, 4, 6. | Auricular electroacupuncture plus acupressure group Acupoints: Lung; Manipulation: general practitioners administered, 2 Wks. 4Hz frequency, 20 mins/session; Chinese cow herb seed acupressure when feeling craving | Sham group Same acupoints/manipulation; Superficially placed needles | N/A | Smoking cessation rate: Significant between-group effect—TG>CG (6-Mo F/U) | Soreness, itch, pain of ears (TG); soreness, itch of ears (TG & CG) |
| TG: n = 40, 18 F, age 24-67y; CG: n = 38, 16 F, age 23-69y; | ||||||
| Inclusion: ≥10 cigarettes/day; >18 years; no previous acupuncture use | ||||||
| White et al. 1998 UK[26] | 76 randomized and 52 completed at Wk 2, Mo 9. | Auricular electroacupuncture group Acupoints: Lung; Manipulation: acupuncturists administered. 100Hz frequency increase to above the threshold of sensation, 20 mins/session, 2 Wks | Sham group Superficially placed needles on location not acupoints | N/A | Smoking cessation rate: NS | N/A |
| TG: n = 38, 21 F, age 41y; CG: n = 38, 18 F, age 43y; | ||||||
| Inclusion: ≥15 cigarettes/day; >21 years; no previous acupuncture use | ||||||
| Georgiou et al. 1998 UK[27] | 265 randomized and 216, 175, 63 completed at Wk 1, Mos 1, 3 (age 43y). | Auricular electroacupuncture group Acupoints: SJ17, SJ18; Manipulation: maximum 1-hour stimulation either 10Hz continuous frequency or 7-14Hz modulated frequency, 1 Wk | Non-specific acupuncture group Acupoints: SI15; Manipulation: stimulation machines disconnected from the electrodes | N/A | Smoking cessation rate/withdrawal symptoms/craving: NS | N/A |
| TG: n = 108; CG: n = 108; | ||||||
| Inclusion: >10 cigarettes/day last year; >18 years; no co-intervention for smoking | ||||||
| Cai et al. 2000 Singapore[29] | 330 randomized and 268 (68 F), 208 completed at 6-session, Mo 3. | Laser auricular acupuncture group Acupoints: Lung, Mouth, Shenmen, Sympathetic; Manipulation: 6328A wavelength, 1mm diameter, 4 mins/session, 6 sessions | Sham group Same acupoints/manipulation; No laser ray | N/A | Daily cigarette consumption/Smoking cessation rate: NS | Headache, giddy, nausea, vomiting (TG: 20; CG: 21) |
| TG: n = 128; CG: n = 140; | ||||||
| Inclusion: smoking≥3 Mos and ≥5 cigarettes/day; 12–18 years | ||||||
| Bier et al. 2002 USA[31] | 141 randomized (71 F, age 46y) and 108, 48 completed at Mos 1, 18. | 1. Auricular-body acupuncture plus education group 2. Auricular-body acupuncture group Auricular acupoints: Kidney, Liver, Lung, Shenmen, Sympathetic; Body acupoints: LI4; Manipulation: acupuncturists administered. No needle stimulation. 30 mins/session, 4 Wks;Educational program: behavioral training, social support, relapse prevention techniques, 5 Wks | Sham acupuncture plus education group Acupoints: 5mm from the real acupoints; Same manipulation/education | N/A | Daily cigarette consumption, Smoking cessation rate: Significant between-group effect—TG1>CG>TG2 (after treatment) | Minor bleeding on needle removal (both TGs) |
| TG1: n = 45; TG2: n = 38; CG: n = 58; | ||||||
| Inclusion: quitting smoking without success≥1; >18 years; no addiction to other drugs | ||||||
| White et al. 2007 UK[28] | 24 randomized and 19, 7 completed at Wks 1, 6. | Auricular acupressure group 1 Acupoints: Lung, Shenmen; Auricular acupressure group 2 Acupoints: Lung; Manipulation: researchers administered. Beads pressed when feeling craving, 6 Wks | No intervention group | NRT, group behavioral therapy | Withdrawal symptom: NS | N/A |
| TG1: n = 6, 2 F, age 51y; TG2: n = 6, 5 F, age 40y; CG: n = 7, 7 F, age 44y; | ||||||
| Inclusion: ≥10 cigarettes/day; >18 years; no co-intervention for smoking | ||||||
| Wu et al. 2007 Taiwan[33] | 118 randomized and completed at Wk 8, Mo 6. | Auricular acupuncture group Acupoints: Lung, Mouth, Shenmen, Sympathetic; Manipulation: acupuncturists administered. 8 Wks | Non-specific acupuncture group Acupoints: Elbow, Eye, Knee, Shoulder; Same manipulation | N/A | Withdrawal symptom: Significant within-group effect—TG (after treatment); | Tenderness sensation (n = 50), dizziness (n = 4), minor bleeding (n = 2), nausea sensation (n = 2) |
| TG: n = 59, 11 F, age 54y; CG: n = 59, 7 F, age 53y; | Daily cigarette consumption: Significant within-group effect—TG & CG (after treatment) | |||||
| Inclusion: smoking>1 year and ≥10 cigarettes/day; ≥18 years; no addiction to other drugs | ||||||
| Yeh et al. 2009 Taiwan[34] | 79 randomized and 59 completed. | Auricular electroacupuncture plus acupressure group Acupoints: Endocrine, Lung, Mouth, Shenmen, Stomach, Tim mee; Manipulation: <60Hz frequency, 20 mins/session, Weekly; Vaccariae seeds acupressure 1 min/time, 3–5 times/day; 6 Wks | Sham group 5mm from the real acupoints; Same manipulation | N/A | Daily cigarette consumption: Significant within-group effect—TG & CG | N/A |
| TG: n = 30, age 28y; CG: n = 29, age 27y; | ||||||
| Inclusion: smoking>1y and >1 cigarette/day; serum cotinine concentration >100ng/ml; no co-intervention for smoking | ||||||
| Chae et al. 2010 Korea[35] | 29 completed. | Body acupuncture group Acupoint: HT7; Manipulation: needle stimulation 30 seconds and withdrawn 20 minutes, 2 days | Non-specific acupuncture group Acupoint: LI10; Manipulation: blunted needle via a device, 2 days | N/A | Withdrawal symptoms: Significant between-group effect—TG>CG | None |
| TG: n = 15; CG: n = 14; | ||||||
| Inclusion: >10 cigarettes/day; >18 years; male; no co-intervention for smoking; no addiction to other drugs | ||||||
| Wing et al. 2010 Hong Kong[36] | 70 randomized and 51 completed at Wk 3, Mo 3. | Auricular acupressure group Auricular acupoints: Brain, Lung, Mouth, Shenmen; Manipulation: beads pressed when feeling craving, ≥3 times/day, 3 Wks | Non-specific acupuncture group Acupoints: non-specific non-meridian points; Same manipulation | N/A | Daily cigarette consumption: Significant within-group effect—TG (after treatment, 3-Mo F/U), CG (after treatment) | Skin allergy (n = 3) |
| TG: n = 38, 12 F, age 47y; CG: n = 32, 9 F, age 46y; | ||||||
| Inclusion: daily cigarette smoking; ≥18 years; no co-intervention for smoking | ||||||
| Lambert et al. 2011 Singapore[30] | 58 randomized and 55 completed. | 10mA body TEAS group Acupoints: LI4, PC6, PC8, TE5; Manipulation: 1 sessions on Day 1, 3 sessions on Day 2 while abstaining from smoking, 26 hours | 1. i5mA TEAS group (intermittent: 3min on and 7min off) 2. Sham TEAS group (no electrical stimulation) Same acupoints/manipulation | N/A | Desire to smoke: Significant between-group effect—TG>both CGs if FTND≥5 | Coughing, giddiness, finger/hand numbness (TG: 9; CG2: 3); runny nose (CG1: 3) |
| TG: n = 21, 6 female, age 25y; CG1: n = 20, 7 female, age 24y; CG2: n = 17, 2 female, age 26y; | ||||||
| Inclusion: smoking>1-year and ≥15 cigarettes/day; FTND score≥4; no NRT within 3-Mo | ||||||
| Fritz et al. 2013 USA[32] | 125 randomized and 105 completed. | Auricular TEAS group Acupoints: Lung, Nicotine, Palate, Shenmen, Zero; Manipulation: acupuncturists administered. 80Hz frequency, 20 mins/session, Weekly, 5 Wks | Sham group Same acupoints/manipulation; No electrical stimulation | 1-hour ‘stop-smoking’ class | Daily cigarette consumption, withdrawal symptoms: NS | 15 reported (no detail) |
| TG: n = 64, 16 F, age 56y; CG: n = 61, 14 F, age 55y; | ||||||
| Inclusion: ≥10 cigarettes/day; PHQ-9<20; urine cotinine≥200mg/ml; >19 years; no co-intervention for smoking | ||||||
| Zhang et al. 2013 Australia[37] | 43 randomized and 19, 12 completed at Wk 8, Mo 3. | Specific auricular acupressure group Acupoints: Hunger, Liver, Lung, Mouth, Shenmen; Manipulation: acupuncturists administered. Beads pressed ≥3 times/day when feeling craving, 8 Wks | Nonspecific acupressure group Acupoints: Clavicle, Helix 2, Occiput, Shoulder, Tooth; Same manipulation | N/A | Daily cigarette consumption, withdrawal symptoms, Smoking cessation rate: NS | Discomfort on ears (TG: 1; CG: 4); Headache, dizziness (CG: 1) |
| TG: n = 20; 12 F, age 50y; CG: n = 23; 13 F, age 50y; | ||||||
| Inclusion: smoking>1-year and >10 cigarettes/day; >18 years; no co-intervention for smoking; no auricular acupuncture last year | ||||||
| Baccetti et al. 2015 Italy[38] | 477 randomized and 472, 447, 445 at Wk 5, Mo 6, Year 1. | 1. Body acupuncture, auricular acupressure plus psychological support group 2. Body acupuncture, auricular acupressure group Acupoints: Pharmacopuncture: 1% lidocaine solution injected into LI20, auricular Zero; Plum-blossom needle: C7 to T5, 0.5, 1.5 and 3Cun from the vertebral spinous processes; Auricular acupressure: Shenmen; Manipulation: medical doctors administered, 5 Wks. Plum-blossom needle 3 times/session. Vaccaria seeds acupressure≥8 times/day when feeling craving, 30 min/session. Group 1 started after the 3rd psychological meeting, group 2 started immediately; Psychological support group: 1.5 hours/time, 9 times/5 Wks | Sham body acupuncture, auricular acupressure plus psychological support group Acupoints: Pharmacopuncture: 0.2cc lidocaine solution pricked below LI20 and Zero; Plum-blossom needle: C7 to T5, 2, 4 and 6 Cun from the vertebral spinous processes; Auricular acupressure: 0.5 cm from Shenmen; Manipulation: needles without tips for plum-blossom treatment | N/A | Smoking cessation rate: NS | Minor bleeding |
| TG1: n = 159, 102 F, age 51y; TG2: n = 162, 103 F, age 50y; CG: n = 156, 100 F, age 48y; | ||||||
| Inclusion: smoking ≥1-year and ≥10 cigarettes/day; >18 years; Italian speaker; no co-intervention for smoking | ||||||
| Hypertension | ||||||
| Macklin et al. 2006 USA[39] | 192 randomized and 188 completed at Wk 10, Mo 12. | 1. Individualized auricular-body acupuncture group Acupoints: prescribed individually; 2. Standardized auricular-body acupuncture at preselected points group Body acupoints: GB20, LI11, LR3, SP6, ST36; Auricular acupoints: Heart, Jiangyagou; Manipulation: acupuncturists administered. Neutral needle stimulation, 30 mins/session, Twice/Wk, 10 Wks | Sham group Body acupoints: 5 which are not acupoints; Auricular acupoints: Darwin’s tubercle, Ear lobe; Manipulation: no manipulation, 10 Wks | No antihypertensive medications | SBP, DBP: NS | Hypertensive urgencies (TG2: 2); congestive heart failure (CG: 1) |
| TG1: n = 64, 30 F, age 57y; TG2: n = 64, 35 F, age 56y; CG: n = 64, 35 F, age 53y; | ||||||
| Inclusion: stable BP: 140/90-179/109mmHg after 8–31 days suspension of antihypertensive medications; ≥18 years; no acupuncture within 6-Mo | ||||||
| Flachskampf et al. 2007 Germany[48] | 160 randomized and 140, 140, 135, 133 completed at Day 3, Wk 6, Mos 3, 6. | Body acupuncture group Acupoints: prescribed individually; Manipulation: acupuncturists administered. 20 mins/session, 22 sessions/6 Wks | Non-specific acupuncture group Acupoints: GB31, GB32, GB34, SI7, etc.; Same manipulation | Maintain antihypertensive medication before study | SBP, DBP: Significant within-group effect—TG (after treatment); Significant between-group effect—TG>CG (after treatment, 3-day F/U) | Pain, atrial fibrillation (TG); pain (CG) |
| TG: n = 72, 33 F, age 59y; CG: n = 68, 40 F, age 58y; | ||||||
| Inclusion: stable BP: 140/90-220/115mmHg; 45–75 years | ||||||
| Yin et al. 2007 Korea[44] | 41 randomized and 30 completed. | Body acupuncture plus exercise group Acupoints: (1) BL25, LI11, ST36 for tonification of the large intestine meridian; (2) BL13, LU9, SP3 for the lung meridian; (3) KI2, KI7, RN4 for the kidney meridian; (4) DU14, GB20, LI1 for the bladder meridian; Manipulation: physicians administered. Needle stimulation until Deqi. 17 sessions, 8 Wks; Exercise: breathing exercise 10 mins/day, walking 30 mins/day, 8 Wks | Sham acupuncture plus exercise group Same acupoints; Manipulation: until Deqi, withdrawn immediately | Maintain antihypertensive medication before study | SBP, DBP: Significant within-group effect—TG; Significant between-group effect—TG>CG (4th-8th Wk) | Bleeding on needle removal (TG: 8) |
| TG: n = 15, 11 F; CG: n = 15, 10 F; | ||||||
| Inclusion: SBP: 120-179mmHg or DBP: 80-99mmHg; SBP: 140-179mmHg or DBP: 90-99mmHg with antihypertensive medications | ||||||
| Zhang et al. 2008 USA[41] | 47 randomized and 45 completed (14 F, age 25y). | Laser body acupuncture group Acupoints: LI4, LI11; Manipulation: 40 infrared laser, 10kHz frequency, 8 mins/session, twice/Wk, 12 sessions | Sham group Same acupoints/manipulation; No activated laser beam | N/A | SBP, DBP: Significant within-group effect—TG | N/A |
| TG: n = 23; CG: n = 22; | ||||||
| Inclusion: SBP: 125-160mmHg and/or DBP: 81-110mmHg; no previous laser therapy use | ||||||
| Zhang et al. 2009 USA[42] | 27 randomized and completed (age 25y). | Body electroacupuncture group Acupoints: LI4, LI11; Manipulation: 100Hz frequency, 15 mins/acupoint/session, Twice/Wk, 5 Wks | Sham group Same acupoints/manipulation; No electric stimulation | Maintain diet, exercise, antihypertensive medications | SBP: Significant within-group effect—TG | N/A |
| TG: n = 13; 5 F; CG: n = 14; 5 F; | ||||||
| Inclusion: SBP: 120-165mmHg; DBP: 80-110mmHg; no co-intervention for hypertension | ||||||
| Kim et al. 2012 Korea[40] | 33 randomized and 28 completed. | Body acupuncture group Acupoints: PC6, ST36; Manipulation: Korean medicine practitioners administered. Needle stimulation until Deqi. 20 mins/session, twice/Wk, 8 Wks | Sham group Acupoints: 1cm from PC6, ST36; Manipulation: no manipulation | No antihypertensive medications during the treatment | Nighttime DBP: Significant within-group effect—TG; Significant between-group effect—TG>CG | Slight injection-site pain, small bleeding (TG) |
| TG: n = 12; CG: n = 16; | ||||||
| Inclusion: SBP: 140-159mmHg or DBP: 90-99mmHg; 18–70 years; no previous antihypertensive medication use | ||||||
| Chen et al. 2013 China[46] | 32 randomized and 30 completed (16 F, age 57y). | Body acupuncture group Acupoints: DU20, DU23, EX-HN1, LI4, LI11, LR3, PC6, SP6, ST9, ST36; Manipulation: acupuncturists administered. Needle stimulation until Deqi. 30 mins/session, 5 days | No intervention group | Maintain antihypertensive medications before study | SBP, DBP: NS | N/A |
| TG: n = 15; CG: n = 15; | ||||||
| Inclusion: SBP≥140mmHg and DBP≥90mmHg without medication; 30–75 years; no acupuncture last year | ||||||
| Sriloy et al. 2015 India[49] | 46 randomized and 38 completed. | Auricular-body acupuncture group Body acupoints: DU20, HT7, LR3, ST36; Auricular acupoint: Shenmen; Manipulation: naturopaths administered. Needle stimulation until Deqi. 20 mins/session | Slow breathing group | N/A | DBP: Significant within-group effect—TG; | N/A |
| TG: n = 19, 4 F, age 48y; CG: n = 19, 6 F, age 50y; | SBP: Significant within-group effect—CG | |||||
| Inclusion: diagnosed hypertension≥3 years; 35–60 years; no previous acupuncture use | ||||||
| Li et al. 2015 USA[43] | 65 randomized and 64, 20 completed at Wk 8, Mo 3. | Body electroacupuncture group Acupoints: PC5, PC6, ST36, ST37; Manipulation: 2-5Hz frequency, 30 mins/session, Weekly, 8 Wks | Non-specific acupuncture group Acupoints: LI6, LI7, GB37, GB39; Same manipulation | N/A | SBP: Significant between-group effect—TG>CG (after treatment, 1-Mo F/U); | None |
| TG: n = 33, 17 F, age 58y; CG: n = 32, 18 F, age 54y; | DBP: NS | |||||
| Inclusion: SBP/DBP≥140-180/90–99mmHg; no antihypertensive medications within 3-day before enrolment | ||||||
| Liu et al. 2015 Korea[45] | 30 randomized and 26 completed at Wks 8, 12. | Body acupuncture group Acupoints: LI11, LR3, PC6, SP4, ST36; Manipulation: needle stimulation until Deqi. 20 mins/session, twice/Wk, 8 Wks | No intervention group | N/A | SBP: Significant within-group effect—TG (after treatment, 4Wk F/U); | None |
| TG: n = 15, 12 F, age 49y; CG: n = 15, 11 F, age 53y; | DBP: Significant within-group effect—TG (after treatment); | |||||
| Inclusion: SBP: 120–159 mmHg or DBP: 80–99 mmHg; 20–65 years; no co-intervention for hypertension; no acupuncture within 6-Mo | SBP, DBP: Significant between-group effect—TG> CG (after treatment, 4Wk F/U) | |||||
| Lin et al. 2016 Taiwan[50] | 80 randomized and completed. | Body acupressure group Acupoints: LR3; Manipulation: press 5 seconds and release 1 second, 30 times | Sham group Acupoints: 1inch from LR3; Same manipulation | N/A | SBP, DBP: Significant within-group effect—TG; Significant between-group effect—TG>CG (immediately, 15-/30-min after acupressure) | N/A |
| TG: n = 40, 20 F, age 59y; CG: n = 40, 20 F, age 63y; | ||||||
| Inclusion: SBP: 150-180mmHg; 40–75 years; no antihypertensive medication within 2h before enrolment | ||||||
| Zhan et al. 2016 China[47] | 174 patients randomized and completed. | 1. Laser body acupuncture plus musical group 2. Laser body acupuncture group Acupoints: LI11, LR3 for liver fire hyperactivity syndrome; KI3, SP6 for yin-deficiency and yang-hyperactivity syndrome; ST36, ST40 for excessive phlegm-dampness syndrome; KI3, RN4 for yin-yang deficiency syndrome; Manipulation: 30 mins/session, daily; 30 days. Group 1: listening to music while laser stimulation (650nm wavelength, 0.5cm diameter). Group 2: needle stimulation until Deqi | Starch tablets 25 mg/tablet, 1 tablet/time, 3 times/day before meal, 30 days | N/A | SBP, DBP: Significant within-group effect—TG1 & TG2; Significant between-group effect—TG1>CG; TG2>CG | N/A |
| TG1: n = 58, 33 F, age 50y; TG2: n = 58, 31 F, age 50y; CG: n = 58, 34 F, age 50y; | ||||||
| Inclusion: SBP: 140-159mmHg and/or DBP: 90-99mmHg; 25–69 years; BMI: 18–30 kg/m2; no previous antihypertensive drugs (or stopped ≥2 Wks) | ||||||
| Obesity | ||||||
| Richards & Marley 1998 Australia[51] | 60 randomized and 50 completed. | Auricular acupuncture group Acupoints: Shenmen, Stomach; Manipulation: acuSlim device. 15–20 mins/session, twice/daily, 4 Wks | Sham group Acupoints: thumb (no acupoints); Same manipulation | Maintain diet | Weight loss ≥2kg, suppression of appetite: Significant between-group effect—TG>CG | N/A |
| TG: n = 28, age 44y; CG: n = 32, age 43y; | ||||||
| Inclusion: BW<120kg; >18 years; stable BW≥3 Mos; no co-intervention for obesity | ||||||
| Mazzoni et al. 1999 Italy[52] | 40 randomized and 22 completed. | Auricular-body acupuncture moxibustion group Acupoints: Sessions 1–3, Moxibustion: BL14, BL15, BL20; body acupoints: DU20, HT9, RN14, RN17, SP1; auricular acupoints: Hunger, Stomach; Sessions 4–8, body acupoints: BL10, BL60, LR13, RN12, RN15, SP7, ST36; auricular acupoints: Hunger, Stomach; Sessions 9–12, body acupoints: DU20, RN14, SJ10, ST40, ST44; auricular acupoints: Shenmen; Manipulation: acupuncturist administered. Weekly, 12 Wks | Sham group Body acupoints: 3mm from the real acupoints; Manipulation: superficial insertion (3-5mm), 12 Wks | No medications for obesity; restricted saturated fats and snacks; daily abdominal self-massage 30–45 minutes | BMI, suppression of appetite: NS | N/A |
| TG: n = 20, 16 F, age 37y; CG: n = 20, 17 F, age 40y; | ||||||
| Inclusion: BMI>30kg/m2; 18–60 years; no other disorders or treatments determining weigh gain | ||||||
| Wei & Liu 2004 China[53] | 195 randomized and completed (187 F, age 36y). | Auricular-body acupuncture group Body acupuncture: Acupoints: LI4, LI11, ST36, ST37, ST44 for excess-heat in stomach and intestines syndrome (syndrome 1); RN6, RN12, SP6, SP9, ST36, ST40 for damp retention due to spleen deficiency syndrome (syndrome 2); BL23, KI6, RN4, SJ6 for kidney qi insufficiency syndrome (syndrome 3); BL18, GB43, LR3, LR8 for liver qi stagnation syndrome (syndrome 4); Auricular acupuncture: Acupoints: Endocrine, Hunger, Lung, Shenmen (syndrome 1); Endocrine, Lung, Spleen, Stomach (syndrome 2); Endocrine, Kidney, Lung, Triple energizers (syndrome 3); Endocrine, Liver, Shenmen (syndrome 4); Manipulation: 30 mins/session, every two-day, 12 sessions | 1. Body acupuncture group Same with the body acupuncture treatment; 2. Auricular acupuncture group Same with the auricular acupuncture treatment; Same manipulation | N/A | Weight loss≥3kg: Significant between-group effect—TG>CG1; TG>CG2 | N/A |
| TG: n = 76; CG1: n = 64; CG2: n = 55; | ||||||
| Inclusion: BMI>25kg/m2 (F)/26kg/m2 (M); no co-intervention for obesity | ||||||
| Hsu et al. 2005 Taiwan[54] | 72 randomized and 63 completed. | Body electroacupuncture group Acupoints: KI14, RN6, RN9, SP6, ST26, ST28, ST40; Manipulation: 42Hz frequency to maximal tolerable intensity. Needle stimulation until Deqi. 40 mins/session, twice/Wk, 6 Wks | 1. Sit-up exercises group 10 times/day, 6 Wks 2. No intervention group | Maintain diet | BW, BMI, WC: Significant between-group effect—TG>CG1; TG>CG2 | Mild ecchymosis (n = 3); abdominal discomfort (n = 1) |
| TG: n = 22, age 40y; CG1: n = 20, age 41y; CG2: n = 21, age 41y; | ||||||
| Inclusion: WC>90cm; female; BMI>30kg/m2; 16–65 years; no co-intervention for obesity within 3-Mo and the study | ||||||
| Elder et al. 2007 USA[55] | 92 randomized and 73 completed. | 1. Qigong group Shaking (5 minutes), Movements (18 minutes), harvest the energy method (5 minutes), 24 Wks; 2. Body Tapas acupressure technique group Acupoints: BL1, EX-HN3, GB21; Manipulation: acupuncturists administered. 1 min/session, daily, 24 Wks | Self-directed support Written materials and maintenance support groups, 24 Wks | N/A | Weight loss of 2.8kg: Significant between-group effect—TG2>TG1 | None |
| TG1: n = 31, 26 F, age 48y; TG2: n = 30, 27 F, age 48y; CG: n = 31, 26 F, age 46y; | ||||||
| Inclusion: BMI: 25–35 kg/m2 (F)/25–40 kg/m2 (M); weight change<10 pounds within 6-Mo; 18–80 years; no co-intervention for obesity within 6-Mo; no previous complementary medicine use; no other disorders determining weigh gain; alcohol<21 drinks/Wk | ||||||
| Hsieh 2007 Taiwan[56] | 70 randomized and 55 completed. | Auricular acupressure group Acupoints: Endocrine, Mouth, Shenmen, Small intestine, Stomach; Manipulation: Japanese magnetic pearl acupressure. 10 mins/session, Weekly, 8 Wks | Sham group Same acupoints; Acupressure tape only | Education on low-calorie diet; maintain physical activity | BMI: Significant within-group effect—TG | N/A |
| TG: n = 27, 24 F; CG: n = 28, 26 F; | ||||||
| Inclusion: BMI≥23kg/m2; 18–20 years; Asian ethics | ||||||
| Yeh & Yeh 2008 Taiwan[57] | 38 randomized and completed. | Auricular acupressure group Acupoints: Endocrine, Mouth, Shenmen, Small intestine, Stomach; Manipulation: beads acupressure before meals, 15 mins/session, Weekly, 9 Wks | No intervention group | Maintain diet, physical activity | WC, HC: Normal weigh participants Significant within-group effect—TG & CG; Obese participants: NS | None |
| TG: n = 19, 16 F, age 33y; CG: n = 19, 16 F, age 33y; | ||||||
| Inclusion: BMI≥27 kg/m2 (obese)/<27 kg/m2 (normal weight); 22–50 years; no acupuncture for obesity within 1-Mo | ||||||
| Nourshahi et al. 2009 Iran[58] | 27 randomized and completed. | 1. Exercise plus low-calorie diet group 3 sessions/Wk, 8 Wks; 2. Auricular-body acupuncture, exercise plus low-calorie diet group Auricular acupoints: Hunger, Shenmen; Body acupoint: ST40; Manipulation: acupuncturists administered. 8 Wks. Body acupuncture 20 mins/session; Lentil seeds auricular acupressure 10 times/30 mins before meals and whenever feeling hungry | No intervention group | N/A | BMI, fat mass: Significant between-group effect—TG1>CG; TG2>CG | N/A |
| TG1: age 42y; TG2: age 40y; CG: age 37y; | ||||||
| Inclusion: fat mass>30%; female | ||||||
| Hsu et al. 2009 Taiwan[59] | 60 randomized and 45 completed. | Auricular acupuncture group Acupoints: Endocrine, Hunger, Shenmen, Stomach; Manipulation: acupuncturists administered. Twice/Wks, 6 Wks | Sham group Same acupoints/manipulation; Needles without tips | Maintain diet | BW, BMI, WC: NS | Minor inflammation (TG: 1); tenderness (TG: 7; CG: 2) |
| TG: n = 23, age 40y; CG: n = 22, age 39y; | ||||||
| Inclusion: BMI >27kg/m2; female; 16–65 years; no co-intervention for obesity within 3-Mo and the study | ||||||
| Hsieh et al. 2010, 2011, 2012 Taiwan[60,61,65] | 84 randomized and 68 completed. | 1. Auricular acupressure (Japanese magnetic pearl) group 2. Auricular acupressure (Vaccaria seeds) group Auricular acupoints: Endocrine, Mouth, Shenmen, Small intestine, Stomach; Manipulation: 10 mins/session/Wk, 8 Wks | Sham group Same acupoints/manipulation; Acupressure tape only | Education on low-calorie diet; maintain physical activity | BMI: Significant within-group effect—TG1 & TG2; | N/A |
| TG1: n = 27, 24 F; TG2: n = 29, 26 F; CG: n = 28, 26 F; | BW, WC: Significant within-group effect—TG1, TG2, & CG; Significant between-group effect—TG2>TG1; | |||||
| Inclusion: WC≥80cm (F)/90cm (M); BMI>23kg/m2; 18–20 years | Waist-to-hip ratio: Significant within-group effect—TG1 & TG2 | |||||
| Rerksuppaphol & Rerksuppaphol 2011 Thailand[62] | 45 randomized and completed. | Body TEAS group Acupoints: RN4, RN6, RN10, RN12, SP15, ST25, ST28; Manipulation: acupuncturists administered. Electrodes with 40Hz frequency, 30 mins/session, twice/Wk, 8 Wks | Body electroacupuncture group Same acupoints; Manipulation: disposable needles with 40Hz frequency, 30 mins/session, twice/Wk, 8 Wks | Maintain diet, exercise, medication for obesity | Weight loss, BMI: Significant within-group effect—TG | None |
| TG: n = 23, age 34y; CG: n = 22, age 33y; | ||||||
| Inclusion: BMI>23kg/m2; WC>80cm; female; >15 years; no co-intervention for obesity | ||||||
| Rerksuppaphol 2012 Thailand[63] | 40 randomized and 29 completed. | Body TEAS plus auricular acupressure group Body acupoints: RN4, RN6, RN10, RN12, SP15, ST25, ST28; Auricular acupoints: Shenmen, Hungry, Stomach; Manipulation: acupuncturists administered. Electrodes with 40Hz frequency, 30 mins/session, twice/Wk, 8 Wks | Auricular acupressure group Same acupoints; Manipulation: magnetic pellets acupressure. Self-stimulation, 10 times/session, 3 sessions/day before meals, 8 Wks | Maintain diet, exercise | BW, BMI, WC, waist-to-hip ratio: Significant within-group effect—TG; | N/A |
| TG: n = 20, age 41y; CG: n = 20, age 32y; | BW, BMI: Significant between-group effect—TG>CG | |||||
| Inclusion: BMI>23kg/m2; female; >15 years; no other medications for obesity | ||||||
| Lien et al. 2012 Taiwan[64] | 90 randomized and 71 completed. | 1. Auricular acupuncture group 2. Auricular acupressure group Acupoints: Endocrine, Hunger, Shenmen, Stomach; Manipulation: acupuncturists administered. Beads acupressure 3 sessions/Wk, 4 Wks | Sham acupuncture group Same acupoints/manipulation; Needles without tips | Maintain diet, lifestyle | BW, BMI, WC: Significant within-group effect—TG1 & TG2 | Dizziness (TG1: 1). |
| TG1: n = 24, age 39y; TG2: n = 24, age 42y; CG: n = 23, age 41y; | ||||||
| Inclusion: BMI≥27kg/m2; female; 16–60 years; no co-intervention for obesity within 2-Mo; no previous auricular acupuncture | ||||||
| Darbandi et al. 2012 Iran[66] | 90 randomized and 86, 84 completed at Wk 6, Mo 2. | Auricular acupressure group Acupoints: Centre of ear, Hunger, Mouth, Sanjiao, Shenmen, Stomach; Manipulation: acupuncturists administered. Vaccaria seed acupressure before meals, 6 Wks | Non-specific acupressure group Acupoints: Hip, Nose, Oesophagus, Spleen; Manipulation: plasters without seeds, 6 Wks | Low-calorie diet | BW, BMI: Significant within-group effect—TG & CG (after treatment) | None |
| TG: n = 43, 37 F, age 38y; CG: n = 43, 37 F, age 38y; | ||||||
| Inclusion: BMI: 25-45kg/m2; 18–55 years; no co-intervention for obesity; no medications for obesity within 3-Mo | ||||||
| Abdi et al. 2012 Iran[67] | 196 randomized and 161 completed at Wks 6, 12. | Body acupuncture group Acupoints: GB28, RN4, RN9, RN12, SP6, ST25. For excess syndromes, LI11, ST40 added; For deficiency syndromes, RN6, SP9 added; Manipulation: acupuncturists administered. Needle stimulation until Deqi. GB28, ST25 applied with electricity at 30-40Hz frequency. 20 mins/session, twice/Wk, 6 Wks | Sham group Acupoints: on the RN meridian, 0.3cm from the real acupoints; Manipulation: superficial needling. Disconnected electric lines | Low-calorie diet | BW, BMI, HC: Significant within-group effect—TG & CG (after treatment, 6Wk F/U); | None |
| TG: n = 79, age 37y; CG: n = 82, age 37y; | WC: Significant within-group effect—TG (after treatment, 6Wk F/U), CG (after treatment) | |||||
| Inclusion: same with Darbandi et al. 2012 | ||||||
| He et al. 2012 China[68] | 60 randomized and completed (age 34y). | Auricular acupressure plus exercise group Acupoints: Endocrine, Hunger, Large intestine, Shenmen, Spleen, Stomach; Manipulation: vaccariae seed acupressure, 10 seconds/time, 3 times/day, 4 Wks | Exercise group Heart rates at 120–150 beats/min, 1 hour/day, 4 Wks | Low-calorie diet; no food after 8PM | BW, BMI, WC: Significant within-group effect—TG & CG; | N/A |
| TG: n = 30; CG: n = 30; | BW: Significant between-group effect—TG>CG | |||||
| Inclusion: BMI≥25kg/m2; WC≥80cm; female; 18–60 years; no medical/drug use for obesity within 2-Mo | ||||||
| Guo et al. 2014 China[69] | 64 randomized and 61 completed (32 F, age 37y). | Body electroacupuncture plus diet group Acupoints: RN4, RN12, SP6, SP9, ST25, ST36, ST40; Manipulation: 1400kcal/diet. 2Hz frequency stimulation, 30 mins/session, daily, 45 days | Diet group 1400kcal/diet. 45 days | N/A | BW: Significant within-group effect—TG & CG | N/A |
| TG: n = 32; CG: n = 32; | ||||||
| Inclusion: BMI ≥28kg/m2 (obese); >18 years | ||||||
| Wu et al. 2014 China[70] | 72 randomized and 65 completed. | Body acupuncture group Acupoints: SP4, SP6, SP8, SP9, SP10, SP14, SP15; Manipulation: acupuncture at 9-11AM. Needle stimulation until Deqi. 30 mins/session, daily, 30 days | Sham group Same acupoints; Manipulation: acupuncture at any time beyond 9-11AM | N/A | BW, BMI, WC, HC: Significant within-group effect—TG & CG | N/A |
| TG: n = 36, age 28y; CG: n = 36, age 28y; | ||||||
| Inclusion: BMI≥25kg/m2; 18–65 years; WC≥80cm (F)/90cm (M); TCM syndrome of spleen deficiency and exuberant dampness; no drug within 6-Mo; no co-intervention for obesity | ||||||
| Kim et al. 2014 Korea[71] | 58 randomized and 49 completed. | Auricular acupressure group Acupoints: Endocrine, Mouth, Shenmen, Small intestine, Stomach; Manipulation: salba seeds acupressure 30 minutes before meals, 5 sec/point, 10 times/point, 3 times/day, 1 Mo | No information | N/A | BW, BMI: Significant within-group effect—TG & CG; Significant between-group effect—TG>CG | N/A |
| TG: n = 25, age 21y; CG: n = 24, age 21y; | ||||||
| Inclusion: BMI≥25kg/m2; female; no previous medication; no co-intervention for obesity | ||||||
| Yeo et al. 2014 Korea[72] | 91 randomized and 58 completed. | Auricular acupuncture group 1 Acupoints: Endocrine, Hunger, Shenmen, Spleen, Stomach; Auricular acupuncture group 2 Acupoint: Hunger; Manipulation: Korean medicine practitioners administered. 8 Wks | Sham group Acupoints: same with TG1; Manipulation: needles removed immediately after insertion, 8 Wks | Low-calorie diet; no extra exercise | BW, BMI: Significant between-group effect—TG1>CG; TG2>CG; | N/A |
| TG1: n = 31, 25 F, age 35y; TG2: n = 30, 25 F, age 39y; CG: n = 30, 25 F, age 43y; | WC: Significant between-group effect—TG1>CG | |||||
| Inclusion: BMI≥23kg/m2; >19 years; daily ambulatory time<2h; stable weight; no co-intervention for obesity within 6-Mo; no addiction to alcohol | ||||||
| Schukro et al. 2014 Austria[73] | 56 randomized and 45, 42 completed at Wks 6, 10. | Auricular electroacupuncture group Acupoints: Colon, Hunger, Stomach; Manipulation: 1Hz frequency. 7AM-11AM, 4 days/Wk, 6 Wks | Sham group Same acupoints/manipulation; No electric stimulation | N/A | BW, BMI: Significant between-group effect—TG>CG (after treatment, 4Wk F/U) | Skin irritations (n = 8) |
| TG: n = 28, age 54y; CG: n = 28, age 50y; | ||||||
| Inclusion: BMI>25kg/m2; female; >18 years; no previous acupuncture use | ||||||
| Darbandi et al. 2014 Iran[74] | 80 randomized and completed. | 1. Body electroacupuncture group Acupoints: same with Abdi et al 2012; Manipulation: acupuncturists administered. 30–40Hz frequency at a maximal tolerable intensity, 20 mins/session, twice/Wk, 6 Wks; 2. Auricular electroacupuncture group Acupoints: Center of ear, Hungry, Mouth, Sanjiao, Shenmen, Stomach; Manipulation: vaccaria seeds acupressure before meals, twice/Wk, 6 Wks | 1. Sham body electroacupuncture group Acupoints: 0.5cun from the real acupoints; Manipulation: superficial insertion. No electric stimulation; 2. Sham auricular electroacupuncture group Acupoints: Esophagus, Hip, Nose, Spleen; Manipulation: plasters without seeds | Low-calorie diet | BMI: Significant between-group effect—TG1>CGs1, 2; TG2>CGs1, 2; | None |
| TG1: n = 20, age 38y; TG2: n = 20, age 39y; CG1: n = 20, age 38y; CG2: n = 20, age 38y; | HC: Significant between-group effect—TG1>CGs1, 2; TG2>CGs1, 2; TG2>TG1; | |||||
| Inclusion: BMI: 30–40kg/m2; male; 18–50 years; no medications for obesity within 3-Mo | WC: Significant between-group effect—TG1>CGs1, 2; TG2>CG2; TG1>TG2 | |||||
| Yeh et al. 2015 Taiwan[75] | 134 randomized and 70 completed (35 F). | Auricular electroacupuncture & acupressure group Acupoints: Endocrine, Hunger, Shenmen, Stomach; Manipulation: researchers administered. 10 Wks. Needle stimulation until Deqi. 2-100Hz frequency, 20 mins/session, Weekly; Vaccariae seeds acupressure 1 min/point, 4 times/day | Non-specific acupuncture group Acupoints: Ankle, Clavicle, Elbow, Shoulder; Same manipulation | Nutrition counselling | BMI: Significant within-group effect—TG & CG | N/A |
| TG: n = 36, age 30y; CG: n = 34, age 33y; | ||||||
| Inclusion: BMI≥27kg/m2; WC≥80cm (F)/90cm (M); 18–50 years; no medication/surgery use for obesity within 3-Mo | ||||||
| He et al. 2015 China[76] | 56 randomized and completed. | Body acupuncture plus massage group Acupoints: LI11, RN6, RN12, SJ6, SP6, SP15, ST21, ST25, ST36; Manipulation: acupuncturists administered. Needle stimulation until Deqi. 30 mins/session, daily, 21 days; Massage: stomach Meridian, Ren Meridian, Dai Meridian (abdomen), 25 mins/session, daily, 21 days | Body acupuncture group Same acupoints/manipulation | Maintain diet; no physical training or exercise | BW, BMI: Significant within-group effect—TG & CG | N/A |
| Inclusion: BMI≥25kg/m2; female; no previous drug use | ||||||
| Jiao et al. 2015 China[77] | 48 randomized and completed. | Body electroacupuncture plus running group Acupoints: SP6, ST36; Manipulation: 50Hz frequency, 45 mins/session, daily, 6 Wks; Running: 45 mins/day, 6 Wks | Running group 45 mins/day, 6 Wks | No overeating | Fat mass: NS | N/A |
| TG: n = 24, age 35y; CG: n = 24, age 36y; | ||||||
| Inclusion: BMI>28kg/m2; male | ||||||
aAdd-on strategy of all the intervention groups.
Wk: Week; TG: treatment group; CG: Control group; F: Female; Age, mean age; Mo: Month; DSM-III-R, Diagnostic and Statistical Manual of Mental Disorders IIIR; NS, not statistically significant; N/A, not available; F/U: follow-up; ICD-10, International Statistical Classification of Diseases and Related Health Problems 10th Revision; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders 4thed; NRT, nicotine replacement therapy; FTND, Fagerstrom Test for Nicotine Dependence; TEAS, transcutaneous electric acupoint stimulation; PHQ-9, 9-item Patient Health Questionnaire; BP, blood pressure; SBP, systolic blood pressure; DBP, diastolic blood pressure; BW, body weight; BMI, body mass index; WC, waist circumference; HC, hip circumference; M: male.
Data syntheses
Cochrane RevMan version 5.3 software was employed to conduct meta-analysis of the outcome measures and heterogeneity was determined using I2 statistic [15]. The meta-analysis included all studies where acupuncture was employed with or without co-interventions, provided that such intervention was given to all groups. However, meta-analyses were conducted only if at least two RCTs were available exploring a specific outcome of a risk factor. Acupuncture approaches shown in the meta-analysis include needle acupuncture (body, aural region, electroacupuncture), laser acupuncture, and acupressure. Analyses were performed separately for type of experimental interventions (acupuncture, acupressure, laser acupuncture, or the combination of acupuncture and acupressure) according to the RCT design. Random effects model (Mantel-Haenszel for dichotomous/categorical variables and inverse variance for continuous variables) was used to calculate mean differences (MD), standardized mean differences (SMD), or risk ratios (RR), and 95% confidence intervals (CI) were reported. Sensitivity analyses were used to test the robustness of statistically significant results for RCTs with low risk versus high risk of bias for the domains selection bias and performance/detection bias. Effects sizes of acupuncture compared to other interventions were shown in Table 3.
Table 3. Effect sizes of acupuncture in comparison to sham acupuncture or no treatment.
| Outcome | RCT number | Participant number | Heterogeneity (I2;Chi2;p) |
Subgroup difference (95% confidence interval) |
p (sub-group effect) |
|
|---|---|---|---|---|---|---|
| Experimental group | Control group | |||||
| Smoking-dependence risk factor—Daily cigarette consumption | ||||||
| Acupressure VS Sham intervention | 2 [36,37] | 58 | 55 | 0%;0.45;0.50 | MD = -2.75 cigarette/day (-5.33, -0.17) | 0.04 |
| Smoking-dependence risk factor—Smoking withdrawal symptoms | ||||||
| Acupuncture VS Sham intervention | 3 [26,33,35] | 89 | 89 | 90%;19.8;<0.001 | SMD = -0.95 (-2.17,0.26) | 0.12 |
| Smoking-dependence risk factor—Smoking cessation rate (short-term) | ||||||
| Acupuncture VS Sham intervention | 3 [26,27,33] | 205 | 205 | 0%;0.70;0.71 | RR = 1.11 (0.85, 1.46) | 0.44 |
| Acupressure VS Sham intervention | 2 [36,37] | 58 | 55 | 0%;0.19;0.66 | RR = 0.39 (0.08, 1.96) | 0.26 |
| Acupuncture plus acupressure VS Sham intervention | 2 [23/24,38] | 179 | 180 | 66%;2.96;0.09 | RR = 2.51 (0.26, 24.24) | 0.43 |
| Smoking-dependence risk factor—Smoking cessation rate (long-term) | ||||||
| Acupuncture VS Sham intervention | 2 [26,33] | 51 | 49 | 0%;0.52;0.47 | RR = 1.13 (0.40, 3.21) | 0.82 |
| Acupressure VS Sham intervention | 2 [36,37] | 49 | 40 | 0%;0;0.95 | RR = 2.43 (0.40, 14.66) | 0.33 |
| Acupuncture plus acupressure VS Sham intervention | 2 [24,38] | 164 | 170 | 22%;1.28;0.26 | RR = 1.97 (0.67, 5.80) | 0.22 |
| Hypertension risk factor—Systolic blood pressure | ||||||
| Acupuncture VS Sham intervention | 2 [40,48] | 84 | 84 | 78%;4.59;0.03 | MD = -0.54 mmHg (-10.69, 9.60) | 0.92 |
| Hypertension risk factor—Diastolic blood pressure | ||||||
| Acupuncture VS Sham intervention | 2 [40,48] | 84 | 84 | 0%;0.89;0.35 | MD = -1.38 mmHg (-4.06, 1.31) | 0.32 |
| Obesity risk factor—Body weight | ||||||
| Acupuncture VS No treatment | 2 [54,69] | 54 | 53 | 50%;1.99;0.16 | MD = -1.12 kg (-5.51, 3.27) | 0.62 |
| Acupressure VS No treatment | 2 [57,71] | 44 | 43 | 32%;1.47;0.23 | MD = -2.87 kg (-6.47, 0.74) | 0.12 |
| Acupuncture VS Sham intervention | 4 [59,64,67,72] | 157 | 157 | 0%;0.73;0.87 | MD = -2.66 kg (-6.05, 0.72) | 0.12 |
| Acupressure VS Sham intervention | 2 [64,66] | 67 | 66 | 0%;0.41;0.52 | MD = -1.01 kg (-4.55, 2.52) | 0.57 |
| Obesity risk factor—Body mass index | ||||||
| Acupressure VS No treatment | 2 [57,71] | 44 | 43 | 49%;1.95;0.16 | MD = -0.41 kg/m2 (-1.56, 0.73) | 0.48 |
| Acupuncture VS Sham intervention | 5 [59,64,67,72,74] | 177 | 177 | 18%;4.88;0.30 | MD = 0.12 kg/m2 (-0.88, 1.13) | 0.81 |
| Acupressure VS Sham intervention | 2 [64,66] | 67 | 66 | 0%;0.26;0.61 | MD = -0.44 kg/m2 (-1.65, 0.78) | 0.48 |
| Obesity risk factor—Waist circumference | ||||||
| Acupuncture VS Sham intervention | 5 [59,64,67,72,74] | 177 | 177 | 0%;1.61;0.81 | MD = -2.79 cm (-4.13, -1.46) | <0.001 |
aMD: Mean difference. SMD: standardized mean difference; RR: risk ratio; I2: the percentage of variation across studies that is due to heterogeneity; Chi2: chi-square test.
Quality assessment
Two authors (DS and WP) independently assessed the risk of bias of all included studies using the Cochrane Risk of Bias Tool for selection bias (random sequence generation and allocation concealment), performance bias (blinding of participants and personnel), detection bias (blinding of outcome assessment), attrition bias (incomplete outcome data), reporting bias (selective outcome reporting), and other bias (Table 4). Disagreements were assessed by a third author. It is worth noting that, due to methodological reasons and the uniqueness of acupuncture treatments, it is not feasible to blind the acupuncturist in acupuncture RCTs. Therefore, we adopted the domain of performance bias and only focused on adequate participant blinding.
Table 4. Risk of bias of the included studies using the Cochrane Risk of Bias Tool.
| Reference | Risk factor | Random sequence generation | Allocation concealment | Blinding of participants and personnela | Blinding of outcome assessment | Incomplete outcome data | Selective reporting | Other bias |
|---|---|---|---|---|---|---|---|---|
| Rampes et al., 1997, UK [21] | Alcohol | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | Low risk |
| Sapir-Weise et al., 1999, Sweden [20] | Alcohol | Unclear | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear |
| Bullock et al., 2002, USA [22] | Alcohol | Low risk | High risk | High risk | Low risk | High risk | Low risk | Unclear |
| Karst et al., 2002, Germany [19] | Alcohol | Unclear | Unclear | Low risk | Low risk | Unclear | Low risk | Unclear |
| Trumpler et al., 2003, Switzerland [18] | Alcohol | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| Kunz et al., 2007, Germany [17] | Alcohol | Unclear | Unclear | High risk | Unclear | High risk | Low risk | High risk |
| Lee et al., 2015, Korea [16] | Alcohol | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Unclear |
| He et al., 1997, Norway [23,24] | Smoking | Low risk | High risk | Low risk | Unclear | Low risk | Low risk | Low risk |
| Waite & Clough, 1998, UK [25] | Smoking | Unclear | Unclear | Low risk | Unclear | High risk | Low risk | Low risk |
| White et al., 1998, UK [26] | Smoking | Low risk | Low risk | Low risk | Low risk | High risk | Low risk | Low risk |
| Georgiou et al., 1998, UK [27] | Smoking | Low risk | High risk | High risk | Low risk | High risk | Low risk | Low risk |
| Cai et al., 2000, Singapore [29] | Smoking | Low risk | High risk | Low risk | Low risk | High risk | Low risk | Low risk |
| Bier et al., 2002, USA [31] | Smoking | Low risk | High risk | Low risk | Low risk | High risk | High risk | Low risk |
| White et al., 2007, UK [28] | Smoking | Low risk | Low risk | High risk | High risk | High risk | Low risk | Unclear |
| Wu et al., 2007, Taiwan [33] | Smoking | Low risk | High risk | Unclear | Unclear | Low risk | Low risk | High risk |
| Yeh et al., 2009, Taiwan [34] | Smoking | Unclear | Unclear | Unclear | Unclear | Unclear | High risk | Low risk |
| Chae et al., 2010, Korea [35] | Smoking | Low risk | High risk | Unclear | Unclear | Unclear | Low risk | Low risk |
| Wing et al., 2010, Hong Kong [36] | Smoking | Low risk | High risk | Unclear | Unclear | High risk | Low risk | Low risk |
| Lambert et al., 2011, Singapore [30] | Smoking | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Fritz et al., 2013, USA [32] | Smoking | Low risk | Low risk | High risk | Low risk | High risk | Low risk | Low risk |
| Zhang et al., 2013, Australia [37] | Smoking | Low risk | Low risk | Low risk | Low risk | High risk | Low risk | Low risk |
| Baccetti et al., 2015, Italy [38] | Smoking | Low risk | High risk | Unclear | Unclear | High risk | Low risk | High risk |
| Macklin et al., 2006, USA [39] | Hypertension | Low risk | low risk | Low risk | Unclear | Low risk | Low risk | High risk |
| Flachskampf et al., 2007, Germany [48] | Hypertension | Low risk | Low risk | Low risk | Unclear | Low risk | Low risk | Unclear |
| Yin et al., 2007, Korea [44] | Hypertension | Low risk | High risk | Low risk | Low risk | High risk | Low risk | Low risk |
| Zhang et al., 2008, USA [41] | Hypertension | Low risk | High risk | Low risk | Unclear | Low risk | Low risk | Unclear |
| Zhang et al., 2009, USA [42] | Hypertension | Low risk | High risk | High risk | Low risk | Low risk | Low risk | High risk |
| Kim et al., 2012, Korea [40] | Hypertension | Low risk | Low risk | Low risk | Low risk | High risk | Low risk | Unclear |
| Chen et al., 2013, China [46] | Hypertension | Unclear | Unclear | High risk | Unclear | Unclear | High risk | Unclear |
| Sriloy et al., 2015, India [49] | Hypertension | Unclear | Low risk | High risk | Unclear | High risk | High risk | High risk |
| Li et al., 2015, USA [43] | Hypertension | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Liu et al., 2015, Korea [45] | Hypertension | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| Lin et al., 2016, Taiwan [50] | Hypertension | Low risk | Low risk | Unclear | Unclear | Low risk | Low risk | High risk |
| Zhan et al., 2016, China [47] | Hypertension | Low risk | High risk | High risk | Unclear | Low risk | Low risk | Unclear |
| Richards & Marley, 1998, Australia [51] | Obesity | Low risk | High risk | High risk | Unclear | High risk | Low risk | Low risk |
| Mazzoni et al., 1999, Italy [52] | Obesity | Unclear | Unclear | High risk | Low risk | High risk | Low risk | Low risk |
| Wei & Liu, 2004, China [53] | Obesity | Unclear | Unclear | High risk | Unclear | Low risk | Unclear | Unclear |
| Hsu et al., 2005, Taiwan [54] | Obesity | Low risk | High risk | High risk | Unclear | Low risk | Low risk | Low risk |
| Elder et al., 2007, USA [55] | Obesity | Unclear | Unclear | High risk | Low risk | High risk | High risk | Low risk |
| Hsieh, 2007, Taiwan [56] | Obesity | Unclear | Unclear | Unclear | Unclear | High risk | Low risk | Unclear |
| Yeh & Yeh, 2008, Taiwan [57] | Obesity | Low risk | High risk | High risk | High risk | Low risk | Low risk | High risk |
| Nourshahi et al., 2009, Iran [58] | Obesity | Unclear | Unclear | High risk | Unclear | Low risk | Low risk | Unclear |
| Hsu et al., 2009, Taiwan [59] | Obesity | Low risk | High risk | Low risk | Unclear | High risk | Low risk | Low risk |
| Hsieh, 2010, Taiwan [60,61,65] | Obesity | Unclear | Unclear | Unclear | Unclear | High risk | High risk | High risk |
| Rerksuppaphol & Rerksuppaphol, 2011, Thailand [62] | Obesity | Low risk | High risk | High risk | High risk | Low risk | Low risk | Low risk |
| Rerksuppaphol, 2012, Thailand [63] | Obesity | Low risk | High risk | High risk | Unclear | High risk | Low risk | High risk |
| Lien et al., 2012, Taiwan [64] | Obesity | Low risk | High risk | Low risk | Unclear | High risk | Low risk | Low risk |
| Darbandi et al., 2012, Iran [66] | Obesity | Low risk | High risk | Unclear | Unclear | Low risk | Low risk | Low risk |
| Abdi et al., 2012, Iran [67] | Obesity | Unclear | Unclear | Unclear | Unclear | High risk | Low risk | Low risk |
| He et al., 2012, China [68] | Obesity | Unclear | Unclear | High risk | Unclear | Low risk | Low risk | High risk |
| Guo et al., 2014, China [69] | Obesity | Unclear | Unclear | High risk | Unclear | Low risk | Low risk | High risk |
| Wu et al., 2014, China [70] | Obesity | Low risk | High risk | Low risk | Unclear | Low risk | Low risk | High risk |
| Kim et al., 2014, Korea [71] | Obesity | Low risk | High risk | High risk | Unclear | High risk | Low risk | Low risk |
| Yeo et al., 2014, Korea [72] | Obesity | Low risk | Low risk | High risk | Unclear | High risk | Low risk | High risk |
| Schukro et al., 2014, Austria [73] | Obesity | Low risk | High risk | High risk | Unclear | High risk | Low risk | Low risk |
| Darbandi et al., 2014, Iran [74] | Obesity | Low risk | High risk | High risk | High risk | Low risk | Low risk | Low risk |
| Yeh et al., 2015, Taiwan [75] | Obesity | Low risk | Low risk | low risk | Unclear | High risk | Low risk | High risk |
| He et al., 2015, China [76] | Obesity | Low risk | High risk | High risk | Unclear | Low risk | Low risk | High risk |
| Jiao et al., 2015, China [77] | Obesity | Low risk | High risk | High risk | Unclear | Low risk | Unclear | Unclear |
aBlinding of participants and personnel: We only focus upon the blinding of participants as blinding the acupuncturists in acupuncture treatments is impossible due to methodological reasons.
Results
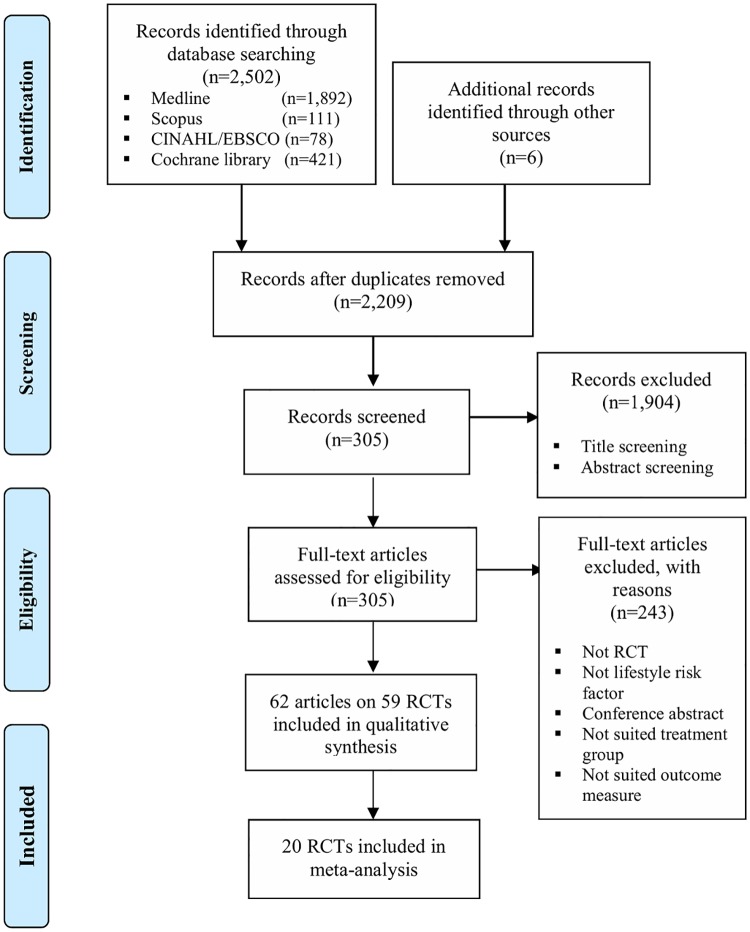
The key database searches identified 2,502 records with another six records from Google Scholar search, of which 299 duplicates were removed. After screening, the full texts of 305 papers were reviewed, of which a total of 62 full-text articles (reporting on 59 RCTs) were considered eligible and included in this systematic review. The PRISMA flowchart of literature search and article selection details has been shown in Fig 1.
Fig 1. PRISMA flowchart of literature search and study selection.
There were 59 RCTs (5,650 participants) regarding the use of acupuncture interventions in treating lifestyle risk factors for stroke, of which 7 RCTs for alcohol-dependence (845 participants), 15 RCTs for smoking-dependence (1,960 participants), 12 RCTs for hypertension (927 participants), and 25 RCTs for obesity (1,918 participants). No publication reported on a trial examining the efficacy of acupuncture for the lifestyle risk factor for stroke of high cholesterol or physical inactivity as a primary outcome.
Alcohol-dependence
Seven RCTs [16–22] focused on acupuncture treatments for alcohol-dependence using outcomes of alcohol craving (four RCTs), alcohol withdrawal symptoms (four RCTs), and drinking days (one RCT). Table 2 shows details of such RCTs’ characteristics and safety-related information. Most of the included studies defined alcohol-dependence according to the 3rd version (revised)/4th version of the Diagnostic and Statistical Manual of Mental Disorders (DSM) or the 10th version of the International Statistical Classification of Diseases and Related Health Problems (ICD) [16–21]. The sample size of RCTs focusing on alcohol-dependence ranged from 20 to 503 participants with only two studies recruiting more than 100 participants.
Psychiatrists/nurses [17,20], acupuncturists [18,22], and oriental medical doctors [16] were reported as administering the acupuncture interventions. The modes of acupuncture delivered within the interventions included both specific and nonspecific/symptom-based auricular acupuncture (five studies), body acupuncture (one study), and combined auricular and body acupuncture (one study). Acupuncture treatment sessions ranged from 30-minutes to 45-minutes. Only one RCT employed needle stimulation technique for the acupuncture treatment of alcohol-dependence [17].
Non-significant differences between acupuncture and control groups for alcohol craving were reported in three RCTs [16,17,20], alcohol withdrawal symptoms in two RCTs [17,18], and drinking days in one RCT [20]. Statistically significant within-intervention group effects were reported for alcohol craving with specific auricular electroacupuncture [21] and alcohol withdrawal symptoms with combined use of auricular and body acupuncture [19], while statistically significant between-group effects were reported for alcohol withdrawal symptoms with symptom-based auricular acupuncture (VS specific auricular acupuncture) [22].
Risk of bias assessment indicated that three RCTs did not report information on random sequence generation, four RCTs failed to apply blinding to participants and personnel, one did not report adequate blinding of outcome assessors, and three failed to report complete outcome data (Table 4). Due to the great heterogeneity regarding intervention details and outcomes applied in the RCTs focusing on alcohol-dependence, no meta-analysis could be conducted.
Smoking-dependence
Fifteen RCTs [23–38] focused on acupuncture treatments for smoking-dependence using outcomes of daily cigarette consumption (eight RCTs), smoking cessation rate (eight RCTs), smoking withdrawal symptoms (six RCTs), desire to smoke (two RCTs), cotinine concentrations (one RCT), and craving (one RCT). The details of such RCTs’ characteristics and safety-related information have been presented in Table 2. The majority of these RCTs defined smoking-dependence according to the number of cigarettes daily and/or smoking period [23–30,32–35,37–38]. The sample size of the RCTs ranged from 29 to 477 participants, with six RCTs recruiting more than 100 participants.
Acupuncturists were reported to administer the acupuncture intervention in seven RCTs [23,24,26,31–33,37], while physicians and researchers were reported to administer the acupuncture intervention in two RCTs [25,38] and one RCT [28], respectively. The modes of acupuncture delievered within the RCTs focusing on smoking-dependence included auricular acupuncture (four RCTs), auricular acupressure (three RCTs), body acupuncture (one RCT), TEAS (two RCTs), combined auricular acupuncture and auricular acupressure (two RCTs), combined auricular acupuncture, body acupuncture, and education (one RCT), combined auricular acupressure, body acupuncture, and psychological support (one RCT), and combined auricular acupuncture, body acupuncture, and auricular acupressure (one RCT). A total of 11 RCTs included acupuncture treatment follow-ups [24–29,31,33,36–38] and most ranged between 3 months to 9 months after the treatment. All electroacupuncture RCTs were conducted over 20-minutes (per session) with different stimulation frequency [23–26,32,34].
Study results reported statistically significant within-intervention group effects for (a) daily cigarette consumption with combined body electroacupuncture, auricular acupuncture and auricular acupressure [23,24], auricular acupuncture [33], combined auricular electroacupuncture and acupressure [34], auricular acupressure [36], (b) desire to smoke with combined body electroacupuncture, auricular acupuncture and auricular acupressure [23,24], and (c) smoking withdrawal symptoms with auricular acupuncture [33]. Statistically significant between-group effects were reported for (a) smoking cessation rate with combined body electroacupuncture, auricular acupuncture and auricular acupressure (VS non-specific acupuncture) [23,24], combined auricular electroacupuncture and acupressure (VS sham acupuncture) [25], combined auricular acupuncture, body acupuncture, and education (VS sham acupuncture plus education) [31], (b) daily cigarette consumption with combined body electroacupuncture, auricular acupuncture and auricular acupressure [23,24], combined auricular acupuncture, body acupuncture, and education [31], (c) desire to smoke with combined body electroacupuncture, auricular acupuncture and auricular acupressure [23,24], TEAS (VS sham TEAS) [30], and (d) smoking withdrawal symptoms with body acupuncture (VS non-specific acupuncture) [35].
Compared to sham acupuncture, meta-analyses demonstrated individuals receiving auricular acupressure for smoking-dependence reported lower numbers of consumed cigarettes per day (two RCTs, MD = -2.75 cigarettes/day; 95%CI: -5.33, -0.17; p = 0.04; heterogeneity: I2 = 0%; Chi2 = 0.45; p = 0.50). However, none of the effect of these two RCTs was robust against selection bias and performance/detection bias. Meta-analysis did not show evidence for post-intervention effect of acupuncture interventions on smoking withdrawal symptoms compared to sham acupuncture (three RCTs, SMD = -0.95; 95%CI: -2.17, 0.26; p = 0.12). In addition, no evidence from meta-analysis has been found with regards to post-intervention effect on smoking cessation rate compared to sham controls, including acupuncture (three RCTs, RR = 1.11; 95% CI: 0.85, 1.46; p = 0.44), auricular acupressure (two RCTs, RR = 0.39; 95% CI: 0.08, 1.96; p = 0.26), and acupuncture plus auricular acupressure (two RCTs, RR = 2.51; 95% CI: 0.26, 24.24; p = 0.43). There was also no evidence for long-term effect on smoking cessation rate, including acupuncture (two RCTs, RR = 1.13; 95% CI: 0.40, 3.21; p = 0.82), auricular acupressure (two RCTs, RR = 2.43; 95% CI: 0.40, 14.66; p = 0.33), and acupuncture plus auricular acupressure (two RCTs, RR = 1.97; 95% CI: 0.67, 5.80; p = 0.22), when compared to sham controls (Table 3). Risk of bias assessment indicated 13 RCTs applied random sequence generation while nine RCTs did not allocate concealment appropriately. Seven RCTs failed to report information on blinding of outcome assessment. Ten RCTs did not provide complete outcome data (Table 4).
Hypertension
Twelve RCTs [39–50] focused on acupuncture treatments for hypertension using outcomes of both SBP and DBP (12 RCTs), nighttime SBP and DBP (one RCT), daytime SBP and DBP (one RCT). See Table 2 for details of these RCTs’ characteristics and safety-related information. Most of these RCTs defined hypertension according to the [varied] upper and lower cut-off points of SBP and DBP levels with/without antihypertensive medication(s). The sample size of these RCTs ranged from 30 to 160 participants, and three of these studies recruited more than 100 participants.
Acupuncturists [39,46,48], physicians [44], Korean medicine practitioners [40], and naturopaths [49] administered acupuncture for hypertension. The modes of acupuncture delivered within the interventions included body acupuncture (eight RCTs), body acupressure (one RCT), combined body and auricular acupuncture (two RCTs), combined body acupuncture and music treatment (one RCT), and combined body acupuncture and exercise (one RCT). Four RCTs followed the effects of acupuncture interventions up to 12 months after treatment [39,43,45,48]. Seven RCTs using needle acupuncture employed stimulation techniques [39,40,44–47,49].
Both statistically significant within-intervention group and between-group effects were reported in five RCTs for (a) SBP as well as DBP levels with body acupuncture (VS non-specific acupuncture) [48], combined body acupuncture and exercise (VS sham acupuncture plus exercise) [44], combined laser body acupuncture with/without music treatment (VS starch tablets) [47], body acupressure (VS sham acupuncture) [50], (b) nighttime DBP level with body acupuncture (VS sham acupuncture) [40]. In addition, study results reported statistically significant within-intervention group effects for (a) SBP as well as DBP levels with laser acupuncture [41], (b) SBP level with body electroacupuncture [42], (c) DBP level with combined body and auricular acupuncture [49], and statistically significant between-group effect for SBP level with body electroacupuncture (VS sham acupuncture) [43].
Meta-analyses did not show evidence for neither post-intervention nor long-term effect of acupuncture interventions on SBP control (two RCTs on acupuncture, MD = -0.54 mmHg; 95%CI: -10.69, 9.60; p = 0.92) and DBP control (two RCTs on acupuncture, MD = -1.38 mmHg; 95%CI: -4.06, 1.31; p = 0.32) compared to sham acupuncture (Table 3). Risk of bias assessment indicated only six hypertension-focused RCTs blinded participants and personnel appropriately and seven RCTs did not report information on blinding of outcome assessment (Table 4).
Obesity
A total of 25 RCTs [51–77] focused on acupuncture treatments for obesity using outcomes of BMI (19 RCTs), BW (including weight loss) (18 RCTs), WC (11 RCTs), hip circumstance (four RCTs), eating suppression (two RCTs), waist-to-hip ratio (two RCTs), and fat mass (two RCTs). See Table 2 for details of the characteristics and safety-related information of these studies. Most of these RCTs defined obesity according to participants’ BMI with/without WC [52–57,59–77]. The sample size of these 25 RCTs ranged from 27 to 196 participants, and three of these studies recruited more than 100 participants.
Among the 11 obesity-focused RCTs that specified the personnel who administered acupuncture, acupuncturists were chosen in nine RCTs [52,55,58,59,62–64,66,67]. The modes of acupuncture delivered within the interventions included auricular acupressure (six RCTs), auricular acupuncture (four RCTs), body acupuncture (four RCTs), Tapas acupressure or TEAS (two RCTs), combined auricular acupuncture and auricular acupressure (one RCT), combined auricular and body acupuncture with/without other intervention(s) (ie. moxibustion, exercise, diet) (three RCTs), auricular acupressure with TEAS or exercise (two RCTs), and body acupuncture with exercise, diet, or massage (three RCTs). Three obesity-focused RCTs followed the effect of acupuncture interventions, from 10-weeks to 12-months after the treatment [66,67,73]. All the electroacupuncture/TEAS studies focusing on BW employed different stimulation frequency with varied treatment durations [54,58,62,63,67,69,70,73,75,77].
Study results reported statistically significant within-intervention group effects for all BW, BMI, and WC with auricular acupressure (BW [60,61,64–66,71]; BMI [56,60,61,64–66,71]; WC [60,61,64,65]), combined auricular acupressure and TEAS [63], combined auricular acupressure and exercise [68], and body acupuncture [67,70]. Additionally, study results reported statistically significant within-intervention group effects for both BW and BMI with TEAS [62] and combined body acupuncture and massage [76]. Statistically significant between-group effects were reported for all BW, BMI, and WC with auricular acupressure (BW [61,61,65,71]; BMI [71]; WC [60,61,65]), auricular acupuncture (BW [51,72,73]; BMI [72,73]; WC [54,74]), and body acupuncture (BW [54]; BMI [54,74]; WC [54,74]). Combined body acupuncture and auricular acupuncture with/without exercise and diet has also shown statistically significant between-group effects for BW [53] and BMI [58], respectively.
Relative to sham acupuncture, meta-analyses only found those receiving acupuncture interventions for obesity reported lower waist circumference (five RCTs, MD = -2.79 cm; 95% CI: -4.13, -1.46; p<0.001; heterogeneity: I2 = 0%; Chi2 = 1.61; p = 0.81). However, after excluding RCTs with other than low risks of selection and performance/detection bias, none of the effect remained statistically significant. In comparison with no treatment intervention, meta-analyses did not show evidence for post-intervention effect of acupuncture interventions on BW (two RCTs on acupuncture, MD = -1.12 kg; 95%CI: -5.51, 3.27; p = 0.62; two RCTs on auricular acupressure, MD = -2.87 Kg; 95%CI: -6.47, 0.74; p = 0.12). Meta-analyses also did not show evidence for post-intervention effect of auricular acupressure interventions on BMI (two RCTs, MD = -0.41 kg/m2; 95%CI: -1.56, 0.73; p = 0.48) compared to no treatment (Table 3). Risk of bias assessment was unclear in numerous obesity-focused RCTs due to a lack of detail in the publications. Specifically, nine RCTs did not report random sequence generation and allocation concealment information. Twelve RCTs failed to report complete outcome data. Fifteen RCTs did not blind participants and personnel and 20 RCTs did not provide information on blinding of outcome assessment (Table 4).
Discussion
This article reports the first systematic review of the effect of acupuncture interventions for lifestyle risk factors for stroke. A number of acupuncture techniques have been used for the management of these lifestyle risk factors and have yielded limited improvements in outcomes. No analysis can be conducted on RCTs focusing on alcohol-dependence and no evidence of the effect of acupuncture treatments on high blood pressure was shown based on meta-analysis. The meta-analysis showed individuals receiving auricular acupressure reported better outcomes in daily cigarette consumption than sham acupressure. Furthermore, acupuncture users have reported better outcomes in reducing waist circumference compared to sham acupuncture. No serious side effects occurred when using acupuncture on these four lifestyle risk factors. However, approximately half of the RCTs focusing on hypertension and obesity did not report safety information of acupuncture users. As such, acupuncture appears to be a relative safe treatment for the management of lifestyle risk factors for stroke.
Some evidence of the benefits of acupuncture and/or auricular acupressure was revealed for RCTs of lifestyle risk factors for stroke—smoking-dependence and obesity—in our review. However, a total of eight and 14 types of acupuncture-related interventions have been examined in RCTs focusing on smoking-dependence and obesity, respectively. The findings reported here highlighted the gaps in the evidence of clinical acupuncture use in the specific field of lifestyle risk factors for stroke and generally. Consistent with findings of prior systematic reviews [9,78], acupuncture involves a range of techniques. Both acupuncture-associated clinical trials and observational studies are required to determine methodology issues such as the use of acupuncture only, acupressure only, or the combination of acupuncture and acupressure, and the further choices of acupuncture like needle acupuncture, electroacupuncture and laser acupuncture. Therefore, future high-quality research is warranted to confirm our preliminary findings and provide robust effect estimates of acupuncture interventions for lifestyle risk factors for stroke.
In our review, approximately half of the RCTs focusing on smoking-dependence and obesity employed auricular acupressure alone or in combination with other acupuncture intervention(s). Acupressure is considered more practical (ease of application by patients themselves) with low cost, compared to other acupuncture treatments [79]. However, no consistent and convincing evidence has been found in this review on whether acupressure is effective for the management of overall lifestyle risk factors for stroke. As a result, there is insufficient evidence to conclude that the use of acupressure could improve the lifestyle risk factors for stroke and more studies are required.
Sham acupuncture is the most frequently employed comparison for acupuncture treatments in general [80] and among people with lifestyle risk factors for stroke which has been shown in our review. Although meta-analysis presented here reported statistically significant benefits of real acupuncture interventions regarding the management of the lifestyle risk factors of smoking-dependence and obesity than sham interventions, none of the effects of the RCTs included in the analyses was robust against potential selection, performance, and detection bias. In addition to the identified design challenges of acupuncture-associated RCTs regarding the choice of control group with the fact that sham acupuncture may also trigger physiological effect [81], future acupuncture-associated RCTs should avoid high risk of bias from lack of allocation concealment and missing outcome data, persuade original investigators to provide sufficient information on blinding of outcome ascertainment and if necessary, choose an appropriate comparable control intervention for clinical acupuncture research.
Some limitations of our systematic review are worth noting. The acupuncture interventions varied greatly across the RCTs of each lifestyle risk factor for stroke included in this review in terms of inclusion criteria of participants, acupuncture forms, acupoint selection, manipulation methods, and frequency/duration of the treatments. Also, this systematic review was restricted to RCTs published in English-language peer-reviewed journals. Furthermore, a proportion of included studies were not registered before they were published, we therefore cannot rule out the possibility of reporting or publication bias. The findings in this systematic review regarding the effect of acupuncture for lifestyle risk factors for stroke should be interpreted with caution. However, compared to previous Cochrane and systematic reviews [9,12,13,82], based on the risk of bias evaluation (Table 4), the methodological quality of RCTs on acupuncture treatments identified in our review has improved over recent years, including regards to random sequence generation application, the reporting of acupuncture treatments, and use of long-term follow-ups.
Conclusion
This review shows no convincing evidence regarding the effect of acupuncture, acupressure, laser acupuncture or their combination use for lifestyle risk factors for stroke. However, the translation of findings of this systematic review may contribute to the evidence-base of potential clinical practice guideline recommendations for stroke prevention.
Supporting information
(DOC)
(PDF)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by the Nancy and Vic Allen Stroke Prevention Fund. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Cerniauskaite M, Quintas R, Koutsogeorgou E, Meucci P, Sattin D, Leonardi M, et al. Quality-of-life and disability in patients with stroke. Am J Phys Med Rehabil. 2012;91:S39–S47. 10.1097/PHM.0b013e31823d4df7 [DOI] [PubMed] [Google Scholar]
- 2.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Executive summary: heart disease and stroke statistics-2015 update. Circulation. 2015;131:434–441. [DOI] [PubMed] [Google Scholar]
- 3.Stroke Foundation. Stroke risk factors. 2017. https://strokefoundation.org.au/About-Stroke/Preventing-stroke/Stroke-risk-factors.
- 4.Gorelick PB. Stroke prevention. An opportunity for efficient utilization of health care resources during the coming decade. Stroke. 1994;25:220–224. [DOI] [PubMed] [Google Scholar]
- 5.Feigin VL, Norrving B, George MG, Foltz JL, Roth GA, Mensah GA. Prevention of stroke: a strategic global imperative. Nat Rev Neurol. 2016;12:501–512. 10.1038/nrneurol.2016.107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gee ME, Bienek A, Campbell NR, Bancej CM, Robitaille C, Kaczorowski J, et al. Prevalence of, and barriers to, preventive lifestyle behaviors in hypertension (from a national survey of Canadians with hypertension). Am J Cardiol. 2012;109:570–575. 10.1016/j.amjcard.2011.09.051 [DOI] [PubMed] [Google Scholar]
- 7.National Center for Complementary and Integrative Health. Acupuncture: In depth. 2016. https://nccih.nih.gov/health/acupuncture/introduction.
- 8.Langevin HM, Schnyer R, MacPherson H, Davis R, Harris RE, Napadow V, et al. Manual and electrical needle stimulation in acupuncture research: pitfalls and challenges of heterogeneity. J Altern Complement Med. 2015;21:113–128. 10.1089/acm.2014.0186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.White AR, Rampes H, Liu JP, Stead LF, Campbell J. Acupuncture and related interventions for smoking cessation. Cochrane Database Syst Rev. 2014;1:CD000009 10.1002/14651858.CD000009.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Center for Complementary and Integrative Health. Acupuncture research—areas of high and low programmatic priorities. 2015. https://nccih.nih.gov/grants/acupuncture/priorities.
- 11.Luo J, Xu H, Liu B. Real world research: a complementary method to establish the effectiveness of acupuncture. BMC Complement Altern Med. 2015;15:153 10.1186/s12906-015-0676-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee H, Kim SY, Park J, Kim YJ, Lee H, Park HJ. Acupuncture for lowering blood pressure: systematic review and meta-analysis. Am J Hypertens. 2009;22:122–128. 10.1038/ajh.2008.311 [DOI] [PubMed] [Google Scholar]
- 13.Belivani M, Dimitroula C, Katsiki N, Apostolopoulou M, Cummings M, Hatzitolios AI. Acupuncture in the treatment of obesity: a narrative review of the literature. Acupunct Med. 2013;31:88–97. 10.1136/acupmed-2012-010247 [DOI] [PubMed] [Google Scholar]
- 14.Chmielnicki B. Evidence based acupuncture: WHO official position. 2016. https://www.evidencebasedacupuncture.org/who-official-position/.
- 15.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee JS, Kim SG, Jung TG, Jung WY, Kim SY. Effect of Zhubin (KI9) acupuncture in reducing alcohol craving in patients with alcohol dependence: a randomized placebo-controlled trial. Chin J Integr Med. 2015;21:307–311. 10.1007/s11655-014-1851-1 [DOI] [PubMed] [Google Scholar]
- 17.Kunz S, Schulz M, Lewitzky M, Driessen M, Rau H. Ear acupuncture for alcohol withdrawal in comparison with aromatherapy: a randomized-controlled trial. Alcohol Clin Exp Res. 2007;31:436–442. 10.1111/j.1530-0277.2006.00333.x [DOI] [PubMed] [Google Scholar]
- 18.Trümpler F, Oez S, Stähli P, Brenner HD, Jüni P. Acupuncture for alcohol withdrawal: a randomized controlled trial. Alcohol Alcohol. 2003;38:369–375. [DOI] [PubMed] [Google Scholar]
- 19.Karst M, Passie T, Friedrich S, Wiese B, Schneider U. Acupuncture in the treatment of alcohol withdrawal symptoms: a randomized, placebo-controlled inpatient study. Addict Biol. 2002;7:415–419. 10.1080/1355621021000006017 [DOI] [PubMed] [Google Scholar]
- 20.Sapir-Weise R, Berglund M, Frank A, Kristenson H. Acupuncture in alcoholism treatment: a randomized out-patient study. Alcohol Alcohol. 1999;34:629–635. [DOI] [PubMed] [Google Scholar]
- 21.Rampes H, Pereira S, Mortimer A, Knowles M. Does electroacupuncture reduce craving for alcohol? A randomized controlled study. Complement Ther Med. 1997;5:19–26. [Google Scholar]
- 22.Bullock ML, Kiresuk TJ, Sherman RE, Lenz SK, Culliton PD, Boucher TA, et al. A large randomized placebo controlled study of auricular acupuncture for alcohol dependence. J Subst Abuse Treat. 2002;22:71–77. [DOI] [PubMed] [Google Scholar]
- 23.He D, Berg JE, Hostmark AT. Effects of acupuncture on smoking cessation or reduction for motivated smokers. Prev Med. 1997;26:208–214. 10.1006/pmed.1996.0125 [DOI] [PubMed] [Google Scholar]
- 24.He D, Medbø J, Høstmark A. Effect of acupuncture on smoking cessation or reduction: an 8-month and 5-year follow-up study. Prev Med. 2001;33:364–372. 10.1006/pmed.2001.0901 [DOI] [PubMed] [Google Scholar]
- 25.Waite NR, Clough JB. A single-blind, placebo-controlled trial of a simple acupuncture treatment in the cessation of smoking. Br J Gen Pract. 1998;48:1487–1490. [PMC free article] [PubMed] [Google Scholar]
- 26.White AR, Resch KL, Ernst E. Randomized trial of acupuncture for nicotine withdrawal symptoms. Arch Intern Med. 1998;158:2251–2255. [DOI] [PubMed] [Google Scholar]
- 27.Georgiou AJ, Spencer CP, Davies GK, Stamp J. Electrical stimulation therapy in the treatment of cigarette smoking. J Subst Abuse. 1998;10:265–274. [DOI] [PubMed] [Google Scholar]
- 28.White AR, Moody RC, Campbell JL. Acupressure for smoking cessation–a pilot study. BMC Complement Altern Med. 2007;7:8 10.1186/1472-6882-7-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cai Y, Zhao C, Wong Song U, Lei Z, Kean LS. Laser acupuncture for adolescent smokers-a randomized double-blind controlled trial. Am J Chin Med. 2000;28:443–449. 10.1142/S0192415X00000520 [DOI] [PubMed] [Google Scholar]
- 30.Lambert C, Berlin I, Lee TL, Hee SW, Tan AS, Picard D, et al. A standardized transcutaneous electric acupoint stimulation for relieving tobacco urges in dependent smokers. Evid Based Complement Alternat Med. 2011;2011:195714 10.1093/ecam/nen074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bier ID, Wilson J, Studt P, Shakleton M. Auricular acupuncture, education, and smoking cessation: a randomized, sham-controlled trial. Am J Public Health. 2002;92:1642–1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fritz DJ, Carney RM, Steinmeyer B, Ditson G, Hill N, Zee-Cheng J. The efficacy of auriculotherapy for smoking cessation: a randomized, placebo-controlled trial. J Am Board Fam Med. 2013;26:61–70. 10.3122/jabfm.2013.01.120157 [DOI] [PubMed] [Google Scholar]
- 33.Wu TP, Chen FP, Liu JY, Lin MH, Hwang SJ. A randomized controlled clinical trial of auricular acupuncture in smoking cessation. J Chin Med Asso. 2007;70:331–338. [DOI] [PubMed] [Google Scholar]
- 34.Yeh ML, Chang CY, Chu NF, Chen HH. A six-week acupoint stimulation intervention for quitting smoking. Am J Chin Med. 2009;37:829–836. 10.1142/S0192415X09007314 [DOI] [PubMed] [Google Scholar]
- 35.Chae Y, Kang OS, Lee HJ, Kim SY, Lee H, Park HK, et al. Effect of acupuncture on selective attention for smoking-related visual cues in smokers. Neurol Res. 2010;32 Suppl 1:27–30. [DOI] [PubMed] [Google Scholar]
- 36.Wing Y, Lee A, Wong E, Leung P, Zhang L, Pang ESY. Auricular acupressure for smoking cessation: a pilot randomized controlled trial. Med Acupunct. 2010;22:265–271. [Google Scholar]
- 37.Zhang AL, Di YM, Worsnop C, May BH, Da Costa C, Xue CC. Ear acupressure for smoking cessation: a randomised controlled trial. Evid Based Complement Alternat Med. 2013;2013:637073 10.1155/2013/637073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baccetti S, Monechi MV, Fre MD, Conti T, Faedda M, Panti P, et al. Smoking cessation with counselling and traditional Chinese medicine (TCM): a randomized controlled trial. Acupuncture and Related Therapies. 2015;3:48–54. [Google Scholar]
- 39.Macklin EA, Wayne PM, Kalish LA, Valaskatgis P, Thompson J, Pian-Smith MC, et al. Stop Hypertension with the Acupuncture Research Program (SHARP). Results of a randomized, controlled clinical trial. Hypertension. 2006;48:838–845. 10.1161/01.HYP.0000241090.28070.4c [DOI] [PubMed] [Google Scholar]
- 40.Kim HM, Cho SY, Park SU, Sohn IS, Jung WS, Moon SK, et al. Can acupuncture affect the circadian rhythm of blood pressure? A randomized, double-blind, controlled trial. J Altern Complement Med. 2012;18:918–923. 10.1089/acm.2011.0508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang J, Marquina N, Oxinos G, Sau A, Ng D. Effect of laser acupoint treatment on blood pressure and body weight—a pilot study. J Chiropr Med. 2008;7:134–139. 10.1016/j.jcm.2008.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang J, Ng D, Sau A. Effects of electrical stimulation of acupuncture points on blood pressure. J Chiropr Med. 2009;8:9–14. 10.1016/j.jcm.2008.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li P, Tjen-A-Looi SC, Cheng L, Liu D, Painovich J, Vinjamury S, et al. Long-lasting reduction of blood pressure by electroacupuncture in patients with hypertension: Randomized controlled trial. Med Acupunct. 2015;27:253–266. 10.1089/acu.2015.1106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yin C, Seo B, Park HJ, Cho M, Jung W, Choue R, et al. Acupuncture, a promising adjunctive therapy for essential hypertension: a double-blind, randomized, controlled trial. Neurol Res. 2007;29 Suppl 1:S98–S103. [DOI] [PubMed] [Google Scholar]
- 45.Liu Y, Park JE, Shin KM, Lee M, Jung HJ, Kim AR, et al. Acupuncture lowers blood pressure in mild hypertension patients: a randomized, controlled, assessor-blinded pilot trial. Complement Ther Med. 2015;23:658–665. 10.1016/j.ctim.2015.06.014 [DOI] [PubMed] [Google Scholar]
- 46.Chen H, Dai J, Zhang X, Wang K, Huang S, Cao Q, et al. Hypothalamus-related resting brain network underlying short-term acupuncture treatment in primary hypertension. Evid Based Complement Alternat Med. 2013;2013:808971 10.1155/2013/808971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhan HR, Hong ZS, Chen YS, Hong HY, Weng ZB, Yang ZB, et al. Non-invasive treatment to grade 1 essential hypertension by percutaneous laser and electric pulse to acupoint with music: A randomized controlled trial. Chin J Integr Med. 2016;22:696–703. 10.1007/s11655-016-2502-5 [DOI] [PubMed] [Google Scholar]
- 48.Flachskampf FA, Gallasch J, Gefeller O, Gan J, Mao J, Pfahlberg AB, et al. Randomized trial of acupuncture to lower blood pressure. Circulation. 2007;115:3121–3129. 10.1161/CIRCULATIONAHA.106.661140 [DOI] [PubMed] [Google Scholar]
- 49.Sriloy M, Nair P, Pranav K, Sathyanath D. Immediate effect of manual acupuncture stimulation of four points versus slow breathing in declination of blood pressure in primary hypertension-A parallel randomized control trial. Acupuncture and Related Therapies. 2015;3:15–18. [Google Scholar]
- 50.Lin GH, Chang WC, Chen KJ, Tsai CC, Hu SY, Chen LL. Effectiveness of acupressure on the Taichong acupoint in lowering blood pressure in patients with hypertension: a randomized clinical trial. Evid Based Complement Alternat Med. 2016;2016:1549658 10.1155/2016/1549658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Richards D, Marley J. Stimulation of auricular acupuncture points in weight loss. Australian Family Physician. 1998;27 Suppl 2:S73–S77. [PubMed] [Google Scholar]
- 52.Mazzoni R, Mannucci E, Rizzello SM, Ricca V, Rotella CM. Failure of acupuncture in the treatment of obesity: a pilot study. Eat Weight Disord. 1999;4:198–202. [DOI] [PubMed] [Google Scholar]
- 53.Wei Q, Liu Z. Treatment of simple obesity with auricular acupuncture, body acupuncture and combination of auricular and body acupuncture. Chinese Journal of Clinical Rehabilitation. 2004;8:4357–4359. [Google Scholar]
- 54.Hsu CH, Hwang KC, Chao CL, Chang HH, Chou P. Electroacupuncture in obese women: a randomized, controlled pilot study. J Womens Health. 2005;14:434–440. [DOI] [PubMed] [Google Scholar]
- 55.Elder C, Ritenbaugh C, Mist S, Aickin M, Schneider J, Zwickey H, et al. Randomized trial of two mind-body interventions for weight-loss maintenance. J Altern Complement Med. 2007;13:67–78. 10.1089/acm.2006.6237 [DOI] [PubMed] [Google Scholar]
- 56.Hsieh CH. Auricular acupressure for weight reduction in obese Asian young adults: a randomized controlled trial. Med Acupunct. 2007;19:181–184. [DOI] [PubMed] [Google Scholar]
- 57.Yeh CH, Yeh SC. Effects of ear points' pressing on parameters related to obesity in non-obese healthy and obese volunteers. J Altern Complement Med. 2008;14:309–314. 10.1089/acm.2007.0678 [DOI] [PubMed] [Google Scholar]
- 58.Nourshahi M, Ahmadizad S, Nikbakht H, Heidarnia MA, Ernst E. The effects of triple therapy (acupuncture, diet and exercise) on body weight: a randomized, clinical trial. Int J Obes. 2009;33:583–587. [DOI] [PubMed] [Google Scholar]
- 59.Hsu CH, Wang CJ, Hwang KC, Lee TY, Chou P, Chang HH. The effect of auricular acupuncture in obese women: a randomized controlled trial. J Womens Health. 2009;18:813–818. [DOI] [PubMed] [Google Scholar]
- 60.Hsieh CH. The effects of auricular acupressure on weight loss and serum lipid levels in overweight adolescents. Am J Chin Med. 2010;38:675–682. 10.1142/S0192415X10008147 [DOI] [PubMed] [Google Scholar]
- 61.Hsieh CH, Su TJ, Fang YW, Chou PH. Effects of auricular acupressure on weight reduction and abdominal obesity in Asian young adults: a randomized controlled trial. Am J Chin Med. 2011;39:433–440. 10.1142/S0192415X11008932 [DOI] [PubMed] [Google Scholar]
- 62.Rerksuppaphol L, Rerksuppaphol S. Efficacy of transcutaneous electrical acupoint stimulation compared to electroacupuncture at the main acupoints for weight reduction in obese Thai women. International Journal of Collaborative Research on Internal Medicine & Public Health. 2011;3:811–820. [Google Scholar]
- 63.Rerksuppaphol L. Efficacy of auricular acupressure combined with transcutaneous electrical acupoint stimulation for weight reduction in obese women. J Med Assoc Thai. 2012;95 Suppl 12:S32–S39. [PubMed] [Google Scholar]
- 64.Lien CY, Liao LL, Chou P, Hsu Ch. Effects of auricular stimulation on obese women: A randomized, controlled clinical trial. European Journal of Integrative Medicine. 2012;4:e45–e53. [Google Scholar]
- 65.Hsieh CH, Su TJ, Fang YW, Chou PH. Efficacy of two different materials used in auricular acupressure on weight reduction and abdominal obesity. Am J Chin Med. 2012;40:713–720. 10.1142/S0192415X1250053X [DOI] [PubMed] [Google Scholar]
- 66.Darbandi M, Darbandi S, Mobarhan MG, Owji AA, Zhao B, Iraji K, et al. Effects of auricular acupressure combined with low-calorie diet on the leptin hormone in obese and overweight Iranian individuals. Acupunct Med. 2012;30:208–213. 10.1136/acupmed-2011-010121 [DOI] [PubMed] [Google Scholar]
- 67.Abdi H, Zhao B, Darbandi M, Ghayour-Mobarhan M, Tavallaie S, Rahsepar AA, et al. The effects of body acupuncture on obesity: anthropometric parameters, lipid profile, and inflammatory and immunologic markers. Scientific World Journal. 2012;2012:603539 10.1100/2012/603539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.He W, Zhou Z, Li J, Wang L, Zhu B, Litscher G. Auricular acupressure plus exercise for treating primary obese women: A randomized controlled clinical trial. Med Acupunct. 2012;24:227–232. [Google Scholar]
- 69.Guo Y, Xing M, Sun W, Yuan X, Dai H, Ding H. Plasma nesfatin-1 level in obese patients after acupuncture: a randomised controlled trial. Acupunct Med. 2014;32:313–317. 10.1136/acupmed-2014-010530 [DOI] [PubMed] [Google Scholar]
- 70.Wu J, Li Q, Chen L, Tian D. Clinical research on using acupuncture to treat female adult abdominal obesity with spleen deficiency and exuberant dampness. J Tradit Chin Med. 2014;34:274–278. [DOI] [PubMed] [Google Scholar]
- 71.Kim D, Ham OK, Kang C, Jun E. Effects of auricular acupressure using Sinapsis alba seeds on obesity and self-efficacy in female college students. J Altern Complement Med. 2014;20:258–264. 10.1089/acm.2012.0283 [DOI] [PubMed] [Google Scholar]
- 72.Yeo S, Kim K, Lim S. Randomised clinical trial of five ear acupuncture points for the treatment of overweight people. Acupunct Med. 2014;32:132–138. 10.1136/acupmed-2013-010435 [DOI] [PubMed] [Google Scholar]
- 73.Schukro RP, Heiserer C, Michalek-Sauberer A, Gleiss A, Sator-Katzenschlager S. The effects of auricular electroacupuncture on obesity in female patients-a prospective randomized placebo-controlled pilot study. Complement Ther Med. 2014;22:21–25. 10.1016/j.ctim.2013.10.002 [DOI] [PubMed] [Google Scholar]
- 74.Darbandi M, Darbandi S, Owji AA, Mokarram P, Mobarhan MG, Fardaei M, et al. Auricular or body acupuncture: which one is more effective in reducing abdominal fat mass in Iranian men with obesity: a randomized clinical trial. J Diabetes Metab Disord. 2014;13:92 10.1186/s40200-014-0092-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yeh ML, Chu NF, Hsu MY, Hsu CC, Chuang YC. Acupoint stimulation on weight reduction for obesity: a randomized sham-controlled study. West J Nurs Res. 2015;37:1517–1530. 10.1177/0193945914548707 [DOI] [PubMed] [Google Scholar]
- 76.He J, Zhang X, Qu Y, Huang H, Liu X, Du J, et al. Effect of combined manual acupuncture and massage on body weight and body mass index reduction in obese and overweight women: a randomized, short-term clinical trial. J Acupunct Meridian Stud. 2015;8:61–65. 10.1016/j.jams.2014.08.001 [DOI] [PubMed] [Google Scholar]
- 77.Jiao C, Zhu X, Zhang H, Du X. EMP acupoint stimulation conducive to increase the effect of weight reduction through aerobic exercise. Int J Clin Exp Med. 2015;8:11317–11321. [PMC free article] [PubMed] [Google Scholar]
- 78.Zhang CS, Yang AW, Zhang AL, May BH, Xue CC. Sham control methods used in ear-acupuncture/ear-acupressure randomized controlled trials: a systematic review. J Altern Complement Med. 2014;20:147–161. 10.1089/acm.2013.0238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Au DW, Tsang HW, Ling PP, Leung CH, Ip PK, Cheung WM. Effects of acupressure on anxiety: a systematic review and meta-analysis. Acupunct Med. 2015;33:353–359. 10.1136/acupmed-2014-010720 [DOI] [PubMed] [Google Scholar]
- 80.World Health Organization. Acupuncture: review and analysis of reports on controlled clinical trials. 2002. http://www.iama.edu/OtherArticles/acupuncture_WHO_full_report.pdf.
- 81.Lewith G. The treatment of tobacco addiction. Complement Ther Med. 1995;3:142–145. [Google Scholar]
- 82.Cho SH, Whang WW. Acupuncture for alcohol dependence: a systematic review. Alcohol Clin Exp Res. 2009;33:1305–1313. 10.1111/j.1530-0277.2009.00959.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.