Abstract
Patients with diabetes are at a high risk of lower extremity amputations and may have a reduced life expectancy. Taiwan has implemented a diabetes pay-for-performance (P4P) program providing team care to improve the control of disease and avoid subsequent complications. Few studies investigated the effects of adopting a nationalized policy to decrease amputation risk in diabetes previously. Our study aimed to analyze the impact of the P4P programs on the incidence of lower extremity amputations in Taiwanese patients with diabetes.
This was a population-based cohort study using the Taiwan National Health Insurance Research Database (which provided coverage for 98% of the total population in Taiwan) from 1998 to 2007. Patients with diabetes were identified based on the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) diagnostic codes. We linked procedure codes to inpatient claims to identify patients hospitalized for nontraumatic lower extremity amputations.
A total of 9738 patients with diabetes with amputations were enrolled (mean age ± standard deviation: 64.4 ± 14.5 years; men: 63.9%). The incidence of nontraumatic diabetic lower extremity amputations decreased over the time period studied (3.79–2.27 per 1000 persons with diabetes). Based on the Cox proportional hazard regression model, male sex (hazard ratio: 1.83, 95% confidence interval [CI] 1.76–1.92), older age, and low socioeconomic status significantly interact with diabetes with respect to the risks of amputation. Patients who did not join the P4P program for diabetes care had a 3.46-fold higher risk of amputation compared with those who joined (95% CI 3.19–3.76).
The amputation rate in Taiwanese diabetic patients decreased over the time period observed. Diabetes in patients with low socioeconomic status is associated with an increased risk of amputations. Our findings suggested that in addition to medical interventions and self-management educations, formulate and implement of medical policies, such as P4P program, might have a significant effect on decreasing the diabetes-related amputation rate.
Keywords: amputations, diabetes, National Health Insurance, pay-for-performance
1. Introduction
People with diabetes are at an increased risk of lower extremity amputations and have a reduced life expectancy.[1] According to a 6.5-year follow-up cohort study to determine mortality, causes of death, and associated risk factors in patients with diabetes after lower extremity amputations, the mortality rate after lower extremity amputations in Taiwanese patients with diabetes is as high as 172.7 per 1000 patient-years, the median survival time was only 4.1 years; however, the most common cause of death was reported to be diabetes mellitus.[2] Nontraumatic lower extremity amputations in patients with diabetes is an important issue that is often overlooked. Lower extremity amputations impose a substantial cost burden to the patients, their families, and society-at-large.[3]
Data on the incidence of amputations can be obtained relatively easily but the figures require very careful interpretation, because there are many factors influencing the decision-making in amputations. Some of these factors include: disease severity, comorbidities, social and individual patient factors, quality of primary care, and prevailing medical opinion.[4]
Taiwan has implemented a pay-for-performance (P4P) program for patients with diabetes. This program rewards doctors, in part, on the basis of the outcome of their patients with diabetes, and has decreased the complications of diabetes since 2001.[5,6] The National Health Insurance of P4P is designed as an integrated team-care program, with the team members including doctors, nurses, dietitians, and other paramedical workers. Patients who join the program need to undergo physical examinations, biochemical tests, and health education regularly.[7] The P4P programs provide team care and recommend self-management education and support; help improve the control of disease; improve nutrient intake in patients with diabetes; and avoid subsequent complications of diabetes.[7,8] Previous studies have discussed the epidemiologic conditions,[9] clinical risk factors, and characteristics of amputations in patients with diabetes,[10,11] and some studies mention the impact of specific treatment, such as early debridement,[12] antibiotic use, multidisciplinary team care for diabetic foot treatment, etc.[13] However, only a few studies have investigated the effects of adopting a nationalized policy for integrating education and therapeutic programs to prevent and decrease amputation risk in patients with diabetes. The aim of our study was to analyze the impact of the P4P programs and comprehensive team care investigations on the incidence of lower extremity amputations in Taiwanese patients with diabetes.
2. Methods
2.1. Study subjects and data sources
This was a population-based cohort study conducted to estimate the incidence and hazard ratio (HR) of nontraumatic lower extremity amputations in Taiwanese patients with diabetes. A universal compulsory National Health Insurance (NHI) program was launched by the Taiwanese government in 1995.[14] About 96% of the total population enrolled in the NHI program,[15] and by the end of 2005, it provided a 98% coverage of the 23 million residents of Taiwan.[14] Those who did not enroll may live overseas.[15] The National Health Insurance Administration established all administrative and claims data in Taiwan, and provided de-identified individual information available to investigators for research purposes. We use the Taiwan NHI Research Database for the period from 1998 to 2007. This study has been approved by the research ethics committee in China Medical University and Hospital (IRB no: CMU-REC-101-012).
2.2. Definition of variables
Diabetes was identified by ICD-9-CM code 250 and A code A181. Based on previous studies, patients we enrolled had at least 1 hospital admission with a diagnostic code indicative of diabetes, or 3 or more outpatient visits with a diabetes-related diagnostic code (primary or secondary diagnostic codes of ICD-9-CM 250, and A codes of A181) within 365 calendar days.[14,16] The accuracy of the diabetes diagnoses was assessed based on the methods from a study that sampled 9000 patients. The patients had a diagnosis of diabetes in the NHI clams data, and confirmed based on patient responses to questionnaire items inquiring as to whether the patient had been informed of a diagnosis of diabetes, or if they had ever been prescribed/used oral hypoglycemic agents or insulin injections (sensitivity 96.9% and positive predictive value 93.9%, respectively).[14,16] We excluded patients diagnosed with diabetes prior to 1997, patients coded with gestational diabetes mellitus, neonatal diabetes mellitus, abnormal glucose tolerance tests, and where there was an uncertainty as to age or sex based on the records. All data sets could be interlinked using personal identification numbers that were unique to each patient. Demographic characteristics recorded were: age (years), sex (man/women), economic status (premium-based salary: separated to 8 groups), low-income household (Yes/No), presence of diabetic complications (7 classifications based on ICD-9 codes, and according to Hogan et al[3] and patients were subsequently stratified into 5 groups), environmental factors (average income of city households by quartile: low = lower than first quartile; middle = between first and third quartile; high = higher than third quartile), the degree of urbanization (graded from 0 to 8, according to the urban-rural gap grading scales, where level 1 indicates the most urbanized areas; level 2, the second most, etc). Level 0 is complete without a few urbanized areas, and in our study, we graded level 0 as level 8. The urbanization scoring was based on the standard classifications using indices such as population, economic activity, residential level, education, public health, environmental quality, family income in all districts,[17] and adopted by Directorate General of Budget, Accounting and Statistics, Taiwan. Primary care institution characteristics (main medical doctor was in the metabolism division: Yes/No; joining the P4P program for diabetes: Yes/No). We collected these variables for patients with nontraumatic lower extremity amputations prior to scheduling of the first amputation.
Nontraumatic lower extremity amputations were defined by amputations that occurred after diabetes was diagnosed. Using the personal identification number, we linked diabetes to inpatient claims (1998–2007) and identified the primary and secondary procedure codes as nontraumatic lower extremity amputations (ICD-9: 84.1 and 84.10–84.18). We excluded external causes of amputations as identified by E codes.
2.3. Statistical analysis
Descriptive data of the 5 dimensions, including demographic characteristics, economic conditions (premium-based salary and low-income households), diabetes complications, environmental factors (average income of city households by quartile and degree of urbanization), and primary care institutional characteristics (main medical doctor was in the metabolism division and joining the P4P program for diabetes or not) are presented as numbers and percentages. The Chi-squared test was used to assess if there were significant statistical differences between the variables in patients with and without amputations. Cox proportional hazard regression models were used to estimate the adjusted HR of lower extremity amputations after controlling for confounders, including demographic characteristics, economic conditions, diabetes complications, environmental factors, and primary care institutional characteristics. The follow-up duration was defined as occurring within the timeframe of 1998 to 2007. The primary end point was considered to be lower extremity amputation. The statistical analyses were performed using SAS (version 9.1; SAS Institute, Cary, NC), and P-values <.05 were considered statistically significant.
3. Results
3.1. Incidence of nontraumatic lower extremity amputations
Based on data from the Taiwan Health Insurance Database from 1998 to 2007 as depicted in Figure 1, there were 1,317,470 patients with diabetes whose data were screened for this study. A total of 9738 patients with diabetes with lower extremity amputations were enrolled (mean age: 64.4 ± 14.5 years, men: 63.9%). The mean age of diabetes diagnosis was 58.38 years with a mean follow-up duration of 5 years (Table 1). As shown in Figure 1 (year 1998: n = 2097, incidence: 3.79 per 1000 persons with diabetes; year 2007: n = 2580, incidence: 2.27 per 1000 persons with diabetes), the incidence of nontraumatic lower extremity amputations decreased by about 40% during the observation period.
Figure 1.
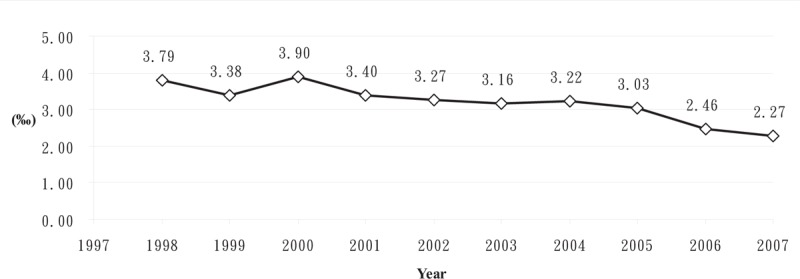
Incidence of nontraumatic lower extremity amputations from 1998 to 2007 in Taiwanese patients with diabetes.
Table 1.
Relative risks and factors associated with nontraumatic lower extremity amputations in patients with diabetes.
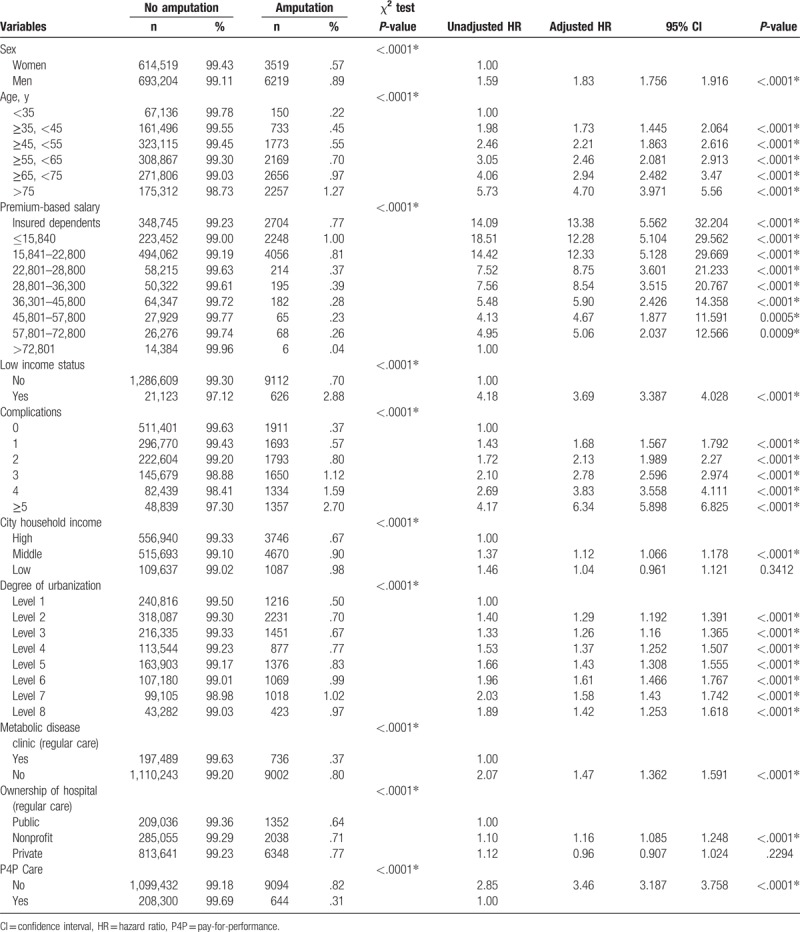
3.2. Characteristics of nontraumatic lower extremity amputations
The characteristics of nontraumatic lower extremity amputations in our study population are presented in Table 1. In summary, men, older age patients, those with low socioeconomic status, and those with more complications related to their diabetes had an increased risk of lower extremity amputations in our study population. Economic conditions also affected the risk of amputation. Patients who had lower incomes had higher amputation rates (the group with premium-based salary lower than New Taiwan Dollar [NT] $15,840 had the highest amputation rate at 1%). The average income of city households and degree of urbanization affected the risk of amputations. Different primary care institutional characteristics were related to nontraumatic lower extremity amputation rates. Patients with their main medical doctor in the metabolism division had lower amputation rates than those whose main medical doctor was not part of the metabolism division. Patients who joined the P4P program for diabetes had lower amputation rates. The Chi-squared test showed statistically significant differences between these variables (Table 1).
The Cox proportional hazard regression model indicated that these groups had increased risks of diabetes-related nontraumatic lower extremity amputations as presented in Table 1. Independent risk factors of amputations in diabetes including male sex, older patients, low socioeconomic status, greater number of complications of diabetes, urban-dweller with low household income, and lower urbanization areas. In addition to the geographic, socioeconomic and clinical characteristics, patients who did not join the P4P program for diabetes care had a 3.46-fold risk of amputation than did who joined (95% confidence interval 3.19–3.76).
4. Discussion
This study which evaluated about 98% of the total diabetic population in Taiwan, revealed that the incidence of nontraumatic lower extremity amputations among patients with diabetes decreases between 1998 and 2007. In addition to age and male sex, the results of our study revealed that there were statistically significant associations between economic condition, diabetes complications, environmental factors, and joining the P4P program for diabetic care, and a risk of diabetic nontraumatic lower extremity amputations. The relationship between the P4P programs for diabetic care and diabetic amputations has been largely unexplored.
The incidence of amputations may vary with race. According to a recent systemic review Databases (i.e., MEDLINE, Embase, psychINFO, AMED, CINAHL, ProQuest Nursing, and Allied Health) were searched and reported that the incidence rate of amputation were higher in patients with diabetes (94.24 per 100,000 people with diabetes) than those without diabetes (3.80 per 100,000 people without diabetes).[18] A hospital-based study of Canada evaluating patients discharged due to lower limb amputation from April, 2006, to March, 2012 reported that the average age-adjusted rate was 22.9 per 100,000 individuals, and the relative risk of diabetes-related lower limb amputations was 28.9.[19] A Chinese cohort study reported the overall amputation rate of patients with diabetic foot disease was 19.03%, and major and minor amputation rates were 2.1% and 16.9%.[20] Another hospital-based study of Chinese patients with diabetes revealed the overall amputation rate was 11.4% of inpatient with diabetic foot disease, and the incidences of minor amputation and major amputation were 5.4% and 6.0%, respectively.[21] A epidemiologic study of lower extremity amputations in Europe, North America, and East Asia exhibited that the highest amputation rates were in the Navajo population (43.9 per 100,000 population per year for first major amputation in men) and the lowest amputation rates were in Madrid, Spain (2.8 per 100,000 per year). The amputation incidence rose with age (especially over 60 years); it was higher in men than women, and diabetes was associated with between 25% and 90% of amputations.[22] Another study evaluated the ethnic differences in lower limb revascularization and amputation rates in England; it enrolled 90 million English hospital admissions between 2003 and 2009 and founded that age adjusted prevalence rate for amputation was 26/100,000 and South Asians experienced the lowest rate of both major lower limb amputation in England.[23]
A study using the NHI claim data evaluated the nontraumatic lower extremity amputation rate in Taiwan and reported that in patients with peripheral artery disease (including diabetic and nondiabetic patient populations), 14.3% of men and 7.4% of women had lower extremity amputations.[24] Another study using the NHI claim data enrolled a total of 500,868 patients with diabetes and 500,248 age- and sex-matched control subjects selected from the ambulatory care claim database (1997). Linking to inpatient claims (1997–2002) reported that the estimated incidence of nontraumatic lower extremity amputations in diabetic men was higher than in diabetic women. Compared to control subjects of the same age and sex, patients with diabetes had significantly increased relative HRs for nontraumatic lower extremity amputations.[25] A previous study enrolled 93,116 Taiwanese patients with diabetes. Of 256,036 patients identified from hospital and clinic databases with a diagnosis of diabetes between 1995 and 1998, 128,572 were randomly selected to be interviewed by telephone between 1995 and 2002. These findings showed that the prevalence of amputations was significantly higher among men than women in cases of type 2 diabetes (0.9% vs 0.7%).[26] A study analyzed the incidence and determined risk factors for of lower extremity amputations in patients with type 2 diabetes mellitus according to the data from the Taiwan National Health Insurance Research Database. The incidence of lower extremity amputations in the Taiwan diabetic population decreased from 2001 to 2010, and the risk factors for amputations were male sex, adult-onset diabetes, heart failure, micro- and macrovascular complications of diabetes, including diabetic neuropathy, retinopathy, peripheral arterial occlusive disease, and stroke.[11]
The possible risk factors for diabetes-related lower limb amputations, as reported in previous studies, include age, sex, educational attainment, renal function, hypertension, heart disease, duration of diabetes, micro- and macrocomplications of diabetes, and glycemic control.[27–29] It is widely known that peripheral arterial disease is an important risk factor for amputation, and the prevalence of peripheral arterial disease was significantly higher in men than in women,[30,31] and this may be one of the reasons why the male sex is associated with a higher risk of lower limb amputations. Many factors influence the decision of whether or not to remove a limb including disease severity, comorbidities, social and individual patient factors, quality of primary care, and prevailing medical opinion.[4] The reported amputation incidences are affected by the selected population, cultural issues, and the structure of health care.[4]
In this study, we evaluated the 5 dimensions including demographic characteristics (sex, age), disease comorbidities (complications of diabetes) and social and individual factors (premium-based salary, low-income households, average income city households by quartile, and degree of urbanization) and the structure of health care (main medical doctor was in the metabolism division, joining the P4P program for diabetes or not).
The Bureau of NHI has implemented P4P programs for diabetes mellitus, tuberculosis, breast cancer, cervical cancer, and asthma since 2001. The P4P program for diabetes care provides financial incentives for health care providers to increase the number of follow-up visits to include enhanced self-care education, diabetes-specific physical examinations such as eye examinations (once a year), and regular laboratory testing for renal function and hemoglobin A1C (four times per year).[6] Although the effects of the P4P programs is inconclusive, a study reported that P4P program for diabetes was associated with a significant increase in regular follow-up visits and significantly lower hospitalization costs.[6] The impact of P4P program on diabetes care and the related incidence of lower extremity amputations has not been discussed in previous studies. According to the results of our study, the P4P program might exert an effect on decreasing diabetes-related amputation rates (patients that did not join the P4P program for diabetes care had a 3.46-fold risk of amputation compared to those who did join). Previous studies have reported that patients who joined the P4P program had a lower risk of developing macrovascular complications of diabetes,[32] and vascular complications of diabetes increase the risk of amputation. The study provides the possible link between P4P and decreased amputation rates in patients with diabetes.
A recent systematic review stated that P4P programs may improve processes of care in ambulatory settings, but the positive associations with improved patient outcomes were limited.[33] Some studies founded that Taiwan's diabetes P4P program increased continuing care, and patients with diabetes with higher physician continuity had a lower HR of mortality.[7,34] P4P participants had higher physician continuity and a lower relative risk of mortality.[7,34] Another study conducted a systematic review and research to better understand the implementation factors that modify the effectiveness of P4P, and concluded that effective program measures should be aligned with organizational goals, undergo evaluation for the effect of implementation, and that the programs should change in response to outcome reports.[35] The designs of P4P programs are very complex and the effects may vary on the basis of their design, context, and implementation processes.[35] Our study reported the impact of the diabetic P4P program on lower extremity amputations in Taiwan and suggested that the P4P program might have a significant independent effect on decreasing diabetes-related amputation rate.
4.1. Limitations
There were several limitations in our study. First, this study analyzed the NHI research database, so those who were not insured could not be analyzed. In addition, we analyzed complications classifications based on ICD-9 codes, may be discrepancies with the actual situation, such as misspecification. Furthermore, because of the retrospective nature of the study, and obtaining all of the patient data from the NHI database, some important information such as lifestyle and health behaviors of the observed patients were not available.
5. Conclusion
Our study concluded that the amputation rate in Taiwanese patients with diabetes decreased over the time period observed. Male sex, older age, and lower socioeconomic status were associated with increasing risks of amputation. The P4P program might have exerted an effect on decreasing the amputation rate in patients with diabetes. Further studies are needed to address the full impact and cost-effectiveness of the P4P program for diabetes care and its effects on lower extremity amputations.
Acknowledgment
The authors are grateful for the National Health Research Institute providing the National Health Insurance Research Database for this study.
Author contributions
Conceptualization: Yi-Jing Sheen, Pei-Tseng Kung, Wei-Yin Kuo, Wen-Chen Tsai.
Data curation: Wei-Yin Kuo, Wen-Chen Tsai.
Formal analysis: Pei-Tseng Kung, Wei-Yin Kuo, Li-Ting Chiu, Wen-Chen Tsai.
Methodology: Wei-Yin Kuo, Li-Ting Chiu, Wen-Chen Tsai.
Project administration: Wei-Yin Kuo.
Resources: Wen-Chen Tsai.
Software: Wei-Yin Kuo, Li-Ting Chiu, Wen-Chen Tsai.
Validation: Pei-Tseng Kung, Li-Ting Chiu, Wen-Chen Tsai.
Writing – original draft: Yi-Jing Sheen.
Writing – review & editing: Yi-Jing Sheen, Pei-Tseng Kung, Wen-Chen Tsai.
Wen-Chen Tsai orcid: 0000-0002-9684-0789.
Footnotes
Abbreviations: CI = confidence interval, HR = hazard ratio, ICD-9-CM = International Classification of Diseases, 9th Revision, Clinical Modification, NHI = National Health Insurance, NT = New Taiwan Dollar, P4P = pay-for-performance.
This study was supported by grants from Taiwan National Science Council (NSC 98-2815-C-029-001-H) and China Medical University and Asia University (CMU105-ASIA-16).
The authors have no conflicts of interest to disclose.
References
- [1].Moxey PW, Hofman D, Hinchliffe RJ, et al. Epidemiological study of lower limb amputation in England between 2003 and 2008. Br J Surg 2010;97:1348–53. [DOI] [PubMed] [Google Scholar]
- [2].Tseng CH, Chong CK, Tseng CP, et al. Mortality, causes of death and associated risk factors in a cohort of diabetic patients after lower-extremity amputation: a 6.5-year follow-up study in Taiwan. Atherosclerosis 2008;197:111–7. [DOI] [PubMed] [Google Scholar]
- [3].Hogan P, Dall T, Nikolov P. Economic costs of diabetes in the US in 2002. Diabetes Care 2003;26:917–32. [DOI] [PubMed] [Google Scholar]
- [4].Jeffcoate WJ, van Houtum WH. Amputation as a marker of the quality of foot care in diabetes. Diabetologia 2004;47:2051–8. [DOI] [PubMed] [Google Scholar]
- [5].Chen TT, Chung KP, Lin IC, et al. The unintended consequence of diabetes mellitus pay-for-performance (P4P) program in Taiwan: are patients with more comorbidities or more severe conditions likely to be excluded from the P4P program? Health Serv Res 2011;46:47–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Lee TT, Cheng SH, Chen CC, et al. A pay-for-performance program for diabetes care in Taiwan: a preliminary assessment. Am J Manag Care 2010;16:65–9. [PubMed] [Google Scholar]
- [7].Yen SM, Kung PT, Sheen YJ, et al. Factors related to continuing care and interruption of P4P program participation in patients with diabetes. Am J Manag Care 2016;22:e18–30. [PubMed] [Google Scholar]
- [8].Chang RE, Lin SP, Aron DC. A pay-for-performance program in Taiwan improved care for some diabetes patients, but doctors may have excluded sicker ones. Health Aff (Millwood) 2012;31:93–102. [DOI] [PubMed] [Google Scholar]
- [9].Huang YY, Lin KD, Jiang YD, et al. Diabetes-related kidney, eye, and foot disease in Taiwan: an analysis of the nationwide data for 2000-2009. J Formos Med Assoc 2012;111:637–44. [DOI] [PubMed] [Google Scholar]
- [10].Cheng LJ, Chen JH, Lin MY, et al. A competing risk analysis of sequential complication development in Asian type 2 diabetes mellitus patients. Sci Rep 2015;5:15687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Lai YJ, Hu HY, Lin CH, et al. Incidence and risk factors of lower extremity amputations in people with type 2 diabetes in Taiwan, 2001–2010. J Diabet 2015;7:260–7. [DOI] [PubMed] [Google Scholar]
- [12].Hsu CR, Chang CC, Chen YT, et al. Organization of wound healing services: the impact on lowering the diabetes foot amputation rate in a ten-year review and the importance of early debridement. Diabetes Res Clin Pract 2015;109:77–84. [DOI] [PubMed] [Google Scholar]
- [13].Cahn A, Elishuv O, Olshtain-Pops K. Establishing a multidisciplinary diabetic foot team in a large tertiary hospital: a workshop. Diabetes Metab Res Rev 2014;30:350–3. [DOI] [PubMed] [Google Scholar]
- [14].Chang CH, Shau WY, Jiang YD, et al. Type 2 diabetes prevalence and incidence among adults in Taiwan during 1999-2004: a national health insurance data set study. Diabet Med 2010;27:636–43. [DOI] [PubMed] [Google Scholar]
- [15].Lu JF, Hsiao WC. Does universal health insurance make health care unaffordable? Lessons from Taiwan. Health Aff (Millwood) 2003;22:77–88. [DOI] [PubMed] [Google Scholar]
- [16].Lin CC, Lai MS, Syu CY, et al. Accuracy of diabetes diagnosis in health insurance claims data in Taiwan. J Formos Med Assoc 2005;104:157–63. [PubMed] [Google Scholar]
- [17].Tzen GH, Wu TW. Characteristics of organizational levels in Taiwan districts. Geographic Res 1986;12:287–323. [Google Scholar]
- [18].Dillon MP, Quigley M, Fatone S. A systematic review describing incidence rate and prevalence of dysvascular partial foot amputation; how both have changed over time and compare to transtibial amputation. Syst Rev 2017;6:230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Imam B, Miller WC, Finlayson HC, et al. Incidence of lower limb amputation in Canada. Can J Public Health 2017;108:e374–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Jiang Y, Ran X, Jia L, et al. Epidemiology of type 2 diabetic foot problems and predictive factors for amputation in China. Int J Low Extrem Wounds 2015;14:19–27. [DOI] [PubMed] [Google Scholar]
- [21].Fei YF, Wang C, Chen DW, et al. Incidence and risk factors of amputation among inpatients with diabetic foot [in Chinese]. Zhonghua Yi Xue Za Zhi 2012;92:1686–9. [PubMed] [Google Scholar]
- [22].Unwin N. Epidemiology of lower extremity amputation in centres in Europe, North America and East Asia. Br J Surg 2000;87:328–37. [DOI] [PubMed] [Google Scholar]
- [23].Ahmad N, Thomas GN, Chan C, et al. Ethnic differences in lower limb revascularisation and amputation rates. Implications for the aetiopathology of atherosclerosis? Atherosclerosis 2014;233:503–7. [DOI] [PubMed] [Google Scholar]
- [24].Chen JJ, Lee CH, Lin LY, et al. Determinants of lower extremity amputation or revascularization procedure in patients with peripheral artery diseases: a population-based investigation. Angiology 2010;62:306–9. [DOI] [PubMed] [Google Scholar]
- [25].Chen HF, Ho CA, Li CY. Age and sex may significantly interact with diabetes on the risks of lower-extremity amputation and peripheral revascularization procedures: evidence from a cohort of a half-million diabetic patients. Diabetes Care 2006;29:2409–14. [DOI] [PubMed] [Google Scholar]
- [26].Tseng CH. Prevalence of lower-extremity amputation among patients with diabetes mellitus: is height a factor? CMAJ 2006;174:319–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Resnick HE, Carter EA, Sosenko JM, et al. Incidence of lower-extremity amputation in American Indians: the Strong Heart Study. Diabetes Care 2004;27:1885–91. [DOI] [PubMed] [Google Scholar]
- [28].Shatnawi NJ, Al-Zoubi NA, Hawamdeh HM, et al. Predictors of major lower limb amputation in type 2 diabetic patients referred for hospital care with diabetic foot syndrome. Diabetes, metabolic syndrome and obesity. Biologics 2018;11:313–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Boyko EJ, Seelig AD, Ahroni JH. Limb- and person-level risk factors for lower-limb amputation in the prospective Seattle Diabetic Foot Study. Diabetes Care 2018;41:891–8. [DOI] [PubMed] [Google Scholar]
- [30].Criqui MH, Aboyans V. Epidemiology of peripheral artery disease. Circ Res 2015;116:1509–26. [DOI] [PubMed] [Google Scholar]
- [31].Cornejo Del Rio V, Mostaza J, Lahoz C, et al. Prevalence of peripheral artery disease (PAD) and factors associated: An epidemiological analysis from the population-based Screening PRE-diabetes and type 2 DIAbetes (SPREDIA-2) study. PLoS One 2017;12:e0186220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Hsieh HM, Lin TH, Lee IC, et al. The association between participation in a pay-for-performance program and macrovascular complications in patients with type 2 diabetes in Taiwan: a nationwide population-based cohort study. Prev Med 2016;85:53–9. [DOI] [PubMed] [Google Scholar]
- [33].Mendelson A, Kondo K, Damberg C, et al. The effects of pay-for-performance programs on health, health care use, and processes of care: a systematic review. Ann Intern Med 2017;166:341–53. [DOI] [PubMed] [Google Scholar]
- [34].Pan CC, Kung PT, Chiu LT, et al. Patients with diabetes in pay-for-performance programs have better physician continuity of care and survival. Am J Manag Care 2017;23:e57–66. [PubMed] [Google Scholar]
- [35].Kondo KK, Damberg CL, Mendelson A, et al. Implementation processes and pay for performance in healthcare: a systematic review. J Gen Intern Med 2016;31:61–9. [DOI] [PMC free article] [PubMed] [Google Scholar]


