Supplemental Digital Content is available in the text
Keywords: campaign, melanoma projections, prevention, skin cancer, ultraviolet radiation
Abstract
Exposure to ultraviolet radiation is the main risk factor for skin cancer. Denmark has one of the highest incidences of skin cancer in the world. In 2007, a long-term sun safety campaign was launched in Denmark. We have evaluated the effects on prevalence of sunburn and modeled the effects on future melanoma incidence.
Sunburn was evaluated by annual cross-sectional surveys representative for the Danish population on age, gender, and region. During 2007–2015, survey data were collected for 33.315 Danes. Cutaneous Melanoma incidences were modeled in the Prevent program, using population projections, historic incidence, sunburn exposure, and relative risk of sunburn on melanoma.
The prevalence of sunburn in Denmark was reduced with 1% annually during 2007 to 2015. The campaign is estimated to have reduced the number of skin cancer cases with 664 annually in 2040 and 14.326 totally during 2007 to 2040. If the campaign was terminated in 2015 and sunburn rates return to precampaign level there would be no annual reduction in 2040 while in total the reduction would be 4.024 cases for 2007 to 2040. A continuous campaign until 2040 would yield annual reductions of 2.121 cases by 2040 and a total of 29.729 cases for the entire period.
We have showed the value of prevention and the value of long-term planning in prevention campaigning. Sunburn use was reduced significantly during 2007–2015 and further reductions are possible. Consequently, we predict significant fewer skin cancer cases as anticipated.
1. Introduction
Exposure to ultraviolet radiation (UVR) is the main risk factor for epidermal skin cancers,[1,2] and intermittent exposure to UVR from the sun and sunbeds, and sunburn history, are important factors in the etiology of melanoma.[3,4] Denmark has experienced a large increases in both melanoma incidence and in keratinocyte skin cancer incidences.[5] Presumably because of change in sun exposure patterns including increased traveling since the 1960s and the introduction and spread of sunbed facilities in the 1980s. About half of the Danish population travel to sunny destinations each year,[6,7] approximately 60% have ever used a sunbed[8] and about 4 in 10 are sunburned annually.[6,9] Additionally, the majority of the Danes are skin type I and II,[10,11] who are not adapted to high intensive UV exposure.
There are several behavioral measures related to cutaneous melanoma (CM) including sunburn as a child, sunburn history, intermittent exposure, for example, sunbathing and number of sunny holydays.[2] The CM risk from being sunburned was estimated by several studies[12] and ranged from (1.1 to 7.6). The most comprehensive review by Gandini et al[3] which was included in the most recent IARC monograph on solar radiation[2] showed an increased risk of CM of OR 2.03 (1.73–2.37) for ever being sunburned. In IARC monograph 100 D, the risk of ultraviolet radiation on keratinocyte cancers are summarized.[13] The included studies showed an increased risk of basal cell carcinoma (BCC) among persons who ever sunburned, except from one study. Regarding squamous cell carcinoma (SCC) increased risks from sunburn in case control studies were not significant while cohort studies showed an significant increased risk from sunburn on SCC.[13] In contrary to the overall etiology of SCC and BCC caused by sunburn, there seems to be a lack of consensus on the magnitude of the risk from sunburn which ranged from OR (95 CI) = 0.8 (0.4–1.8) to 3.6 (1.9–6.8) for BCC and 0.8 (0.4–1.8) to 1.7 (1.1–2.5) for SCC. Additionally, the development of skin cancer may vary in duration from exposure to malignancy depending on a range of factors, for example, type of skin cancer, exposure pattern and genetics.[14–16]
In 2007, the Danish Sun Safety campaign was launched to reduce the UV exposure including sunburn and to increase awareness and promote the use of sun protection strategies to be used in the peak period of UVR exposure. The 4 key advices were: seek shade, wear a sun hat and use protective clothing, use sunscreen, and do not use sunbeds. The campaign was a multicomponent campaign including use of television advertising, social media, print media, press, public affairs, structural prevention, and volunteer efforts in several settings like kindergartens, music festivals, running events. The main component was an annual media campaign in late spring or summer. The campaign team was very diverse and composed of 50% creative communication and 50% analytical evaluation personnel securing all campaign components being part of an iterative quality assurance process.
The aims of this study are to show the effects of the Danish Sun Safety Campaign targeted exposure in the natural sun from 2007 to 2015 by using sunburn as our primary outcome, and to calculate future changes in skin cancer incidences 2007–2040 as a result of change in sunburn.
2. Materials and methods
2.1. Overview
We estimated the effect of the Danish Sun Safety Campaign during 2007 to 2015 in terms of annual reduction in sunburn fraction. We modeled projections of future cancer incidence, introducing the effects of the campaign and compared with status quo using realistic and conservative estimates of relative risks in the intervention scenarios to obtain an indication of the long-term impact of the campaign interventions on cancer incidence.
2.2. Questionnaire and measurements
In Table 1 included variables from the questionnaire is shown. Respondents were asked about sunburn within the past 12 months/past summer, and the answers were grouped into “burned” and “not burned” (not within the past 12 months/summer) in Table 2. During 2007 to 2015, the questionnaire for evaluation was revised annually as a consequence of campaign learning. Most important are the changes in our main proxy measurement for UV radiation damage: sunburn. In 2012, the question was changed from sunburn in general to a battery type question that included sunburn; in Denmark, in sunny vacation, in sunbed and in other place. In 2012, the question and answer categories were changed from “How many times did you sunburn?” (>5 times, 3–5 times, 1–2 times, No) to “Did you experience sunburn in the following places?” (Yes, No): In Denmark, In Sunny Vacation, and in Other Place. The education variable included 7–10 options during the period, and it was condensed into the 3 categories shown in Table 1.
Table 1.
Distribution of demographic characteristics in cross-sectional samples of 33.315 Danes 2007–2015.
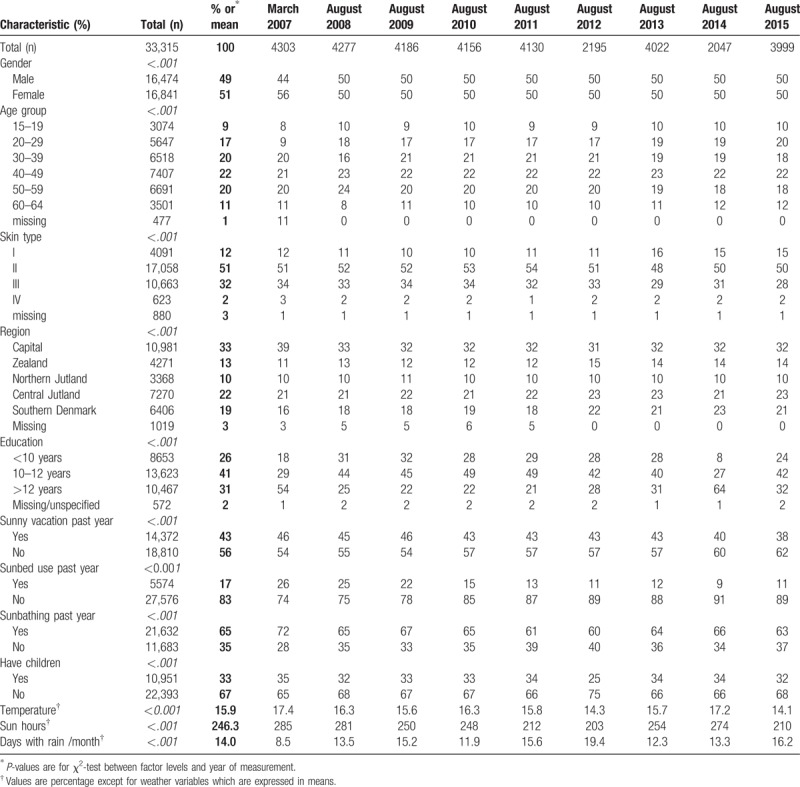
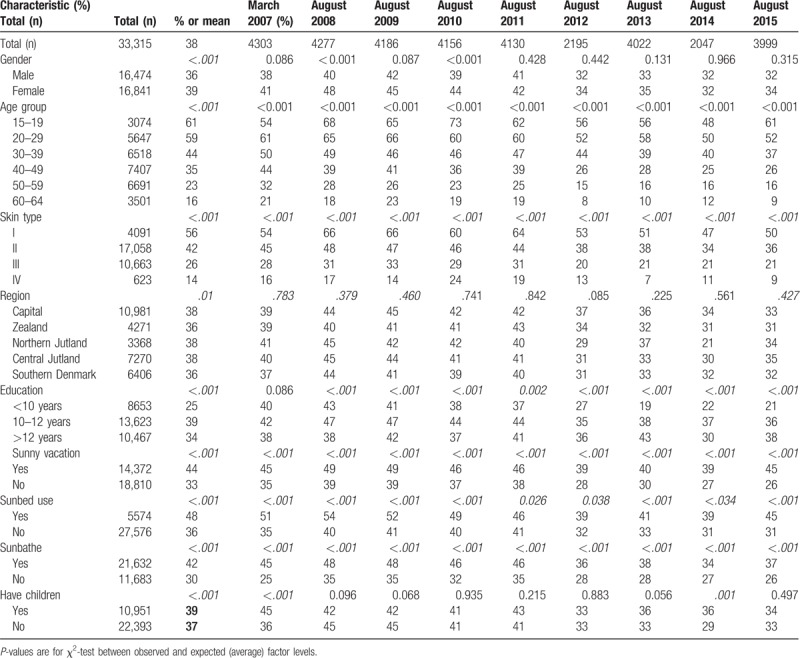
Table 2.
Distribution of sunburn frequency by demographic characteristics and year of measurement in cross-sectional samples of 33.315 Danes 2007-15.
Data were collected by computer-assisted web interview by Epinion (2007 and 2014–15) and Userneeds (2008–2013). Data were collected as representative by gender, age, region, and education. Different levels of education were used and they differ between years. Since 2009, as there were limited number of internet panels available which could provide the data requested, it was a requirement that maximum 25% of the participants were allowed to participate in the survey the following year, because answering a questionnaire could influence the behavior. Differences in demographic variables exist between years as data collection and panel composition evolved as well. Age was included as 5- or 10-year age groups. Teenagers were kept as “15 to 19 years” as their behavior was shown to differ from the adult population.[17]
Approval from the national committee on health research ethics was not required as the project did not include human material, but only “pure” data, for example, numbers, signs, and statistical material.
2.3. Analysis
The homogeneity of sunburn, time of survey and demographic variables by “burned” and “not burned” was examined. The outcome “sunburn, yes/no” was analyzed by logistic regression. The factors included in the model as categorical variables were gender, age, education, skin type, having children, and geographical region. The accumulated sun hours and average temperature of June and July were included in the analysis as Danes are more prone to sunbathe when the weather conditions makes it possible and significant differences occurred during the analysis period. The question about sunbathing was included in the analysis to distinguish between intentional and nonintentional tanning.[1] For the initial measurements in 2007, there was no higher age limit and persons 65 and older were categorized as missing to be able to compare over time. Factors with a statistically significant different distribution were included as possible explanations. Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. The P values from the logistic regression analysis refer to tests for variation between the factor levels by time (year) in Figure 1. In Table 3 time (year) was included as linear variable to estimate the average reduction. For all tests, P values < .05 were considered statistically significant. The procedure logistic in SAS version 9.3 (SAS Institute, Cary, NC) was used for the analyses.
Figure 1.
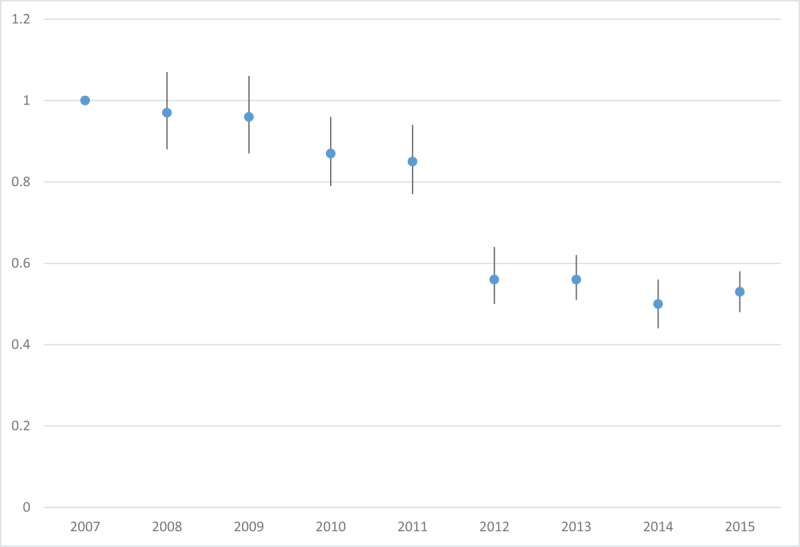
Development in sunburn in the Danish population by time since campaign launch in 2007. Values are OR (95CI) adjusted for gender, age, education, region, and skin type. The decrease between years 2007–2011, and 2012–2015, respectively, is influenced by the changed sunburn question. The annual decrease of sunburn is 1%, (adjusted for demographic factors).
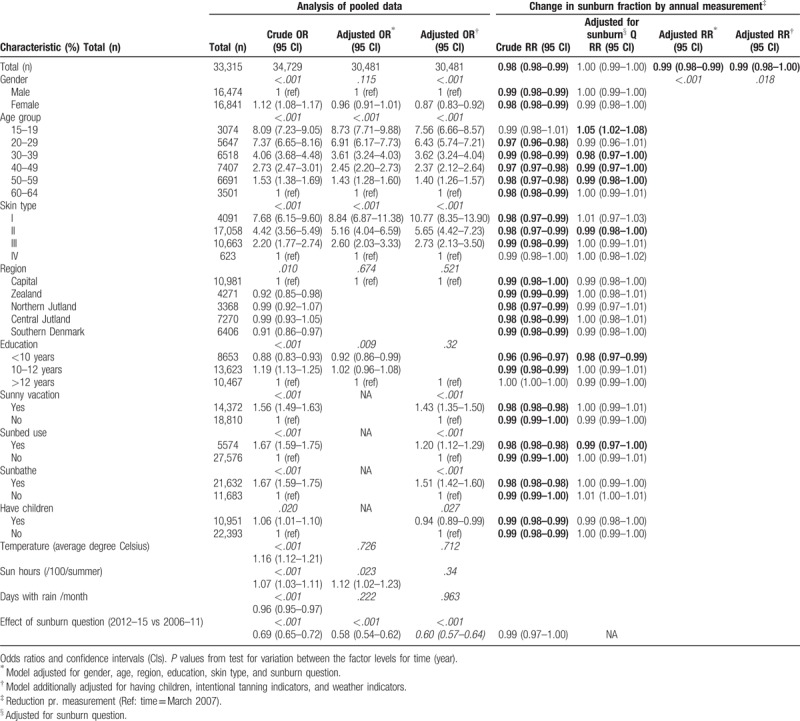
Table 3.
Logistic regression analysis of sunburn by demographic factors and annual decrease in sunburn 2007–2015.
For the projections of cancer incidence, we assumed that the change in annual sunburn rate could be used as a proxy measure for the change in population fraction that ever experienced sunburn, corresponding to a 1% decrease annually. This was based on experienced relation between ever use/recent use change in sunbed use, which were quite similar.[18] We chose this assumption as population fraction of ever use was not available for the examined period. The assumption also relies on the fact that persons who experienced sunburn once are more often sunburned again and vice versa. For example, reduction in sunburn in our results is mainly driven by those who sometimes burn (skin type II), and not those who always burn (type I) and neither among those who seldom/never burn (type III/IV). The assumption also relies on better estimates from cross-sectional surveys with 1 year recall only, than from surveys recalling sunburn history of a lifetime. Finally, as sunburn is a proxy measure for excess UV exposure and for intermittent sun exposure it is likely that the sunburn influence on cutaneous melanoma is similar in etiology to the influence of sunbed use on melanoma in having a relatively short latency time from exposure to disease.[3,16,19]
2.4. The prevent model
Prevent[20,21] was used to estimate projections of future incidence. This program was adapted for the Eurocadet project to model future cancer incidence by implementation of lifestyle preventive strategies. Prevent calculated the percentages of potentially prevented cases under the scenario of interest as compared to the status quo scenario. If the scenario of interest is no exposure or exposure with minimum impact on risk this percentage is interpretable as the population attributable fraction of sunburn experience, respectively, on skin cancer (CM, SCC, and BCC) incidence by the year 2040: they represent the numbers of cases that would be prevented had the population not been sun burned and therefore the fraction of melanoma skin cancer cases attributable to these risk factors. Three types of data are needed to run the model; demographic data (current and projected population sizes by age and sex), risk factor-related data (prevalence, changes in prevalence as a result of interventions and risk estimates), and disease incidence data (cancer rates and estimated annual percentage change to account for trends in disease incidence that are not associated with modeled risk factor data). The projected numbers of new cancer cases were computed based on the demographic data and under different scenarios of changes in the prevalence of risk factors. Results are projected rates and numbers with and without modeled interventions on risk factor prevalence.
2.5. Exposure: Sunburn
Sunburn is the primary outcome exposure variable in the literature as proxy for UVR exposure.[13] The prevalence of sunburn was derived from sun behavior questionnaires of The Danish Sun Safety Campaign as described above.[22] The campaign was the only institution in Denmark collecting data on UVR exposure continuously since 2007. The change in prevalence of sunburn applied in the population projections was from logistic regression analysis.
2.6. Incidence data
National incidence rates for melanoma skin cancer (ICD-10 code: C43) and keratinocyte skin cancer (C44) by sex and 5-year age groups were retrieved from NORDCAN.[5] The EAPC (estimated annual percentage change) for men and women for the past 25 years, respectively, was 6.4% and 10.9% increase for SCC, 5.4% and 7.4% for BCC and 4.4% and 4.5% for melanoma.[5] We chose to use a uniform conservative 4% increase in skin cancer rates for men and women for the modeling. The EAPC was applied for the first 15 years after which it remained constant at this level. For sensitivity analysis, we applied respectively 0 and 30 years.
2.7. Population projections
From Statistics Denmark, we obtained the size of the population on January 1st, of the corresponding period of the latest available incidence data by 1-year age category and sex as well as forecasted population sizes for each year up to 2040 by 5-year age categories and sex, using the medium national growth estimates.
2.8. Effect of sunburn on the incidence of skin cancer
Relative risks for sunburn and risk of melanoma skin cancer were derived from the largest meta-analysis, on the subject, which was also referenced in IARC monograph.[3,13] Persons who were sunburned had a pooled relative risk of developing melanoma skin cancer of 2.03 (1.73–2.37) compared to those who had not experienced sunburn.[4] As we do not have a consensus estimate for the relative risk for SCC and BCC for sunburn we have chosen 3 estimates within the relative risk range reported. For SCC and BCC we have chosen a lower, a middle and a higher estimate within the reported RR range.[13] For SCC we chose the estimates 1.1, 1.3, 1.5 and for BCC the estimates 1.2, 1.6, and 2.0. The estimates were used as the relative risks and risk functions in our modeling (Fig. 2). The middle estimates for the main analysis and lower and higher estimates for sensitivity analysis. The relative risks were assumed equal for all age groups and across time.[21] The effect of a risk factor exposure on cancer incidence may have a long latency time. Prevent accommodates this through 2 time lags: the time that the risk remains unchanged after a decline in risk factor exposure (LAT) and the period during which the changes in risk factor exposure gradually affect the risk of cancer, eventually reaching risk levels of the non-exposed (LAG).[20] For this study, we used for sunburn a LAT of 2 years and a LAG of 5 years for melanoma and 2 years LAT, 8 years LAG for the keratinocyte cancers, in all cases LAG was modeled as a linearly declining risk. As LAT and LAG for sunburn on risk of skin cancer are not estimated precisely short time periods were chosen from the knowledge of intermittent exposure pathway[1] and the experiences from Iceland[16] and sunbed use in young people.[23]
Figure 2.
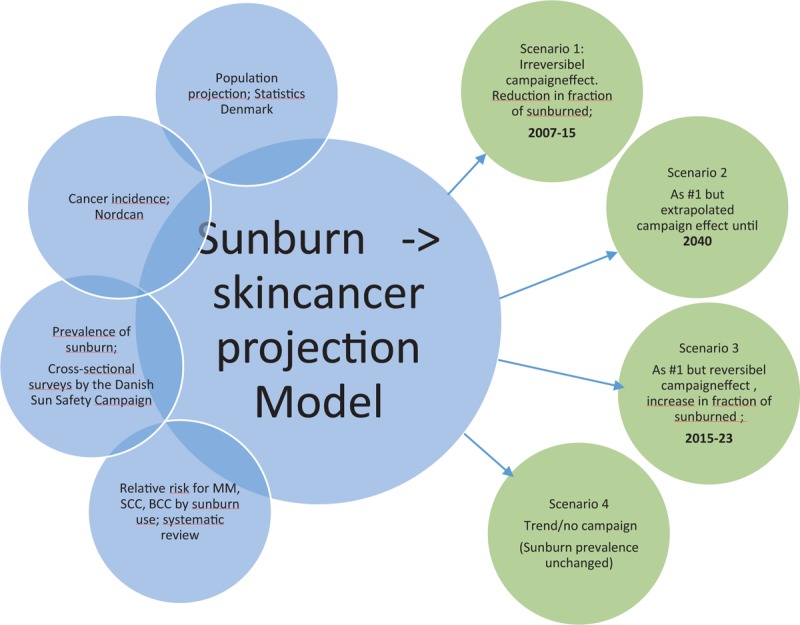
Illustration of data projections and scenarios.
We have modeled the development in future skin cancer incidence in Denmark in 4 scenarios:
Scenario 1: We assume the campaign is discontinued after 2015 and that the sunburn rate remains constant afterwards (Irreversible campaign effect)
Scenario 2: The campaign is assumed to continue with same reduction rate until the calculation terminates in 2040 (Potential campaign effect)
Scenario 3: Similar to scenario 1 except, we have modeled a conservative “spring effect” where the sunburn prevalence returns to pre campaign level in the inverse rate as it was reduced 2015–2023 (reversible campaign effect)
Scenario 4: The expected trend if sunburn prevalence is unchanged (trend/no campaign effect)
We have also applied sensitivity analyses to the conservative scenario 3. We have used the applied EAPC for 0, respectively 30 years instead of 15. We have applied a combined LAT+LAG time of either zero or twice the time, of the original scenario. Finally, for keratinocyte cancers we applied the lower and higher RR as stated above while melanoma RR was held constant.
3. Results
Table 1 shows the distribution of demographic factors, intentional tanning behaviors, and ambient factors possibly influencing outdoor behavior by survey year. Gender is evenly distributed by survey year except for baseline in 2007, where more women participated. The baseline survey also included fewer young people. In 2013 and 2015, more participants designated themselves as skin type I. Differences in length of education and having children also exists. Sunbed use decreased, while participants also reported that fewer people went for a sunny vacation. Sunbathing decreased likewise. Ambient weather factors varied significantly during the campaign period.
Table 2 shows the distribution of sunburn fraction by demographic factors, intentional tanning behaviors and ambient factors by survey year. The sunburn fraction was higher among females, by decreasing age and paler skin type. Sunburn was the highest among persons with 10 to 12 years of education and among persons engaging in intentional tanning behaviors: sunbathing, sunbed use and sunny vacations. In Figure 1, the risk of sunburn by year is shown in relation to the baseline survey. The risk is shown as odds-ratio and 95% confidence intervals from logistic regression adjusted for demographic factors. It also shows the importance of adjusting for differences in method of sunburn determination between the 2 periods 2007 to 2011 and 2012 to 2015. The regression analysis is shown in Table 3. The left part of the table analysis of the pooled data shows that the factors influencing sunburn the most are age group and skin type. Young people and pale skin types burn the most. All factors are significant in the unadjusted analysis. In the adjusted model, we included gender, age, skin type, education, number of sun hours and sunburn question. We also added a model including additionally the intentional tanning behaviors to show their relation to sunburn. Persons who have been sunbathing, in a sunny vacation, or in a sunbed in the past year have an increased risk of sunburn relative to people who did not. In the right part of Table 3, the change in sunburn by survey year is shown. The second column of the right part shows the crude reduction by demographic factor. It appears that there was an increase in sunburn among the youngest age group, while persons aged 30 to 59 reported a decrease in sunburn. A decrease was also shown for persons with skin type II, <10 years of education and sunbed users. The third column shows the fully adjusted result of the campaign, which is a reduction in sunburn of more than 1% annually, during 2007 to 2015. The last column shows an adjusted model which included additionally the intentional tanning behaviors. The estimate did not change by their inclusion.
3.1. The prevalence of sunburn's influence on future skin cancer (CM, SCC, BCC) incidence
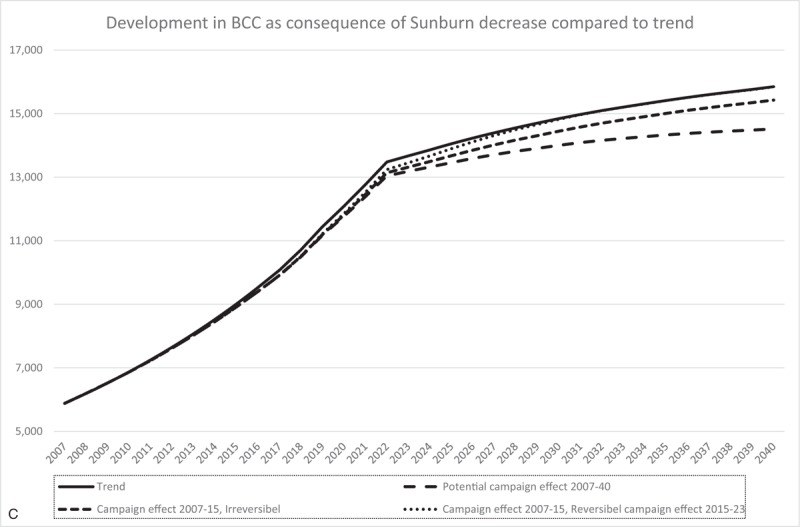
In Figure 3 A–C, we have modeled the development in the number of future skin cancer incidence cases according to 4 scenarios in Denmark. Due to large differences between skin cancer types, the Y-axis in Figure 3 A–C are not comparable. The effect of scenario 1 (Irreversibel Campaign effect) is 150 CM, 95 SCC, and 419 BCC fewer cases annually in 2040 and 3440 CM, 1865 SCC and 9021 BCC cases fewer in total during 2007–2040. If the effect of the campaign is continued until 2040 (scenario 2) there will be 492 CM, 301 SCC, and 1.328 BCC fewer cases pr. year in 2040 and totally 7.219 CM, 3.933 SCC and 18.573 BCC fewer cases during 2007–2040. Finally if the campaign effect is reversed in 2015 (scenario 3) it would have resulted in no difference in annual CM, SCC and BCC cancer cases in 2040, but however 945 CM, 490 SCC and 2.589 BCC fewer cases in total during 2007–2040. The results are summarized in Figure 4. In the sensitivity projections for scenario 3 (Fig. S1), where EAPC, LAT+LAG and OR was examined there was a minimum of 538 CM cases, respectively and a maximum of 1056 cases fewer during 2007 to 2040. Likewise, there was a minimum/maximum of 2.263/ 4.954 fewer skin cancer cases totally 2007 to 2040. In Table S1 we have shown reductions in percentage of the total for scenarios 1–3 and for sensitivity variations of scenario 3. The relative reductions are larger for irreversible effects compared to reversible as well as a continued campaign with constant efficacy shows the largest reduction. In addition, sensitivity variations of scenario 3 were robust to changes in cancer incidence and time to effect.
Figure 3.
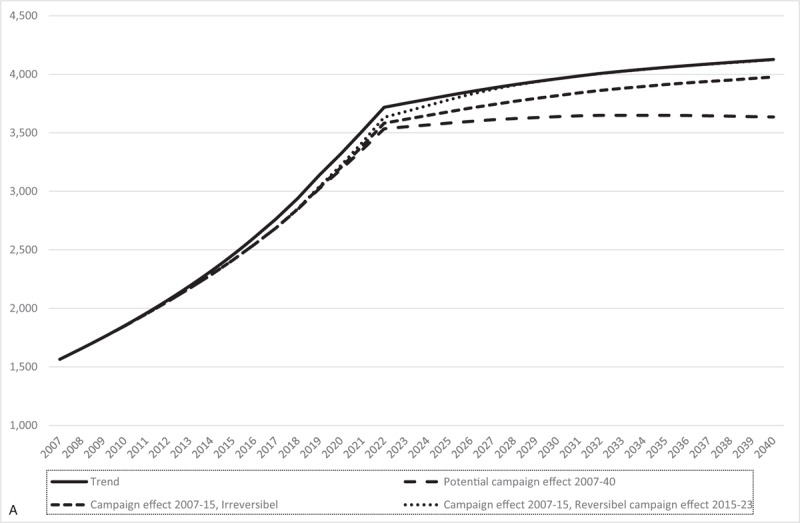
(A) The expected number of CM cases, when experienced sunburn is unchanged, when a potential campaign effect is continued until 2040, there is a reversible or irreversible campaign effect. Assumed estimated annual percentage change 2007–2022 (4% increase) and 2022–2040 (0% constant). LAT time of 2 years and LAG time of 5 years. (B) The expected number of SCC cases, when experienced sunburn is unchanged, when a potential campaign effect is continued until 2040, there is a reversible or irreversible campaign effect. Assumed estimated annual percentage change 2007–2022 (4% increase) and 2022–2040 (0% constant). LAT time of 2 years and LAG time of 8 years. (C) The expected number of BCC cases, when experienced sunburn is unchanged, when a potential campaign effect is continued until 2040, there is a reversible or irreversible campaign effect. Assumed estimated annual percentage change 2007–2022 (4% increase) and 2022–2040 (0% constant). LAT time of 2 years and LAG time of 8 years. BCC = basal cell carcinoma, CM = cutaneous melanoma.
Figure 3 (Continued).
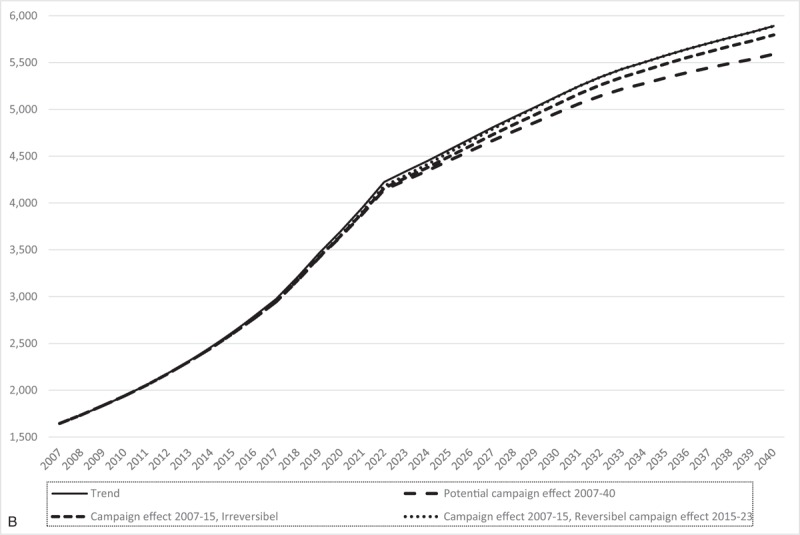
(A) The expected number of CM cases, when experienced sunburn is unchanged, when a potential campaign effect is continued until 2040, there is a reversible or irreversible campaign effect. Assumed estimated annual percentage change 2007–2022 (4% increase) and 2022–2040 (0% constant). LAT time of 2 years and LAG time of 5 years. (B) The expected number of SCC cases, when experienced sunburn is unchanged, when a potential campaign effect is continued until 2040, there is a reversible or irreversible campaign effect. Assumed estimated annual percentage change 2007–2022 (4% increase) and 2022–2040 (0% constant). LAT time of 2 years and LAG time of 8 years. (C) The expected number of BCC cases, when experienced sunburn is unchanged, when a potential campaign effect is continued until 2040, there is a reversible or irreversible campaign effect. Assumed estimated annual percentage change 2007–2022 (4% increase) and 2022–2040 (0% constant). LAT time of 2 years and LAG time of 8 years. BCC = basal cell carcinoma, CM = cutaneous melanoma.
Figure 3 (Continued).
(A) The expected number of CM cases, when experienced sunburn is unchanged, when a potential campaign effect is continued until 2040, there is a reversible or irreversible campaign effect. Assumed estimated annual percentage change 2007–2022 (4% increase) and 2022–2040 (0% constant). LAT time of 2 years and LAG time of 5 years. (B) The expected number of SCC cases, when experienced sunburn is unchanged, when a potential campaign effect is continued until 2040, there is a reversible or irreversible campaign effect. Assumed estimated annual percentage change 2007–2022 (4% increase) and 2022–2040 (0% constant). LAT time of 2 years and LAG time of 8 years. (C) The expected number of BCC cases, when experienced sunburn is unchanged, when a potential campaign effect is continued until 2040, there is a reversible or irreversible campaign effect. Assumed estimated annual percentage change 2007–2022 (4% increase) and 2022–2040 (0% constant). LAT time of 2 years and LAG time of 8 years. BCC = basal cell carcinoma, CM = cutaneous melanoma.
Figure 4.
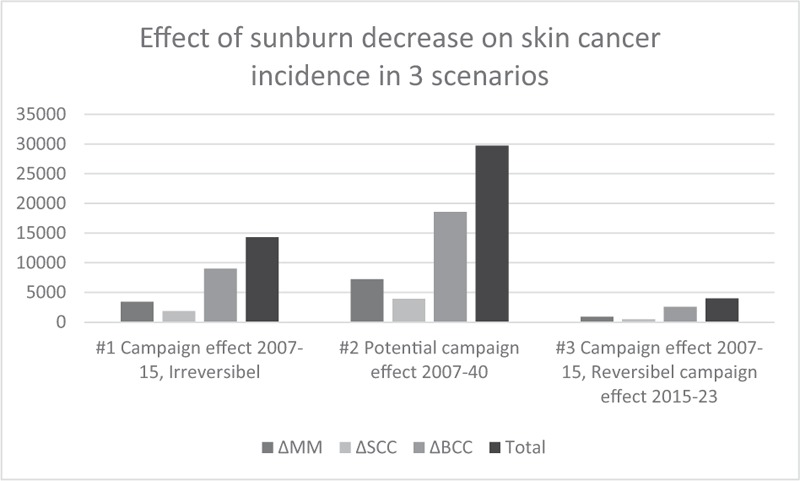
The cumulative number of skin cancers in 3 scenarios of the sunburn decrease compared to trend.
4. Discussion
We have shown that the Danish Sun Safety Campaign reduced the sunburn prevalence significantly during 2007 to 2015, with a decreasing trend in sunburn of 1% annually. We have modeled how these results influence on future cancer incidence for the period 2007 to 2040. The continuity of the campaign has a major influence on the number of future skin cancer cases. The main conservative result of what we already expect to have achieved by a decrease in sunburn during 2007 to 2015 was 4.024 fewer skin cancer cases (945 CM, 490 SCC, 2.589 BCC)in total during 2007 to 2040, however as the campaign is still active until at least 2018 the reversed campaign effect is not expected as yet. Therefore, the actual number of saved skin cancer cases is likely to be significantly higher. We have also showed the potential of continued persistent campaigning with large annual reductions in 2040 of more than 2.000 fewer cases for a campaign with constant efficacy.
4.1. Strengths and limitations
This study's unique strengths is the possibility of long time planning, securing the continuity in the campaign to secure comparable evaluations over the entire period as well as long term funding has made the high continuous campaign pressure possible.
A potential limitation is the risk that the high awareness created by the campaign could cause social desirability bias meaning, for example, that persons would falsely state no to sunburn in questionnaires. Similarly selection bias may occur, for example, that sunbathers who burn more often would be less prone to participate in surveys of this subject. As the surveys were allowed to include maximum of 25% repeated participants they may be less likely to answer that they were sunburned or they may have changed their behavior as a result of participation in a questionnaire
Regarding a prognosis of the cancer incidence in absolute numbers, there are unknown indicators we were not able to include in the model like improved diagnostics, equipment,[24] or changes in other kinds of UV exposure. However, as we are using the difference between 2 cancer incidence rates this has minor influence on results. The model accuracy is as good as the data input, and the assumptions made for the different scenarios. The data validity for CM, SCC, and BCC provided by NORDCAN and the Danish Cancer Registry is high; valid and representative population data on sunburn was collected. It is however also important to emphasize that our results are a projection of the development of the skin cancer incidence in Denmark focusing on saved fraction of cancer cases and not on absolute numbers of cancer cases. The reason that the skin cancer incidence in the years already passed is different from the actual incidence development is because additional factors are involved. About year 2002 to 2004, the dermatoscope was introduced among dermatologists in Denmark, which probably increased the rate of detection[24] in a period. In the following period a plateau is seen around 2011.[5] Most likely, the decreased incidence rate is a consequence of the earlier detection/treatment an effect also seen in various screening programs. The increased skin cancer incidence created awareness in the media of the disease up through the 1990s and in 2007, the multicomponent intervention of the Danish Sun Safety Campaign increased this awareness manifold. The increased awareness could also lead to an increase in e.g. mole check by the general physician which again could lead to an increased number of diagnoses. We were not able to measure these influences on the incidence rate.
Limitations also included the assumption of using the relative risk of ever sunburned with the modified estimates of annual sunburn. However, our sensitivity analysis shows that the proportion of avoidable skin cancer cases were robust to changes in cancer incidence, latency time, and relative risk.
The changes in the sunburn question may have influenced the analysis; however, we included sunburn question in the analysis and since the interval was widened from past summer to past 12 months and since the second change increased the possibility to state a sunburn in several settings and recall a sunburn, any bias would increase the fraction of sunburn in our analysis.
4.2. Reduction in sunburn rate
Australia was the first country to implement skin cancer prevention campaigns.[25,26] They showed increases in body cover of 3% annually, 2002 to 2012, an initial increase in sunscreen use and almost a reduction in sunburn of 50% during 1987 to 2002 corresponding to approximately 4% annually.[27–29] This is comparable to the efforts of the Danish Sun Safety Campaign. However, the decline in Denmark is smaller and seems to have occurred more steadily. A systematic review of skin cancer interventions found 143 potential studies of which 7 were included as large multicomponent community wide interventions comparable to the intervention we have described.[30] The 7 studies were mainly reporting the Australian results. The other studies were primarily evaluated by increases in sunscreen use. Our results are the first European estimates of sunburn, the main skin cancer predictor, in a long-term multicomponent intervention. None of the interventions executed until now, including this study, had objectively UV-validated evaluation questionnaires available.[11,31] This could increase precision in estimates in evaluations in the future.
4.3. Consequences
Because of our intervention, a significant proportion of the expected morbidity and mortality from Cutaneous Melanoma in Denmark is avoided in the future. The annual cost of skin cancer in Denmark was estimated to 33.3 million € in 2004 to 2008. An American study showed that costs of skin cancer increased by 25% pr. year in the 5-year-period from 2002–2006 to 2007–2011,[32] which may also be the trend in Denmark. The number of melanoma cases in Denmark (2010–2014) has increased with 54% since the Danish cost evaluation (1353 ->2085 cases). This emphasizes both the economic and health potential of the results. Hence, the total benefits of the Danish Sun Safety Campaign are even larger than what we have shown. For a government administration perspective, structural interventions to reduce sunburn and other UV-risk behavior, in the Danish population and other countries with skin cancer challenges, is encouraged and was previously shown to be cost effective.[33]
5. Conclusion
The Danish Sun Safety Campaign has significantly reduced the sunburn frequency in the Danish population in the period 2007 to 2015. As a consequence of these results and a continued campaign pressure, we expect fewer skin cancer cases in Denmark in the future. Our results confirm previous results of the value of skin cancer prevention and the value of long term planning in behavioral prevention.
Acknowledgments
The efforts of the Danish Sun Safety Campaign were possible by donations from the philanthropic foundation, TrygFonden.
Author contributions
Conceptualization: Brian Køster, Maria K H Meyer, Therese M-L Andersson, Gerda Engholm, Peter Dalum.
Data curation: Brian Køster, Maria K H Meyer, Therese M-L Andersson, Gerda Engholm, Peter Dalum.
Formal analysis: Brian Køster.
Funding acquisition: Peter Dalum.
Investigation: Brian Køster, Maria K H Meyer.
Methodology: Brian Køster, Maria K H Meyer, Therese M-L Andersson, Gerda Engholm, Peter Dalum.
Project administration: Brian Køster, Maria K H Meyer, Peter Dalum.
Resources: Therese M-L Andersson, Gerda Engholm, Peter Dalum.
Software: Therese M-L Andersson, Gerda Engholm.
Writing – original draft: Brian Køster.
Writing – review & editing: Brian Køster, Maria K H Meyer, Therese M-L Andersson, Gerda Engholm, Peter Dalum.
Brian Køster orcid: 0000-0001-8352-3066
Supplementary Material
Footnotes
Abbreviations: BCC = basal cell carcinoma, CI = confidence interval, CM = cutaneous melanoma, EAPC = estimated annual percentage change, OR = odds ratio, SCC = squamous cell carcinoma, UVR = ultraviolet radiation.
Funding: This study was supported by TrygFonden.
Data sharing: Dataset available from the corresponding author.
Conflicts of interest: The authors have declared that no competing interests exist. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Supplemental Digital Content is available for this article.
References
- [1].Armstrong BK, Kricker A. The epidemiology of UV induced skin cancer. J Photochem Photobiol B 2001;63:8–18. [DOI] [PubMed] [Google Scholar]
- [2].IARC, Radiation: Volume 100 D—a review of human carcinogens. International Agency for Research on Cancer (IARC), World Health Organization (WHO), 2012. [Google Scholar]
- [3].Gandini S, Sera F, Cattaruzza MS, et al. Meta-analysis of risk factors for cutaneous melanoma: II. Sun exposure. Eur J Cancer 2005;41:45–60. [DOI] [PubMed] [Google Scholar]
- [4].Veierod MB, Adami HO, Lund E, et al. Sun and solarium exposure and melanoma risk: effects of age, pigmentary characteristics, and nevi. Cancer Epidemiol Biomarkers Prev 2010;19:111–20. [DOI] [PubMed] [Google Scholar]
- [5].Engholm G, et al. NORDCAN: Cancer Incidence, Mortality, Prevalence and Survival in the Nordic Countries, Version 7.3 (08.07.2016). Association of the Nordic Cancer Registries. Danish Cancer Society. Available at: http://www.ancr.nu Accessed on 15/08/2016. 2016. [Google Scholar]
- [6].Koster B, Thorgaard C, Philip A, et al. Vacations to sunny destinations, sunburn, and intention to tan: a cross-sectional study in Denmark, 2007–2009. Scand J Public Health 2011;39:64–9. [DOI] [PubMed] [Google Scholar]
- [7].Behrens C.L., Schiøth C., Christensen A.S. Sun habits of the Danes in sunny vacations 2015 Report in Danish. 2016. Available at: www.skrunedforsolen.dk Accessed January 2018 [Google Scholar]
- [8].Koster B, Thorgaard C, Philip A, et al. Sunbed use and campaign initiatives in the Danish population, 2007–2009: a cross-sectional study. J Eur Acad Dermatol Venereol 2011;25:1351–5. [DOI] [PubMed] [Google Scholar]
- [9].Koster B, Thorgaard C, Philip A, et al. Prevalence of sunburn and sun-related behaviour in the Danish population: a cross-sectional study. Scand J Public Health 2010;38:548–52. [DOI] [PubMed] [Google Scholar]
- [10].Fitzpatrick T. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol 1988;124:869. [DOI] [PubMed] [Google Scholar]
- [11].Køster B, Søndergaard J, Nielsen JB, et al. The validated sun exposure questionnaire—association of objective and subjective measures of sun exposure in a Danish population based sample. Br J Dermatol 2016;176:446–56. [DOI] [PubMed] [Google Scholar]
- [12].Elwood JM, Jopson J. Melanoma and sun exposure: an overview of published studies. Int J Cancer 1997;73:198–203. [DOI] [PubMed] [Google Scholar]
- [13].Monograph 100 D—Solar and Ultraviolet Radiation. 2011;Lyon, France: IARC, 35–102. [Google Scholar]
- [14].Autier P, Doré JF, Eggermont AM, et al. Epidemiological evidence that UVA radiation is involved in the genesis of cutaneous melanoma. Curr Opin Oncol 2011;23:189–96. [DOI] [PubMed] [Google Scholar]
- [15].Sulem P, Gudbjartsson DF, Stacey SN, et al. Genetic determinants of hair, eye and skin pigmentation in Europeans. Nat Genet 2007;39:1443–52. [DOI] [PubMed] [Google Scholar]
- [16].Héry C, Tryggvadóttir L, Sigurdsson T, et al. A melanoma epidemic in Iceland: possible influence of sunbed use. Am J Epidemiol 2010;172:6. [DOI] [PubMed] [Google Scholar]
- [17].Branstrom R, Brandberg Y, Holm L, et al. Beliefs, knowledge and attitudes as predictors of sunbathing habits and use of sun protection among Swedish adolescents. Eur J Cancer Prev 2001;10:337–45. [DOI] [PubMed] [Google Scholar]
- [18].Julie H. Mortensen, C.L.B., Brian Køster, Danskernes solariebrug 2016 – Notat [Sunbed habits of the Danes 2016- Brief (in Danish)]. 2016. [Google Scholar]
- [19].Tryggvadottir L, Gislum M, Hakulinen T, et al. Trends in the survival of patients diagnosed with malignant melanoma of the skin in the Nordic countries 1964–2003 followed up to the end of 2006. Acta Oncol 2010;49:665–72. [DOI] [PubMed] [Google Scholar]
- [20].Soerjomataram I, de Vries E, Engholm G, et al. Impact of a smoking and alcohol intervention programme on lung and breast cancer incidence in Denmark: an example of dynamic modelling with Prevent. Eur J Cancer 2010;46:2617–24. [DOI] [PubMed] [Google Scholar]
- [21].Barendregt J. [Accessed January 2018]. Available at: http://www.epigear.com/index_files/prevent.html [cited 2016 01.10.2016] [Google Scholar]
- [22]. [Accessed January 2018]. Available at: www.skrunedforsolen.dk [cited 2018] [Google Scholar]
- [23].Lazovich D, Isaksson Vogel R, Weinstock MA, et al. Association between indoor tanning and melanoma in younger men and women. JAMA Dermatol 2016;152:268–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Helvind NM, Hölmich LR, Smith S, et al. Incidence of in situ and invasive melanoma in Denmark from 1985 through 2012: A National Database Study of 24,059 Melanoma Cases. JAMA Dermatol 2015;151:1087–95. [DOI] [PubMed] [Google Scholar]
- [25].Montague M, Borland R, Sinclair C. Slip! Slop! Slap! and SunSmart, 1980–2000: skin cancer control and 20 years of population-based campaigning. Health Educ Behav 2001;28:290–305. [DOI] [PubMed] [Google Scholar]
- [26].Marks R. Skin cancer control in the 1990's, from slip! Slop! Slap! To sun smart. Australas J Dermatol 1990;31:1–4. [DOI] [PubMed] [Google Scholar]
- [27].Dobbinson SJW, Jamsen KM, Herd NL, et al. Weekend sun protection and sunburn in Australia -Trends (1987-2002) and association with sunsmart television advertising. Am J Prev Med 2008;34:94–101. [DOI] [PubMed] [Google Scholar]
- [28].Dixon HG, Lagerlund M, Spittal MJ, et al. Use of sun-protective clothing at outdoor leisure settings from 1992 to 2002: serial cross-sectional observation survey. Cancer Epidemiol Biomarkers Prev 2008;17:428–34. [DOI] [PubMed] [Google Scholar]
- [29].Makin JK, Warne CD, Dobbinson SJ, et al. Population and age-group trends in weekend sun protection and sunburn over two decades of the SunSmart program in Melbourne, Australia. Br J Dermatol 2012;168:154–61. [DOI] [PubMed] [Google Scholar]
- [30].Sandhu PK, Elder R, Patel M, et al. Community-wide interventions to prevent skin cancer: two community guide systematic reviews. Am J Prev Med 2016;51:531–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Koster B, Søndergaard J, Nielsen JB, et al. Knowledge deficit, attitude and behavior scales association to objective measures of sun exposure and sunburn in a Danish population based sample. PLoS One 2017;12:e0178190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Guy GP, Jr, Machlin SR, Ekwueme DU, et al. Prevalence and costs of skin cancer treatment in the U.S., 2002–2006 and 2007–2011. Am J Prev Med 2015;48:183–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Gordon LG, Rowell D. Health system costs of skin cancer and cost-effectiveness of skin cancer prevention and screening: a systematic review. Eur J Cancer Prev 2014;24:141–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


