Abstract
Rationale:
Radiating leg pain usually originates from the lumbar spine and occasionally from peripheral lesions. Here we report a case involving a patient with radiating pain in the right leg who exhibited 2 suspicious lesions, including 1 spinal lesion and 1 extraspinal cystic mass lesion, on magnetic resonance imaging. Polydeoxyribonucleotide sodium (PDRN) was recently noted as such a substitute. PDRN has anti-inflammatory effects, as it lowers the expression of inflammatory cytokines including interleukin-6 and tumor necrosis factor-alpha.
Patient concerns:
A 51-year-old man (weight, 93 kg; height, 168 cm) working as a bus driver presented at the pain clinic with continuous right buttock pain, radiating leg pain and a tingling sensation involving the calf and dorsum of the foot, since 1 week.
Diagnoses:
He was definitively diagnosed using differential blocks, which revealed the cyst to be the actual cause of the pain.
Interventions:
Surgical resection was not feasible because of the position of the cyst; therefore, corticosteroid injection under ultrasonographic guidance was attempted. However, this provided short-term relief. Subsequently, a solution containing PDRN was injected around the piriformis muscle and repeated 3 more times at intervals of 2 weeks.
Outcomes:
After PDRN injection, we conducted two follow-up monitoring every two months for 2 months. Last follow-up, the patient no longer complained of pain. this resulted in relatively long-term relief from pain.
Lessons:
The findings from this case suggest that PDRN is an effective alternative for steroids in patients with radiating leg pain, although its efficacy and safety needs to be evaluated in further large-scale studies.
Keywords: case report, epidural block, polydeoxyribonucleotide, ultrasonography
1. Introduction
Spinal stenosis and herniated lumbar disc (HLD) are frequent causes of radiating leg pain. Shoji et al reported that the prevalence of spinal stenosis in the general Japanese population aged 40 to 79 years is 5.7%.[1] The preconceived notion that the cause of radiating leg pain is generally spinal stenosis or HLD can result in the misdiagnosis of patients with double lesions. To prevent this, diagnostic nerve blocks are occasionally used to determine the actual cause of the pain.[2]
A ganglion cyst may occur in any joint or tendon, with the most common site being the wrist.[3] In general, a ganglion cyst is asymptomatic, although problems such as nerve root compression and myelopathy may arise depending on its location and size.[4,5] The rate of spontaneous resolution of untreated ganglion cysts is 40% to 58%.[3] The majority of patients with a ganglion cyst receive nonsurgical treatment such as aspiration with or without steroids, sclerotherapy, and hyaluronidase therapy. The recurrence rate after surgical excision of ganglion cysts at the elbow joint or in the hand was reported to be 15% to 40%, with surgical complications.[6]
Although epidural steroid injection is beneficial due to their anti-inflammatory effects,[7] the use of glucocorticoids is limited as it may cause multiple adverse effects. Many studies have sought substitutes for glucocorticoids.[8] Polydeoxyribonucleotide was recently noted as such a substitute.[9] Polydeoxyribonucleotide sodium (PDRN) has anti-inflammatory effects, as it lowers the expression of inflammatory cytokines including interleukin-6 and tumor necrosis factor-alpha. PDRN has not displayed any adverse effects.[9]
Here we report a case involving a 51-year-old man with radiating leg pain who exhibited 2 suspicious lesions, including 1 spinal lesion and 1 extraspinal cystic mas lesion, on magnetic resonance imaging (MRI). He was definitively diagnosed using differential blocks, which revealed the cyst to be the actual cause of the pain. Long-term pain relief was successfully achieved by the injection of PDRN under ultrasonographic guidance.
Approval from the Institutional Review Board of the corresponding author's affiliated university was obtained to carry out this study. The approval included a Waiver of Informed Consent, since the study did not include direct contact with the study population, and all patient identifiers were removed from the data set on initial collection.
2. Case report
A 51-year-old man (weight, 93 kg; height, 168 cm) working as a bus driver presented at the pain clinic with continuous right buttock pain, radiating leg pain and a tingling sensation involving the calf and dorsum of the foot, for 1 week. His pain aggravated while lying down and was relieved in the upright position, because of which he could hardly sleep. The Numeric Rating Scale (NRS) score for pain was 8/10. The patient had experienced similar pain 7 years ago and had undergone discectomy at the L3/4 and L5/S1 levels. However, the pain and tingling sensation persisted and he required treatment for symptom improvement. At the current presentation, no underlying disease was noted except hypertension, and the findings of physical and neurological examinations were normal. Electrodiagnosis revealed radiculopathy at the L5 level on the right side. MRI showed moderate to severe central canal stenosis at the L4/5 level and right-sided disc extrusion with compression of the S1 nerve root, with evidence of the previous discectomy at the L5/S1 level (Fig. 1A and B). In addition, a cystic mass was observed at the inner aspect of the right sciatic foramen (lateral to the internal iliac vessels) that extended to the posterior part of the right hip joint (length, 7.6 cm). The nodule showed increased signal intensity on T2-weighted images, and T1gadolinium imaging showed a hypotonic signal that was enhanced around the nodule This was tentatively diagnosed as a ganglion cyst originating from the right hip joint (Fig. 1C and D).
Figure 1.
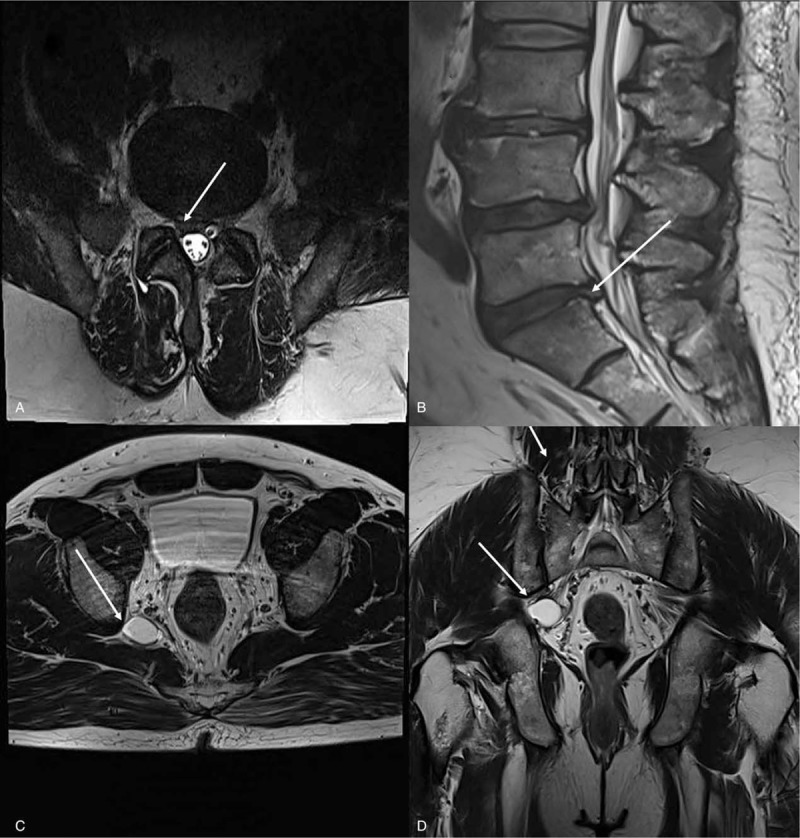
Axial T2-weighted MRI showing disk extrusion, Rt. central zone, mild∼moderate degree compression of Rt .S1 nerve root (A). Sagittal view (B), Axial T2-weighted MRI showing cystic mass in inner aspect of rt. sciatic foramen (lateral to internal iliac vessels) extending to posterior portion of rt. hip joint (C), Sagittal view (D). MRI = magnetic resonance imaging.
The patient received transforaminal epidural steroid injection (TFESI) with 0.5% bupivacaine 1 mL, normal saline 4 mL, and dexamethasone 1 mg at the L5/S1, S1, and S2 levels; however, this only provided short-term relief (Fig. 2 A, B). The S1 and S2 root blocks were attempted again, with no improvement in the outcome (Fig. 2C and D).
Figure 2.
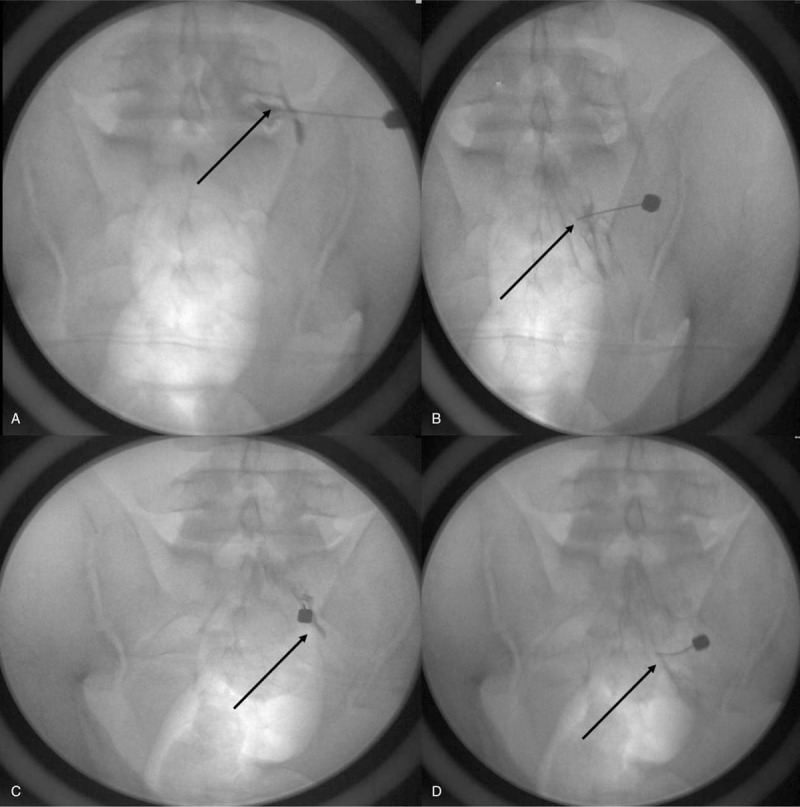
An anteroposterior fluoroscopic image taken during a contrast injection for a right L5 (A), S1 (B,C) and S2(D) transforaminal epidural steroid injection.
The ineffectiveness of TFESI indicated that the patient's leg symptoms originated from the extraspinal cyst, not the spine. Ultrasonography (US)-guided aspiration was considered, but the mass was not visible on US because it was located at the inner aspect of the sciatic foramen. Surgical excision was the next strategy, but this was also not feasible because the site was packed with nerves and blood vessels. The tenderest point was identified in the area of the piriformis muscle, above the course of the sciatic nerve around the greater sciatic foramen as identified on US. An injection of 0.5% bupivacaine 1 mL, normal saline 9 mL, and triamcinolone 8 mg was administered around the piriformis muscle under ultrasonographic guidance (Fig. 3), and the patient experienced radiating paresthesia. The NRS score for pain decreased to 5 for 7 days, and the same injection was repeated once a week for 2 weeks. During this period, a score of 4 was maintained and the patient could sleep relatively well. Subsequently, he did not visit the clinic for 42 days, after which he presented with severe pain, particularly in the dorsum of the foot. His NRS score was 7, and he could not even lie down for 2 hours. This time, a solution of 0.5% bupivacaine 1 mL, normal saline 1 mL, and HiDR (PDRN 5.625 mg/3 mL, BMI, Korea) was injected at the same site and repeated 3 more times at intervals of 2 weeks. The pain gradually decreased and disappeared in the region from the buttock to the dorsum of the foot. There was no pain for 2 months after that and the patient could sleep normally. After injection, we conducted 2 follow-up monitoring every 2 months for 2 months. Last follow-up, the patient no longer complained of pain. If symptoms reappeared or worsen in the future, he will visit again.
Figure 3.
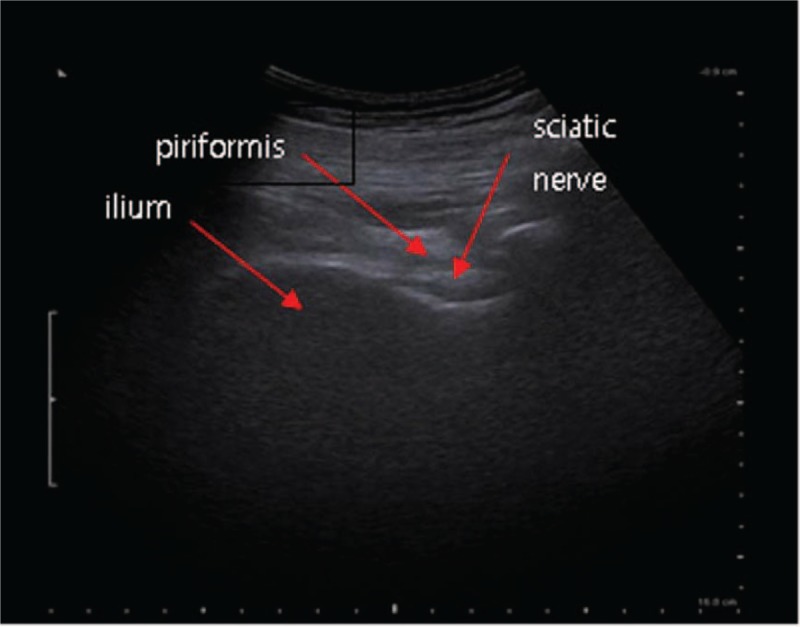
Ultrasonography guided sciatic nerve block.
3. Discussion
TFESI is a useful modality for achieving relief from radiating leg pain associated with HLD or spinal stenosis.[10,11] It is considered to provide short-term (2–4 weeks) pain relief in a proportion of patients with HLD. Multiple fluoroscopy-guided TFESIs or caudal injections are recommended for mid-term relief from radiating leg pain in patients with HLD or neurogenic intermittent claudication associated with spinal stenosis. In addition to its therapeutic value, TFESI has been considered to have good diagnostic value. Huston and Slipman recommended the injection of 0.5 to 1 mL of a local anesthetic at each level for diagnostic purposes;[2] however, we used 5 mL mixed with a corticosteroid because the differential points were not in adjacent segments of the spine, with the hope that long-term relief would be achieved if the cause of the pain was in the spine. However, TFESI was not effective, and the mass suspected to be a ganglion cyst was considered to be the cause of the pain.
The mass observed on MRI was not actually confirmed to be a ganglion cyst because it was not resected. However, it appeared as a ganglion cyst on MRI. According to Spinner et al, all hip-related intraneural ganglia originate from the hip joint, and in several cases, the connecting articular branch can be identified through considerable efforts.[12] He also reported that ganglion cysts could originate from the anterior or posterior capsule. The anterior capsule could give rise to obturator or femoral cysts, while the posterior capsule could give rise to sciatic or supragluteal intraneural cysts. Kalaci et al and Campeas et al reported ganglion cysts compressing the femoral nerve and obturator nerve, respectively.[13,14] In particular, Campeas et al reported a cyst in the obturator canal, which is connected with the inferior capsule of the hip joint.[14] Lee et al and Park et al reported ganglion cysts compressing the pudendal nerve and sciatic nerve, respectively.[15,16] Spinner et al emphasized that the connecting branch should be identified in order to minimize the postoperative recurrence rate, even though it is not always possible.[12] Lee et al and Park et al aspirated the cyst under ultrasonographic guidance and observed no recurrence for a long time.[15,16] Even though recurrence is a possibility, nonsurgical treatment is easy to repeat.[15,16] Nonsurgical treatment should be the first option considering the high recurrence rate after surgery. In the present case, even though a connecting branch was not found, the ganglion cyst was believed to be originated from the hip joint. Non-surgical treatment was selected because aspiration and resection were not feasible and achieved good outcomes.
PDRN has recently been noticed for its unique properties. It is a mixture of deoxyribonucleotides with molecular weights between 50 and 1500 KDa and originates from the sperm DNA of Oncorhynchus mykiss (Salmon trout) or Oncorhynchus keta (Chum Salmon).[17] Squadrito et al speculated that PDRN is a prodrug that can generate active deoxyribonucleotides, nucleosides, and bases that interact with the adenosine type 2a (A2a) receptor, because an adenosine A2 receptor antagonist, 3,7-dimethyl-1-propargylxanthine (DMPX), which has more affinity for A2a than for A2b, was found to block several effects of PDRN.[17] They also suggested another action mechanism known as the “salvage pathway.”[17] Here, PDRN generates nucleotides and nucleosides that can aid in DNA synthesis, which results in normal cell proliferation.[17] According to these pathways, PDRN has tissue-repairing, anti-ischemic, and anti-inflammatory properties. Finally, the authors introduced other similar drugs with different properties to show that PDRN has unique properties.[17] Nonselective adenosine receptor activators such as adenosine and dipyridamole result in unwanted side effects. The only other A2a receptor agonist, regadenoson, has been approved by Food and Drug Administration (FDA) as a pharmacological stress agent for use in myocardial perfusion imaging, and additional actions of this drug have not been elucidated. Defibrotide, another drug comprising a mixture of oligonucleotides with molecular weights between 16 and 20 KDa, is derived from the DNA of porcine intestinal mucosa and exhibits profibrinolytic, antithrombotic, thrombolytic, anti-ischemic, anti-rejection, and anti-angiogenic effects different from those of PDRN.[17]
Till date, many studies have revealed the effects of PDRN on pathologies involving various tissues, including the skin, bones, cartilages, and tendons.[18] However, studies about the effects of PDRN on the musculoskeletal system are relatively few. Kim et al reported 2 cases of ischiofemoral impingement syndrome, where more than 5 US-guided injections of PDRN at the belly and origin and insertion sites of the quadratus femoris muscle resulted in pain relief for more than 6 months, with no recurrence.[19] He mentioned about the futility of conventional prolotherapy, steroid injections, nonsteroidal anti-inflammatory drugs, and physical therapy, among other treatments, which had been attempted before PDRN injections.[19] Lim et al reported a case of posterior tibial tendon dysfunction after ankle syndesmotic surgery, where 4 US-guided injections of PDRN at the belly of the tibialis posterior muscle and nearby tendon not only relieved pain but also improved function.[20] Yoon et al reported a case-controlled retrospective study, in which 106 patients with chronic nontraumatic refractory rotator cuff disease who were unresponsive to at least 1 month of conservative treatment chose either PDRN injections or other treatment options.[21] The PDRN group showed an improvement in pain-related outcome measurements (shoulder pain and disability index, visual analog scale score, number of analgesic ingestions per day) without any changes in objective indicators (isometric strength of abductors, active range of motion, and maximal tear size of tendons) at 3 months.[21] He speculated that these findings were a result of the anti-inflammatory effects, and not the tissue-repairing effects, of PDRN.[21] However, he recommended PDRN as a substitute for steroids, considering the many side effects of steroids in addition to its short-term effects.[21] Recently, a study reported the application of PDRN in a new field.[8] Kang et al attempted TFESI with PDRN 3 times for a patient with high blood glucose levels due to noninsulin-dependent diabetes mellitus.[8] The result was good, and the patient has been in good health during the follow-up period of 6 months. He also recommended PDRN as a substitute for steroids, particularly in patients with diabetes.[8] As Squadrito et al reported, PDRN is safe because it is extracted and purified at high temperatures and derived from spermatozoa, which eliminates any immunological side effects.[17] He also stated that no toxic effects were reported from any animal studies, and postmarketing surveillance studies conducted over the past 5 years have confirmed an excellent safety profile.[17]
In the present case as well, the outcomes of PDRN with regard to relief from radiating leg pain caused by a ganglion cyst-like mass lesion were superior to those of steroid injections. The findings from this case suggest that PDRN can be used as a substitute for steroids in all regions, including the epidural space. However, further large-scale studies on the efficacy and safety of PDRN are necessary before this drug gets official approval as a substitute for steroids in radiating pain. To the best of my knowledge, this is the first report on the successful use of PDRN injections for the treatment of radiating pain originating from a ganglion cyst compressing the sciatic nerve.
Author contributions
Conceptualization: Yongbum Park.
Data curation: Woo Yong Lee, Ki Deok Park, Yongbum Park.
Investigation: Woo Yong Lee, Ki Deok Park, Yongbum Park.
Methodology: Ki Deok Park, Yongbum Park.
Supervision: Yongbum Park.
Validation: Woo Yong Lee.
Writing – original draft: Woo Yong Lee, Ki Deok Park.
Writing – review & editing: Woo Yong Lee, Ki Deok Park, Yongbum Park.
Footnotes
Abbreviations: HLD = herniated lumbar disc, MRI = magnetic resonance imaging, NRS = Numeric Rating Scale, PDRN = polydeoxyribonucleotide sodium, TFESI = transforaminal epidural steroid injection, US = ultrasonography.
WYL and KDP contributed equally to this work as first authors.
The authors have no conflicts of interest to disclose.
References
- [1].Yabuki S, Fukumori N, Takegami M, et al. Prevalence of lumbar spinal stenosis, using the diagnostic support tool, and correlated factors in Japan: a population-based study. J Orthop Sci 2013;18:893–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Huston CW, Slipman CW. Diagnostic selective nerve root blocks: indications and usefulness. Phys Med Rehabil Clin N Am 2002;13:545–65. [DOI] [PubMed] [Google Scholar]
- [3].Suen M, Fung B, Lung CP. Treatment of ganglion cysts. ISRN Orthop 2013;2013:940615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Kazanci B, Tehli O, Turkoglu E, et al. Bilateral thoracic ganglion cyst: a rare case report. J Korean Neurosurg Soc 2013;53:309–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kim SW, Choi JH, Kim MS, et al. A ganglion cyst in the second lumbar intervertebral foramen. J Korean Neurosurg Soc 2011;49:237–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Soren A. Pathogenesis, clinic, and treatment of ganglion. Arch Orthop Traum Surg 1982;99:247–52. [DOI] [PubMed] [Google Scholar]
- [7].Pasieka AM, Rafacho A. Impact of glucocorticoid excess on glucose tolerance: clinical and preclinical evidence. Metabolites 2016;6:E24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Kang KN, Kim TW, Koh JW, et al. Effect of transforaminal epidural polydeoxyribonucleotide injections on lumbosacral radiculopathy: A case report. Medicine (Baltimore) 2017;96:e7174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kim JY, Pak CS, Park JH, et al. Effects of polydeoxyribonucleotide in the treatment of pressure ulcers. J Korean Med Sci 2014;29:222–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kreiner DS, Hwang SW, Easa JE, et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J 2014;14:180–91. [DOI] [PubMed] [Google Scholar]
- [11].Kreiner DS, Shaffer WO, Baisden JL, et al. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update). Spine J 2013;13:734–43. [DOI] [PubMed] [Google Scholar]
- [12].Spinner RJ, Hébert-Blouin MN, Tanaka S, et al. Hip- and pelvic-related intraneural ganglia. J Neurosurg 2010;112:1353–6. [DOI] [PubMed] [Google Scholar]
- [13].Kalaci A, Dogramaci Y, Sevinç TT, et al. Femoral nerve compression secondary to a ganglion cyst arising from a hip joint: a case report and review of the literature. J Med Case Rep 2009;3:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Campeas S, Rafii M. Pelvic presentation of a hip joint ganglion a case report. Bull Hosp Jt Dis 2002-2003;61:89–92. [PubMed] [Google Scholar]
- [15].Lee JW, Lee SM, Lee DG. Pudendal nerve entrapment syndrome due to a ganglion cyst: a case report. Ann Rehabil Med 2016;40:741–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Park JH, Jeong HJ, Shin HK, et al. Piriformis ganglion: an uncommon cause of sciatica. Orthop Traumatol Surg Res 2016;102:257–60. [DOI] [PubMed] [Google Scholar]
- [17].Squadrito F, Bitto A, Irrera N, et al. Pharmacological activity and clinical use of PDRN. Front Pharmacol 2017;8:224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Veronesi F, Dallari D, Sabbioni G, et al. Polydeoxyribonucleotides (PDRNs) from skin to musculoskeletal tissue regeneration via adenosine A2A receptor involvement. J Cell Physiol 2017;232:2299–307. [DOI] [PubMed] [Google Scholar]
- [19].Kim WJ, Shin HY, Koo GH, et al. Ultrasound-guided prolotherapy with polydeoxyribonucleotide sodium in ischiofemoral impingement syndrome. Pain Pract 2014;14:649–55. [DOI] [PubMed] [Google Scholar]
- [20].Lim TH, Cho HR, Kang KN, et al. The effect of polydeoxyribonucleotide prolotherapy on posterior tibial tendon dysfunction after ankle syndesmotic surgery: A case report. Medicine (Baltimore) 2016;95:e5346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Yoon YC, Lee DH, Lee MY, et al. Polydeoxyribonucleotide injection in the treatment of chronic supraspinatus tendinopathy: a case-controlled, retrospective, comparative study with 6-month follow-up. Arch Phys Med Rehabil 2017;98:874–80. [DOI] [PubMed] [Google Scholar]


