Abstract
Introduction:
The effect of high-flow nasal cannula (HFNC) on adult post cardiothoracic operation remains controversial. We conducted a meta-analysis of randomized controlled trials to evaluate the effect of HFNC and conventional oxygen therapy (COT) on postcardiothoracic surgery.
Methods:
A search was conducted in Embase, MEDLINE, Ovid, and Cochrane databases until December, 2017 for all the controlled study to compare HFNC with COT in adult postcardiothoracic surgery. Two authors extracted data and assessed the quality of each study independently. The meta-analysis was performed by using RevMan 5.3. The primary outcome was the rate of escalation of respiratory support rate and pulmonary complications; secondary outcome included the length of intensive care unit (ICU) stay and length of hospital stay and the rate of intubation.
Results:
Four studies that involved 649 patients were included in the analysis. No significant heterogeneity was found in outcome measures. Compared with COT, HFNC were associated with a significant reduction in the escalation of respiratory support (odds ratio [OR] = 0.44, 95% confidence interval [CI] = 0.29−0.66, P < .001) and pulmonary complications (OR = 0.28, 95% CI = 0.13−0.6, P = .001). There were no significant differences in the reintubation rate (OR = 0.33, 95% CI = 0.02−5.39, P = .43), length of ICU stay (weighted mean difference = 0.11; 95% CI = −0.44 −0.26, P = .14) or length of hospital stay (weighted mean difference = −0.15, 95% CI = −0.46 −0.17, P = .36) between the 2 groups. No severe complications were reported in either group.
Conclusion:
The HFNC could reduce respiratory support and pulmonary complications, and it could be safely administered for adult postcardiothoracic surgery. Further large-scale, randomized, and controlled trials are needed to update this finding.
Keywords: cardiothoracic surgery, high-flow nasal cannula, meta-analysis, oxygen therapy
1. Introduction
High-flow nasal cannula (HFNC) oxygen therapy as a new model of respiratory support is more and more widely used in clinical and various fields. HFNC therapy can deliver up to 100% heated and humidified oxygen via a wide-bore nasal cannula at a very high-flow rate of 60 L/min.[1–3] Compared with conventional oxygen therapy (COT), HFNC has several advantages: to produce positive airway pressure[4] and reduce the anatomical dead space[5]; to produce a predictable sustained partial pressure of oxygen (FiO2)[6]; to increase oxygenation (PaO2/FiO2) and reduce room oxygen dilution[1,7]; to improve mucociliary movements to remove sputum[2,8]; to reduce the upper airway resistance and breathing work,[9] increase the coordination of chest, and abdomen movement.[10,11] Some studies demonstrate that HFNC can improve comfort and oxygenation,[12–14] and alleviate dyspnea.[15] For these advantages, HFNC has been proven to be a safe and effective treatment for acute respiratory failure (RF) for adults.[16–19]
So far, clinical experience about the effect of HFNC on postcardiothoracic patients is little. Patients undergoing cardiothoracic surgery are at significant risk of postoperative pulmonary complications. These complications may increase morbidity and mortality, and lead to longer period to stay in intensive care unit (ICU) and hospital.[20] It is reported that the incidence of pulmonary complications after cardiac surgery ranges is from 8% to 79%.[21] HFNC significantly also reduced the rate of reintubation.[14] Thus, the purpose of this meta-analysis is to assess if HFNC can reduce the respiratory support, pulmonary complications, and period to stay in ICU and hospital.
2. Materials and methods
This study was conducted according to Cochrane Handbook for Systematic Reviews of Interventions. Results followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.[8] This study was approved by the ethic committee from the First Affiliated Hospital of Xi’an Medical University (FAHXMU).
2.1. Search strategy and selection criteria
A comprehensive computer search was conducted in Embase, MEDLINE, Ovid, and Cochrane Library databases inception up to December 2017. We used the keywords of “high-flow nasal cannula” or “high-flow oxygen therapy” or “nasal high-flow oxygen therapy” or “oxygen therapy” and “cardiac surgery” or “cardiothoracic surgery” or “thoracic surgery” or “lung-resection surgery” in different combinations for the searches.
Oxygen therapies included HFNC oxygen therapy, COT. HFNC oxygen therapy was described as the delivery of oxygen through a heated humidifier and nasal cannula at a flow rate >15 L/min. COT can be delivered using low-flow devices (up to 15 L/min) such as nasal cannulas, or masks.
After removing duplicates, full-text articles were reviewed if they met the following criteria: randomized controlled trials (RCTs) or randomized controlled prospective trials; patients were divided into HFNC and COT groups; adult patients after cardiothoracic surgery (including cardiac, thoracic, lung surgery); one of the following outcomes: respiratory escalation therapy; ICU stay time; length of hospitalization time; pulmonary complications; reintubation rate.
2.2. Data extraction and risk of bias assessment
Each eligible study was enrolled and data extraction were included author, year of publication, patient grouping, number of subjects, methods of oxygen delivery, the way of respiratory support, ICU stay time, length of hospitalization time, pulmonary complications, and reintubation rate.
Two investigators assessed the quality of trials by using Cochrane collaboration risk of bias tool.[8] The following 7 assessment items was used to evaluate bias in each trial included the analysis: random sequence generation; allocation sequence concealment; blinding of participants and personnel; blinding of outcome assessment; completeness of outcome data; selective reporting, and other sources of bias, which were each graded as low, uncertain, or high risk of bias. Two reviewers made judgments independently. In cases of disagreement, resolution was first resolved by discussion and then by consulting a third author for arbitration.
2.3. Statistical analysis
The meta-analysis was performed using RevMan 5.3 software (RevMan 5.3; The Cochrane Collaboration, Oxford, United Kingdom) for data analysis. Heterogeneity between studies was evaluated using the Chi-squared test, and P-value of <.1with I2 > 50% indicated significant heterogeneity. We used the random effects model to calculate the results of both the binary and continuous data, regardless of statistical heterogeneity. Otherwise, fixed effects model was used. The results were graphically displayed using forest plots, and potential publication bias was analyzed by visual inspection of the funnel plot. For binary data such as reintubation rate were expressed as the odds ratio (OR) and 95% confidence intervals (CIs), and for continuous data such as length of ICU stays were expressed as the weighted mean differences (MDs) and 95% CIs. The results were expressed using P-values. P < .05 was considered statistically significant.
3. Results
From the literature search, 366 potentially eligible records were identified. After searching for duplicates, screening titles, and abstracts, we reviewed 14 records in full text, in which 10 studies were excluded. Two of these articles were published in children,[22,23] 2 were no relevant control group,[24,25] 1 lung transplant was not included our outcomes,[26] and 3 of the literature did not report the main outcome[27–29] and 2 trials were controlled studies of HFNC after abdominal surgery,[30,31] eventually 4 trials were enrolled in our final analysis.[32–35] The process for literature search and study selection is presented in Figure 1.
Figure 1.
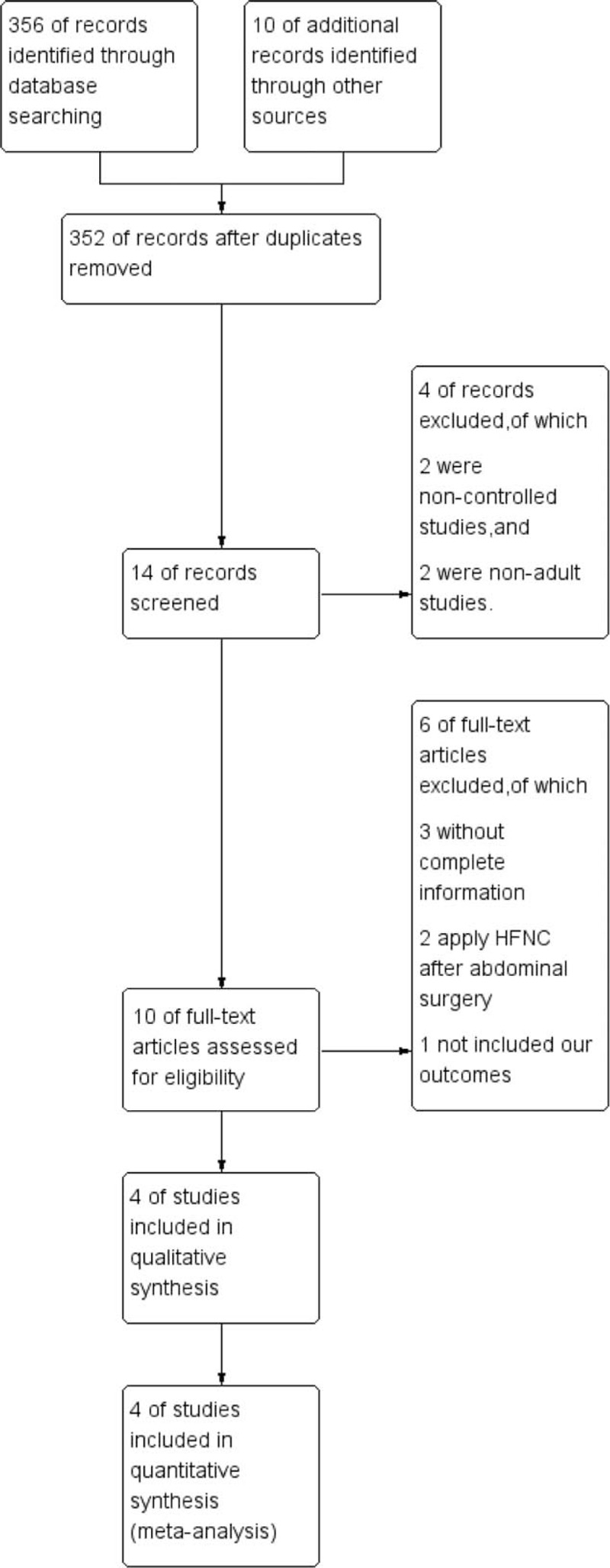
Flow diagram of literature search.
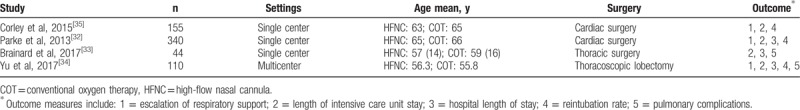
A total of 649 cardiothoracic surgical patients were involved in the present meta-analysis. Of these cases, 324 patients were randomly assigned to the HFNC group, and 325 patients were assigned to the COT group. The basic characteristics of all included patients are shown in Table 1.
Table 1.
The basic characteristics of the recruited patients.
3.1. Risk of bias of the included studies
The risk of each study bias and overall risk of bias were evaluated by using Cochrane collaboration risk of bias tool. The details of the results are presented in Figures 2 and 3.
Figure 2.
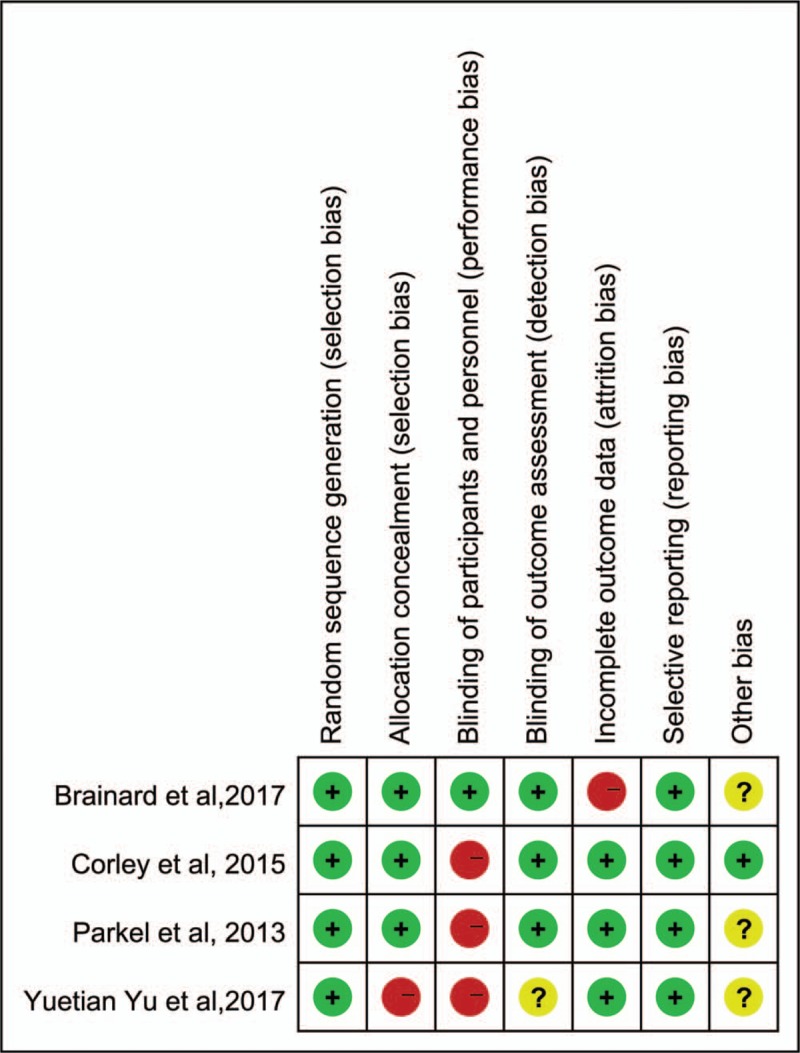
Summary of risk of bias. Red circles represent high risk of bias, green circles represent low risk of bias and yellow circles indicate represent unclear risk of bias.
Figure 3.
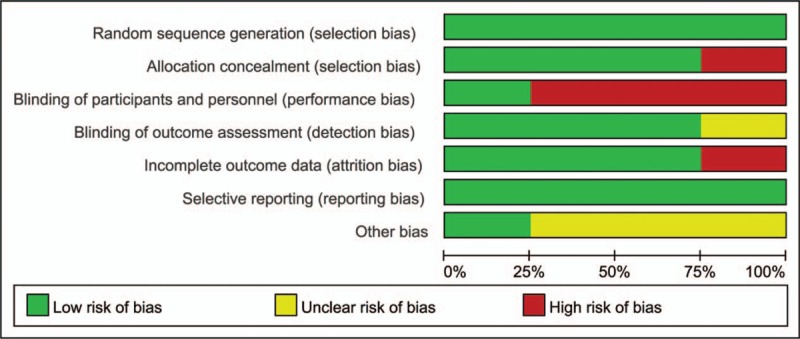
Overall risk of bias using the Cochrane risk of bias tool.
3.2. Escalation of respiratory support
A total of 3 studies reported the rate of escalation of respiratory support.[32,34,35] The escalation of respiratory support in COT group is regarded as use of HFNC, NIV, or reintubation. The escalation of respiratory support in HFNC group is regarded as use of NIV or reintubation. There was a statistically significant difference (OR = 0.44, 95% CI = 0.29−0.66, P < .001) between HFNC and COT group. Compared with COT, HFNC can significantly reduce the need of respiratory support, which with less heterogeneity in each study (I2 = 0%) using a fixed-effect model for analysis (Fig. 4A).
Figure 4.
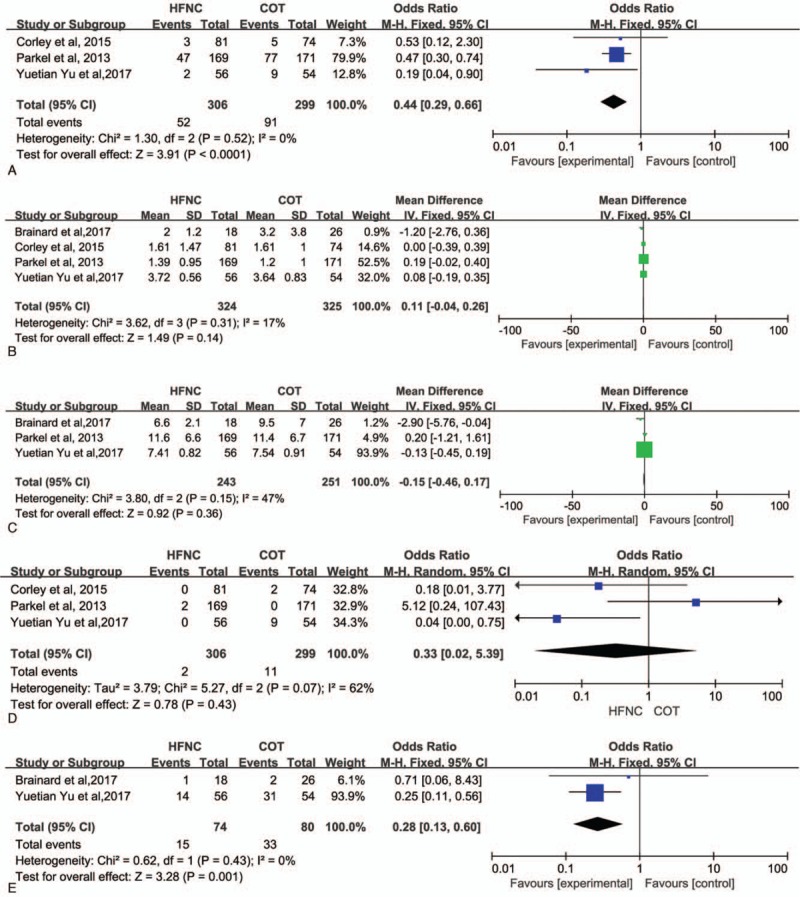
(A) Escalation of respiratory support of the high-flow nasal cannula and conventional oxygen therapy groups. (B) Length of intensive care unit stay of the high-flow nasal cannula and conventional oxygen therapy groups. (C) Length of hospital stay of the high-flow nasal cannula and conventional oxygen therapy groups. (D) Reintubation rates of the high-flow nasal cannula and conventional oxygen therapy groups. (E) Pulmonary complications rate of the high-flow nasal cannula and conventional oxygen therapy groups. COT = conventional oxygen therapy, HFNC = high-flow nasal cannula.
3.3. Length of ICU stay
All of the 4 studies reported the length of ICU stay.[32–35] There were no significant differences between HFNC and COT groups (weighted MD = 0.11; 95% CI = −0.44 −0.26; z = 1.49, P = .14). There was no significant heterogeneity (χ2 = 3.62, df = 3, P = .31; I2 = 17%) among the studies in Figure 4B.
3.4. Length of hospital stay
A total of 3 studies reported the length of hospital stay.[32–34] There were no significant differences between the HFNC and COT groups (weighted MD = −0.15, 95% CI = −0.46 −0.17, z = 0.92, P = .36). There was no significant heterogeneity (χ2 = 3.8, df = 2, P = .15; I2 = 47%) among the studies in Figure 4C.
3.5. Reintubation rate
Three studies reported a reintubation rate.[32,34,35] There was no significant difference in reintubation rate between HFNC and COT groups (OR = 0.33, 95% CI = 0.02−5.39, P = .43, Fig. 4D). A significant heterogeneity was observed between the 3 included studies (χ2 = 5.27, df = 2, P = .07; I2 = 62%).
3.6. Pulmonary complications
Two studies reported pulmonary complications,[33,34] such as atelectasis, suspected pneumonia, hypoxemia, and hypercapnia. There was significant difference in pulmonary complications between 2 groups (OR = 0.28, 95% CI = 0.13−0.6, P = .001, Fig. 4E). No significant heterogeneity was observed between 2 included studies (χ2 = 0.62, df = 1, P = .43; I2 = 0%).
4. Discussion
The HFNC has been used in various clinical fields as a noninvasive method and meets the patients for all age, such as infants, children, and adults. It has been used for multiple indications, including hypoxemic RF, immunocompromised patients with acute RF, cardiogenic pulmonary edema, and prophylactic therapy for RF after surgery and extubation.[8] In addition, HFNC has also been used in ARDS[36] and OSA.[37,38]
Corley et al[29] reported HFNC could reduce respiratory rate and improve oxygenation by increasing both EELV and tidal volume for postcardiac surgical patients firstly. Furthermore, HFNC are most beneficial for patients with higher body mass indexes. Then Parke et al[32] found that HFNC did not significantly increase SpO2/FiO2 ratio, but reduced the requirement for escalation of respiratory support after cardiac surgery. Recently, more and more studies focus on the effect of HFNC on postcardiac surgical patients. Our study shows HFNC can reduce the need of respiratory support and pulmonary complications.
Although high-quality trials and rigorous methodology are adopted, our study has still several limitations. Firstly, only 4 trials are analyzed and sample is not too large in 2 trials (n < 110).[33,34] The ratio of sample between experimental group and control group in 2 trials is close to 1:1, and the design of control group is reasonable. The weight of these 2 studies is important in the meta-analysis. Clinical heterogeneity is also limited to current data. Temporary heterogeneity cannot be reduced by subgroup analysis. Secondly, we involve the patients with various conditions (age, weight, type of operation, postoperative extubation, oxygen therapy equipment), which will affect the reliability of conclusions and the strength of evidence. In addition, articles enrolled are published in English, which may lead to a certain publication bias.
The funnel plot may not detect the publication bias when sample is not enough large and also shows an essential inherent difference between large sample and small sample because of heterogeneity. If more clinical trials are available in future, the meta-analysis needs to be updated in time.
In summary, HFNC has the advantages of reducing the need of respiratory support and pulmonary complications after adult cardiothoracic surgery compared with COT. Previous studies have confirmed that HFNC has obvious advantages of comfort and convenience,[39,40] thus HFNC can be used clinically as a respiratory support option for adults cardiothoracic surgery. However, due to the strength of evidence and few available clinical studies, HFNC is still enough not to be a clinical recommendation, and needs to be confirmed by a multicenter randomized controlled trial. More clinical trials on HFNC in postcardiothoracic surgery are expected to be conducted.
5. Conclusion
The HFNC could reduce respiratory support and pulmonary complications, and it could be safely administered for adult postcardiothoracic surgery. Further large-scale, randomized, and controlled trials are needed to update this finding.
Acknowledgment
The authors express gratitude to the study participants and research personnel for their involvement in the study.
Author contributions
WSY is responsible for study design, literature search and manuscript preparation. WX is responsible for collection and analysis of data. CW is responsible for data collection. ZB is responsible for analysis of data.
Conceptualization: Xiu Wu, Bin Zhang.
Supervision: Shengyu Wang.
Writing – original draft: Xiu Wu, Wei Cao.
Footnotes
Abbreviations: ARDS = acute respiratory distress syndrome, BMI = body mass index, CI = confidence interval, COT = conventional oxygen therapy, HFNC = high-flow nasal cannula, ICU = intensive care unit, NIV = noninvasive ventilation, OR = odds ratio, OSA = obstructive sleep apnea, RF = respiratory failure.
This study was supported by funds from Respiratory Prevention and Treatment Center of Shaanxi Provincial Government (2016HXKF09), Shaanxi Province Key Program Fund (2017SF-256).
The authors have no conflicts of interest to disclose.
References
- [1].Sotello D, Rivas M, Mulkey Z, et al. High-flow nasal cannula oxygen in adult patients: a narrative review. Am J Med Sci 2015;349:179–85. [DOI] [PubMed] [Google Scholar]
- [2].Spoletini G, Alotaibi M, Blasi F, et al. Heated humidified high-flow nasal oxygen in adults: mechanisms of action and clinical implications. Chest 2015;148:253–61. [DOI] [PubMed] [Google Scholar]
- [3].Nishimura M. High-flow nasal cannula oxygen therapy in adults: physiological benefits, indication, clinical benefits, and adverse effects. Respir Care 2016;61:529–41. [DOI] [PubMed] [Google Scholar]
- [4].Parke R, McGuinness S, Eccleston M. Nasal high-flow therapy delivers low level positive airway pressure. Br J Anaesth 2009;103:886–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Dysart K, Miller TL, Wolfson MR, et al. Research in high flow therapy: mechanisms of action. Respir Med 2009;103:1400–5. [DOI] [PubMed] [Google Scholar]
- [6].Wagstaff TA, Soni N. Performance of six types of oxygen delivery devices at varying respiratory rates. Anaesthesia 2007;62:492–503. [DOI] [PubMed] [Google Scholar]
- [7].Nishimura M. High-flow nasal cannula oxygen therapy in adults. J Intensive Care 2015;3:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Lee JH, Rehder KJ, Williford L, et al. Use of high flow nasal cannula in critically ill infants, children, and adults: a critical review of the literature. Intensive Care Med 2013;39:247–57. [DOI] [PubMed] [Google Scholar]
- [9].Cuquemelle E, Pham T, Papon JF, et al. Heated and humidified high-flow oxygen therapy reduces discomfort during hypoxemic respiratory failure. Respir Care 2012;57:1571–7. [DOI] [PubMed] [Google Scholar]
- [10].Itagaki T, Okuda N, Tsunano Y, et al. Effect of high-flow nasal cannula on thoraco-abdominal synchrony in adult critically ill patients. Respir Care 2014;59:70–4. [DOI] [PubMed] [Google Scholar]
- [11].Sztrymf B, Messika J, Bertrand F, et al. Beneficial effects of humidified high flow nasal oxygen in critical care patients: a prospective pilot study. Intensive care medicine 2011;37:1780–6. [DOI] [PubMed] [Google Scholar]
- [12].Roca O, Riera J, Torres F, et al. High-flow oxygen therapy in acute respiratory failure. Respir Care 2010;55:408–13. [PubMed] [Google Scholar]
- [13].Rittayamai N, Tscheikuna J, Rujiwit P. High-flow nasal cannula versus conventional oxygen therapy after endotracheal extubation: a randomized crossover physiologic study. Respir Care 2014;59:485–90. [DOI] [PubMed] [Google Scholar]
- [14].Maggiore SM, Idone FA, Vaschetto R, et al. Nasal high-flow versus Venturi mask oxygen therapy after extubation. Effects on oxygenation, comfort, and clinical outcome. Am J Respir Crit Care Med 2014;190:282–8. [DOI] [PubMed] [Google Scholar]
- [15].Lenglet H, Sztrymf B, Leroy C, et al. Humidified high flow nasal oxygen during respiratory failure in the emergency department: feasibility and efficacy. Respir Care 2012;57:1873–8. [DOI] [PubMed] [Google Scholar]
- [16].Ricard JD. High flow nasal oxygen in acute respiratory failure. Minerva Anestesiol 2012;78:836–41. [PubMed] [Google Scholar]
- [17].Rello J, Perez M, Roca O, et al. High-flow nasal therapy in adults with severe acute respiratory infection: a cohort study in patients with 2009 influenza A/H1N1v. J Crit Care 2012;27:434–9. [DOI] [PubMed] [Google Scholar]
- [18].Sztrymf B, Messika J, Mayot T, et al. Impact of high-flow nasal cannula oxygen therapy on intensive care unit patients with acute respiratory failure: a prospective observational study. J Crit Care 2012;27:324.e9–13. [DOI] [PubMed] [Google Scholar]
- [19].Song HZ, Gu JX, Xiu HQ, et al. The value of high-flow nasal cannula oxygen therapy after extubation in patients with acute respiratory failure. Clinics (Sao Paulo) 2017;72:562–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Pasquina P, Merlani P, Granier JM, et al. Continuous positive airway pressure versus noninvasive pressure support ventilation to treat atelectasis after cardiac surgery. Anesth Analg 2004;99:1001–8. [DOI] [PubMed] [Google Scholar]
- [21].Wynne R, Botti M. Postoperative pulmonary dysfunction in adults after cardiac surgery with cardiopulmonary bypass: clinical significance and implications for practice. Am J Crit Care 2004;13:384–93. [PubMed] [Google Scholar]
- [22].Testa G, Iodice F, Ricci Z, et al. Comparative evaluation of high-flow nasal cannula and conventional oxygen therapy in paediatric cardiac surgical patients: a randomized controlled trial. Interact Cardiovasc Thorac Surg 2014;19:456–61. [DOI] [PubMed] [Google Scholar]
- [23].Shioji N, Iwasaki T, Kanazawa T, et al. Physiological impact of high-flow nasal cannula therapy on postextubation acute respiratory failure after pediatric cardiac surgery: a prospective observational study. J Intensive Care 2017;5:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Stephan F, Berard L, Rezaiguia-Delclaux S, et al. High-flow nasal cannula therapy versus intermittent noninvasive ventilation in obese subjects after cardiothoracic surgery. Respir Care 2017;62:1193–202. [DOI] [PubMed] [Google Scholar]
- [25].Stephan F, Barrucand B, Petit P, et al. High-flow nasal oxygen vs noninvasive positive airway pressure in hypoxemic patients after cardiothoracic surgery: a randomized clinical trial. JAMA 2015;313:2331–9. [DOI] [PubMed] [Google Scholar]
- [26].Roca O, de Acilu MG, Caralt B, et al. Humidified high flow nasal cannula supportive therapy improves outcomes in lung transplant recipients readmitted to the intensive care unit because of acute respiratory failure. Transplantation 2015;99:1092–8. [DOI] [PubMed] [Google Scholar]
- [27].Ansari BM, Hogan MP, Collier TJ, et al. A randomized controlled trial of high-flow nasal oxygen (optiflow) as part of an enhanced recovery program after lung resection surgery. Ann Thorac Surg 2016;101:459–64. [DOI] [PubMed] [Google Scholar]
- [28].Parke RL, McGuinness SP, Eccleston ML. A preliminary randomized controlled trial to assess effectiveness of nasal high-flow oxygen in intensive care patients. Respir Care 2011;56:265–70. [DOI] [PubMed] [Google Scholar]
- [29].Corley A, Caruana LR, Barnett AG, et al. Oxygen delivery through high-flow nasal cannulae increase end-expiratory lung volume and reduce respiratory rate in post-cardiac surgical patients. Br J Anaesth 2011;107:998–1004. [DOI] [PubMed] [Google Scholar]
- [30].Tu G, He H, Yin K, et al. High-flow nasal cannula versus noninvasive ventilation for treatment of acute hypoxemic respiratory failure in renal transplant recipients. Transplant Proc 2017;49:1325–30. [DOI] [PubMed] [Google Scholar]
- [31].Futier E, Paugam-Burtz C, Godet T, et al. Effect of early postextubation high-flow nasal cannula vs conventional oxygen therapy on hypoxaemia in patients after major abdominal surgery: a French multicentre randomised controlled trial (OPERA). Intensive Care Med 2016;42:1888–98. [DOI] [PubMed] [Google Scholar]
- [32].Parke R, McGuinness S, Dixon R, et al. Open-label, phase II study of routine high-flow nasal oxygen therapy in cardiac surgical patients. Br J Anaesth 2013;111:925–31. [DOI] [PubMed] [Google Scholar]
- [33].Brainard J, Scott BK, Sullivan BL, et al. Heated humidified high-flow nasal cannula oxygen after thoracic surgery - a randomized prospective clinical pilot trial. J Crit Care 2017;40:225–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Yu Y, Qian X, Liu C, et al. Effect of high-flow nasal cannula versus conventional oxygen therapy for patients with thoracoscopic lobectomy after extubation. Can Respir J 2017;2017:7894631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Corley A, Bull T, Spooner AJ, et al. Direct extubation onto high-flow nasal cannulae post-cardiac surgery versus standard treatment in patients with a BMI ≥30: a randomised controlled trial. Intensive Care Med 2015;41:887–94. [DOI] [PubMed] [Google Scholar]
- [36].Messika J, Ben Ahmed K, Gaudry S, et al. Use of high-flow nasal cannula oxygen therapy in subjects with ARDS: a 1-year observational study. Respir Care 2015;60:162–9. [DOI] [PubMed] [Google Scholar]
- [37].Hawkins S, Huston S, Campbell K, et al. High-flow, heated, humidified air via nasal cannula treats CPAP-intolerant children with obstructive sleep apnea. J Clin Sleep Med 2017;13:981–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Wu X, Cao W, Wang SY. High flow nasal cannula in obstructive sleep apnea hypopnea syndrome [in Chinese]. Zhonghua Jie He He Hu Xi Za Zhi 2017;49:712–4. [DOI] [PubMed] [Google Scholar]
- [39].Mikalsen IB, Davis P, Oymar K. High flow nasal cannula in children: a literature review. Scand J Trauma Resusc Emerg Med 2016;24:93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Frat JP, Brugiere B, Ragot S, et al. Sequential application of oxygen therapy via high-flow nasal cannula and noninvasive ventilation in acute respiratory failure: an observational pilot study. Respir Care 2015;60:170–8. [DOI] [PubMed] [Google Scholar]


